ANAPHYLAXIS RAPID RECOGNITION TREATMENT THOMAS A LUPOLI DO




- Slides: 48
ANAPHYLAXIS: RAPID RECOGNITION & TREATMENT THOMAS A. LUPOLI, DO ALLERGY/IMMUNOLOGY Cardiovascular & Medicine Symposium
Disclaimers and Disclosures Aerocrine Speakers Bureau Executive Board Member-- Florida Allergy, Asthma & Immunology Society
Disclosures No financial conflict of interests
Objectives Review the physiologic mechanisms causing systemic allergic reactions Identify early warning signs of anaphylaxis to allow for rapid recognition of systemic allergic reactions Discuss the importance of early treatment of anaphylaxis
Justice Potter Stewart 1964 • One of the most famous phrases in the entire history of the Supreme Court • Jacobellis v. Ohio • “The Lovers”
Justice Potter Stewart In regard to the definition of pornography: I shall not today attempt further to define the kinds of material I understand to be embraced within that shorthand description [“hardcore pornography"]; and perhaps I could never succeed in intelligibly doing so. But I know it when I see it, and the motion picture involved in this case is not that!

Anaphylaxis Severe life-threatening generalized or systemic hypersensitivity reaction Rapid onset (seconds to minutes) Clinical diagnosis Anaphylactic shock is the end-stage
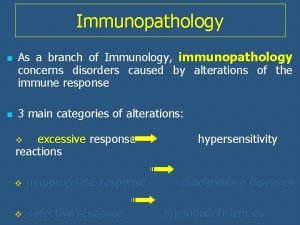
Classification � Immunologic Ig. E mediated Non-Ig. E mediated (formerly anaphylactoid) � Nonimmunologic Direct mast cell degranulation (opioids, exercise or cold induced)
Incidence ? ? ? 1. 2 -12% incidence of US population (2001)
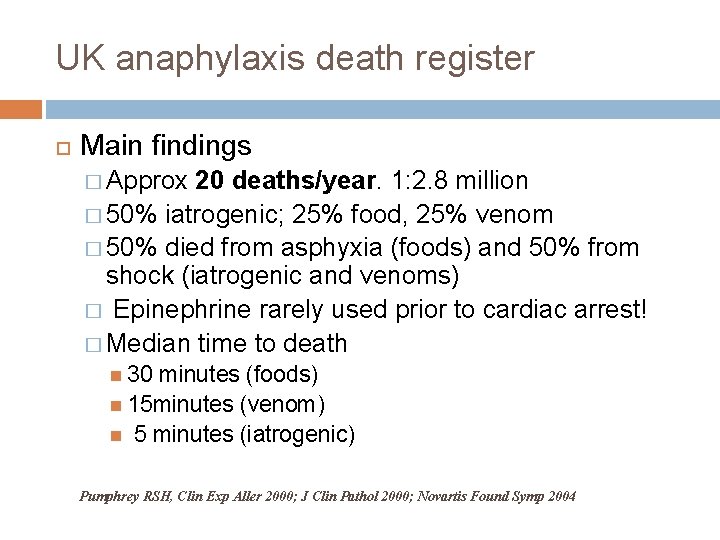
UK anaphylaxis death register Objective � To understand circumstances leading to death in anaphylaxis Methods � Running since 1992 � Detailed information obtained from medical records, coroners offices, medical staff
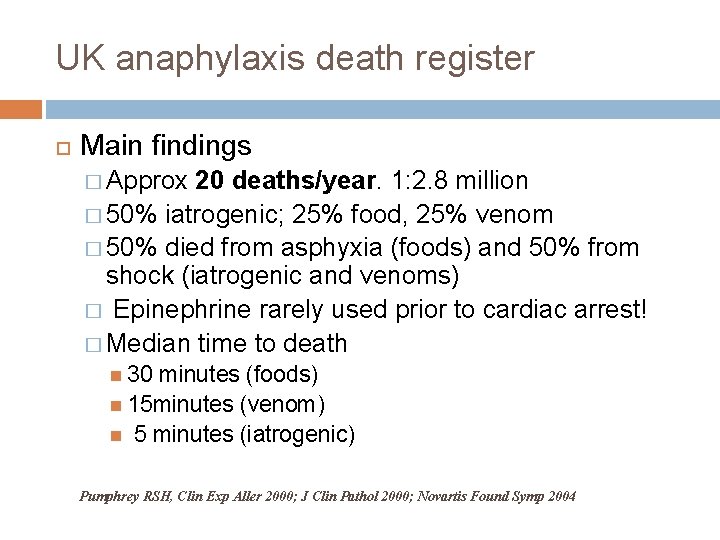
