Case Studies are descriptive studies that are prepared









- Slides: 39
Case Studies are descriptive studies that are prepared for illustrating novel, unusual, or atypical features identified in patients in anesthesia practice and they potentially generate new research questions. In compliance with the Health Insurance Portability and Accountability Act (HIPPA) all patient data has been de-identified and every attempt has been made to ensure patient privacy and data security.
Acute Pericarditis and Urgent Pericardial Window: A Case Report Jessica Sadvari BSN, RN, SRNA
Objectives • Review structure and anatomy of the pericardium • Detail the physiological changes that occur with acute pericarditis and pericardial tamponade • Describe the anesthesia implications and management of acute pericarditis
Patient Background • • HPI: 26 y. o. viral pericarditis s/p influenza 176. 7 kg, 183 cm tall, BMI 53 Preop VS: HR: 79, BP: 149/87, RR: 32, Sp 02: 95% RA ASA: 4 E • • PMH: Morbid obesity No home medications No previous surgeries
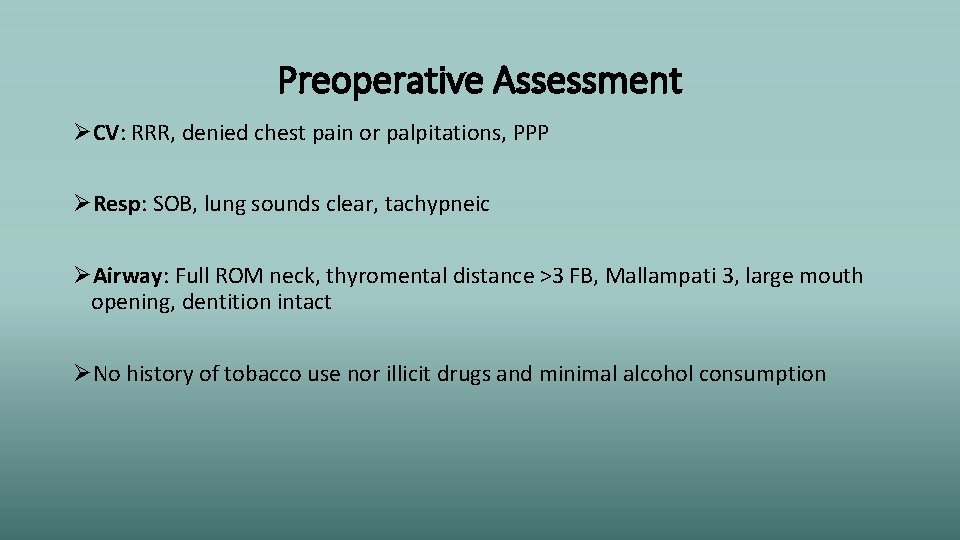
Preoperative Assessment ØCV: RRR, denied chest pain or palpitations, PPP ØResp: SOB, lung sounds clear, tachypneic ØAirway: Full ROM neck, thyromental distance >3 FB, Mallampati 3, large mouth opening, dentition intact ØNo history of tobacco use nor illicit drugs and minimal alcohol consumption
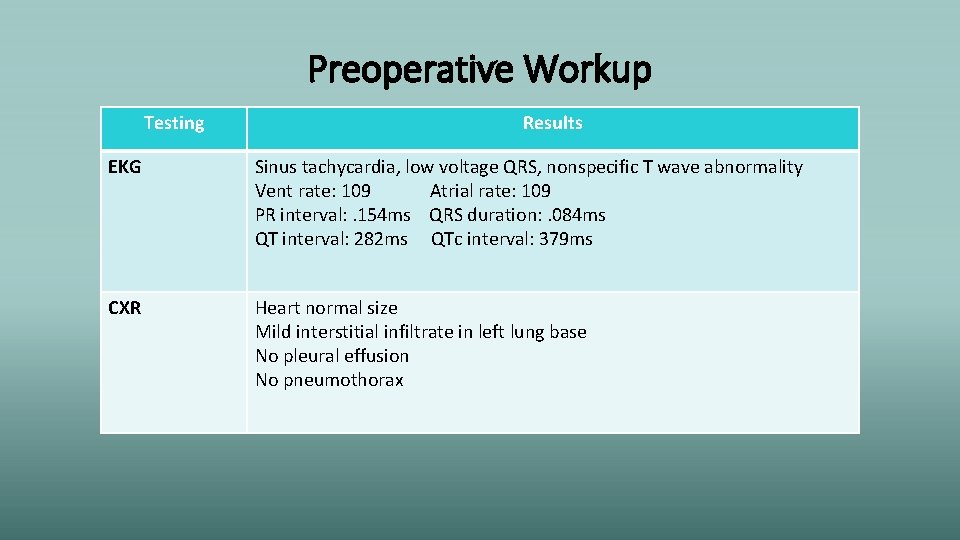
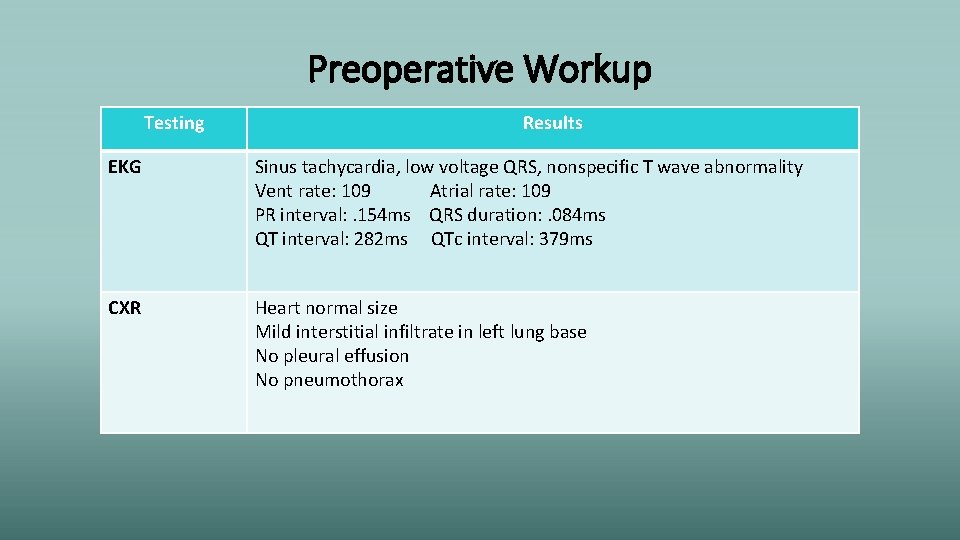
Preoperative Workup Testing Results EKG Sinus tachycardia, low voltage QRS, nonspecific T wave abnormality Vent rate: 109 Atrial rate: 109 PR interval: . 154 ms QRS duration: . 084 ms QT interval: 282 ms QTc interval: 379 ms CXR Heart normal size Mild interstitial infiltrate in left lung base No pleural effusion No pneumothorax

