Assay Results vs Selfreported Chlamydial Infections Does Measurement

- Slides: 24
Assay Results vs. Self-reported Chlamydial Infections: Does Measurement Discrepancy Vary by Level of Risk Behavior? Bonita Iritani, 1 Denise Hallfors, 1 Carol A. Ford, 2 Carolyn Tucker Halpern, 2 William C. Miller 2 1 Pacific Institute for Research and Evaluation 2 UNC - Chapel Hill Funded by NIH-NIDA, Denise Hallfors, PI
Reasons for Focusing on Chlamydia Most common bacterial STI Has clear recommendations for screening among females
Sources of Chlamydia Estimates of chlamydial infections often based on reported cases, clinic-based studies Limitations – Not representative of general population – Miss asymptomatic infections Population-based studies that are conducted typically rely on self-reports
Self-reported Infections Limitations of self-reports – Miss asymptomatic infections when screening inadequate Screening recommended for all sexually active females ≤ 25 years – Miss people with poor access to health care – Some respondents may not report accurately (Harrington et al, 2001) By comparing self-reports with biological test results, could look for infections missing from self-reports
Study Objectives Use National Longitudinal Study of Adolescent Health (Add Health) – Nationally representative sample of young adults To assess prevalence of prior chlamydia testing To compare the prevalence of chlamydial infections identified by self-reports vs. assay results
Data Add Health http: //www. cpc. unc. edu/addhealth/ Sample for present analyses: – Wave 3 2001 – 2002 18 -26 years old – Nonmissing data for chlamydia self-reports and assay results (N=12, 359)
Chlamydia Measures Tested for Chlamydia (self-report) – past 12 months Self-report Chlamydia Diagnosis– past 12 months Biological Test of Chlamydia – Urine samples collected at interview
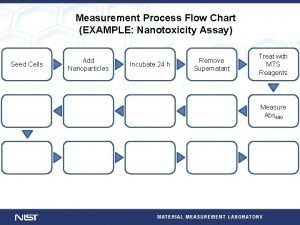
