AQA A Level Psychology Paper 3 Schizophrenia Lesson
- Slides: 35
AQA A Level Psychology Paper 3: Schizophrenia Lesson 1 – What is Schizophrenia?
What is Schizophrenia? Schizophrenia is a serious psychological disorder characterised by severe disruptions in psychological functioning and a loss of contact with reality. • The symptoms of Schizophrenia are typically divided into positive and negative symptoms. • Positive symptoms are those which appear to reflect an excess or distortion of normal functions. • Negative symptoms are those that appear to reflect a diminution or loss of normal functions which often appear during periods of low or absent positive symptoms. • Diagnosis of Schizophrenia requires a months duration of two or more positive symptoms.
Clinical Characteristics; Some facts and figures… • In most countries the life time risk of being diagnosed with schizophrenia is 1%. • Usually onsets between the ages of 15 and 45. • Equally common in both genders. • Appears in men 4 or 5 years earlier than women. • Distinction; – Acute; appears suddenly (usually after a stressful time) very disturbed behaviour. – Chronic; a gradual change, after months or years of deterioration, more obvious signs appear (hallucination)
What is Schizophrenia? Positive and Negative Symptoms • The symptoms of Schizophrenia are typically divided into positive and negative symptoms. • Positive symptoms are those which appear to reflect an excess or distortion of normal functions. • Negative symptoms are those that appear to reflect a diminution or loss of normal functions which often appear during periods of low or absent positive symptoms. • Diagnosis of Schizophrenia requires a months duration of two or more positive symptoms.
Specification Content; What the AQA say you should know… • Reliability and validity in diagnosis and classification schizophrenia, including reference to: 1. 2. 3. 4. Co-morbidity Culture Bias Gender Bias Symptom Overlap
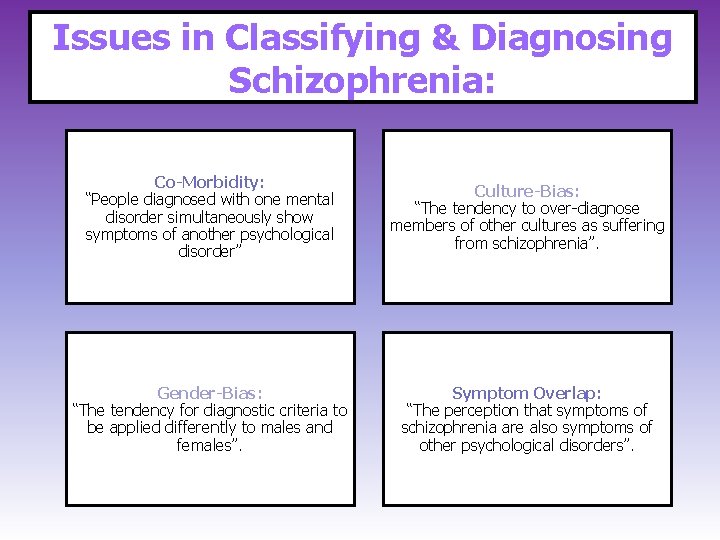
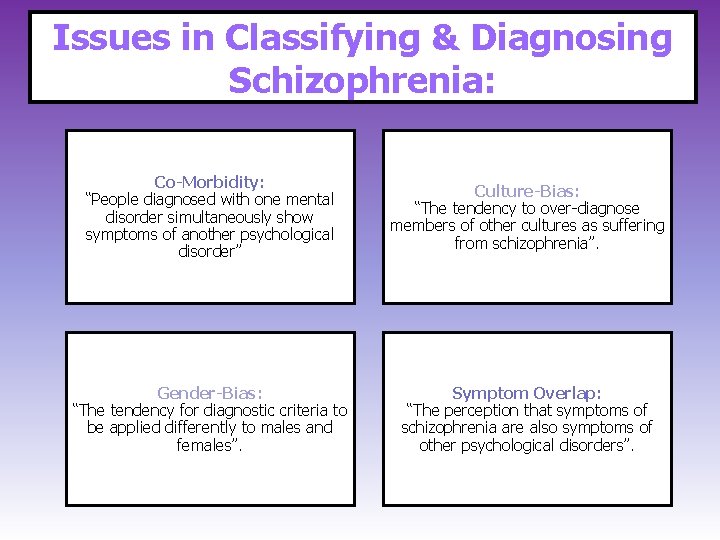
Issues in Classifying & Diagnosing Schizophrenia: Co-Morbidity: “People diagnosed with one mental disorder simultaneously show symptoms of another psychological disorder” Culture-Bias: “The tendency to over-diagnose members of other cultures as suffering from schizophrenia”. Gender-Bias: “The tendency for diagnostic criteria to be applied differently to males and females”. Symptom Overlap: “The perception that symptoms of schizophrenia are also symptoms of other psychological disorders”.
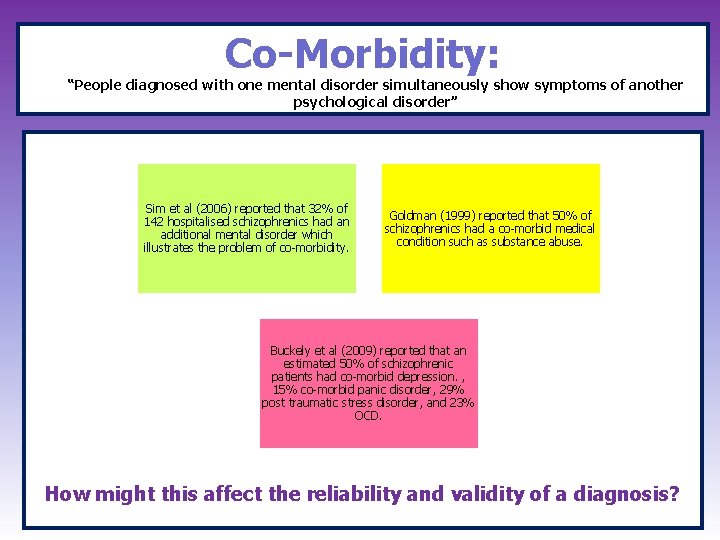
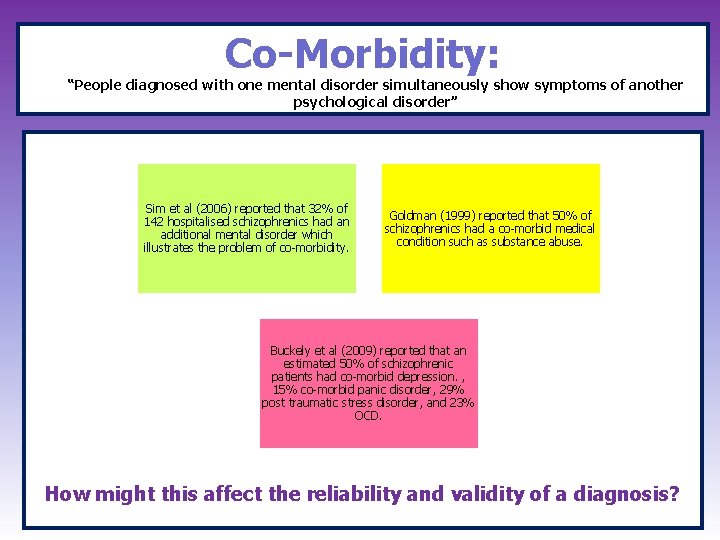
Co-Morbidity: “People diagnosed with one mental disorder simultaneously show symptoms of another psychological disorder” Sim et al (2006) reported that 32% of 142 hospitalised schizophrenics had an additional mental disorder which illustrates the problem of co-morbidity. Goldman (1999) reported that 50% of schizophrenics had a co-morbid medical condition such as substance abuse. Buckely et al (2009) reported that an estimated 50% of schizophrenic patients had co-morbid depression. , 15% co-morbid panic disorder, 29% post traumatic stress disorder, and 23% OCD. How might this affect the reliability and validity of a diagnosis?
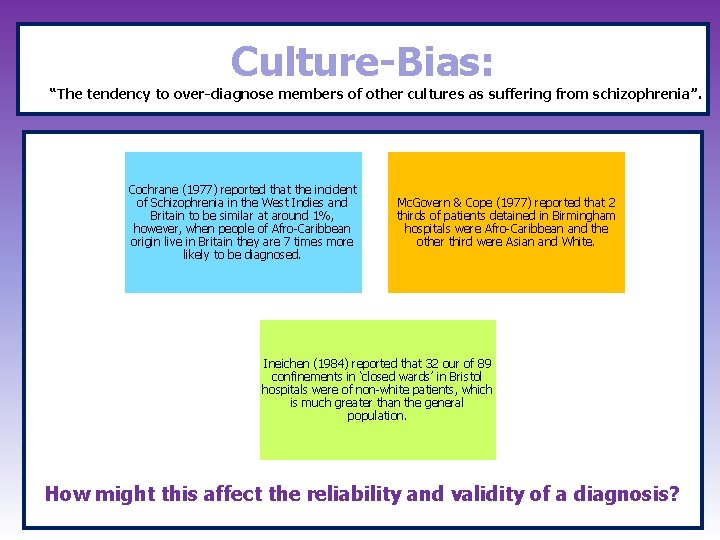
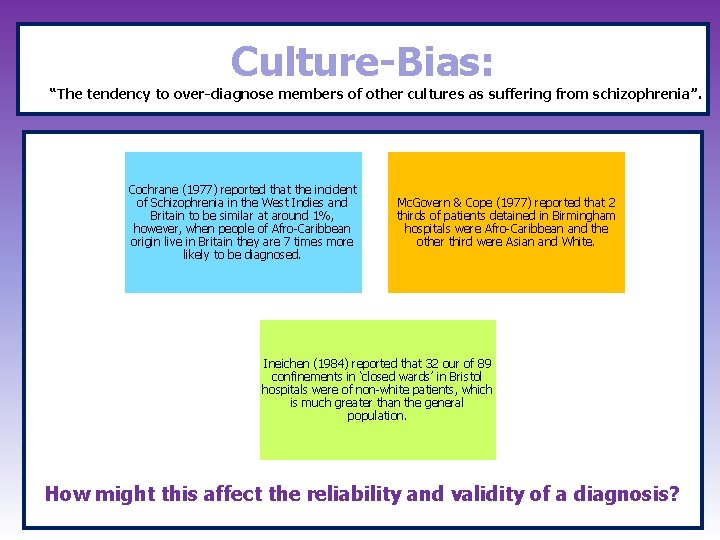
Culture-Bias: “The tendency to over-diagnose members of other cultures as suffering from schizophrenia”. Cochrane (1977) reported that the incident of Schizophrenia in the West Indies and Britain to be similar at around 1%, however, when people of Afro-Caribbean origin live in Britain they are 7 times more likely to be diagnosed. Mc. Govern & Cope (1977) reported that 2 thirds of patients detained in Birmingham hospitals were Afro-Caribbean and the other third were Asian and White. Ineichen (1984) reported that 32 our of 89 confinements in ‘closed wards’ in Bristol hospitals were of non-white patients, which is much greater than the general population. How might this affect the reliability and validity of a diagnosis?