Preoperative Workup Testing ECHO Results Abnormal with early tamponade physiology LV: Size and function normal EF 55 -60% No regional wall motion abnormalities Wall thickness mildly increased Normal diastolic function RV: Systolic function normal, est. peak pressure 36 mm. Hg LA: mildly dilated MV & TV: mild regurgitation Pericardium: Large pericardial effusion circumferential to the heart No internal echoes Mild RV chamber collapse for <50% cardiac cycle Mild LA chamber collapse for >50% cardiac cycle
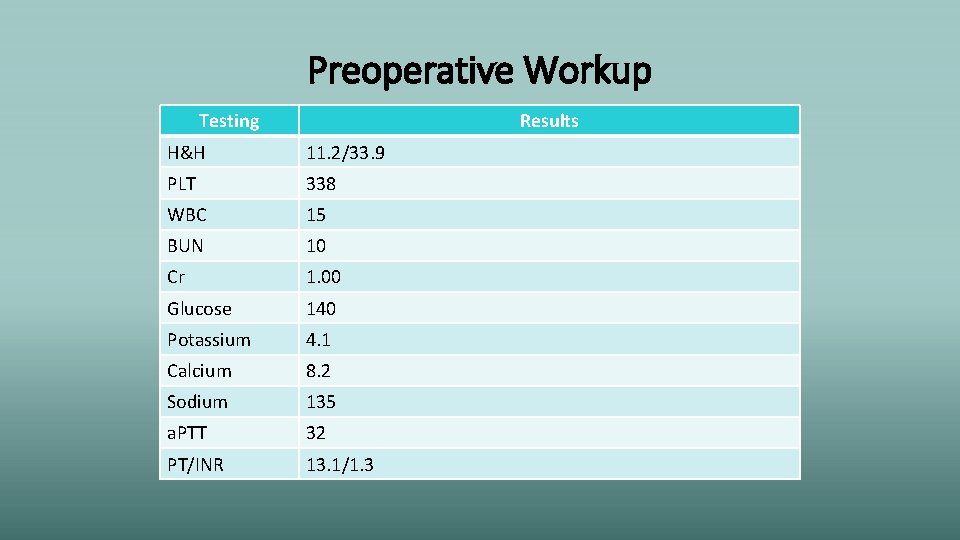
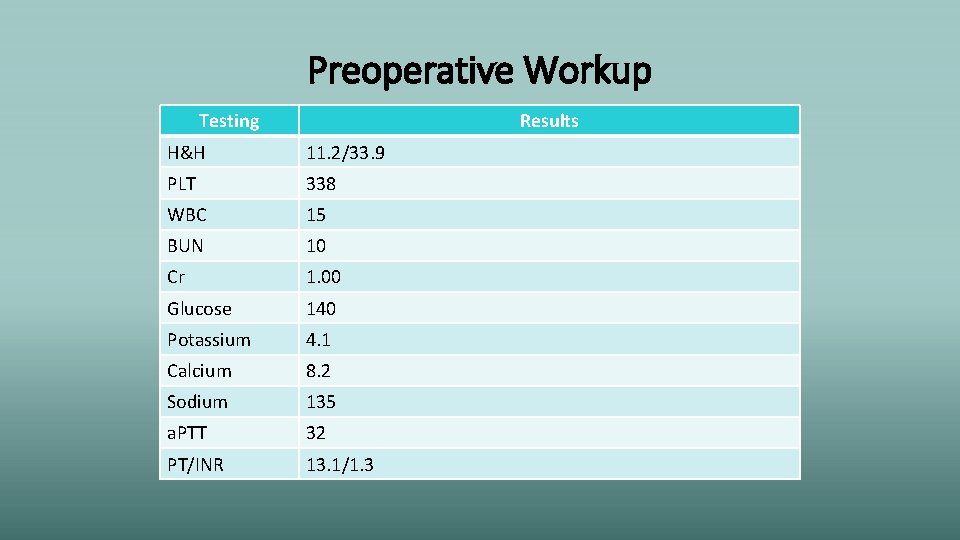
Preoperative Workup Testing Results H&H 11. 2/33. 9 PLT 338 WBC 15 BUN 10 Cr 1. 00 Glucose 140 Potassium 4. 1 Calcium 8. 2 Sodium 135 a. PTT 32 PT/INR 13. 1/1. 3
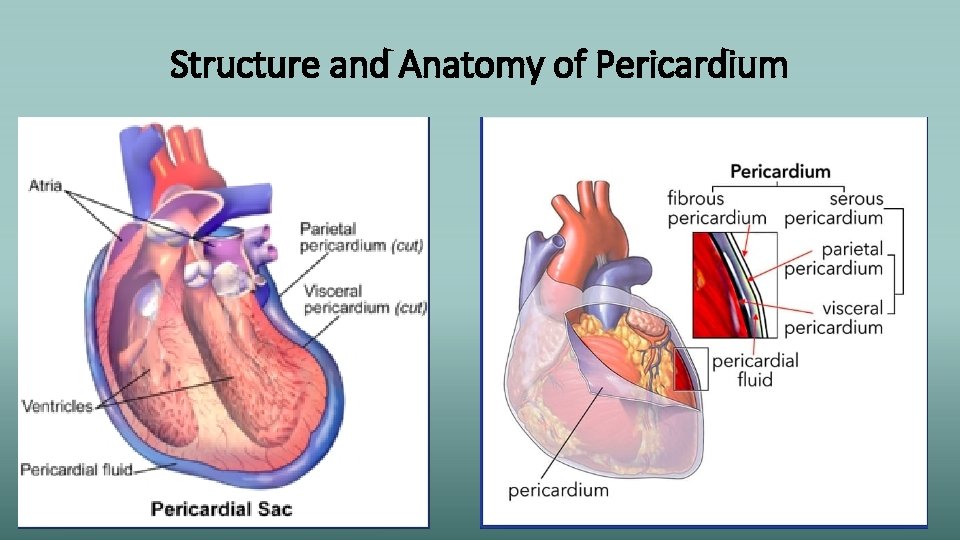
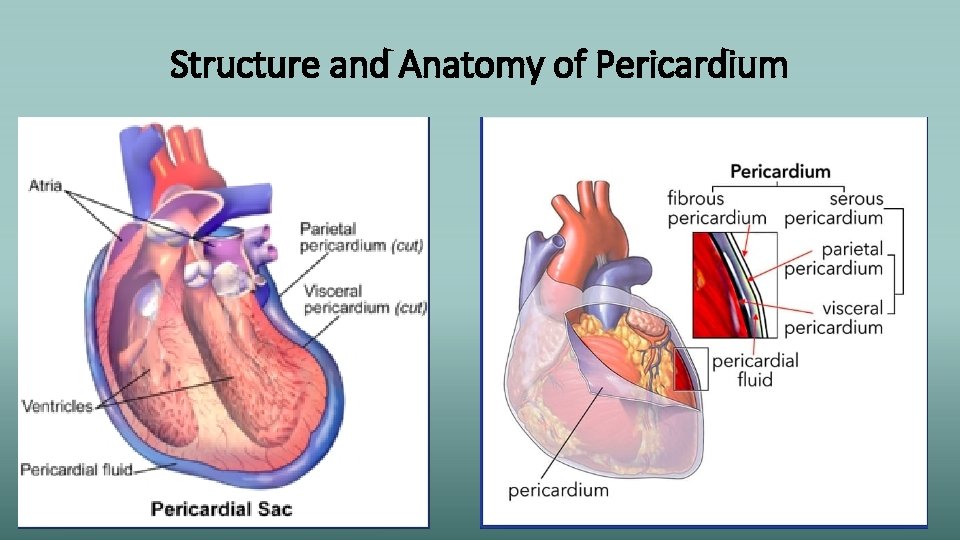
Structure and Anatomy of Pericardium

Structure and Anatomy of Pericardium (Elisha, 2014)
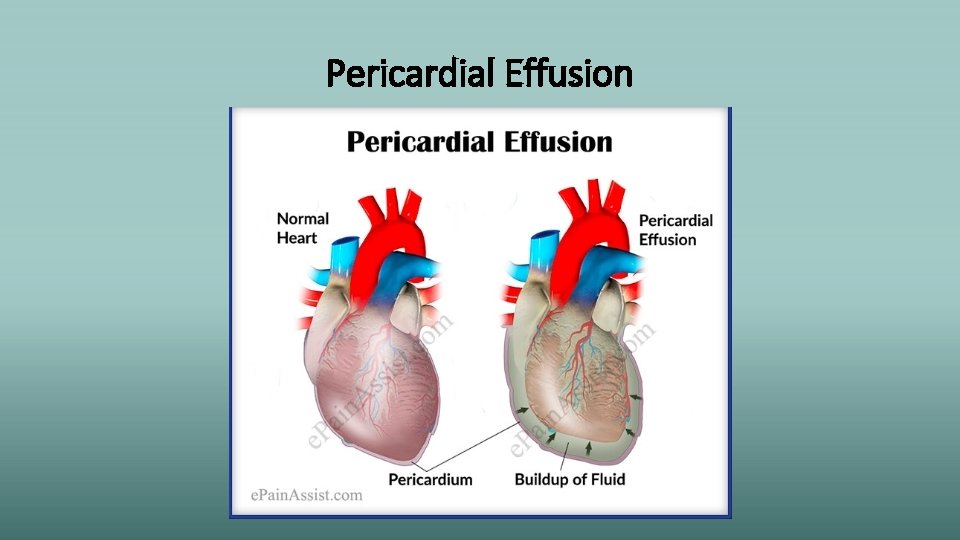
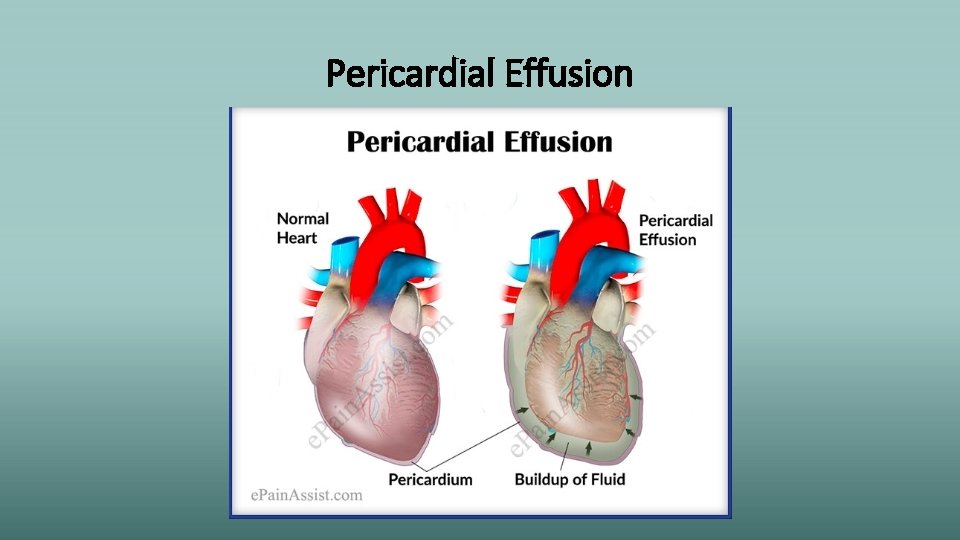
Pericardial Effusion
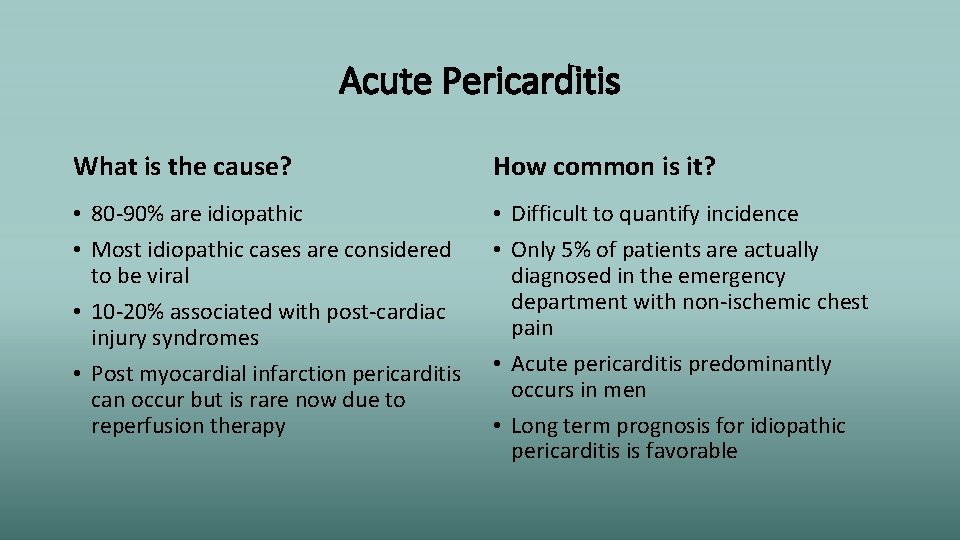
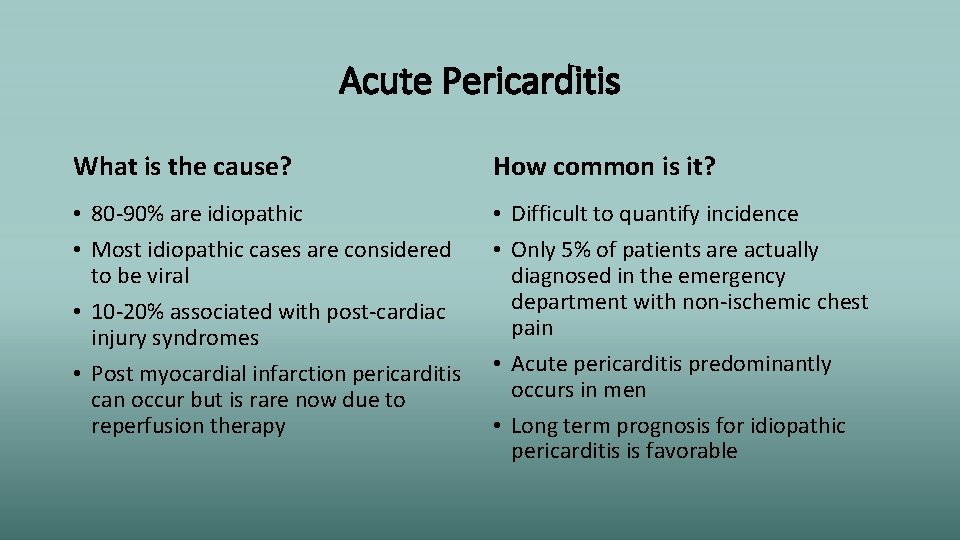
Acute Pericarditis What is the cause? How common is it? • 80 -90% are idiopathic • Most idiopathic cases are considered to be viral • 10 -20% associated with post-cardiac injury syndromes • Post myocardial infarction pericarditis can occur but is rare now due to reperfusion therapy • Difficult to quantify incidence • Only 5% of patients are actually diagnosed in the emergency department with non-ischemic chest pain • Acute pericarditis predominantly occurs in men • Long term prognosis for idiopathic pericarditis is favorable