UK anaphylaxis death register Main findings � Approx 20 deaths/year. 1: 2. 8 million � 50% iatrogenic; 25% food, 25% venom � 50% died from asphyxia (foods) and 50% from shock (iatrogenic and venoms) � Epinephrine rarely used prior to cardiac arrest! � Median time to death 30 minutes (foods) 15 minutes (venom) 5 minutes (iatrogenic) Pumphrey RSH, Clin Exp Aller 2000; J Clin Pathol 2000; Novartis Found Symp 2004


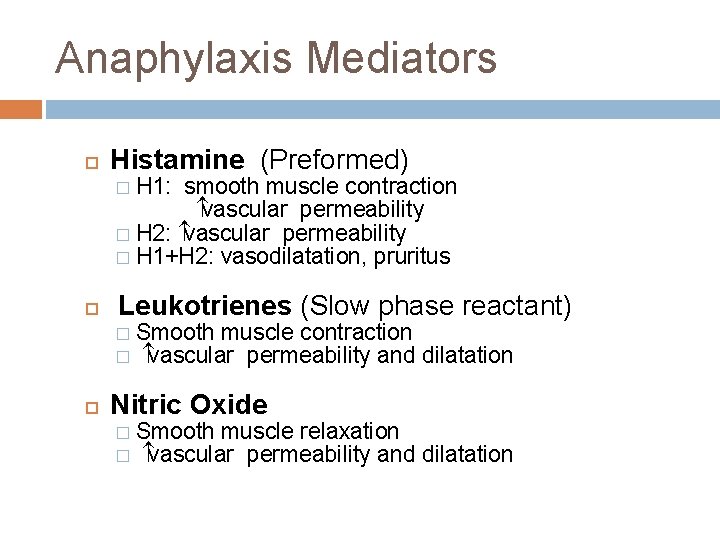
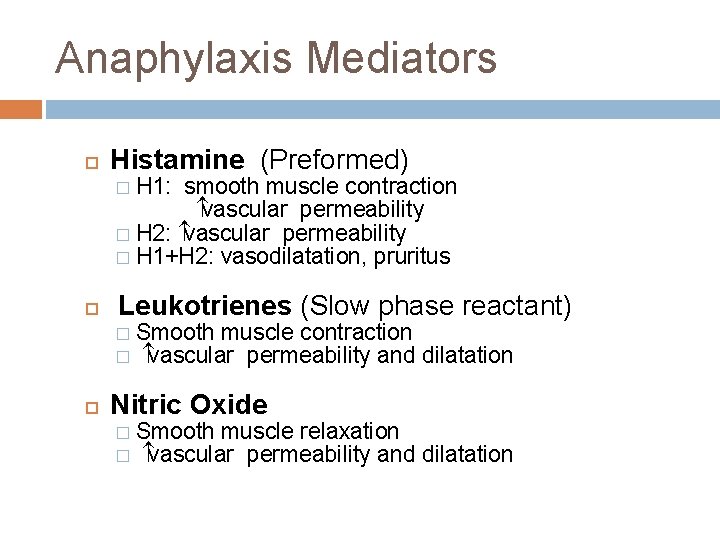
Anaphylaxis Mediators Histamine (Preformed) H 1: smooth muscle contraction vascular permeability � H 2: vascular permeability � H 1+H 2: vasodilatation, pruritus � Leukotrienes (Slow phase reactant) � � Smooth muscle contraction vascular permeability and dilatation Nitric Oxide � � Smooth muscle relaxation vascular permeability and dilatation
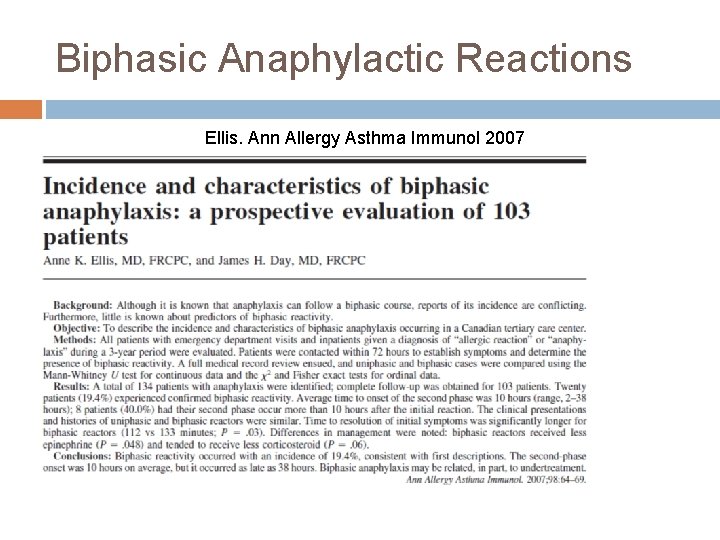
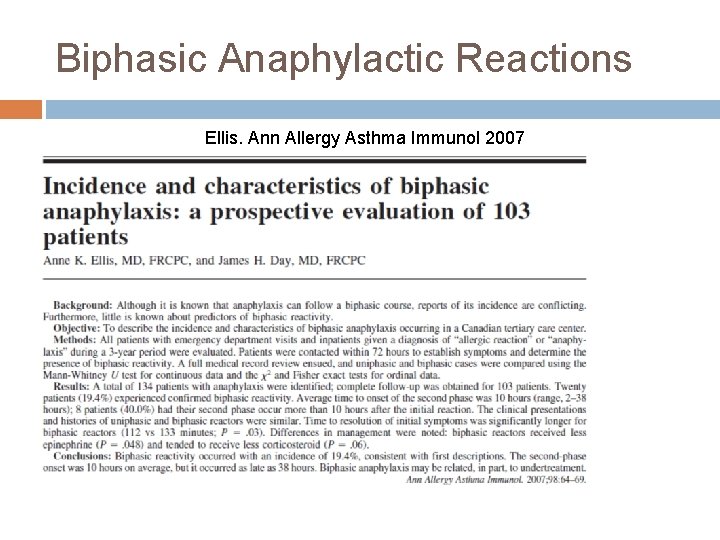
Biphasic Anaphylactic Reactions Ellis. Ann Allergy Asthma Immunol 2007
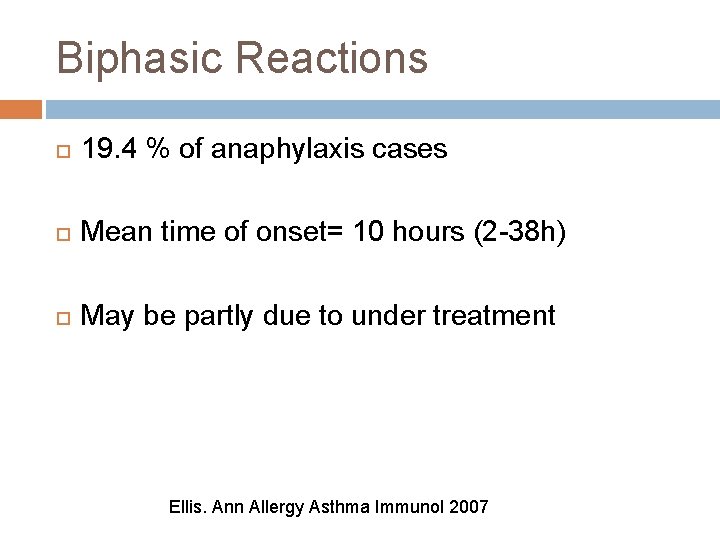
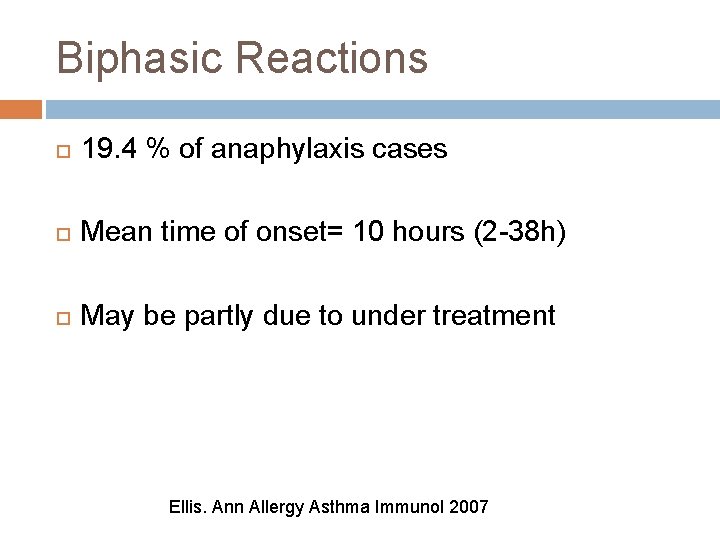
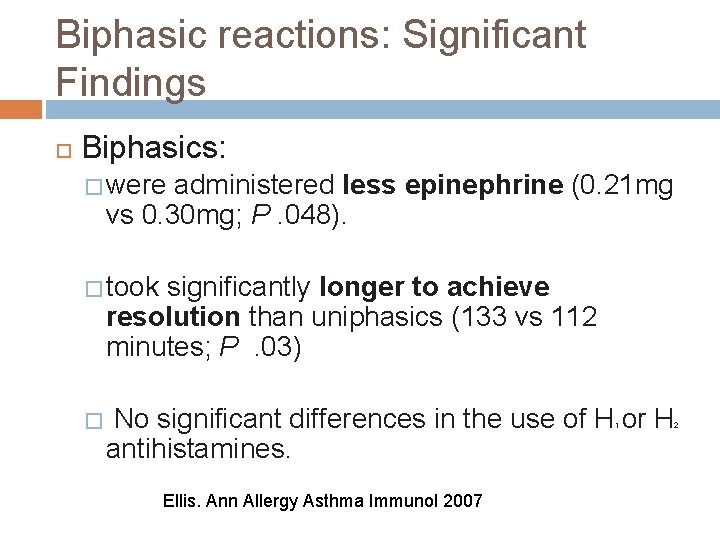
Biphasic Reactions 19. 4 % of anaphylaxis cases Mean time of onset= 10 hours (2 -38 h) May be partly due to under treatment Ellis. Ann Allergy Asthma Immunol 2007
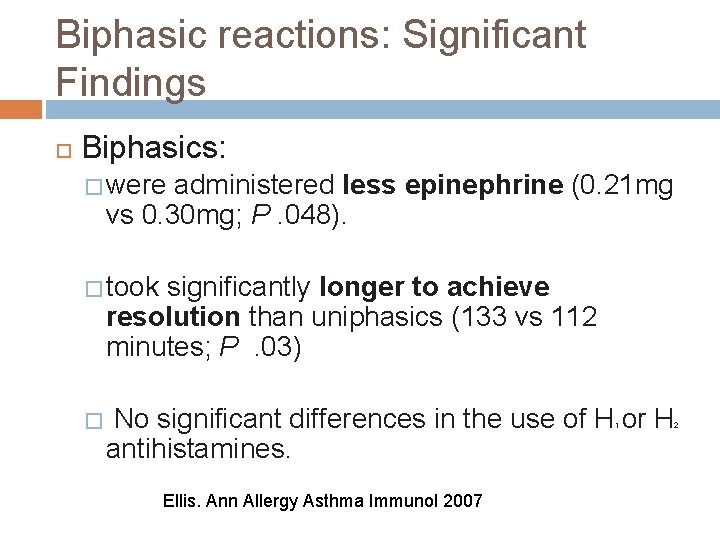
Biphasic reactions: Significant Findings Biphasics: � were administered less epinephrine (0. 21 mg vs 0. 30 mg; P. 048). � took significantly longer to achieve resolution than uniphasics (133 vs 112 minutes; P. 03) � No significant differences in the use of H or H antihistamines. 1 Ellis. Ann Allergy Asthma Immunol 2007 2
Biphasics: Non-significant findings � Biphasics had lower rate of corticosteroid use (P. 07) � Corticosteroid dose tended to be lower in those having biphasic reactions (P. 06).
