Antioxidant Enzymes Activity in Gingiva and Gingival Crevicular












- Slides: 49
Antioxidant Enzymes Activity in Gingiva and Gingival Crevicular Fluid in Chronic Periodontitis Patients: Correlation with Some Potent Periodontopathogens Gamal Kenawy*, Abdul Fattah Amer**, Akram El awady**, Hisham Mahdy***, and Radi Massoud** * Medical Biochemistry, Riyadh Colleges of Dentistry and Pharmacy ** Oral Medicine and Periodontology, College of Dentistry, Al-Azhar University *** Microbiology, College of Medicine, Al-Azhar University
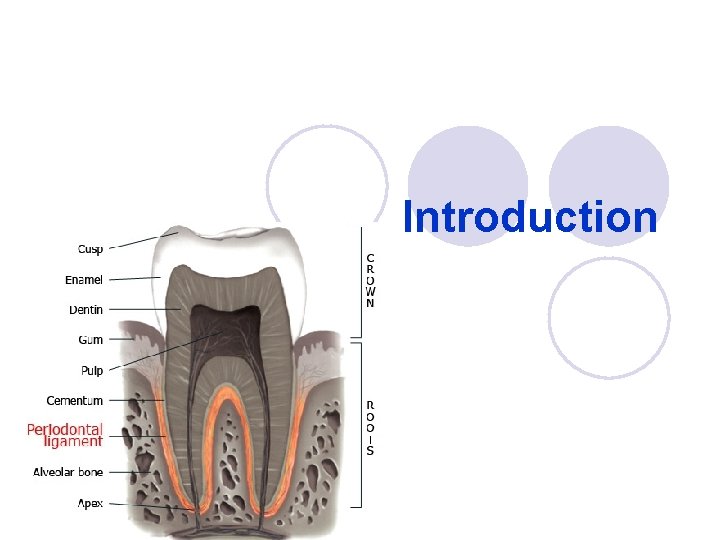
Introduction

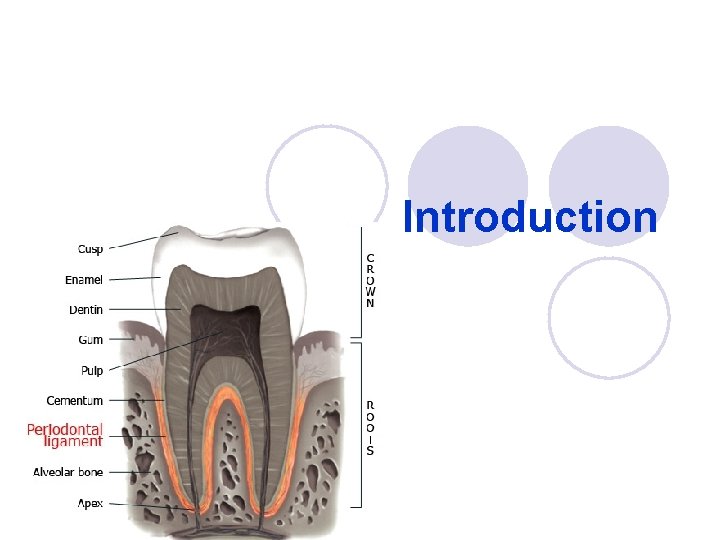
Periodontal Disease l Periodontal disease is a common chronic adult condition that, left untreated, can lead to tooth loss. l Chronic periodontitis results in inflammation within the supporting tissues of the teeth, progressive attachment and bone loss. This is the most frequently occurring form of periodontal disease.
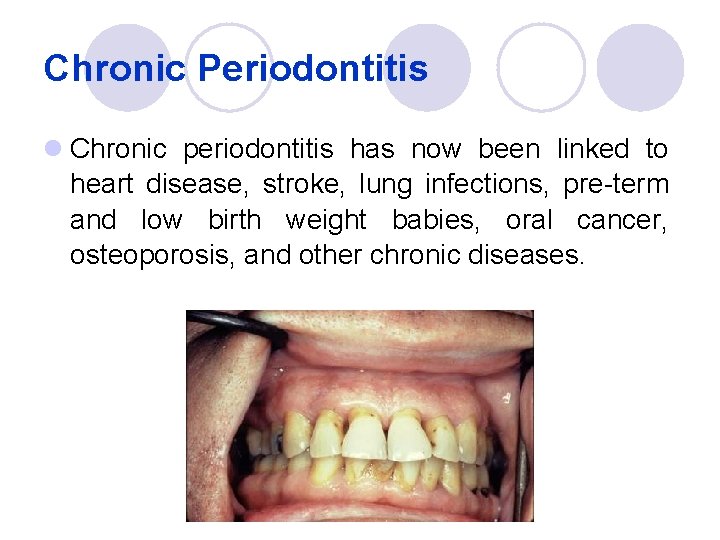
Chronic Periodontitis l Chronic periodontitis has now been linked to heart disease, stroke, lung infections, pre-term and low birth weight babies, oral cancer, osteoporosis, and other chronic diseases.

Chronic periodontitis l Causes ¡ Chronic gingivitis ¡ Occlusal trauma ¡ Improper application of orthodontic appliance (excess force) Pathology l Destruction of periodontal ligament l Formation of periodontal pocket l Resorption of alveolar bone l Loosening of teeth
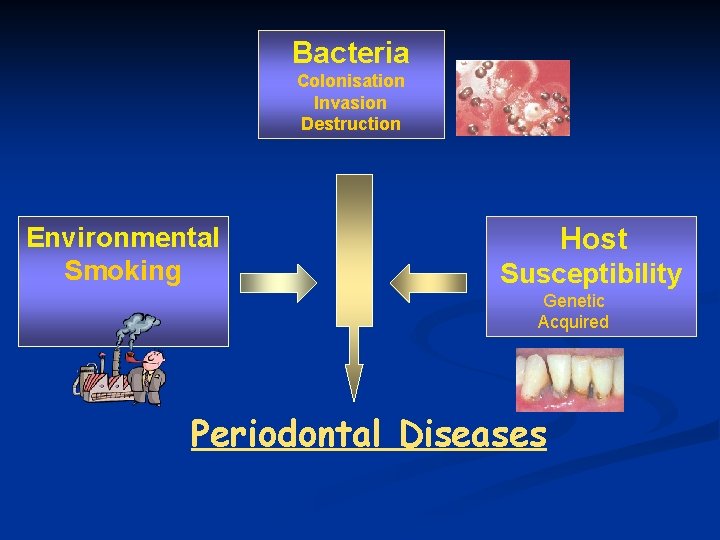
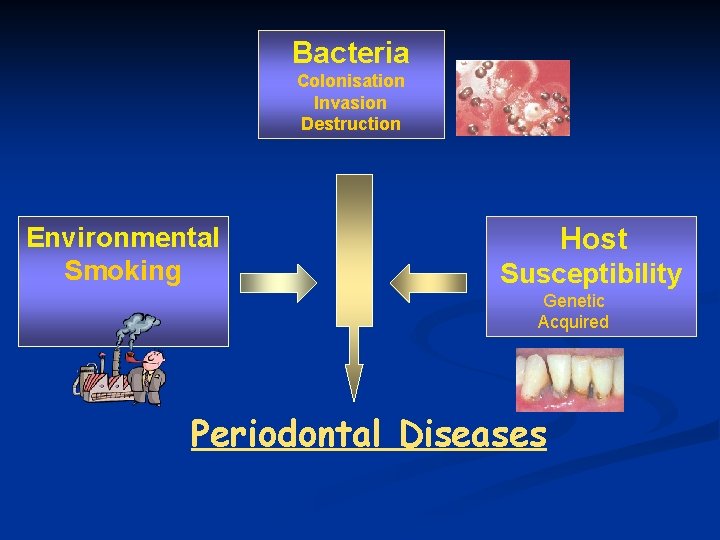
Bacteria Colonisation Invasion Destruction Environmental Smoking Host Susceptibility Genetic Acquired Periodontal Diseases
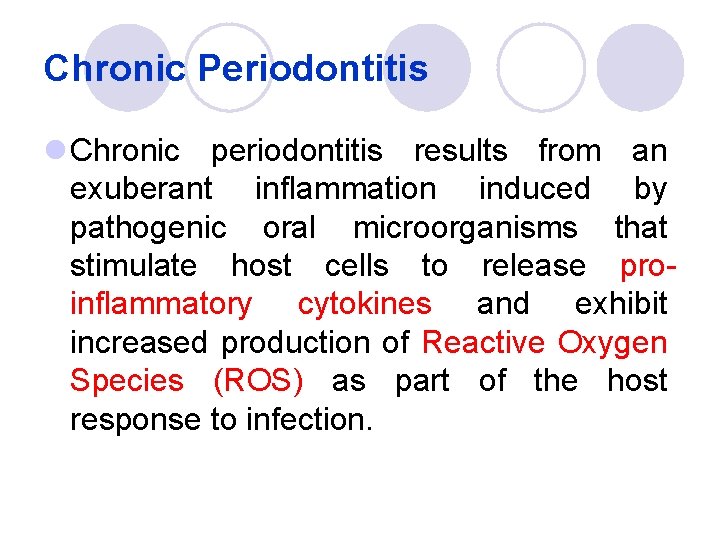
Chronic Periodontitis l Chronic periodontitis results from an exuberant inflammation induced by pathogenic oral microorganisms that stimulate host cells to release proinflammatory cytokines and exhibit increased production of Reactive Oxygen Species (ROS) as part of the host response to infection.

