AQA A Level Psychology Paper 1 Psychopathology Specification
- Slides: 41
AQA A Level Psychology Paper 1: Psychopathology
Specification Content: What the AQA say you should know… Definitions of abnormality including; – Deviation from Social Norms – Deviation from Ideal Mental Health – Failure to Function Adequately – Statistical Infrequency
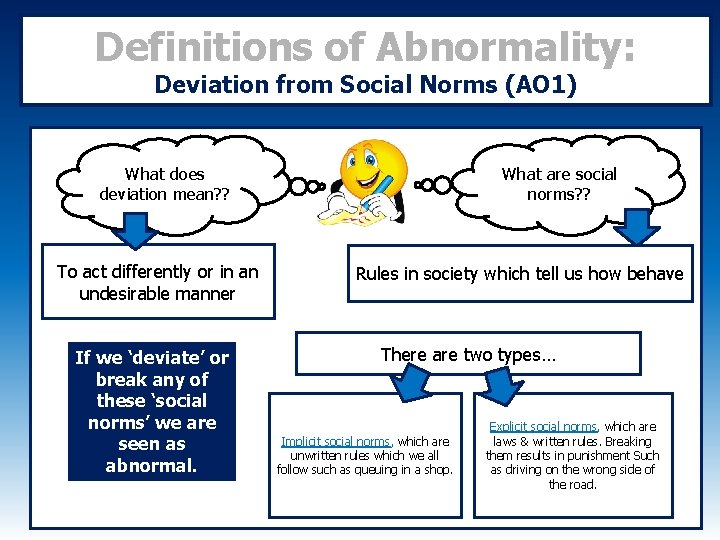
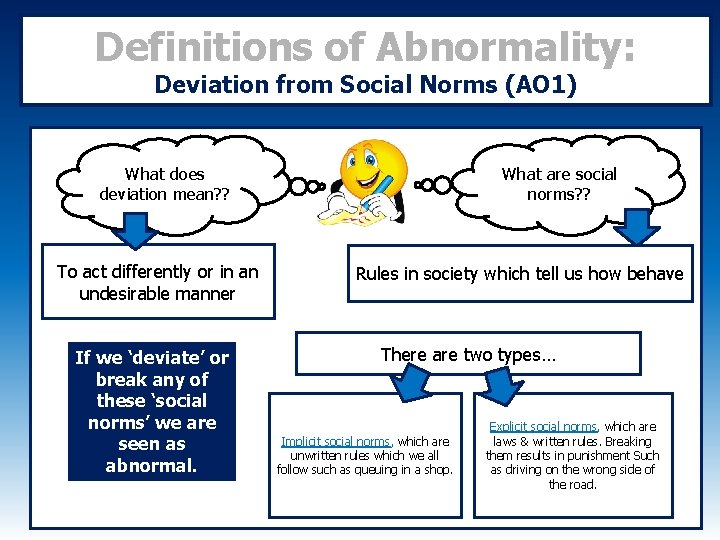
Definitions of Abnormality: Deviation from Social Norms (AO 1) What does deviation mean? ? To act differently or in an undesirable manner If we ‘deviate’ or break any of these ‘social norms’ we are seen as abnormal. What are social norms? ? Rules in society which tell us how behave There are two types… Implicit social norms, which are unwritten rules which we all follow such as queuing in a shop. Explicit social norms, which are laws & written rules. Breaking them results in punishment Such as driving on the wrong side of the road.
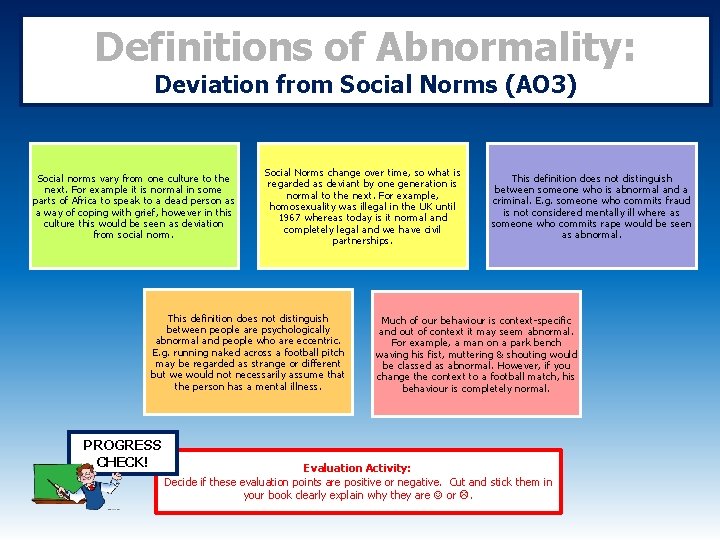
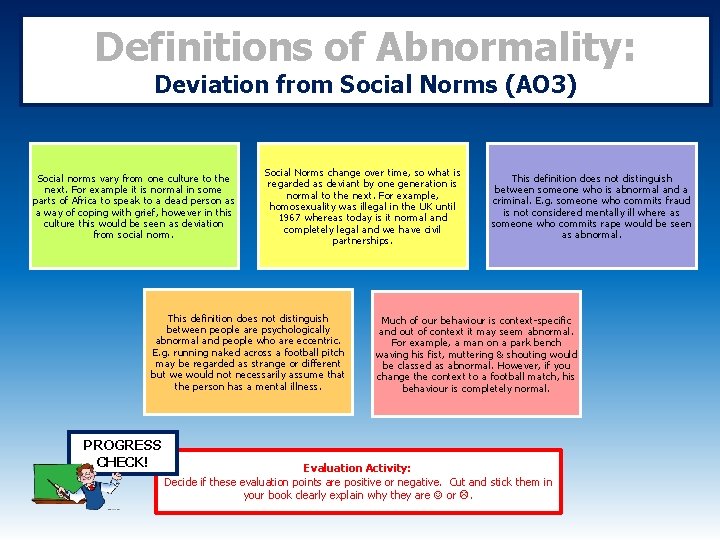
Definitions of Abnormality: Deviation from Social Norms (AO 3) Social norms vary from one culture to the next. For example it is normal in some parts of Africa to speak to a dead person as a way of coping with grief, however in this culture this would be seen as deviation from social norm. Social Norms change over time, so what is regarded as deviant by one generation is normal to the next. For example, homosexuality was illegal in the UK until 1967 whereas today is it normal and completely legal and we have civil partnerships. This definition does not distinguish between people are psychologically abnormal and people who are eccentric. E. g. running naked across a football pitch may be regarded as strange or different but we would not necessarily assume that the person has a mental illness. PROGRESS CHECK! This definition does not distinguish between someone who is abnormal and a criminal. E. g. someone who commits fraud is not considered mentally ill where as someone who commits rape would be seen as abnormal. Much of our behaviour is context-specific and out of context it may seem abnormal. For example, a man on a park bench waving his fist, muttering & shouting would be classed as abnormal. However, if you change the context to a football match, his behaviour is completely normal. Evaluation Activity: Decide if these evaluation points are positive or negative. Cut and stick them in your book clearly explain why they are or .
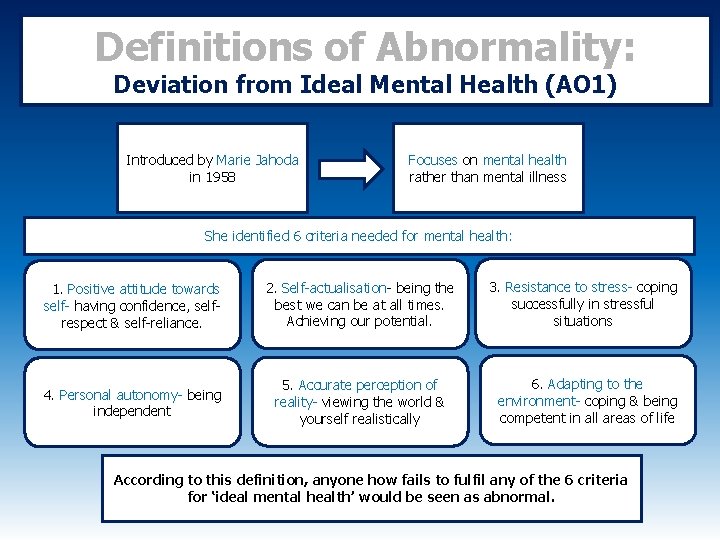
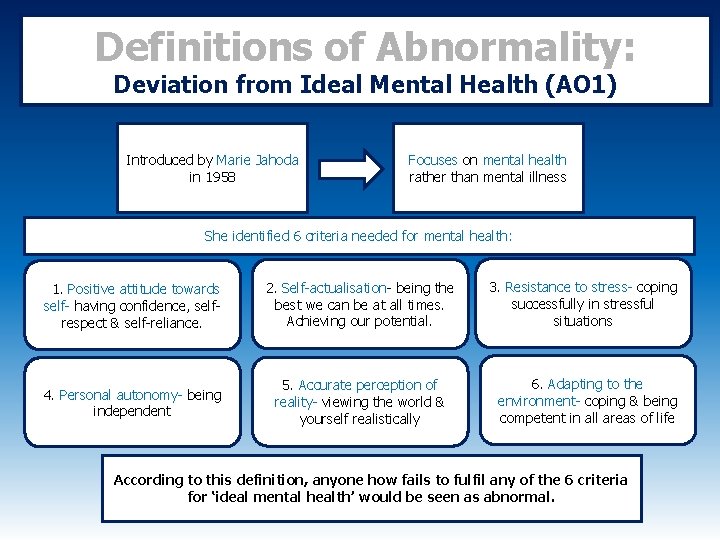
Definitions of Abnormality: Deviation from Ideal Mental Health (AO 1) Introduced by Marie Jahoda in 1958 Focuses on mental health rather than mental illness She identified 6 criteria needed for mental health: 11. Positive attitude towards self- having confidence, selfrespect & self-reliance. 2. Self-actualisation- being the best we can be at all times. Achieving our potential. 4. Personal autonomy- being independent 5. Accurate perception of reality- viewing the world & yourself realistically 3. Resistance to stress- coping successfully in stressful situations 6. Adapting to the environment- coping & being competent in all areas of life According to this definition, anyone how fails to fulfil any of the 6 criteria for ‘ideal mental health’ would be seen as abnormal.
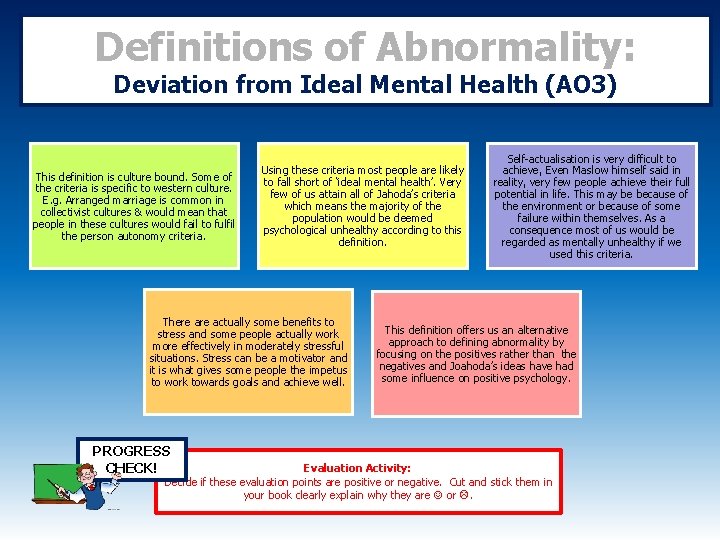
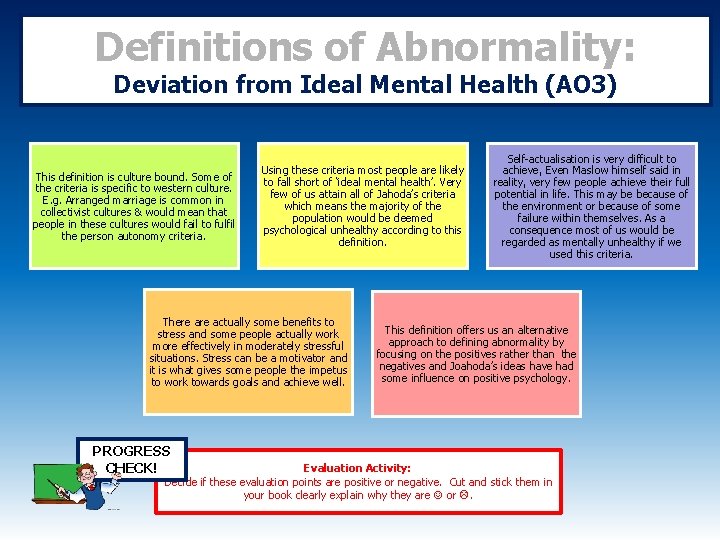
Definitions of Abnormality: Deviation from Ideal Mental Health (AO 3) This definition is culture bound. Some of the criteria is specific to western culture. E. g. Arranged marriage is common in collectivist cultures & would mean that people in these cultures would fail to fulfil the person autonomy criteria. Using these criteria most people are likely to fall short of ‘ideal mental health’. Very few of us attain all of Jahoda’s criteria which means the majority of the population would be deemed psychological unhealthy according to this definition. There actually some benefits to stress and some people actually work more effectively in moderately stressful situations. Stress can be a motivator and it is what gives some people the impetus to work towards goals and achieve well. PROGRESS CHECK! Self-actualisation is very difficult to achieve, Even Maslow himself said in reality, very few people achieve their full potential in life. This may be because of the environment or because of some failure within themselves. As a consequence most of us would be regarded as mentally unhealthy if we used this criteria. This definition offers us an alternative approach to defining abnormality by focusing on the positives rather than the negatives and Joahoda’s ideas have had some influence on positive psychology. Evaluation Activity: Decide if these evaluation points are positive or negative. Cut and stick them in your book clearly explain why they are or .
