C S O M Investigations Treatment Dr Vishal











- Slides: 54

C. S. O. M. : Investigations & Treatment Dr. Vishal Sharma
Investigations for T. T. D. • Examination under microscope • Ear discharge swab: for culture sensitivity • Pure tone audiometry • Patch test • X-ray mastoid: B/L 300 lateral oblique (Schuller) Done when cortical mastoidectomy is required in ear discharge refractory to antibiotics
Uses of Audiometry • Presence of hearing loss • Degree of hearing loss • Type of hearing loss • Hearing of other ear • Record to compare hearing post-operatively • Medico legal purpose
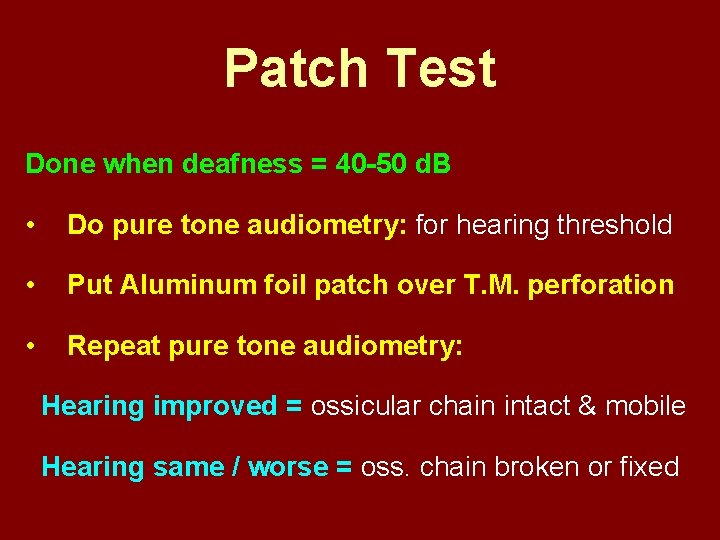
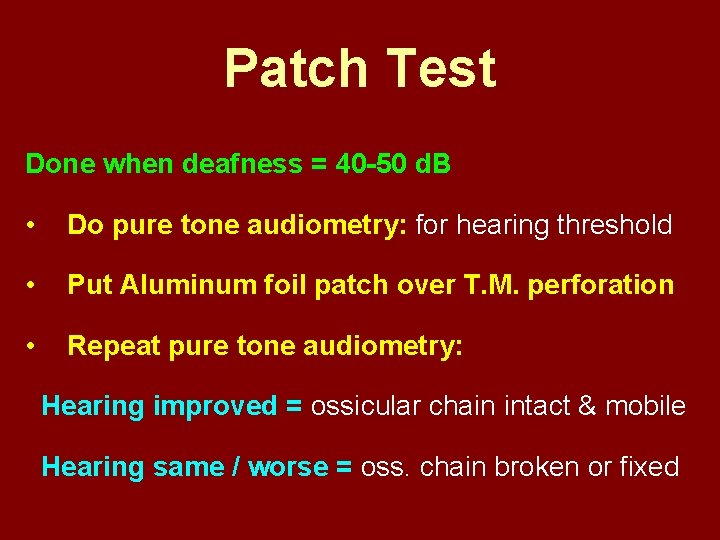
Patch Test Done when deafness = 40 -50 d. B • Do pure tone audiometry: for hearing threshold • Put Aluminum foil patch over T. M. perforation • Repeat pure tone audiometry: Hearing improved = ossicular chain intact & mobile Hearing same / worse = oss. chain broken or fixed
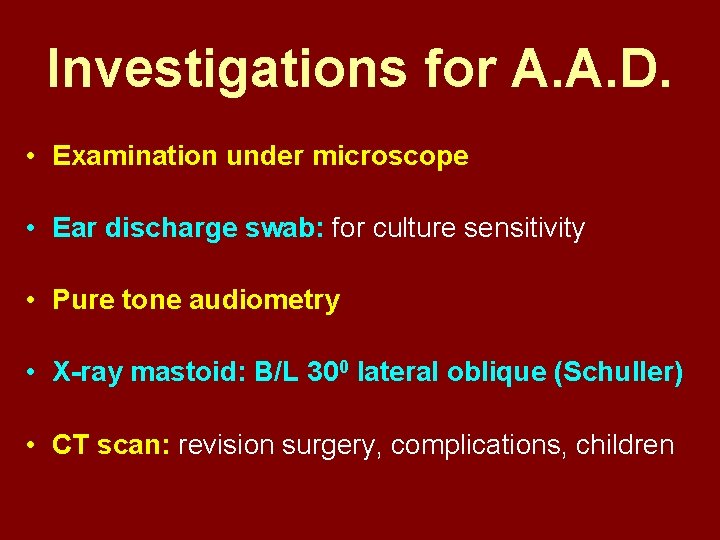
Investigations for A. A. D. • Examination under microscope • Ear discharge swab: for culture sensitivity • Pure tone audiometry • X-ray mastoid: B/L 300 lateral oblique (Schuller) • CT scan: revision surgery, complications, children
