Anaphylaxis Rapid recognition and treatment DR jarahzadeh Intensivist













- Slides: 53

Anaphylaxis Rapid recognition and treatment DR jarahzadeh Intensivist
ANAPHYLAXIS In a few seconds it was extremely ill; breathing became distressful and panting; it could scarcely drag itself along, lay on its side, was seized with diarrhea, vomited blood and died in twenty five minutes. Charles Richet 1902
ANAPHYLAXIS Instead of inducing tolerance ( prophylaxis), Richet’s experiments in dogs injected with sea anemone toxin resulted in lethal responses to doses previously tolerated. He coined the word ‘ana’ (without) ‘phylaxis (protection). He won the Nobel prize for this work.
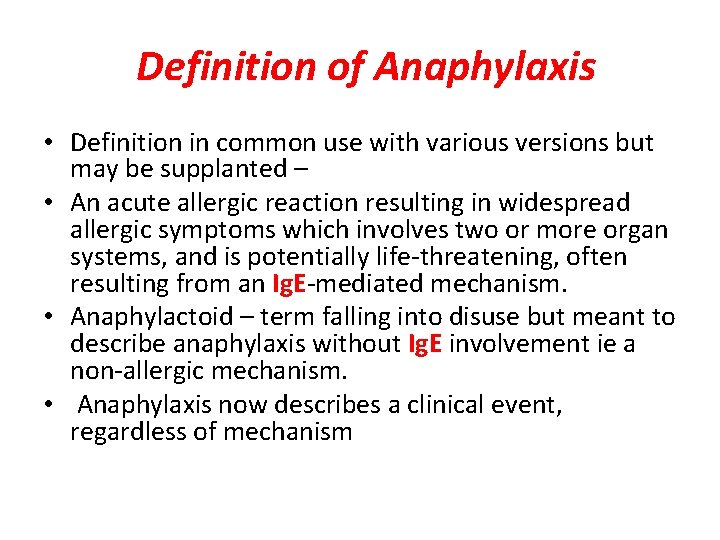
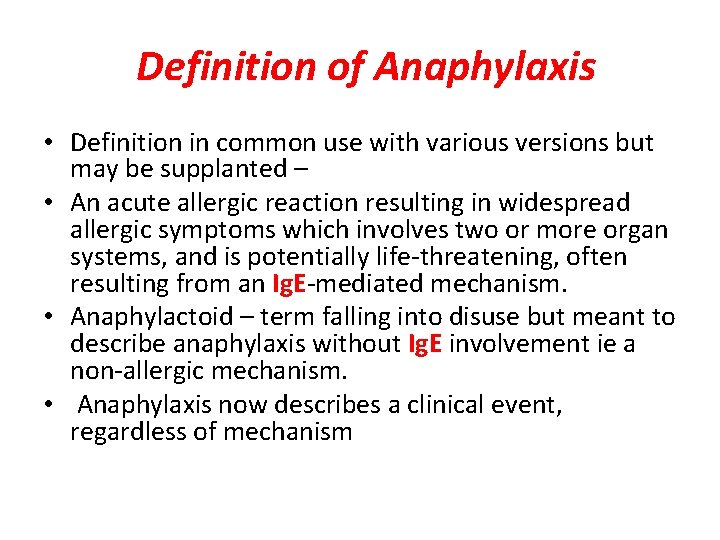
Definition of Anaphylaxis • Definition in common use with various versions but may be supplanted – • An acute allergic reaction resulting in widespread allergic symptoms which involves two or more organ systems, and is potentially life-threatening, often resulting from an Ig. E-mediated mechanism. • Anaphylactoid – term falling