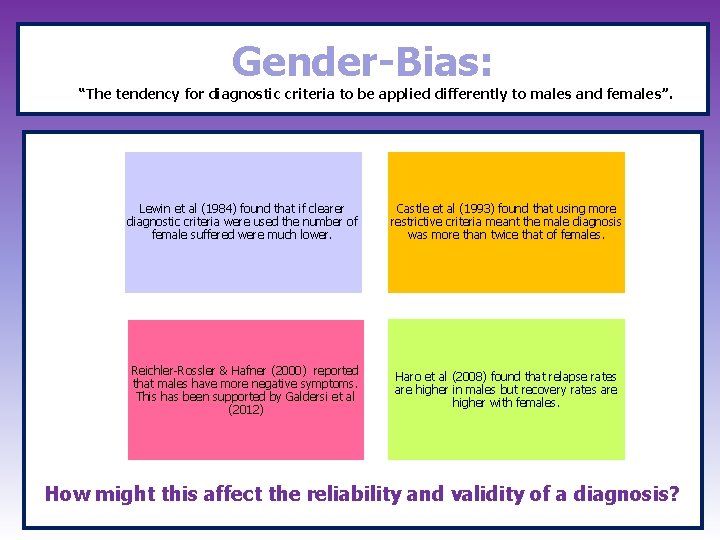
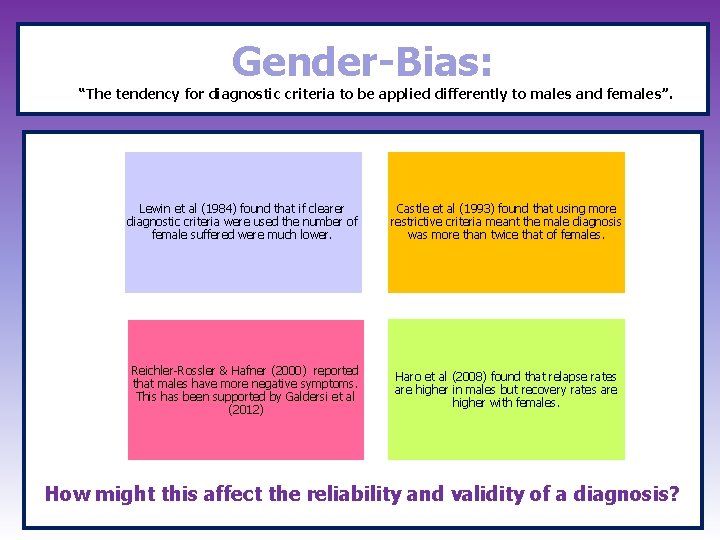
Gender-Bias: “The tendency for diagnostic criteria to be applied differently to males and females”. Lewin et al (1984) found that if clearer diagnostic criteria were used the number of female suffered were much lower. Castle et al (1993) found that using more restrictive criteria meant the male diagnosis was more than twice that of females. Reichler-Rossler & Hafner (2000) reported that males have more negative symptoms. This has been supported by Galdersi et al (2012) Haro et al (2008) found that relapse rates are higher in males but recovery rates are higher with females. How might this affect the reliability and validity of a diagnosis?
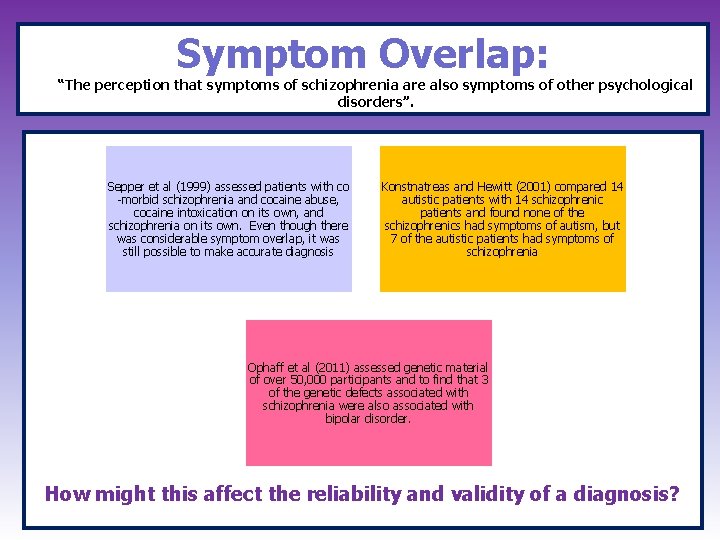
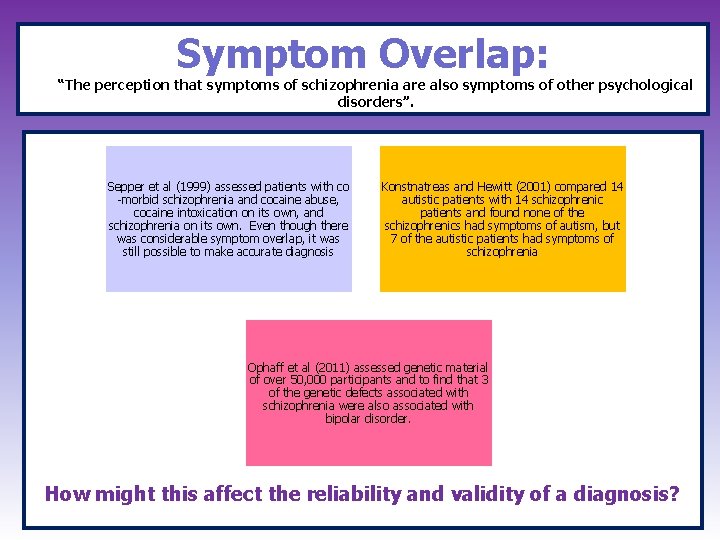
Symptom Overlap: “The perception that symptoms of schizophrenia are also symptoms of other psychological disorders”. Sepper et al (1999) assessed patients with co -morbid schizophrenia and cocaine abuse, cocaine intoxication on its own, and schizophrenia on its own. Even though there was considerable symptom overlap, it was still possible to make accurate diagnosis Konstnatreas and Hewitt (2001) compared 14 autistic patients with 14 schizophrenic patients and found none of the schizophrenics had symptoms of autism, but 7 of the autistic patients had symptoms of schizophrenia Ophaff et al (2011) assessed genetic material of over 50, 000 participants and to find that 3 of the genetic defects associated with schizophrenia were also associated with bipolar disorder. How might this affect the reliability and validity of a diagnosis?
Specification Content; What the AQA say you should know… Biological explanations for schizophrenia: – Genetics – The Dopamine Hypothesis – Neural correlates.
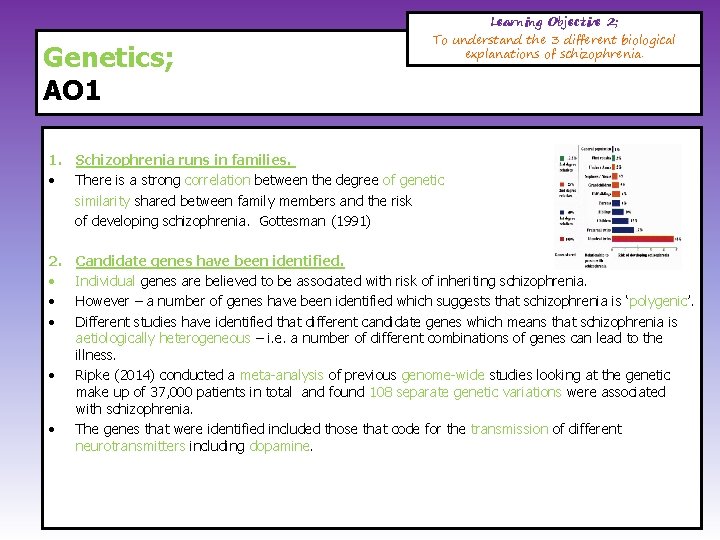
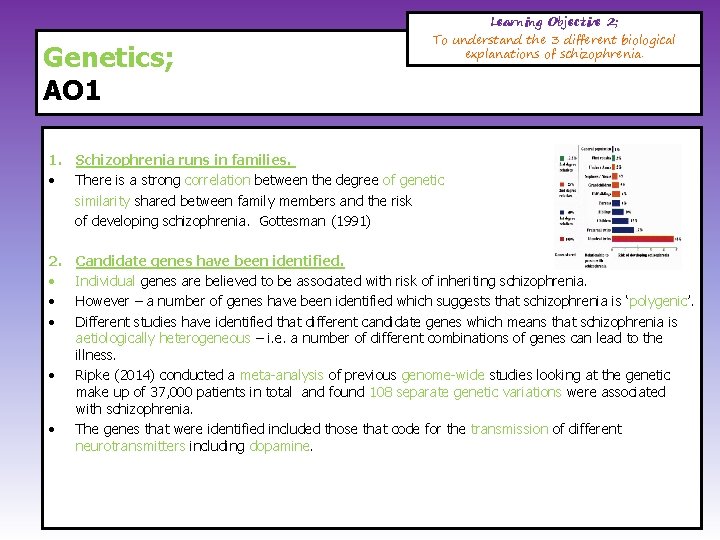
Genetics; AO 1 Learning Objective 2; To understand the 3 different biological explanations of schizophrenia. 1. Schizophrenia runs in families. • There is a strong correlation between the degree of genetic similarity shared between family members and the risk of developing schizophrenia. Gottesman (1991) 2. • • • Candidate genes have been identified. Individual genes are believed to be associated with risk of inheriting schizophrenia. However – a number of genes have been identified which suggests that schizophrenia is ‘polygenic’. Different studies have identified that different candidate genes which means that schizophrenia is aetiologically heterogeneous – i. e. a number of different combinations of genes can lead to the illness. Ripke (2014) conducted a meta-analysis of previous genome-wide studies looking at the genetic make up of 37, 000 patients in total and found 108 separate genetic variations were associated with schizophrenia. The genes that were identified included those that code for the transmission of different neurotransmitters including dopamine.