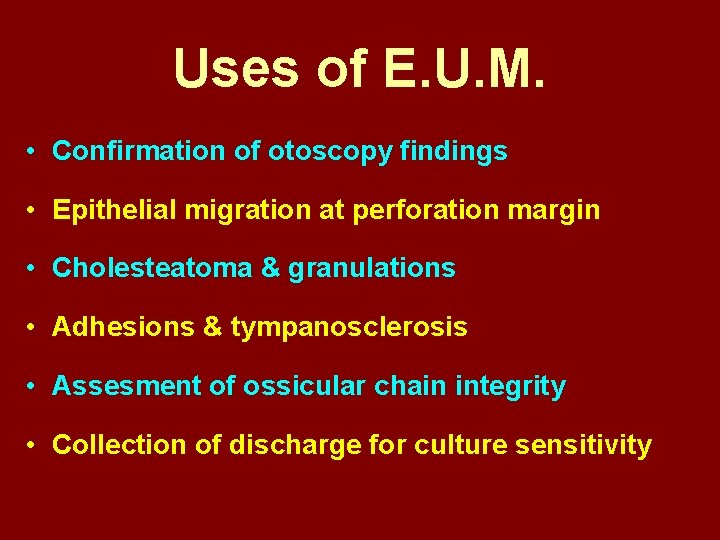
Uses of E. U. M. • Confirmation of otoscopy findings • Epithelial migration at perforation margin • Cholesteatoma & granulations • Adhesions & tympanosclerosis • Assesment of ossicular chain integrity • Collection of discharge for culture sensitivity
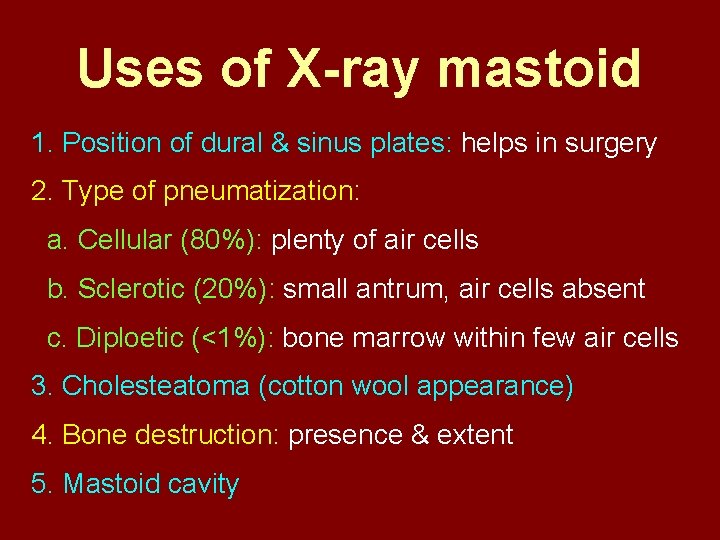
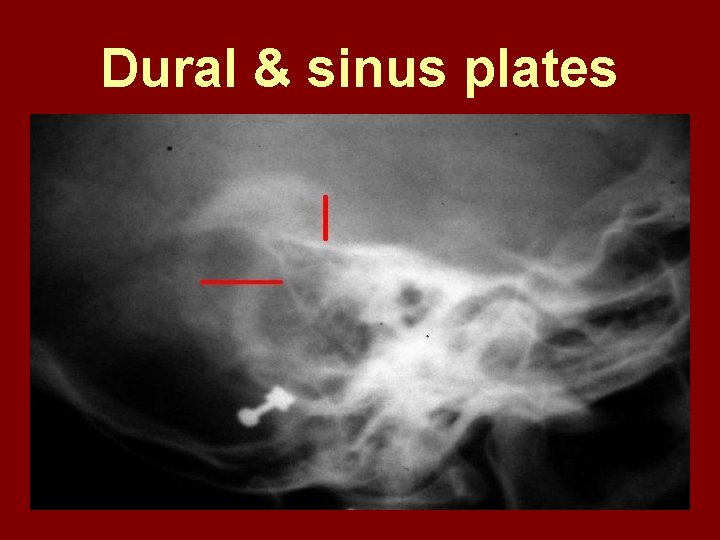
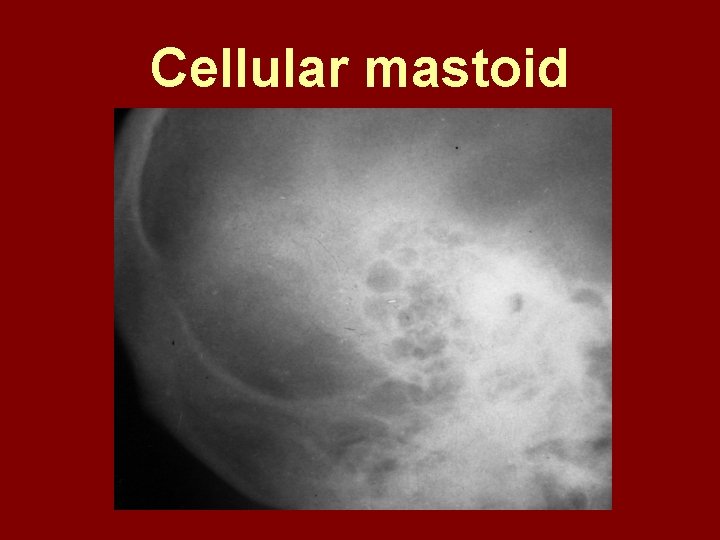
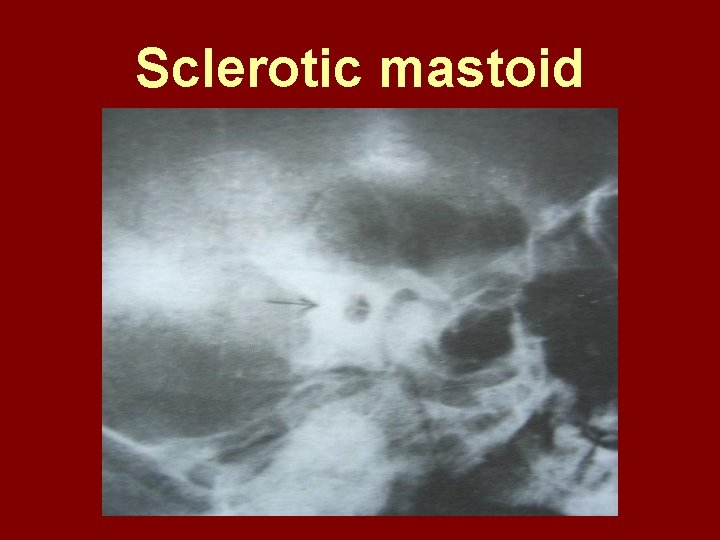
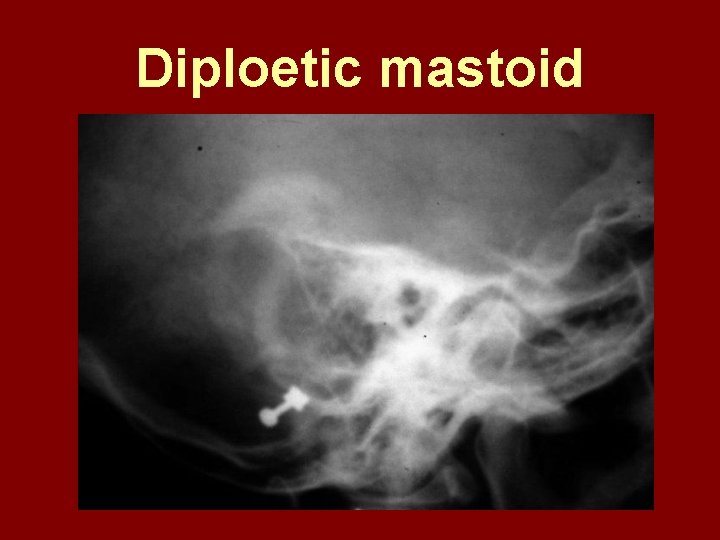
Uses of X-ray mastoid 1. Position of dural & sinus plates: helps in surgery 2. Type of pneumatization: a. Cellular (80%): plenty of air cells b. Sclerotic (20%): small antrum, air cells absent c. Diploetic (<1%): bone marrow within few air cells 3. Cholesteatoma (cotton wool appearance) 4. Bone destruction: presence & extent 5. Mastoid cavity
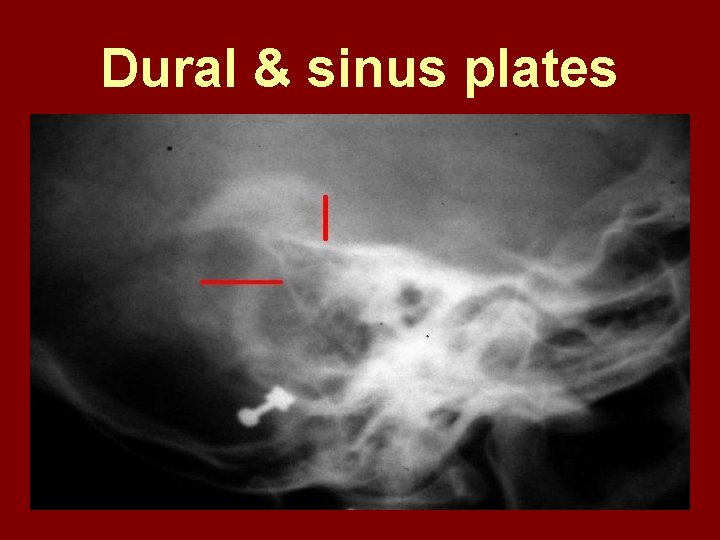
Dural & sinus plates
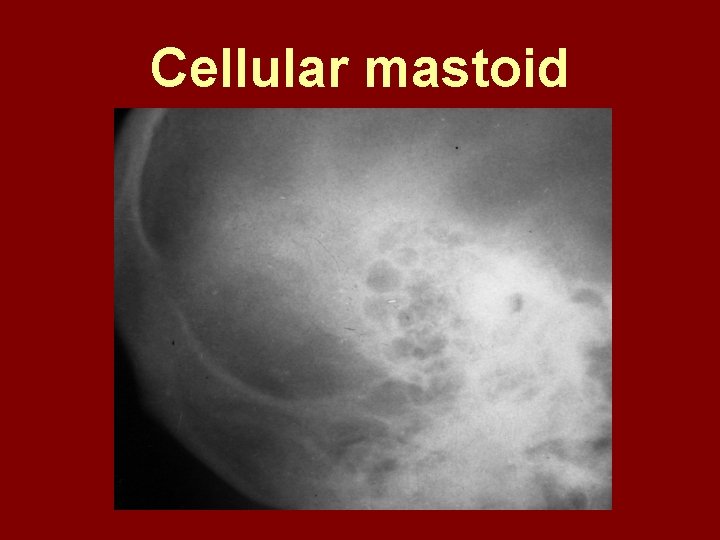
Cellular mastoid
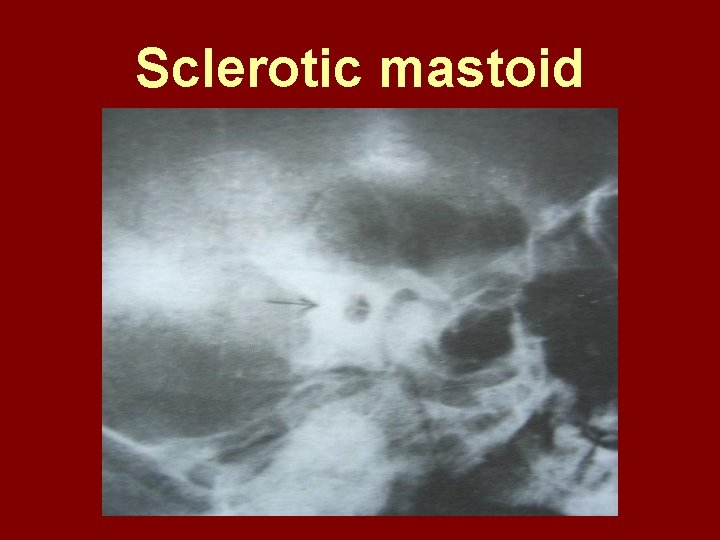
Sclerotic mastoid
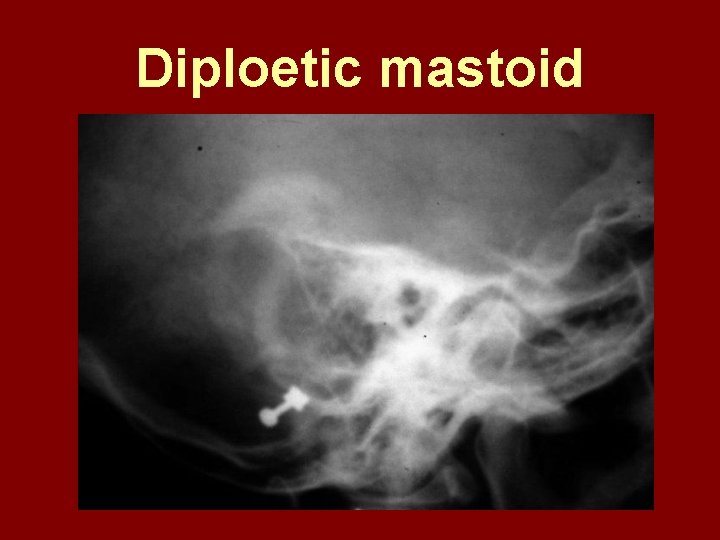