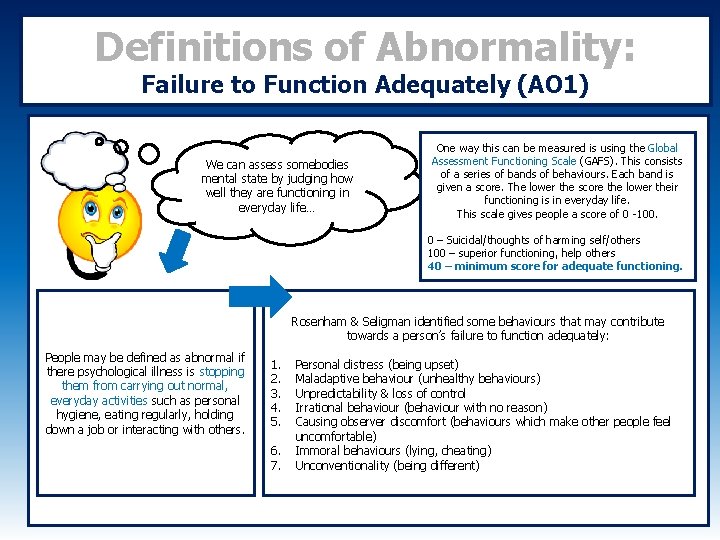
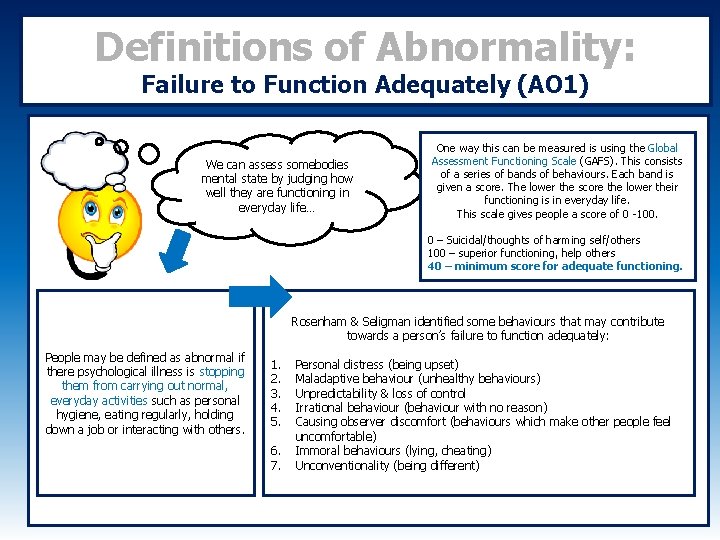
Definitions of Abnormality: Failure to Function Adequately (AO 1) We can assess somebodies mental state by judging how well they are functioning in everyday life… One way this can be measured is using the Global Assessment Functioning Scale (GAFS). This consists of a series of bands of behaviours. Each band is given a score. The lower the score the lower their functioning is in everyday life. This scale gives people a score of 0 -100. 0 – Suicidal/thoughts of harming self/others 100 – superior functioning, help others 40 – minimum score for adequate functioning. Rosenham & Seligman identified some behaviours that may contribute towards a person’s failure to function adequately: People may be defined as abnormal if there psychological illness is stopping them from carrying out normal, everyday activities such as personal hygiene, eating regularly, holding down a job or interacting with others. 1. 2. 3. 4. 5. 6. 7. Personal distress (being upset) Maladaptive behaviour (unhealthy behaviours) Unpredictability & loss of control Irrational behaviour (behaviour with no reason) Causing observer discomfort (behaviours which make other people feel uncomfortable) Immoral behaviours (lying, cheating) Unconventionality (being different)
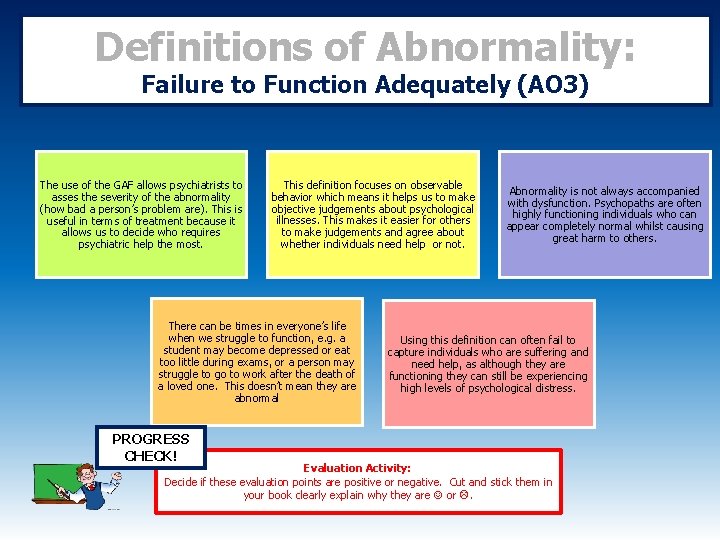
Definitions of Abnormality: Failure to Function Adequately (AO 3) The use of the GAF allows psychiatrists to asses the severity of the abnormality (how bad a person’s problem are). This is useful in terms of treatment because it allows us to decide who requires psychiatric help the most. This definition focuses on observable behavior which means it helps us to make objective judgements about psychological illnesses. This makes it easier for others to make judgements and agree about whether individuals need help or not. There can be times in everyone’s life when we struggle to function, e. g. a student may become depressed or eat too little during exams, or a person may struggle to go to work after the death of a loved one. This doesn’t mean they are abnormal PROGRESS CHECK! Abnormality is not always accompanied with dysfunction. Psychopaths are often highly functioning individuals who can appear completely normal whilst causing great harm to others. Using this definition can often fail to capture individuals who are suffering and need help, as although they are functioning they can still be experiencing high levels of psychological distress. Evaluation Activity: Decide if these evaluation points are positive or negative. Cut and stick them in your book clearly explain why they are or .
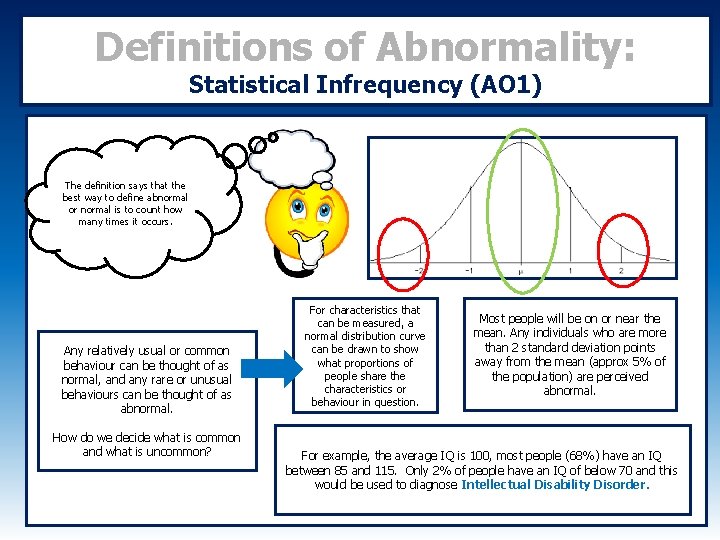
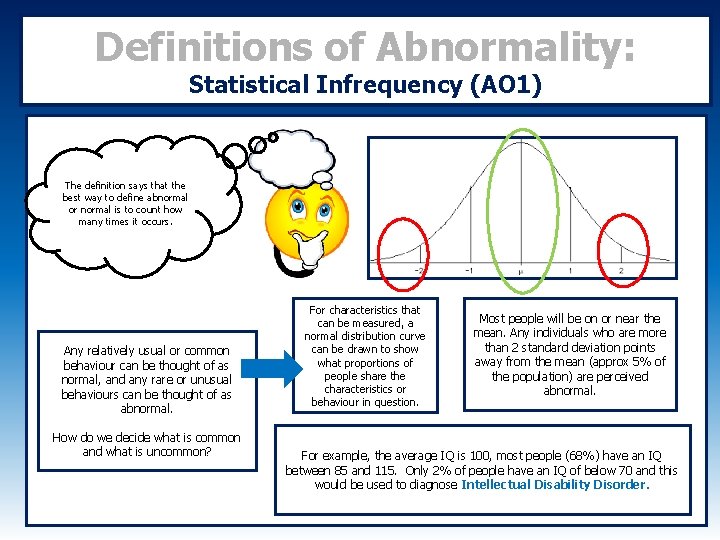
Definitions of Abnormality: Statistical Infrequency (AO 1) The definition says that the best way to define abnormal or normal is to count how many times it occurs. Any relatively usual or common behaviour can be thought of as normal, and any rare or unusual behaviours can be thought of as abnormal. How do we decide what is common and what is uncommon? For characteristics that can be measured, a normal distribution curve can be drawn to show what proportions of people share the characteristics or behaviour in question. Most people will be on or near the mean. Any individuals who are more than 2 standard deviation points away from the mean (approx 5% of the population) are perceived abnormal. For example, the average IQ is 100, most people (68%) have an IQ between 85 and 115. Only 2% of people have an IQ of below 70 and this would be used to diagnose Intellectual Disability Disorder.
Definitions of Abnormality: Statistical Infrequency (AO 3) Not all statistically infrequent behaviours are seen as abnormal. Some rare behaviours and characteristics are positive and seen as desirable. E. g. Being highly intelligent would be statistically infrequent but not abnormal. This definition has real life applications and is actually used in the diagnosis of some illnesses (such as intellectual disability disorder). This definition is a useful part of clinical assessment of psychological illness. Some abnormal behaviours can occur frequently: It is not the case that abnormal, as in unhelpful and painful, behaviours occur rarely. Depression is an example, where it is argued that 25% of the population will experience a mental health issue at some point in their lives. The decision of where to start the "abnormal" classification is arbitrary. Who decides what is statistically rare and how do they decide? For example, if an IQ of 70 is the cut-off point, how can we justify saying someone with 69 is abnormal, and someone with 70 normal? PROGRESS CHECK! Evaluation Activity: Decide if these evaluation points are positive or negative. Cut and stick them in your book clearly explain why they are or .
Specification Content: What the AQA say you should know… Behavioural, Emotional and Cognitive Characteristics of Phobias.
Clinical Characteristics of Phobias: What is a phobia? Phobias are a type of anxiety disorder. A Phobia is an intense irrational fear to an object, place or situation. Phobias are characterised by uncontrollable and extreme fears which are disproportionate to any actual risk of danger. Understanding Activity: What are the key words? Highlight no more than 5 and then come up with your own definition of a phobia in your learning book. PROGRESS CHECK!
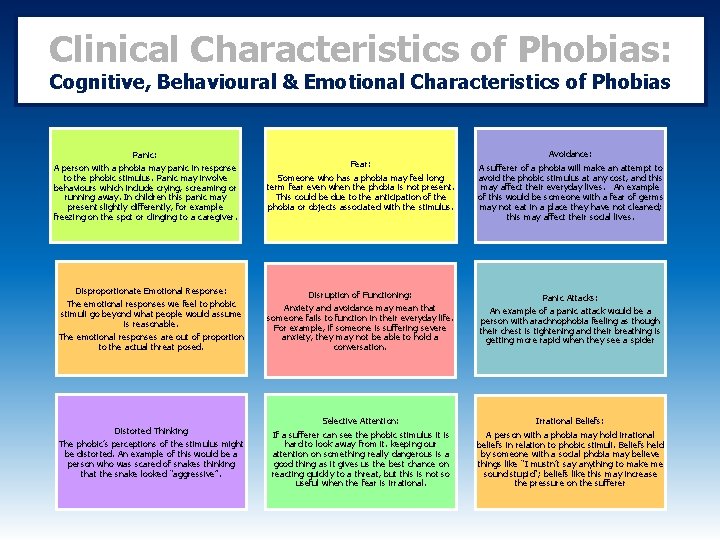
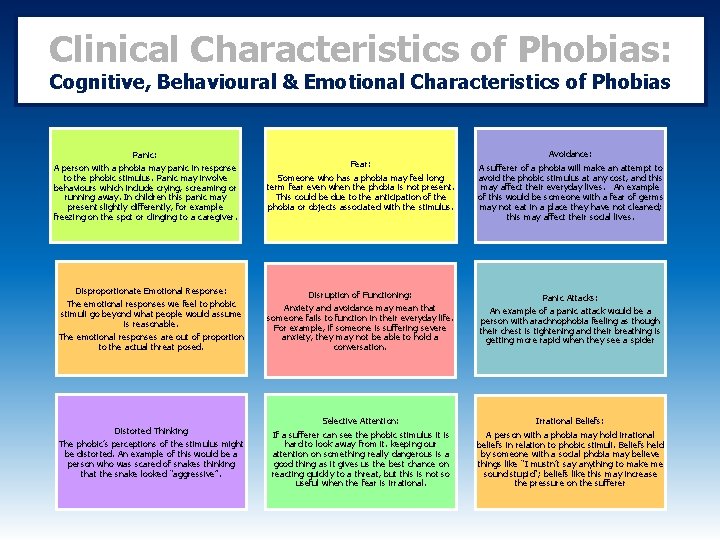
Clinical Characteristics of Phobias: Cognitive, Behavioural & Emotional Characteristics of Phobias Fear: Someone who has a phobia may feel long term fear even when the phobia is not present. This could be due to the anticipation of the phobia or objects associated with the stimulus. Avoidance: A sufferer of a phobia will make an attempt to avoid the phobic stimulus at any cost, and this may affect their everyday lives. An example of this would be someone with a fear of germs may not eat in a place they have not cleaned; this may affect their social lives. Disproportionate Emotional Response: The emotional responses we feel to phobic stimuli go beyond what people would assume is reasonable. The emotional responses are out of proportion to the actual threat posed. Disruption of Functioning: Anxiety and avoidance may mean that someone fails to function in their everyday life. For example, if someone is suffering severe anxiety, they may not be able to hold a conversation. Panic Attacks: An example of a panic attack would be a person with arachnophobia feeling as though their chest is tightening and their breathing is getting more rapid when they see a spider Distorted Thinking The phobic’s perceptions of the stimulus might be distorted. An example of this would be a person who was scared of snakes thinking that the snake looked “aggressive”. Selective Attention: If a sufferer can see the phobic stimulus it is hard to look away from it. keeping our attention on something really dangerous is a good thing as it gives us the best chance on reacting quickly to a threat, but this is not so useful when the fear is irrational. Irrational Beliefs: A person with a phobia may hold irrational beliefs in relation to phobic stimuli. Beliefs held by someone with a social phobia may believe things like “I mustn’t say anything to make me sound stupid”; beliefs like this may increase the pressure on the sufferer Panic: A person with a phobia may panic in response to the phobic stimulus. Panic may involve behaviours which include crying, screaming or running away. In children this panic may present slightly differently, for example freezing on the spot or clinging to a caregiver.
