ANTENATAL HYDRONEPHROSIS HASAN FARSI 1 What would you



- Slides: 40
ANTENATAL HYDRONEPHROSIS HASAN FARSI 1
What would you do if you have: n n n 32 -week fetus with normal amniotic fluid and suspected ureteropelvic junction. 36 -week fetus with suspected posterior urethral valves without oligohydramnios. 23 -week fetus with suspected PUV and oligohydramnios with bladder electrolytes suggestive of good renal function. 2
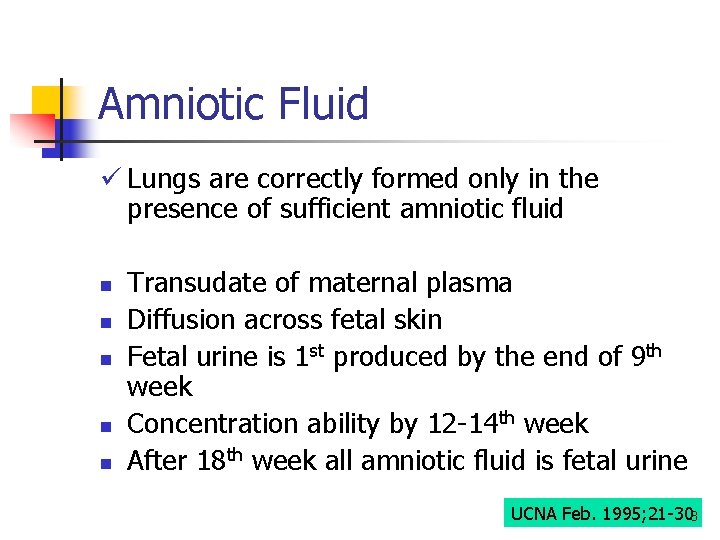
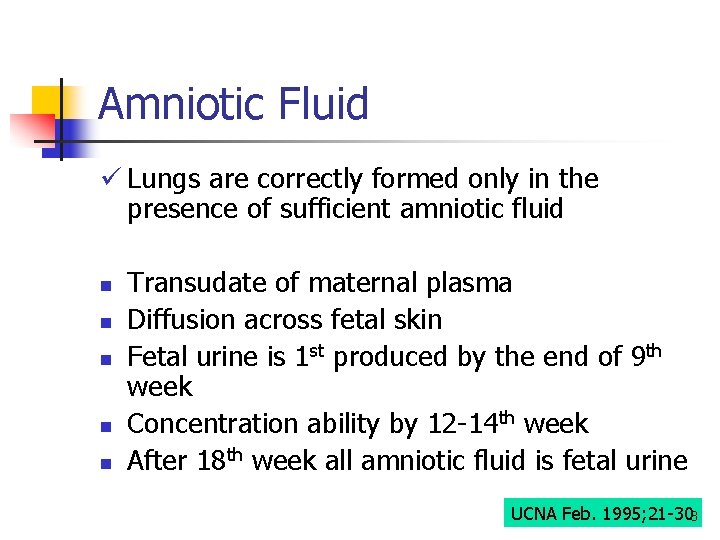
Amniotic Fluid ü Lungs are correctly formed only in the presence of sufficient amniotic fluid n n n Transudate of maternal plasma Diffusion across fetal skin Fetal urine is 1 st produced by the end of 9 th week Concentration ability by 12 -14 th week After 18 th week all amniotic fluid is fetal urine UCNA Feb. 1995; 21 -303
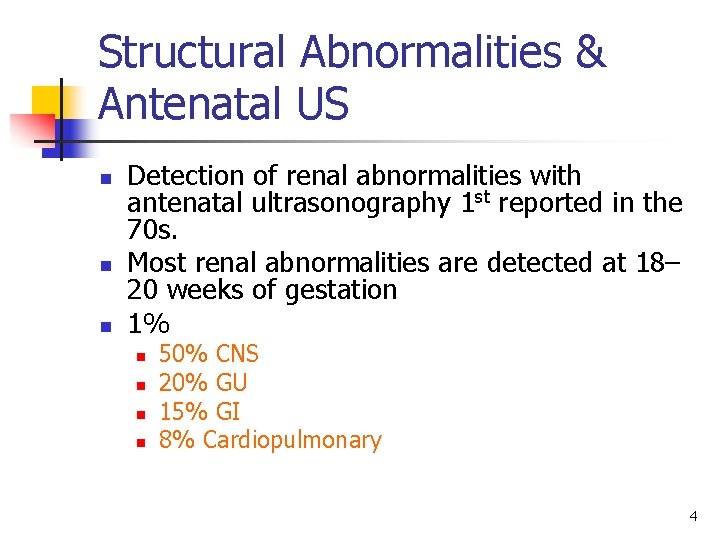
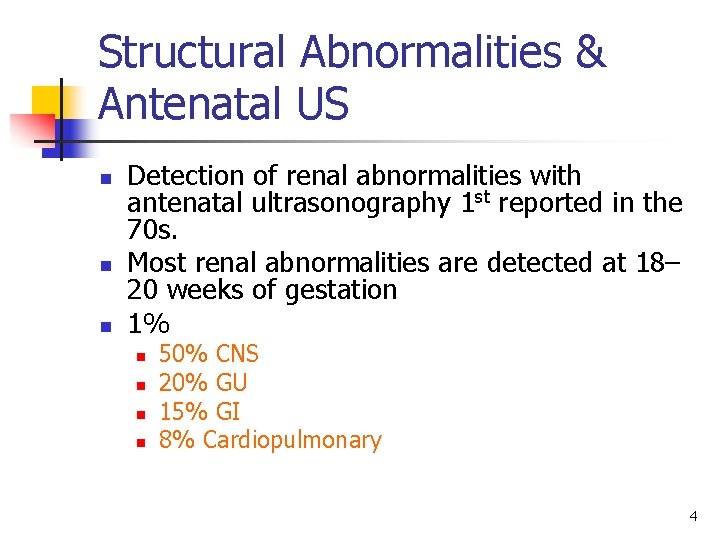
Structural Abnormalities & Antenatal US n n n Detection of renal abnormalities with antenatal ultrasonography 1 st reported in the 70 s. Most renal abnormalities are detected at 18– 20 weeks of gestation 1% n n 50% CNS 20% GU 15% GI 8% Cardiopulmonary 4
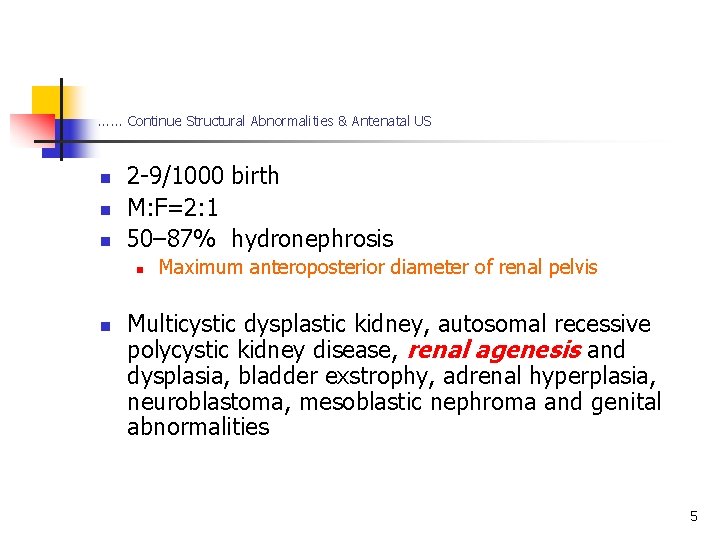
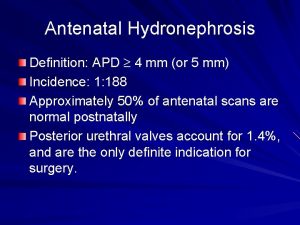
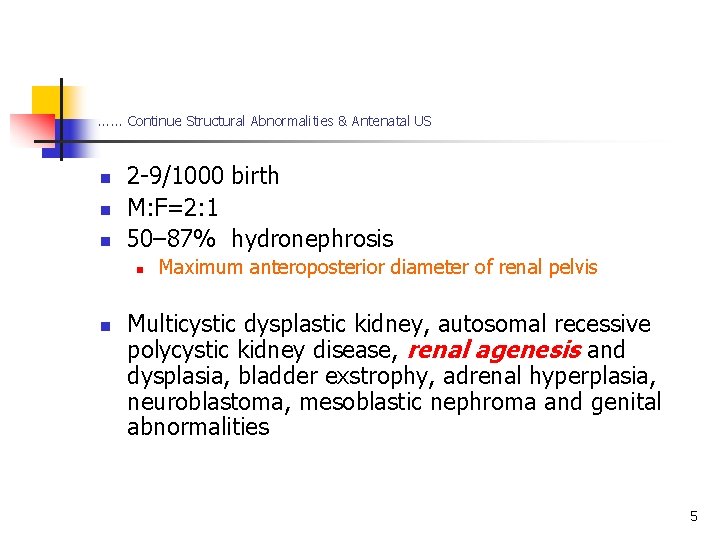
. . . Continue Structural Abnormalities & Antenatal US n n n 2 -9/1000 birth M: F=2: 1 50– 87% hydronephrosis n n Maximum anteroposterior diameter of renal pelvis Multicystic dysplastic kidney, autosomal recessive polycystic kidney disease, renal agenesis and dysplasia, bladder exstrophy, adrenal hyperplasia, neuroblastoma, mesoblastic nephroma and genital abnormalities 5
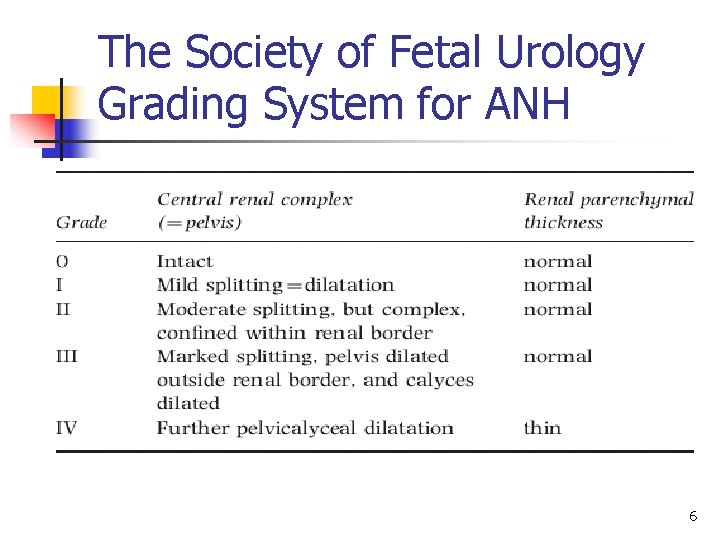