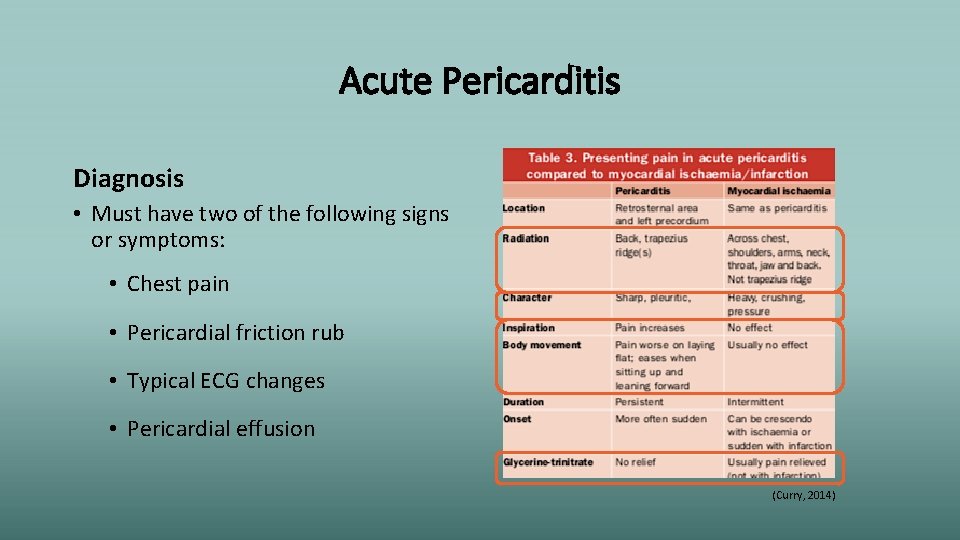
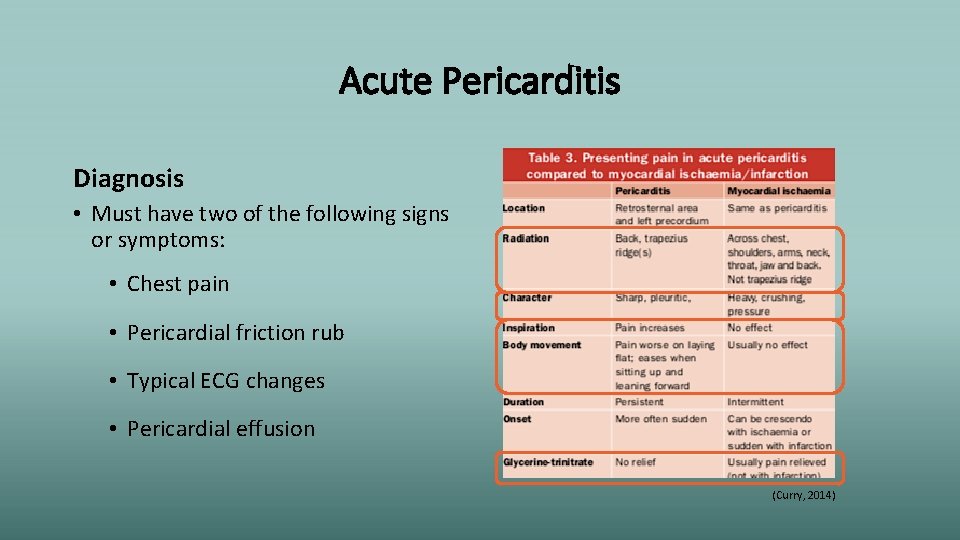
Acute Pericarditis Diagnosis • Must have two of the following signs or symptoms: • Chest pain • Pericardial friction rub • Typical ECG changes • Pericardial effusion (Curry, 2014)
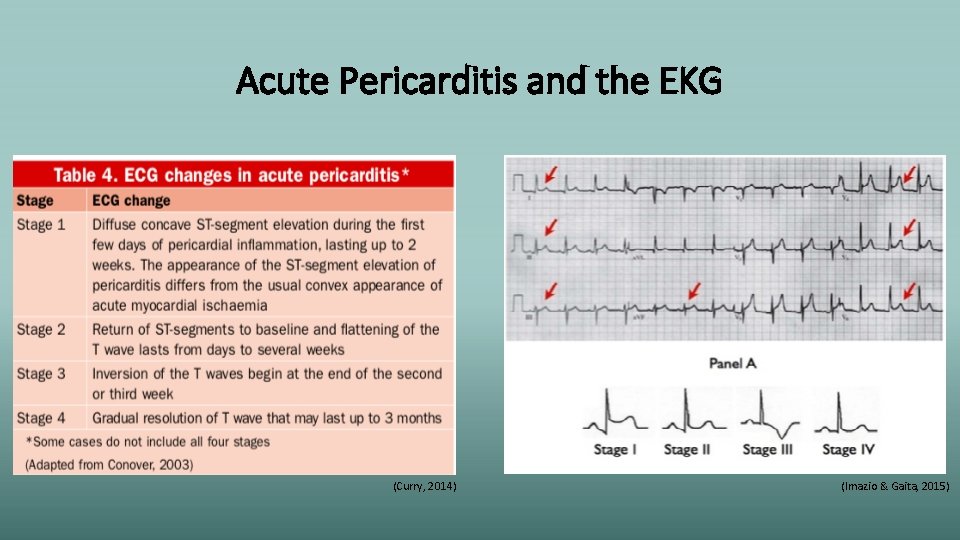
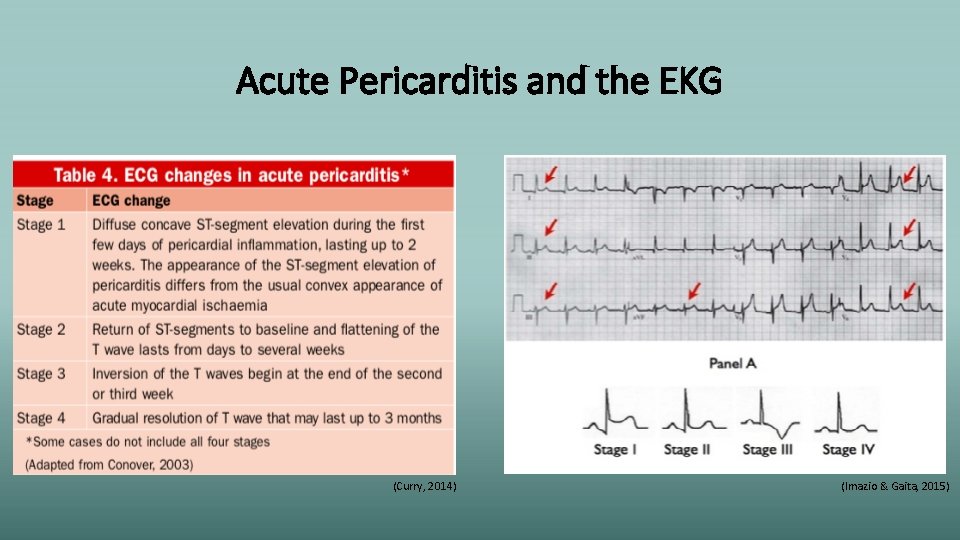
Acute Pericarditis and the EKG (Curry, 2014) (Imazio & Gaita, 2015)

Acute Pericarditis and the EKG (Curry, 2014)
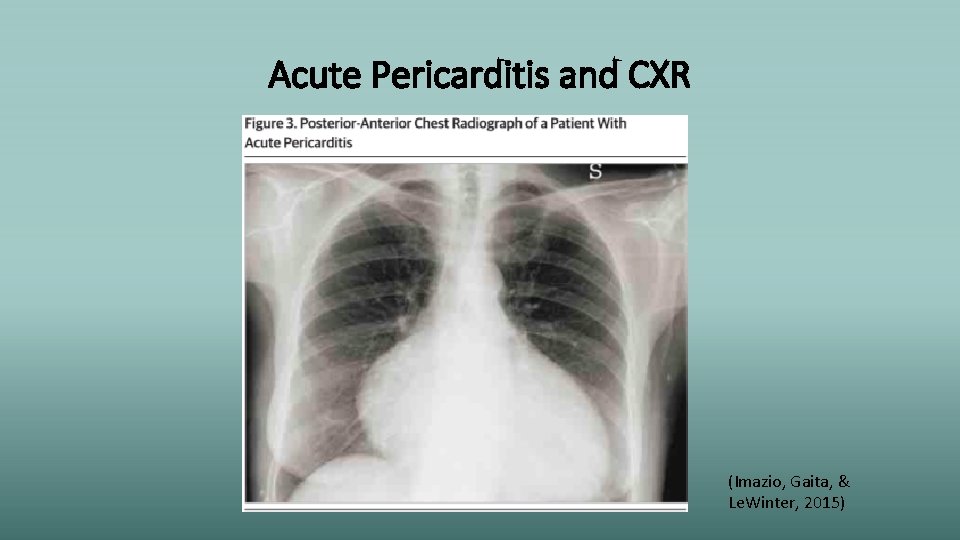
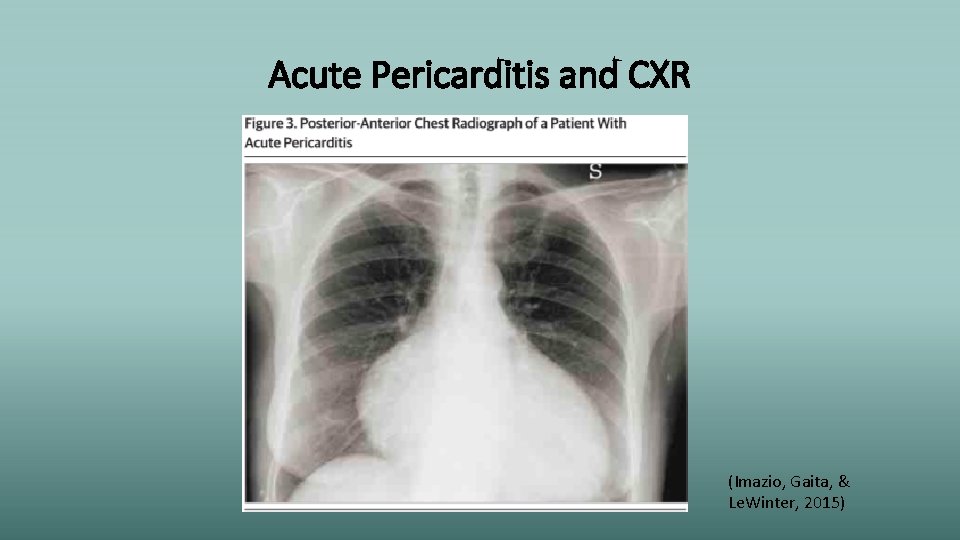
Acute Pericarditis and CXR (Imazio, Gaita, & Le. Winter, 2015)
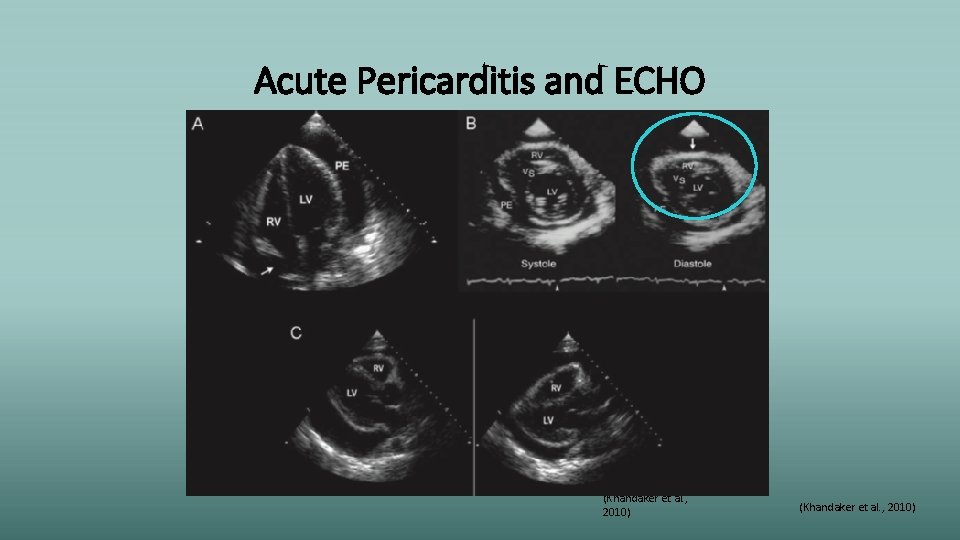
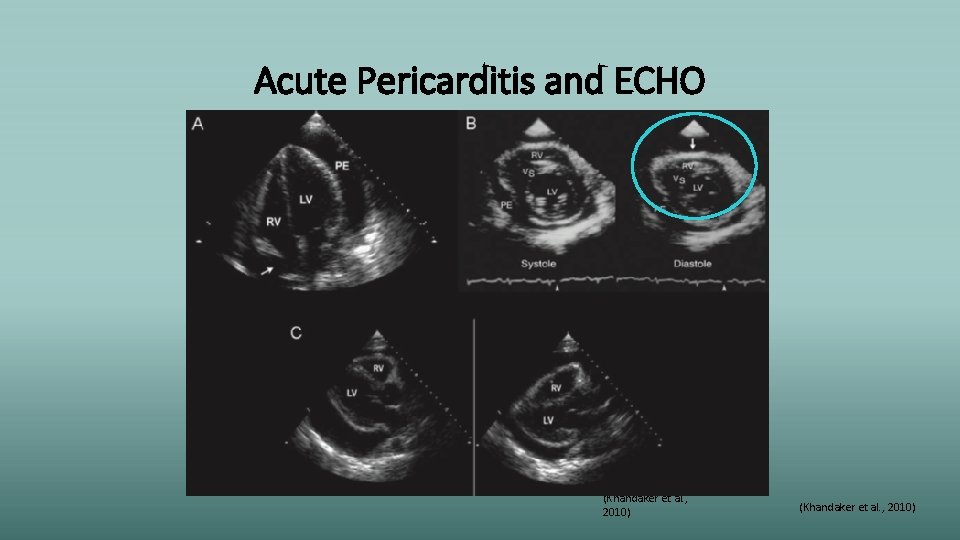
Acute Pericarditis and ECHO (Khandaker et al. , 2010)
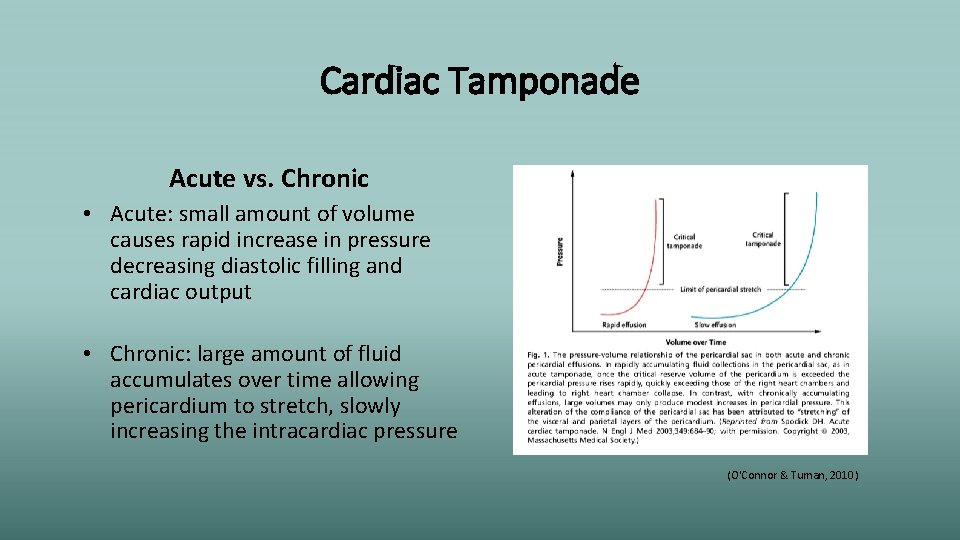
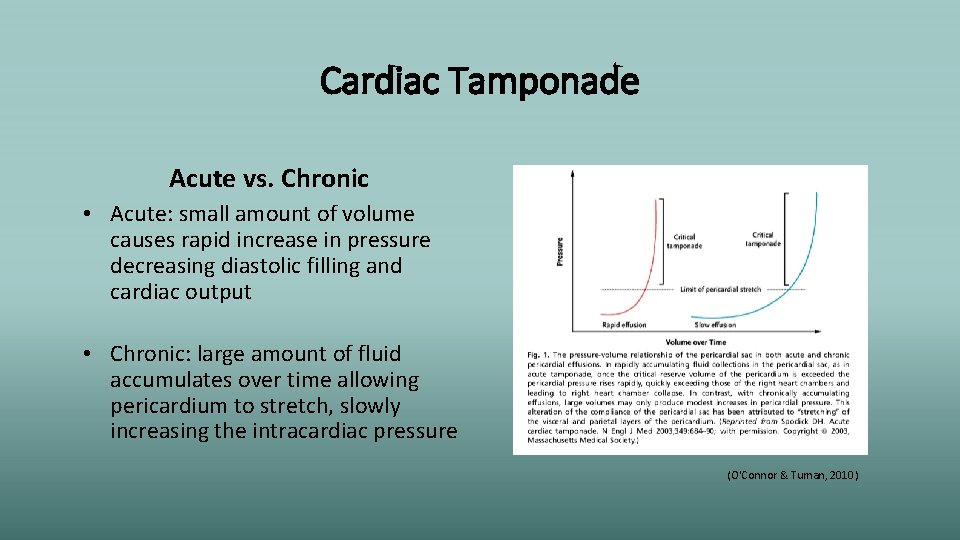
Cardiac Tamponade Acute vs. Chronic • Acute: small amount of volume causes rapid increase in pressure decreasing diastolic filling and cardiac output • Chronic: large amount of fluid accumulates over time allowing pericardium to stretch, slowly increasing the intracardiac pressure (O'Connor & Tuman, 2010)

Cardiac Tamponade Durand et al. (2009) (Khandaker et al. , 2010)
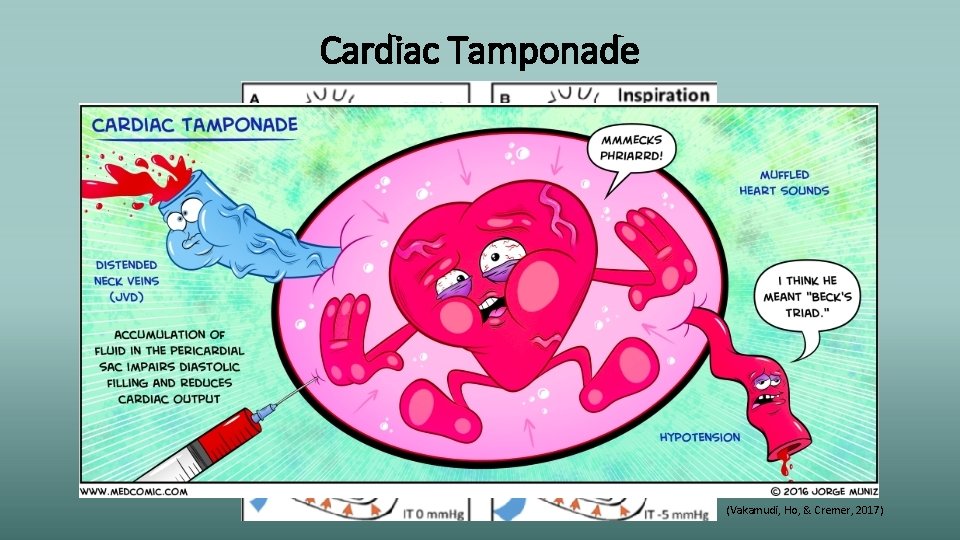
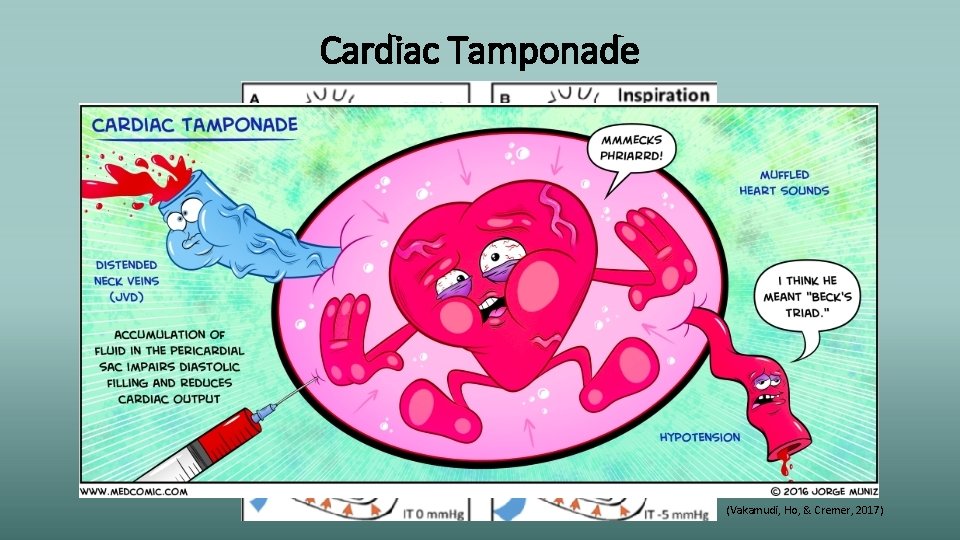
Cardiac Tamponade (Vakamudi, Ho, & Cremer, 2017)
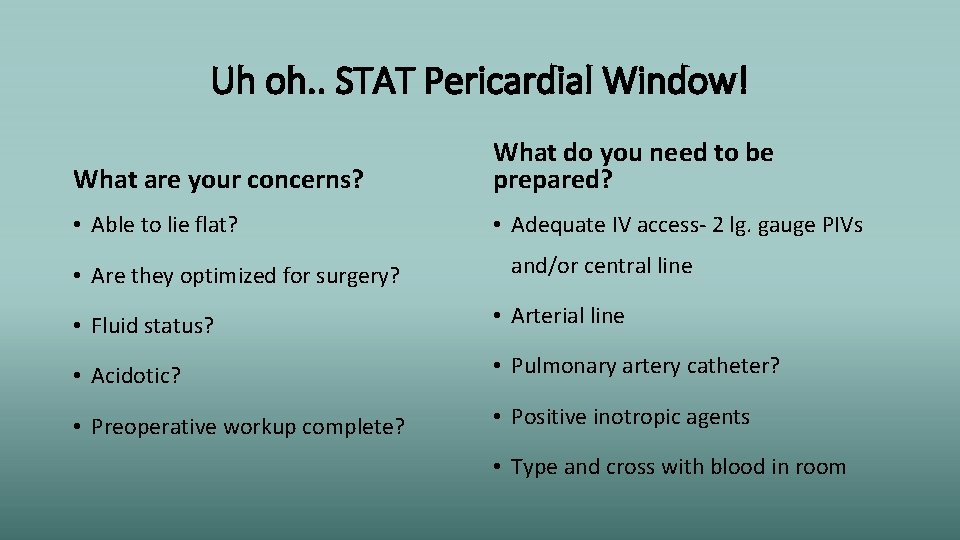
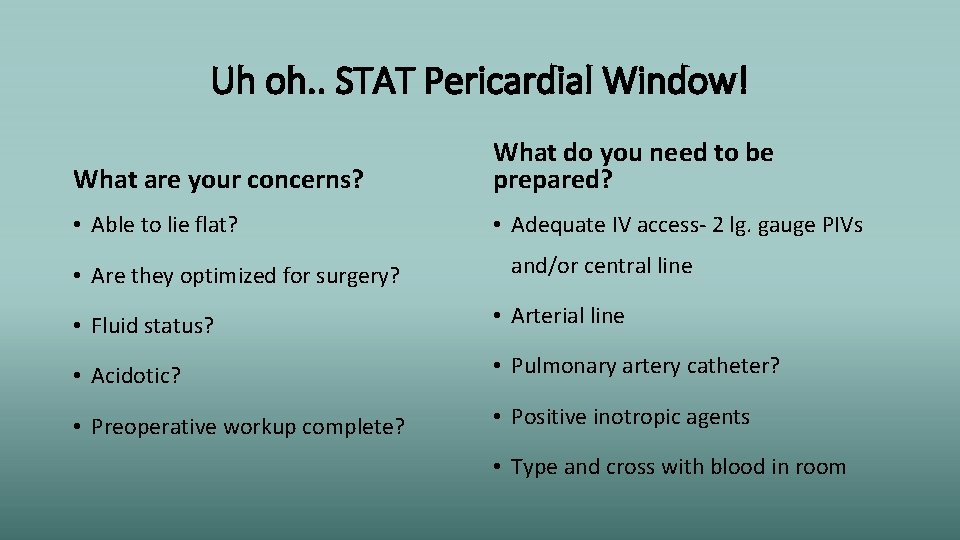
Uh oh. . STAT Pericardial Window! What are your concerns? What do you need to be prepared? • Able to lie flat? • Adequate IV access- 2 lg. gauge PIVs • Are they optimized for surgery? and/or central line • Fluid status? • Arterial line • Acidotic? • Pulmonary artery catheter? • Preoperative workup complete? • Positive inotropic agents • Type and cross with blood in room