Ratio of Test/Self-report Ratio = biological test prevalence/self-report prevalence – If all infections diagnosed and reported, people having an infection over 12 months > people with infection on one day – Ratio > 1 indicates infections missing in selfreports
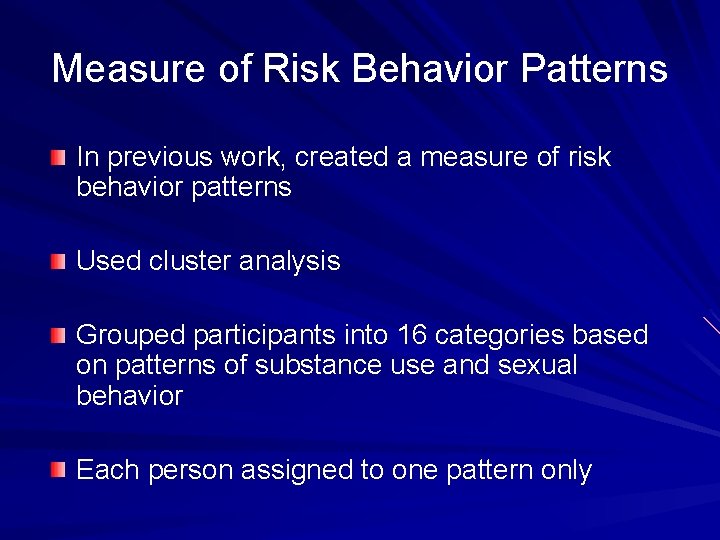
Measure of Risk Behavior Patterns In previous work, created a measure of risk behavior patterns Used cluster analysis Grouped participants into 16 categories based on patterns of substance use and sexual behavior Each person assigned to one pattern only
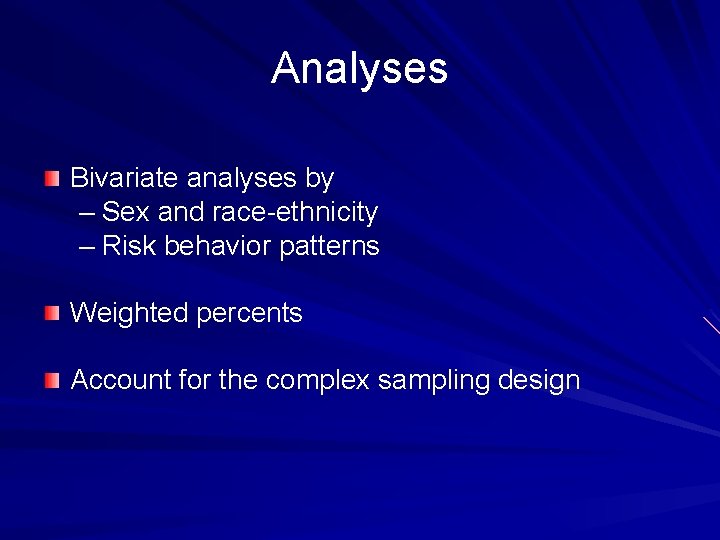
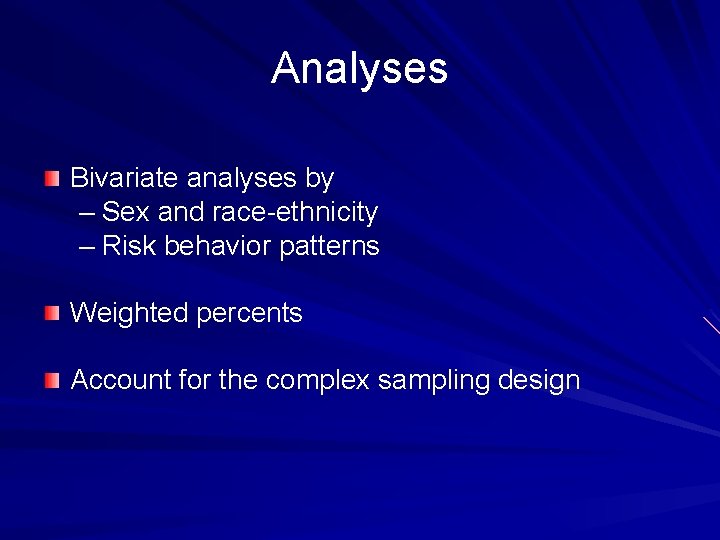
Analyses Bivariate analyses by – Sex and race-ethnicity – Risk behavior patterns Weighted percents Account for the complex sampling design
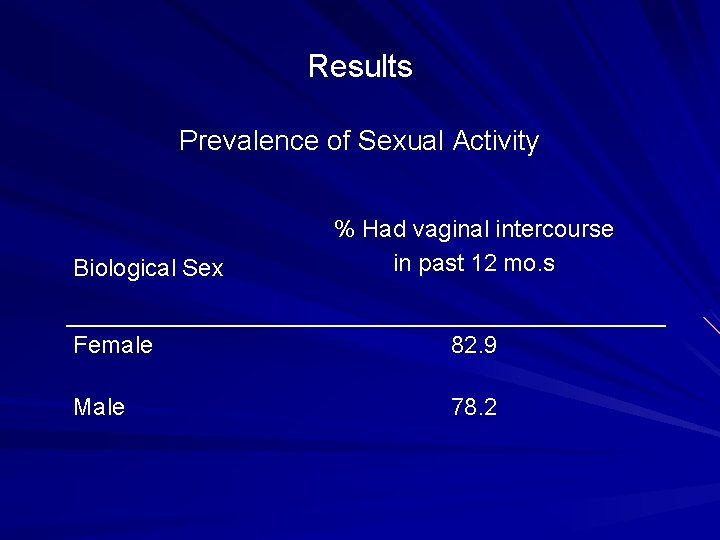
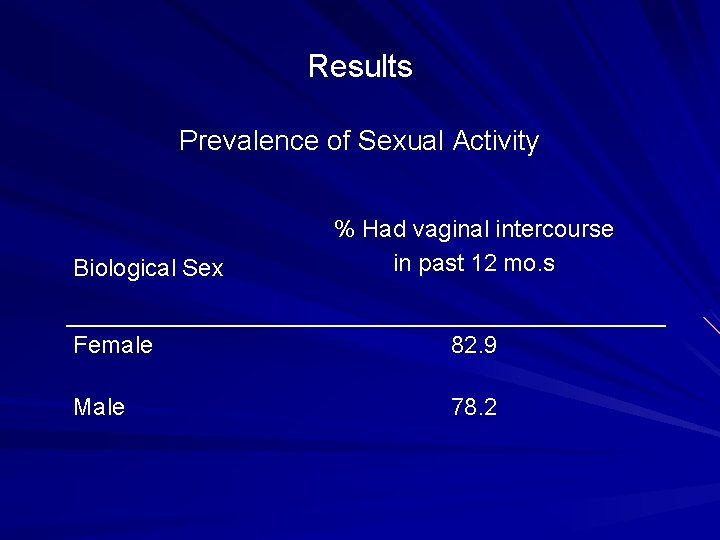
Results Prevalence of Sexual Activity Biological Sex % Had vaginal intercourse in past 12 mo. s Female 82. 9 Male 78. 2
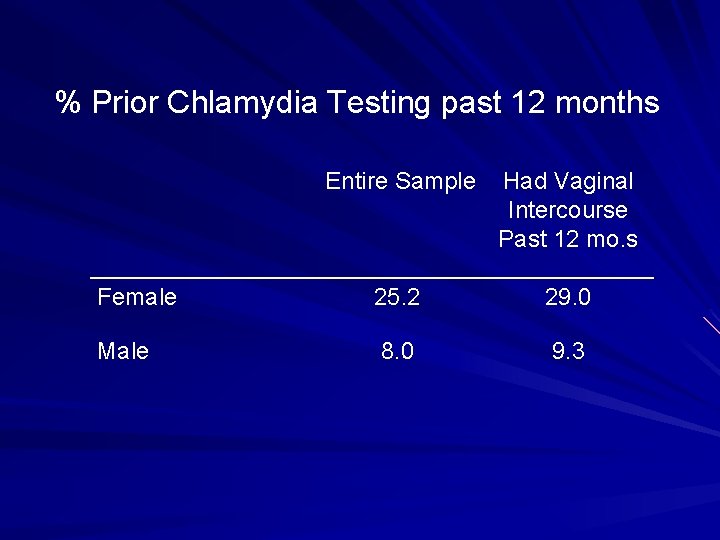
