Anesthesia for Intracranial Aneurysm Surgery Pekka O Talke
- Slides: 21
Anesthesia for Intracranial Aneurysm Surgery Pekka O. Talke, MD
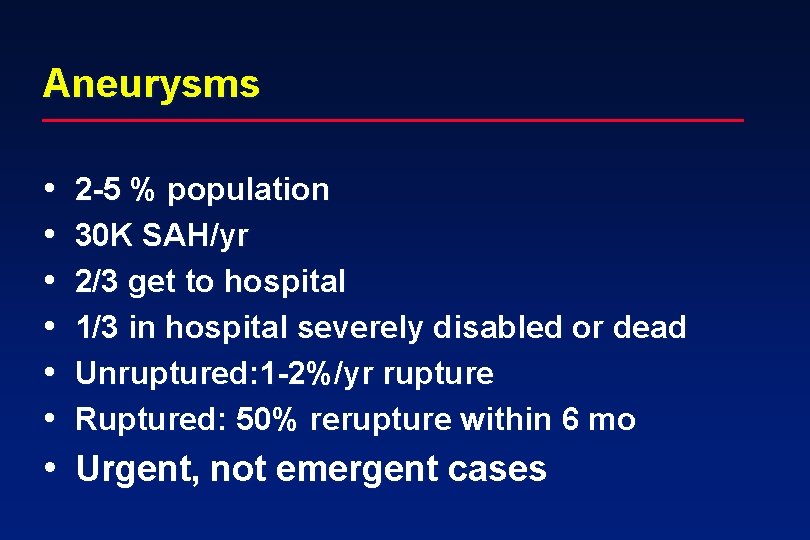
Aneurysms • • • 2 -5 % population 30 K SAH/yr 2/3 get to hospital 1/3 in hospital severely disabled or dead Unruptured: 1 -2%/yr rupture Ruptured: 50% rerupture within 6 mo • Urgent, not emergent cases
Surgeons • Lawton
Anesthetic Goals • • • Prevent aneurysm rupture (avoid hypertension) Decrease ICP (surgical exposure, retraction) Maintain CPP (>70 mm. Hg) Prevent cerebral ischemia from retraction Good operating conditions (NO movement, brain relaxation for exposure)
Patients, preop • Symptomatic/asymptomatic • Ruptured (SAH grade, myocardial effects), • • • unruptured Possibly intubated Location and size of aneurysm Intracranial mass effect from SAH (increased ICP) Neurologic deficits and symptoms Timing, vasospasm
Preop • One IV • Premedicate with up to 2 mg of midazolam if normal mental status. • Remind of potential post op intubation • Adequate fluid loading (5 to 7 ml/kg of LR, angio)
Induction • • • Routine monitors Propofol or thiopental Fentanyl 5 ug/kg in divided doses prior to intubation • Muscle relaxant (roc). • Arterial cannula before intubation • Avoid hypertension (propofol) and hypotension (CPP, vasospasm)
Induction cont. • • • Ceftriaxone 1 gm, 4 -10 mg decadron, 1 gm/kg mannitol. Tape eyes with tagaderms (prep solution) Temp probe, foley Additional IV (limited access, 300 cc to liters of blood loss) Compression stockings
Positioning • Supine, bump • Long cases, lots of padding (pink and blue foam) • Table turned typically 90 degrees • Head down? , aeroplaning • After draping minimal/no access to face (secure ET well)
Maintenance • Oxygen • Propofol infusion (50 -200 ug/kg/min) (SSEPs, EEG) • Inhalation agent (<0. 25 MAC Isoflurane). Muscle relaxation (vec, panc) • Moderate hyperventilation (ET CO 2 30 mm. Hg) • Euvolemia to 500 cc more (LR) • Moderate hypothermia (34 o. C)
Burst supression • • When requested by surgeon Thiopental 125 mg (5 cc) doses Till 70 -80% EEG burst supression Redose as needed Turn fentanyl infusion off Reduce propofol infusion rate Support CPP with phenylephrine infusion
Clipping • • • Temporary clips (golden) Permanent clips (silver) Aneurysm manipulation before clipping (bleed) Record clip on/off times Maintain CPP during temporary clipping Start closing, warming and more fluid loading after clipping
Toward the end • First indication of end of surgery when clip aneurysm (60 min) • Normalize CO 2 once dura closed or earlier if lots of intracranial space • Reduce propofol if possible, and titrate in labetalol
Toward the end cont. • Turn propofol infusion off about 10 min before wakeup • Reverse relaxation once Mayfied pins have been removed • Attempt to wakeup patient. Unlikely if more than 1 gm of thiopental given.