Diploetic mastoid
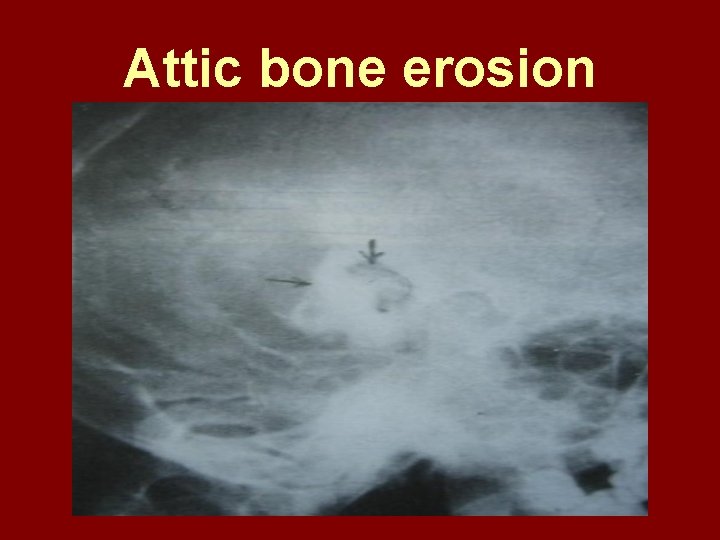
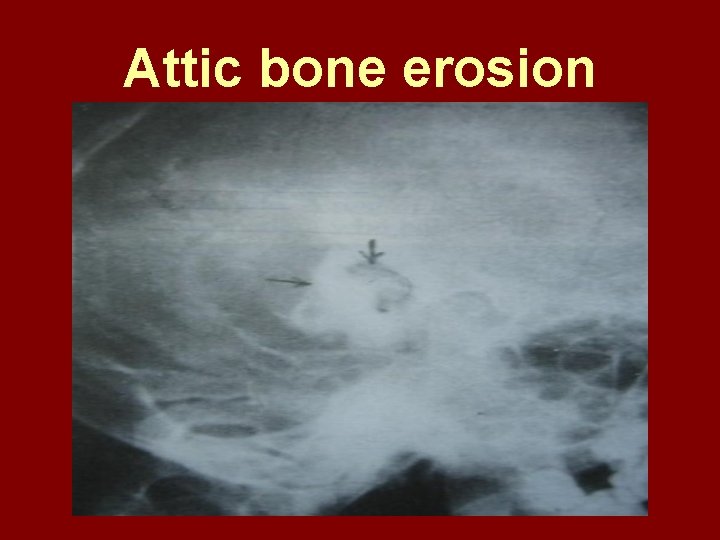
Attic bone erosion
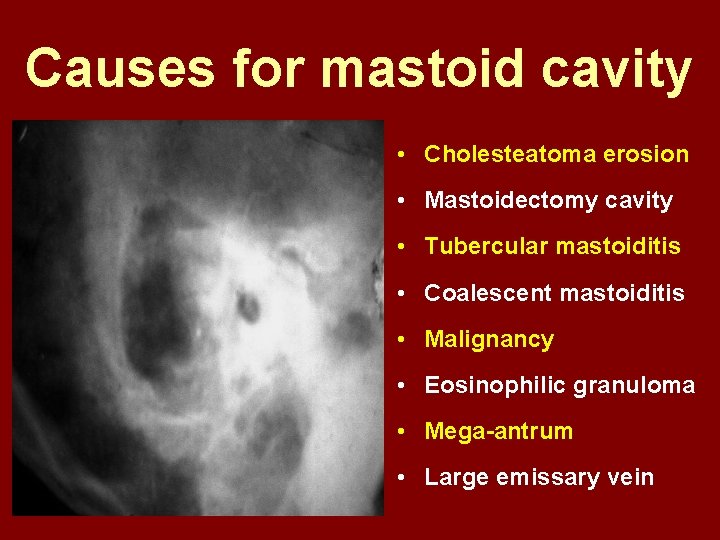
Causes for mastoid cavity • Cholesteatoma erosion • Mastoidectomy cavity • Tubercular mastoiditis • Coalescent mastoiditis • Malignancy • Eosinophilic granuloma • Mega-antrum • Large emissary vein
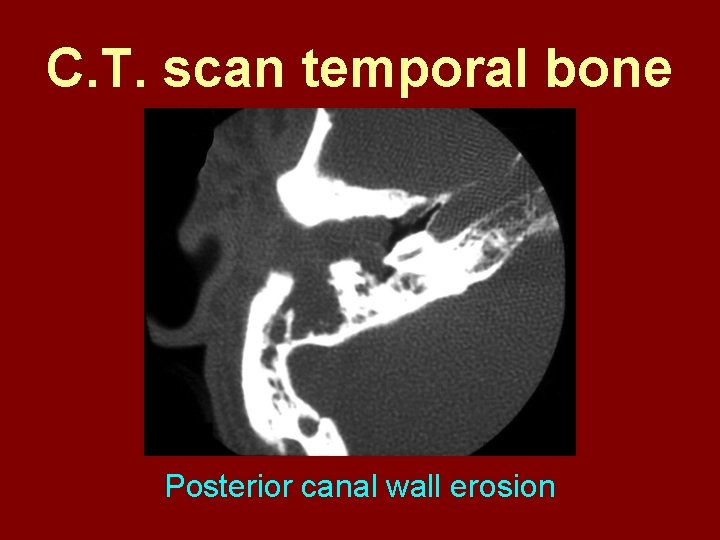
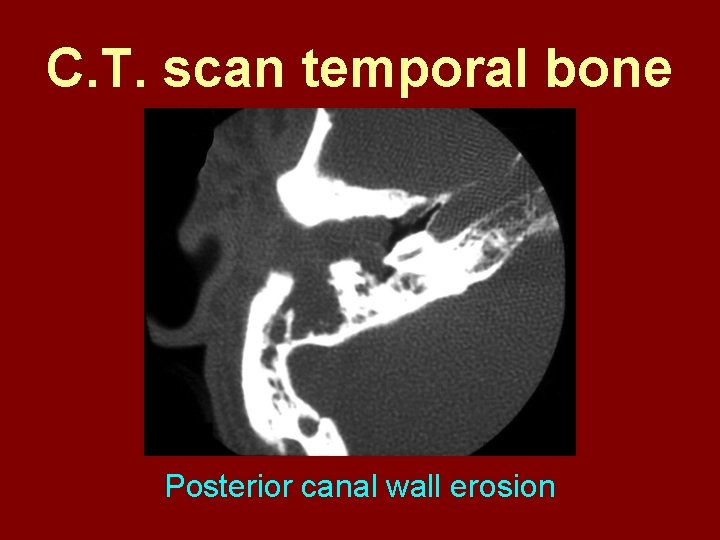
C. T. scan temporal bone Posterior canal wall erosion
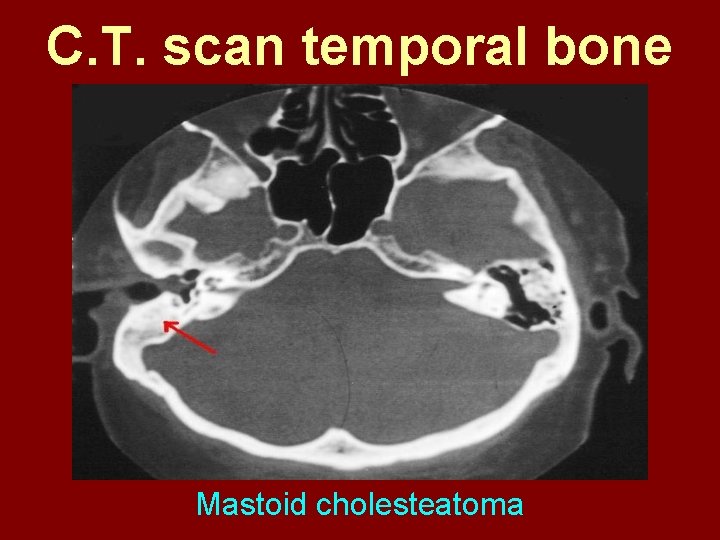
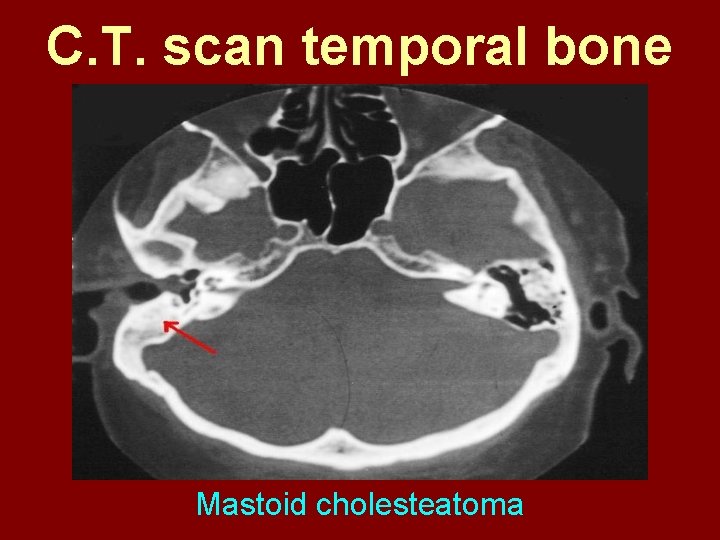
C. T. scan temporal bone Mastoid cholesteatoma

Treatment for Tubo-tympanic Disease

Non-surgical Treatment • Precautions • Aural toilet • Antibiotics: Systemic & Topical • Antihistamines: Systemic & Topical • Nasal decongestant: Systemic & Topical • Treatment of respiratory infection & allergy • Tympanic membrane patcher
Precautions • Encourage breast feeding with child’s head raised. Avoid bottle feeding. • Avoid forceful nose blowing • Plug E. A. C. with Vaseline smeared cotton while bathing & avoid swimming • Avoid putting oil & self-cleaning of E. A. C.