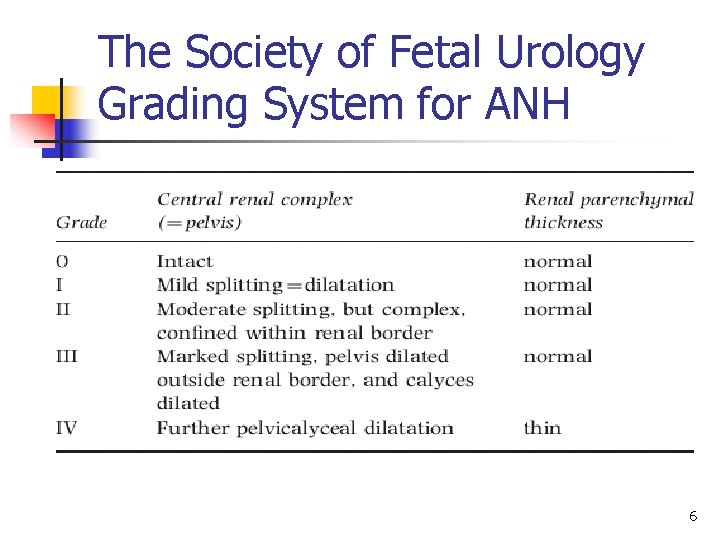
The Society of Fetal Urology Grading System for ANH 6
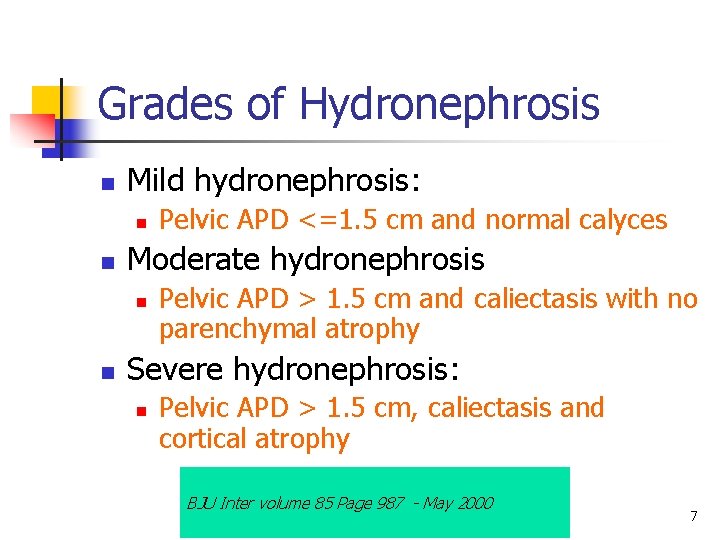
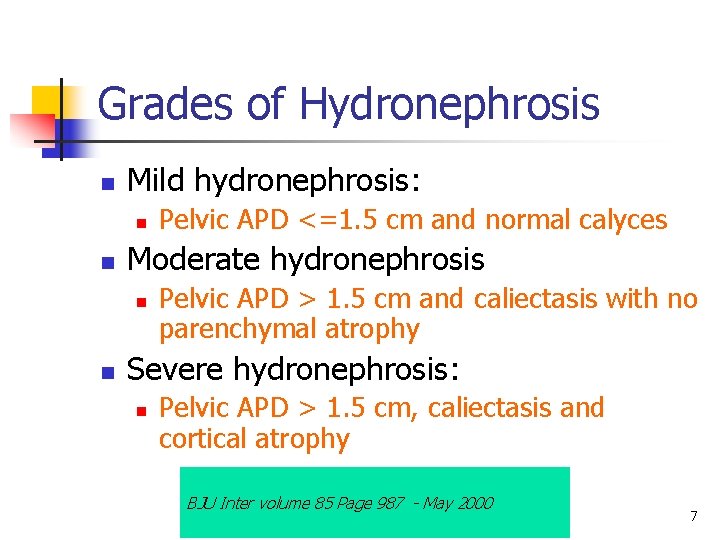
Grades of Hydronephrosis n Mild hydronephrosis: n n Moderate hydronephrosis n n Pelvic APD <=1. 5 cm and normal calyces Pelvic APD > 1. 5 cm and caliectasis with no parenchymal atrophy Severe hydronephrosis: n Pelvic APD > 1. 5 cm, caliectasis and cortical atrophy BJU Inter volume 85 Page 987 - May 2000 7
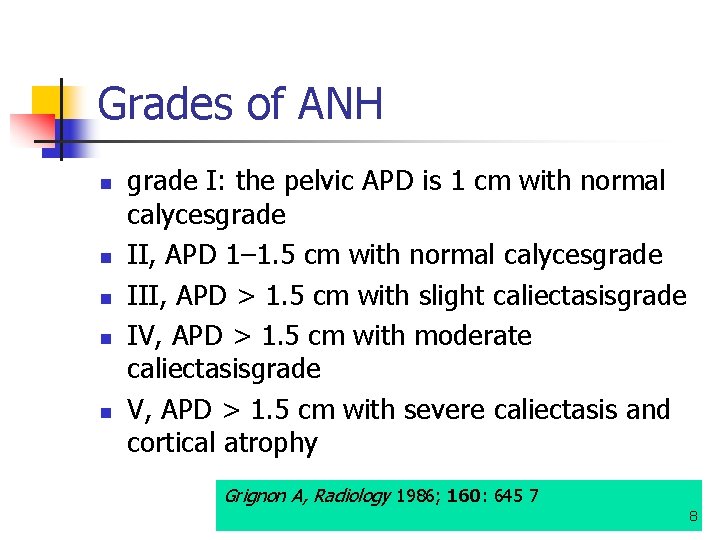
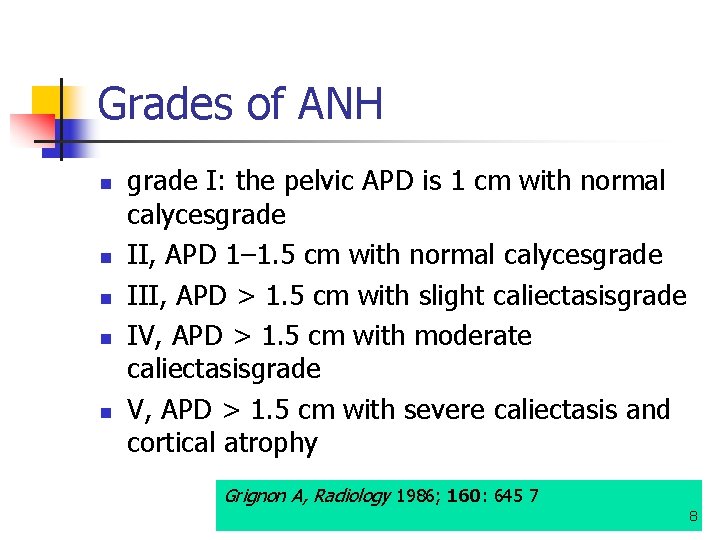
Grades of ANH n n n grade I: the pelvic APD is 1 cm with normal calycesgrade II, APD 1– 1. 5 cm with normal calycesgrade III, APD > 1. 5 cm with slight caliectasisgrade IV, APD > 1. 5 cm with moderate caliectasisgrade V, APD > 1. 5 cm with severe caliectasis and cortical atrophy Grignon A, Radiology 1986; 160: 645 7 8
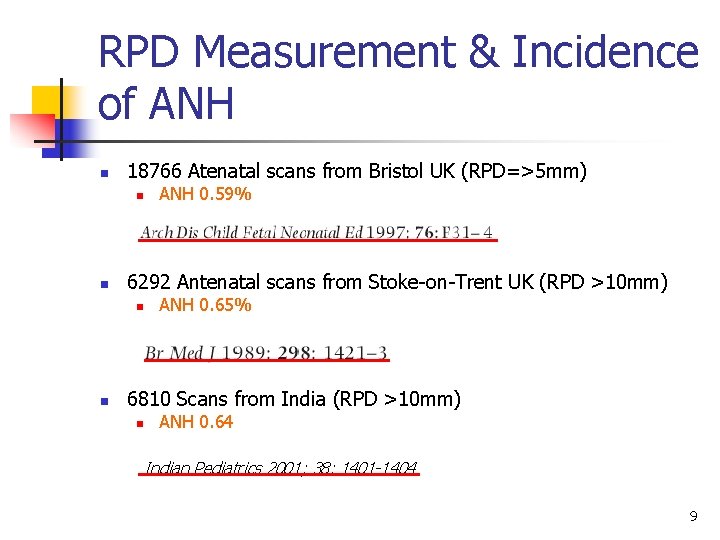
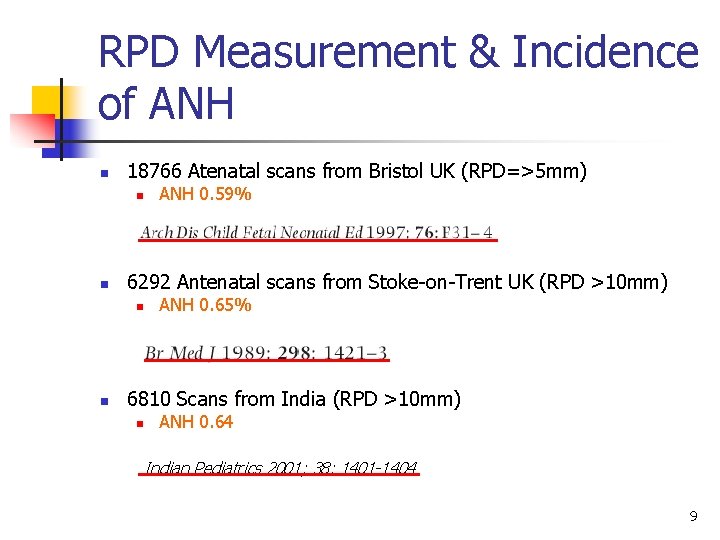
RPD Measurement & Incidence of ANH n 18766 Atenatal scans from Bristol UK (RPD=>5 mm) n n 6292 Antenatal scans from Stoke-on-Trent UK (RPD >10 mm) n n ANH 0. 59% ANH 0. 65% 6810 Scans from India (RPD >10 mm) n ANH 0. 64 Indian Pediatrics 2001; 38: 1401 -1404 9
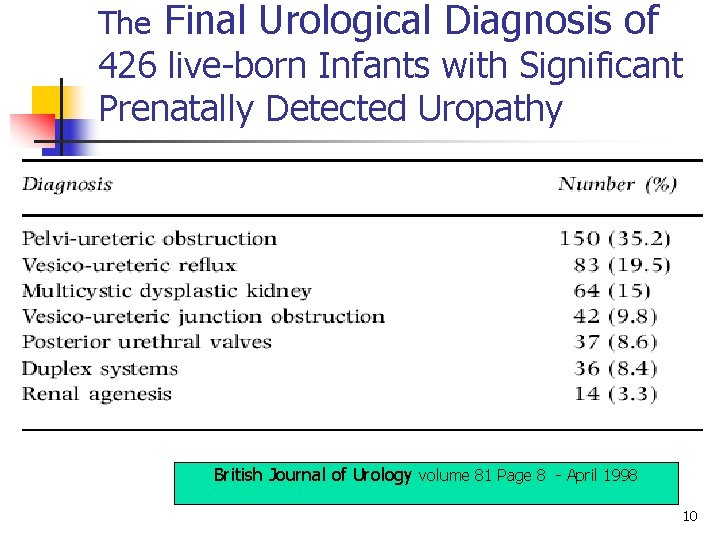
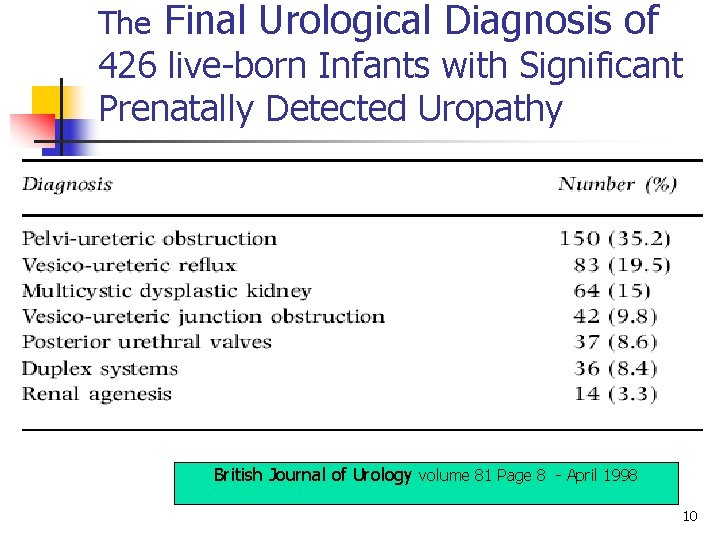
The Final Urological Diagnosis of 426 live-born Infants with Significant Prenatally Detected Uropathy British Journal of Urology volume 81 Page 8 - April 1998 10
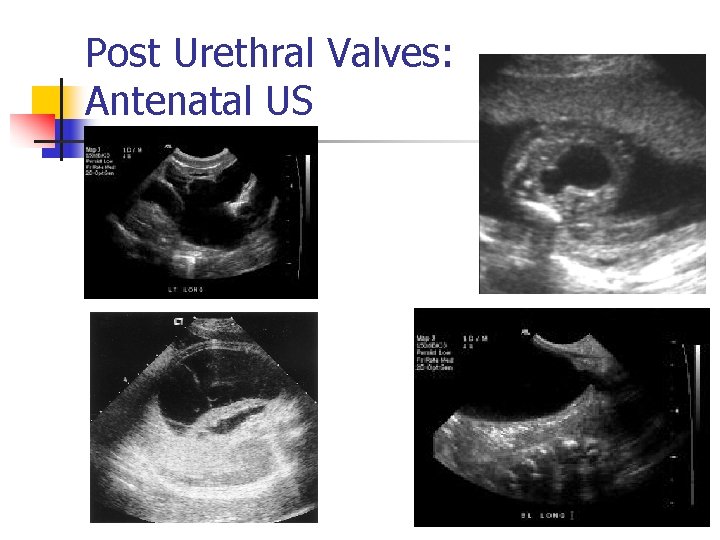
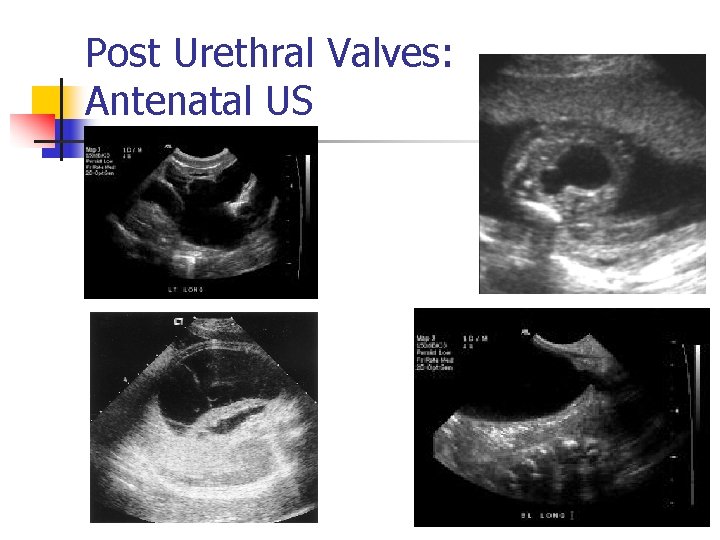
Post Urethral Valves: Antenatal US 11
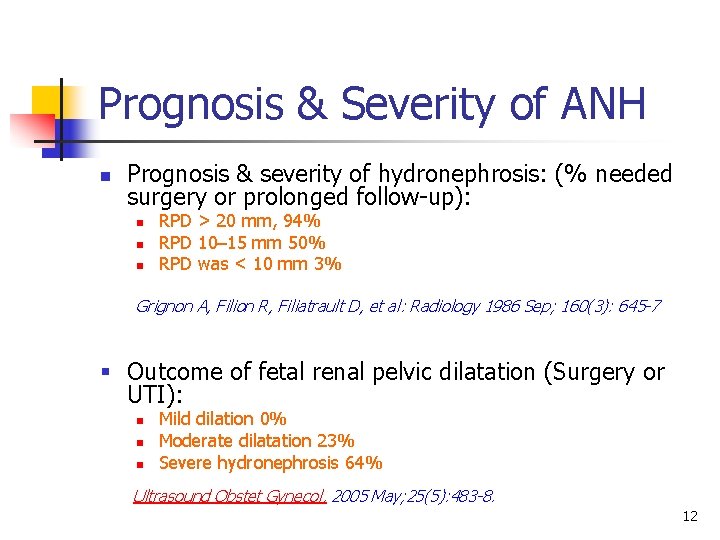
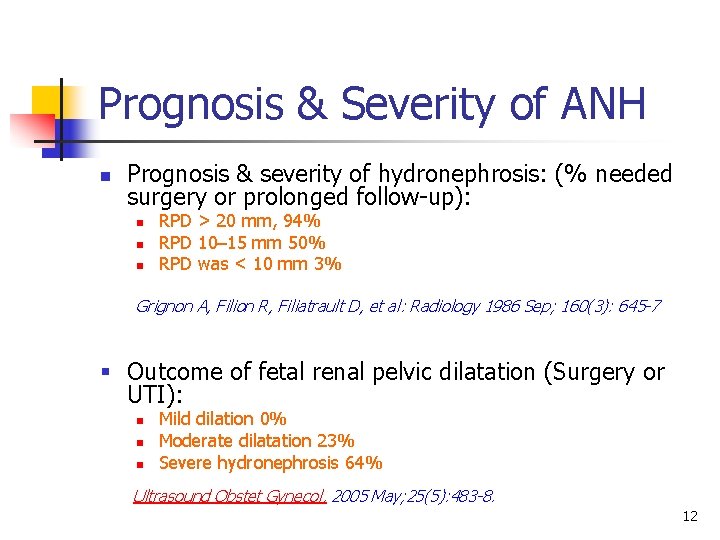