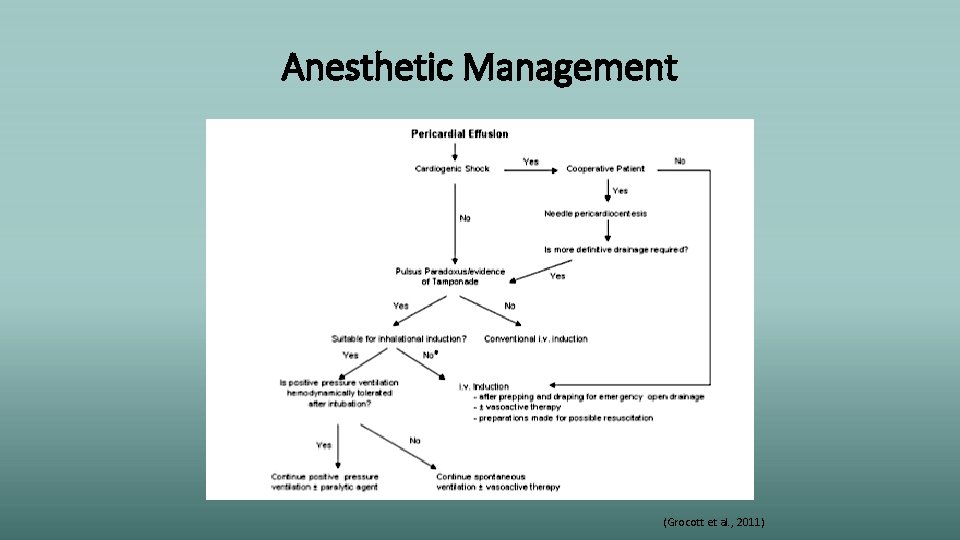
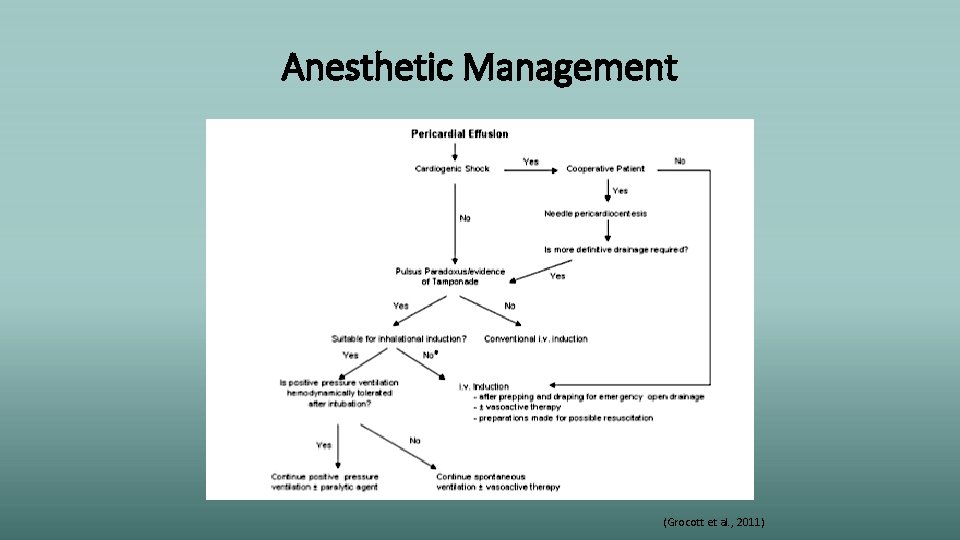
Anesthetic Management (Grocott et al. , 2011)

Pharmacologic Considerations • Ketamine: non-competitive NMDA-receptor antagonist, “dissociative anesthetic”, increases sympathetic outflow, indirect myocardial stimulation and direct myocardial depressant, preserves respiratory drive, increases salivation, profound analgesia • Etomidate: GABA-a agonist, with minimal cardiac depression and vasodilationuseful for HD stable induction, respiratory depression, adrenocorticoid suppression • Propofol: GABA-a agonist, most notably causes vasodilation and myocardial depression, depression of airway reflexes
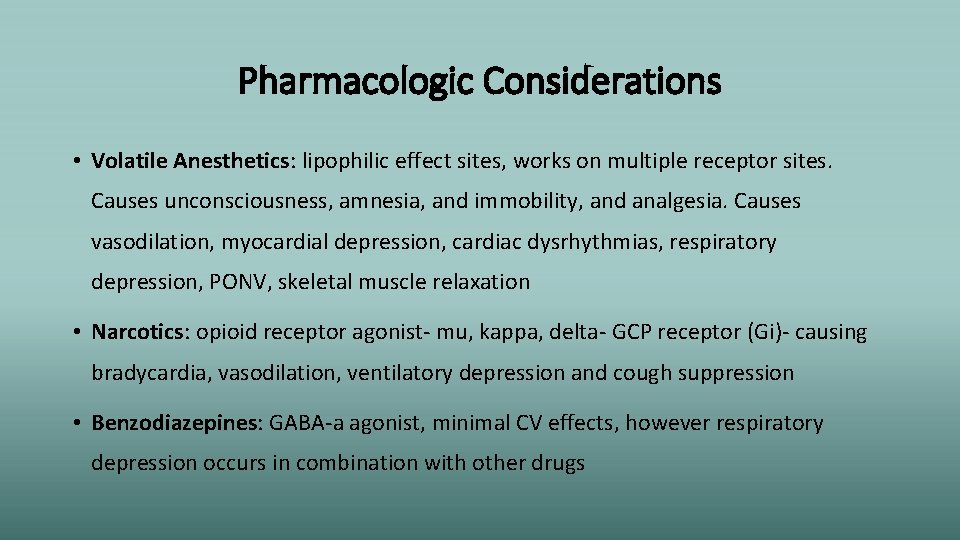
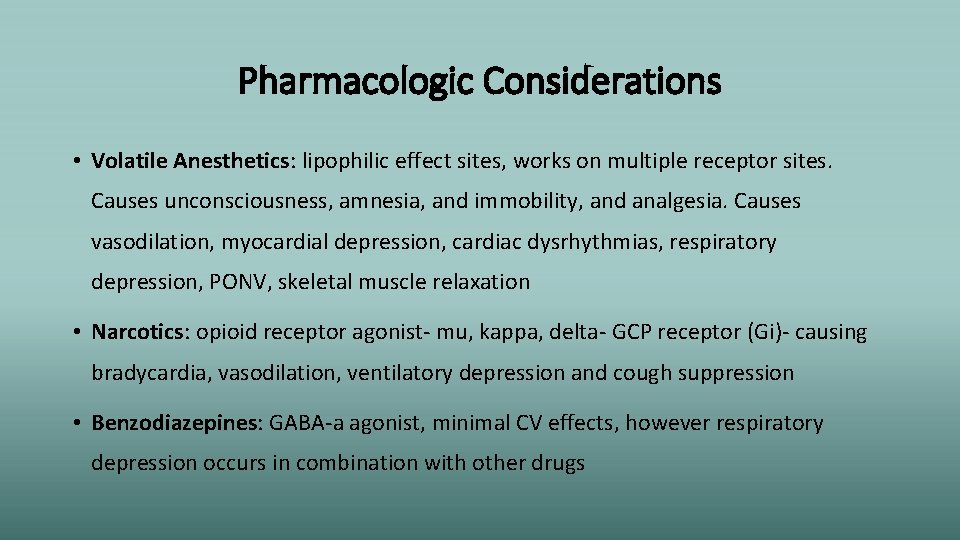
Pharmacologic Considerations • Volatile Anesthetics: lipophilic effect sites, works on multiple receptor sites. Causes unconsciousness, amnesia, and immobility, and analgesia. Causes vasodilation, myocardial depression, cardiac dysrhythmias, respiratory depression, PONV, skeletal muscle relaxation • Narcotics: opioid receptor agonist- mu, kappa, delta- GCP receptor (Gi)- causing bradycardia, vasodilation, ventilatory depression and cough suppression • Benzodiazepines: GABA-a agonist, minimal CV effects, however respiratory depression occurs in combination with other drugs

Intraoperative Management (Elisha, 2014)
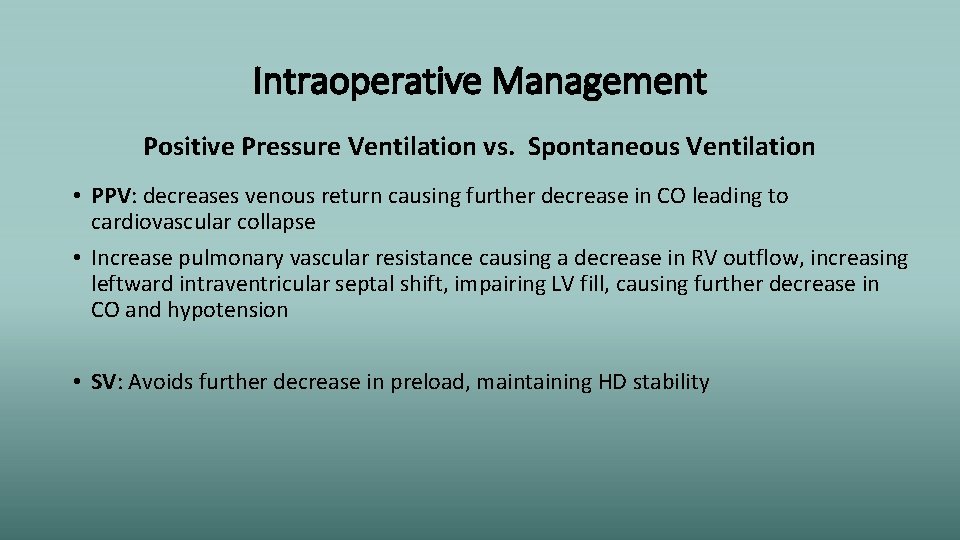
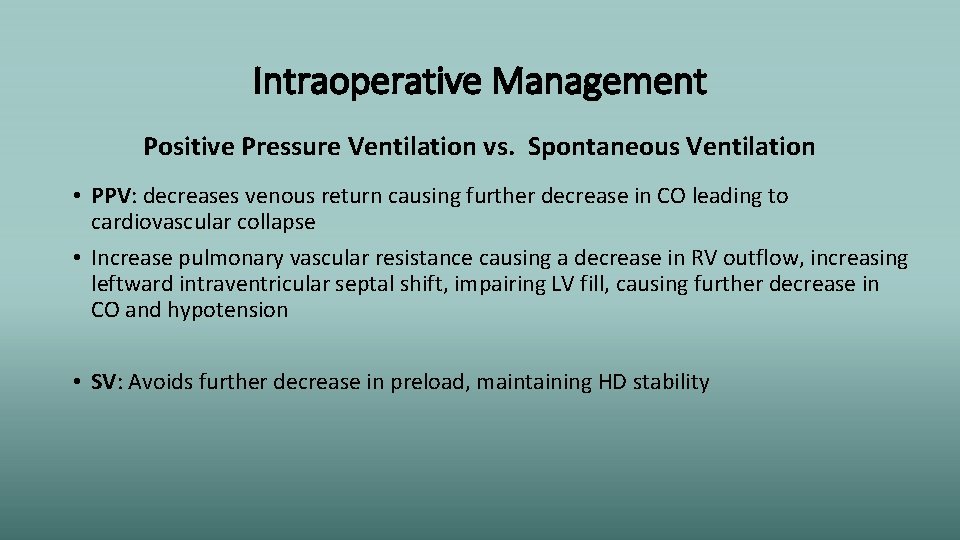