Specification Content: What the AQA say you should know… The behavioural approach to explaining phobias; • The Two-Process Model – Classical and Operant conditioning.
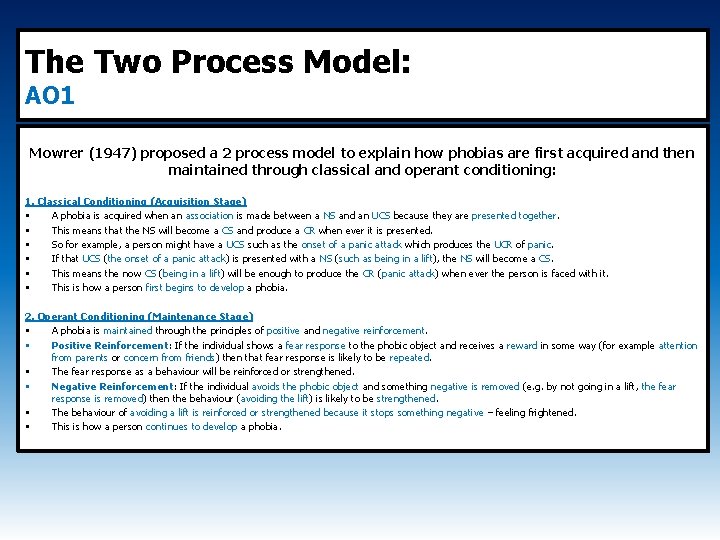
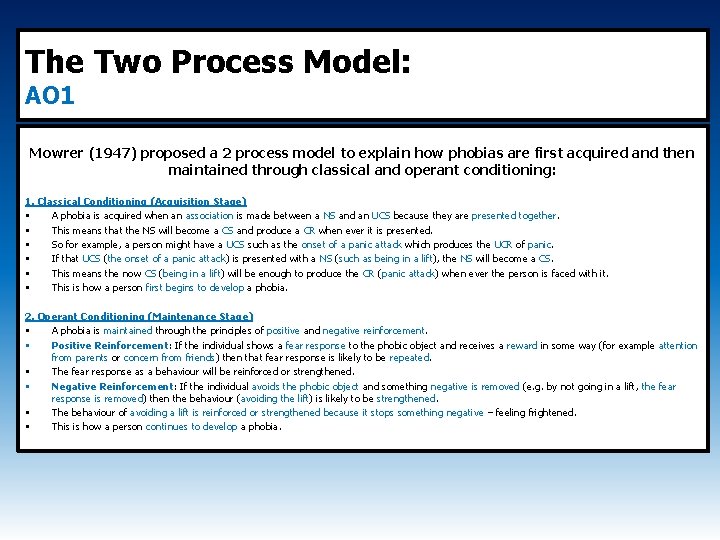
The Two Process Model: AO 1 Mowrer (1947) proposed a 2 process model to explain how phobias are first acquired and then maintained through classical and operant conditioning: 1. Classical Conditioning (Acquisition Stage) • A phobia is acquired when an association is made between a NS and an UCS because they are presented together. • This means that the NS will become a CS and produce a CR when ever it is presented. • So for example, a person might have a UCS such as the onset of a panic attack which produces the UCR of panic. • If that UCS (the onset of a panic attack) is presented with a NS (such as being in a lift), the NS will become a CS. • This means the now CS (being in a lift) will be enough to produce the CR (panic attack) when ever the person is faced with it. • This is how a person first begins to develop a phobia. 2. Operant Conditioning (Maintenance Stage) • A phobia is maintained through the principles of positive and negative reinforcement. • Positive Reinforcement: If the individual shows a fear response to the phobic object and receives a reward in some way (for example attention from parents or concern from friends) then that fear response is likely to be repeated. • The fear response as a behaviour will be reinforced or strengthened. • Negative Reinforcement: If the individual avoids the phobic object and something negative is removed (e. g. by not going in a lift, the fear response is removed) then the behaviour (avoiding the lift) is likely to be strengthened. • The behaviour of avoiding a lift is reinforced or strengthened because it stops something negative – feeling frightened. • This is how a person continues to develop a phobia.
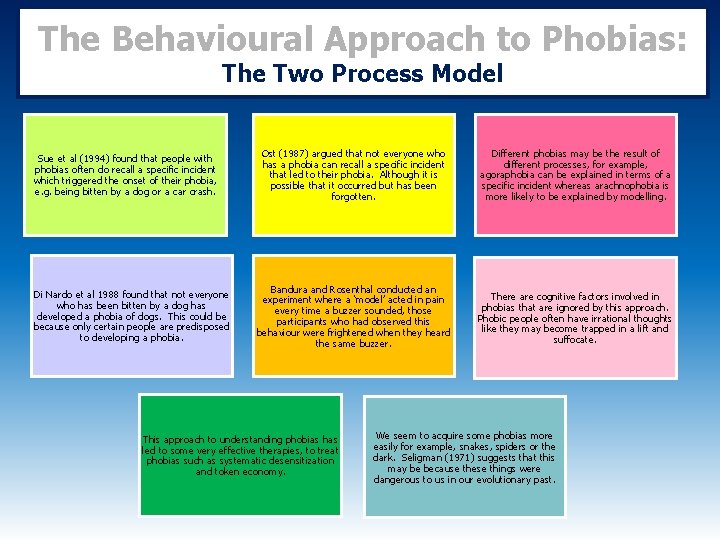
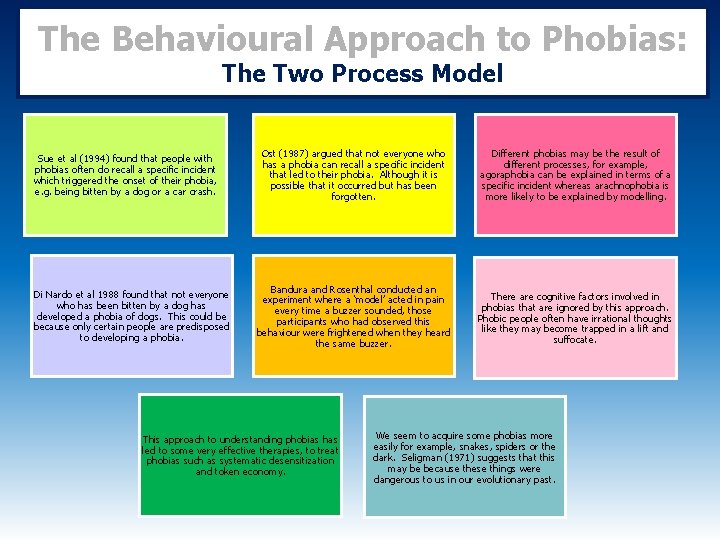
The Behavioural Approach to Phobias: The Two Process Model Sue et al (1994) found that people with phobias often do recall a specific incident which triggered the onset of their phobia, e. g. being bitten by a dog or a car crash. Di Nardo et al 1988 found that not everyone who has been bitten by a dog has developed a phobia of dogs. This could be because only certain people are predisposed to developing a phobia. Ost (1987) argued that not everyone who has a phobia can recall a specific incident that led to their phobia. Although it is possible that it occurred but has been forgotten. Different phobias may be the result of different processes, for example, agoraphobia can be explained in terms of a specific incident whereas arachnophobia is more likely to be explained by modelling. Bandura and Rosenthal conducted an experiment where a ‘model’ acted in pain every time a buzzer sounded, those participants who had observed this behaviour were frightened when they heard the same buzzer. There are cognitive factors involved in phobias that are ignored by this approach. Phobic people often have irrational thoughts like they may become trapped in a lift and suffocate. This approach to understanding phobias has led to some very effective therapies, to treat phobias such as systematic desensitization and token economy. We seem to acquire some phobias more easily for example, snakes, spiders or the dark. Seligman (1971) suggests that this may be because these things were dangerous to us in our evolutionary past.
Specification Content: What the AQA say you should know… The behavioural approach to treating phobias: • Systematic Desensitisation, including relaxation and use of hierarchy. • Flooding.
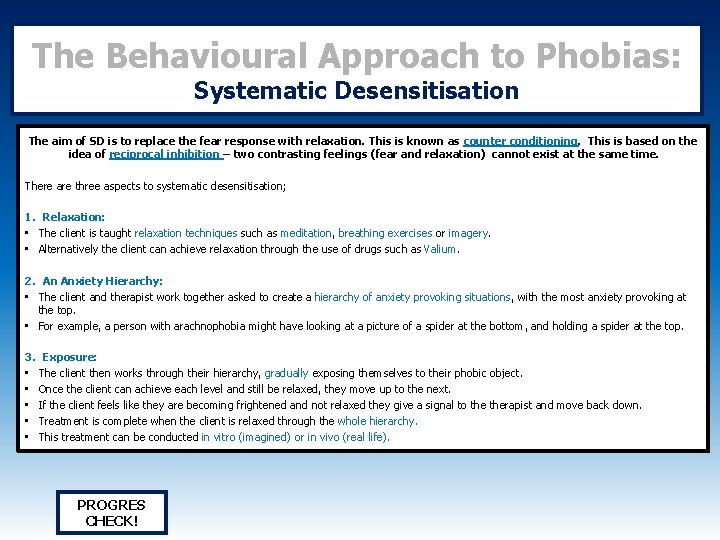
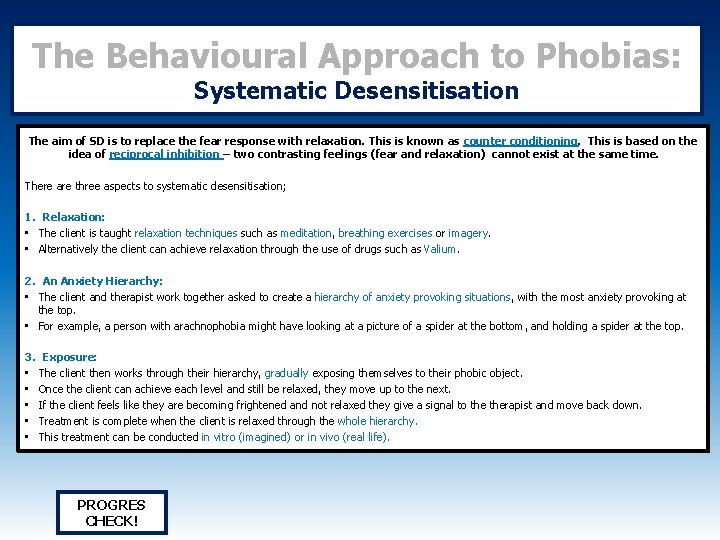
The Behavioural Approach to Phobias: Systematic Desensitisation The aim of SD is to replace the fear response with relaxation. This is known as counter conditioning. This is based on the idea of reciprocal inhibition – two contrasting feelings (fear and relaxation) cannot exist at the same time. There are three aspects to systematic desensitisation; 1. Relaxation: • The client is taught relaxation techniques such as meditation, breathing exercises or imagery. • Alternatively the client can achieve relaxation through the use of drugs such as Valium. 2. An Anxiety Hierarchy: • The client and therapist work together asked to create a hierarchy of anxiety provoking situations, with the most anxiety provoking at the top. • For example, a person with arachnophobia might have looking at a picture of a spider at the bottom, and holding a spider at the top. 3. Exposure: • The client then works through their hierarchy, gradually exposing themselves to their phobic object. • Once the client can achieve each level and still be relaxed, they move up to the next. • If the client feels like they are becoming frightened and not relaxed they give a signal to therapist and move back down. • Treatment is complete when the client is relaxed through the whole hierarchy. • This treatment can be conducted in vitro (imagined) or in vivo (real life). PROGRES CHECK!