Prognosis & Severity of ANH n Prognosis & severity of hydronephrosis: (% needed surgery or prolonged follow-up): n n n RPD > 20 mm, 94% RPD 10– 15 mm 50% RPD was < 10 mm 3% Grignon A, Filion R, Filiatrault D, et al: Radiology 1986 Sep; 160(3): 645 -7 § Outcome of fetal renal pelvic dilatation (Surgery or UTI): n n n Mild dilation 0% Moderate dilatation 23% Severe hydronephrosis 64% Ultrasound Obstet Gynecol. 2005 May; 25(5): 483 -8. 12
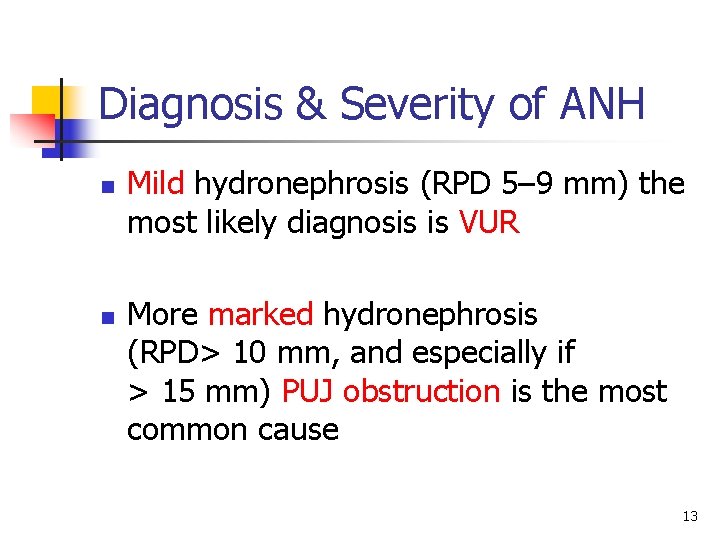
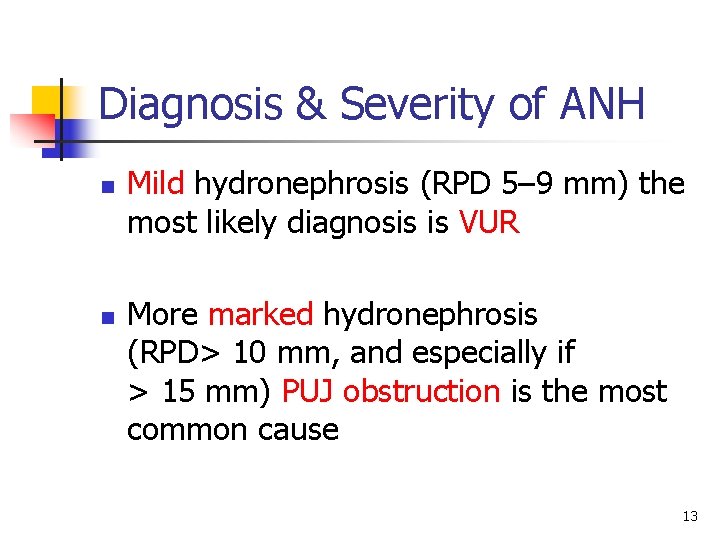
Diagnosis & Severity of ANH n Mild hydronephrosis (RPD 5– 9 mm) the most likely diagnosis is VUR n More marked hydronephrosis (RPD> 10 mm, and especially if > 15 mm) PUJ obstruction is the most common cause 13
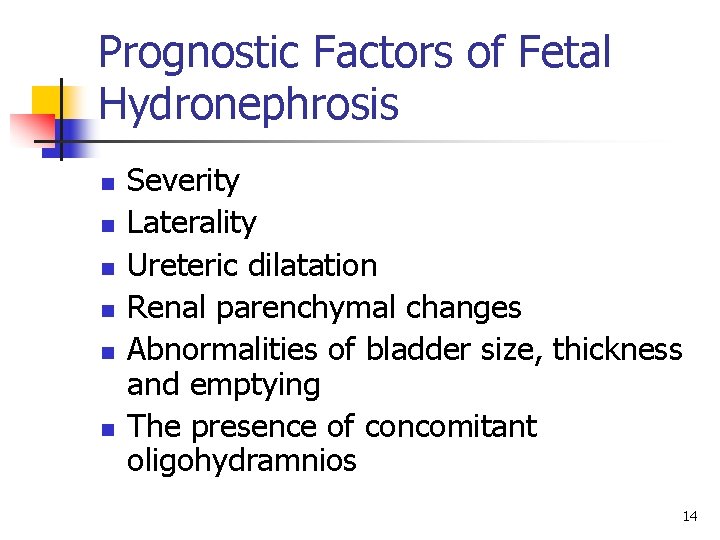
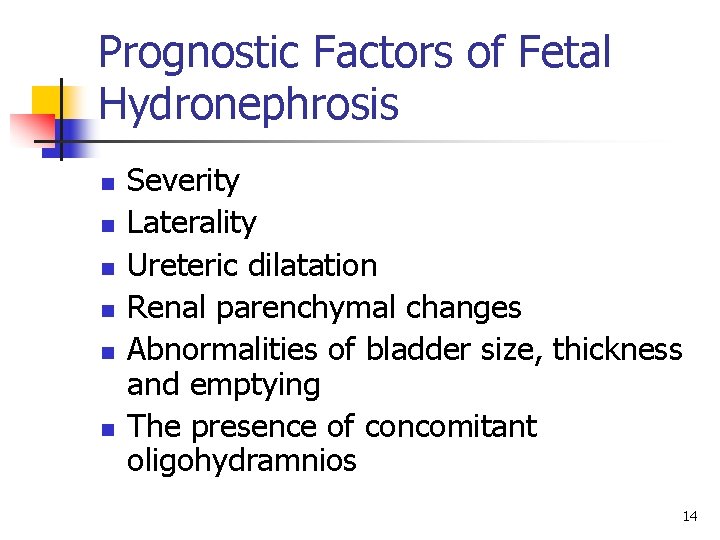
Prognostic Factors of Fetal Hydronephrosis n n n Severity Laterality Ureteric dilatation Renal parenchymal changes Abnormalities of bladder size, thickness and emptying The presence of concomitant oligohydramnios 14
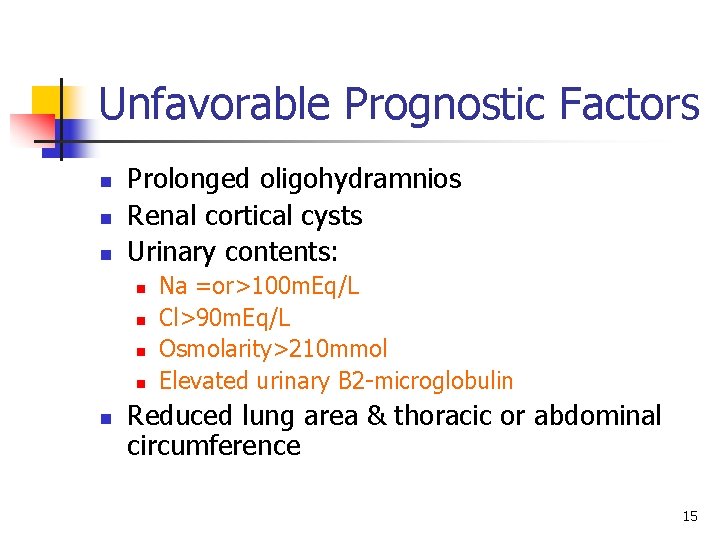
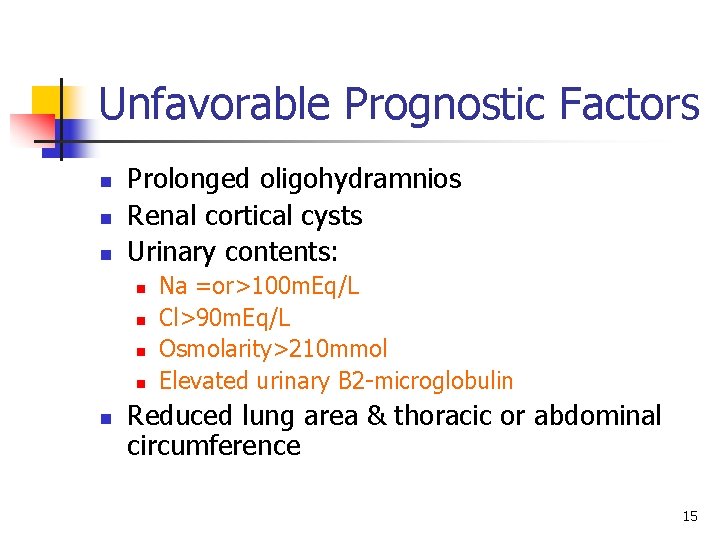
Unfavorable Prognostic Factors n n n Prolonged oligohydramnios Renal cortical cysts Urinary contents: n n n Na =or>100 m. Eq/L Cl>90 m. Eq/L Osmolarity>210 mmol Elevated urinary B 2 -microglobulin Reduced lung area & thoracic or abdominal circumference 15
Antenatal Counseling n n Enormous distress to parents Communication difficulties between the relevant specialists Limited understanding of the natural history Many anomalies may have no long term consequence 16
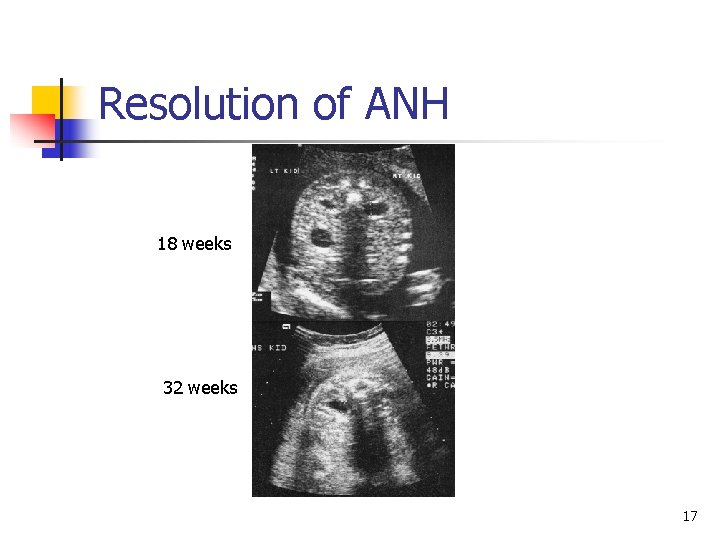
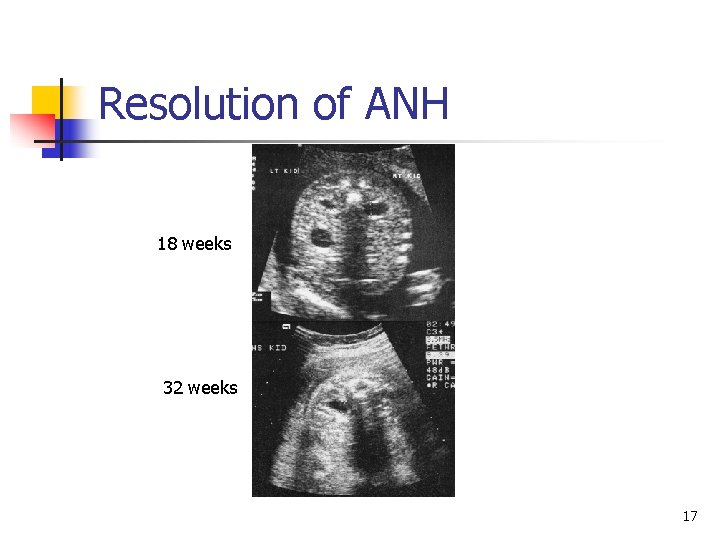
Resolution of ANH 18 weeks 32 weeks 17
