Arteries are thickwalled vessels that transport O 2




- Slides: 25

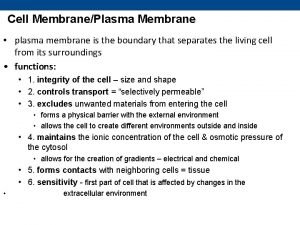
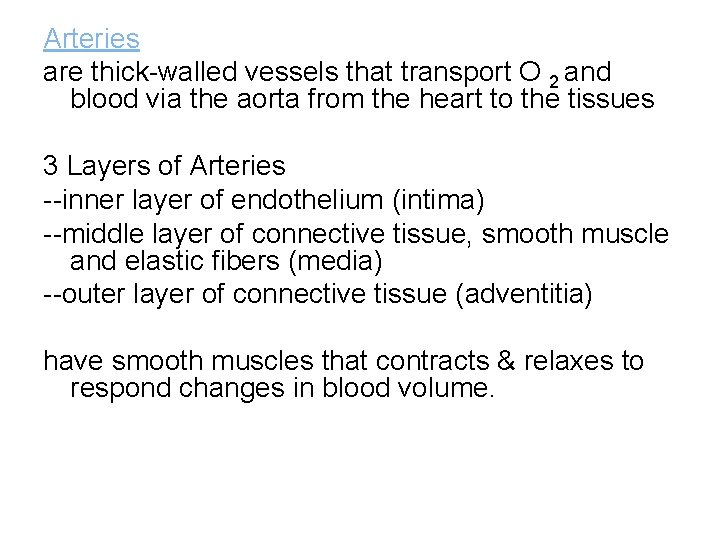
Arteries are thick-walled vessels that transport O 2 and blood via the aorta from the heart to the tissues 3 Layers of Arteries --inner layer of endothelium (intima) --middle layer of connective tissue, smooth muscle and elastic fibers (media) --outer layer of connective tissue (adventitia) have smooth muscles that contracts & relaxes to respond changes in blood volume.
• Veins are thin-walled vessels that transport deoxygenated blood from the capillaries back to the right side of the heart • 3 Layers – intima, media, adventitia there is little smooth muscle & connective tissue • makes the veins more distensible they accumulate large volumes of blood • Major veins, particularly in the lower extremities, have one-way valves--- allow blood flow against gravity • Valves allow blood to be pumped back to the heart but prevent it from draining back into the periphery