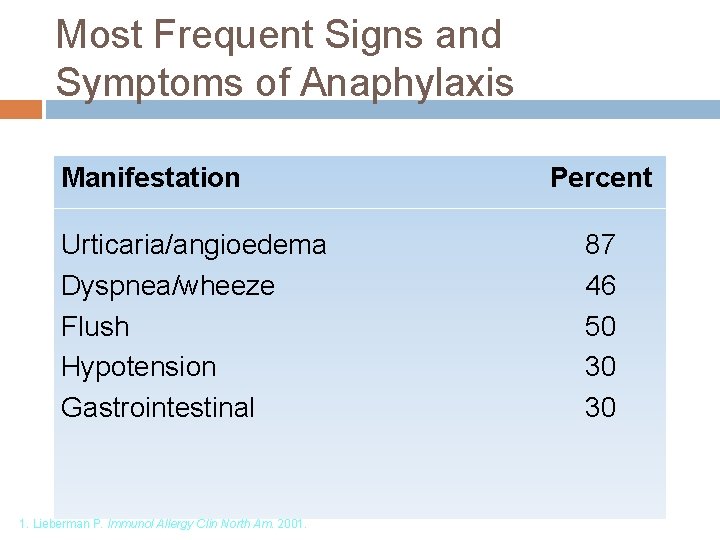
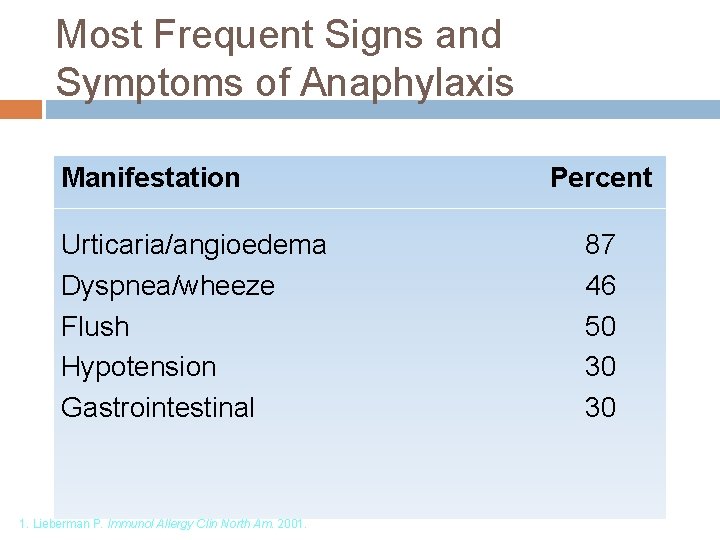
Most Frequent Signs and Symptoms of Anaphylaxis Manifestation Urticaria/angioedema Dyspnea/wheeze Flush Hypotension Gastrointestinal 1. Lieberman P. Immunol Allergy Clin North Am. 2001. Percent 87 46 50 30 30
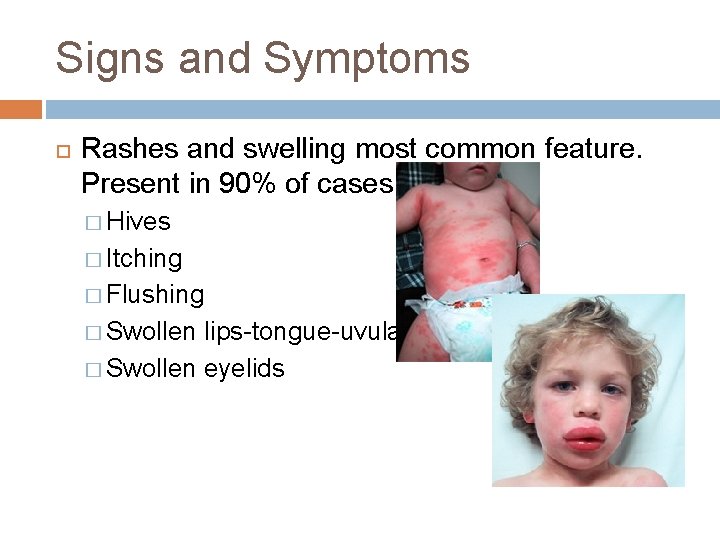
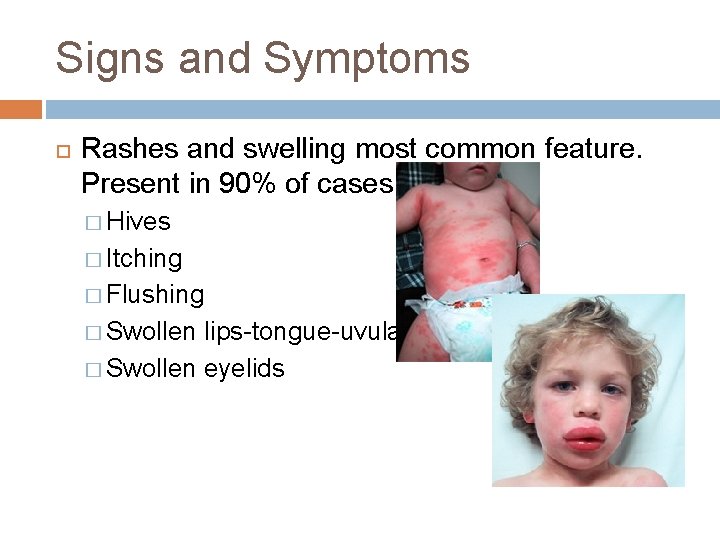
Signs and Symptoms Rashes and swelling most common feature. Present in 90% of cases. � Hives � Itching � Flushing � Swollen lips-tongue-uvula � Swollen eyelids
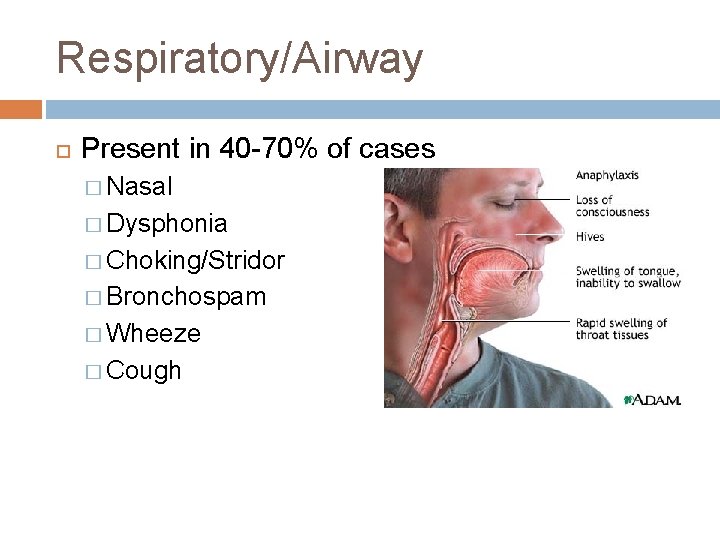
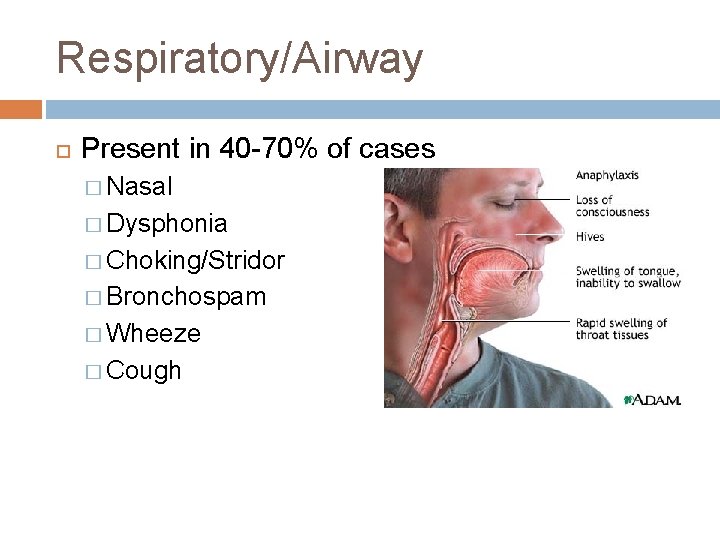
Respiratory/Airway Present in 40 -70% of cases � Nasal � Dysphonia � Choking/Stridor � Bronchospam � Wheeze � Cough
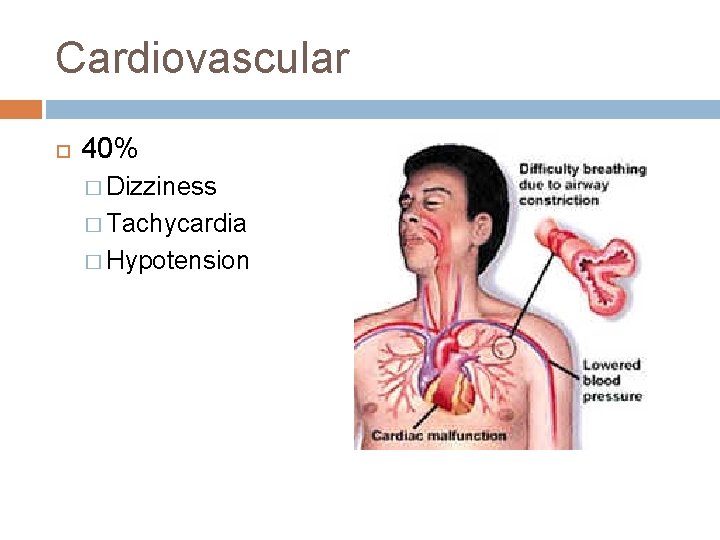
Cardiovascular 40% � Dizziness � Tachycardia � Hypotension
GI Symptoms 30 -40% of cases �Cramping �N/V �Diarrhea
Anaphylaxis Criteria 1 Skin or mucosal tissue involvement plus: Respiratory symptoms or Hypotension
