Case Studies are descriptive studies that are prepared




- Slides: 17
Case Studies are descriptive studies that are prepared for illustrating novel, unusual, or atypical features identified in patients in anesthesia practice and they potentially generate new research questions. In compliance with the Health Insurance Portability and Accountability Act (HIPPA) all patient data has been de-identified and every attempt has been made to ensure patient privacy and data security.

Anesthetic Management of a Vascular Surgery Patient at Risk For Alcohol Withdrawal Syndrome Elizabeth Pritchard BSN, RN, SRNA
Patient Summary and Background Patient: Comorbidities: • 71 -year-old male • Presented with severe pain and gangrene • Scheduled surgery: • Peripheral Arterial Disease • Hypertension • Alcohol Use Disorder • Femoral-popliteal bypass graft & trans-metatarsal amputation
Peripheral Arterial Disease Risks Indications for surgery • 20% of population • Non-white race • Male gender • Increased age • Smoking • Patients with diabetics, hypertension, and CRI • Intermittent claudication • Ischemic rest pain • Gangrene Management • Medical Optimization • ~10% myocardial injury
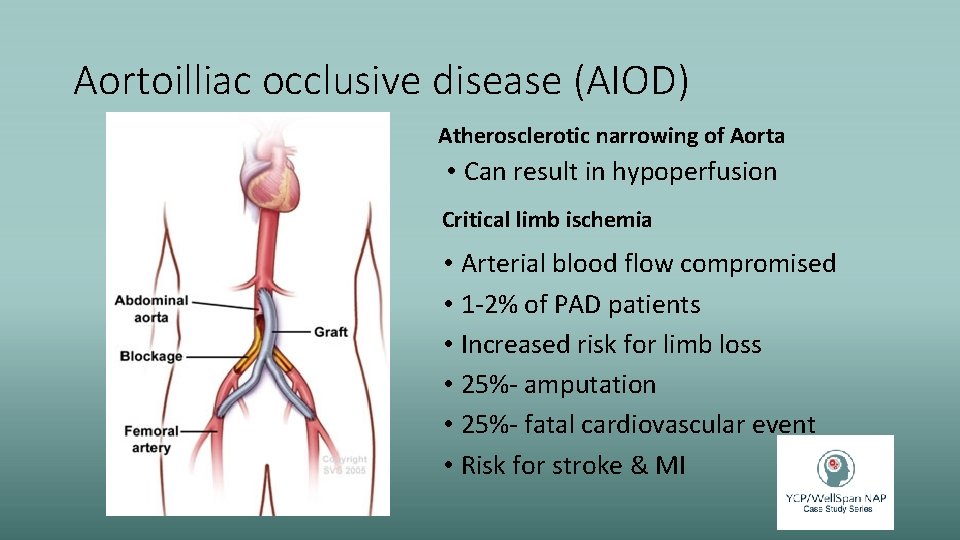
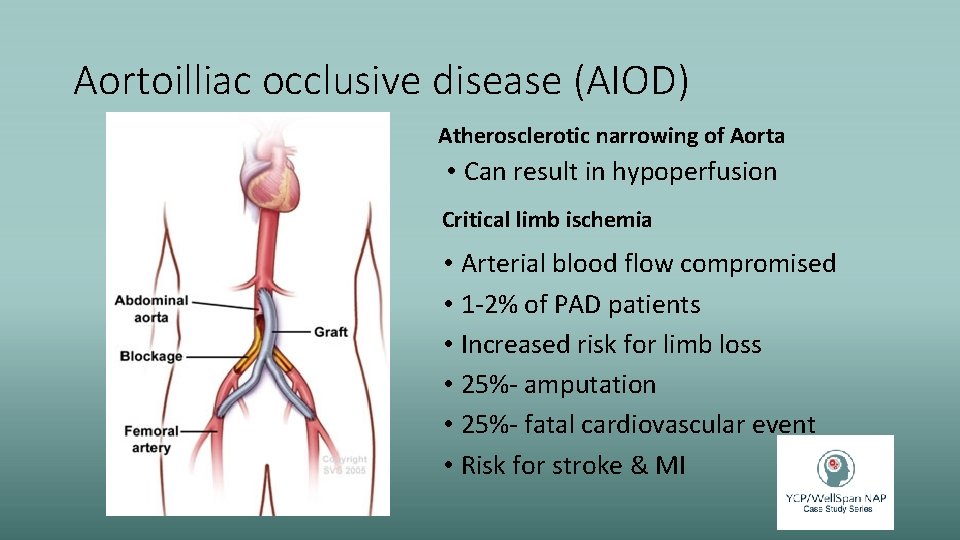
Aortoilliac occlusive disease (AIOD) Atherosclerotic narrowing of Aorta • Can result in hypoperfusion Critical limb ischemia • Arterial blood flow compromised • 1 -2% of PAD patients • Increased risk for limb loss • 25%- amputation • 25%- fatal cardiovascular event • Risk for stroke & MI

Alcohol Use • Metabolized by zero-order kinetics ACUTE • CNS depression • Disinhibition of inhibitory pathways • Cardiorespiratory Depression
Alcohol Use Disorders • Increased risk for aspiration • Liver synthesis dysfunction • Decreased circulating plasma cholinesterase • MAC level alterations • Heart Failure • Decreased Lung Volumes • Peripheral nerve and neuropsychiatric diseases • Nutritional deficiencies • Wernicke’s Encephalopathy • Folic Acid deficiency • Neuropathies and weakness • HTN