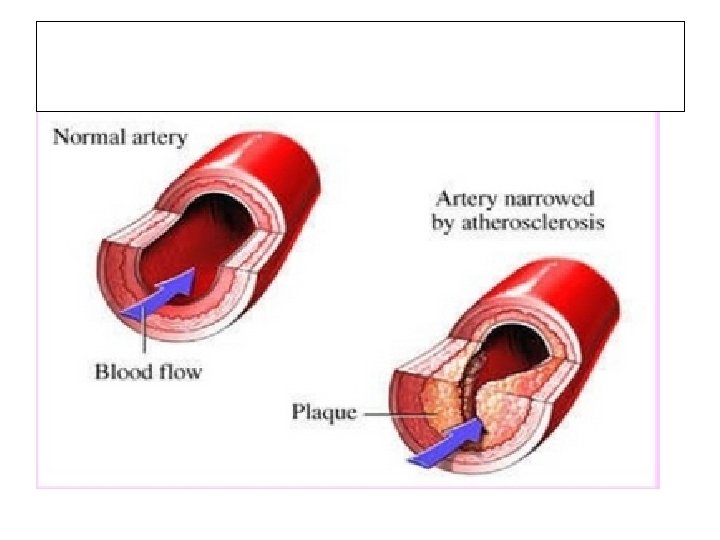
PHERIPHERAL ARTERIAL DISEASE • Definition: stenosis or occlusion in the aorta or arteries of the limbs, that leads to reduction in blood flow and hence 0 2 through the peripheral vessels • The decreased blood flow results in nerve and tissue damage to the extremities
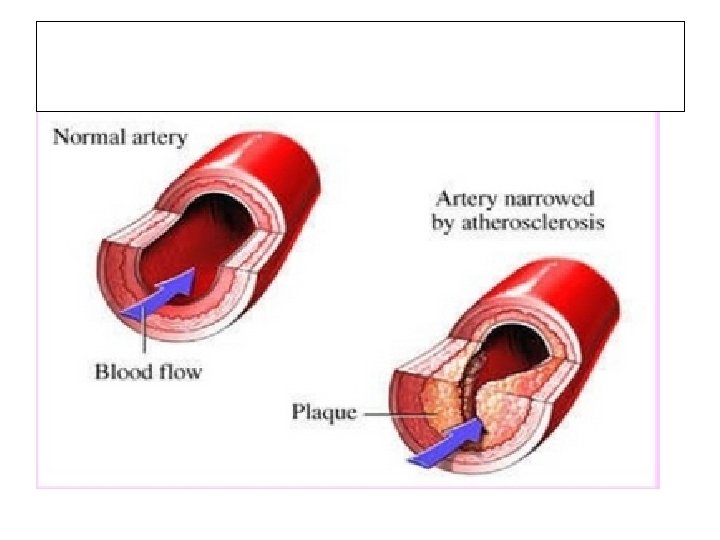
• atherosclerosis is the leading cause of PAD in patients >40 years old • other causes: -thrombosis -embolism -vasculitis -fibromuscular dysplasia -entrapment -cystic adventitial disease -trauma


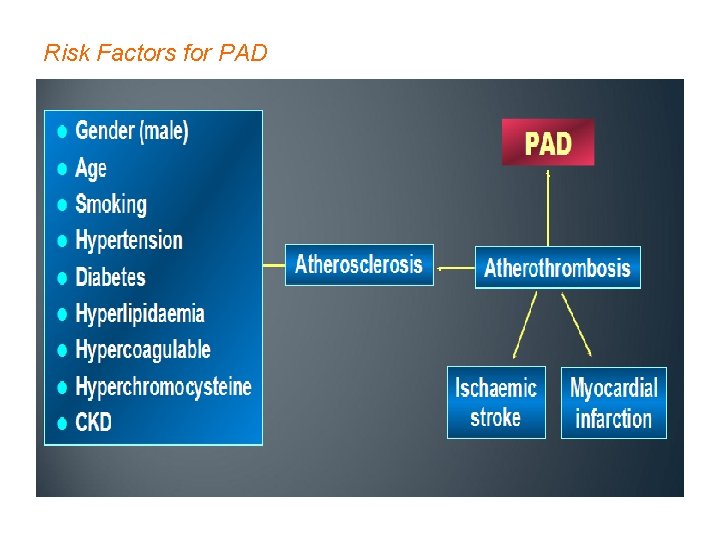
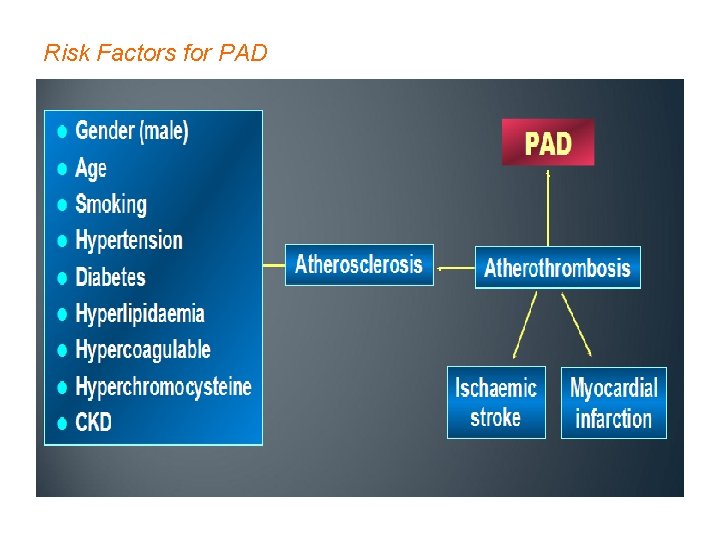
Risk Factors for PAD
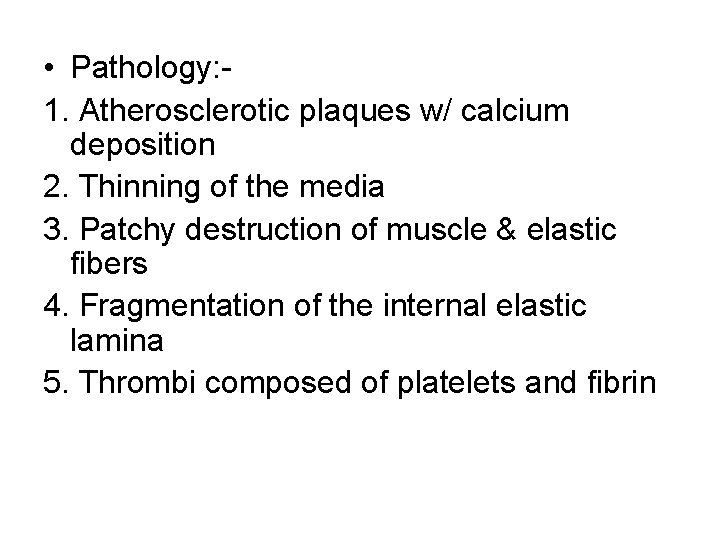
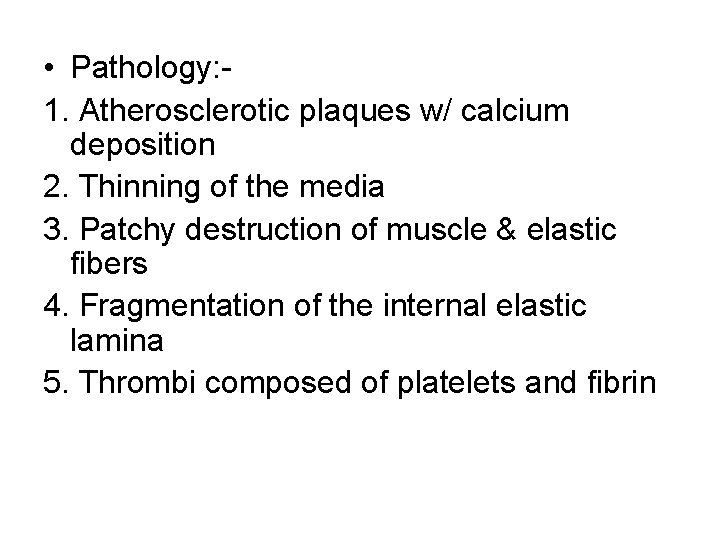
• Pathology: - 1. Atherosclerotic plaques w/ calcium deposition 2. Thinning of the media 3. Patchy destruction of muscle & elastic fibers 4. Fragmentation of the internal elastic lamina 5. Thrombi composed of platelets and fibrin
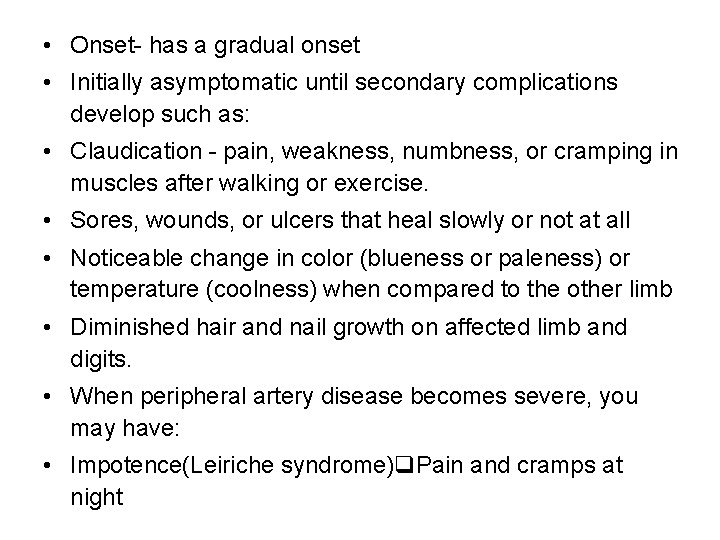
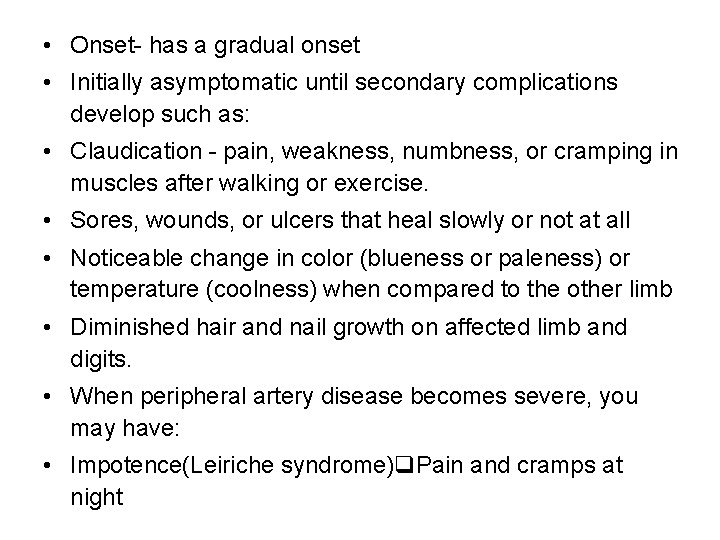