Aural Toilet Done only for active stage – Dry mopping with cotton swab – Suction clearance: best method – Gentle irrigation (wet mopping) 1. 5% acetic acid solution used T. I. D. Removes accumulated debris Acidic p. H discourages bacterial growth
Antibiotics Topical Antibiotics: Ciprofloxacin, Gentamicin, Tobramycin Antibiotics + Steroid: for polyps, granulations Neosporin + Betamethasone / Hydrocortisone Oral Antibiotics: for severe infections Cefuroxime, Cefaclor, Cefpodoxime, Cefixime

Antihistamines & Decongestants Antihistamines Systemic decongestants Chlorpheniramine Pseudoephedrine Cetirizine Phenylephrine Fexofenadine Topical decongestants Loratidine Oxymetazoline Levo-cetrizine Xylometazoline Azelastine (topical) Hypertonic saline
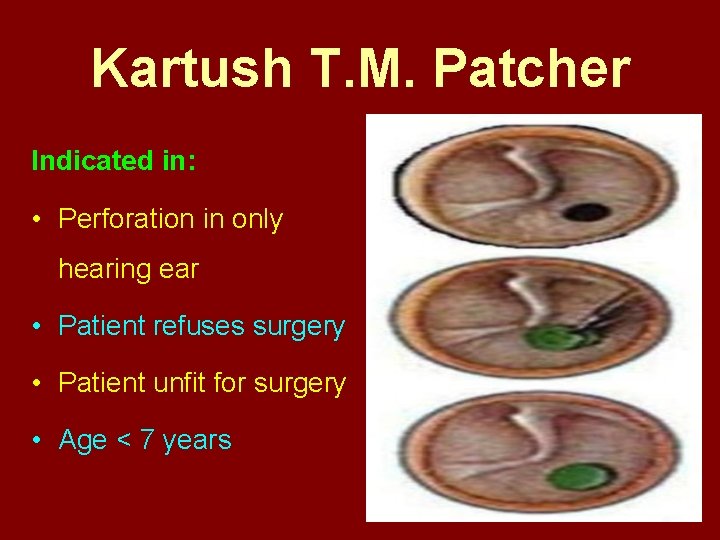
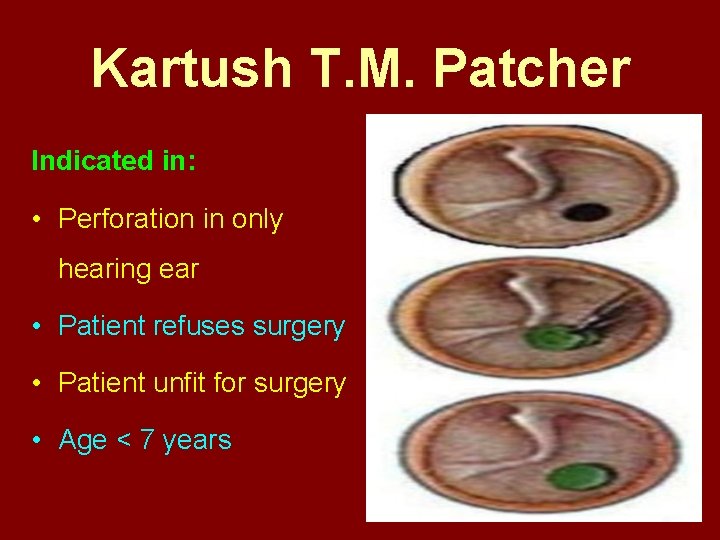
Kartush T. M. Patcher Indicated in: • Perforation in only hearing ear • Patient refuses surgery • Patient unfit for surgery • Age < 7 years
Surgical Treatment Indicated in inactive or quiescent stage • Myringoplasty • Tympanoplasty Indicated in active stage • Cortical Mastoidectomy • Aural polypectomy
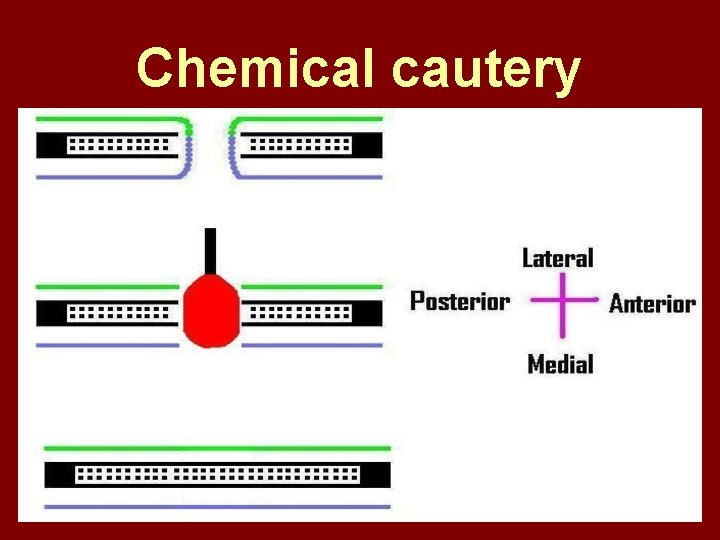
Methods to close perforation T. M. perforation < 2 mm § Chemical cautery with silver nitrate § Fat grafting § Myringoplasty if these measures fail T. M. perforation > 2 mm § Tympanic membrane patcher § Myringoplasty
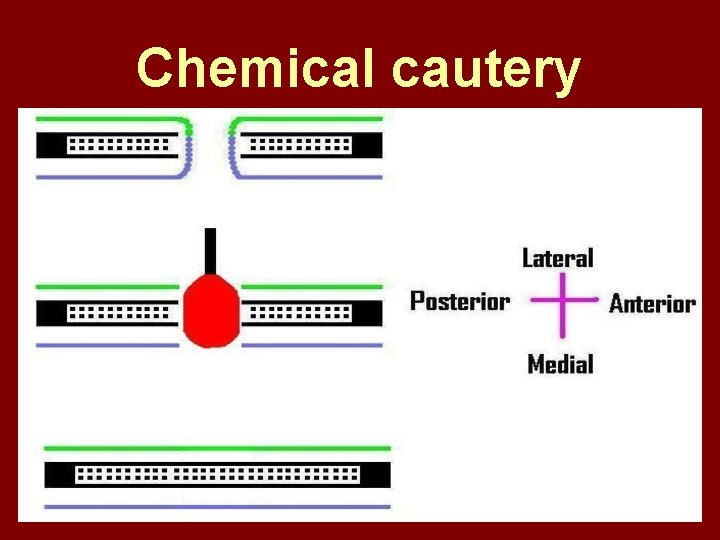
Chemical cautery
Approaches to middle ear

Wilde’s post-aural incision
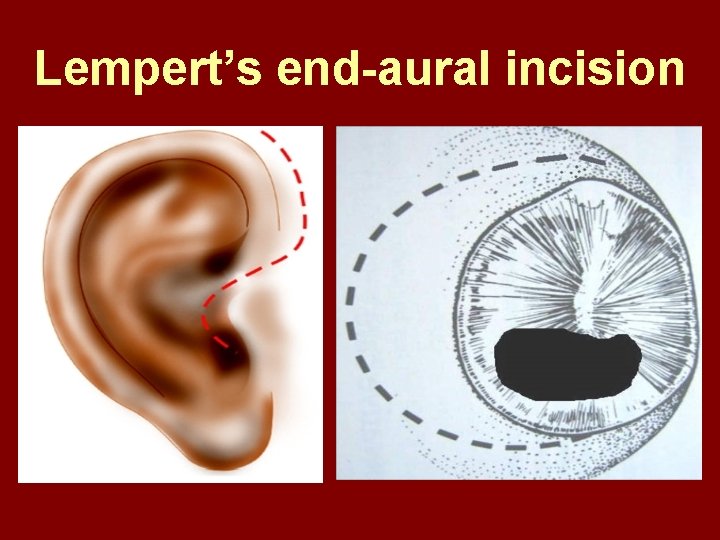
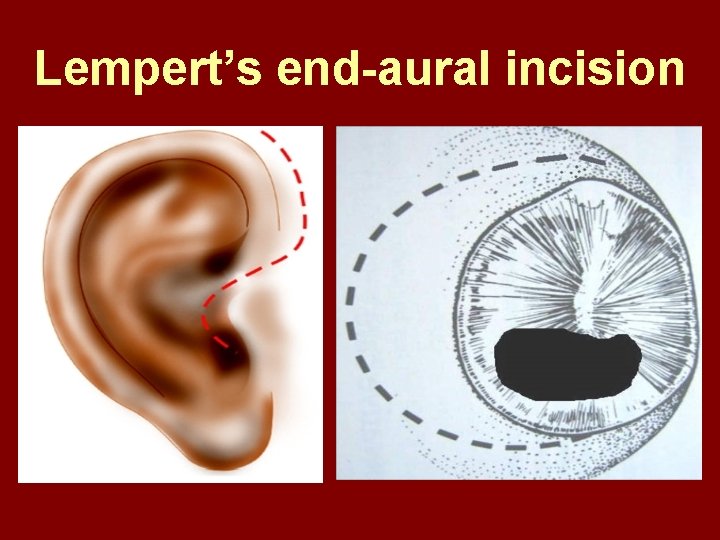
Lempert’s end-aural incision