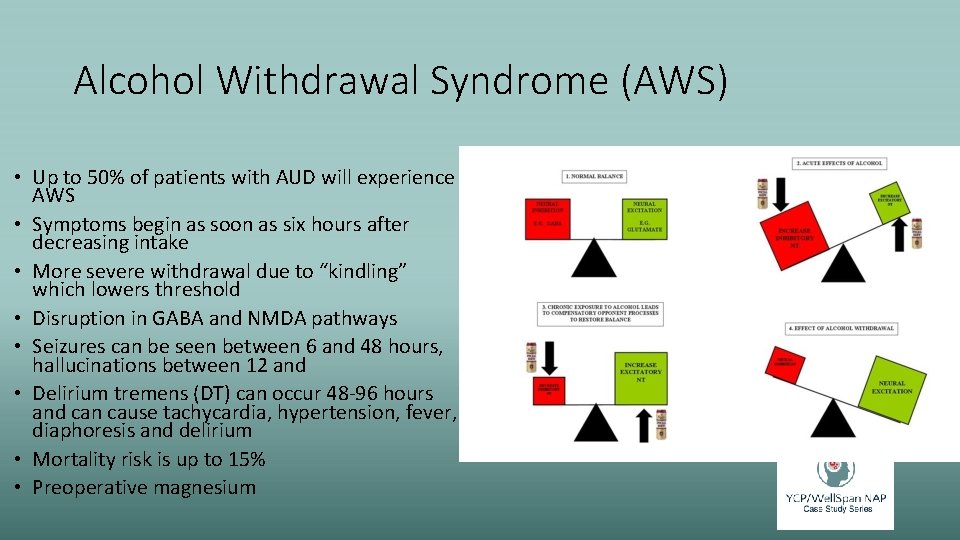
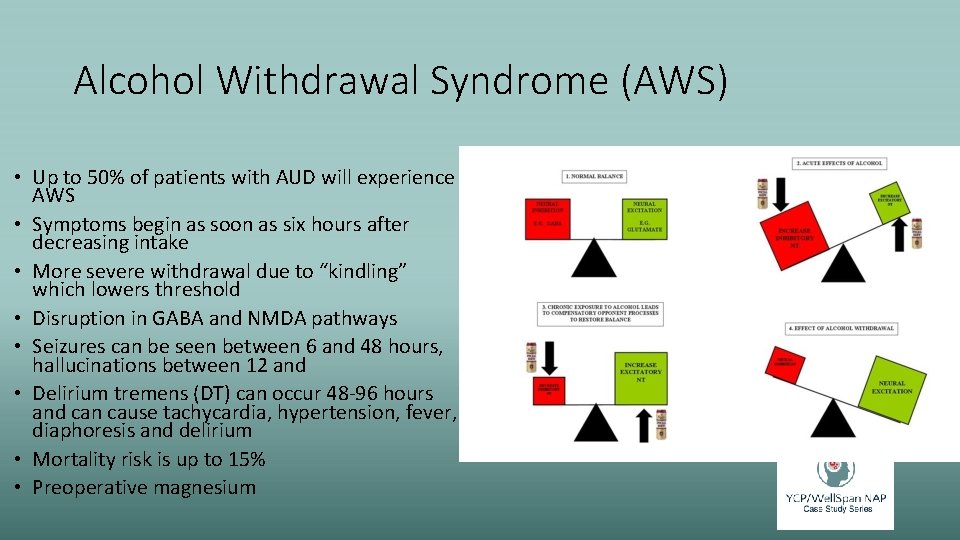
Alcohol Withdrawal Syndrome (AWS) • Up to 50% of patients with AUD will experience AWS • Symptoms begin as soon as six hours after decreasing intake • More severe withdrawal due to “kindling” which lowers threshold • Disruption in GABA and NMDA pathways • Seizures can be seen between 6 and 48 hours, hallucinations between 12 and • Delirium tremens (DT) can occur 48 -96 hours and can cause tachycardia, hypertension, fever, diaphoresis and delirium • Mortality risk is up to 15% • Preoperative magnesium
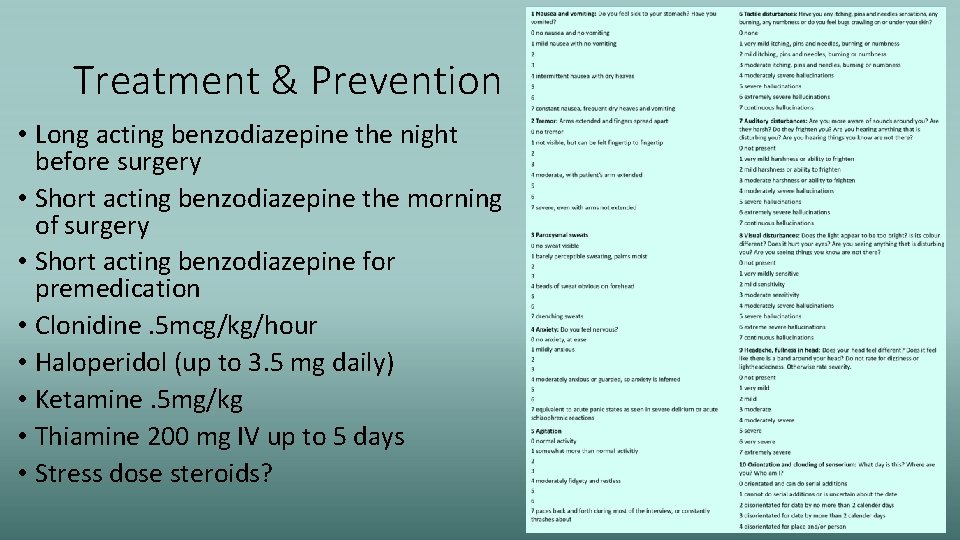
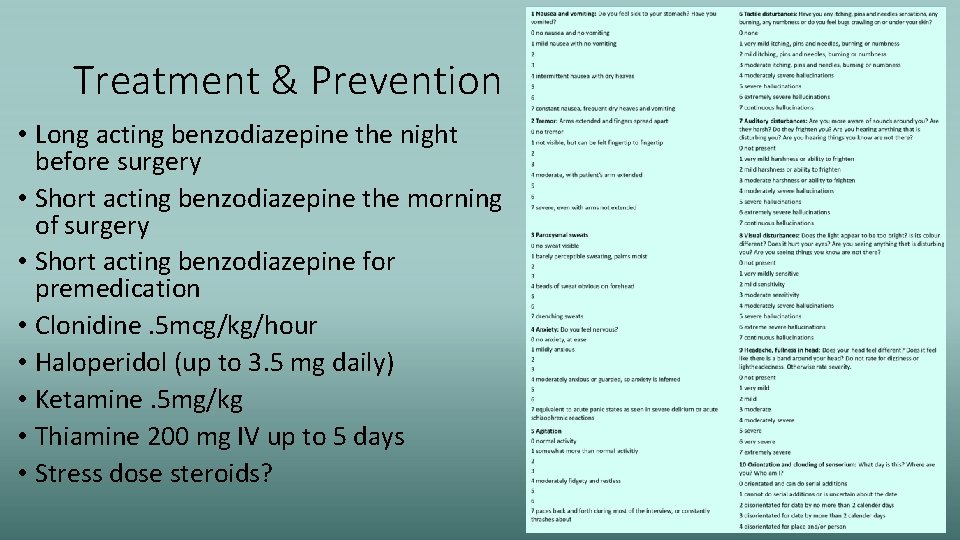
Treatment & Prevention • Long acting benzodiazepine the night before surgery • Short acting benzodiazepine the morning of surgery • Short acting benzodiazepine for premedication • Clonidine. 5 mcg/kg/hour • Haloperidol (up to 3. 5 mg daily) • Ketamine. 5 mg/kg • Thiamine 200 mg IV up to 5 days • Stress dose steroids?