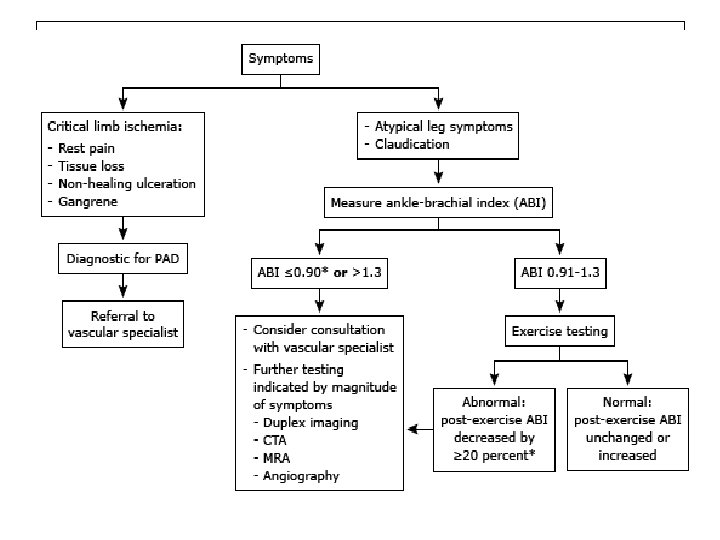
• Onset- has a gradual onset • Initially asymptomatic until secondary complications develop such as: • Claudication - pain, weakness, numbness, or cramping in muscles after walking or exercise. • Sores, wounds, or ulcers that heal slowly or not at all • Noticeable change in color (blueness or paleness) or temperature (coolness) when compared to the other limb • Diminished hair and nail growth on affected limb and digits. • When peripheral artery disease becomes severe, you may have: • Impotence(Leiriche syndrome) Pain and cramps at night
The 5 P’s • Pulselessness • Paralysis • Paraesthesia • Pain • Pallor

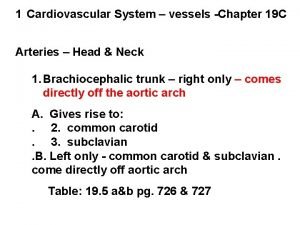
• Primary sites of involvement: 1. femoral and popliteal arteries 2. tibial and peroneal 3. abdominal aorta and iliac arteries atherosclerotic lesions occur preferentially at : a. ) arterial branch pointsb. b) sites of increased turbulencec. c) altered shear stressd. d) site of intimal injury