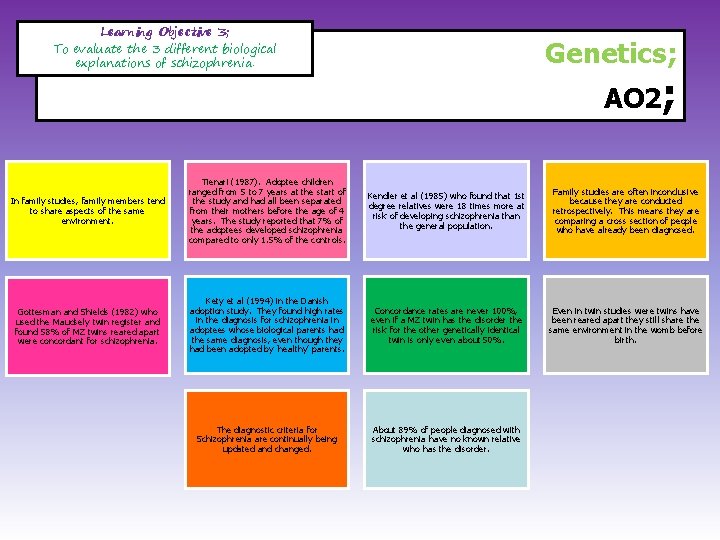
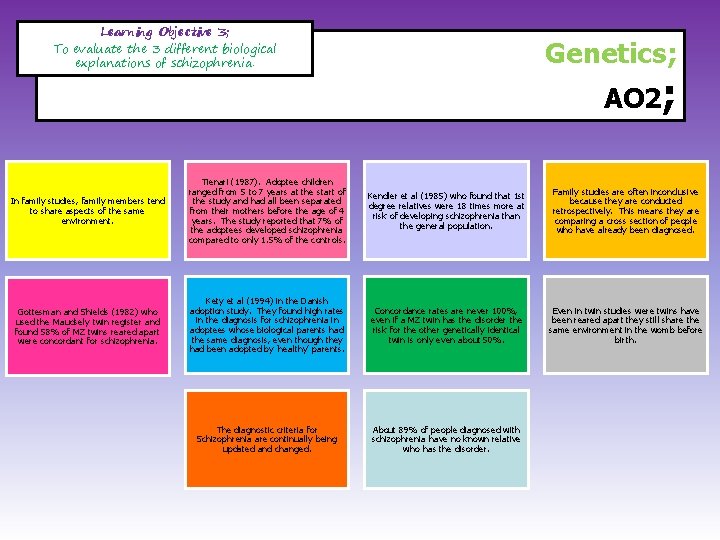
Learning Objective 3; To evaluate the 3 different biological explanations of schizophrenia. Genetics; AO 2; In family studies, family members tend to share aspects of the same environment. Tienari (1987). Adoptee children ranged from 5 to 7 years at the start of the study and had all been separated from their mothers before the age of 4 years. The study reported that 7% of the adoptees developed schizophrenia compared to only 1. 5% of the controls. Kendler et al (1985) who found that 1 st degree relatives were 18 times more at risk of developing schizophrenia than the general population. Family studies are often inconclusive because they are conducted retrospectively. This means they are comparing a cross section of people who have already been diagnosed. Gottesman and Shields (1982) who used the Maudsely twin register and found 58% of MZ twins reared apart were concordant for schizophrenia. Kety et al (1994) in the Danish adoption study. They found high rates in the diagnosis for schizophrenia in adoptees whose biological parents had the same diagnosis, even though they had been adopted by ‘healthy’ parents. Concordance rates are never 100%, even if a MZ twin has the disorder the risk for the other genetically identical twin is only even about 50%. Even in twin studies were twins have been reared apart they still share the same environment in the womb before birth. The diagnostic criteria for Schizophrenia are continually being updated and changed. About 89% of people diagnosed with schizophrenia have no known relative who has the disorder.
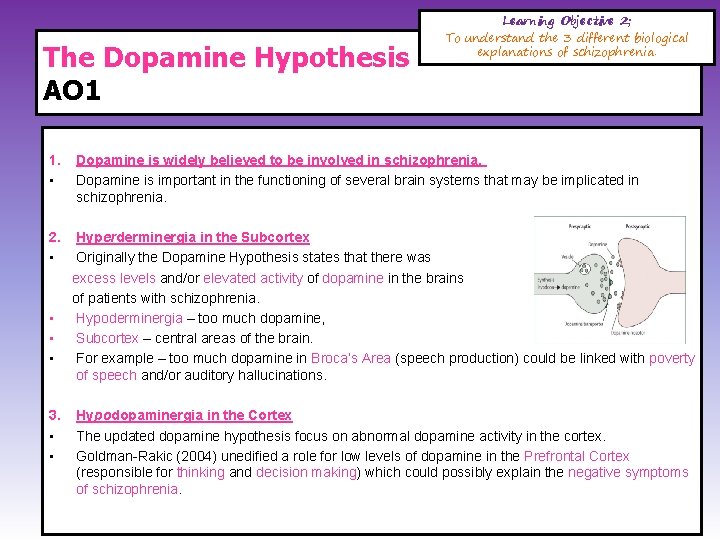
The Dopamine Hypothesis AO 1 Learning Objective 2; To understand the 3 different biological explanations of schizophrenia. 1. • Dopamine is widely believed to be involved in schizophrenia. Dopamine is important in the functioning of several brain systems that may be implicated in schizophrenia. 2. • Hyperderminergia in the Subcortex Originally the Dopamine Hypothesis states that there was excess levels and/or elevated activity of dopamine in the brains of patients with schizophrenia. Hypoderminergia – too much dopamine, Subcortex – central areas of the brain. For example – too much dopamine in Broca’s Area (speech production) could be linked with poverty of speech and/or auditory hallucinations. • • • 3. • • Hypodopaminergia in the Cortex The updated dopamine hypothesis focus on abnormal dopamine activity in the cortex. Goldman-Rakic (2004) unedified a role for low levels of dopamine in the Prefrontal Cortex (responsible for thinking and decision making) which could possibly explain the negative symptoms of schizophrenia.
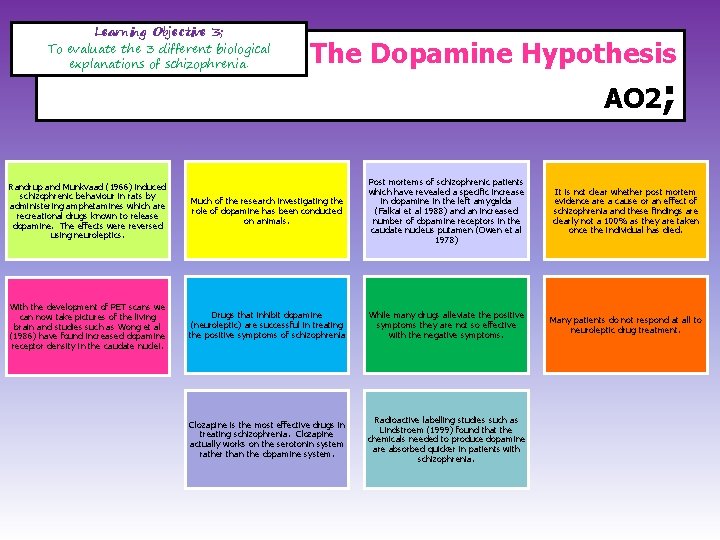
Learning Objective 3; To evaluate the 3 different biological explanations of schizophrenia. Randrup and Munkvaad (1966) induced schizophrenic behaviour in rats by administering amphetamines which are recreational drugs known to release dopamine. The effects were reversed using neuroleptics. With the development of PET scans we can now take pictures of the living brain and studies such as Wong et al (1986) have found increased dopamine receptor density in the caudate nuclei. The Dopamine Hypothesis AO 2; Much of the research investigating the role of dopamine has been conducted on animals. Post mortems of schizophrenic patients which have revealed a specific increase in dopamine in the left amygalda (Falkai et al 1988) and an increased number of dopamine receptors in the caudate nucleus putamen (Owen et al 1978) It is not clear whether post mortem evidence are a cause or an effect of schizophrenia and these findings are clearly not a 100% as they are taken once the individual has died. Drugs that inhibit dopamine (neuroleptic) are successful in treating the positive symptoms of schizophrenia While many drugs alleviate the positive symptoms they are not so effective with the negative symptoms. Many patients do not respond at all to neuroleptic drug treatment. Clozapine is the most effective drugs in treating schizophrenia. Clozapine actually works on the serotonin system rather than the dopamine system. Radioactive labelling studies such as Lindstroem (1999) found that the chemicals needed to produce dopamine are absorbed quicker in patients with schizophrenia.