Case Study: • Patient presentation • 71 year-old white male • PMH: • • Hypertension Diabetes Peripheral arterial disease Alcohol use disorder • PSH: • Right to left femoral bypass in 2010 with 4 th and 5 th transmetatarsal amputation • Aortobifemoral graft 2010 • Discharged to SNF on lisinopril and aspirin. • Lost to follow up and presented in September of 2018 with dry gangrene, pain and contraction of his right lower extremity
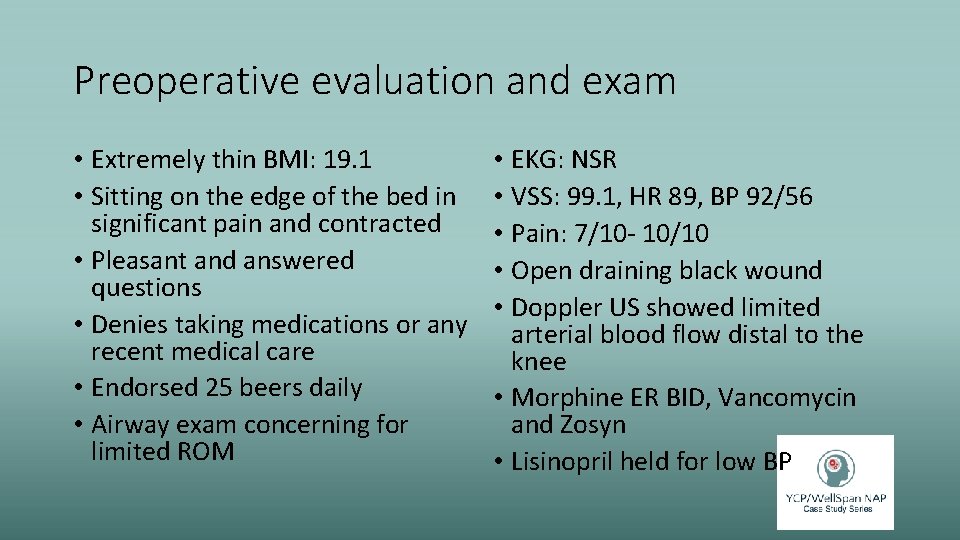
Preoperative evaluation and exam • Extremely thin BMI: 19. 1 • Sitting on the edge of the bed in significant pain and contracted • Pleasant and answered questions • Denies taking medications or any recent medical care • Endorsed 25 beers daily • Airway exam concerning for limited ROM • EKG: NSR • VSS: 99. 1, HR 89, BP 92/56 • Pain: 7/10 - 10/10 • Open draining black wound • Doppler US showed limited arterial blood flow distal to the knee • Morphine ER BID, Vancomycin and Zosyn • Lisinopril held for low BP
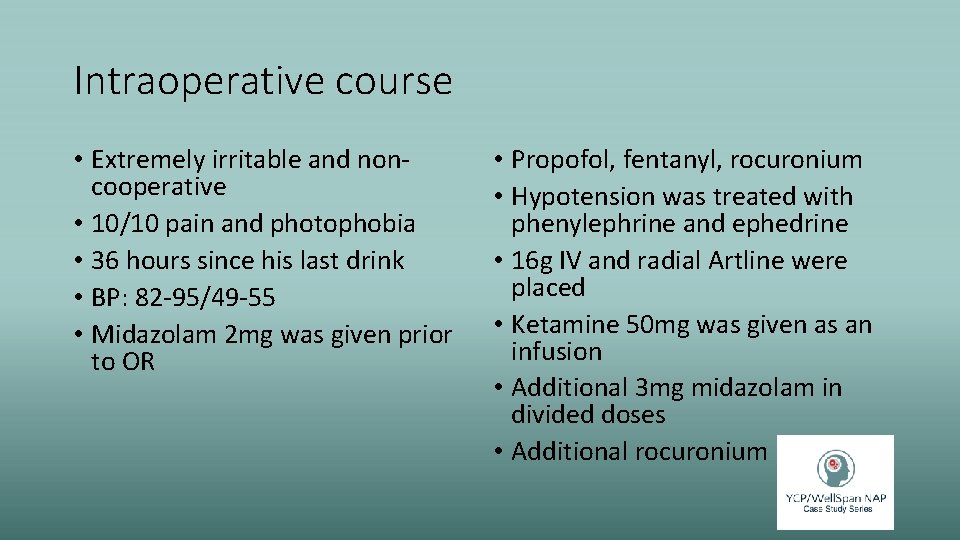
Intraoperative course • Extremely irritable and noncooperative • 10/10 pain and photophobia • 36 hours since his last drink • BP: 82 -95/49 -55 • Midazolam 2 mg was given prior to OR • Propofol, fentanyl, rocuronium • Hypotension was treated with phenylephrine and ephedrine • 16 g IV and radial Artline were placed • Ketamine 50 mg was given as an infusion • Additional 3 mg midazolam in divided doses • Additional rocuronium