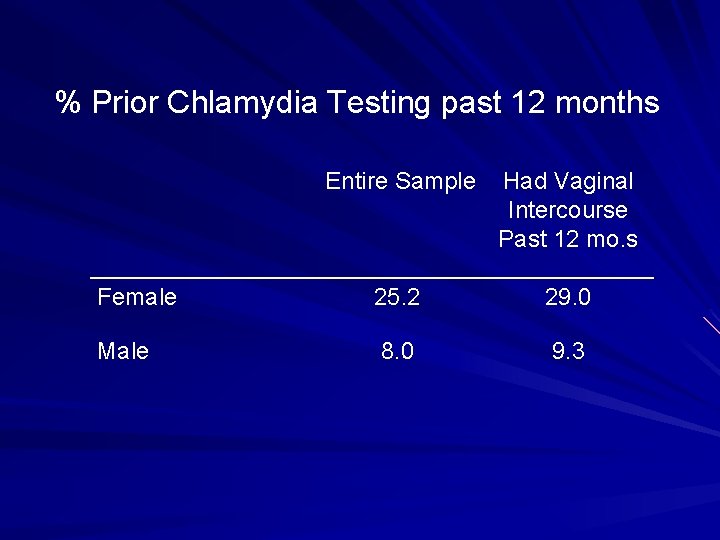
% Prior Chlamydia Testing past 12 months Entire Sample Had Vaginal Intercourse Past 12 mo. s Female 25. 2 29. 0 Male 8. 0 9. 3
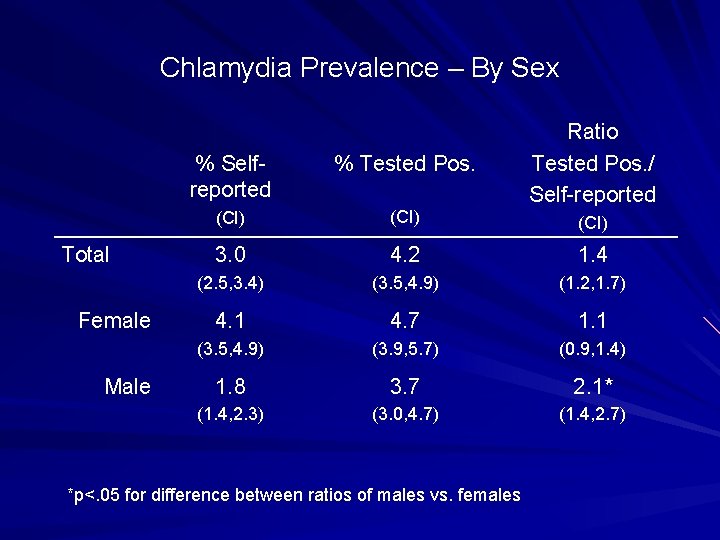
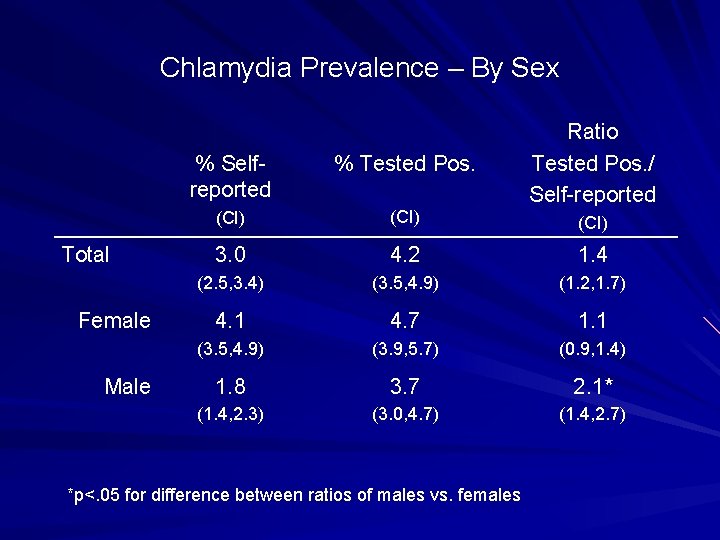
Chlamydia Prevalence – By Sex Total Female Male Ratio Tested Pos. / Self-reported % Selfreported % Tested Pos. (CI) 3. 0 4. 2 1. 4 (2. 5, 3. 4) (3. 5, 4. 9) (1. 2, 1. 7) 4. 1 4. 7 1. 1 (3. 5, 4. 9) (3. 9, 5. 7) (0. 9, 1. 4) 1. 8 3. 7 2. 1* (1. 4, 2. 3) (3. 0, 4. 7) (1. 4, 2. 7) *p<. 05 for difference between ratios of males vs. females (CI)
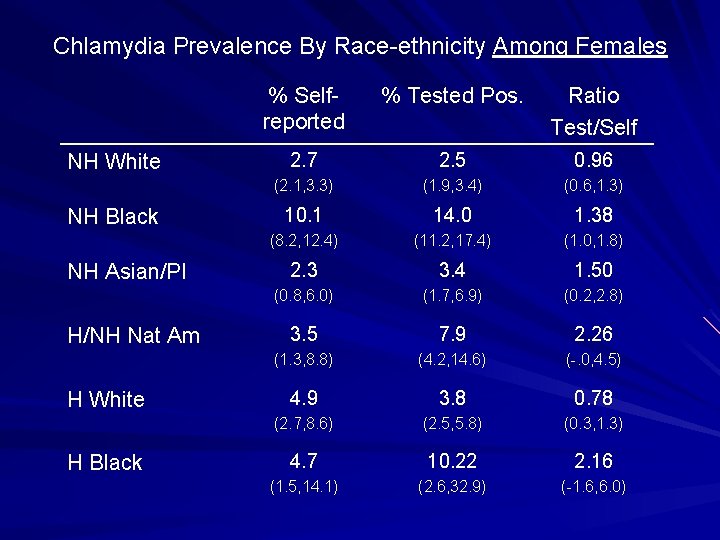
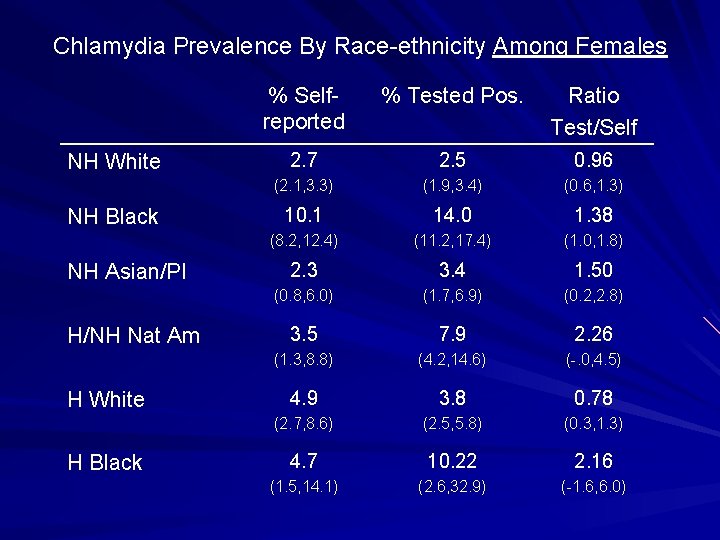
Chlamydia Prevalence By Race-ethnicity Among Females NH White NH Black NH Asian/PI H/NH Nat Am H White H Black % Selfreported % Tested Pos. Ratio Test/Self 2. 7 2. 5 0. 96 (2. 1, 3. 3) (1. 9, 3. 4) (0. 6, 1. 3) 10. 1 14. 0 1. 38 (8. 2, 12. 4) (11. 2, 17. 4) (1. 0, 1. 8) 2. 3 3. 4 1. 50 (0. 8, 6. 0) (1. 7, 6. 9) (0. 