Fetal Intervention I. II. III. IV. No intervention: Regular US Termination of pregnancy (up to 23 weeks) Induction of labor Prenatal intervention Only at an experienced institution under approved protocols 18
Intervention n n n Male fetus Second trimester Severe hydroureteronephrosis Bilateral Reasonable fetal urinary indicators Progressive oligohydramnios. 19
Prenatal Intervention for Urinary Obstruction n For most fetuses intervention is not necessary Decompression will restore amniotic fluid---> prevent development of fetal pulmonary hypoplasia ? ? Arrest or reverse renal cystic dysplastic changes 20
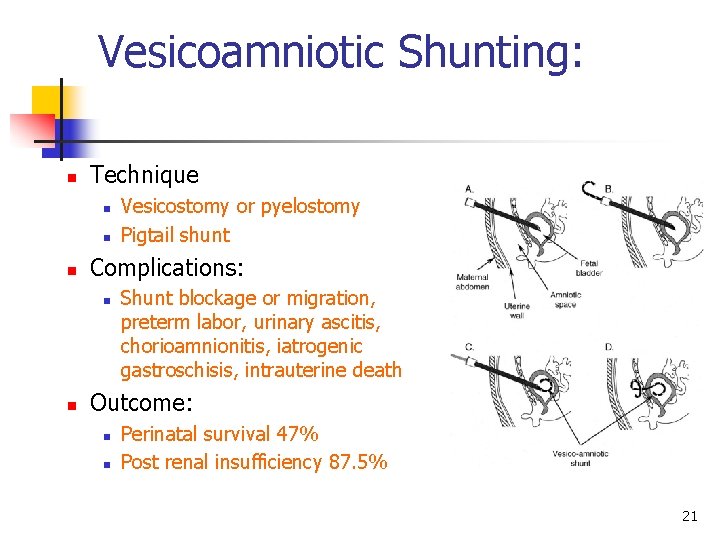
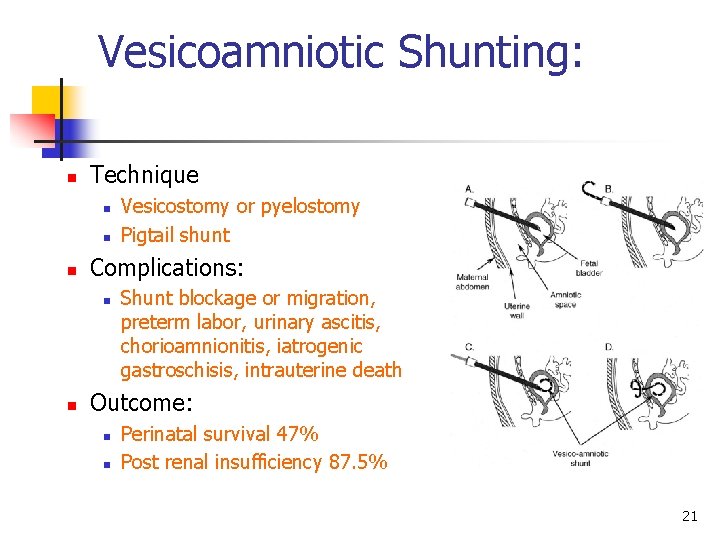
Vesicoamniotic Shunting: n Technique n n n Complications: n n Vesicostomy or pyelostomy Pigtail shunt Shunt blockage or migration, preterm labor, urinary ascitis, chorioamnionitis, iatrogenic gastroschisis, intrauterine death Outcome: n n Perinatal survival 47% Post renal insufficiency 87. 5% 21
Prenatal Evaluation and Treatment for Fetal Lower Urinary Tract Obstruction" n The long term outcomes for shunts in fetal bladder outlet obstruction: n Etiology: n n Posterior urethral valves 39% Urethral atresia 22% Prune Belly Syndrome 39%. Outcome: n n More than 45% had a GFR of >70 ml/min 22% had renal insufficiency 33% were ultimately on dialysis 33% had a transplant Society for Fetal Urology 35 th Biannual Meeting 2005 22
Fetal Cystoscopy n n n US guided 1. 3 mm fetoscope Cannula thru maternal then fetal abdomen then fetal bladder Laser ablation of valves Results n 9 fetuses: 4 success n 2 viable at birth n 1 died age 4 months from bronchopneumonia and one died age 3 m from necrotizing enterocolitis 23