Intraoperative Management Positive Pressure Ventilation vs. Spontaneous Ventilation • PPV: decreases venous return causing further decrease in CO leading to cardiovascular collapse • Increase pulmonary vascular resistance causing a decrease in RV outflow, increasing leftward intraventricular septal shift, impairing LV fill, causing further decrease in CO and hypotension • SV: Avoids further decrease in preload, maintaining HD stability
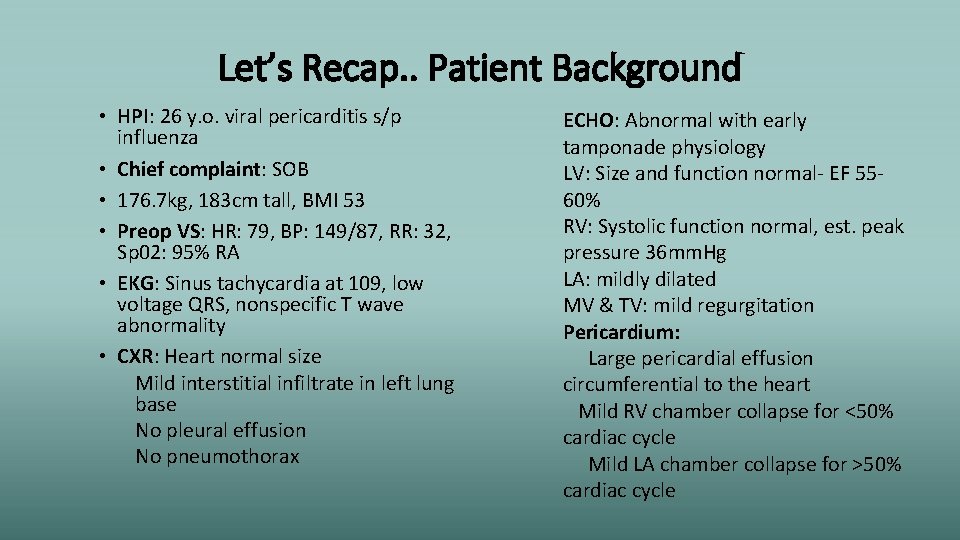
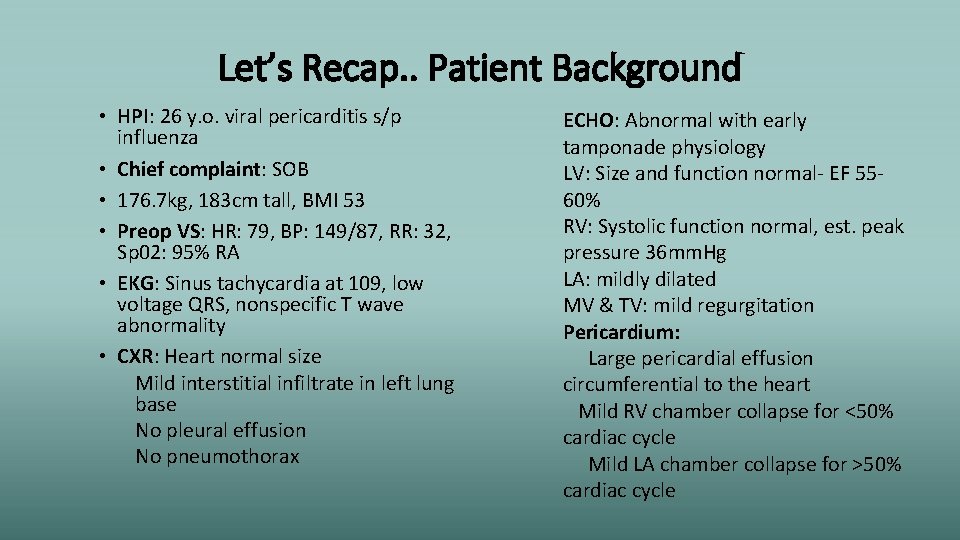
Let’s Recap. . Patient Background • HPI: 26 y. o. viral pericarditis s/p influenza • Chief complaint: SOB • 176. 7 kg, 183 cm tall, BMI 53 • Preop VS: HR: 79, BP: 149/87, RR: 32, Sp 02: 95% RA • EKG: Sinus tachycardia at 109, low voltage QRS, nonspecific T wave abnormality • CXR: Heart normal size Mild interstitial infiltrate in left lung base No pleural effusion No pneumothorax ECHO: Abnormal with early tamponade physiology LV: Size and function normal- EF 5560% RV: Systolic function normal, est. peak pressure 36 mm. Hg LA: mildly dilated MV & TV: mild regurgitation Pericardium: Large pericardial effusion circumferential to the heart Mild RV chamber collapse for <50% cardiac cycle Mild LA chamber collapse for >50% cardiac cycle
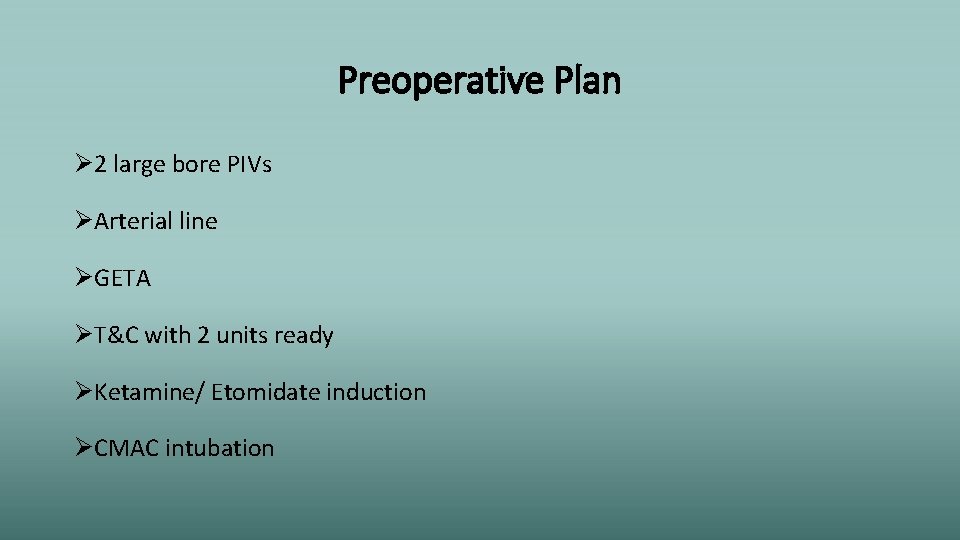
Preoperative Plan Ø 2 large bore PIVs ØArterial line ØGETA ØT&C with 2 units ready ØKetamine/ Etomidate induction ØCMAC intubation

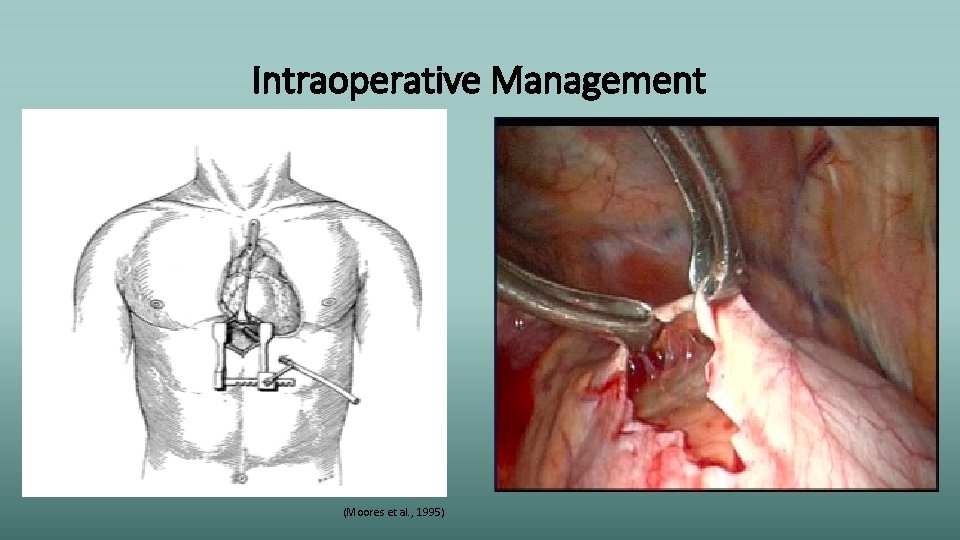
Intraoperative Course Induction Maintenance • Radial and brachial arterial line attempts unsuccessful • Patient prepped and draped prior to induction • Induced with 100 mg Lidocaine, 10 mg Etomidate, and 100 mg Ketamine • Intubated with CMAC with HOB up 30 degrees • Placed on ventilator on SIMV-VC mode • Started Sevoflurane • Incision → tachycardic at 110, hypertensive at 175/110 • Increased Sevo and 200 mg succinylcholine administered • 50 mg rocuronium followed