2, 2. 8) 3. 5 7. 9 2. 26 (1. 3, 8. 8) (4. 2, 14. 6) (-. 0, 4. 5) 4. 9 3. 8 0. 78 (2. 7, 8. 6) (2. 5, 5. 8) (0. 3, 1. 3) 4. 7 10. 22 2. 16 (1. 5, 14. 1) (2. 6, 32. 9) (-1. 6, 6. 0)
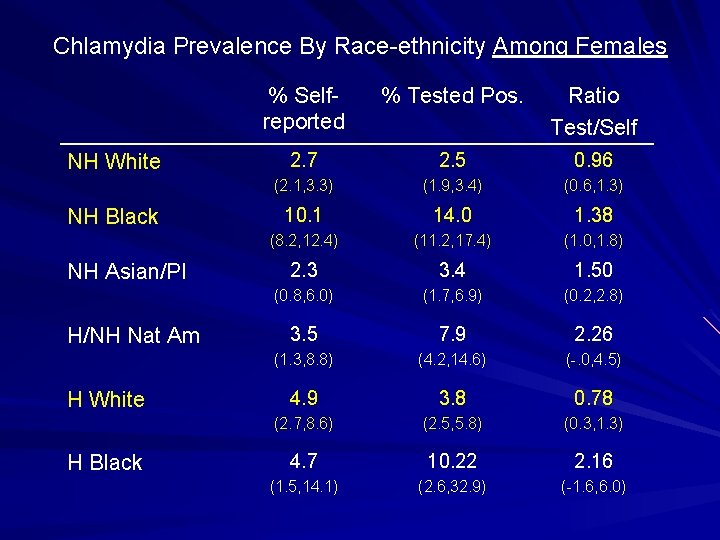
Chlamydia Prevalence By Race-ethnicity Among Females NH White NH Black NH Asian/PI H/NH Nat Am H White H Black % Selfreported % Tested Pos. Ratio Test/Self 2. 7 2. 5 0. 96 (2. 1, 3. 3) (1. 9, 3. 4) (0. 6, 1. 3) 10. 1 14. 0 1. 38 (8. 2, 12. 4) (11. 2, 17. 4) (1. 0, 1. 8) 2. 3 3. 4 1. 50 (0. 8, 6. 0) (1. 7, 6. 9) (0. 2, 2. 8) 3. 5 7. 9 2. 26 (1. 3, 8. 8) (4. 2, 14. 6) (-. 0, 4. 5) 4. 9 3. 8 0. 78 (2. 7, 8. 6) (2. 5, 5. 8) (0. 3, 1. 3) 4. 7 10. 22 2. 16 (1. 5, 14. 1) (2. 6, 32. 9) (-1. 6, 6. 0)
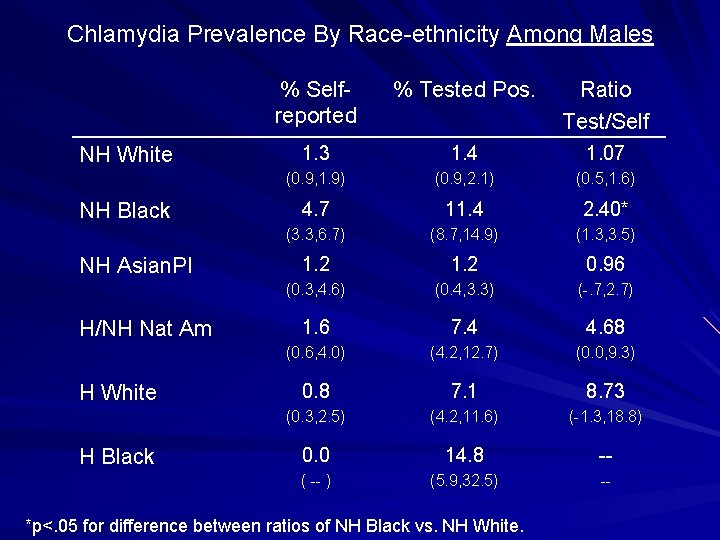
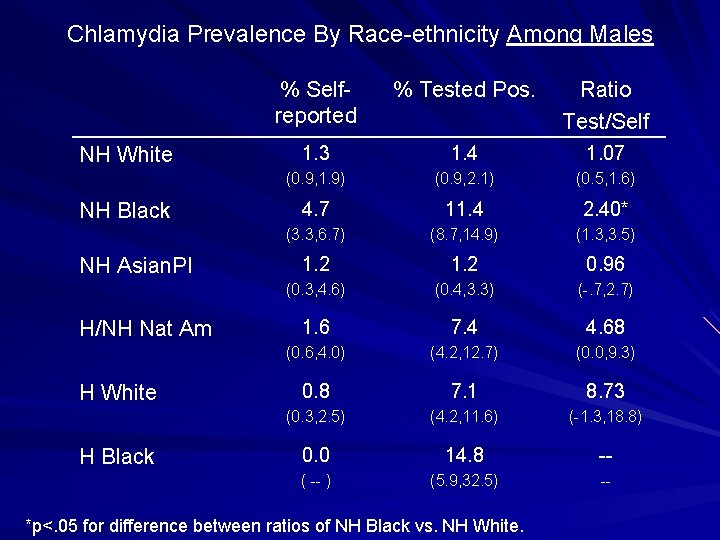
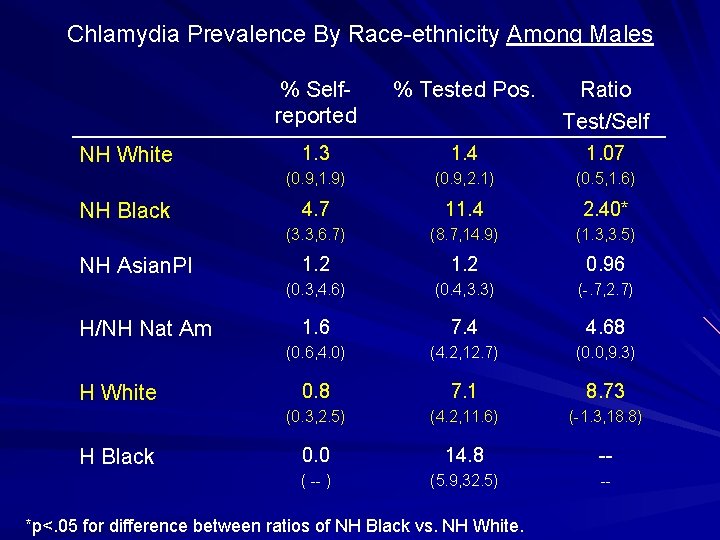