Recovery • Wake patient up as soon as possible • Extubate if possible • Prevent post op hypertension (bleed). Labetalol • Transport to ICU with monitor and oxygen • Head up position
Potential Complications • Delayed awakening from anesthesia • Cerebral ischemia (retraction, temporary clips, vasospasm) • Brain swelling • Intraoperative hemorrhage
Aneurysm rupture • Reasonably common • Intubation, pinning, skin insicion, surgical manipulation • Maintain intravascular volume (blood in the room, get help) • • • Maintain CPP Adequate anesthesia Thiopental before temporary clipping
Vasospasm • • Only if SAH 5 -14 days after SAH Leading cause of SAH morbidity (infarct) Maintain CPP at all times (neo infusion, volume) • HHH therapy • Consider CVP measurement
What’s new? • Retractor pressure • Temp control • Normotension
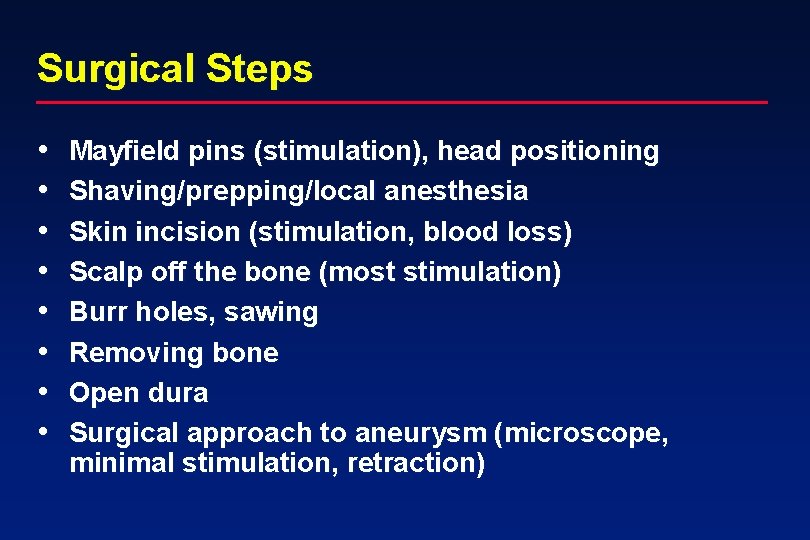
Surgical Steps • • Mayfield pins (stimulation), head positioning Shaving/prepping/local anesthesia Skin incision (stimulation, blood loss) Scalp off the bone (most stimulation) Burr holes, sawing Removing bone Open dura Surgical approach to aneurysm (microscope, minimal stimulation, retraction)
Surgical Steps cont. • • Burst supression Temporary clips, permanent clip(s) Close (60 min) Dura (water tight) Bone flap Scalp and skin Dressing, remove pins
 Turbidity
Turbidity Wake talke
Wake talke Anesthesia for bariatric surgery
Anesthesia for bariatric surgery Edu.mui.ac.ir
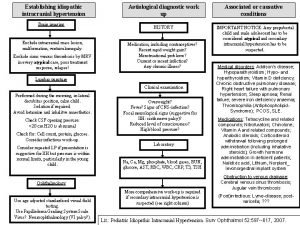
Edu.mui.ac.ir Intracranial hypotension radiopedia
Intracranial hypotension radiopedia Intracranial mass
Intracranial mass Intracranial regulation nursing
Intracranial regulation nursing Patient condition
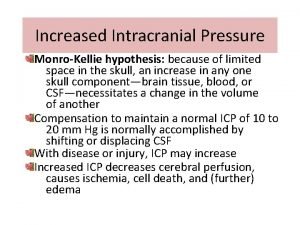
Patient condition Intracranial pressure
Intracranial pressure Increased intracranial pressure ati
Increased intracranial pressure ati Decorticate vs decerebrate
Decorticate vs decerebrate Intracranial teratoma
Intracranial teratoma How does meningitis cause increased intracranial pressure
How does meningitis cause increased intracranial pressure Copyright
Copyright Intracranial hypertension
Intracranial hypertension Minecraft mob vote
Minecraft mob vote Cushing's triad vitals
Cushing's triad vitals Ventricular wall aneurysm
Ventricular wall aneurysm Berry aneurysm
Berry aneurysm Aneurysm
Aneurysm Stent graft
Stent graft Avm vs aneurysm
Avm vs aneurysm