Anaphylaxis Criteria 2 Any 2 of the below occuring rapidly after exposure to a likely allergen for that patient : � Rash or swelling � Respiratory compromise � Hypotension � Acute gastrointestinal symptoms
Anaphylaxis Criteria 3 Reduced BP after exposure to a known allergen
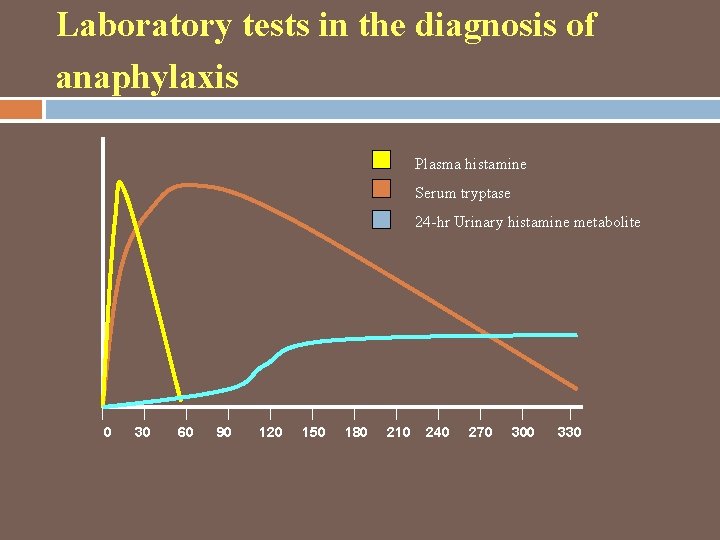
Laboratory Testing Serum tryptase � Draw 5 minutes to 3 hours of symptom onset. Plasma histamine � 5 to 15 minutes of the onset of anaphylaxis symptoms, gone by 1 hour after event � Tricky � Not usually performed
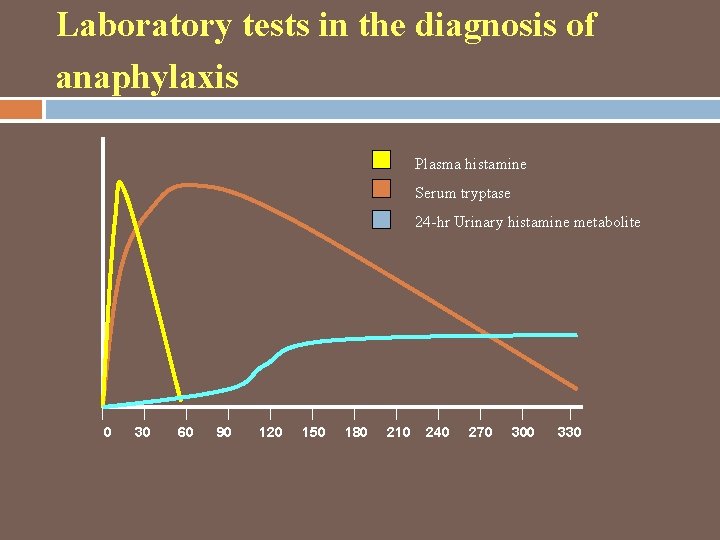
Laboratory tests in the diagnosis of anaphylaxis Plasma histamine Serum tryptase 24 -hr Urinary histamine metabolite 0 30 60 90 120 150 180 210 240 270 300 330
Causes of Ig. E-Mediated Anaphylaxis Foods � Shellfish, tree nuts, peanuts (adults) � Tree nuts, peanut, soy, cow’s milk, shellfish, finned fish, wheat (children), egg white Antibiotics and other medications � Beta lactams, sulfa, NMBs Foreign proteins � Latex, hymenoptera venoms, heterologous sera, protamine, seminal fluid, plasma
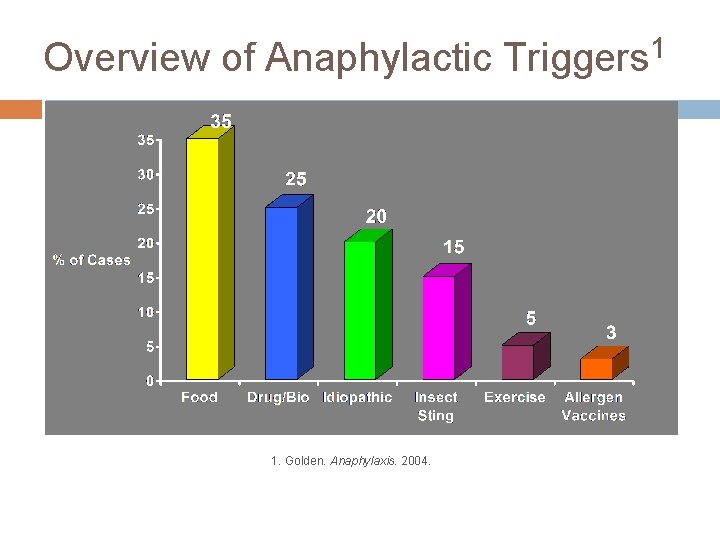
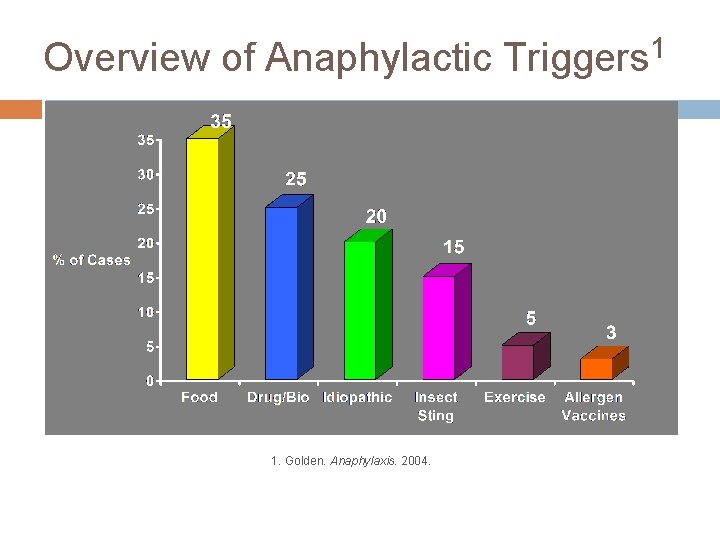