INTERMITTENT CLAUDICATION • Definition: pain, ache, cramp, numbness or sense of fatigue in the muscles, occurs during exercise and relieved by rest. • common in lower than upper extremities the site of claudication is DISTAL to the location of the occlusive lesion
• Buttock and hip – aortoiliac disease Leriche syndrome triad - claudication, absent femoral pulses and erectile dysfunction. • Thigh – aortoiliac or common femoral artery • Upper two-thirds of the calf – superficial femoral artery • Lower one-third of the calf – popliteal artery • Foot claudication – tibial or peroneal artery
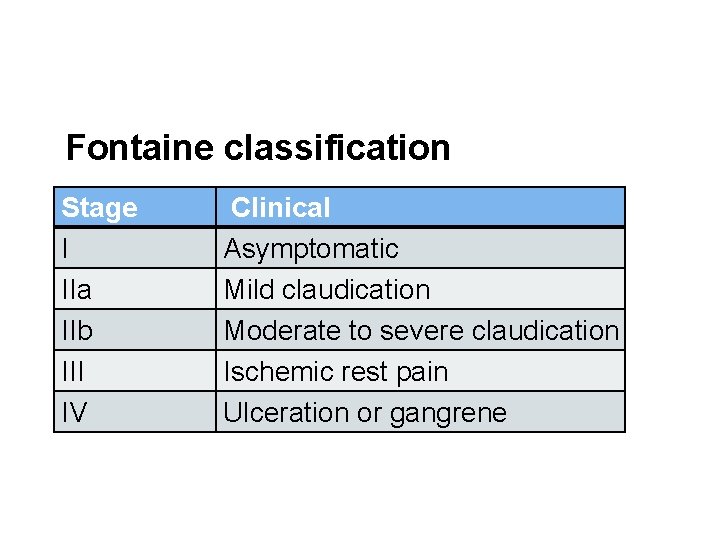
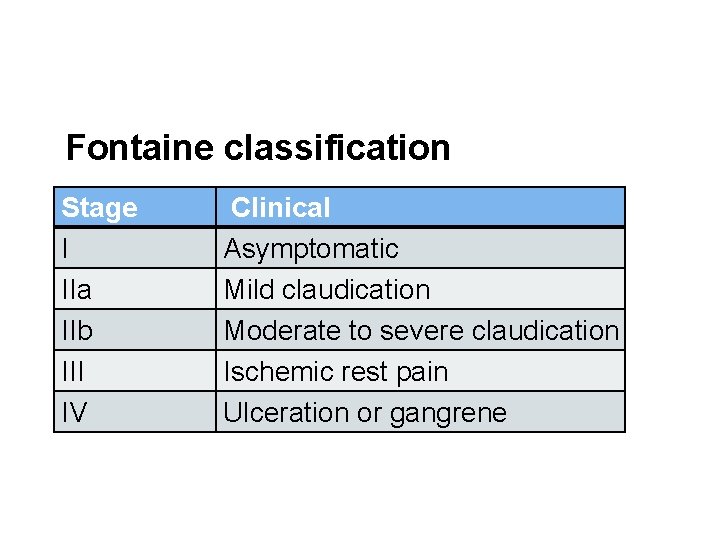
Fontaine classification Stage I IIa IIb III IV Clinical Asymptomatic Mild claudication Moderate to severe claudication Ischemic rest pain Ulceration or gangrene
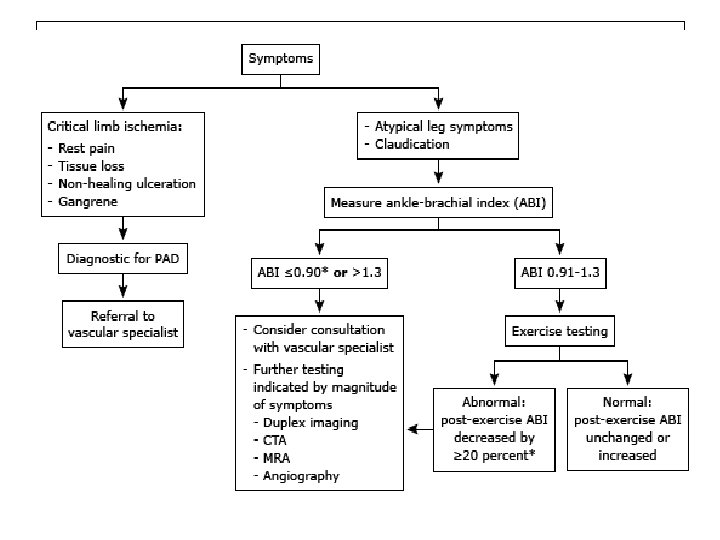
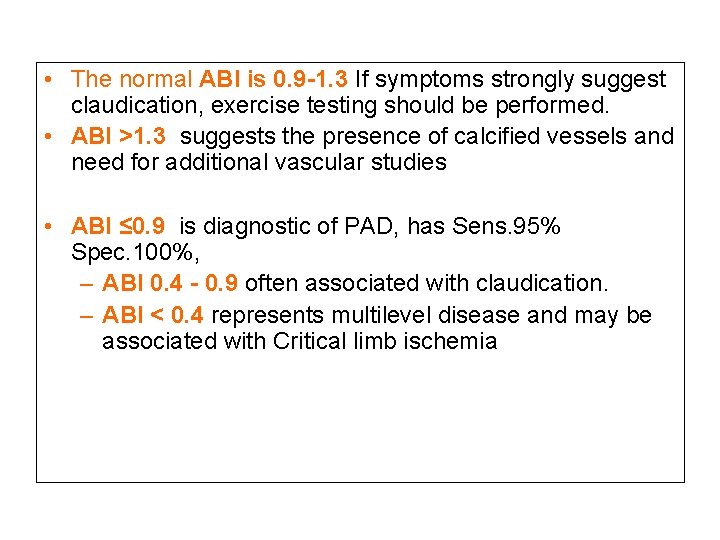
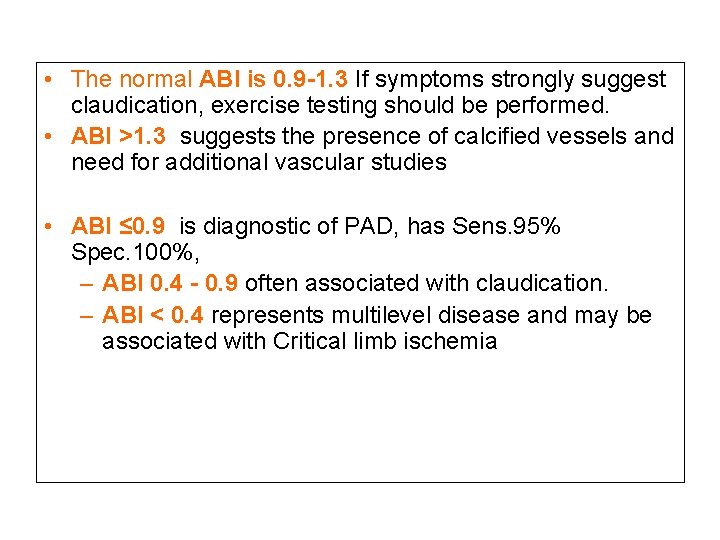