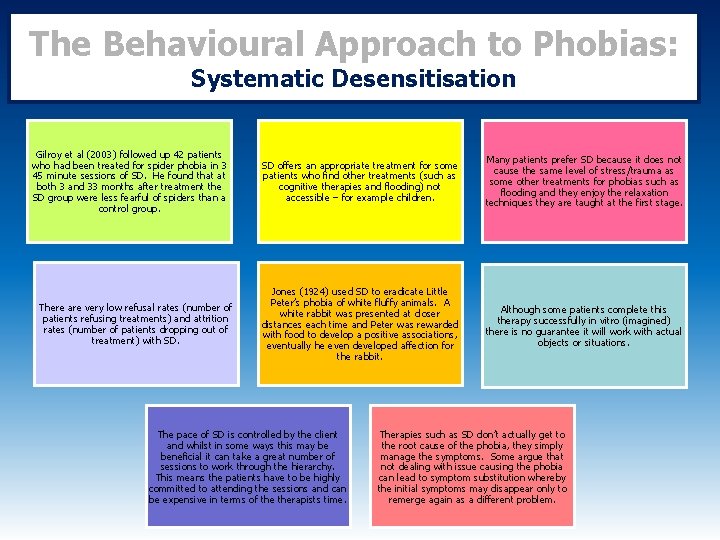
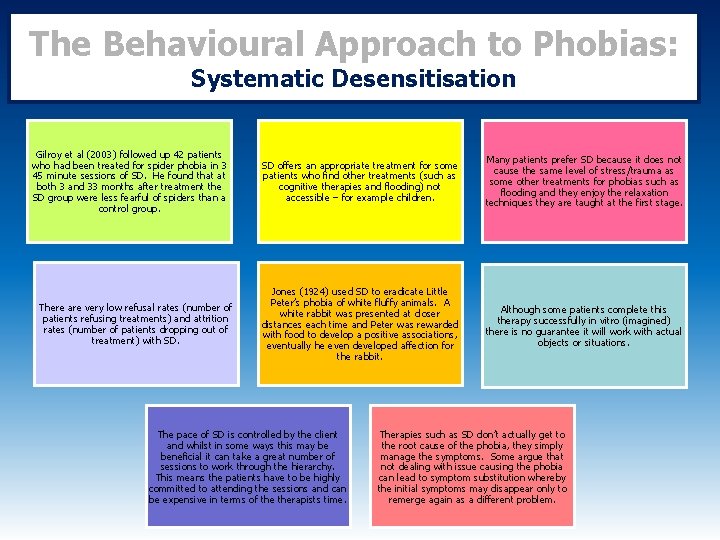
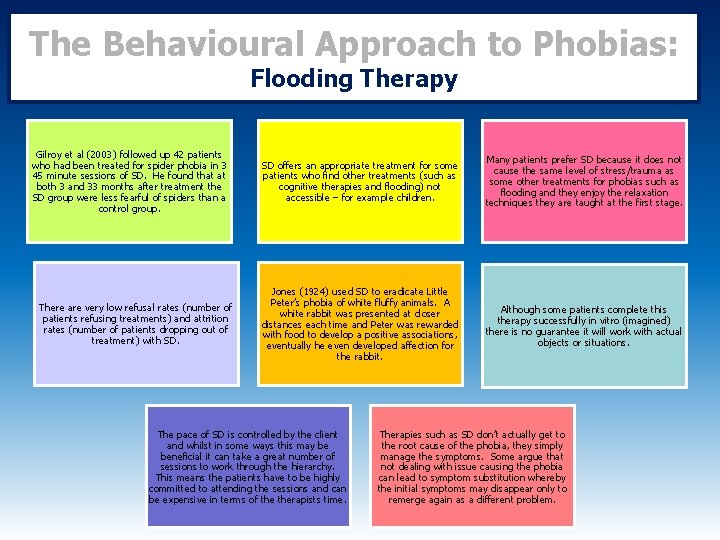
The Behavioural Approach to Phobias: Systematic Desensitisation Gilroy et al (2003) followed up 42 patients who had been treated for spider phobia in 3 45 minute sessions of SD. He found that at both 3 and 33 months after treatment the SD group were less fearful of spiders than a control group. There are very low refusal rates (number of patients refusing treatments) and attrition rates (number of patients dropping out of treatment) with SD. SD offers an appropriate treatment for some patients who find other treatments (such as cognitive therapies and flooding) not accessible – for example children. Many patients prefer SD because it does not cause the same level of stress/trauma as some other treatments for phobias such as flooding and they enjoy the relaxation techniques they are taught at the first stage. Jones (1924) used SD to eradicate Little Peter’s phobia of white fluffy animals. A white rabbit was presented at closer distances each time and Peter was rewarded with food to develop a positive associations, eventually he even developed affection for the rabbit. Although some patients complete this therapy successfully in vitro (imagined) there is no guarantee it will work with actual objects or situations. The pace of SD is controlled by the client and whilst in some ways this may be beneficial it can take a great number of sessions to work through the hierarchy. This means the patients have to be highly committed to attending the sessions and can be expensive in terms of therapists time. Therapies such as SD don’t actually get to the root cause of the phobia, they simply manage the symptoms. Some argue that not dealing with issue causing the phobia can lead to symptom substitution whereby the initial symptoms may disappear only to remerge again as a different problem.
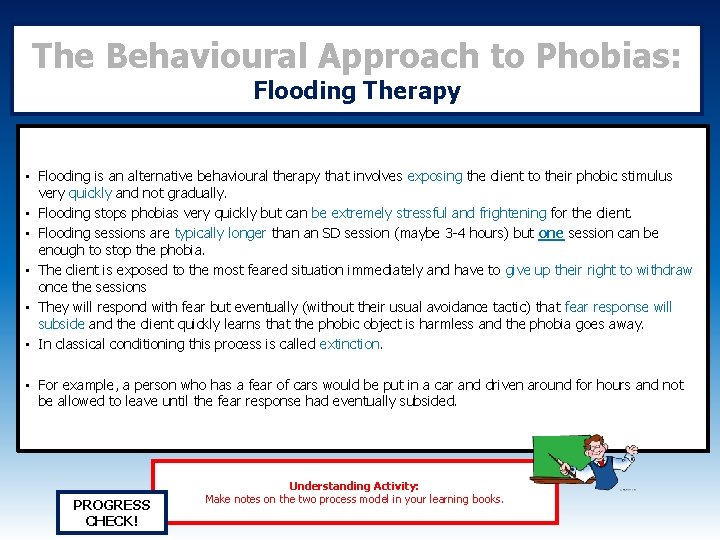
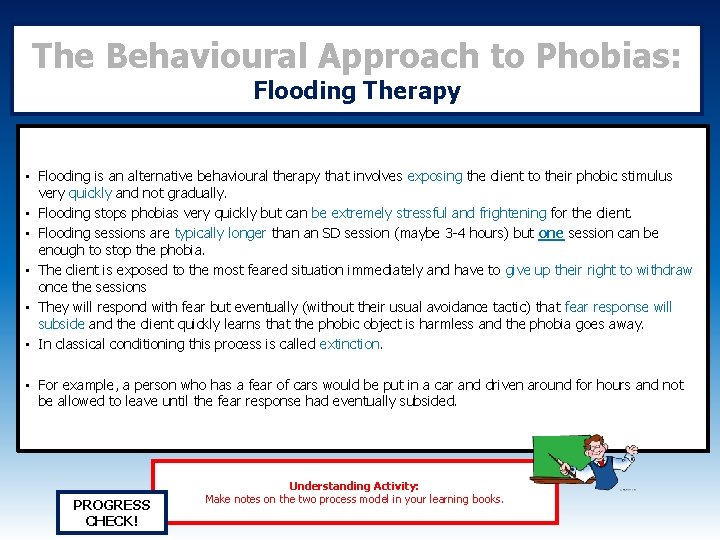
The Behavioural Approach to Phobias: Flooding Therapy • Flooding is an alternative behavioural therapy that involves exposing the client to their phobic stimulus very quickly and not gradually. • Flooding stops phobias very quickly but can be extremely stressful and frightening for the client. • Flooding sessions are typically longer than an SD session (maybe 3 -4 hours) but one session can be enough to stop the phobia. • The client is exposed to the most feared situation immediately and have to give up their right to withdraw once the sessions • They will respond with fear but eventually (without their usual avoidance tactic) that fear response will subside and the client quickly learns that the phobic object is harmless and the phobia goes away. • In classical conditioning this process is called extinction. • For example, a person who has a fear of cars would be put in a car and driven around for hours and not be allowed to leave until the fear response had eventually subsided. PROGRESS CHECK! Understanding Activity: Make notes on the two process model in your learning books.
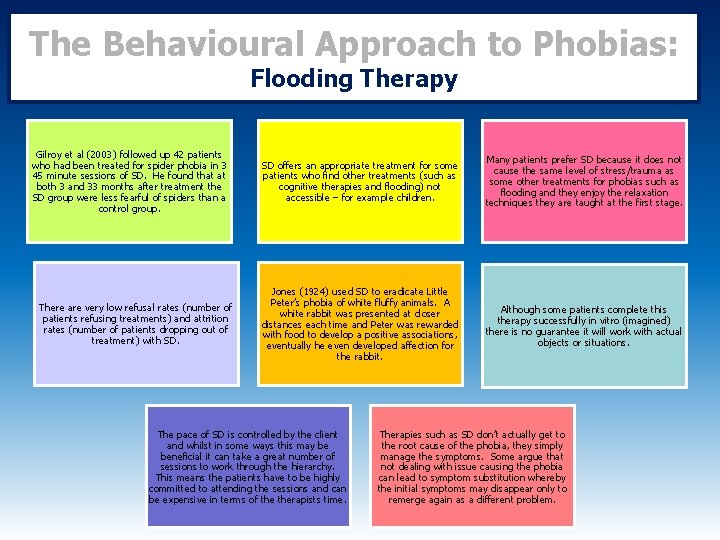
The Behavioural Approach to Phobias: Flooding Therapy Gilroy et al (2003) followed up 42 patients who had been treated for spider phobia in 3 45 minute sessions of SD. He found that at both 3 and 33 months after treatment the SD group were less fearful of spiders than a control group. There are very low refusal rates (number of patients refusing treatments) and attrition rates (number of patients dropping out of treatment) with SD. SD offers an appropriate treatment for some patients who find other treatments (such as cognitive therapies and flooding) not accessible – for example children. Many patients prefer SD because it does not cause the same level of stress/trauma as some other treatments for phobias such as flooding and they enjoy the relaxation techniques they are taught at the first stage. Jones (1924) used SD to eradicate Little Peter’s phobia of white fluffy animals. A white rabbit was presented at closer distances each time and Peter was rewarded with food to develop a positive associations, eventually he even developed affection for the rabbit. Although some patients complete this therapy successfully in vitro (imagined) there is no guarantee it will work with actual objects or situations. The pace of SD is controlled by the client and whilst in some ways this may be beneficial it can take a great number of sessions to work through the hierarchy. This means the patients have to be highly committed to attending the sessions and can be expensive in terms of therapists time. Therapies such as SD don’t actually get to the root cause of the phobia, they simply manage the symptoms. Some argue that not dealing with issue causing the phobia can lead to symptom substitution whereby the initial symptoms may disappear only to remerge again as a different problem.
Specification Content: What the AQA say you should know… Behavioural, Emotional and Cognitive Characteristics of Depression.
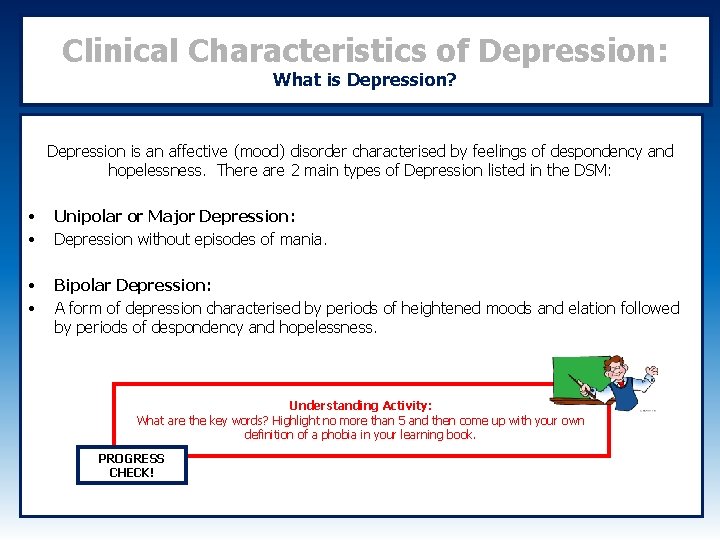
Clinical Characteristics of Depression: What is Depression? Depression is an affective (mood) disorder characterised by feelings of despondency and hopelessness. There are 2 main types of Depression listed in the DSM: • • Unipolar or Major Depression: Depression without episodes of mania. • • Bipolar Depression: A form of depression characterised by periods of heightened moods and elation followed by periods of despondency and hopelessness. Understanding Activity: What are the key words? Highlight no more than 5 and then come up with your own definition of a phobia in your learning book. PROGRESS CHECK!