Overview of Anaphylactic Triggers 1 1. Golden. Anaphylaxis. 2004.
Non-Ig. E mediated anaphylaxis Formerly known as anaphylactoid reactions � Radiocontrast Media Many are direct mast cell degranulators � Opiates
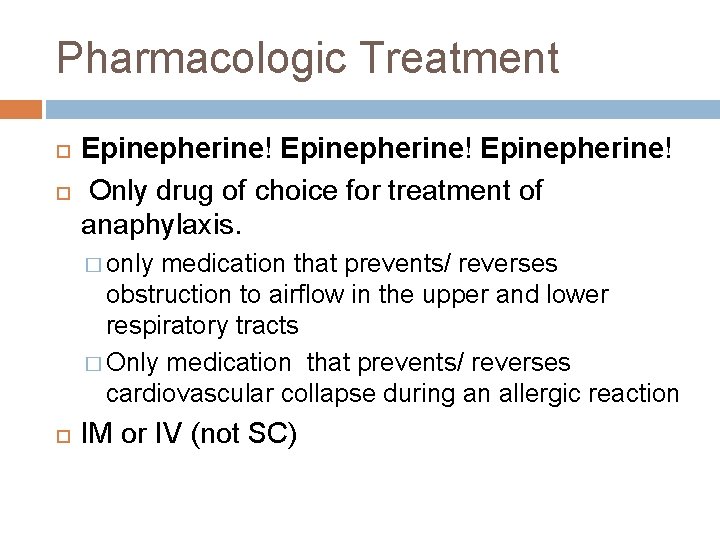
Pharmacologic Treatment Epinepherine! Only drug of choice for treatment of anaphylaxis. � only medication that prevents/ reverses obstruction to airflow in the upper and lower respiratory tracts � Only medication that prevents/ reverses cardiovascular collapse during an allergic reaction IM or IV (not SC)
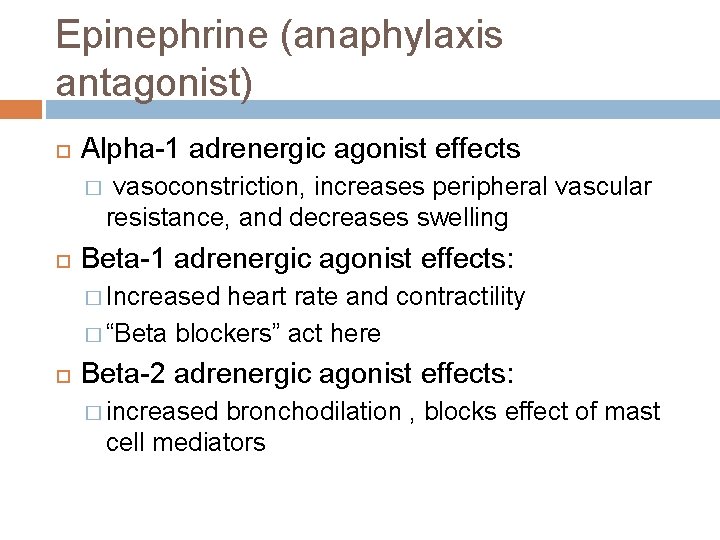
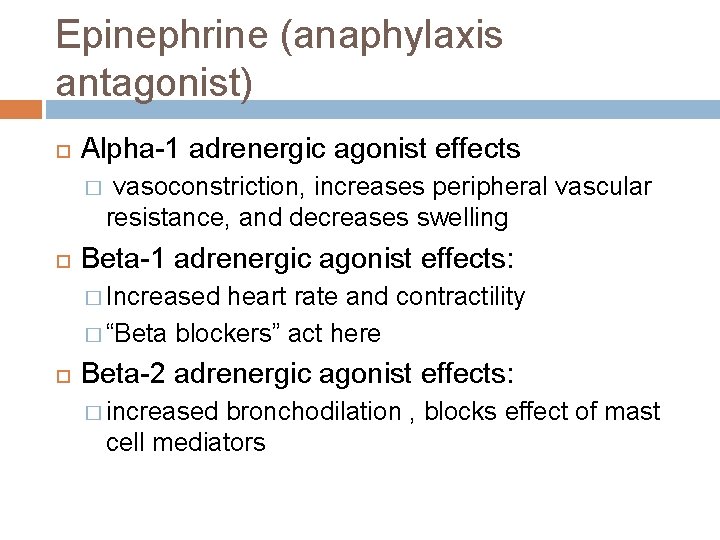
Epinephrine (anaphylaxis antagonist) Alpha-1 adrenergic agonist effects � vasoconstriction, increases peripheral vascular resistance, and decreases swelling Beta-1 adrenergic agonist effects: � Increased heart rate and contractility � “Beta blockers” act here Beta-2 adrenergic agonist effects: � increased bronchodilation , blocks effect of mast cell mediators
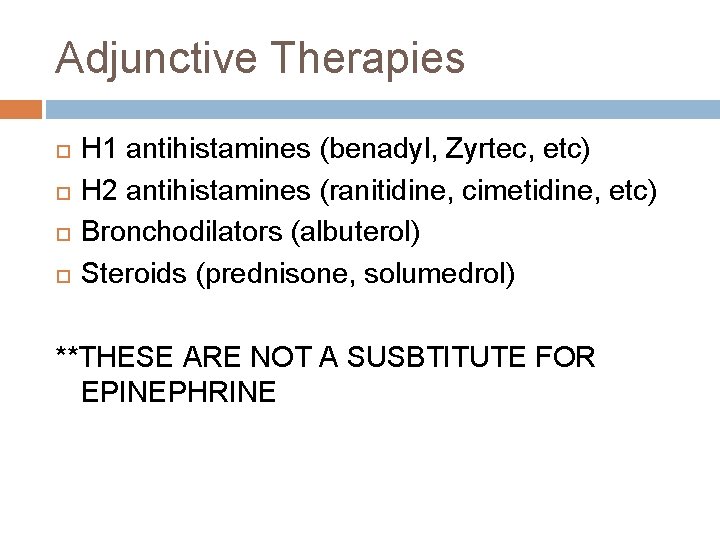