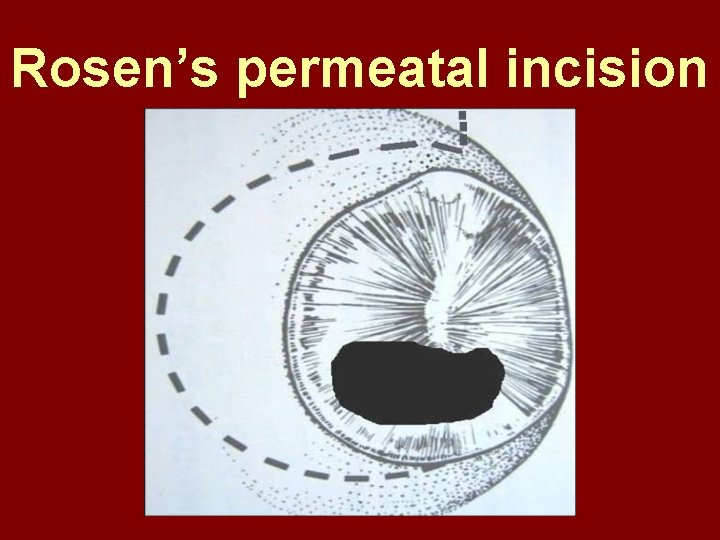
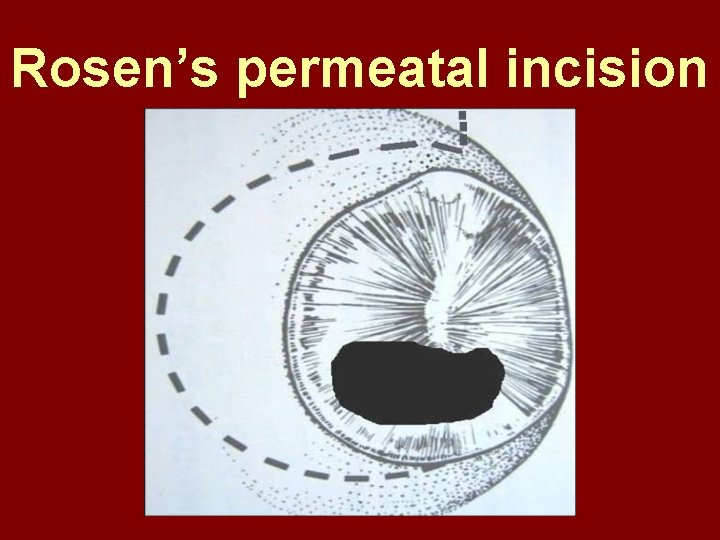
Rosen’s permeatal incision

Hearing Restoration Myringoplasty: • surgical closure of tympanic membrane perforation Ossiculoplasty: • surgical reconstruction of ossicular chain Tympanoplasty: • Surgical removal of disease + reconstruction of hearing mechanism without mastoid surgery
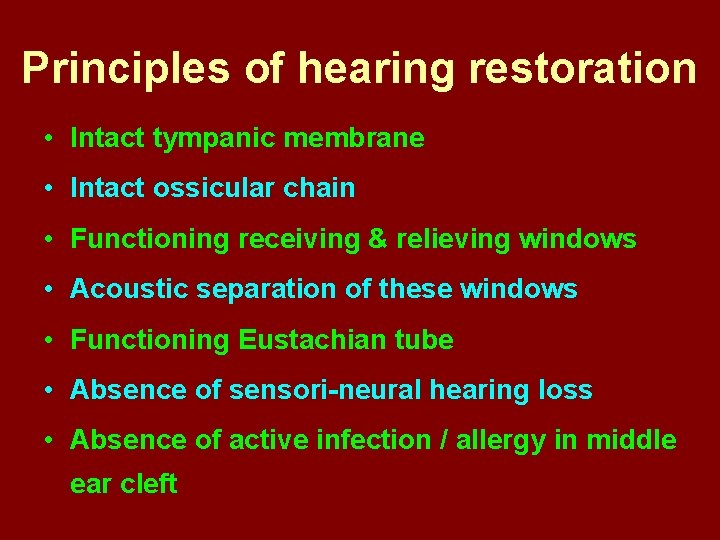
Principles of hearing restoration • Intact tympanic membrane • Intact ossicular chain • Functioning receiving & relieving windows • Acoustic separation of these windows • Functioning Eustachian tube • Absence of sensori-neural hearing loss • Absence of active infection / allergy in middle ear cleft
Myringoplasty
Aims • Permanently stop ear discharge: dry, safe ear • Improve hearing: provided: 1. ossicles are intact + mobile; 2. absence of sensori-neural deafness • Prevention of: tympanosclerosis, adhesions, vertigo, S. N. H. L. (cochlear exposure to loud sound) • Wearing of hearing aid • Occupational: military, pilots • Recreation: swimming, diving
Contraindications • Purulent ear discharge • Otitis externa • Respiratory allergy • Age < 7 yr (Eustachian tube not fully developed) • Only hearing ear • Cholesteatoma
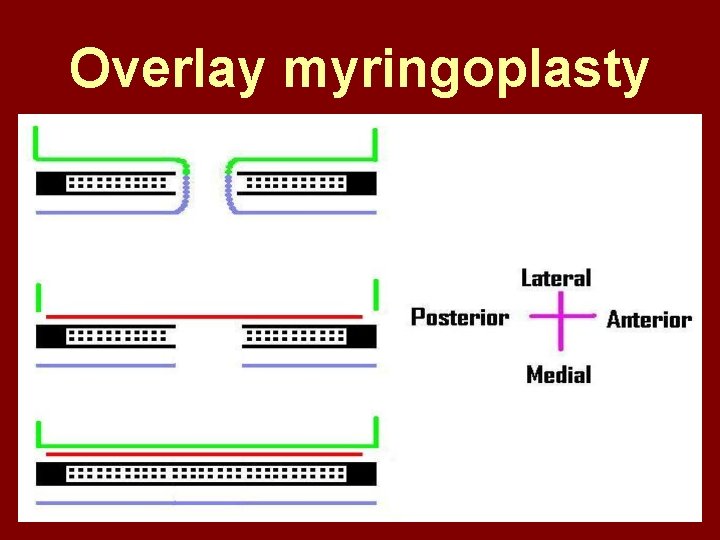
Methods Techniques: • Underlay: graft placed medial to fibrous annulus • Overlay: graft placed lateral to fibrous annulus Grafts used: • Temporalis fascia, Tragal perichondrium, Vein graft, Fascia lata, Dura mater
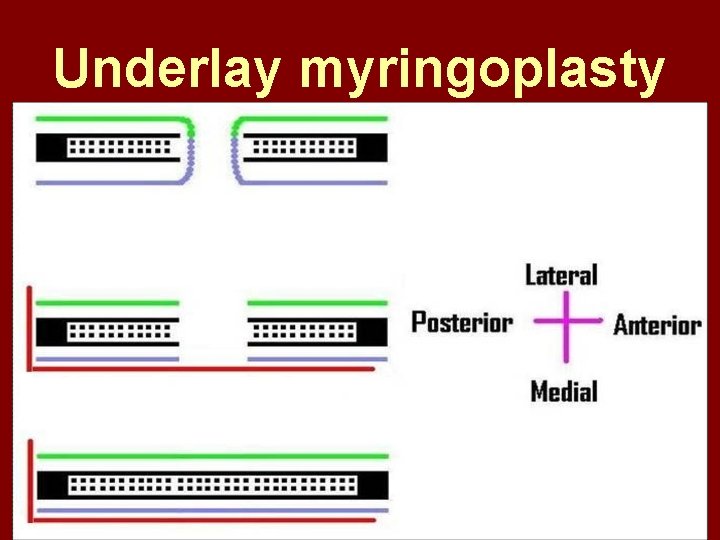
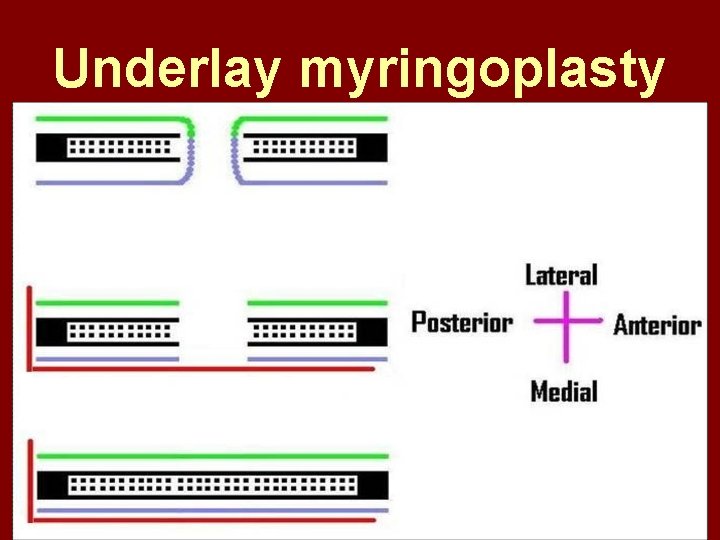
Underlay myringoplasty
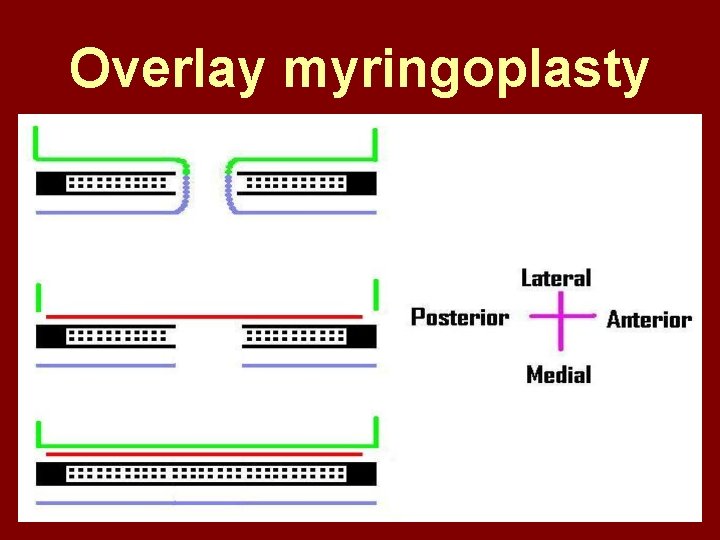