n n n A survey instrument was mailed to all members of the Society for Fetal Urology. 7 case scenarios that addressed critical decision points in patients with antenatally detected genitourinary abnormalities. A total of 112 of 188 Society for Fetal Urology members (60%) completed the survey. J UROL Vol. 164, 1052– 1056, September 2000 24
n 32 -week fetus with normal amniotic fluid and suspected ureteropelvic junction: n n 99% observation & serial US 36 -week fetus with suspected posterior urethral valves without oligohydramnios: n n Most respondents elected no intervention 27% induce early delivery 25
…continue n 23 -week fetus with suspected PUV and oligohydramnios with bladder electrolytes suggestive of good renal function: n n n Intervene antenatally using a vesicoamniotic shunt (71%) Serial aspiration (7%) Amnioinfusion (7%). 26
Conclusion n Situations that warrant antenatal intervention for a genitourinary abnormality are exceedingly low and may include: n n Cases of oligohydramnios Suspected favorable renal function Absence of life threatening congenital abnormalities. In cases with normal amniotic fluid antenatal intervention is not recommended regardless of the detected abnormality. 27
……. . continue Conclusion n n No evidence exists demonstrating the benefit of antenatal intervention in terms of renal function and only in a select number of cases will it benefit pulmonary function. To our knowledge no scientific data exist that demonstrate the long-term benefit of early delivery of cases with antenatally detected, genitourinary abnormalities. 28