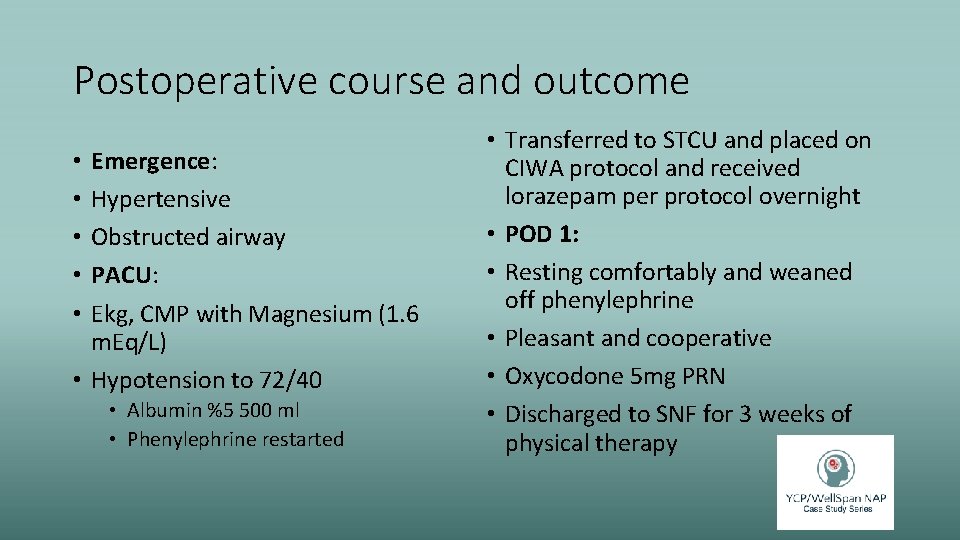
Postoperative course and outcome Emergence: Hypertensive Obstructed airway PACU: Ekg, CMP with Magnesium (1. 6 m. Eq/L) • Hypotension to 72/40 • • • Albumin %5 500 ml • Phenylephrine restarted • Transferred to STCU and placed on CIWA protocol and received lorazepam per protocol overnight • POD 1: • Resting comfortably and weaned off phenylephrine • Pleasant and cooperative • Oxycodone 5 mg PRN • Discharged to SNF for 3 weeks of physical therapy

Discussion & Lessons learned • Standardized protocols for screening and treatment • Optimizing patient vs emergent surgery • Overlapping disease processes • CAD and increased oxygen demand • AUD and AWS have high rates of undetected • Anesthetic medications can mask signs and symptoms of AWS • Regional anesthesia in patients at risk for AWS? • Missed aspects of recommendations • Preoperative optimization on floor
Questions? • What type of screening or • What communication methods assessment do you perform or tools would provide a more preoperatively on patients that comprehensive plan of care for endorse alcohol use both related these vulnerable patients? to withdrawal potential and cardiovascular complications.