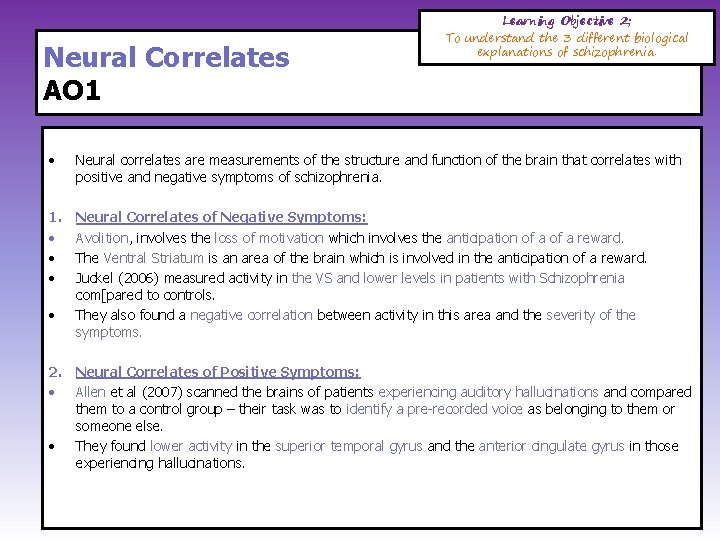
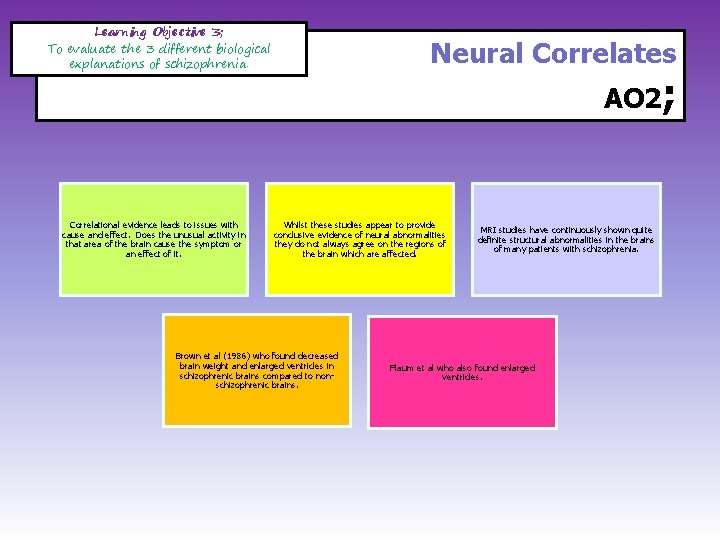
Neural Correlates AO 1 Learning Objective 2; To understand the 3 different biological explanations of schizophrenia. • Neural correlates are measurements of the structure and function of the brain that correlates with positive and negative symptoms of schizophrenia. 1. • • • Neural Correlates of Negative Symptoms: Avolition, involves the loss of motivation which involves the anticipation of a reward. The Ventral Striatum is an area of the brain which is involved in the anticipation of a reward. Juckel (2006) measured activity in the VS and lower levels in patients with Schizophrenia com[pared to controls. They also found a negative correlation between activity in this area and the severity of the symptoms. • 2. Neural Correlates of Positive Symptoms: • Allen et al (2007) scanned the brains of patients experiencing auditory hallucinations and compared them to a control group – their task was to identify a pre-recorded voice as belonging to them or someone else. • They found lower activity in the superior temporal gyrus and the anterior cingulate gyrus in those experiencing hallucinations.
Learning Objective 3; To evaluate the 3 different biological explanations of schizophrenia. Correlational evidence leads to issues with cause and effect. Does the unusual activity in that area of the brain cause the symptom or an effect of it. Neural Correlates AO 2; Whilst these studies appear to provide conclusive evidence of neural abnormalities they do not always agree on the regions of the brain which are affected. Brown et al (1986) who found decreased brain weight and enlarged ventricles in schizophrenic brains compared to nonschizophrenic brains. MRI studies have continuously shown quite definite structural abnormalities in the brains of many patients with schizophrenia. Flaum et al who also found enlarged ventricles.
Specification Content; What the AQA say you should know… Psychological explanations for schizophrenia: • family dysfunction • cognitive explanations, including dysfunctional thought processing.
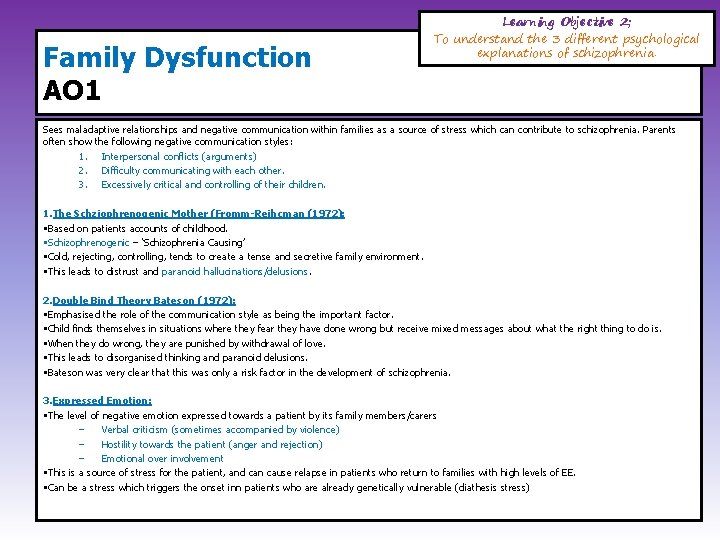
Family Dysfunction AO 1 Learning Objective 2; To understand the 3 different psychological explanations of schizophrenia. Sees maladaptive relationships and negative communication within families as a source of stress which can contribute to schizophrenia. Parents often show the following negative communication styles: 1. Interpersonal conflicts (arguments) 2. Difficulty communicating with each other. 3. Excessively critical and controlling of their children. 1. The Schziophrenogenic Mother (Fromm-Reihcman (1972): • Based on patients accounts of childhood. • Schizophrenogenic – ‘Schizophrenia Causing’ • Cold, rejecting, controlling, tends to create a tense and secretive family environment. • This leads to distrust and paranoid hallucinations/delusions. 2. Double Bind Theory Bateson (1972): • Emphasised the role of the communication style as being the important factor. • Child finds themselves in situations where they fear they have done wrong but receive mixed messages about what the right thing to do is. • When they do wrong, they are punished by withdrawal of love. • This leads to disorganised thinking and paranoid delusions. • Bateson was very clear that this was only a risk factor in the development of schizophrenia. 3. Expressed Emotion: • The level of negative emotion expressed towards a patient by its family members/carers – Verbal criticism (sometimes accompanied by violence) – Hostility towards the patient (anger and rejection) – Emotional over involvement • This is a source of stress for the patient, and can cause relapse in patients who return to families with high levels of EE. • Can be a stress which triggers the onset inn patients who are already genetically vulnerable (diathesis stress)
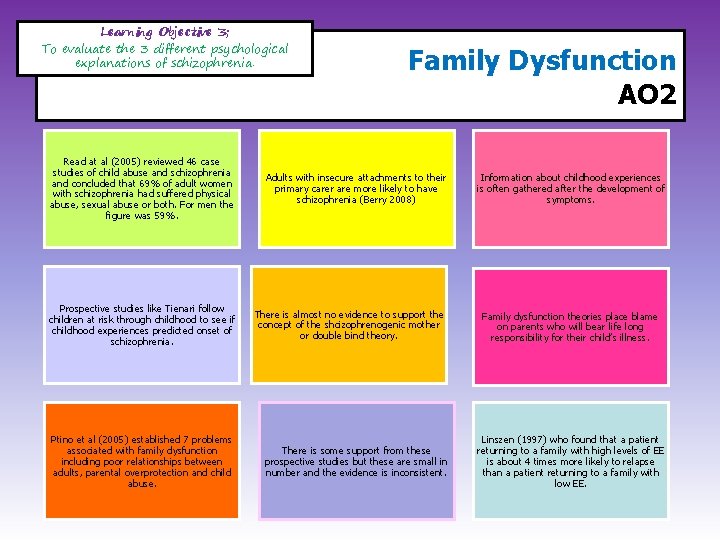
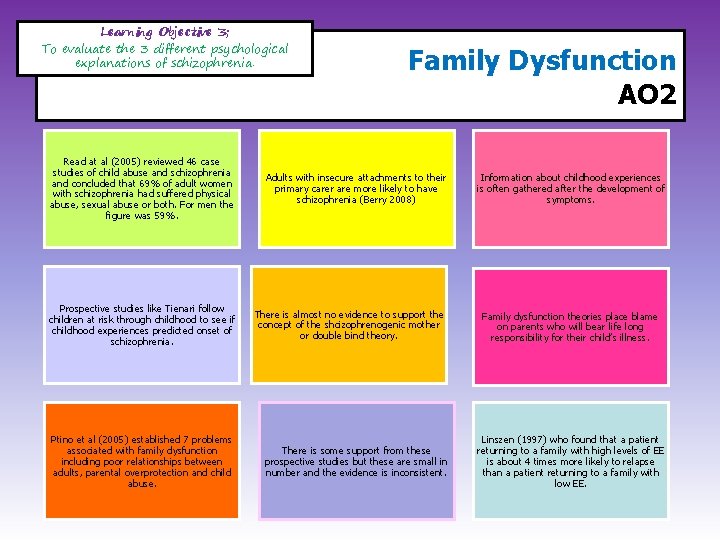
Learning Objective 3; To evaluate the 3 different psychological explanations of schizophrenia. Read at al (2005) reviewed 46 case studies of child abuse and schizophrenia and concluded that 69% of adult women with schizophrenia had suffered physical abuse, sexual abuse or both. For men the figure was 59%. Prospective studies like Tienari follow children at risk through childhood to see if childhood experiences predicted onset of schizophrenia. Ptino et al (2005) established 7 problems associated with family dysfunction including poor relationships between adults, parental overprotection and child abuse. Family Dysfunction AO 2 Adults with insecure attachments to their primary carer are more likely to have schizophrenia (Berry 2008) There is almost no evidence to support the concept of the shcizophrenogenic mother or double bind theory. There is some support from these prospective studies but these are small in number and the evidence is inconsistent. Information about childhood experiences is often gathered after the development of symptoms. Family dysfunction theories place blame on parents who will bear life long responsibility for their child’s illness. Linszen (1997) who found that a patient returning to a family with high levels of EE is about 4 times more likely to relapse than a patient returning to a family with low EE.