Postnatal Investigations n n n Abdominal mass Deficient abdominal wall Undescended testes Palpable bladder Renal profile US within 1 week (earlier ? ? false because of the physiological oliguria) 29
When to perform US post delivery n Renal obstruction may be underestimated or missed on a renal sonogram obtained 6 days after birth. A sonogram obtained 6 weeks after birth is more specific for detecting obstruction. AJR Am J Roentgenol. 1995 Apr; 164(4): 963 -7. 30

…. . continue Postnatal Investigations n n n Is it unilateral or bilateral? Is it solitary kidney? Are there associated anomalies? ? Prophylactic antibiotics Hydronephrosis =obstruction 31
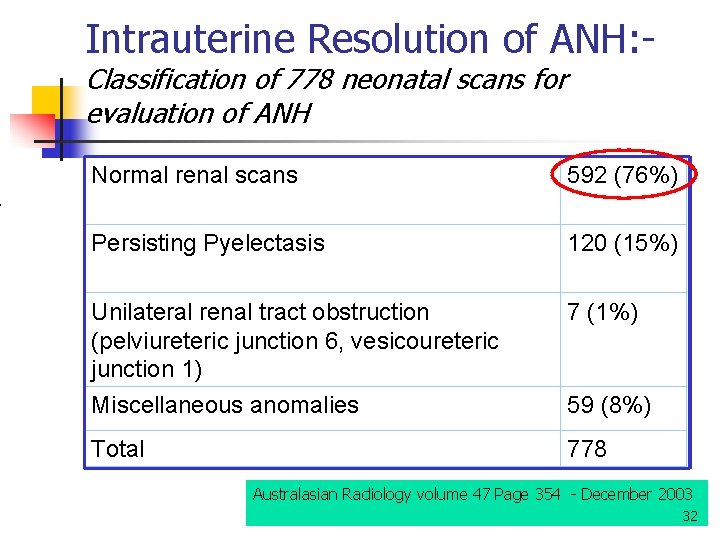
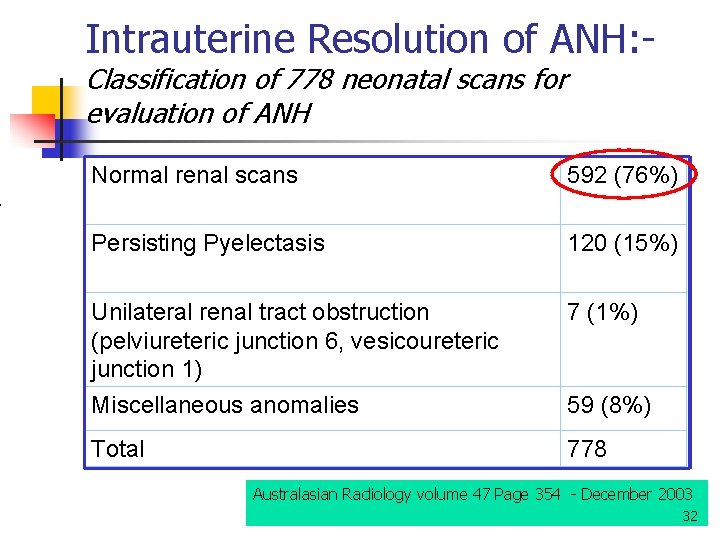
Intrauterine Resolution of ANH: - Classification of 778 neonatal scans for evaluation of ANH Normal renal scans 592 (76%) Persisting Pyelectasis 120 (15%) Unilateral renal tract obstruction (pelviureteric junction 6, vesicoureteric junction 1) 7 (1%) Miscellaneous anomalies 59 (8%) Total 778 Australasian Radiology volume 47 Page 354 - December 2003 32
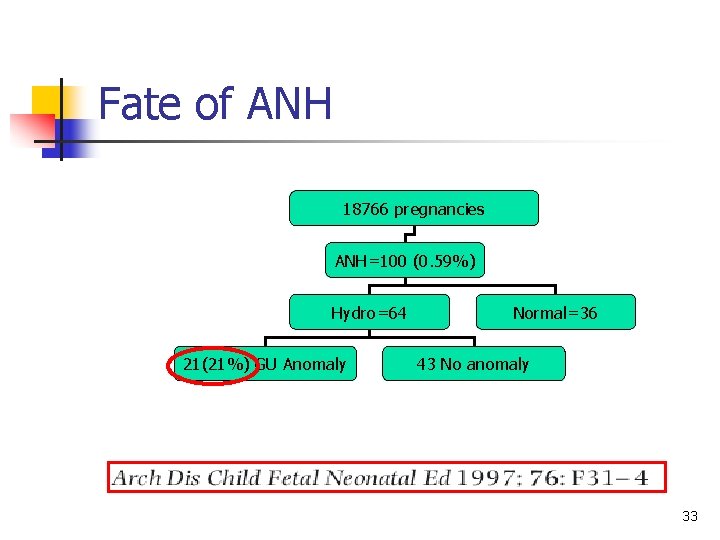
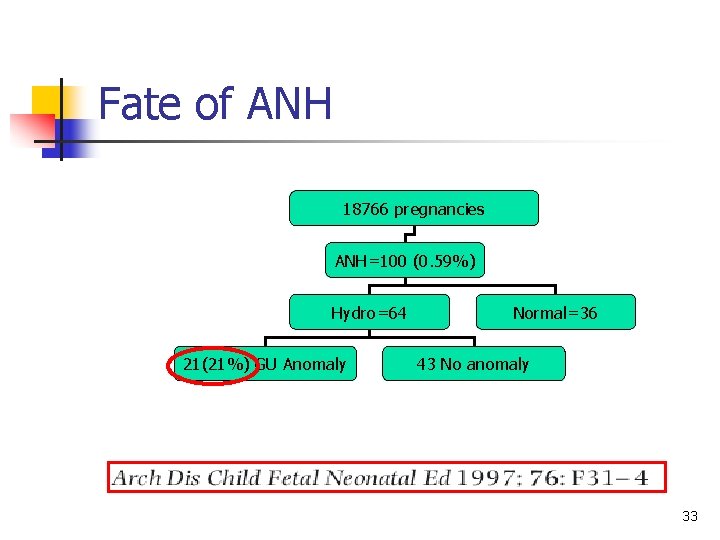
Fate of ANH 18766 pregnancies ANH=100 (0. 59%) Hydro=64 21(21%) GU Anomaly Normal=36 43 No anomaly 33
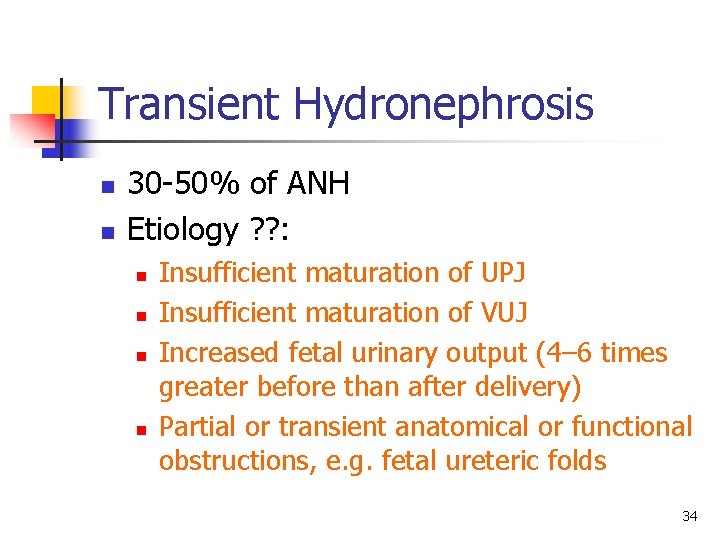
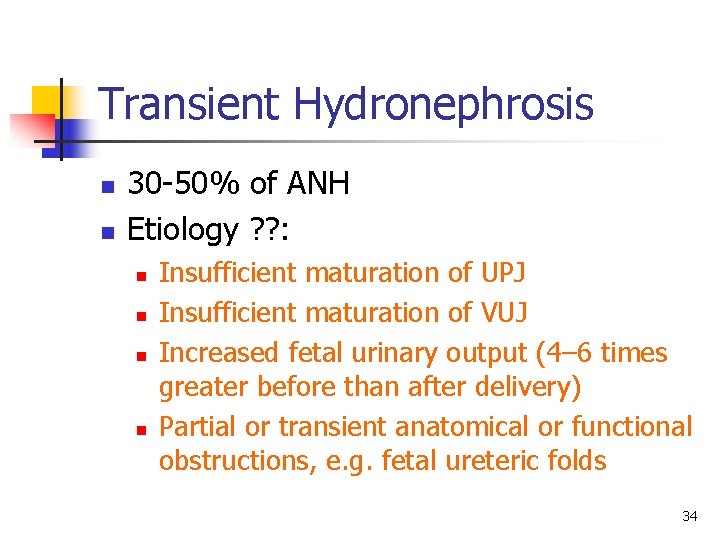
Transient Hydronephrosis n n 30 -50% of ANH Etiology ? ? : n n Insufficient maturation of UPJ Insufficient maturation of VUJ Increased fetal urinary output (4– 6 times greater before than after delivery) Partial or transient anatomical or functional obstructions, e. g. fetal ureteric folds 34
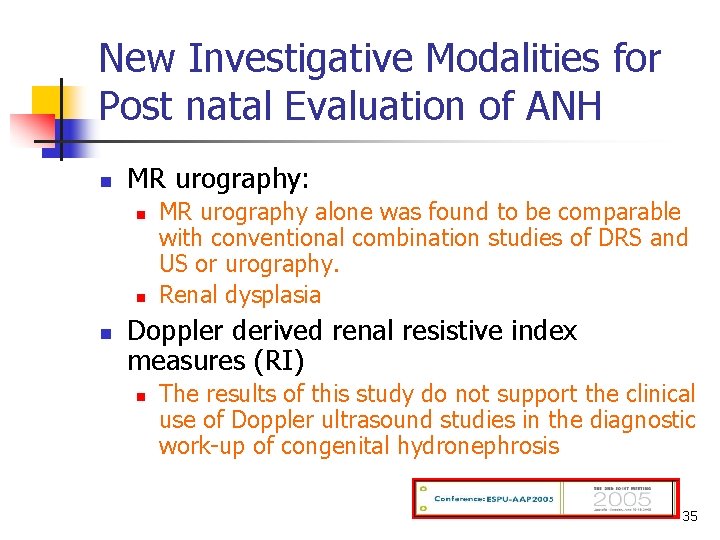
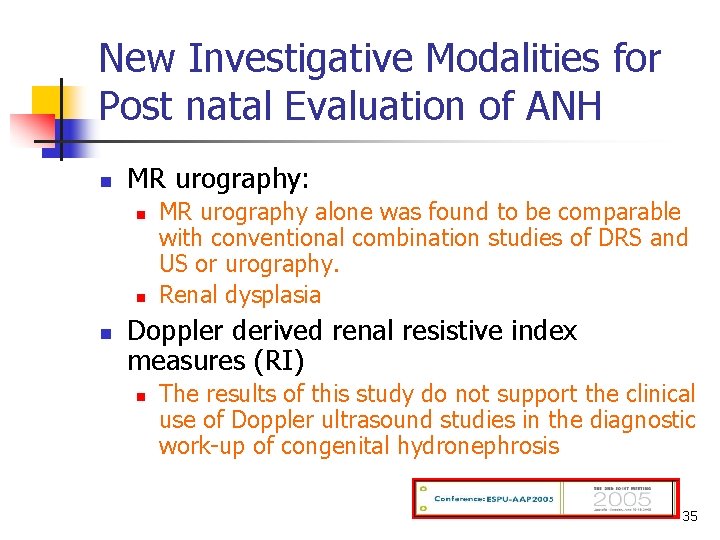