What are Reactive Oxygen Species (ROS)? • ROS are highly reactive oxidizing agents include: a. Oxygen derived free radicals (e. g. Superoxide anion O 2. -) b. Oxygen-derived non radical species (e. g. H 2 O 2) • ROS are potentially harmful to cells, causing oxidation of lipids, proteins and DNA.

ROS and Chronic Periodontitis l It has been suggested that ROS are capable of inducing periodontal tissue destruction and are associated with osteoclastic bone resorption, commonly associated with periodontitis.
External Sources of ROS • Cigarette smoke • Environmental pollutants • Radiations • Ultraviolet radiations • Ozone • Certain drugs • Pesticides • Anesthetics Smoking 10 Quad Trillion free radicals per cigarette!
Internal Sources of ROS • • • Mitochondria Inflammation Phagocytes Xanthine oxidase Arachidonate pathways Ischemia/Reperfusion
Antioxidants l Antioxidants neutralize ROS in body tissues. l Antioxidant compounds include: l Ascorbic acid (vitamin C) l α-Tocopherol (vitamin E) l Glutathione l Lipoic acid l Uric acid l Carotenes

Antioxidant Sources A diet rich in FRUITS and VEGETABLES And Nutritional Supplements
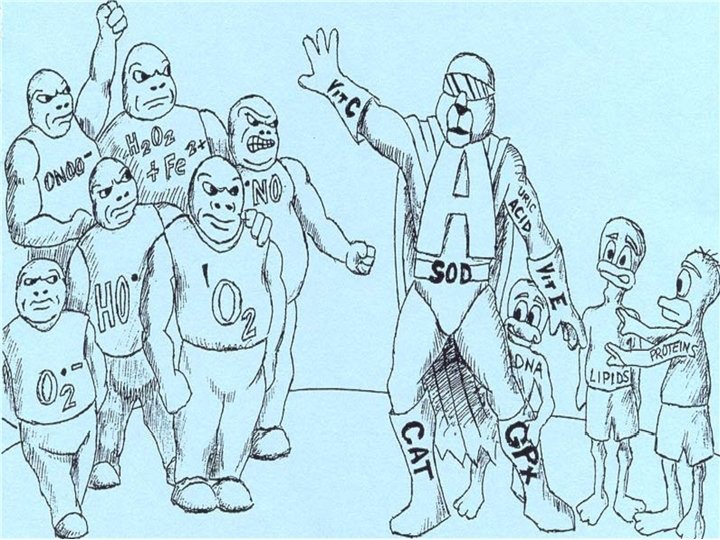
Antioxidant Enzymes l Antioxidant enzymes, including Superoxide Dismutase (SOD), Catalase (CAT), and Glutathione Peroxidase (GPx) are naturally produced enzymes that have evolved for cellular protection against oxidative stress and ROS. l They detoxify ROS to harmless substances such as water and ordinary oxygen.

The Constant Battle ROS are toxins that cause cell and DNA damage Antioxidants combat ROS to prevent cell damage and maintain health
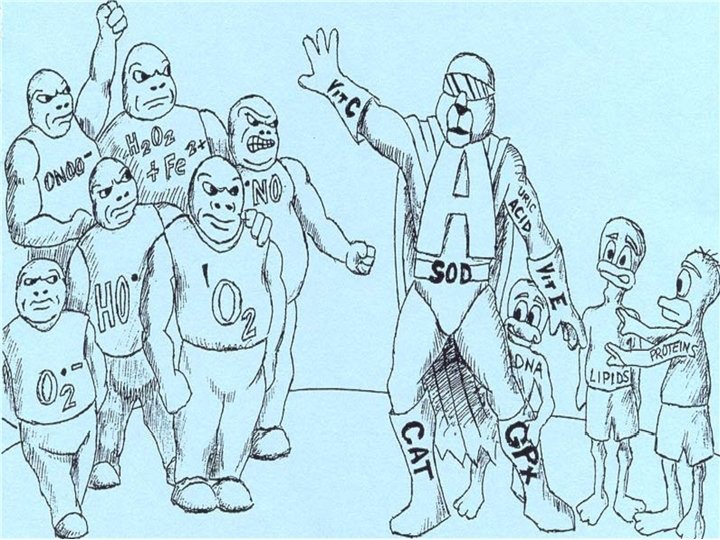
ROS vs. Antioxidants l In health, the balance is maintained among ROS and antioxidants while under pathological conditions, the balance may be tilted towards the oxidative stress with increase in ROS levels.
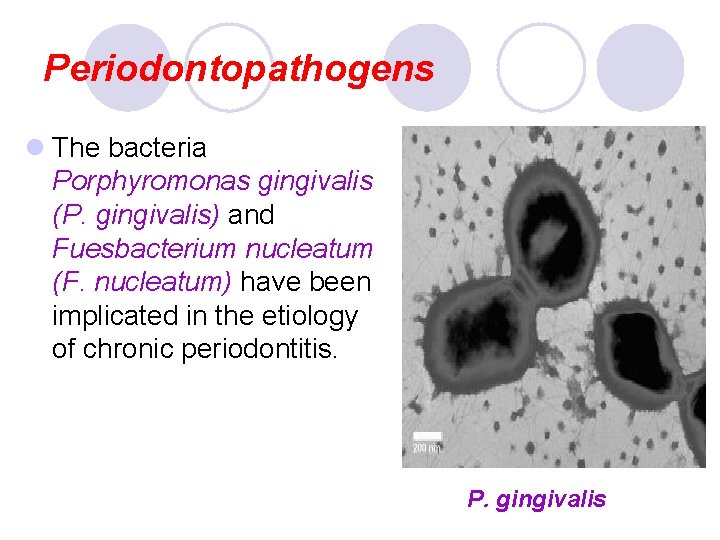