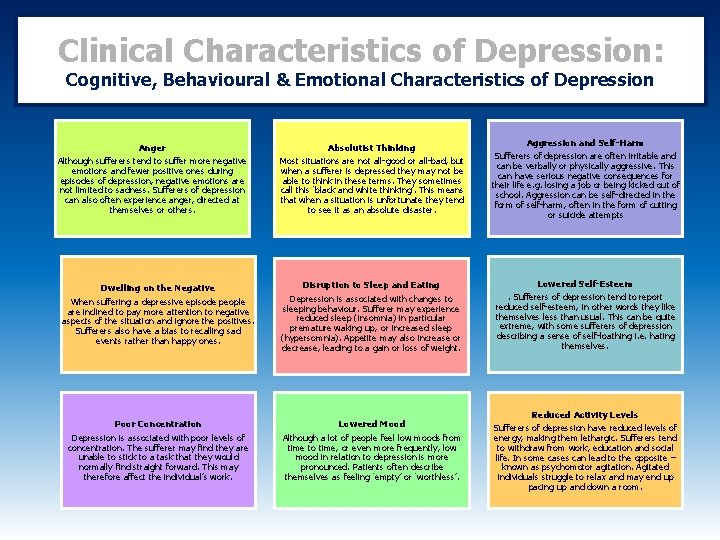
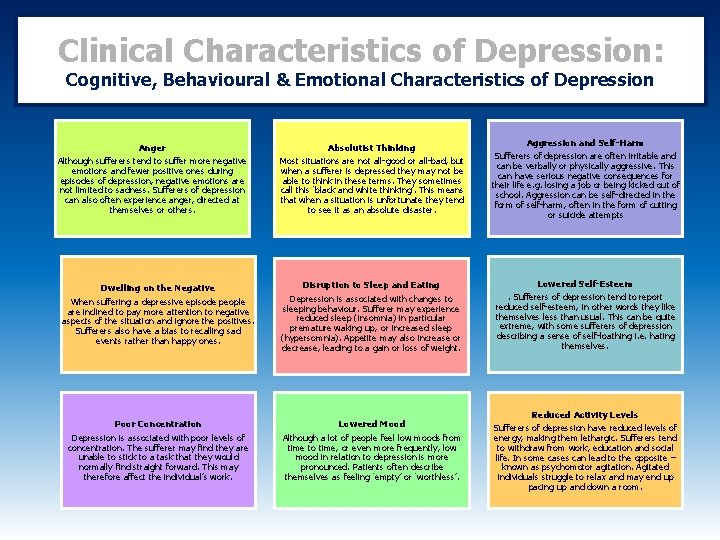
Clinical Characteristics of Depression: Cognitive, Behavioural & Emotional Characteristics of Depression Absolutist Thinking Most situations are not all-good or all-bad, but when a sufferer is depressed they may not be able to think in these terms. They sometimes call this ‘black and white thinking’. This means that when a situation is unfortunate they tend to see it as an absolute disaster. Aggression and Self-Harm Sufferers of depression are often irritable and can be verbally or physically aggressive. This can have serious negative consequences for their life e. g. losing a job or being kicked out of school. Aggression can be self-directed in the form of self-harm, often in the form of cutting or suicide attempts Dwelling on the Negative When suffering a depressive episode people are inclined to pay more attention to negative aspects of the situation and ignore the positives. Sufferers also have a bias to recalling sad events rather than happy ones. Disruption to Sleep and Eating Depression is associated with changes to sleeping behaviour. Sufferer may experience reduced sleep (insomnia) in particular premature waking up, or increased sleep (hypersomnia). Appetite may also increase or decrease, leading to a gain or loss of weight. Lowered Self-Esteem. Sufferers of depression tend to report reduced self-esteem, in other words they like themselves less than usual. This can be quite extreme, with some sufferers of depression describing a sense of self-loathing i. e. hating themselves. Poor Concentration Depression is associated with poor levels of concentration. The sufferer may find they are unable to stick to a task that they would normally find straight forward. This may therefore affect the individual’s work. Lowered Mood Although a lot of people feel low moods from time to time, or even more frequently, low mood in relation to depression is more pronounced. Patients often describe themselves as feeling ‘empty’ or ‘worthless’. Reduced Activity Levels Sufferers of depression have reduced levels of energy, making them lethargic. Sufferers tend to withdraw from work, education and social life. In some cases can lead to the opposite – known as psychomotor agitation. Agitated individuals struggle to relax and may end up pacing up and down a room. Anger Although sufferers tend to suffer more negative emotions and fewer positive ones during episodes of depression, negative emotions are not limited to sadness. Sufferers of depression can also often experience anger, directed at themselves or others.
Specification Content: What the AQA say you should know… The cognitive approach to explaining depression: • Beck’s Negative Triad • Ellis’s ABC Model
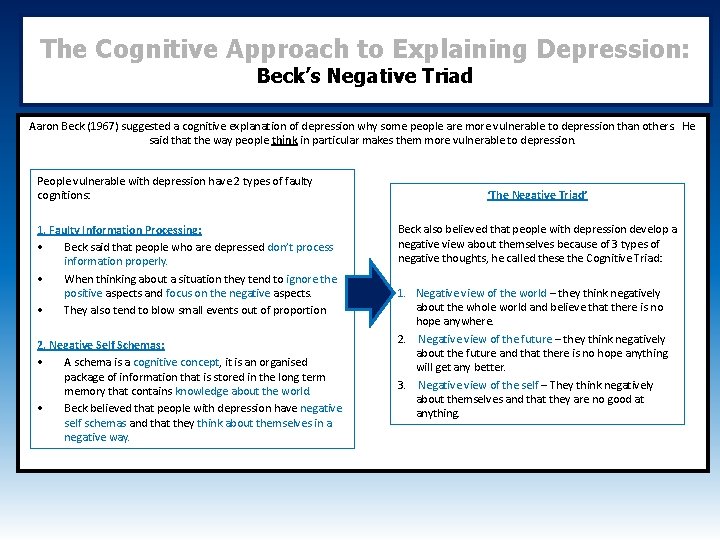
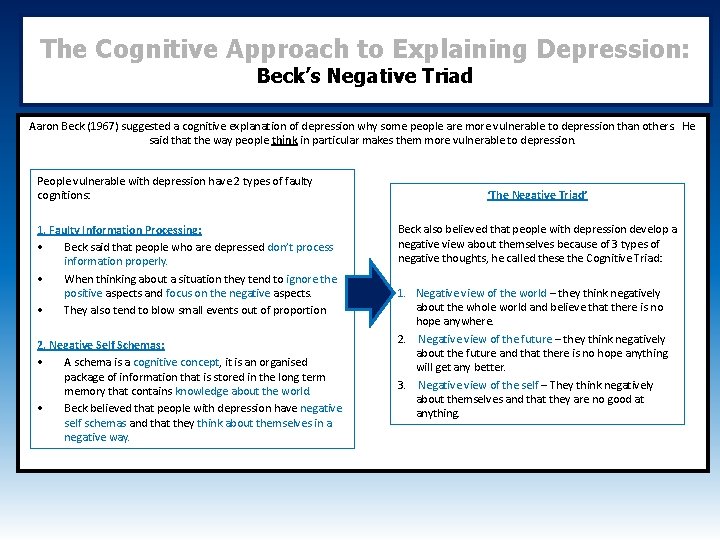
The Cognitive Approach to Explaining Depression: Beck’s Negative Triad Aaron Beck (1967) suggested a cognitive explanation of depression why some people are more vulnerable to depression than others. He said that the way people think in particular makes them more vulnerable to depression. People vulnerable with depression have 2 types of faulty cognitions: 1. Faulty Information Processing; • Beck said that people who are depressed don’t process information properly. • When thinking about a situation they tend to ignore the positive aspects and focus on the negative aspects. • They also tend to blow small events out of proportion 2. Negative Self Schemas: • A schema is a cognitive concept, it is an organised package of information that is stored in the long term memory that contains knowledge about the world. • Beck believed that people with depression have negative self schemas and that they think about themselves in a negative way. ‘The Negative Triad’ Beck also believed that people with depression develop a negative view about themselves because of 3 types of negative thoughts, he called these the Cognitive Triad: 1. Negative view of the world – they think negatively about the whole world and believe that there is no hope anywhere. 2. Negative view of the future – they think negatively about the future and that there is no hope anything will get any better. 3. Negative view of the self – They think negatively about themselves and that they are no good at anything.
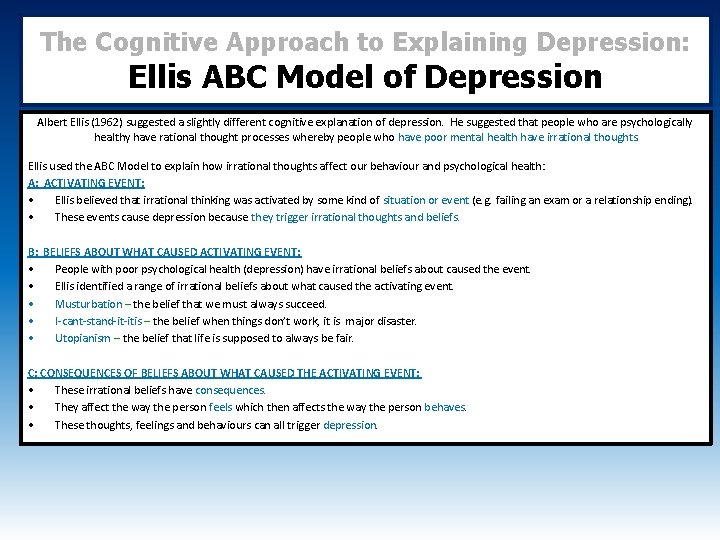
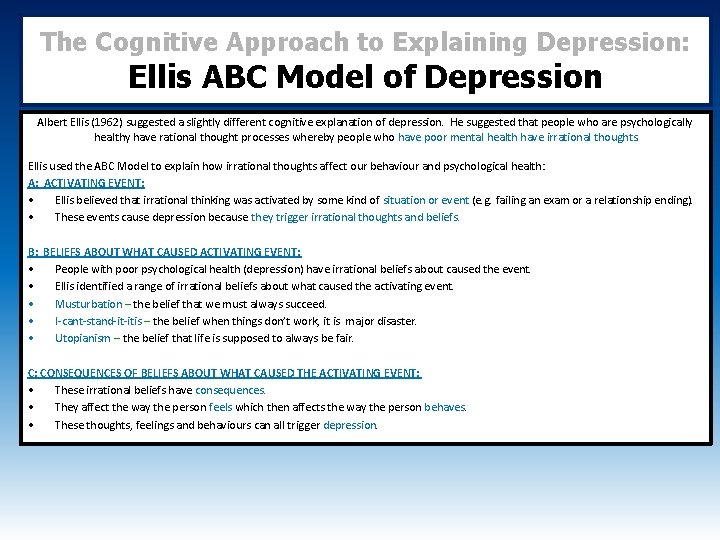
The Cognitive Approach to Explaining Depression: Ellis ABC Model of Depression Albert Ellis (1962) suggested a slightly different cognitive explanation of depression. He suggested that people who are psychologically healthy have rational thought processes whereby people who have poor mental health have irrational thoughts. Ellis used the ABC Model to explain how irrational thoughts affect our behaviour and psychological health: A: ACTIVATING EVENT: • Ellis believed that irrational thinking was activated by some kind of situation or event (e. g. failing an exam or a relationship ending). • These events cause depression because they trigger irrational thoughts and beliefs. B: BELIEFS ABOUT WHAT CAUSED ACTIVATING EVENT: • People with poor psychological health (depression) have irrational beliefs about caused the event. • Ellis identified a range of irrational beliefs about what caused the activating event. • Musturbation – the belief that we must always succeed. • I-cant-stand-it-itis – the belief when things don’t work, it is major disaster. • Utopianism – the belief that life is supposed to always be fair. C: CONSEQUENCES OF BELIEFS ABOUT WHAT CAUSED THE ACTIVATING EVENT: • These irrational beliefs have consequences. • They affect the way the person feels which then affects the way the person behaves. • These thoughts, feelings and behaviours can all trigger depression.