Overlay myringoplasty
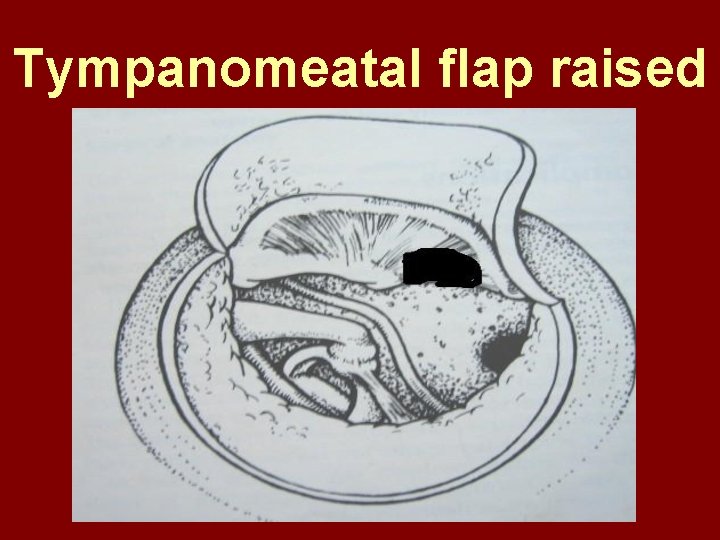
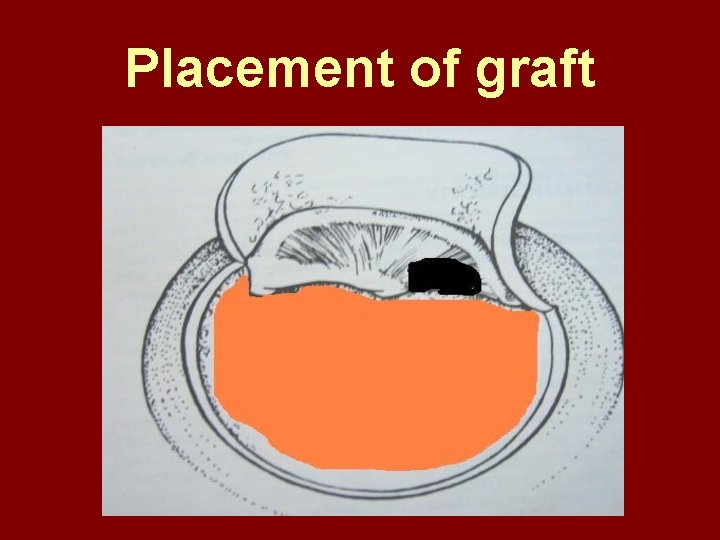
Steps of underlay myringoplasty
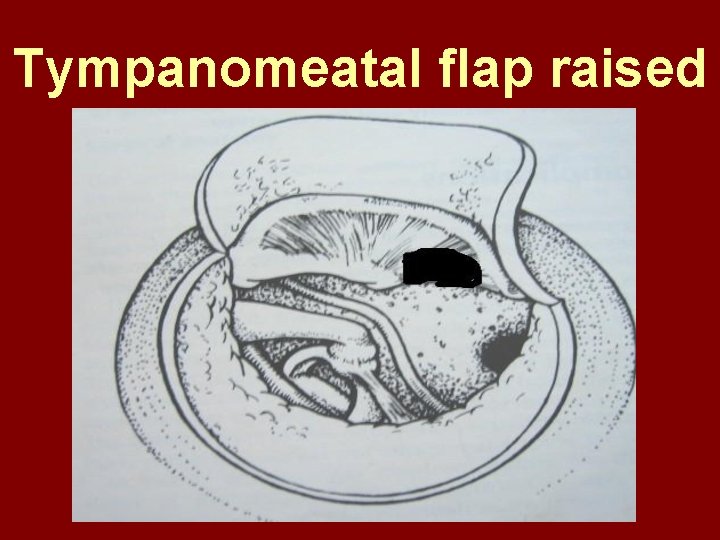
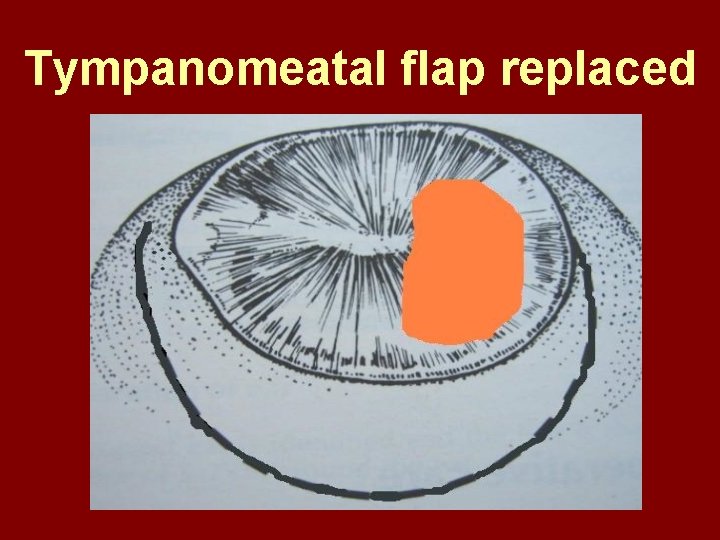
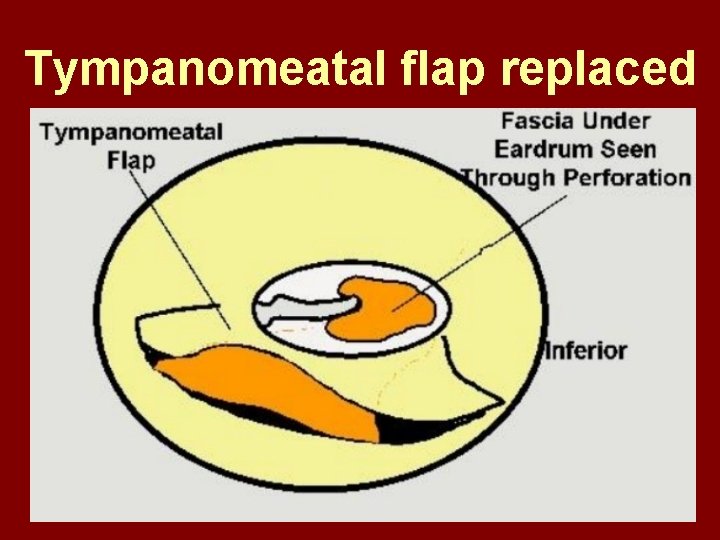
Tympanomeatal flap raised
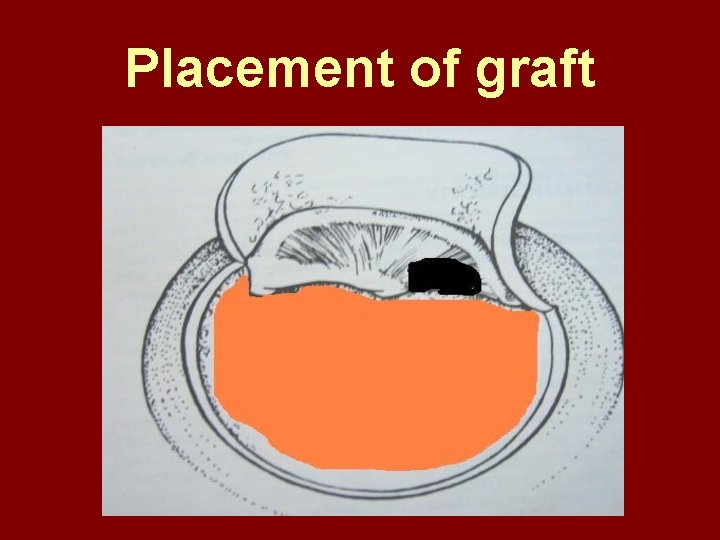
Placement of graft
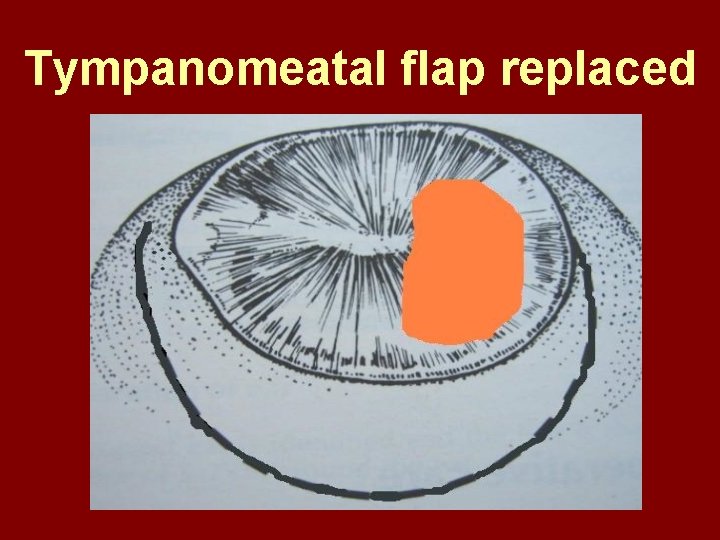
Tympanomeatal flap replaced
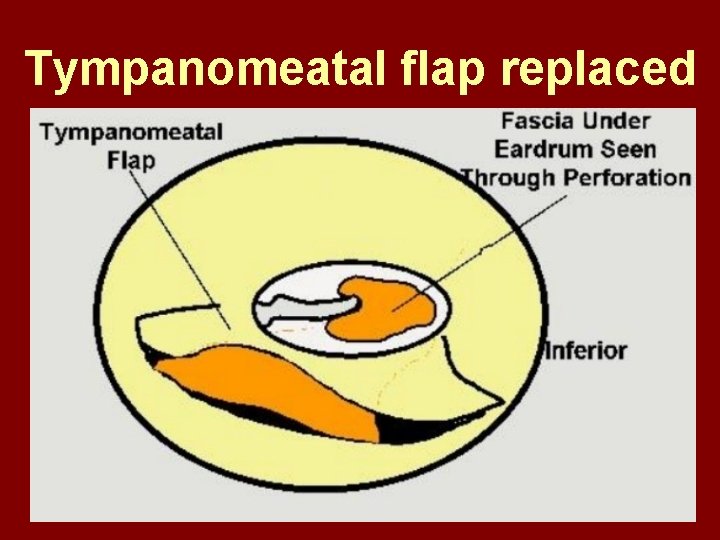
Tympanomeatal flap replaced


Why temporalis fascia? • Basal metabolic rate lowest (best survival rate) • Easily harvested by post-aural incision • Its an autograft, so no rejection • Same thickness as normal tympanic membrane • Large size graft can be harvested • Good resistance to infection
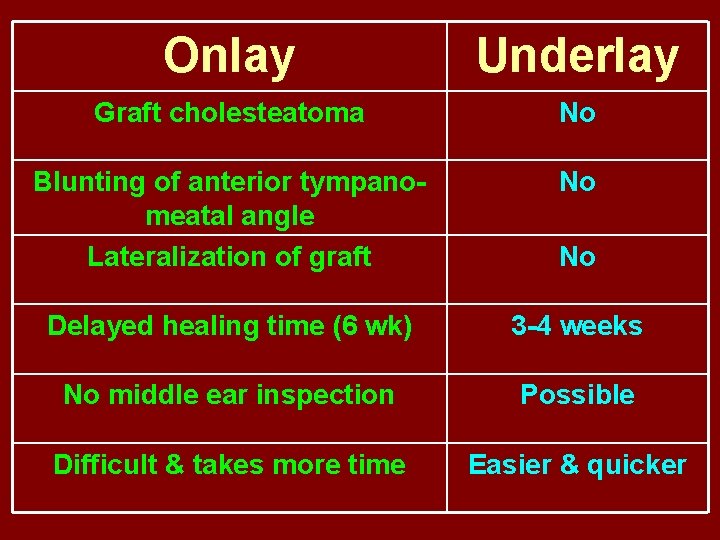
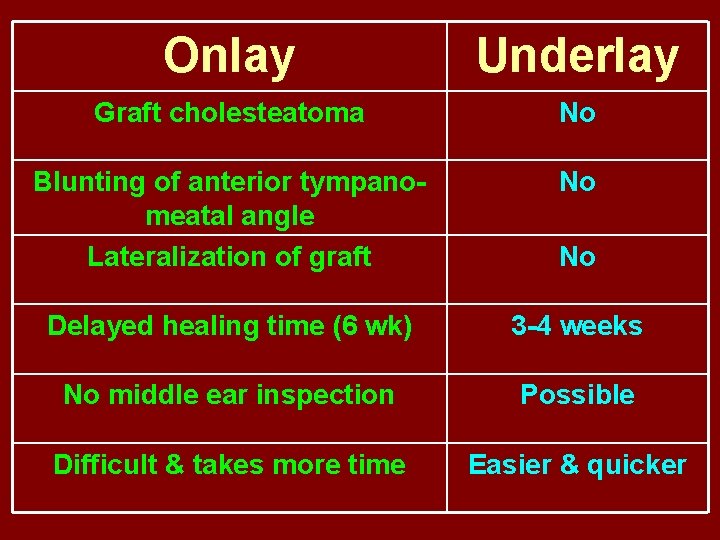
Onlay Underlay Graft cholesteatoma No Blunting of anterior tympanomeatal angle Lateralization of graft No Delayed healing time (6 wk) 3 -4 weeks No middle ear inspection Possible Difficult & takes more time Easier & quicker No
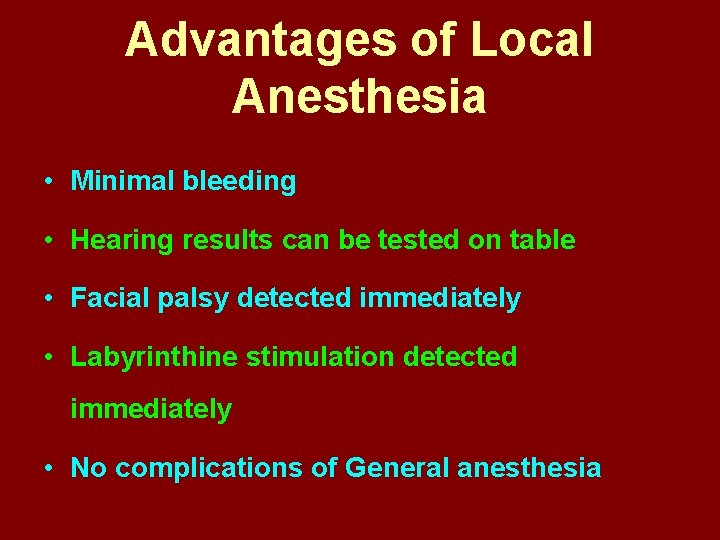
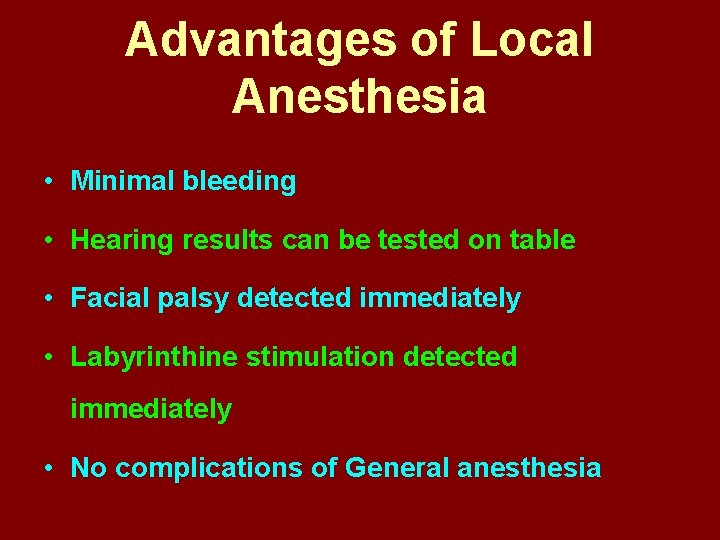
Advantages of Local Anesthesia • Minimal bleeding • Hearing results can be tested on table • Facial palsy detected immediately • Labyrinthine stimulation detected immediately • No complications of General anesthesia
Tympanoplasty
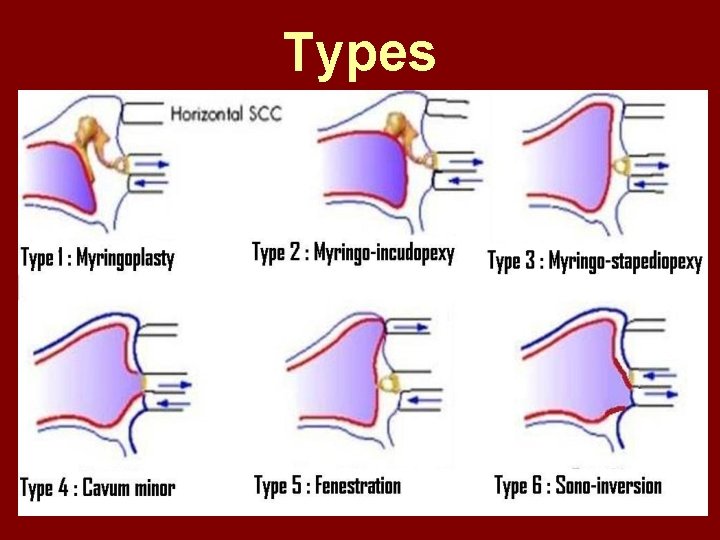
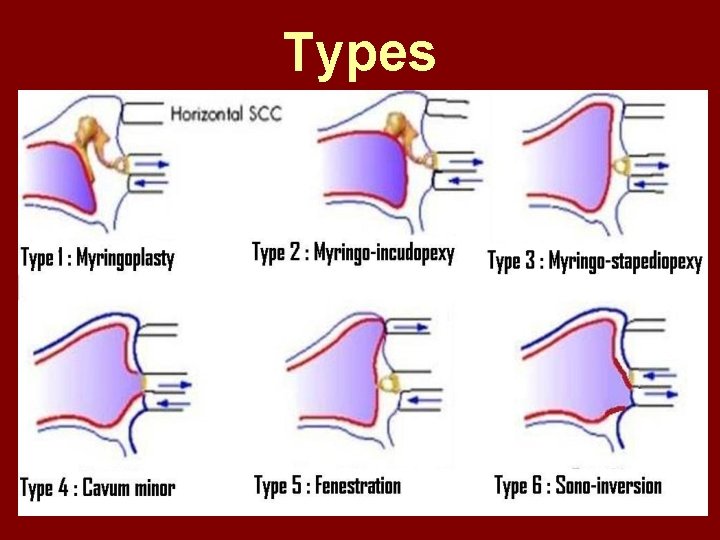
Types
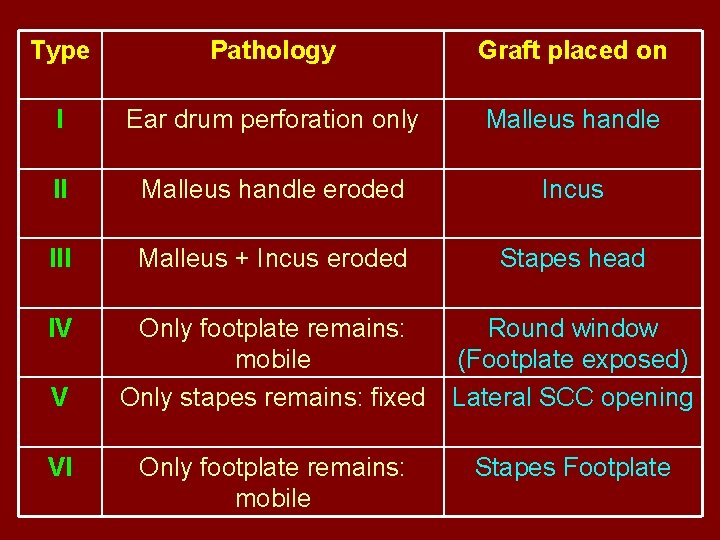
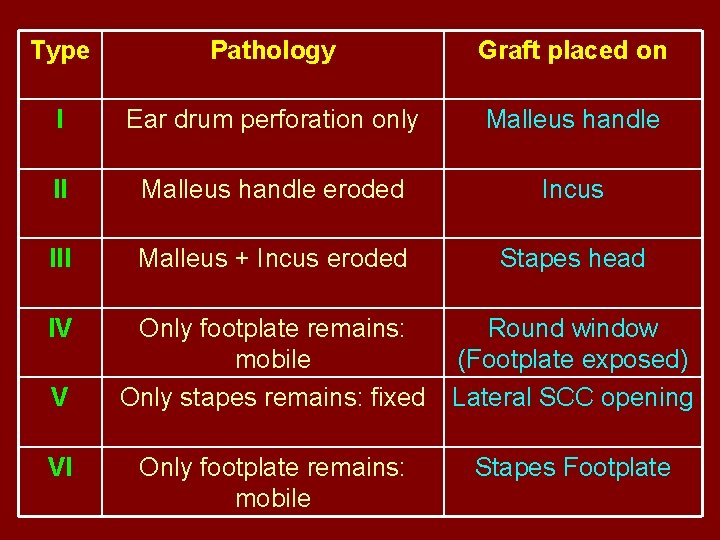