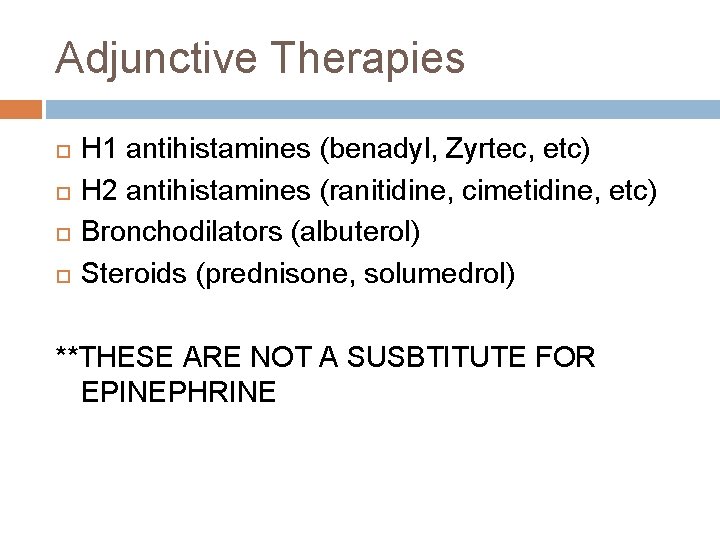
Adjunctive Therapies H 1 antihistamines (benadyl, Zyrtec, etc) H 2 antihistamines (ranitidine, cimetidine, etc) Bronchodilators (albuterol) Steroids (prednisone, solumedrol) **THESE ARE NOT A SUSBTITUTE FOR EPINEPHRINE
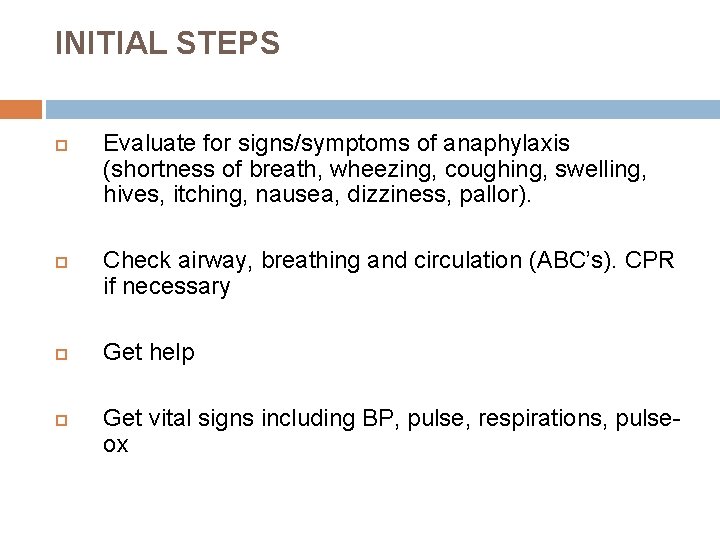
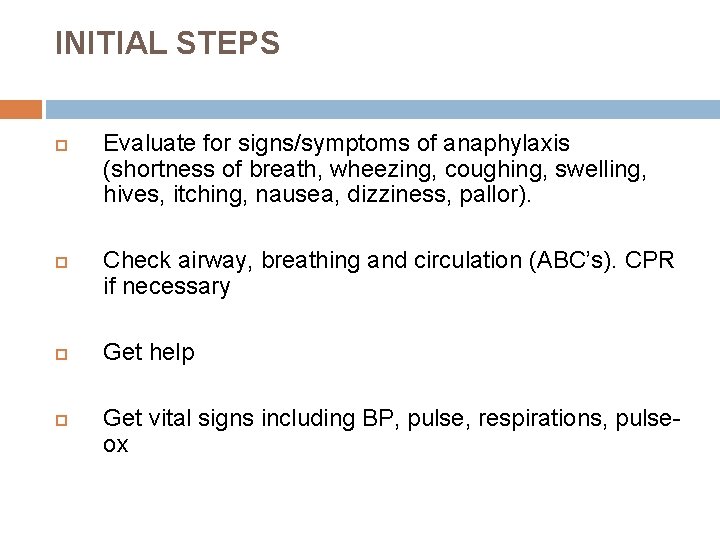
INITIAL STEPS Evaluate for signs/symptoms of anaphylaxis (shortness of breath, wheezing, coughing, swelling, hives, itching, nausea, dizziness, pallor). Check airway, breathing and circulation (ABC’s). CPR if necessary Get help Get vital signs including BP, pulse, respirations, pulseox
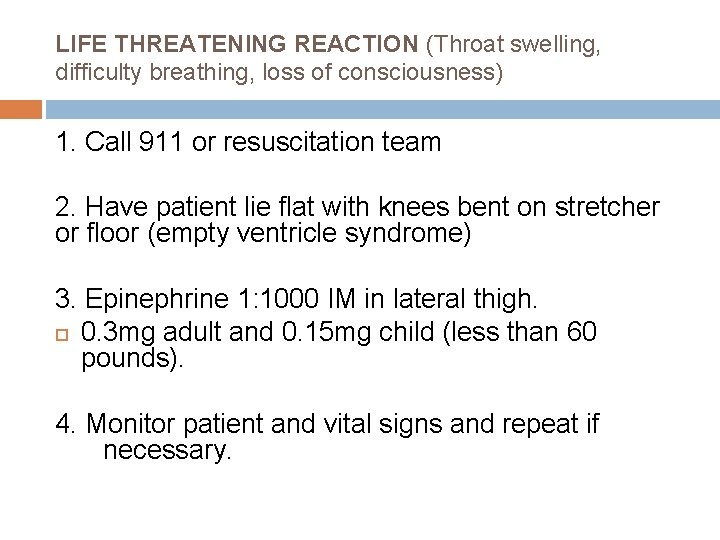
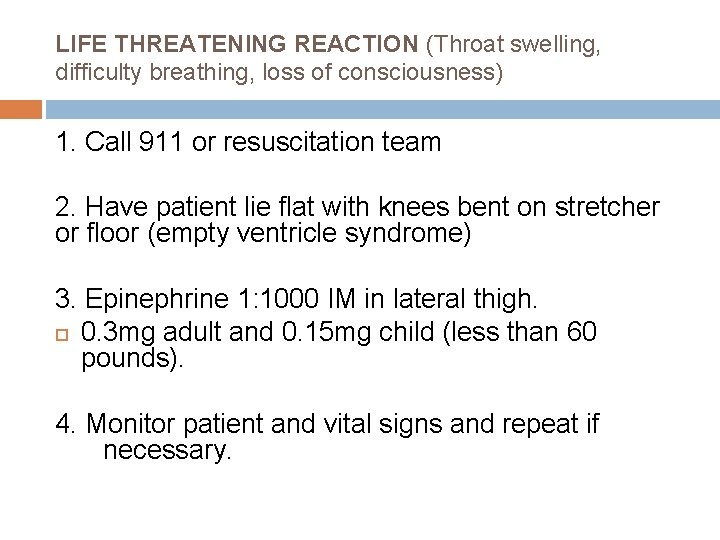
LIFE THREATENING REACTION (Throat swelling, difficulty breathing, loss of consciousness) 1. Call 911 or resuscitation team 2. Have patient lie flat with knees bent on stretcher or floor (empty ventricle syndrome) 3. Epinephrine 1: 1000 IM in lateral thigh. 0. 3 mg adult and 0. 15 mg child (less than 60 pounds). 4. Monitor patient and vital signs and repeat if necessary.