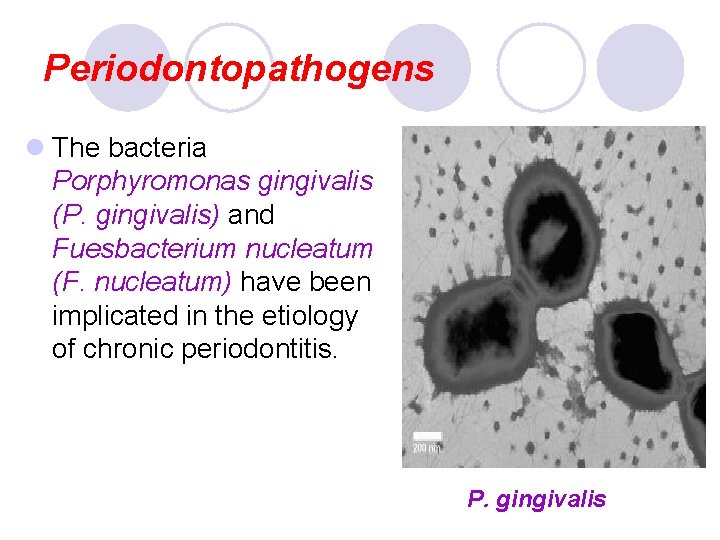
Periodontopathogens l The bacteria Porphyromonas gingivalis (P. gingivalis) and Fuesbacterium nucleatum (F. nucleatum) have been implicated in the etiology of chronic periodontitis. P. gingivalis
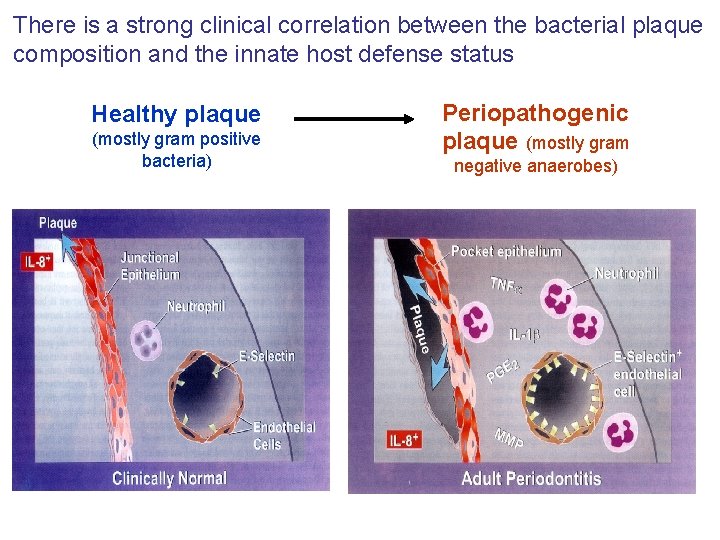
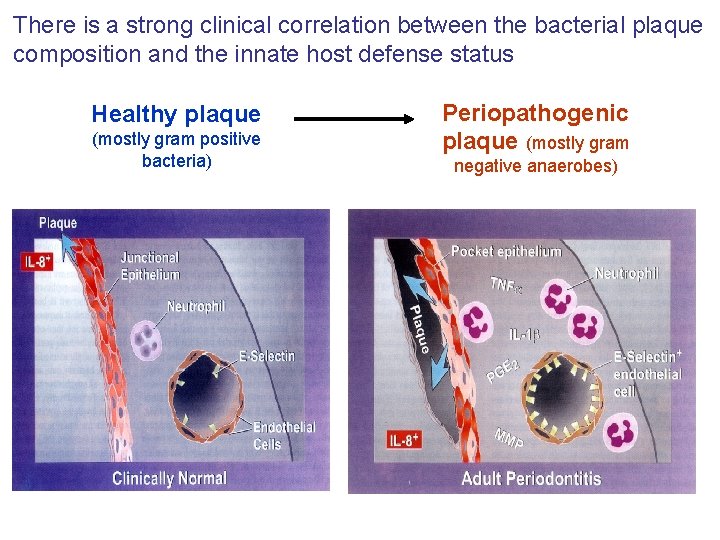
There is a strong clinical correlation between the bacterial plaque composition and the innate host defense status Healthy plaque (mostly gram positive bacteria) Periopathogenic plaque (mostly gram negative anaerobes)
Aim of Work
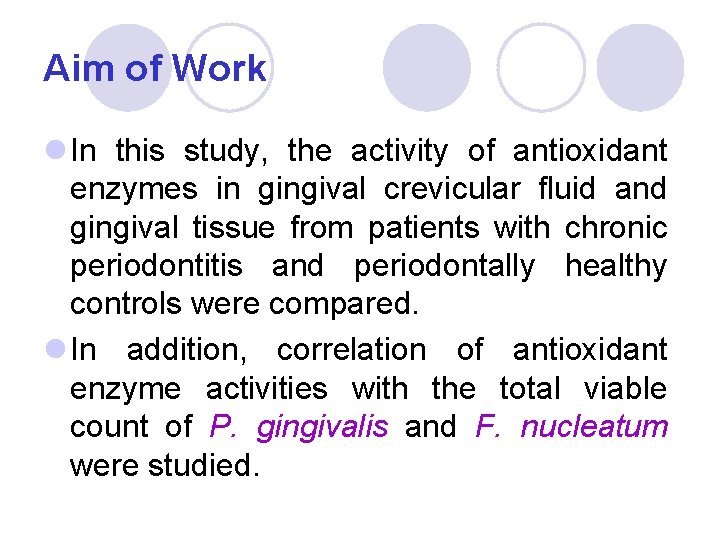
Aim of Work l In this study, the activity of antioxidant enzymes in gingival crevicular fluid and gingival tissue from patients with chronic periodontitis and periodontally healthy controls were compared. l In addition, correlation of antioxidant enzyme activities with the total viable count of P. gingivalis and F. nucleatum were studied.
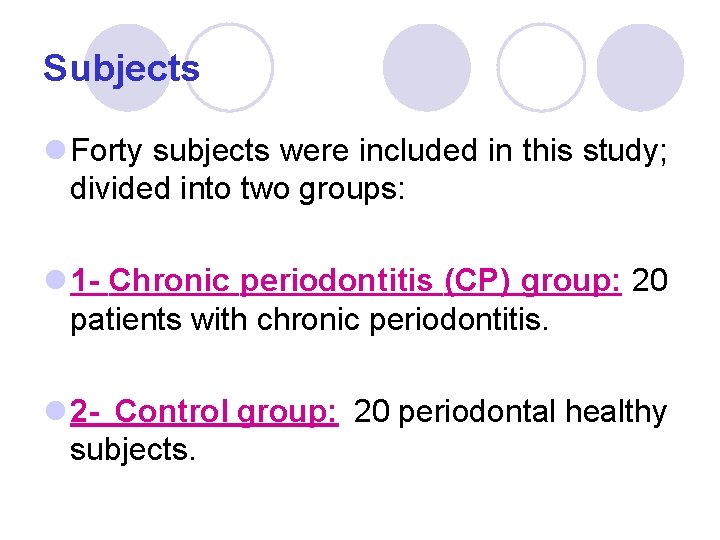
Subjects l Forty subjects were included in this study; divided into two groups: l 1 - Chronic periodontitis (CP) group: 20 patients with chronic periodontitis. l 2 - Control group: 20 periodontal healthy subjects.
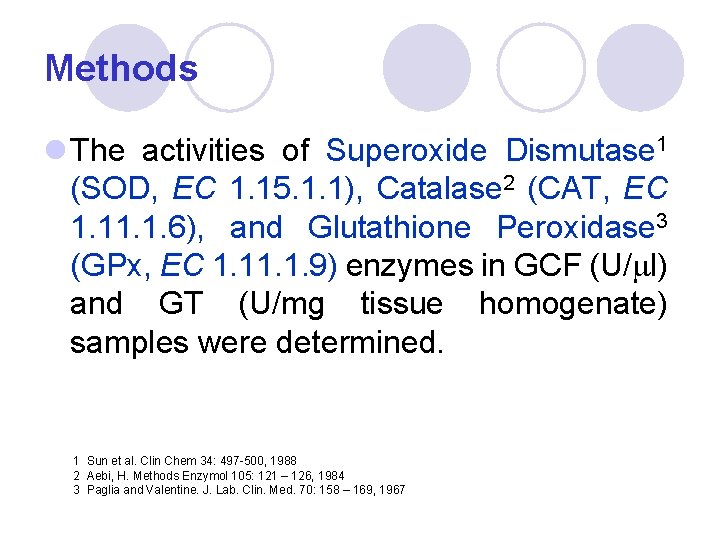
Methods l The activities of Superoxide Dismutase 1 (SOD, EC 1. 15. 1. 1), Catalase 2 (CAT, EC 1. 1. 6), and Glutathione Peroxidase 3 (GPx, EC 1. 1. 9) enzymes in GCF (U/ml) and GT (U/mg tissue homogenate) samples were determined. 1 Sun et al. Clin Chem 34: 497 -500, 1988 2 Aebi, H. Methods Enzymol 105: 121 – 126, 1984 3 Paglia and Valentine. J. Lab. Clin. Med. 70: 158 – 169, 1967
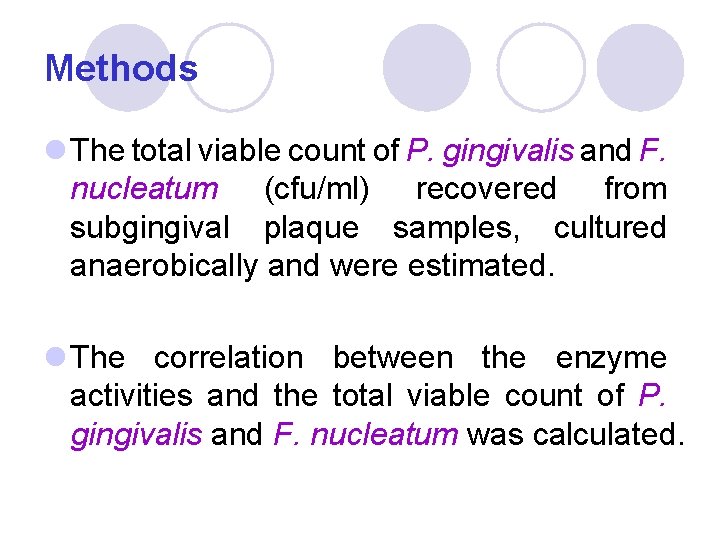
Methods l The total viable count of P. gingivalis and F. nucleatum (cfu/ml) recovered from subgingival plaque samples, cultured anaerobically and were estimated. l The correlation between the enzyme activities and the total viable count of P. gingivalis and F. nucleatum was calculated.