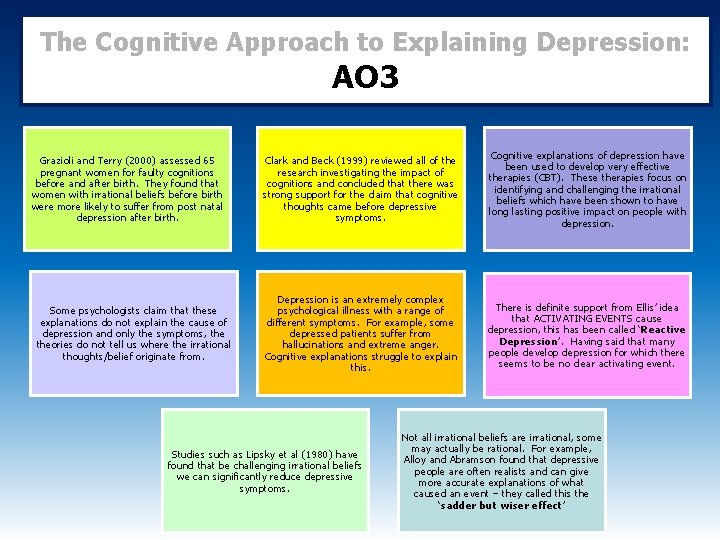
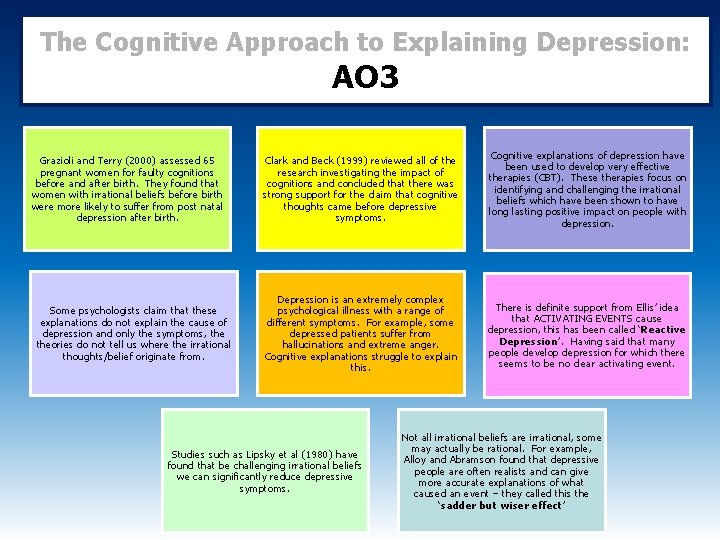
The Cognitive Approach to Explaining Depression: AO 3 Grazioli and Terry (2000) assessed 65 pregnant women for faulty cognitions before and after birth. They found that women with irrational beliefs before birth were more likely to suffer from post natal depression after birth. Some psychologists claim that these explanations do not explain the cause of depression and only the symptoms, theories do not tell us where the irrational thoughts/belief originate from. Clark and Beck (1999) reviewed all of the research investigating the impact of cognitions and concluded that there was strong support for the claim that cognitive thoughts came before depressive symptoms. Cognitive explanations of depression have been used to develop very effective therapies (CBT). These therapies focus on identifying and challenging the irrational beliefs which have been shown to have long lasting positive impact on people with depression. Depression is an extremely complex psychological illness with a range of different symptoms. For example, some depressed patients suffer from hallucinations and extreme anger. Cognitive explanations struggle to explain this. There is definite support from Ellis’ idea that ACTIVATING EVENTS cause depression, this has been called ‘Reactive Depression’. Having said that many people develop depression for which there seems to be no clear activating event. Studies such as Lipsky et al (1980) have found that be challenging irrational beliefs we can significantly reduce depressive symptoms. Not all irrational beliefs are irrational, some may actually be rational. For example, Alloy and Abramson found that depressive people are often realists and can give more accurate explanations of what caused an event – they called this the ‘sadder but wiser effect’
Specification Content: What the AQA say you should know… The Cognitive approach to treating depression, Cognitive behaviour therapy (CBT), including challenging irrational thoughts.
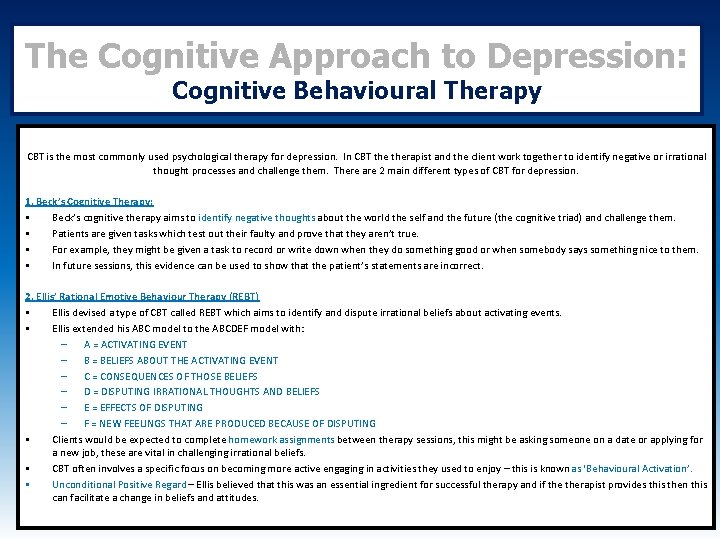
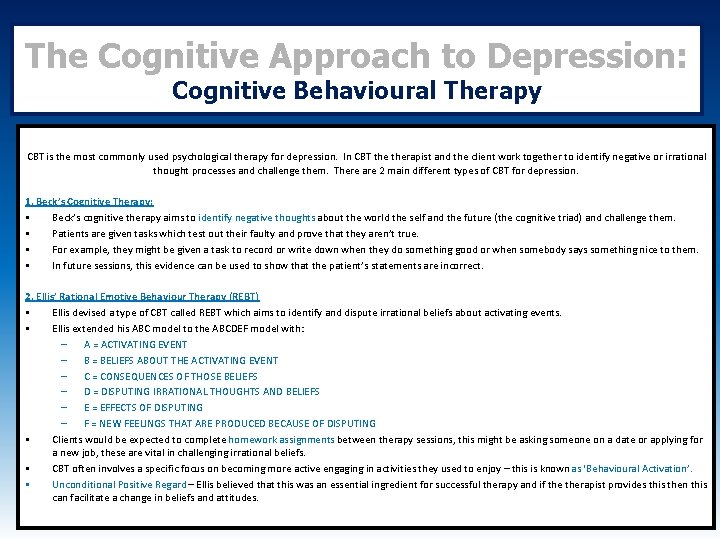
The Cognitive Approach to Depression: Cognitive Behavioural Therapy CBT is the most commonly used psychological therapy for depression. In CBT therapist and the client work together to identify negative or irrational thought processes and challenge them. There are 2 main different types of CBT for depression. 1. Beck’s Cognitive Therapy: • Beck’s cognitive therapy aims to identify negative thoughts about the world the self and the future (the cognitive triad) and challenge them. • Patients are given tasks which test out their faulty and prove that they aren’t true. • For example, they might be given a task to record or write down when they do something good or when somebody says something nice to them. • In future sessions, this evidence can be used to show that the patient’s statements are incorrect. 2. Ellis’ Rational Emotive Behaviour Therapy (REBT) • Ellis devised a type of CBT called REBT which aims to identify and dispute irrational beliefs about activating events. • Ellis extended his ABC model to the ABCDEF model with: – A = ACTIVATING EVENT – B = BELIEFS ABOUT THE ACTIVATING EVENT – C = CONSEQUENCES OF THOSE BELIEFS – D = DISPUTING IRRATIONAL THOUGHTS AND BELIEFS – E = EFFECTS OF DISPUTING – F = NEW FEELINGS THAT ARE PRODUCED BECAUSE OF DISPUTING • Clients would be expected to complete homework assignments between therapy sessions, this might be asking someone on a date or applying for a new job, these are vital in challenging irrational beliefs. • CBT often involves a specific focus on becoming more active engaging in activities they used to enjoy – this is known as ‘Behavioural Activation’. • Unconditional Positive Regard – Ellis believed that this was an essential ingredient for successful therapy and if therapist provides this then this can facilitate a change in beliefs and attitudes.
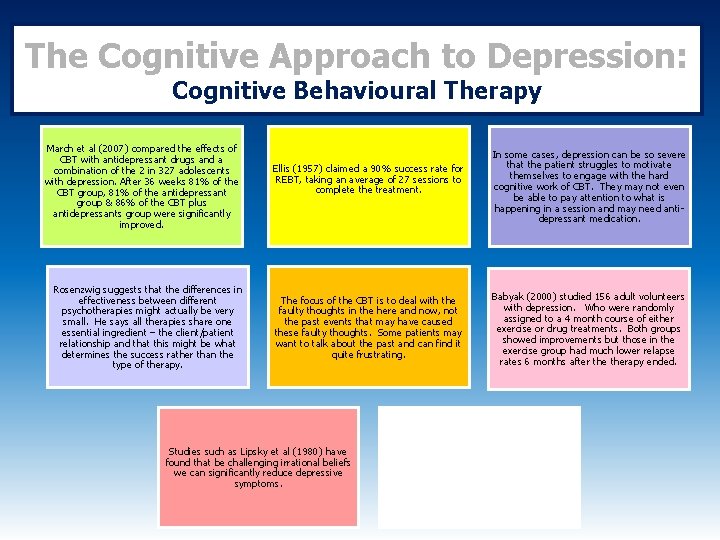
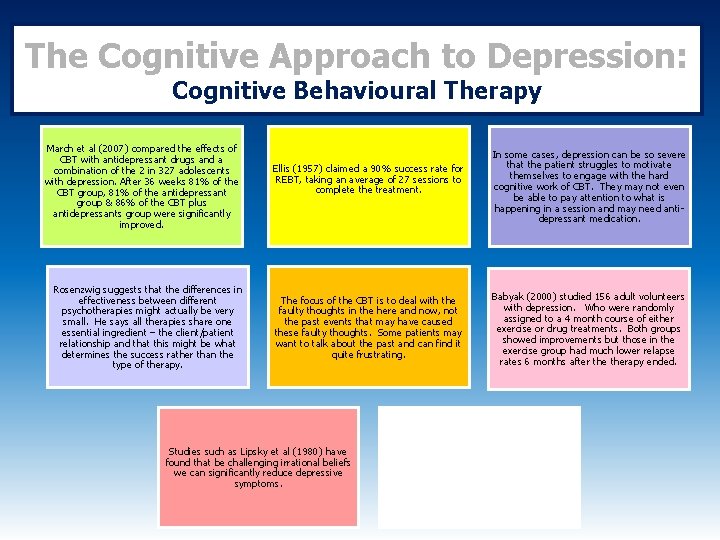
The Cognitive Approach to Depression: Cognitive Behavioural Therapy March et al (2007) compared the effects of CBT with antidepressant drugs and a combination of the 2 in 327 adolescents with depression. After 36 weeks 81% of the CBT group, 81% of the antidepressant group & 86% of the CBT plus antidepressants group were significantly improved. Rosenzwig suggests that the differences in effectiveness between different psychotherapies might actually be very small. He says all therapies share one essential ingredient – the client/patient relationship and that this might be what determines the success rather than the type of therapy. Ellis (1957) claimed a 90% success rate for REBT, taking an average of 27 sessions to complete the treatment. The focus of the CBT is to deal with the faulty thoughts in the here and now, not the past events that may have caused these faulty thoughts. Some patients may want to talk about the past and can find it quite frustrating. Studies such as Lipsky et al (1980) have found that be challenging irrational beliefs we can significantly reduce depressive symptoms. In some cases, depression can be so severe that the patient struggles to motivate themselves to engage with the hard cognitive work of CBT. They may not even be able to pay attention to what is happening in a session and may need antidepressant medication. Babyak (2000) studied 156 adult volunteers with depression. Who were randomly assigned to a 4 month course of either exercise or drug treatments. Both groups showed improvements but those in the exercise group had much lower relapse rates 6 months after therapy ended.
Specification Content: What the AQA say you should know… • Behavioural, Emotional and Cognitive Characteristics of OCD. • The biological approach to explaining OCD: Genetic and Neural explanations. • The biological approach to treating OCD: Drug Therapy
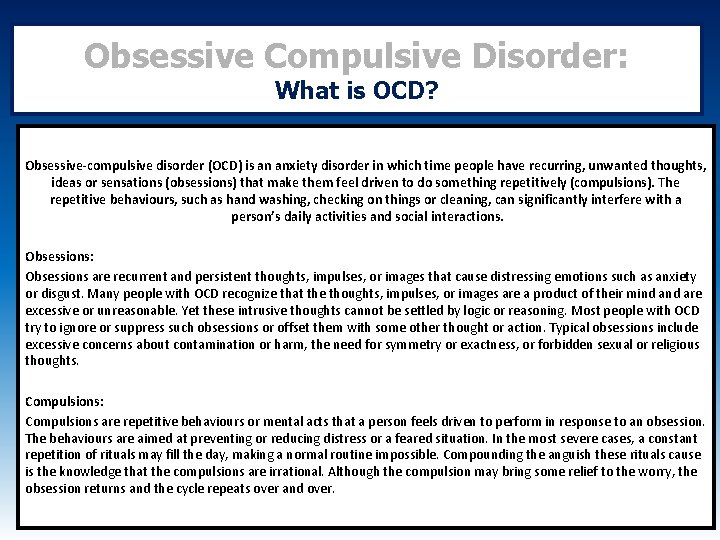
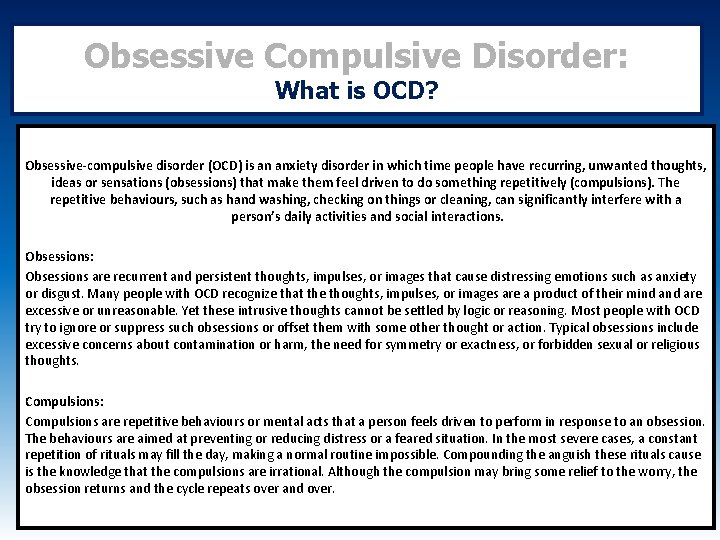
Obsessive Compulsive Disorder: What is OCD? Obsessive-compulsive disorder (OCD) is an anxiety disorder in which time people have recurring, unwanted thoughts, ideas or sensations (obsessions) that make them feel driven to do something repetitively (compulsions). The repetitive behaviours, such as hand washing, checking on things or cleaning, can significantly interfere with a person’s daily activities and social interactions. Obsessions: Obsessions are recurrent and persistent thoughts, impulses, or images that cause distressing emotions such as anxiety or disgust. Many people with OCD recognize that the thoughts, impulses, or images are a product of their mind are excessive or unreasonable. Yet these intrusive thoughts cannot be settled by logic or reasoning. Most people with OCD try to ignore or suppress such obsessions or offset them with some other thought or action. Typical obsessions include excessive concerns about contamination or harm, the need for symmetry or exactness, or forbidden sexual or religious thoughts. Compulsions: Compulsions are repetitive behaviours or mental acts that a person feels driven to perform in response to an obsession. The behaviours are aimed at preventing or reducing distress or a feared situation. In the most severe cases, a constant repetition of rituals may fill the day, making a normal routine impossible. Compounding the anguish these rituals cause is the knowledge that the compulsions are irrational. Although the compulsion may bring some relief to the worry, the obsession returns and the cycle repeats over and over.