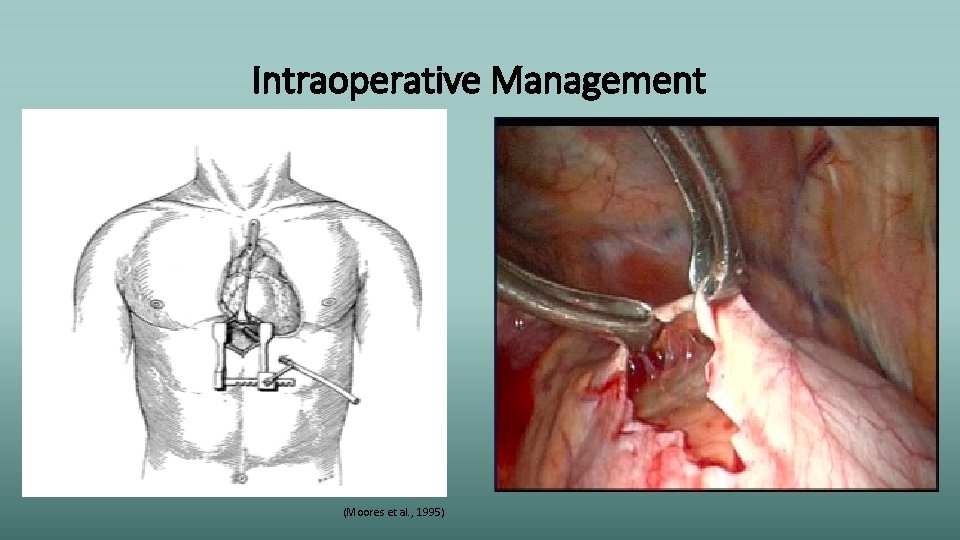
Intraoperative Management (Moores et al. , 1995)
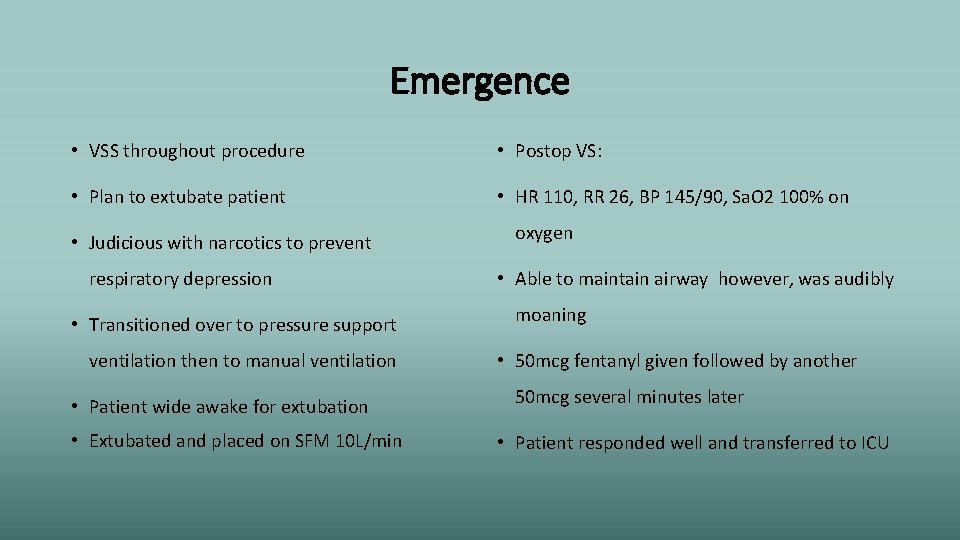
Emergence • VSS throughout procedure • Postop VS: • Plan to extubate patient • HR 110, RR 26, BP 145/90, Sa. O 2 100% on • Judicious with narcotics to prevent respiratory depression • Transitioned over to pressure support ventilation then to manual ventilation • Patient wide awake for extubation • Extubated and placed on SFM 10 L/min oxygen • Able to maintain airway however, was audibly moaning • 50 mcg fentanyl given followed by another 50 mcg several minutes later • Patient responded well and transferred to ICU
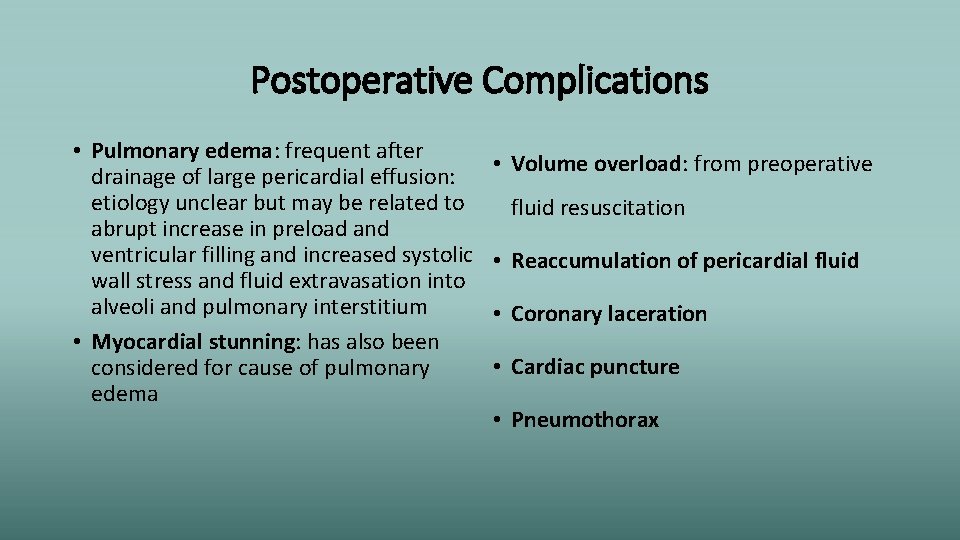
Postoperative Complications • Pulmonary edema: frequent after drainage of large pericardial effusion: etiology unclear but may be related to abrupt increase in preload and ventricular filling and increased systolic wall stress and fluid extravasation into alveoli and pulmonary interstitium • Myocardial stunning: has also been considered for cause of pulmonary edema • Volume overload: from preoperative fluid resuscitation • Reaccumulation of pericardial fluid • Coronary laceration • Cardiac puncture • Pneumothorax
Postoperative Course • Did well- no further surgeries necessary • Remained extubated • POD 1 - patient in good spirits, moving around in room, ambulating to bedside chair • VSS • Pain well managed with PCA • Discussion of removal of chest tube the next day with possible discharge home the day after that • Patient had no major complaints other than minimal to moderate pain, and fatigue