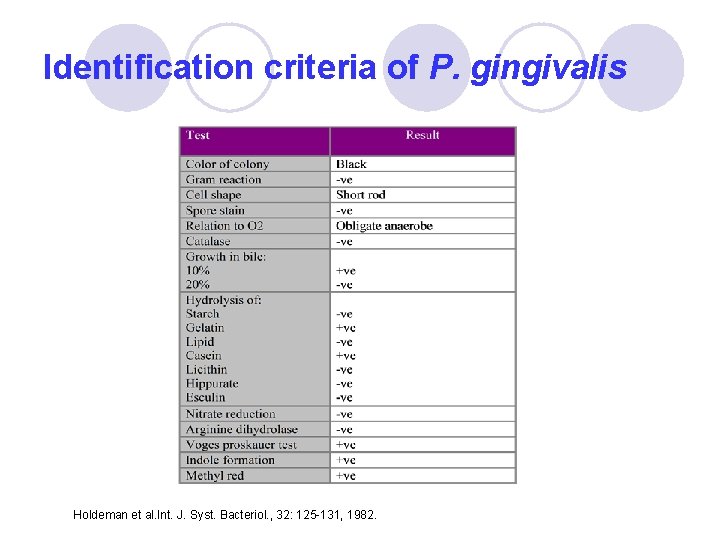
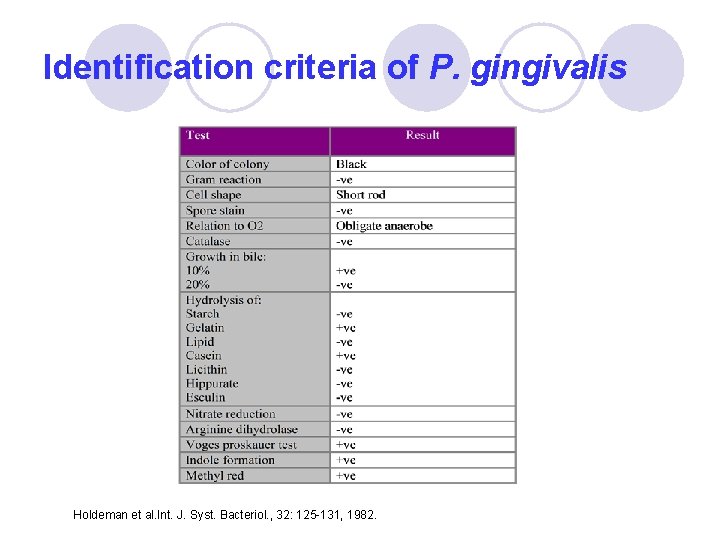
Identification criteria of P. gingivalis Holdeman et al. Int. J. Syst. Bacteriol. , 32: 125 -131, 1982.

P. gingivalis Agar (P. GING)
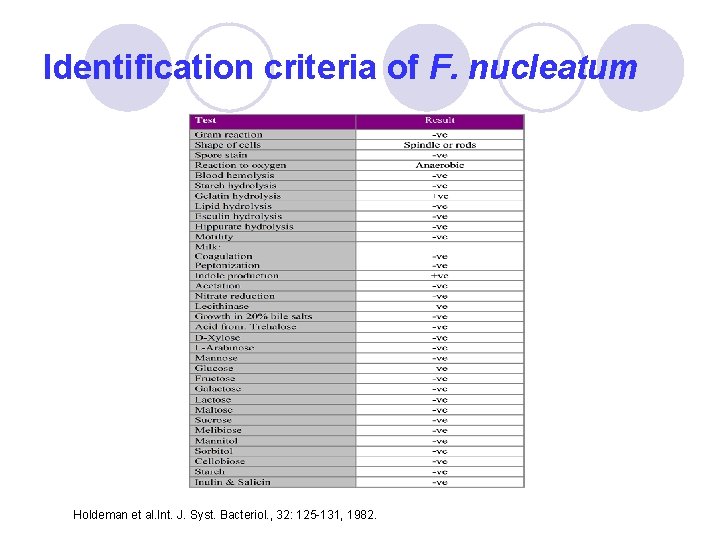
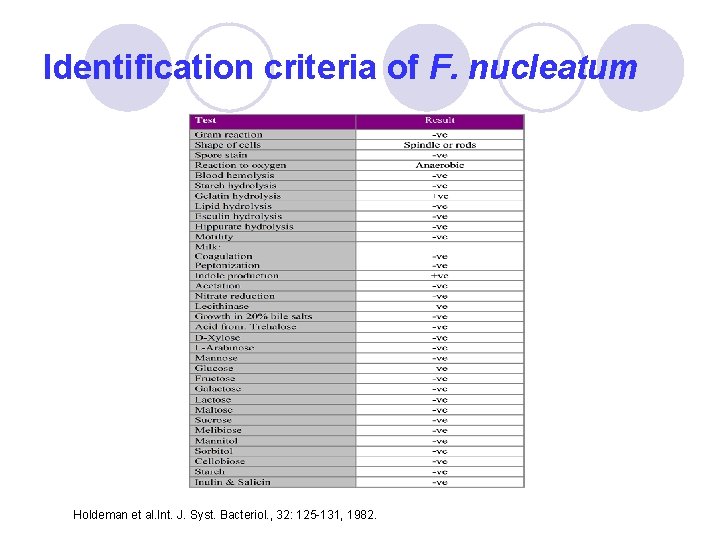
Identification criteria of F. nucleatum Holdeman et al. Int. J. Syst. Bacteriol. , 32: 125 -131, 1982.
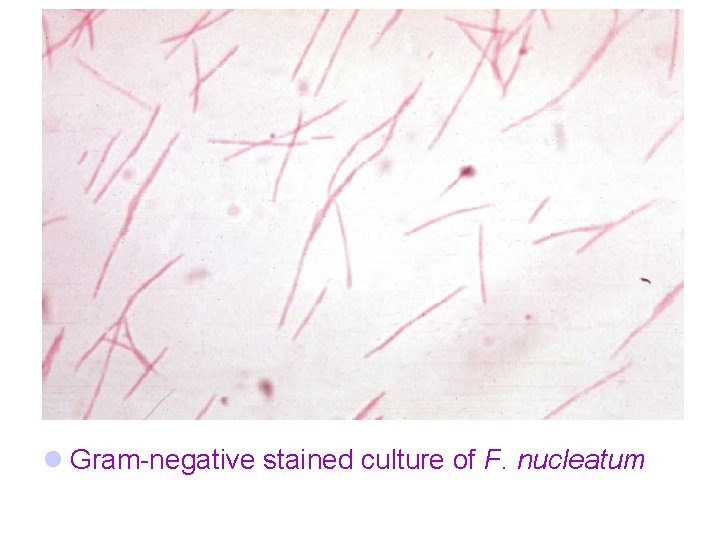
l Gram-negative stained culture of F. nucleatum

RESULTS
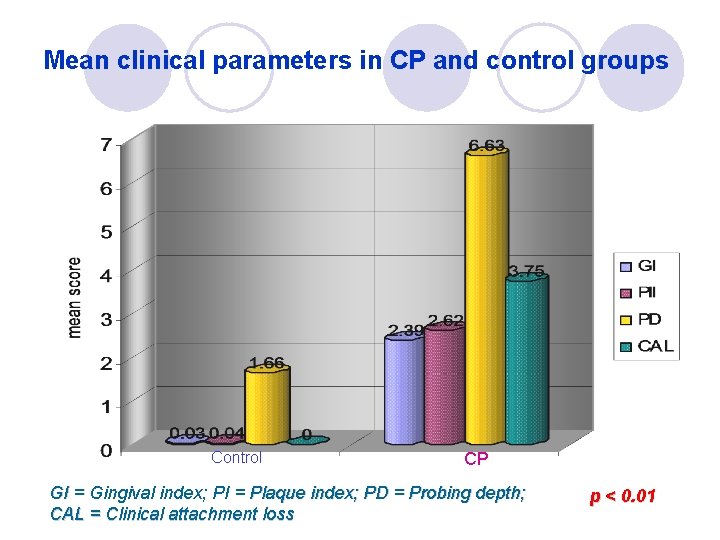
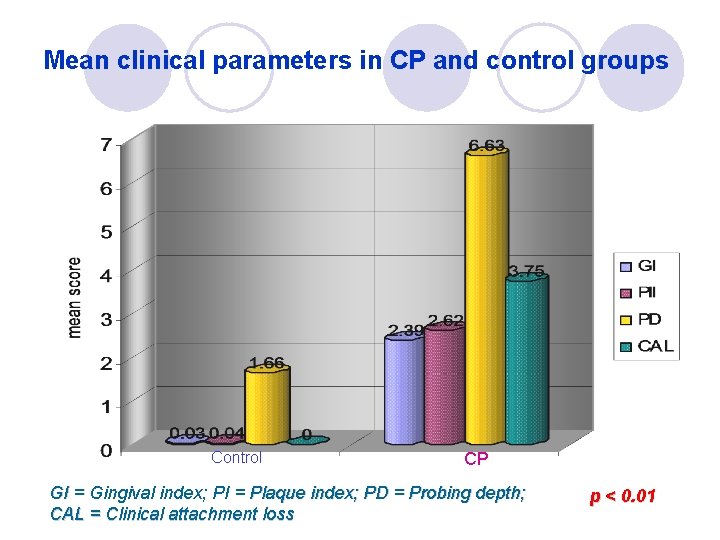
Mean clinical parameters in CP and control groups Control CP GI = Gingival index; PI = Plaque index; PD = Probing depth; CAL = Clinical attachment loss p < 0. 01
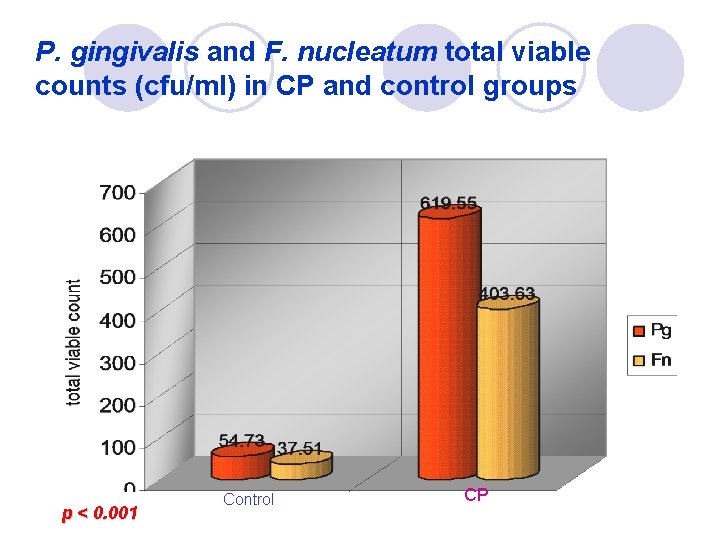
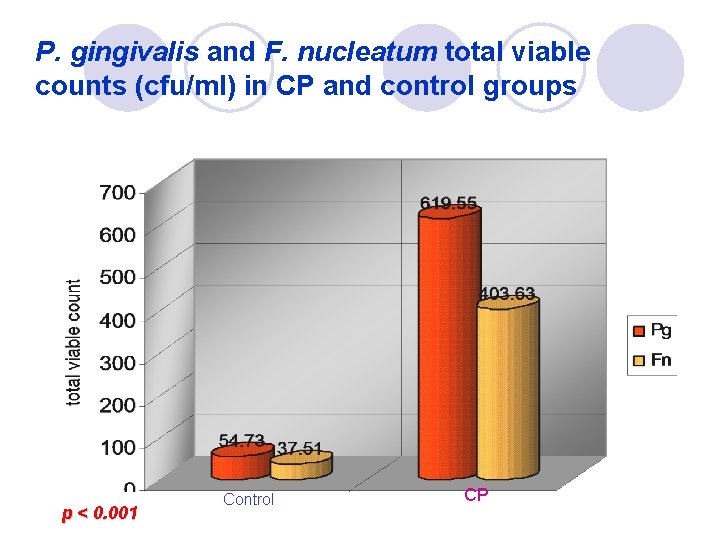
P. gingivalis and F. nucleatum total viable counts (cfu/ml) in CP and control groups p < 0. 001 Control CP
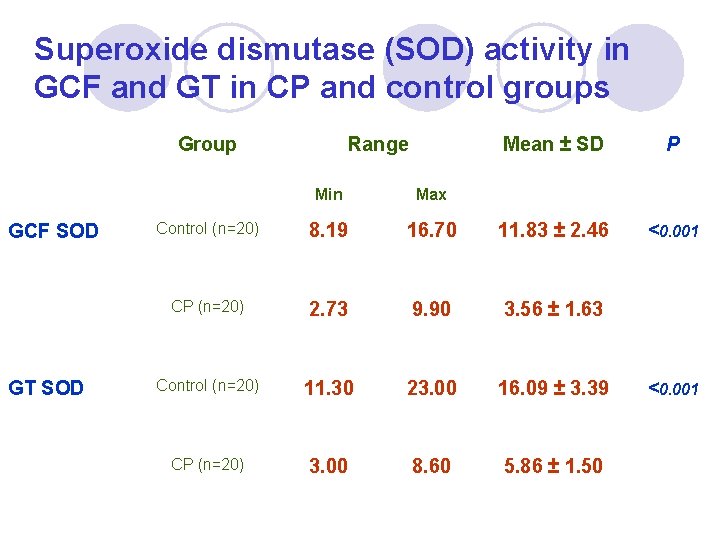
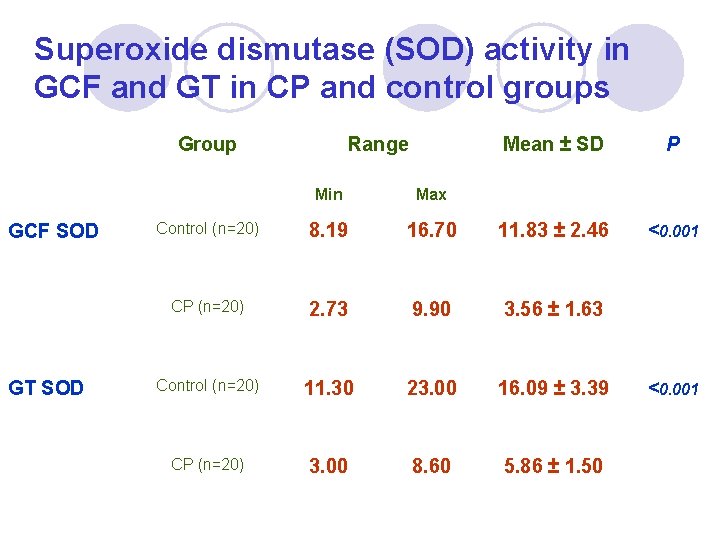
Superoxide dismutase (SOD) activity in GCF and GT in CP and control groups Group GCF SOD GT SOD Range Mean ± SD P <0. 001 Min Max Control (n=20) 8. 19 16. 70 11. 83 ± 2. 46 CP (n=20) 2. 73 9. 90 3. 56 ± 1. 63 Control (n=20) 11. 30 23. 00 16. 09 ± 3. 39 CP (n=20) 3. 00 8. 60 5. 86 ± 1. 50 <0. 001
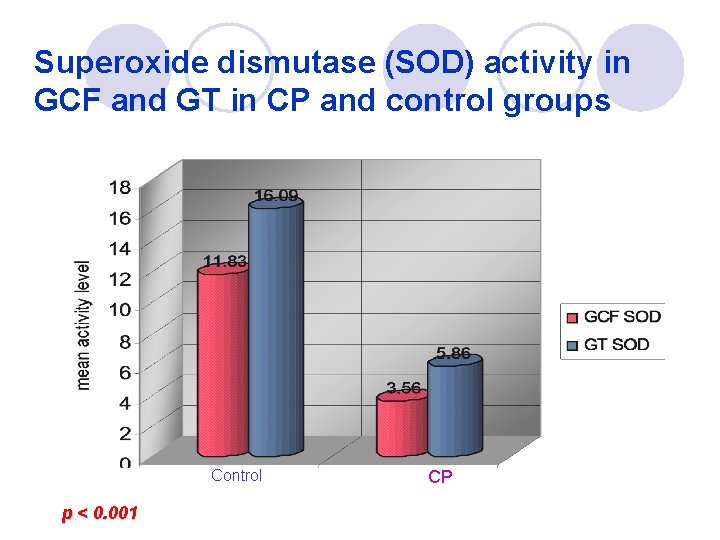
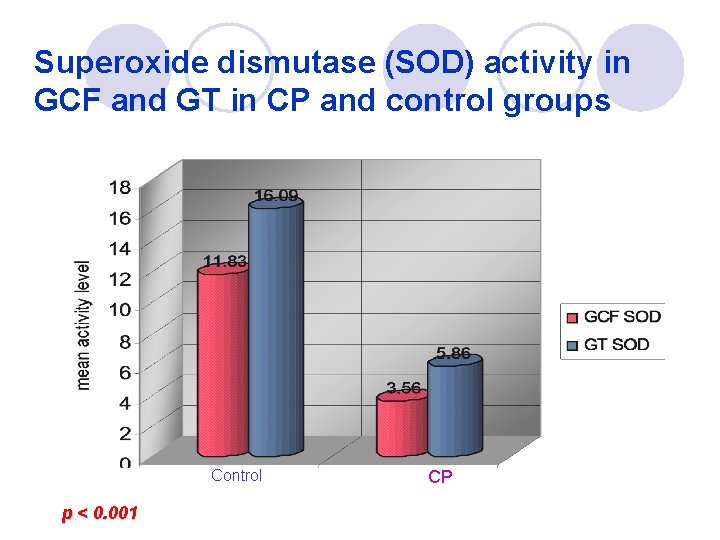
Superoxide dismutase (SOD) activity in GCF and GT in CP and control groups Control p < 0. 001 CP