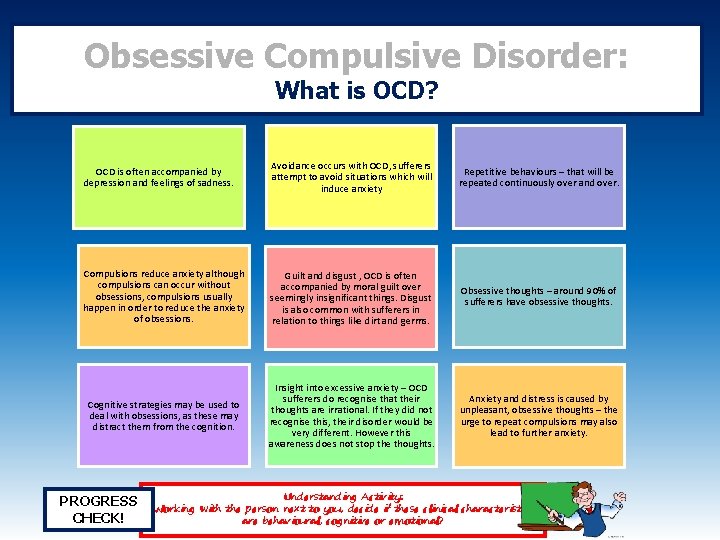
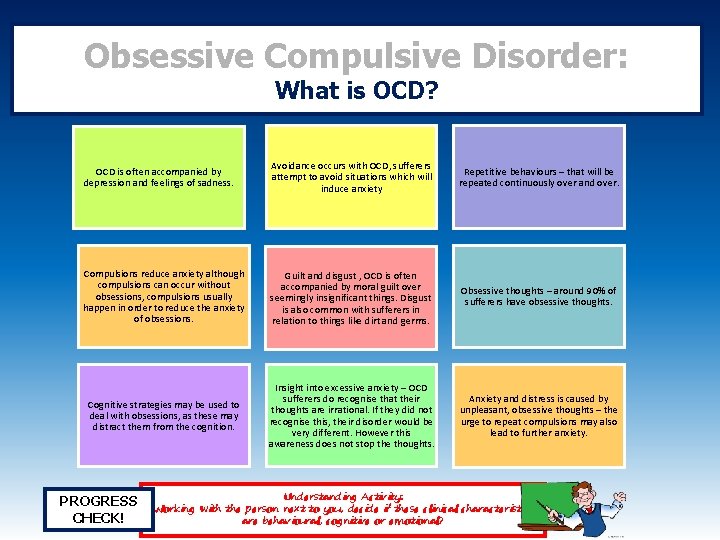
Obsessive Compulsive Disorder: What is OCD? OCD is often accompanied by depression and feelings of sadness. Avoidance occurs with OCD, sufferers attempt to avoid situations which will induce anxiety Repetitive behaviours – that will be repeated continuously over and over. Compulsions reduce anxiety although compulsions can occur without obsessions, compulsions usually happen in order to reduce the anxiety of obsessions. Guilt and disgust , OCD is often accompanied by moral guilt over seemingly insignificant things. Disgust is also common with sufferers in relation to things like dirt and germs. Obsessive thoughts – around 90% of sufferers have obsessive thoughts. Cognitive strategies may be used to deal with obsessions, as these may distract them from the cognition. Insight into excessive anxiety – OCD sufferers do recognise that their thoughts are irrational. If they did not recognise this, their disorder would be very different. However this awareness does not stop the thoughts. Anxiety and distress is caused by unpleasant, obsessive thoughts – the urge to repeat compulsions may also lead to further anxiety. PROGRESS CHECK! Understanding Activity: Working with the person next to you, decide if these clinical characteristics are behavioural, cognitive or emotional?
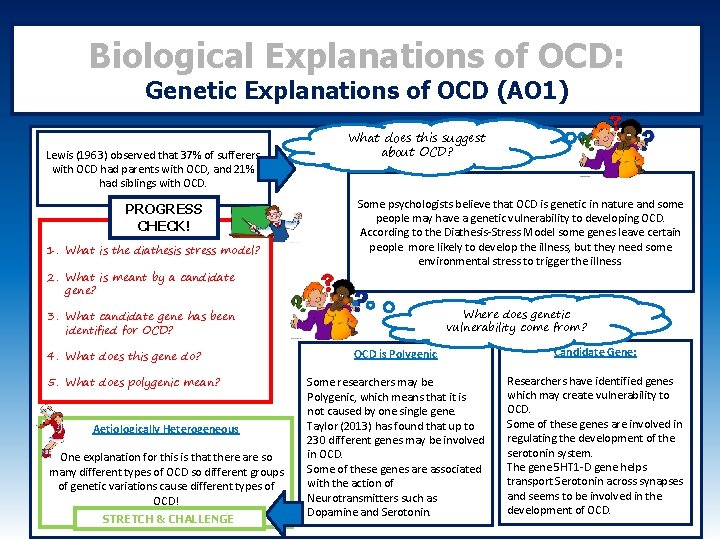
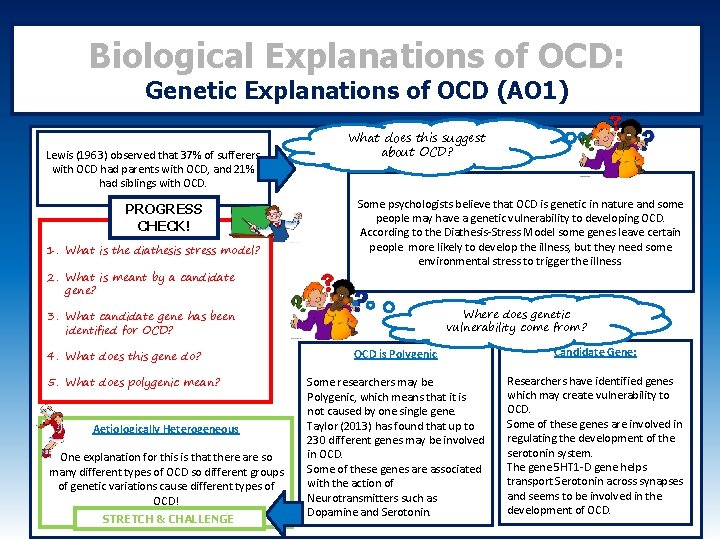
Biological Explanations of OCD: Genetic Explanations of OCD (AO 1) Lewis (1963) observed that 37% of sufferers with OCD had parents with OCD, and 21% had siblings with OCD. PROGRESS CHECK! 1. What is the diathesis stress model? 2. What is meant by a candidate gene? What does this suggest about OCD? Some psychologists believe that OCD is genetic in nature and some people may have a genetic vulnerability to developing OCD. According to the Diathesis-Stress Model some genes leave certain people more likely to develop the illness, but they need some environmental stress to trigger the illness. Where does genetic vulnerability come from? 3. What candidate gene has been identified for OCD? 4. What does this gene do? 5. What does polygenic mean? Aetiologically Heterogeneous One explanation for this is that there are so many different types of OCD so different groups of genetic variations cause different types of OCD! STRETCH & CHALLENGE OCD is Polygenic Candidate Gene: Some researchers may be Polygenic, which means that it is not caused by one single gene. Taylor (2013) has found that up to 230 different genes may be involved in OCD. Some of these genes are associated with the action of Neurotransmitters such as Dopamine and Serotonin. Researchers have identified genes which may create vulnerability to OCD. Some of these genes are involved in regulating the development of the serotonin system. The gene 5 HT 1 -D gene helps transport Serotonin across synapses and seems to be involved in the development of OCD.
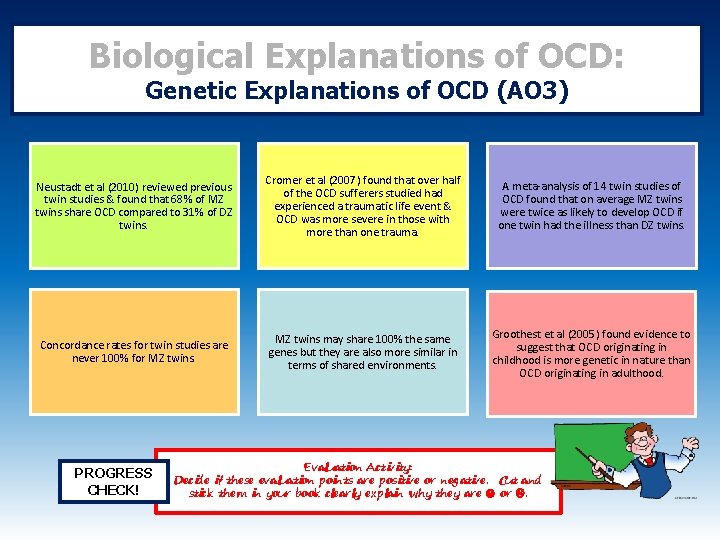
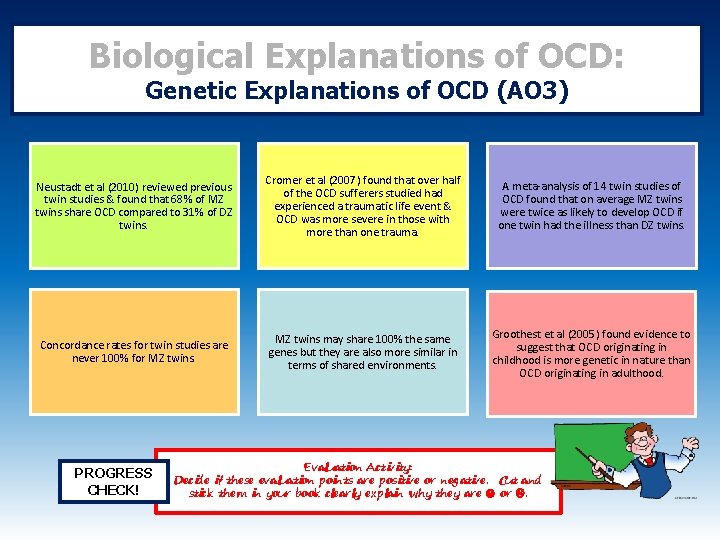
Biological Explanations of OCD: Genetic Explanations of OCD (AO 3) Neustadt et al (2010) reviewed previous twin studies & found that 68% of MZ twins share OCD compared to 31% of DZ twins. Cromer et al (2007) found that over half of the OCD sufferers studied had experienced a traumatic life event & OCD was more severe in those with more than one trauma. A meta-analysis of 14 twin studies of OCD found that on average MZ twins were twice as likely to develop OCD if one twin had the illness than DZ twins. Concordance rates for twin studies are never 100% for MZ twins may share 100% the same genes but they are also more similar in terms of shared environments. Groothest et al (2005) found evidence to suggest that OCD originating in childhood is more genetic in nature than OCD originating in adulthood. PROGRESS CHECK! Evaluation Activity: Decide if these evaluation points are positive or negative. Cut and stick them in your book clearly explain why they are or .