Type Pathology Graft placed on I Ear drum perforation only Malleus handle II Malleus handle eroded Incus III Malleus + Incus eroded Stapes head IV Only footplate remains: mobile Only stapes remains: fixed Round window (Footplate exposed) Lateral SCC opening Only footplate remains: mobile Stapes Footplate V VI
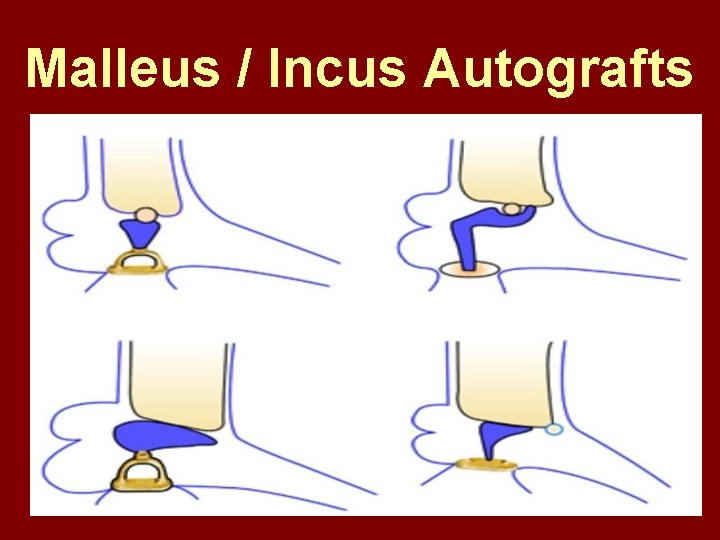
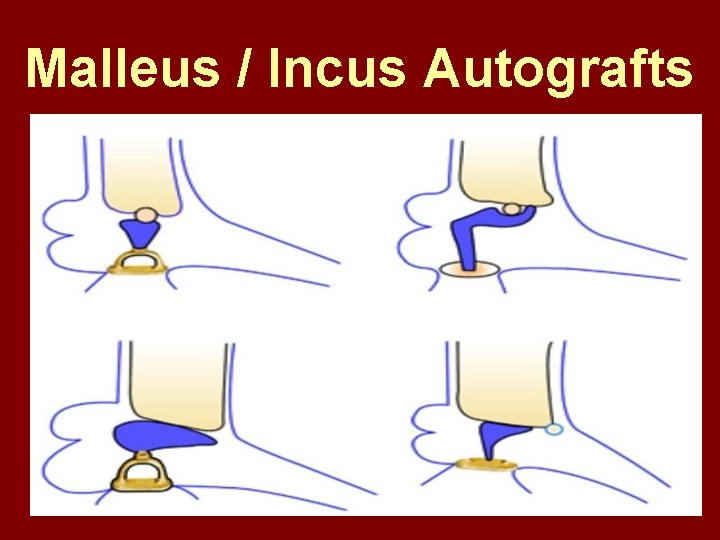
Malleus / Incus Autografts



Thank You
 Vishal patel novartis
Vishal patel novartis Vishal sundaram
Vishal sundaram Vishal thakkar nose
Vishal thakkar nose Plasma cell dyscrasia
Plasma cell dyscrasia Style
Style Dr vishal jaiswal
Dr vishal jaiswal Vishal gupta bits pilani
Vishal gupta bits pilani Principle of surveying
Principle of surveying Camcer
Camcer Link tree vishal tiwari
Link tree vishal tiwari Vishal manghnani
Vishal manghnani Verifact investigations
Verifact investigations Guide to computer forensics and investigations
Guide to computer forensics and investigations Chapter 6 fingerprints
Chapter 6 fingerprints Chs investigations
Chs investigations Chs investigations
Chs investigations Why aren t descriptive investigations repeatable
Why aren t descriptive investigations repeatable 3 weeks pregnant ultrasound
3 weeks pregnant ultrasound Heatherdowns bmv
Heatherdowns bmv Guide to computer forensics and investigations 5th edition
Guide to computer forensics and investigations 5th edition Nrich maths investigations
Nrich maths investigations Statistical investigations unit 3 section a
Statistical investigations unit 3 section a Investigations
Investigations Scientific investigations
Scientific investigations Iliac region
Iliac region Craigslist investigations