New Investigative Modalities for Post natal Evaluation of ANH n MR urography: n n n MR urography alone was found to be comparable with conventional combination studies of DRS and US or urography. Renal dysplasia Doppler derived renal resistive index measures (RI) n The results of this study do not support the clinical use of Doppler ultrasound studies in the diagnostic work-up of congenital hydronephrosis 35
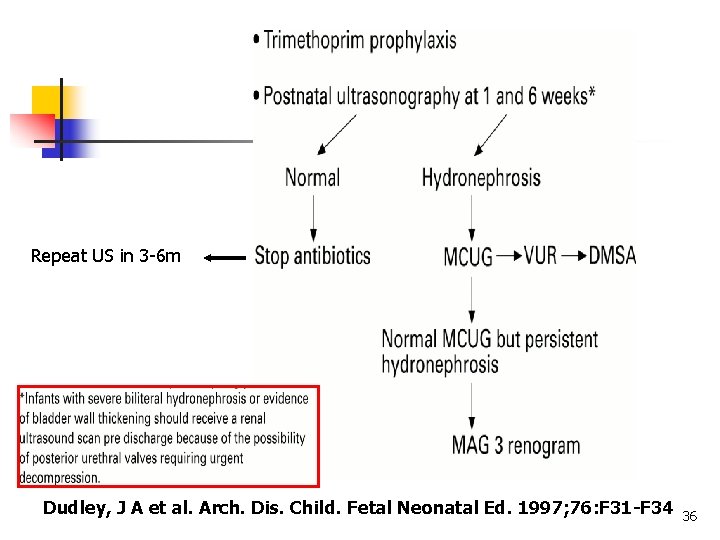
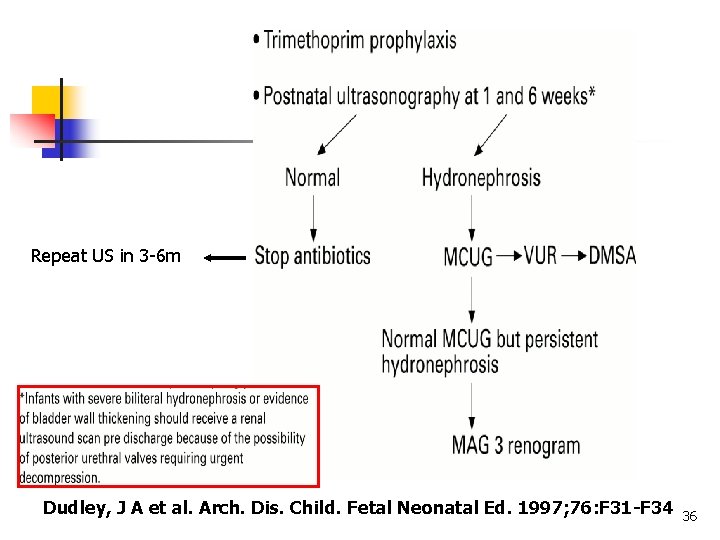
Repeat US in 3 -6 m Dudley, J A et al. Arch. Dis. Child. Fetal Neonatal Ed. 1997; 76: F 31 -F 34 36

Persistent Hydronephrosis without Obstruction n 10 -15% 50% resolves by 12 months Needs long time follow-up 37
Take Home Messages n n n Antental hydronephrosis is not uncommon With the high percentage of history of consanguinity, the incidence might be higher in Saudi Arabia The Obstetrician should be vigilant in looking for it during the routine antenatal visits. 38
. . . continue Take Home Messages n n No evidence exists demonstrating the benefit of antenatal intervention in terms of renal function and only in a select number of cases will it benefit pulmonary function. To our knowledge no scientific data exist that demonstrate the long-term benefit of early delivery of cases with antenatally detected, genitourinary abnormalities. 39

u o Y k n a h T 40
 Staghorn calculus
Staghorn calculus Potter face oligohydramnios
Potter face oligohydramnios Congenital hydronephrosis
Congenital hydronephrosis Fetal hydronephrosis ultrasound grading
Fetal hydronephrosis ultrasound grading Nursing management of hydronephrosis
Nursing management of hydronephrosis Nursing management of hydronephrosis
Nursing management of hydronephrosis Peritonitis radiopedia