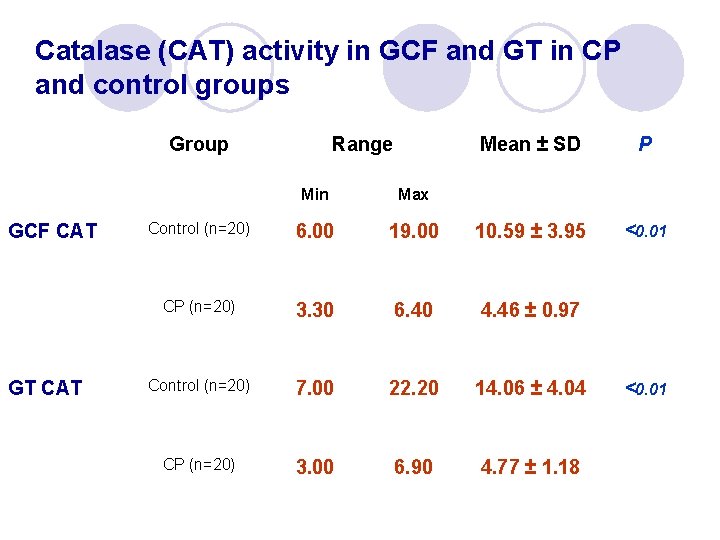
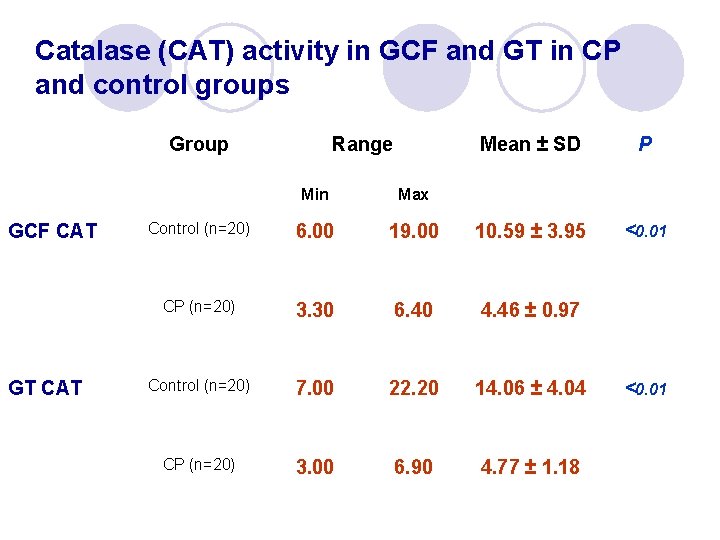
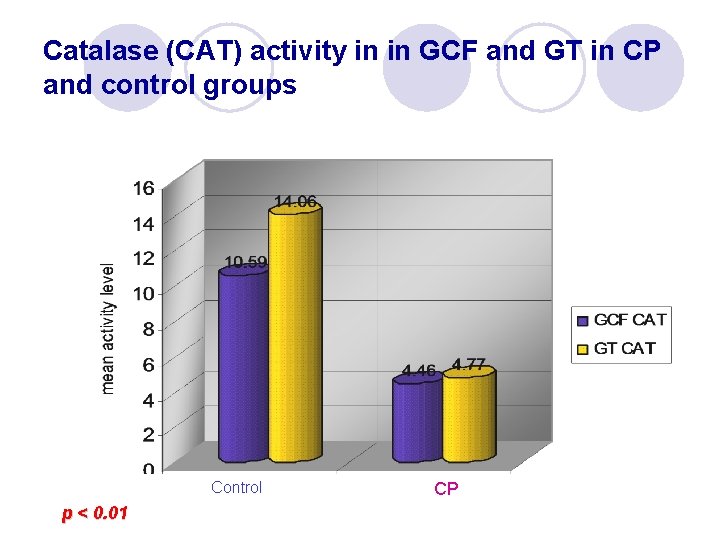
Catalase (CAT) activity in GCF and GT in CP and control groups Group GCF CAT GT CAT Range Mean ± SD P <0. 01 Min Max Control (n=20) 6. 00 19. 00 10. 59 ± 3. 95 CP (n=20) 3. 30 6. 40 4. 46 ± 0. 97 Control (n=20) 7. 00 22. 20 14. 06 ± 4. 04 CP (n=20) 3. 00 6. 90 4. 77 ± 1. 18 <0. 01
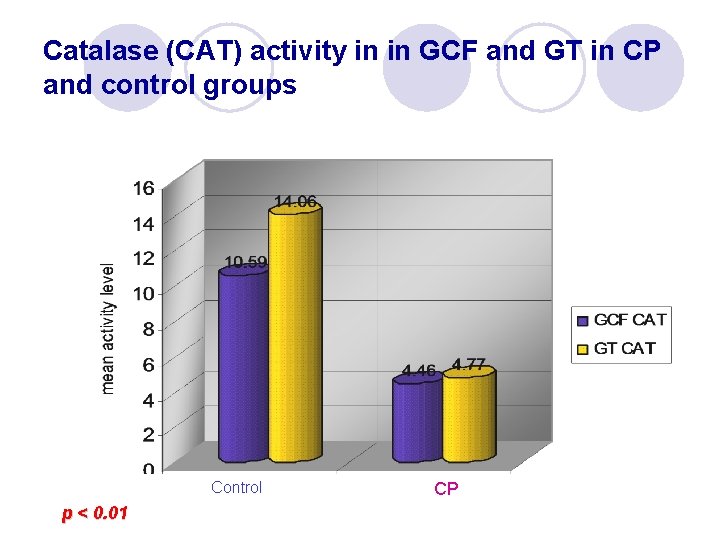
Catalase (CAT) activity in in GCF and GT in CP and control groups Control p < 0. 01 CP
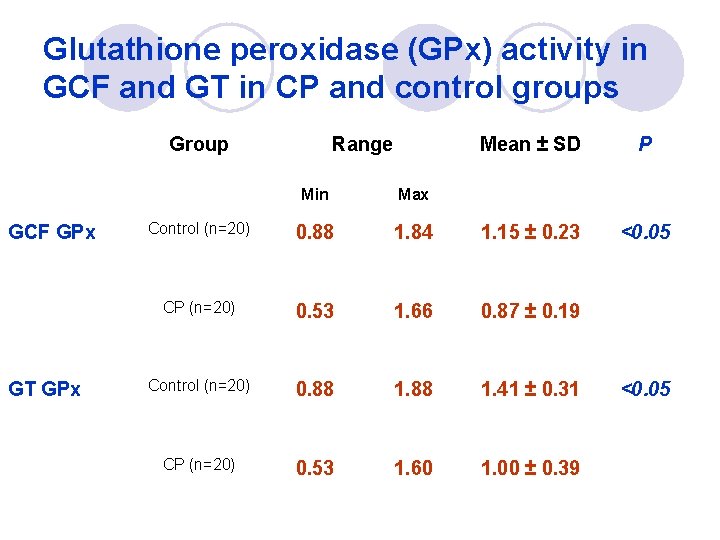
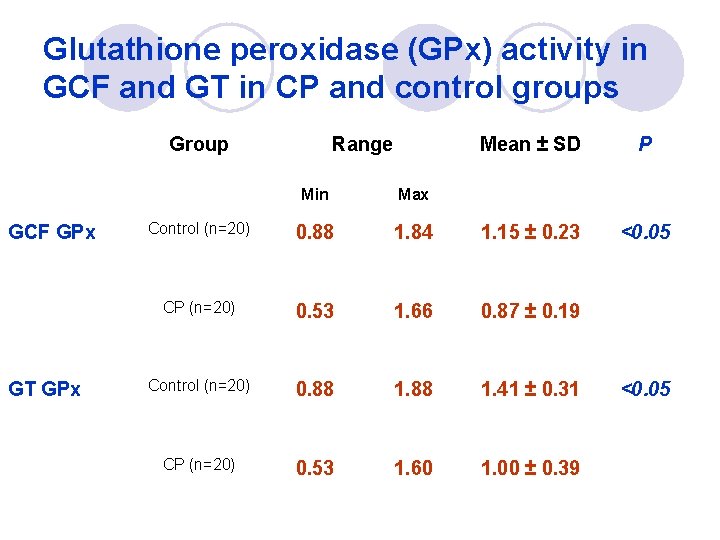
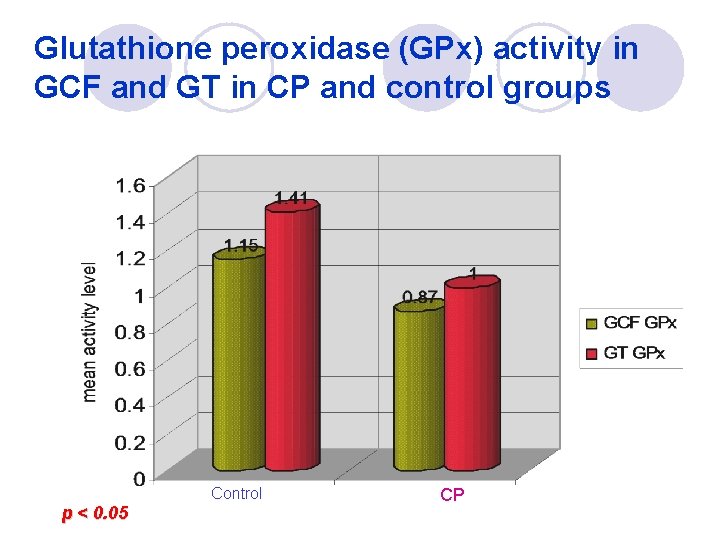
Glutathione peroxidase (GPx) activity in GCF and GT in CP and control groups Group GCF GPx GT GPx Range Mean ± SD P <0. 05 Min Max Control (n=20) 0. 88 1. 84 1. 15 ± 0. 23 CP (n=20) 0. 53 1. 66 0. 87 ± 0. 19 Control (n=20) 0. 88 1. 41 ± 0. 31 CP (n=20) 0. 53 1. 60 1. 00 ± 0. 39 <0. 05
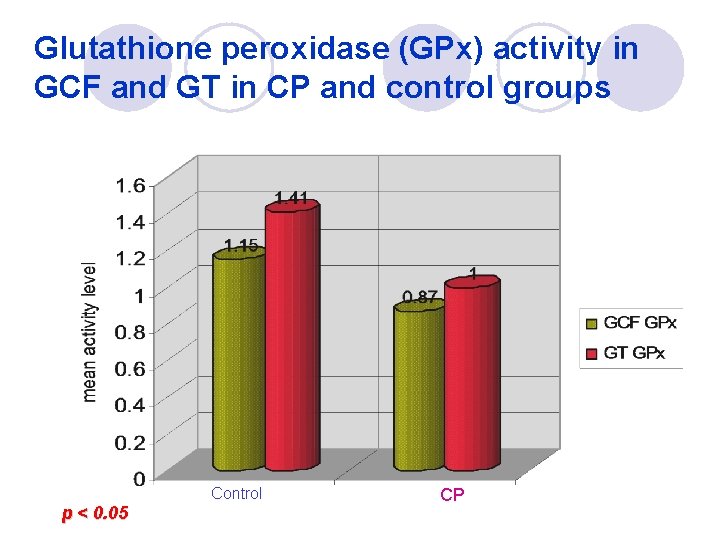
Glutathione peroxidase (GPx) activity in GCF and GT in CP and control groups Control p < 0. 05 CP

Pearson’s correlation coefficient between clinical parameters and periodontal pathogens P. gingivalis F. nucleatum Gingival Index (GI) 0. 738* 0. 757* Plaque Index (PI) 0. 703* 0. 779* Probing Depth (PD) 0. 751* 0. 818* Clinical Attachment Loss (CAL) 0. 638* 0. 795* ** significant * p < 0. 01 Correlation at p< 0. 01
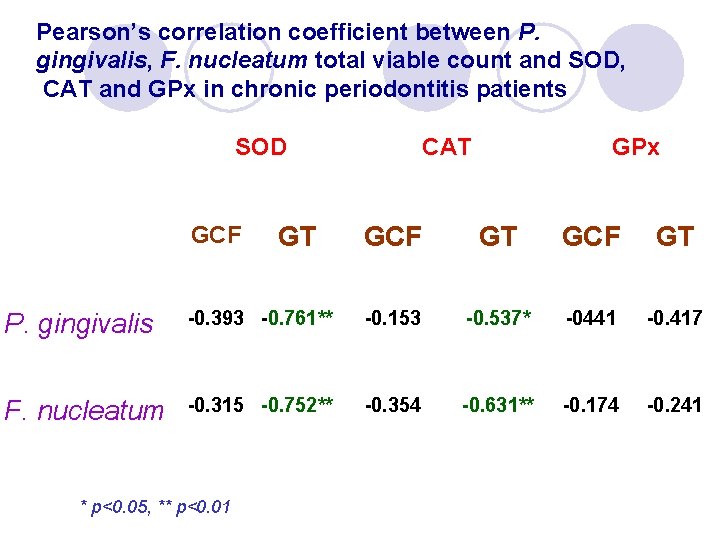
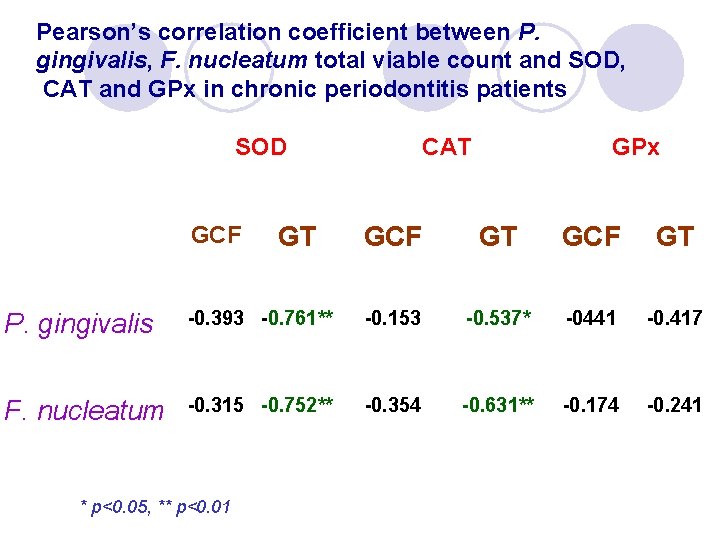