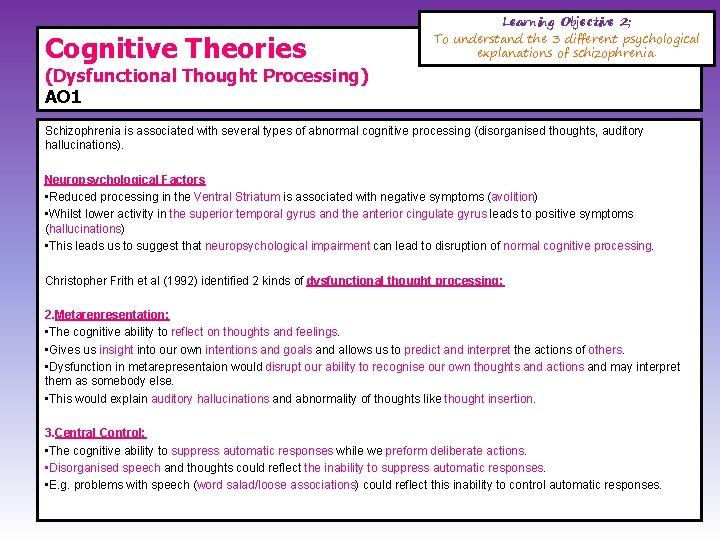
Cognitive Theories Learning Objective 2; To understand the 3 different psychological explanations of schizophrenia. (Dysfunctional Thought Processing) AO 1 Schizophrenia is associated with several types of abnormal cognitive processing (disorganised thoughts, auditory hallucinations). Neuropsychological Factors • Reduced processing in the Ventral Striatum is associated with negative symptoms (avolition) • Whilst lower activity in the superior temporal gyrus and the anterior cingulate gyrus leads to positive symptoms (hallucinations) • This leads us to suggest that neuropsychological impairment can lead to disruption of normal cognitive processing. Christopher Frith et al (1992) identified 2 kinds of dysfunctional thought processing: 2. Metarepresentation: • The cognitive ability to reflect on thoughts and feelings. • Gives us insight into our own intentions and goals and allows us to predict and interpret the actions of others. • Dysfunction in metarepresentaion would disrupt our ability to recognise our own thoughts and actions and may interpret them as somebody else. • This would explain auditory hallucinations and abnormality of thoughts like thought insertion. 3. Central Control: • The cognitive ability to suppress automatic responses while we preform deliberate actions. • Disorganised speech and thoughts could reflect the inability to suppress automatic responses. • E. g. problems with speech (word salad/loose associations) could reflect this inability to control automatic responses.
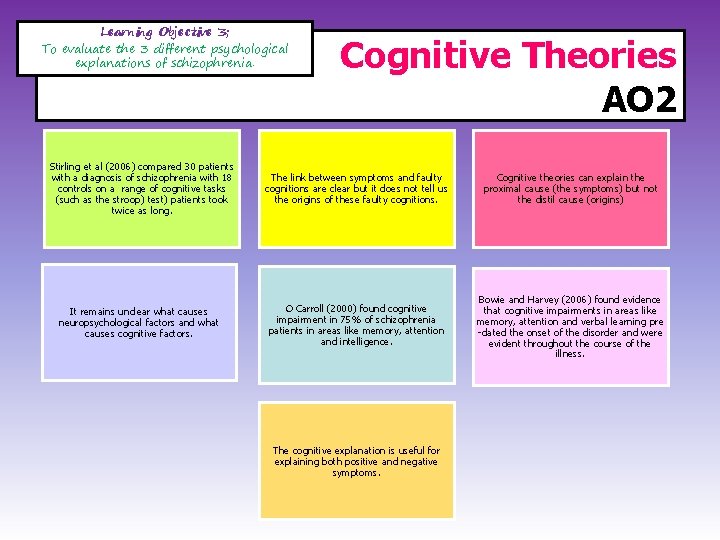
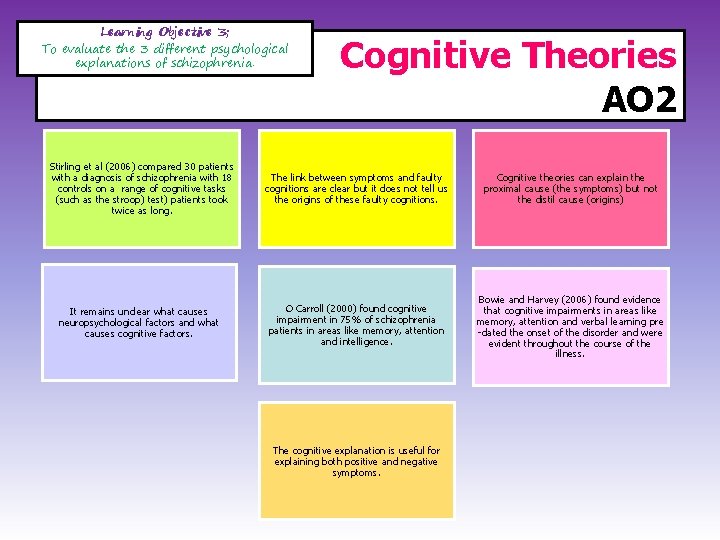
Learning Objective 3; To evaluate the 3 different psychological explanations of schizophrenia. Cognitive Theories AO 2 Stirling et al (2006) compared 30 patients with a diagnosis of schizophrenia with 18 controls on a range of cognitive tasks (such as the stroop) test) patients took twice as long. The link between symptoms and faulty cognitions are clear but it does not tell us the origins of these faulty cognitions. Cognitive theories can explain the proximal cause (the symptoms) but not the distil cause (origins) It remains unclear what causes neuropsychological factors and what causes cognitive factors. O Carroll (2000) found cognitive impairment in 75% of schizophrenia patients in areas like memory, attention and intelligence. Bowie and Harvey (2006) found evidence that cognitive impairments in areas like memory, attention and verbal learning pre -dated the onset of the disorder and were evident throughout the course of the illness. The cognitive explanation is useful for explaining both positive and negative symptoms.
Specification Content; What the AQA say you should know… Drug Therapy: –Typical Antipsychotics –Atypical Antipsychotics.
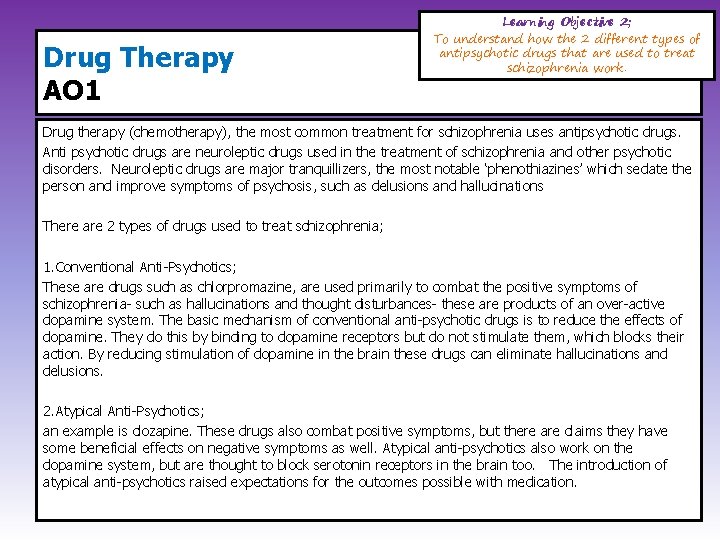
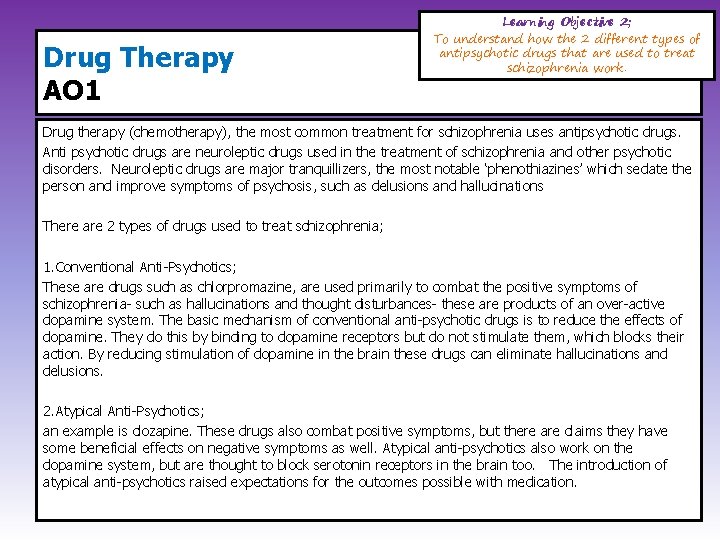
Drug Therapy AO 1 Learning Objective 2; To understand how the 2 different types of antipsychotic drugs that are used to treat schizophrenia work. Drug therapy (chemotherapy), the most common treatment for schizophrenia uses antipsychotic drugs. Anti psychotic drugs are neuroleptic drugs used in the treatment of schizophrenia and other psychotic disorders. Neuroleptic drugs are major tranquillizers, the most notable ‘phenothiazines’ which sedate the person and improve symptoms of psychosis, such as delusions and hallucinations There are 2 types of drugs used to treat schizophrenia; 1. Conventional Anti-Psychotics; These are drugs such as chlorpromazine, are used primarily to combat the positive symptoms of schizophrenia- such as hallucinations and thought disturbances- these are products of an over-active dopamine system. The basic mechanism of conventional anti-psychotic drugs is to reduce the effects of dopamine. They do this by binding to dopamine receptors but do not stimulate them, which blocks their action. By reducing stimulation of dopamine in the brain these drugs can eliminate hallucinations and delusions. 2. Atypical Anti-Psychotics; an example is clozapine. These drugs also combat positive symptoms, but there are claims they have some beneficial effects on negative symptoms as well. Atypical anti-psychotics also work on the dopamine system, but are thought to block serotonin receptors in the brain too. The introduction of atypical anti-psychotics raised expectations for the outcomes possible with medication.