Peritonitis radiopedia Elena in arabic writing
Elena in arabic writing Farsi 1
Farsi 1 Farsi 101
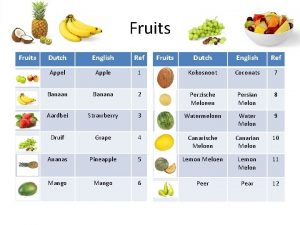
Farsi 101 Fruits in netherlands
Fruits in netherlands Cyrus tabrizi caviar
Cyrus tabrizi caviar Farsi tts
Farsi tts Would rather form
Would rather form Would you rather + verb
Would you rather + verb Banc plus checklist
Banc plus checklist Antenatal class adalah
Antenatal class adalah Ballottement
Ballottement Banc plus checklist
Banc plus checklist Conclusion of antenatal care
Conclusion of antenatal care Antenatal visit according to who
Antenatal visit according to who Antenatal visit
Antenatal visit Etiolgy
Etiolgy Antenatal care summary
Antenatal care summary Antenatal intrapartum and postnatal
Antenatal intrapartum and postnatal Fundal grip
Fundal grip Nice antenatal and postnatal mental health
Nice antenatal and postnatal mental health Antenatal investigations
Antenatal investigations Antenatal care definition
Antenatal care definition Mcug
Mcug If you had studied hard, you wouldn't failed the exam.
If you had studied hard, you wouldn't failed the exam. Major prophets
Major prophets If you died tonight would you go to heaven
If you died tonight would you go to heaven If you could be invisible what would you do and why?
If you could be invisible what would you do and why? Expenseondemand
Expenseondemand Condition type 3
Condition type 3 Present unreal conditional)
Present unreal conditional) If i could have three wishes they would be
If i could have three wishes they would be If+past perfect
If+past perfect Expressing preference would rather
Expressing preference would rather Hasan dam
Hasan dam