Chlamydia Prevalence By Race-ethnicity Among Males NH White NH Black NH Asian. PI H/NH Nat Am H White H Black % Selfreported % Tested Pos. Ratio Test/Self 1. 3 1. 4 1. 07 (0. 9, 1. 9) (0. 9, 2. 1) (0. 5, 1. 6) 4. 7 11. 4 2. 40* (3. 3, 6. 7) (8. 7, 14. 9) (1. 3, 3. 5) 1. 2 0. 96 (0. 3, 4. 6) (0. 4, 3. 3) (-. 7, 2. 7) 1. 6 7. 4 4. 68 (0. 6, 4. 0) (4. 2, 12. 7) (0. 0, 9. 3) 0. 8 7. 1 8. 73 (0. 3, 2. 5) (4. 2, 11. 6) (-1. 3, 18. 8) 0. 0 14. 8 -- ( -- ) (5. 9, 32. 5) -- *p<. 05 for difference between ratios of NH Black vs. NH White.
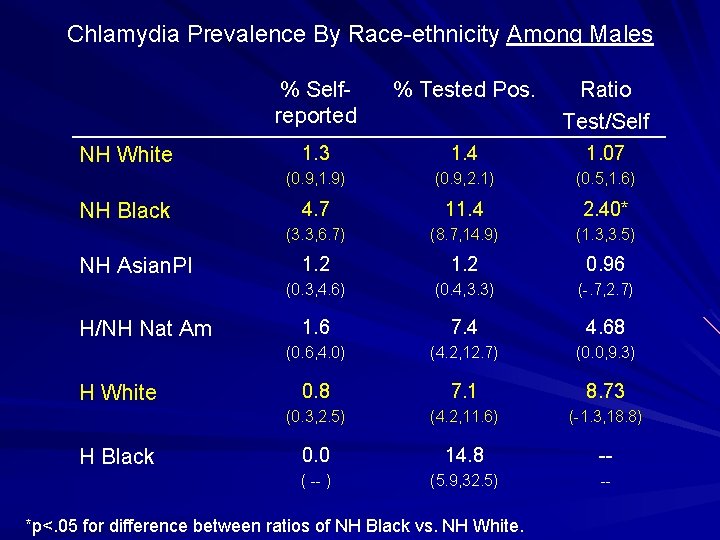
Chlamydia Prevalence By Race-ethnicity Among Males NH White NH Black NH Asian. PI H/NH Nat Am H White H Black % Selfreported % Tested Pos. Ratio Test/Self 1. 3 1. 4 1. 07 (0. 9, 1. 9) (0. 9, 2. 1) (0. 5, 1. 6) 4. 7 11. 4 2. 40* (3. 3, 6. 7) (8. 7, 14. 9) (1. 3, 3. 5) 1. 2 0. 96 (0. 3, 4. 6) (0. 4, 3. 3) (-. 7, 2. 7) 1. 6 7. 4 4. 68 (0. 6, 4. 0) (4. 2, 12. 7) (0. 0, 9. 3) 0. 8 7. 1 8. 73 (0. 3, 2. 5) (4. 2, 11. 6) (-1. 3, 18. 8) 0. 0 14. 8 -- ( -- ) (5. 9, 32. 5) -- *p<. 05 for difference between ratios of NH Black vs. NH White.