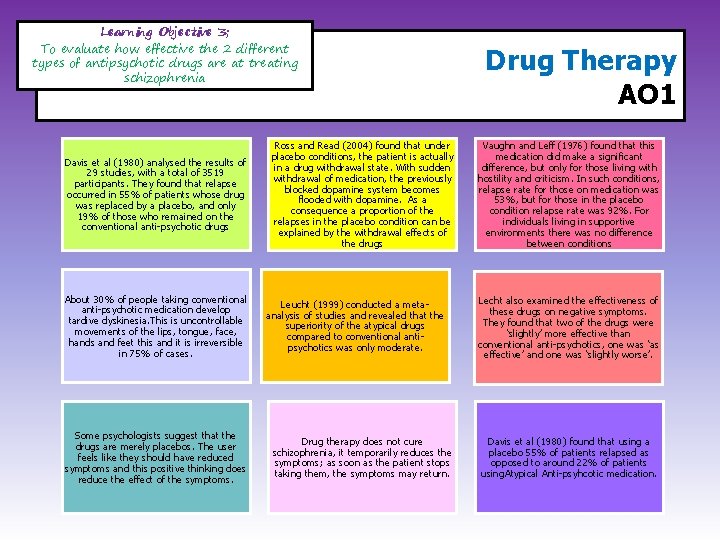
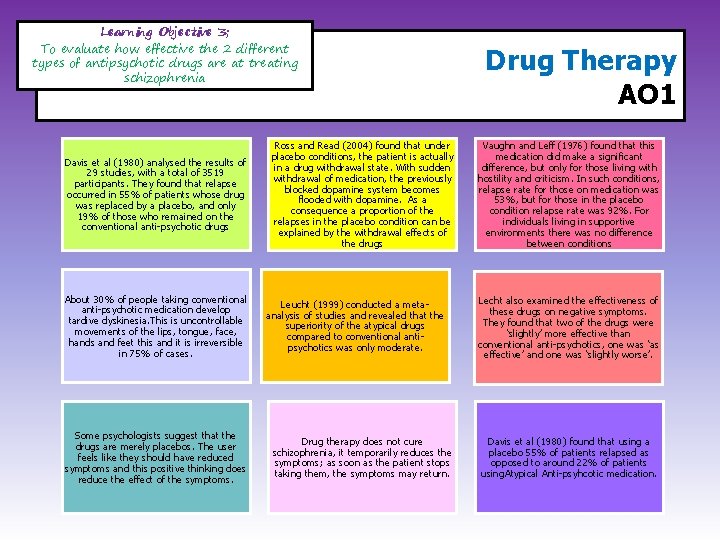
Learning Objective 3; To evaluate how effective the 2 different types of antipsychotic drugs are at treating schizophrenia Davis et al (1980) analysed the results of 29 studies, with a total of 3519 participants. They found that relapse occurred in 55% of patients whose drug was replaced by a placebo, and only 19% of those who remained on the conventional anti-psychotic drugs About 30% of people taking conventional anti-psychotic medication develop tardive dyskinesia. This is uncontrollable movements of the lips, tongue, face, hands and feet this and it is irreversible in 75% of cases. Some psychologists suggest that the drugs are merely placebos. The user feels like they should have reduced symptoms and this positive thinking does reduce the effect of the symptoms. Ross and Read (2004) found that under placebo conditions, the patient is actually in a drug withdrawal state. With sudden withdrawal of medication, the previously blocked dopamine system becomes flooded with dopamine. As a consequence a proportion of the relapses in the placebo condition can be explained by the withdrawal effects of the drugs Leucht (1999) conducted a metaanalysis of studies and revealed that the superiority of the atypical drugs compared to conventional antipsychotics was only moderate. Drug therapy does not cure schizophrenia, it temporarily reduces the symptoms; as soon as the patient stops taking them, the symptoms may return. Drug Therapy AO 1 Vaughn and Leff (1976) found that this medication did make a significant difference, but only for those living with hostility and criticism. In such conditions, relapse rate for those on medication was 53%, but for those in the placebo condition relapse rate was 92%. For individuals living in supportive environments there was no difference between conditions Lecht also examined the effectiveness of these drugs on negative symptoms. They found that two of the drugs were ‘slightly’ more effective than conventional anti-psychotics, one was ‘as effective’ and one was ‘slightly worse’. Davis et al (1980) found that using a placebo 55% of patients relapsed as opposed to around 22% of patients using. Atypical Anti-psyhcotic medication.
Specification Content; What the AQA say you should know… Treatment of Schizophrenia: • Cognitive Behaviour Therapy • Family Therapy Management of Schizophrenia: • Token Economies
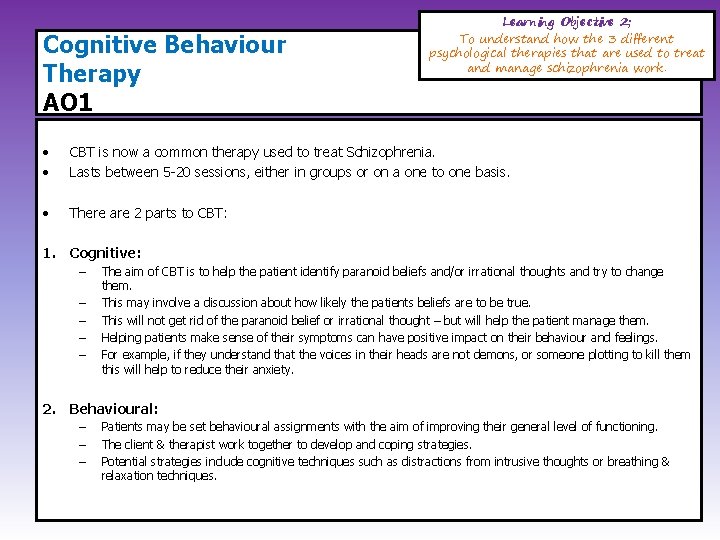
Cognitive Behaviour Therapy AO 1 Learning Objective 2; To understand how the 3 different psychological therapies that are used to treat and manage schizophrenia work. • • CBT is now a common therapy used to treat Schizophrenia. Lasts between 5 -20 sessions, either in groups or on a one to one basis. • There are 2 parts to CBT: 1. Cognitive: – – – The aim of CBT is to help the patient identify paranoid beliefs and/or irrational thoughts and try to change them. This may involve a discussion about how likely the patients beliefs are to be true. This will not get rid of the paranoid belief or irrational thought – but will help the patient manage them. Helping patients make sense of their symptoms can have positive impact on their behaviour and feelings. For example, if they understand that the voices in their heads are not demons, or someone plotting to kill them this will help to reduce their anxiety. 2. Behavioural: – – – Patients may be set behavioural assignments with the aim of improving their general level of functioning. The client & therapist work together to develop and coping strategies. Potential strategies include cognitive techniques such as distractions from intrusive thoughts or breathing & relaxation techniques.
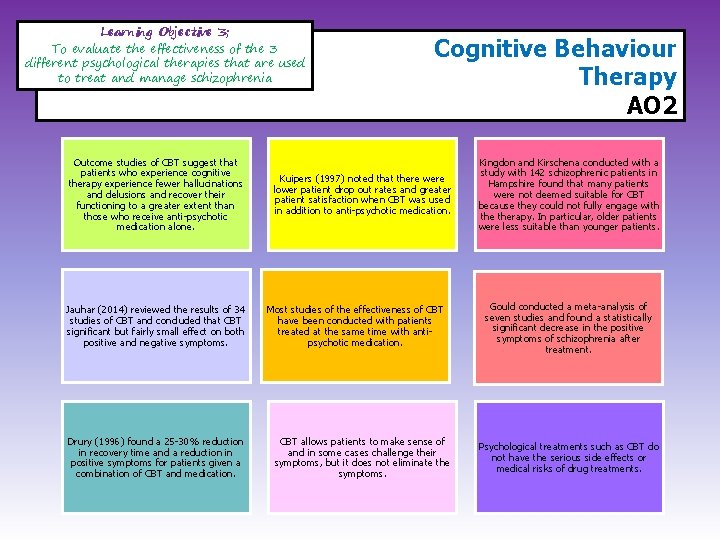
Learning Objective 3; To evaluate the effectiveness of the 3 different psychological therapies that are used to treat and manage schizophrenia Outcome studies of CBT suggest that patients who experience cognitive therapy experience fewer hallucinations and delusions and recover their functioning to a greater extent than those who receive anti-psychotic medication alone. Jauhar (2014) reviewed the results of 34 studies of CBT and concluded that CBT significant but fairly small effect on both positive and negative symptoms. Drury (1996) found a 25 -30% reduction in recovery time and a reduction in positive symptoms for patients given a combination of CBT and medication. Cognitive Behaviour Therapy AO 2 Kuipers (1997) noted that there were lower patient drop out rates and greater patient satisfaction when CBT was used in addition to anti-psychotic medication. Most studies of the effectiveness of CBT have been conducted with patients treated at the same time with antipsychotic medication. CBT allows patients to make sense of and in some cases challenge their symptoms, but it does not eliminate the symptoms. Kingdon and Kirschena conducted with a study with 142 schizophrenic patients in Hampshire found that many patients were not deemed suitable for CBT because they could not fully engage with therapy. In particular, older patients were less suitable than younger patients. Gould conducted a meta-analysis of seven studies and found a statistically significant decrease in the positive symptoms of schizophrenia after treatment. Psychological treatments such as CBT do not have the serious side effects or medical risks of drug treatments.