• The normal ABI is 0. 9 -1. 3 If symptoms strongly suggest claudication, exercise testing should be performed. • ABI >1. 3 suggests the presence of calcified vessels and need for additional vascular studies • ABI ≤ 0. 9 is diagnostic of PAD, has Sens. 95% Spec. 100%, – ABI 0. 4 - 0. 9 often associated with claudication. – ABI < 0. 4 represents multilevel disease and may be associated with Critical limb ischemia
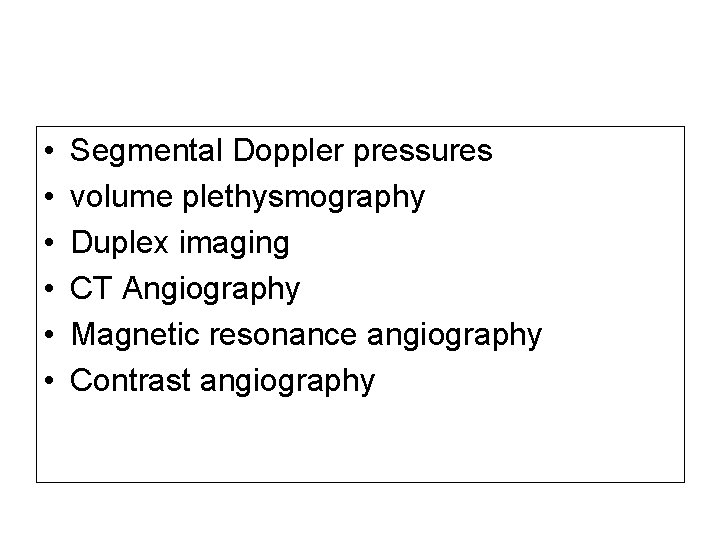
• • • Segmental Doppler pressures volume plethysmography Duplex imaging CT Angiography Magnetic resonance angiography Contrast angiography
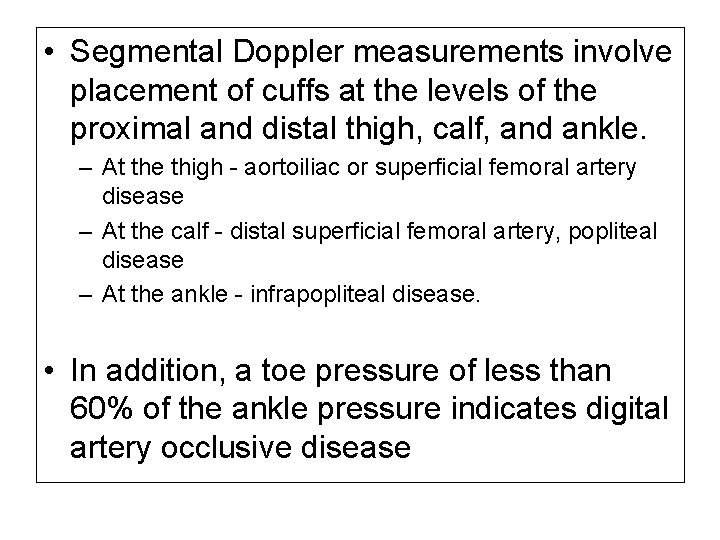
• Segmental Doppler measurements involve placement of cuffs at the levels of the proximal and distal thigh, calf, and ankle. – At the thigh - aortoiliac or superficial femoral artery disease – At the calf - distal superficial femoral artery, popliteal disease – At the ankle - infrapopliteal disease. • In addition, a toe pressure of less than 60% of the ankle pressure indicates digital artery occlusive disease
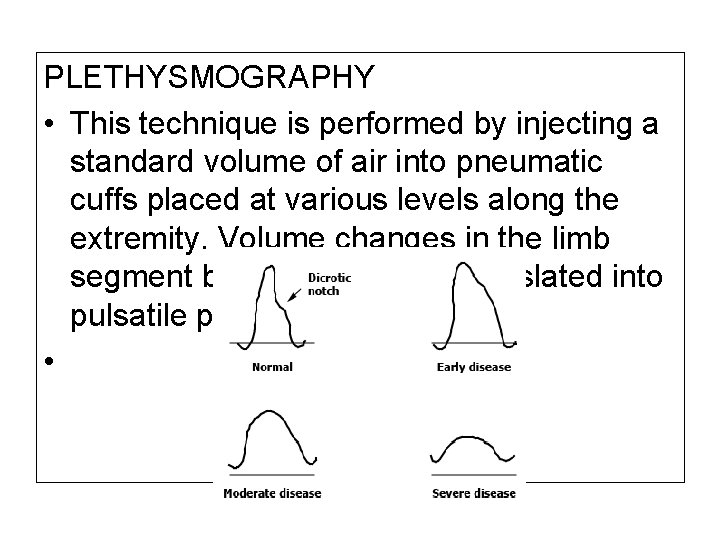
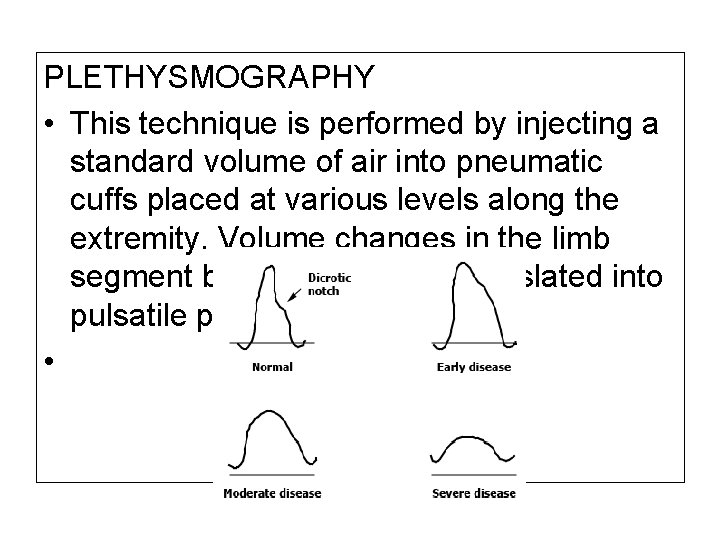