Thank you!
References Curry, S. (2014). Acute pericarditis: An overview. British Journal of Cardiac Nursing, 9(3), 124 -131. Durand, M. , Lamarche, Y. , & Denault, A. (2009). Pericardial tamponade. Canadian Journal of Anaesthesia, 56, 443 -448. doi: 10. 1007/s 12630 -009 -9080 -3 Elisha, S. (2014). Cardiovascular anatomy, physiology, pathophysiology, and anesthesia management. In J. J. Nagelhout & K. L. Plaus (Eds. ), Nurse anesthesia (5 th ed. , pp. 470 -509). St. Louis, Missouri: Elsevier Saunders. Garcia, P. , Whalin, M. K. , & Sebel, P. S. (2013). Intravenous Anesthetics. In H. C. Hemmings Jr. & T. D. Egan (Eds. ), Pharmacology and physiology for anesthesia: Foundations and clinical application (1 st ed. , pp. 137 -158). Philadelphia, Pa: Elsevier. Grocott, H. P. , Gulati, H. , Srinathan, S. , & Machensen, G. B. (2011). Anesthesia and the patient with pericardial disease. Canadian Journal of Anaesthesia, 58, 952 -966. doi: 10. 1007/s 12630 -011 -9557 -8 Hudson, A. E. , Herold, K. F. , & Hemmings, H. C. (2013). Pharmacology of inhaled anesthetics. In H. C. Hemmings Jr. & T. D. Egan (Eds. ), Pharmacology and physiology for anesthesia: Foundations and clinical application (1 st ed. , Vol. 2013, pp. 159 -179). Philadelphia, Pa: Elsevier. Imazio, M. , & Gaita, F. (2015). Diagnosis and treatment of pericarditis. Heart, 101(14), 1159 -1168. doi: 10. 1136/ heartjnl-2014 -306362 Imazio, M. , Gaita, F. , & Le. Winter, M. (2015). Evaluation and treatment of pericarditis: A systematic review. JAMA: Journal of the American Medical Association, 314(14), 1498 -1506.