Craigslist investigations Statistical investigations examples
Statistical investigations examples Guide to computer forensics and investigations
Guide to computer forensics and investigations Pasco county cpi
Pasco county cpi Sbp prophylaxis guidelines
Sbp prophylaxis guidelines Cholesterol treatment trialists collaboration
Cholesterol treatment trialists collaboration Wast water treatment
Wast water treatment Microvas treatment
Microvas treatment Aspergilloma treatment duration
Aspergilloma treatment duration Hypothyroidism treatment in pregnancy
Hypothyroidism treatment in pregnancy Hyperthyroidism treatment
Hyperthyroidism treatment Class a sludge
Class a sludge Fat embolism treatment
Fat embolism treatment Approach to stridor
Approach to stridor Care and treatment reviews
Care and treatment reviews Julie woodside
Julie woodside Insomnia treatments
Insomnia treatments Dermatitis perioral treatment
Dermatitis perioral treatment Che 333
Che 333 Periodontal treatment of medically compromised patients
Periodontal treatment of medically compromised patients What is hepatitis b
What is hepatitis b Agnosia treatment market trends
Agnosia treatment market trends Deccan water treatment
Deccan water treatment Non allergic rhinitis treatment
Non allergic rhinitis treatment Providing improper or unprofessional treatment or care
Providing improper or unprofessional treatment or care Nails connect
Nails connect Menorrhagia treatment
Menorrhagia treatment Hyponatremia correction formula
Hyponatremia correction formula Trauma awareness and treatment center utah
Trauma awareness and treatment center utah Iddt training
Iddt training