PLETHYSMOGRAPHY • This technique is performed by injecting a standard volume of air into pneumatic cuffs placed at various levels along the extremity. Volume changes in the limb segment below the cuff are translated into pulsatile pressure. •
DUPLEX IMAGING • in experienced hands, provide accurate localization and quantification of lesions; it can also help differentiate stenosis from occlusions, an advantage over segmental Doppler pressures or plethysmography. • However, a great deal of time and expertise are required, this modality is not the first choice for screening. • useful tool in following known lesions for evidence of progression and for monitoring vascular reconstructions
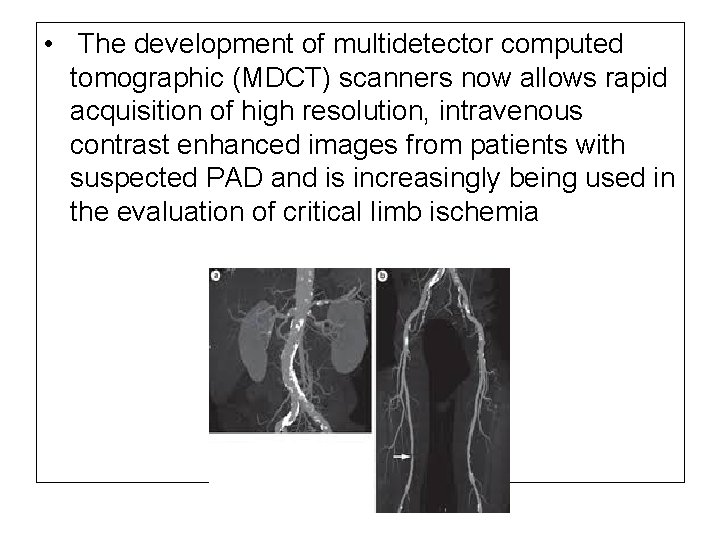
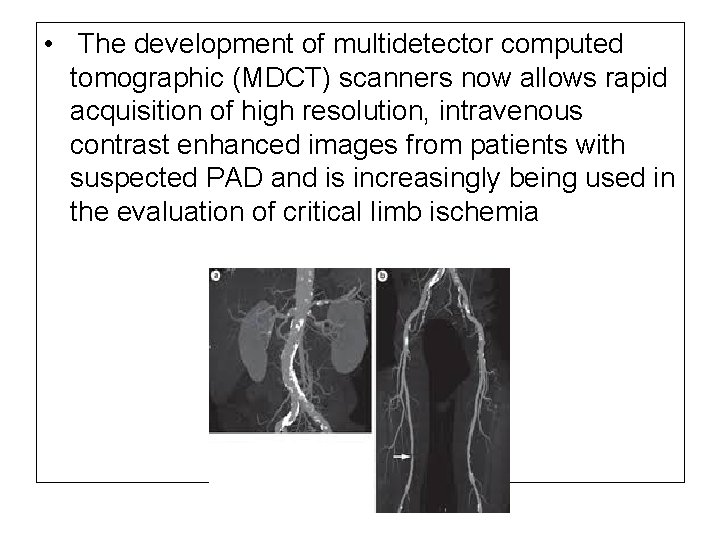
• The development of multidetector computed tomographic (MDCT) scanners now allows rapid acquisition of high resolution, intravenous contrast enhanced images from patients with suspected PAD and is increasingly being used in the evaluation of critical limb ischemia