References Khandaker, M. H. , Espinosa, R. E. , Nishimura, R. A. , Sinak, L. J. , Hayes, S. N. , Melduni, R. M. , & Oh, J. K. (2010). Pericardial disease: Diagnosis and management. In Mayo Clinic Proceedings, 85(6), 572 -593. Le. Winter, M. M. (2014). Acute Pericarditis. The New England Journal of Medicine, 371(25), 2410 -2416. doi: 10. 1056/NEJMcp 1404070 Moores, D. W. , Allen, K. B. , Penfield Faber, L. , Dziuban, W. , Gillman, D. J. , Warren, W. H. , . . . Lininger, L. (1995). Subxiphoid pericardial drainage for pericardial tamponade. The Journal of Thoracic and Cardiovascular Surgery, 109(3), 546 -552. O'Connor, C. J. , & Tuman, K. J. (2010). The intraoperative management of patients with pericardial tamponade. Anesthesiology Clinics, 28(1), 87 -96. doi: 10. 1016/j. anclin. 2010. 011 Ogura, T. , & Egan, T. D. (2013). Opioid Agonists and Antagonists. In H. C. Hemmings & T. D. Egan (Eds. ), Pharmacology and physiology for anesthesia: Foundations and clinical application (1 st ed. , pp. 253 -271). Philadelphia, Pa: Elsevier. Rodriguez, E. R. , & Tan, C. D. (2017). Structure and anatomy of the human pericardium. Progress in Cardiovascular Diseases, 59(4), 327 -340. doi: 10. 1016/j. pcad. 2016. 12. 010 Vakamudi, S. , Ho, N. , & Cremer, P. C. (2017). Pericardial effusions: Causes, diagnosis, and management. Progress in Cardiovascular Diseases, 59(4), 380 -388. doi: 10. 1016/j. pcad. 2016. 12. 009
Discussion • This facility did not have a CV surgeon, nor did they have a CVICU or perfusionist. . Would you have proceeded or transferred the patient?

Discussion • How would you have managed this case? How have you managed this type of case in the past?
Discussion • What do you think could have been done better? What have you learned from previous cases you have managed?