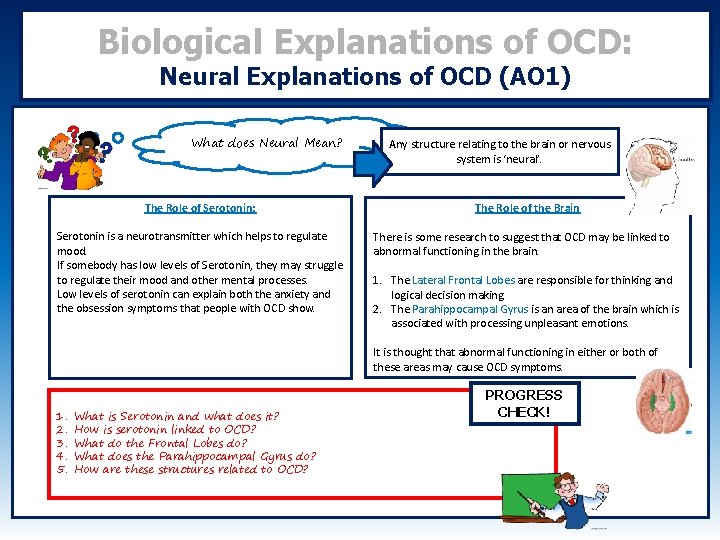
Biological Explanations of OCD: Neural Explanations of OCD (AO 1) What does Neural Mean? The Role of Serotonin: Serotonin is a neurotransmitter which helps to regulate mood. If somebody has low levels of Serotonin, they may struggle to regulate their mood and other mental processes. Low levels of serotonin can explain both the anxiety and the obsession symptoms that people with OCD show. Any structure relating to the brain or nervous system is ‘neural’. The Role of the Brain There is some research to suggest that OCD may be linked to abnormal functioning in the brain. 1. The Lateral Frontal Lobes are responsible for thinking and logical decision making. 2. The Parahippocampal Gyrus is an area of the brain which is associated with processing unpleasant emotions. It is thought that abnormal functioning in either or both of these areas may cause OCD symptoms. 1. 2. 3. 4. 5. What is Serotonin and what does it? How is serotonin linked to OCD? What do the Frontal Lobes do? What does the Parahippocampal Gyrus do? How are these structures related to OCD? PROGRESS CHECK!
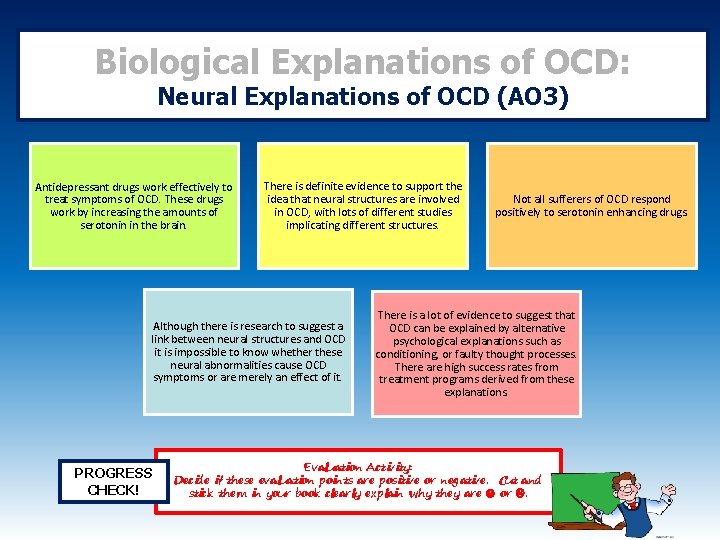
Biological Explanations of OCD: Neural Explanations of OCD (AO 3) Antidepressant drugs work effectively to treat symptoms of OCD. These drugs work by increasing the amounts of serotonin in the brain. There is definite evidence to support the idea that neural structures are involved in OCD, with lots of different studies implicating different structures. Although there is research to suggest a link between neural structures and OCD it is impossible to know whether these neural abnormalities cause OCD symptoms or are merely an effect of it. PROGRESS CHECK! Not all sufferers of OCD respond positively to serotonin enhancing drugs. There is a lot of evidence to suggest that OCD can be explained by alternative psychological explanations such as conditioning, or faulty thought processes. There are high success rates from treatment programs derived from these explanations. Evaluation Activity: Decide if these evaluation points are positive or negative. Cut and stick them in your book clearly explain why they are or .
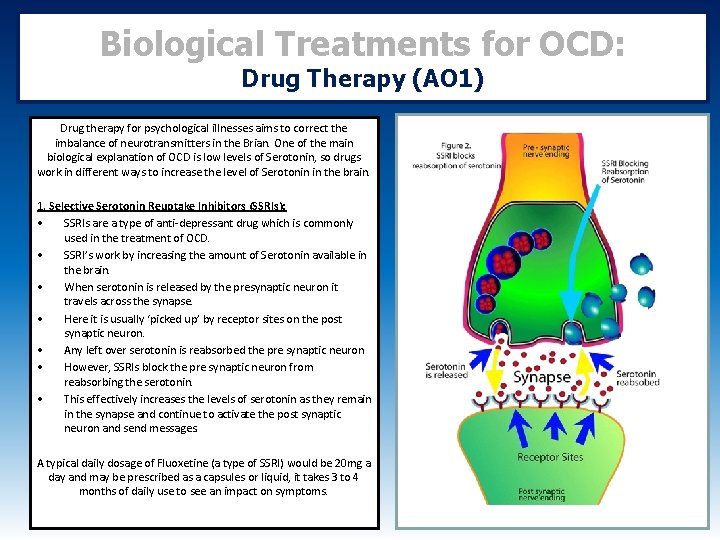
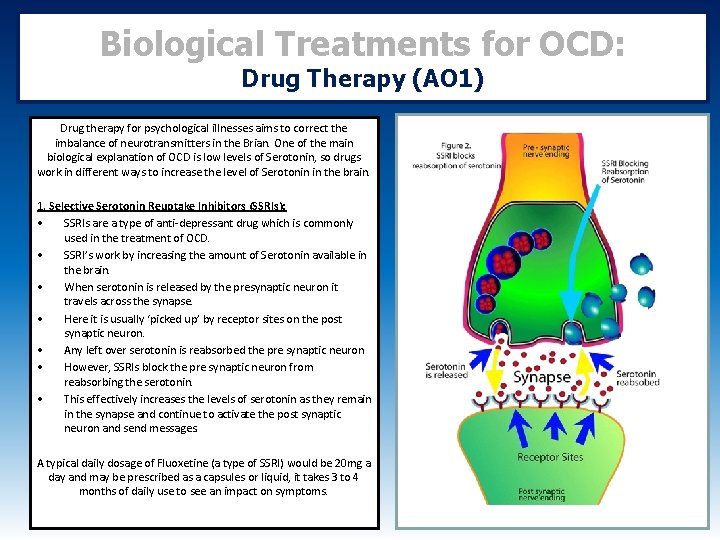
Biological Treatments for OCD: Drug Therapy (AO 1) Drug therapy for psychological illnesses aims to correct the imbalance of neurotransmitters in the Brian. One of the main biological explanation of OCD is low levels of Serotonin, so drugs work in different ways to increase the level of Serotonin in the brain. 1. Selective Serotonin Reuptake Inhibitors (SSRIs): • SSRIs are a type of anti-depressant drug which is commonly used in the treatment of OCD. • SSRI’s work by increasing the amount of Serotonin available in the brain. • When serotonin is released by the presynaptic neuron it travels across the synapse. • Here it is usually ‘picked up’ by receptor sites on the post synaptic neuron. • Any left over serotonin is reabsorbed the pre synaptic neuron • However, SSRIs block the pre synaptic neuron from reabsorbing the serotonin. • This effectively increases the levels of serotonin as they remain in the synapse and continue to activate the post synaptic neuron and send messages. A typical daily dosage of Fluoxetine (a type of SSRI) would be 20 mg a day and may be prescribed as a capsules or liquid, it takes 3 to 4 months of daily use to see an impact on symptoms.
Biological Treatments for OCD: Drug Therapy (AO 1) Where SSRIs are not effective, dosage of fluoxetine may be increased to 60 mg a day, or it may be combined with another drug. Sometimes different types of anti-depressant drugs are used, as people respond differently to different types of drug. Some alternative drug treatments are; • • • Tricyclics are older forms of anti-depressants such as clomipramine. These have been shown to work on OCD and have the same effects on neural pathways as SSRIs. However side effects of these drugs tend to be more severe. These drugs are used as a last resort once SSRIs have not worked. • • SNRIs (Serotonin Noradrenaline Reuptake Inhibitors) These drugs work on both serotonin and noradrenaline. They have the same action on Serotonin as Noradrenaline. They are newer drugs that are used as a second line of defence for OCD.
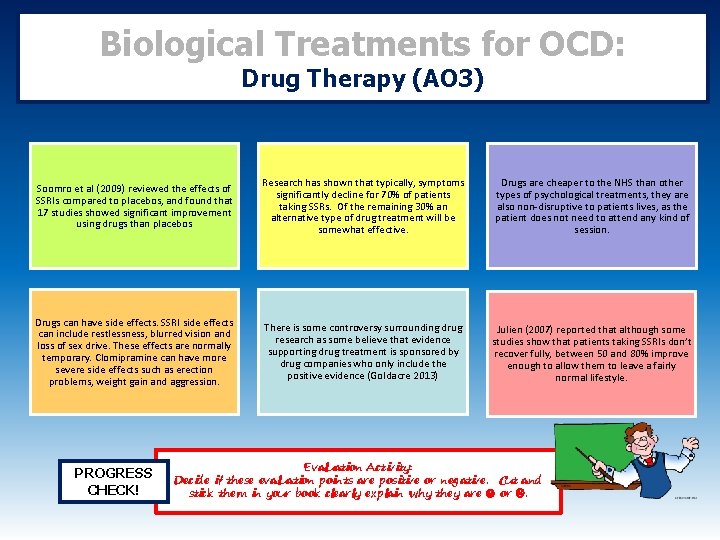
Biological Treatments for OCD: Drug Therapy (AO 3) Soomro et al (2009) reviewed the effects of SSRIs compared to placebos, and found that 17 studies showed significant improvement using drugs than placebos Research has shown that typically, symptoms significantly decline for 70% of patients taking SSRs. Of the remaining 30% an alternative type of drug treatment will be somewhat effective. Drugs are cheaper to the NHS than other types of psychological treatments, they are also non-disruptive to patients lives, as the patient does not need to attend any kind of session. Drugs can have side effects. SSRI side effects can include restlessness, blurred vision and loss of sex drive. These effects are normally temporary. Clomipramine can have more severe side effects such as erection problems, weight gain and aggression. There is some controversy surrounding drug research as some believe that evidence supporting drug treatment is sponsored by drug companies who only include the positive evidence (Goldacre 2013) Julien (2007) reported that although some studies show that patients taking SSRIs don’t recover fully, between 50 and 80% improve enough to allow them to leave a fairly normal lifestyle. PROGRESS CHECK! Evaluation Activity: Decide if these evaluation points are positive or negative. Cut and stick them in your book clearly explain why they are or .
 Schaffer and emerson stages of attachment
Schaffer and emerson stages of attachment Aqa a level psychology paper 1
Aqa a level psychology paper 1 Equity theory a level psychology
Equity theory a level psychology Aqa a level chemistry paper 1 2020
Aqa a level chemistry paper 1 2020 Aqa epq specification
Aqa epq specification Aqa english specification
Aqa english specification Aqa product design specification
Aqa product design specification Upper specification limit and lower specification limit
Upper specification limit and lower specification limit Natural variations operations management
Natural variations operations management Aqa english language paper 1
Aqa english language paper 1 Geography paper 1 case studies aqa
Geography paper 1 case studies aqa English language paper 2 transactional writing
English language paper 2 transactional writing Aqa english language paper 2 rail disasters mark scheme
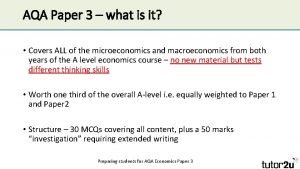
Aqa english language paper 2 rail disasters mark scheme Economics paper 3 aqa
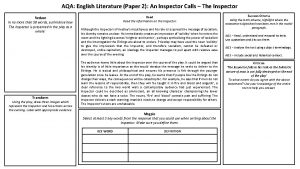
Economics paper 3 aqa English literature paper 1 inspector calls
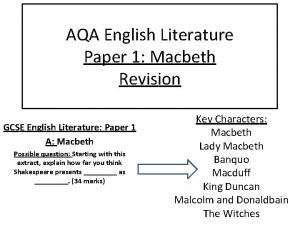
English literature paper 1 inspector calls English literature paper 1 macbeth and inspector calls
English literature paper 1 macbeth and inspector calls Aqa rpe past papers
Aqa rpe past papers Aqa history gcse papers
Aqa history gcse papers Sqi english structure
Sqi english structure Aqa english literature paper 1 2019 a christmas carol
Aqa english literature paper 1 2019 a christmas carol Biological paradigm of psychopathology
Biological paradigm of psychopathology Multipath model of psychopathology
Multipath model of psychopathology Multidimensional integrative approach to psychopathology
Multidimensional integrative approach to psychopathology What is psychopathology
What is psychopathology The supernatural tradition
The supernatural tradition Speech errors examples
Speech errors examples Psychopathology
Psychopathology Developmental psychopathology approach
Developmental psychopathology approach Multidimensional approach to psychopathology
Multidimensional approach to psychopathology Saira has a fear of cats
Saira has a fear of cats Gas exchange in fish a level biology aqa
Gas exchange in fish a level biology aqa Antonin artaud bbc bitesize
Antonin artaud bbc bitesize Aqa physics required practicals
Aqa physics required practicals Aqa a level physics data sheet
Aqa a level physics data sheet Social and political protest writing examples
Social and political protest writing examples Aqa a level art and design
Aqa a level art and design Art gcse aqa
Art gcse aqa Art and design a level aqa
Art and design a level aqa Aqa a level biology transition guide answers
Aqa a level biology transition guide answers Mid tudor crisis essay aqa
Mid tudor crisis essay aqa Wpfapp
Wpfapp Process specification in iot
Process specification in iot