• remains the gold standard • It should be performed in patients without a contraindication who are expected to undergo revascularization. • A complete study of the aorta, iliac, femoral, popliteal, and run-off vessels is usually done on both sides since atherosclerotic disease is usually bilateral and occurs at multiple levels
 Antigentest åre
Antigentest åre Chiến lược kinh doanh quốc tế của walmart
Chiến lược kinh doanh quốc tế của walmart Gây tê cơ vuông thắt lưng
Gây tê cơ vuông thắt lưng Block xoang nhĩ độ 2 type 1
Block xoang nhĩ độ 2 type 1 Tìm độ lớn thật của tam giác abc
Tìm độ lớn thật của tam giác abc Sau thất bại ở hồ điển triệt
Sau thất bại ở hồ điển triệt Thể thơ truyền thống
Thể thơ truyền thống Hãy nói thật ít để làm được nhiều
Hãy nói thật ít để làm được nhiều Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Tôn thất thuyết là ai
Tôn thất thuyết là ai Ngoại tâm thu thất chùm đôi
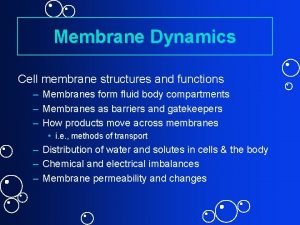
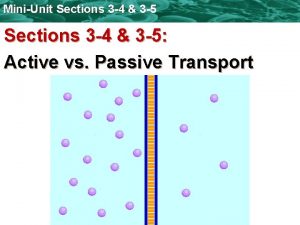
Ngoại tâm thu thất chùm đôi Primary active transport and secondary active transport
Primary active transport and secondary active transport Unlike passive transport, active transport requires *
Unlike passive transport, active transport requires * Bioflix activity membrane transport diffusion
Bioflix activity membrane transport diffusion Passive transport vs active transport venn diagram
Passive transport vs active transport venn diagram Primary active transport vs secondary active transport
Primary active transport vs secondary active transport Bioflix activity membrane transport active transport
Bioflix activity membrane transport active transport Active vs passive transport venn diagram
Active vs passive transport venn diagram Primary vs secondary active transport
Primary vs secondary active transport Passive trnasport
Passive trnasport Anastomsis
Anastomsis Respiratory system nasal cavity
Respiratory system nasal cavity Endothelium
Endothelium Arteries, veins, capillaries
Arteries, veins, capillaries Arteries of the upper limb
Arteries of the upper limb Axillary artery branches
Axillary artery branches