Family Therapy AO 1 Learning Objective 2; To understand how the 3 different psychological therapies that are used to treat and manage schizophrenia work. • • Family Therapy with families rather than the actual patient. This therapy aims to improve the quality of communication within the family. • There a range of different approaches to family therapy – but today the most common is trying to reduce the risk of relapse by reducing levels of Expressed Emotion. • Family Therapy which aims to reduce EE might: Form a therapeutic alliance between family members. Reduce the stress of caring for a relative with schizophrenia Improve the ability of the family to anticipate and solves problems. Reduce anger and/or guilt in family members. Help family members achieve a balance between caring for the relative and having their own life. ü Improve families understanding about schizophrenia ü Improve family members behaviour towards the relative with schizophrenia. ü ü ü
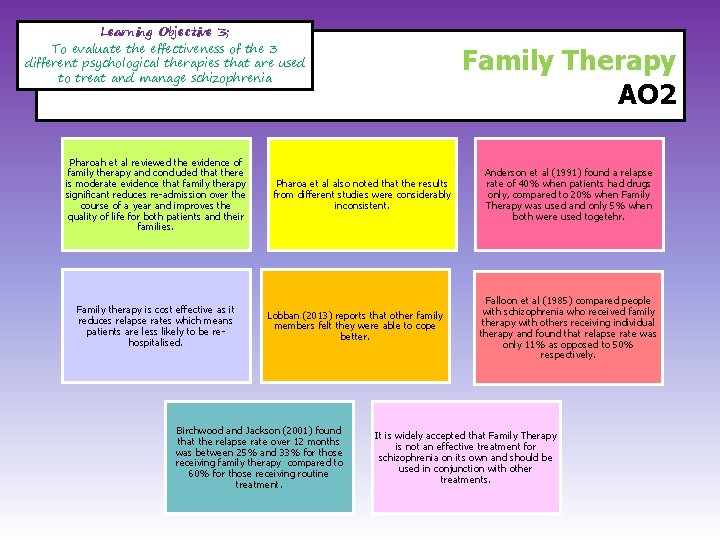
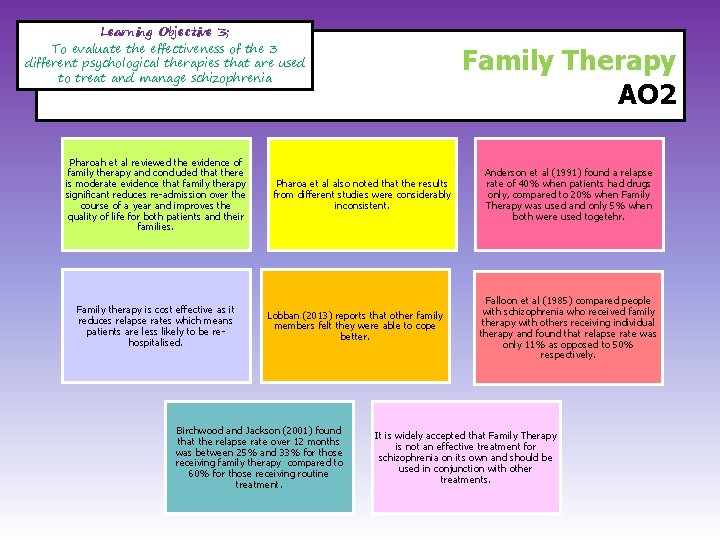
Learning Objective 3; To evaluate the effectiveness of the 3 different psychological therapies that are used to treat and manage schizophrenia Pharoah et al reviewed the evidence of family therapy and concluded that there is moderate evidence that family therapy significant reduces re-admission over the course of a year and improves the quality of life for both patients and their families. Family therapy is cost effective as it reduces relapse rates which means patients are less likely to be rehospitalised. Family Therapy AO 2 Pharoa et al also noted that the results from different studies were considerably inconsistent. Lobban (2013) reports that other family members felt they were able to cope better. Birchwood and Jackson (2001) found that the relapse rate over 12 months was between 25% and 33% for those receiving family therapy compared to 60% for those receiving routine treatment. Anderson et al (1991) found a relapse rate of 40% when patients had drugs only, compared to 20% when Family Therapy was used and only 5% when both were used togetehr. Falloon et al (1985) compared people with schizophrenia who received family therapy with others receiving individual therapy and found that relapse rate was only 11% as opposed to 50% respectively. It is widely accepted that Family Therapy is not an effective treatment for schizophrenia on its own and should be used in conjunction with other treatments.
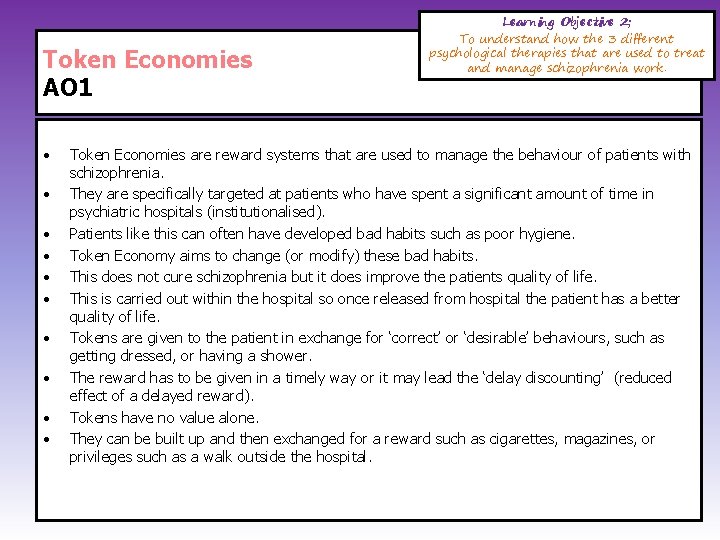
Token Economies AO 1 • • • Learning Objective 2; To understand how the 3 different psychological therapies that are used to treat and manage schizophrenia work. Token Economies are reward systems that are used to manage the behaviour of patients with schizophrenia. They are specifically targeted at patients who have spent a significant amount of time in psychiatric hospitals (institutionalised). Patients like this can often have developed bad habits such as poor hygiene. Token Economy aims to change (or modify) these bad habits. This does not cure schizophrenia but it does improve the patients quality of life. This is carried out within the hospital so once released from hospital the patient has a better quality of life. Tokens are given to the patient in exchange for ‘correct’ or ‘desirable’ behaviours, such as getting dressed, or having a shower. The reward has to be given in a timely way or it may lead the ‘delay discounting’ (reduced effect of a delayed reward). Tokens have no value alone. They can be built up and then exchanged for a reward such as cigarettes, magazines, or privileges such as a walk outside the hospital.
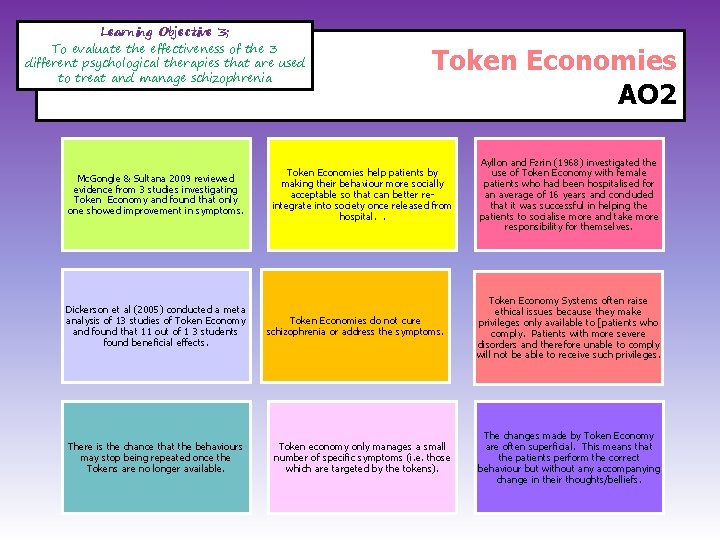
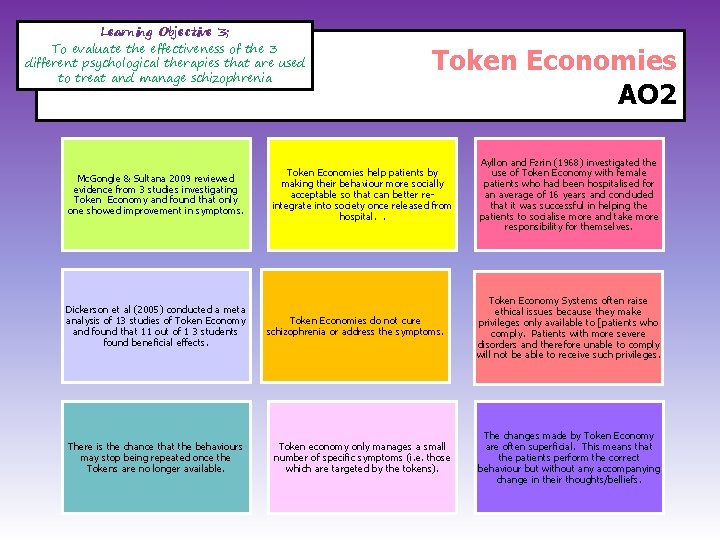
Learning Objective 3; To evaluate the effectiveness of the 3 different psychological therapies that are used to treat and manage schizophrenia Mc. Gongle & Sultana 2009 reviewed evidence from 3 studies investigating Token Economy and found that only one showed improvement in symptoms. Dickerson et al (2005) conducted a meta analysis of 13 studies of Token Economy and found that 11 out of 1 3 students found beneficial effects. There is the chance that the behaviours may stop being repeated once the Tokens are no longer available. Token Economies AO 2 Token Economies help patients by making their behaviour more socially acceptable so that can better reintegrate into society once released from hospital. . Token Economies do not cure schizophrenia or address the symptoms. Token economy only manages a small number of specific symptoms (i. e. those which are targeted by the tokens). Ayllon and Fzrin (1968) investigated the use of Token Economy with female patients who had been hospitalised for an average of 16 years and concluded that it was successful in helping the patients to socialise more and take more responsibility for themselves. Token Economy Systems often raise ethical issues because they make privileges only available to [patients who comply. Patients with more severe disorders and therefore unable to comply will not be able to receive such privileges. The changes made by Token Economy are often superficial. This means that the patients perform the correct behaviour but without any accompanying change in their thoughts/belliefs.