Pearson’s correlation coefficient between P. gingivalis, F. nucleatum total viable count and SOD, CAT and GPx in chronic periodontitis patients SOD GCF GT CAT GPx GCF GT P. gingivalis -0. 393 -0. 761** -0. 153 -0. 537* -0441 -0. 417 F. nucleatum -0. 315 -0. 752** -0. 354 -0. 631** -0. 174 -0. 241 * p< 0. 05 , ** p<0. 05, ** 0. 01 p<0. 01

Correlation of GT SOD with P. gingivalis total viable count in chronic periodontitis patients l r = -0. 761, p<0. 01
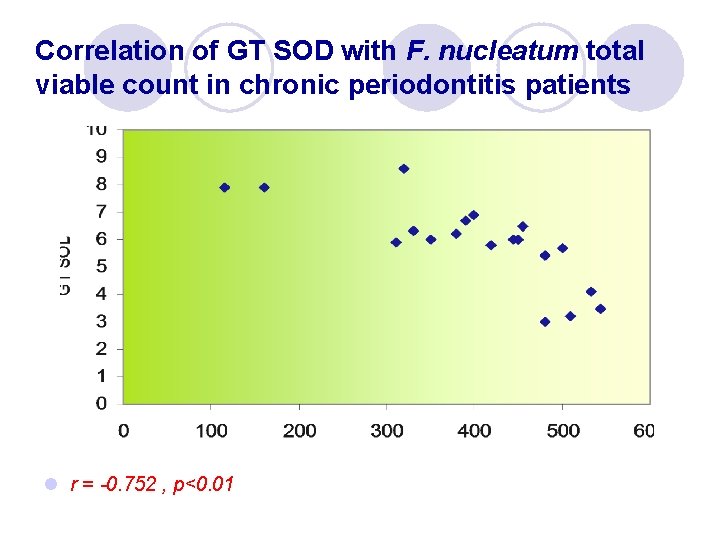
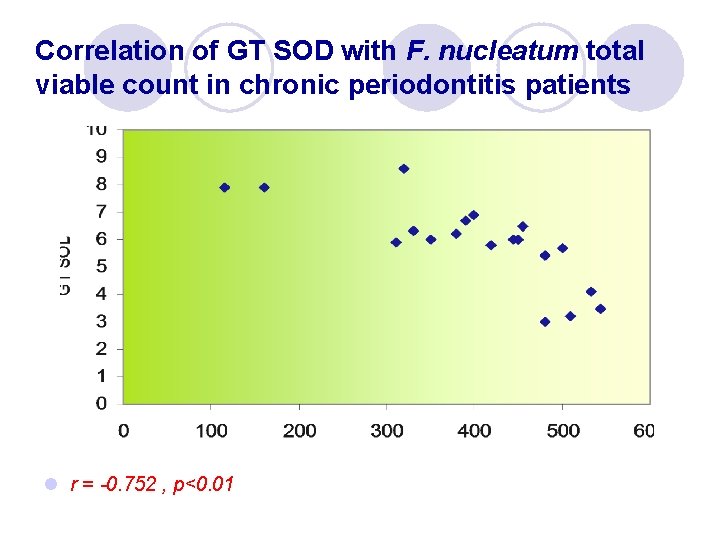
Correlation of GT SOD with F. nucleatum total viable count in chronic periodontitis patients l r = -0. 752 , p<0. 01
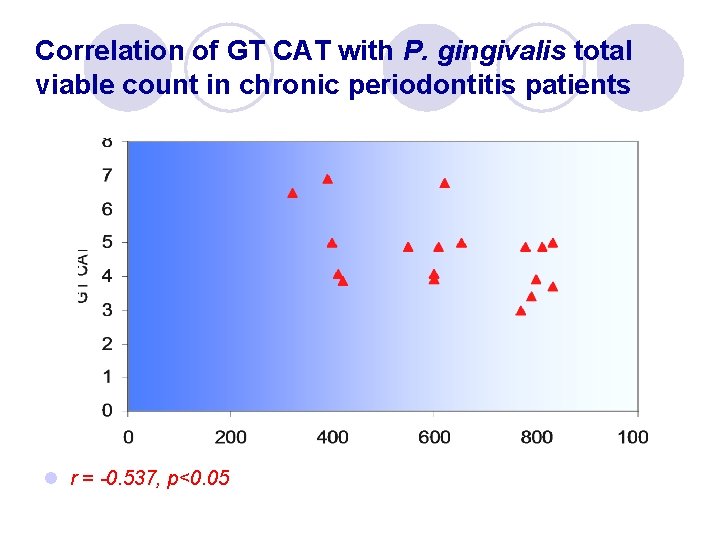
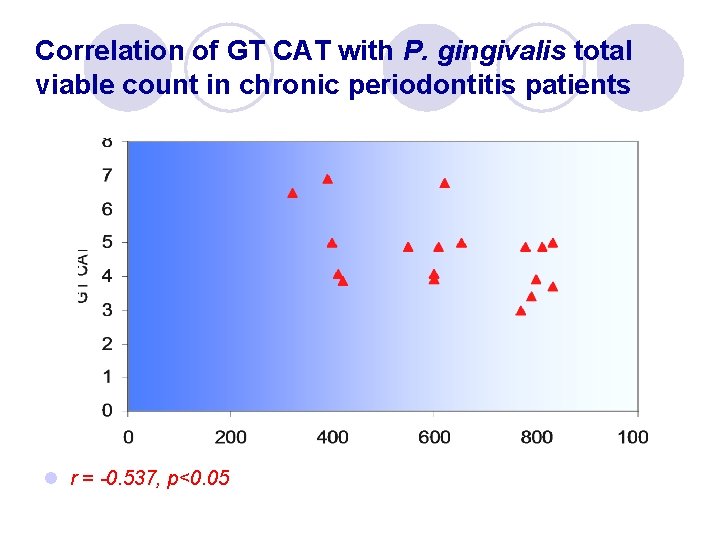
Correlation of GT CAT with P. gingivalis total viable count in chronic periodontitis patients l r = -0. 537, p<0. 05
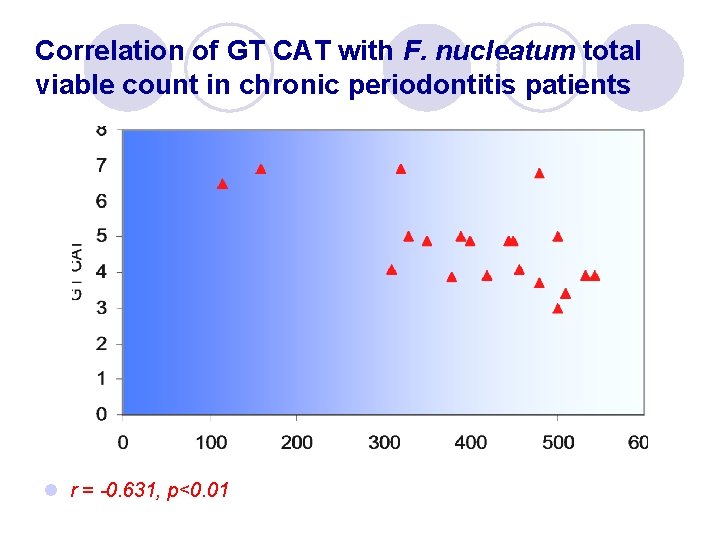
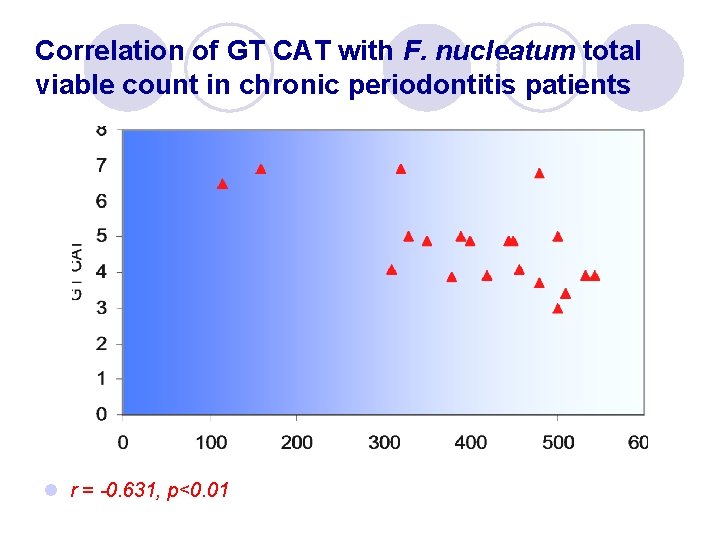
Correlation of GT CAT with F. nucleatum total viable count in chronic periodontitis patients l r = -0. 631, p<0. 01
Conclusion

Conclusion l The lower activities of antioxidant enzymes in the GCF and GT in chronic periodontitis patients can participate directly and indirectly in tissue destruction that coincident to periodontal disease and, probably may have an inference in treatment modalities of periodontal disease.
Conclusion l P. gingivalis and F. nucleatum could be implicated as true pathogens in predisposition of chronic periodontitis. l These peridontopathogens may have a role in suppression of antioxidant enzymes synthesis or decreasing their activities.