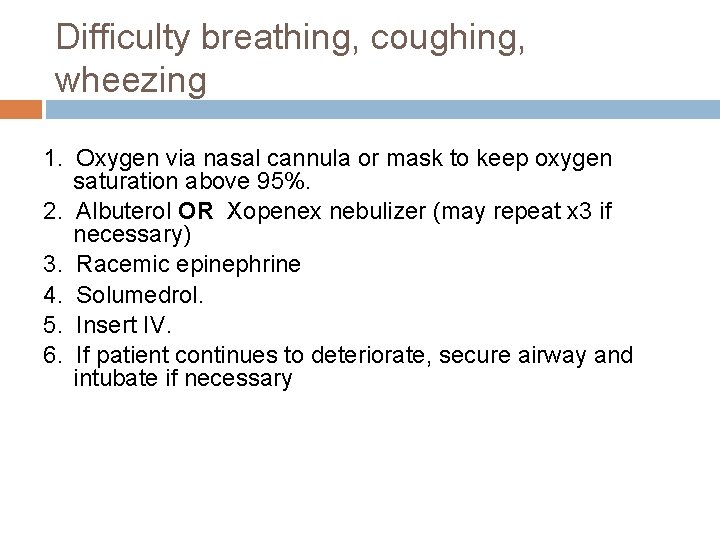
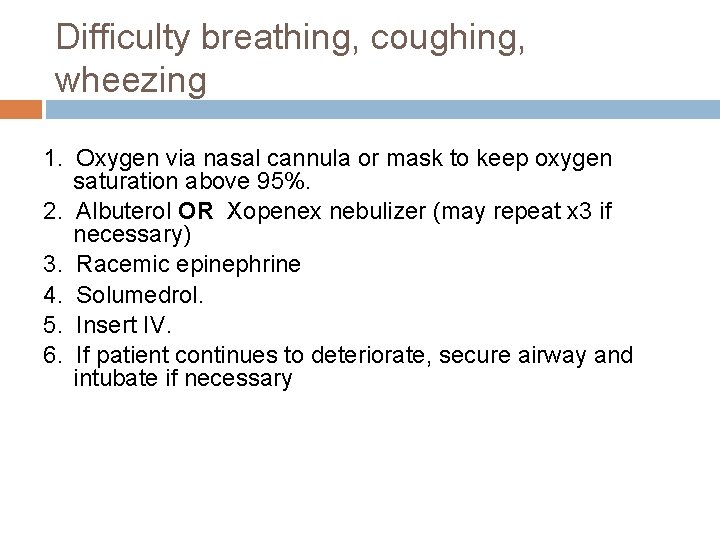
Difficulty breathing, coughing, wheezing 1. Oxygen via nasal cannula or mask to keep oxygen saturation above 95%. 2. Albuterol OR Xopenex nebulizer (may repeat x 3 if necessary) 3. Racemic epinephrine 4. Solumedrol. 5. Insert IV. 6. If patient continues to deteriorate, secure airway and intubate if necessary
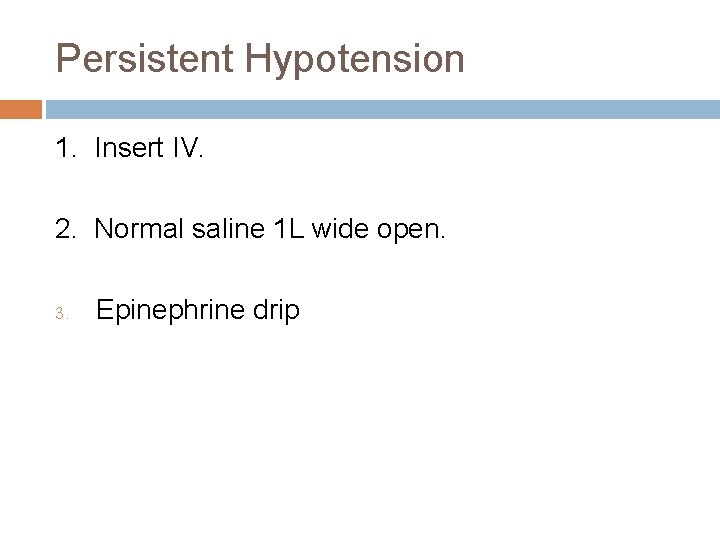
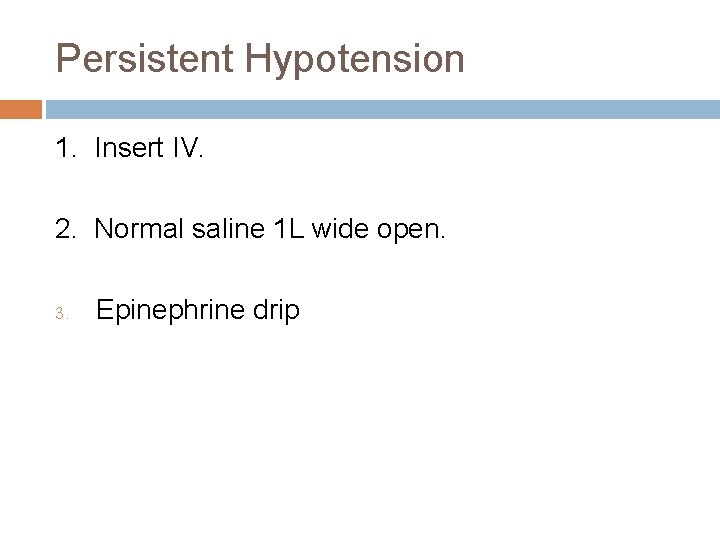
Persistent Hypotension 1. Insert IV. 2. Normal saline 1 L wide open. 3. Epinephrine drip
Bradycardia (HR less than 60) 1. Epinephrine 2. Atropine
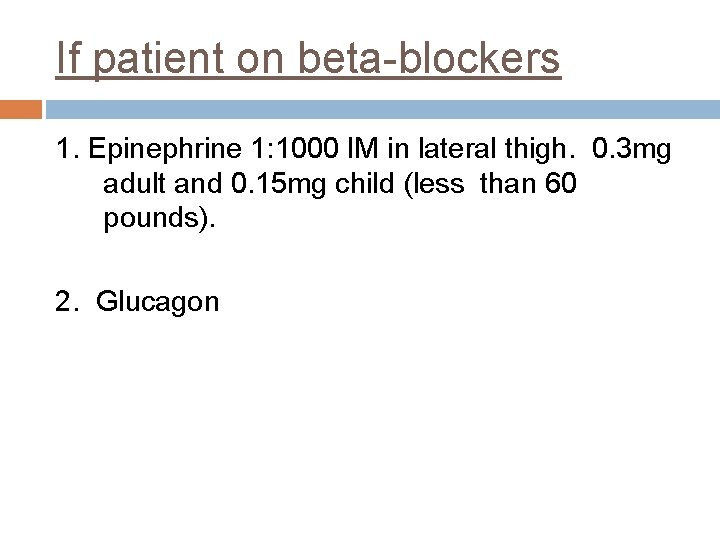
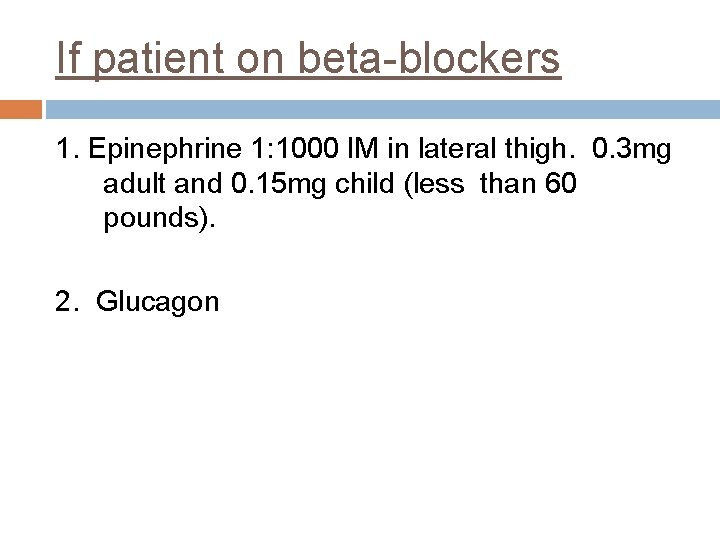
If patient on beta-blockers 1. Epinephrine 1: 1000 IM in lateral thigh. 0. 3 mg adult and 0. 15 mg child (less than 60 pounds). 2. Glucagon
Anaphylaxis Fatalities @ 4% Increased Risk � Rapid onset of symptoms, Delayed Epi, Beta Blockade, severe hypotension, bradycardia, sustained bronchospasm, poor response to epinephrine � Adrenal Insufficiency � Asthma � Coronary Artery Disease *Ref. Van der Klauw et al. Clin Exp Allergy 1996; 26: 1355 -1363.
What about heart disease? Healthy heart: mast cells are present throughout the myocardium � myocardial fibers, blood vessels, coronary artery intima. In CAD, mast cell number and density of cardiac mast cells is increased because mast cells are also present in atherosclerotic plaques, where they contribute to atherogenesis.
What about chronic CAD? Histamines + leukotrienes + platelet-activating factor and others can lead to coronary artery spasm. 1 anaphylaxis itself can cause vasospasm, arrhythmias, and myocardial infarction in patients, including children, with healthy hearts. Triggiani M, Patella V, Staiano RI, Granata F, Marone G. Allergy and the cardiovascular system. Clin Exp Immunol. 2008; 153(suppl 1): 7– 11
Epi: No absolute contraindications Risk of death or disability from ischemic encephalopathy due to inadequately treated anaphylaxis usually outweighs other concerns Existing evidence clearly favors the benefit of epinephrine administration in anaphylaxis. Sound clinical judgment is essential.
Long Term Management Identification of culprit and cross reactants Strict avoidance Epinephrine auto-injector
ANAPHYLAXIS: KNOW IT WHEN YOU SEE IT ! …and make Justice Potter Stewart proud!
References The diagnosis and management of anaphylaxis: A practice parameter. 2010 Update. J Allergy Clin Immunol. 2010; 126: 477 -80. Drug Allergy: An Updated Practice Parameter. Ann Allergy, Asthma & Immunol. 2010; 105. Grammer LC, Greenberger PA. Patterson’s Allergic Disease. 2009; 7 th edition.