into disuse but meant to describe anaphylaxis without Ig. E involvement ie a non-allergic mechanism. • Anaphylaxis now describes a clinical event, regardless of mechanism
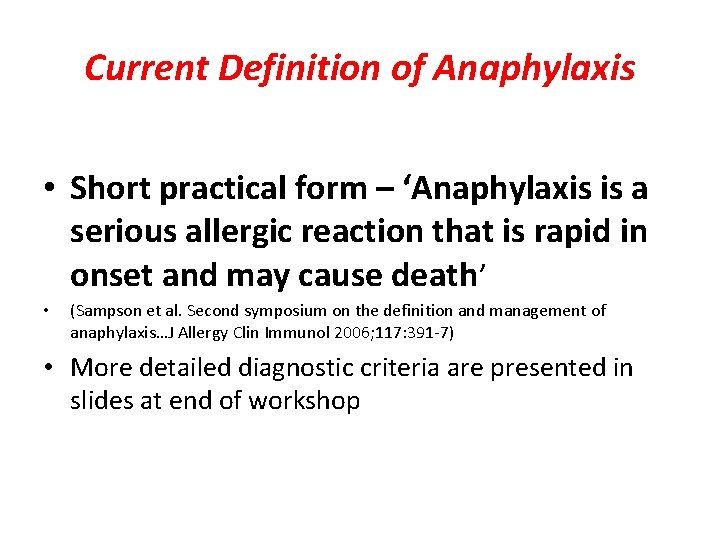
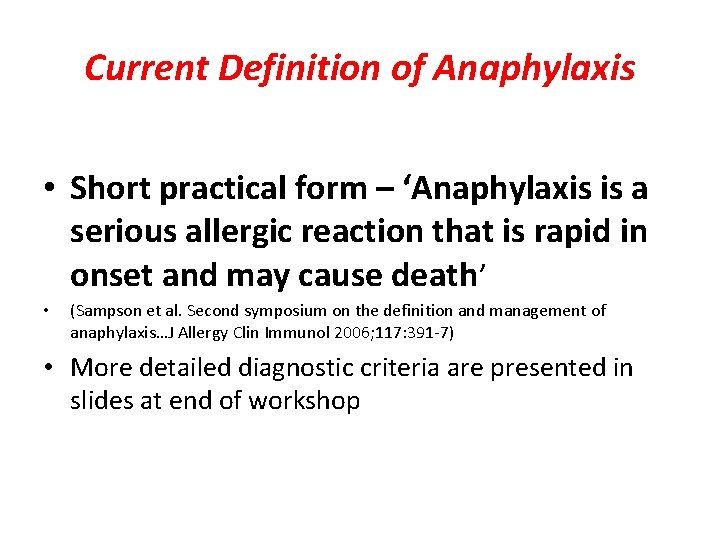
Current Definition of Anaphylaxis • Short practical form – ‘Anaphylaxis is a serious allergic reaction that is rapid in onset and may cause death’ • (Sampson et al. Second symposium on the definition and management of anaphylaxis…J Allergy Clin Immunol 2006; 117: 391 -7) • More detailed diagnostic criteria are presented in slides at end of workshop

Anaphylaxis is highly likely when any ONE of the following 3 criteria is fulfilled: 1. Acute onset of an illness (minutes to several hours) with involvement of the skin, mucosal tissue, or both (eg, generalized hives, pruritus or flushing, swollen lips-tongue-uvula) AND AT LEAST ONE OF THE FOLLOWING A. Respiratory compromise (eg, dyspnea, wheeze-bronchospasm, reduced PEF in older children and adults, stridor, hypoxemia) B. Reduced BP* or associated symptoms of end-organ dysfunction (eg, hypotonia, collapse, syncope, incontinence)