References Devereaux, P. J. , Yang, H. , Yusuf, S. , Guyatt, G. , Leslie, K. , Villar, J. C. , . . . POISE Study Group. (2008). Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): A randomised controlled trial. Lancet, 371(9627), 1839 -1847. doi: 10. 1016/S 0140 -6736(08)60601 -7 Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014; 130(24): 2215– 2245 Kork, F. , Neumann, T. , & Spies, C. (2010). Perioperative management of patients with alcohol, tobacco and drug dependency. Current Opinion in Anaesthesiology, 23(3), 384 -390. doi: 10. 1097/ACO. 0 b 013 e 3283391 f 79 Littleton, J. (1998). Neurochemical mechanisms underlying alcohol withdrawal. Alcohol Health and Research World, 22(1), 13. Mostafaie, K. , Bedenis, R. , & Harrington, D. (2015). Beta-adrenergic blockers for perioperative cardiac risk reduction in people undergoing vascular surgery. The Cochrane Database of Systematic Reviews, 1, CD 006342. doi: 10. 1002/14651858. CD 006342. pub 2 Olin, J. W. & Sealove, B. A. (2010). Peripheral artery disease: Current insight into the disease and its diagnosis and management. Mayo Clinic Proceedings, 85(7), 678 -692. doi: 10. 4065/mcp. 2010. 0133 Puz, C. A. , & Stokes, S. J. (2005). Alcohol withdrawal syndrome: Assessment and treatment with the use of the clinical institute withdrawal assessment for alcohol-revised. Critical Care Nursing Clinics of North America, 17(3), 297 -304. doi: 10. 1016/j. ccell. 2005. 04. 001 Schuckit, M. A. (2014). Recognition and management of withdrawal delirium (delirium tremens). The New England Journal of Medicine, 371(22), 2109 -2113. doi: 10. 1056/NEJMra 1407298 Substance Abuse and Mental Health Services Administration (SAMHSA). 2015 National Survey on Drug Use and Health (NSDUH). Table 5. 6 A—Substance Use Disorder in Past Year among Persons Aged 18 or Older, by Demographic Characteristics: Numbers in Thousands, 2014 and 2015. Available at: https: //www. samhsa. gov/data/sites/default/files/NSDUH-Det. Tabs-2015/NSDUH-Det. Tabs-2015. htm#tab 5 -6 a. Accessed 12/18/18. Substance Abuse and Mental Health Services Administration (SAMHSA). 2015 National Survey on Drug Use and Health (NSDUH). Table 5. 6 B—Substance Use Disorder in Past Year among Persons Aged 18 or Older, by Demographic Characteristics: Percentages, 2014 and 2015. Available at: https: //www. samhsa. gov/data/sites/default/files/NSDUH-Det. Tabs-2015/NSDUH-Det. Tabs-2015. htm#tab 5 -6 b. Accessed 12/18/18. Tetrault, J. M. , & O'Connor, P. G. (2008). Substance abuse and withdrawal in the critical care setting. Critical care clinics, 24(4), 767 -788. doi: 10. 1016/j. ccc. 2008. 05. 005 Long J B Suresh S 2017 Clinical anesthesia. Valentine, E. & Ochroch, E. A. (2017). Anesthesia for Vascular and Endovascular Surgery. In P. G. (Valentine, & Ochroch, 2017), B. F. Cullen, R. K. Stoelting, M. K. Cahalan, M. C. Stock, R. Ortega, . . . N. F. Holt (Ed. ), Clinical anesthesia (8 th ed. , pp. 1113 -1139). Philadelphia, PA: Wolters Kluwer. 20180404213833538859010