Conclusion l The negative correlation between total viable count of P. gingivalis and F. nucleatum with the antioxidant enzyme activities in chronic periodontitis patients may be applied as diagnostic and/or prognostic periodontal tool.
Conclusion l The findings of the present study may provide opportunities to develop a novel antioxidant therapy that function not only as antioxidants in the traditional sense but, also, act as antiinflammatory agent to overcome the unwanted effects of the inflammatory process upon periodontal tissues.

Thank you for your attention
 Inverse bevel incision
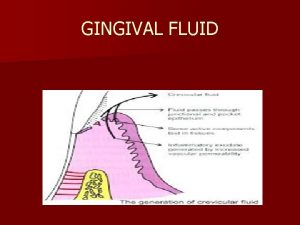
Inverse bevel incision Crevicular fluid
Crevicular fluid Antioxidant classification
Antioxidant classification Antioxidant system
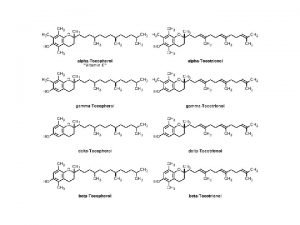
Antioxidant system Antioxidant chemical structure
Antioxidant chemical structure Antioxidant free radical
Antioxidant free radical Vitamin e as antioxidant
Vitamin e as antioxidant Antioxidant means
Antioxidant means Antioxidant graphite electrode
Antioxidant graphite electrode Modified stillman technique
Modified stillman technique Life preserver shape of gingiva
Life preserver shape of gingiva Resilient gingiva meaning
Resilient gingiva meaning кератолинин
кератолинин Flaccid gingiva
Flaccid gingiva Gingiva
Gingiva Tooth development
Tooth development Gingival lifler