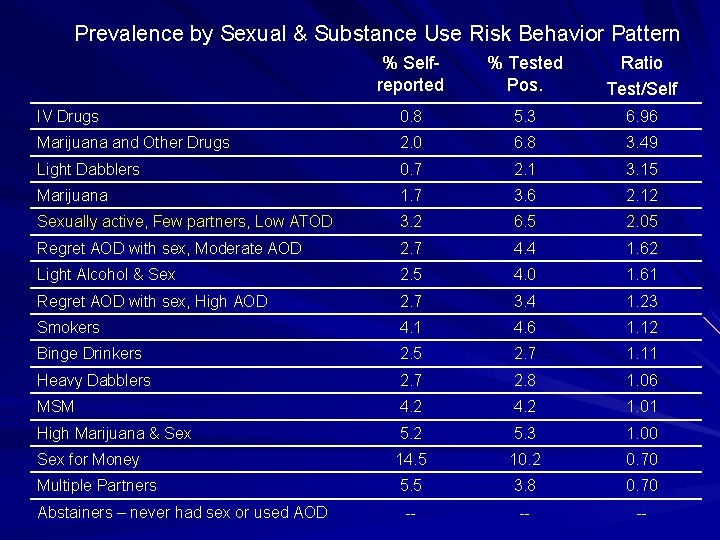
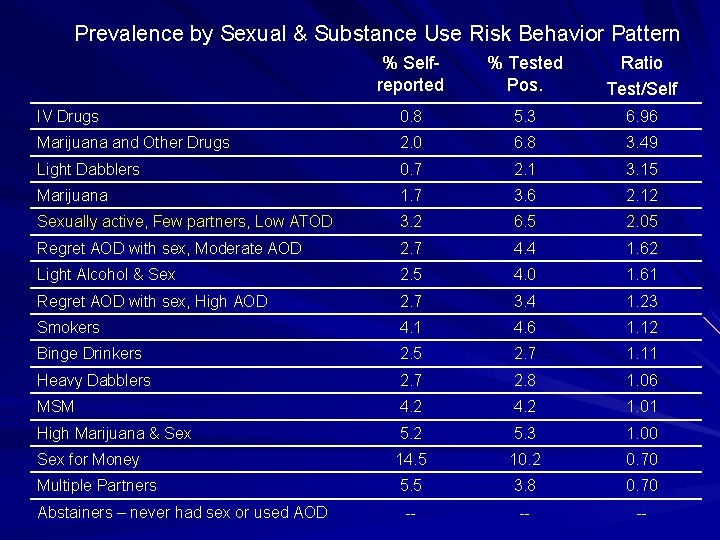
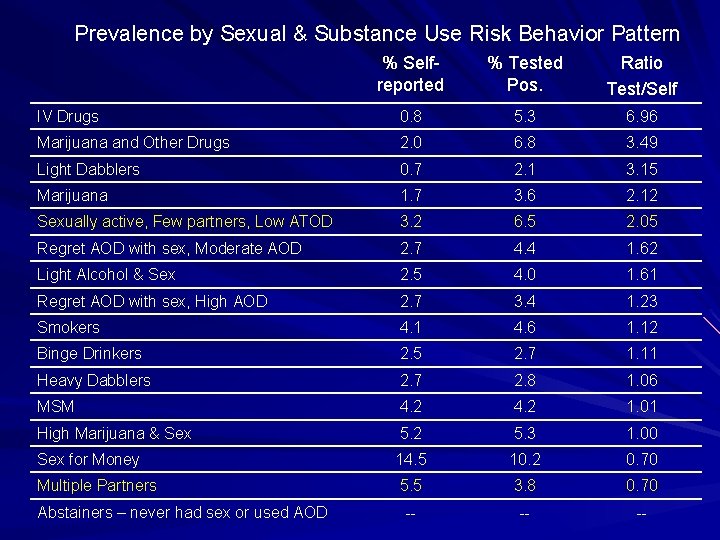
Prevalence by Sexual & Substance Use Risk Behavior Pattern % Selfreported % Tested Pos. Ratio Test/Self IV Drugs 0. 8 5. 3 6. 96 Marijuana and Other Drugs 2. 0 6. 8 3. 49 Light Dabblers 0. 7 2. 1 3. 15 Marijuana 1. 7 3. 6 2. 12 Sexually active, Few partners, Low ATOD 3. 2 6. 5 2. 05 Regret AOD with sex, Moderate AOD 2. 7 4. 4 1. 62 Light Alcohol & Sex 2. 5 4. 0 1. 61 Regret AOD with sex, High AOD 2. 7 3. 4 1. 23 Smokers 4. 1 4. 6 1. 12 Binge Drinkers 2. 5 2. 7 1. 11 Heavy Dabblers 2. 7 2. 8 1. 06 MSM 4. 2 1. 01 High Marijuana & Sex 5. 2 5. 3 1. 00 Sex for Money 14. 5 10. 2 0. 70 Multiple Partners 5. 5 3. 8 0. 70 -- -- -- Abstainers – never had sex or used AOD
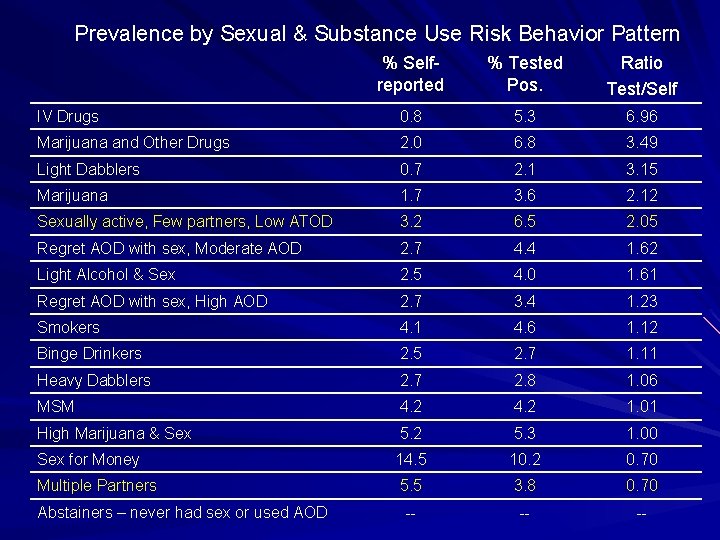
Prevalence by Sexual & Substance Use Risk Behavior Pattern % Selfreported % Tested Pos. Ratio Test/Self IV Drugs 0. 8 5. 3 6. 96 Marijuana and Other Drugs 2. 0 6. 8 3. 49 Light Dabblers 0. 7 2. 1 3. 15 Marijuana 1. 7 3. 6 2. 12 Sexually active, Few partners, Low ATOD 3. 2 6. 5 2. 05 Regret AOD with sex, Moderate AOD 2. 7 4. 4 1. 62 Light Alcohol & Sex 2. 5 4. 0 1. 61 Regret AOD with sex, High AOD 2. 7 3. 4 1. 23 Smokers 4. 1 4. 6 1. 12 Binge Drinkers 2. 5 2. 7 1. 11 Heavy Dabblers 2. 7 2. 8 1. 06 MSM 4. 2 1. 01 High Marijuana & Sex 5. 2 5. 3 1. 00 Sex for Money 14. 5 10. 2 0. 70 Multiple Partners 5. 5 3. 8 0. 70 -- -- -- Abstainers – never had sex or used AOD
Conclusions Prevalence of chlamydia testing is low – Screening guidelines for females not achieved (only 29% of sexually active young women were tested)
Infections Missing from Self-reports 4% were infected on interview day, but only 3% self-reported infection in entire past 12 months Infections particularly missing among – males compared to females – NH black males compared to white males – Some lower risk behavior categories