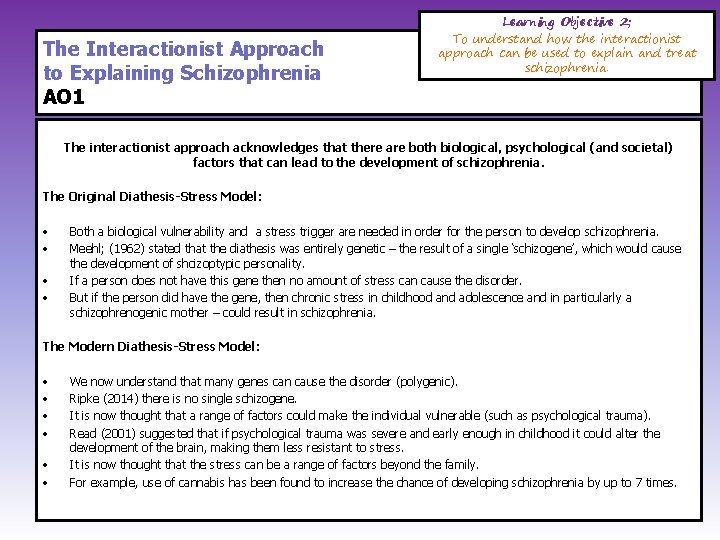
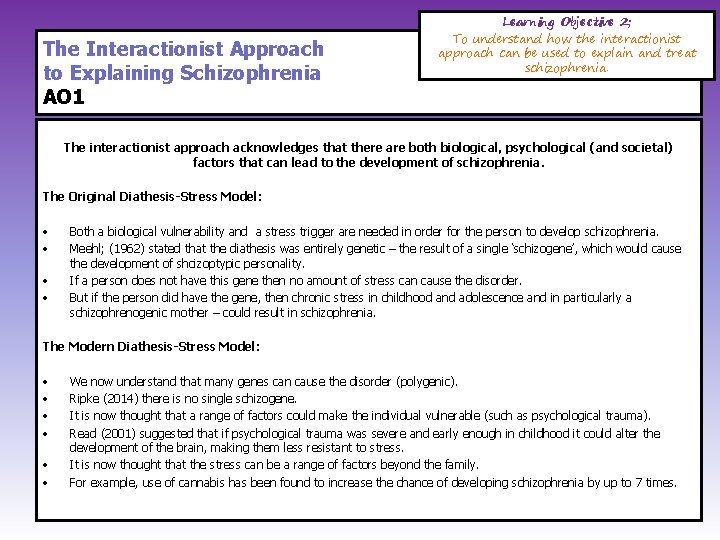
The Interactionist Approach to Explaining Schizophrenia AO 1 Learning Objective 2; To understand how the interactionist approach can be used to explain and treat schizophrenia. The interactionist approach acknowledges that there are both biological, psychological (and societal) factors that can lead to the development of schizophrenia. The Original Diathesis-Stress Model: • • Both a biological vulnerability and a stress trigger are needed in order for the person to develop schizophrenia. Meehl; (1962) stated that the diathesis was entirely genetic – the result of a single ‘schizogene’, which would cause the development of shcizoptypic personality. If a person does not have this gene then no amount of stress can cause the disorder. But if the person did have the gene, then chronic stress in childhood and adolescence and in particularly a schizophrenogenic mother – could result in schizophrenia. The Modern Diathesis-Stress Model: • • • We now understand that many genes can cause the disorder (polygenic). Ripke (2014) there is no single schizogene. It is now thought that a range of factors could make the individual vulnerable (such as psychological trauma). Read (2001) suggested that if psychological trauma was severe and early enough in childhood it could alter the development of the brain, making them less resistant to stress. It is now thought that the stress can be a range of factors beyond the family. For example, use of cannabis has been found to increase the chance of developing schizophrenia by up to 7 times.
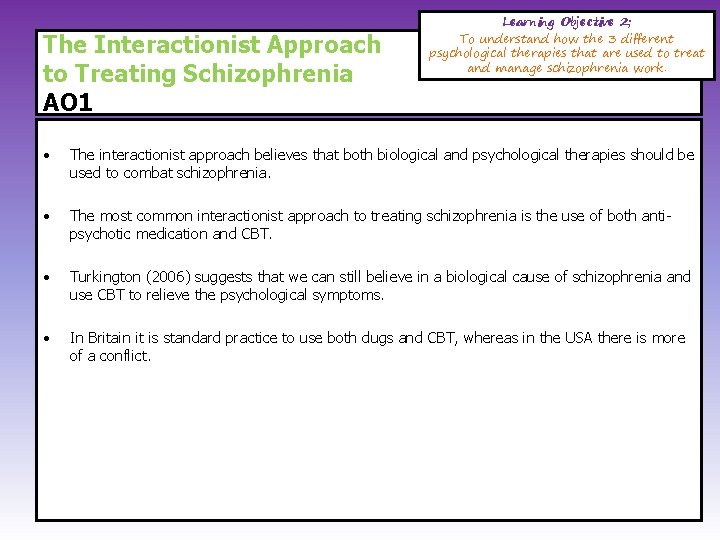
The Interactionist Approach to Treating Schizophrenia AO 1 Learning Objective 2; To understand how the 3 different psychological therapies that are used to treat and manage schizophrenia work. • The interactionist approach believes that both biological and psychological therapies should be used to combat schizophrenia. • The most common interactionist approach to treating schizophrenia is the use of both antipsychotic medication and CBT. • Turkington (2006) suggests that we can still believe in a biological cause of schizophrenia and use CBT to relieve the psychological symptoms. • In Britain it is standard practice to use both dugs and CBT, whereas in the USA there is more of a conflict.
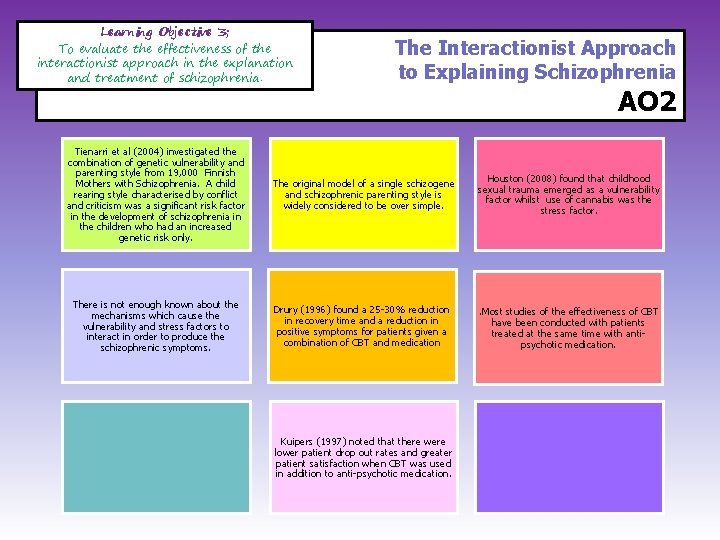
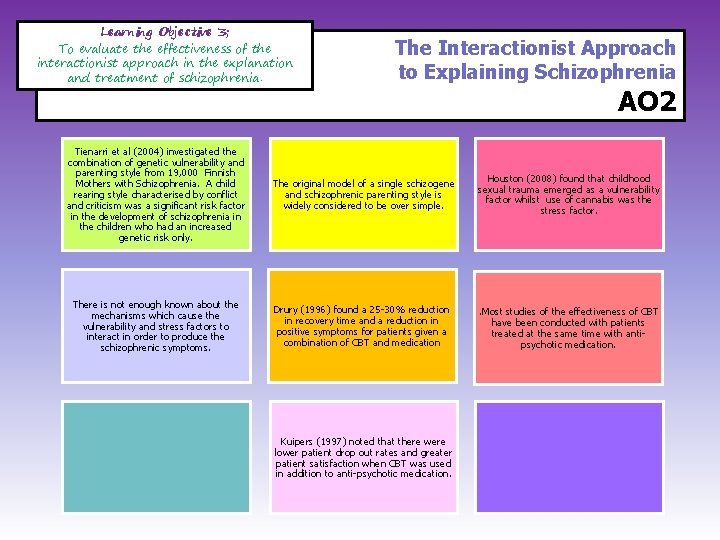
Learning Objective 3; To evaluate the effectiveness of the interactionist approach in the explanation and treatment of schizophrenia. The Interactionist Approach to Explaining Schizophrenia AO 2 Tienarri et al (2004) investigated the combination of genetic vulnerability and parenting style from 19, 000 Finnish Mothers with Schizophrenia. A child rearing style characterised by conflict and criticism was a significant risk factor in the development of schizophrenia in the children who had an increased genetic risk only. The original model of a single schizogene and schizophrenic parenting style is widely considered to be over simple. Houston (2008) found that childhood sexual trauma emerged as a vulnerability factor whilst use of cannabis was the stress factor. There is not enough known about the mechanisms which cause the vulnerability and stress factors to interact in order to produce the schizophrenic symptoms. Drury (1996) found a 25 -30% reduction in recovery time and a reduction in positive symptoms for patients given a combination of CBT and medication . Most studies of the effectiveness of CBT have been conducted with patients treated at the same time with antipsychotic medication. Kuipers (1997) noted that there were lower patient drop out rates and greater patient satisfaction when CBT was used in addition to anti-psychotic medication.