Gingival lifler Sinus tract adalah
Sinus tract adalah Gingival diseases
Gingival diseases Contour of gingiva in gingivitis
Contour of gingiva in gingivitis Gingiva
Gingiva Gingival sulcus
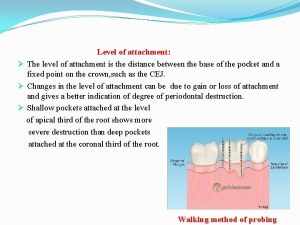
Gingival sulcus Biologic width definition
Biologic width definition Gingival curettage indications
Gingival curettage indications Pristine gingiva
Pristine gingiva Calculus teeth
Calculus teeth Gingival index
Gingival index Activity corrections
Activity corrections Microtopography of gingival wall
Microtopography of gingival wall Periodontal case study
Periodontal case study How to identify mesial and distal gmt
How to identify mesial and distal gmt Anoxemia gingival
Anoxemia gingival Type of clasp in rpd
Type of clasp in rpd Bevel in class 3 composite
Bevel in class 3 composite Forward and backward caries definition
Forward and backward caries definition Blacks classification
Blacks classification Petele koplik
Petele koplik Bevel definition in dentistry
Bevel definition in dentistry Dientes de ramfjord
Dientes de ramfjord Gingival index
Gingival index Cutit bisturiu gingival
Cutit bisturiu gingival Axial wall
Axial wall Afta juventus
Afta juventus Circlet clasp
Circlet clasp Gingival hyperplasia
Gingival hyperplasia Gingival sulcus
Gingival sulcus Birleşim epiteli
Birleşim epiteli Dual arch impression technique
Dual arch impression technique Lizereu gingival burton
Lizereu gingival burton Rpi direct retainer
Rpi direct retainer