Possible Reasons Some respondents may not be answering accurately Many infections are undiagnosed – Due to low levels of chlamydia screening
Acknowledgments This research was supported by grant R 01 -DA 14496 -4 from the National Institute on Drug Abuse, Denise Hallfors, PI. We thank Martha W. Waller and Jon M. Hussey for consultation. This research uses data from Add Health, a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by a grant P 01 -HD 31921 from the National Institute of Child Health and Human Development, with cooperative funding from 17 other agencies. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Persons interested in obtaining data files from Add Health should contact Add Health, Carolina Population Center, 123 W. Franklin Street, Chapel Hill, NC 27516 -2524 (www. cpc. unc. edu/addhealth/contract. html).

 Opportunistic infections
Opportunistic infections Methotrexate yeast infection
Methotrexate yeast infection Opportunistic infections
Opportunistic infections A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Understanding the mirai botnet
Understanding the mirai botnet Storch infections
Storch infections Storch infections
Storch infections Bone and joint infections
Bone and joint infections Infections opportunistes digestives
Infections opportunistes digestives Eye infections
Eye infections Postpartum infections
Postpartum infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Genital infections
Genital infections Genital infections
Genital infections Cell lysis complement system
Cell lysis complement system Acute gingival infections
Acute gingival infections Christian warburg assay
Christian warburg assay Local lymph node assay
Local lymph node assay Bca assay 원리
Bca assay 원리 Sucrose lysis test
Sucrose lysis test Asante hiv-1 rapid recency assay
Asante hiv-1 rapid recency assay Principle of assay of ibuprofen
Principle of assay of ibuprofen Assay of sodium benzoate
Assay of sodium benzoate Photon assay technology
Photon assay technology Betatace
Betatace