Thanks! Questions? ? ? Office number: (904) 730 -4870 tomlupoli@gmail. com
 Anaphylaxis treatment
Anaphylaxis treatment Anaphylaxis treatment
Anaphylaxis treatment Neuhaus rapid word recognition chart
Neuhaus rapid word recognition chart Fcps and mrcp
Fcps and mrcp Shawn lupoli umbc
Shawn lupoli umbc Arduino leonardo lcd
Arduino leonardo lcd Primitivo lupoli
Primitivo lupoli Shawn lupoli
Shawn lupoli Nbestbuy
Nbestbuy Hypersensitivity types and examples
Hypersensitivity types and examples Anaphylaxis onset
Anaphylaxis onset Ig
Ig Anaphylaxis
Anaphylaxis Causes of anaphylactic reaction
Causes of anaphylactic reaction Brighton collaboration level 1
Brighton collaboration level 1 How to draw up epinephrine
How to draw up epinephrine Epinephrine dosage emt
Epinephrine dosage emt Nap anaphylaxis
Nap anaphylaxis Reaction
Reaction Angioedema anaphylaxis
Angioedema anaphylaxis Allergist delta dental
Allergist delta dental Anaphlaxis
Anaphlaxis Anaphylaxis
Anaphylaxis Anaphylatoxins
Anaphylatoxins Anaphylaxis photos
Anaphylaxis photos Interprofessional care for anaphylaxis
Interprofessional care for anaphylaxis Pathologist and anthropologist
Pathologist and anthropologist Suspected cancer recognition and referral
Suspected cancer recognition and referral Julia speech recognition
Julia speech recognition Kinect for windows runtime
Kinect for windows runtime Pdf text recognition
Pdf text recognition Recognition heuristic
Recognition heuristic Logo for certificate of appreciation
Logo for certificate of appreciation Exploring self-attention for image recognition
Exploring self-attention for image recognition Problem recognition adalah
Problem recognition adalah Paul hrycewicz
Paul hrycewicz Electron speech recognition
Electron speech recognition Object detection matlab
Object detection matlab Wow employee recognition program
Wow employee recognition program Fuzzy logic in pattern recognition
Fuzzy logic in pattern recognition Convolutional neural networks for visual recognition
Convolutional neural networks for visual recognition Amichai painsky
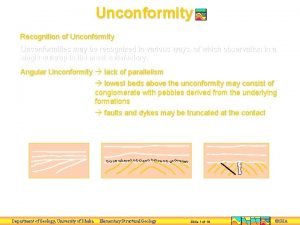
Amichai painsky Recognition of unconformity
Recognition of unconformity Face recognition
Face recognition Ann kruse pwc
Ann kruse pwc Htk speech recognition tutorial
Htk speech recognition tutorial Ros object recognition
Ros object recognition Praise, recognition and power are_______.
Praise, recognition and power are_______. Recognition and regard for oneself and one's abilities: *
Recognition and regard for oneself and one's abilities: *