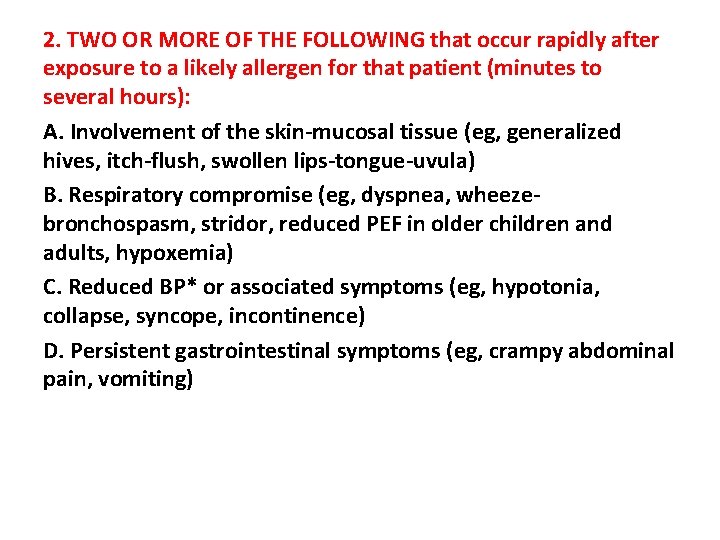
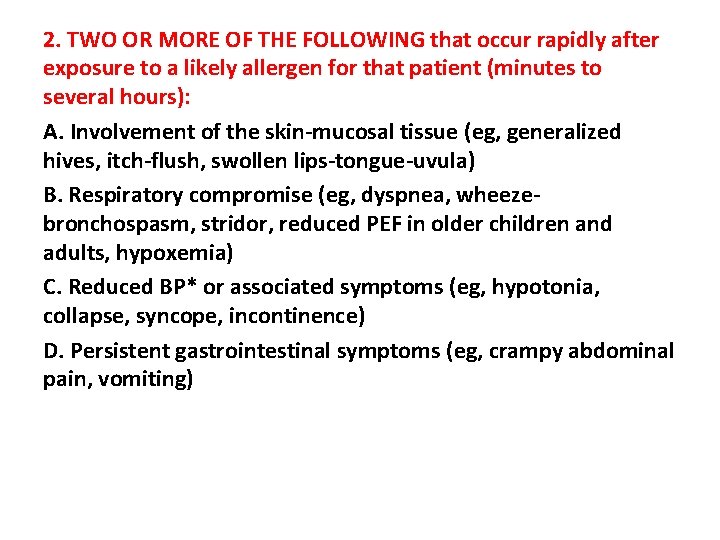
2. TWO OR MORE OF THE FOLLOWING that occur rapidly after exposure to a likely allergen for that patient (minutes to several hours): A. Involvement of the skin-mucosal tissue (eg, generalized hives, itch-flush, swollen lips-tongue-uvula) B. Respiratory compromise (eg, dyspnea, wheezebronchospasm, stridor, reduced PEF in older children and adults, hypoxemia) C. Reduced BP* or associated symptoms (eg, hypotonia, collapse, syncope, incontinence) D. Persistent gastrointestinal symptoms (eg, crampy abdominal pain, vomiting)
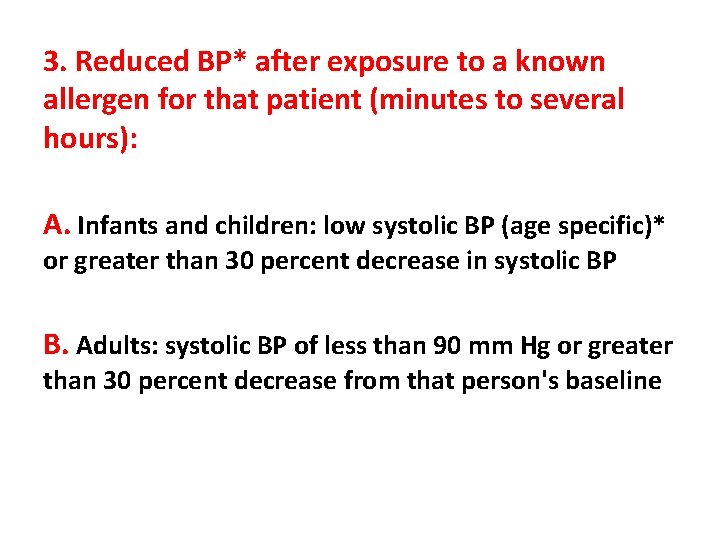
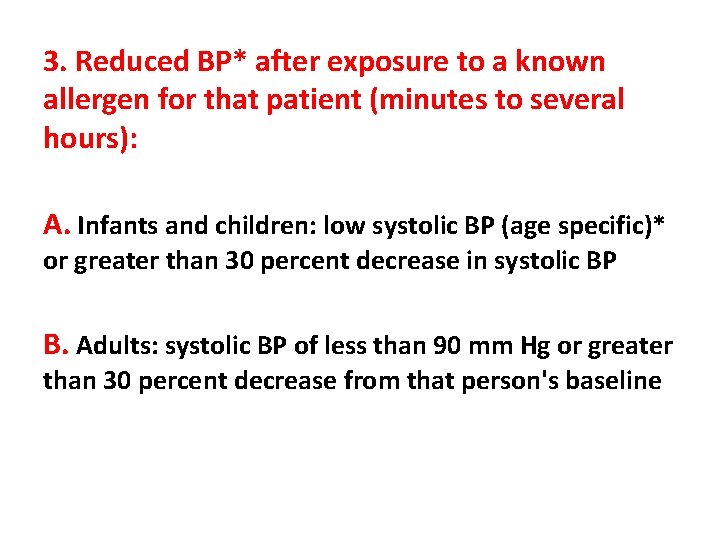
3. Reduced BP* after exposure to a known allergen for that patient (minutes to several hours): A. Infants and children: low systolic BP (age specific)* or greater than 30 percent decrease in systolic BP B. Adults: systolic BP of less than 90 mm Hg or greater than 30 percent decrease from that person's baseline
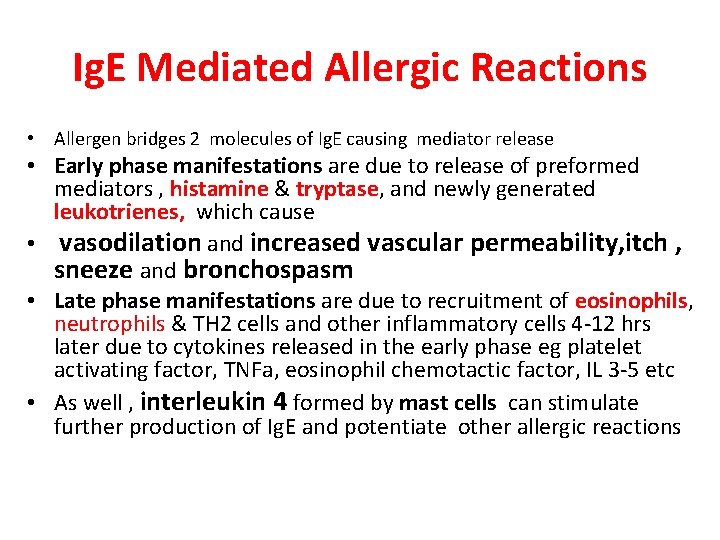
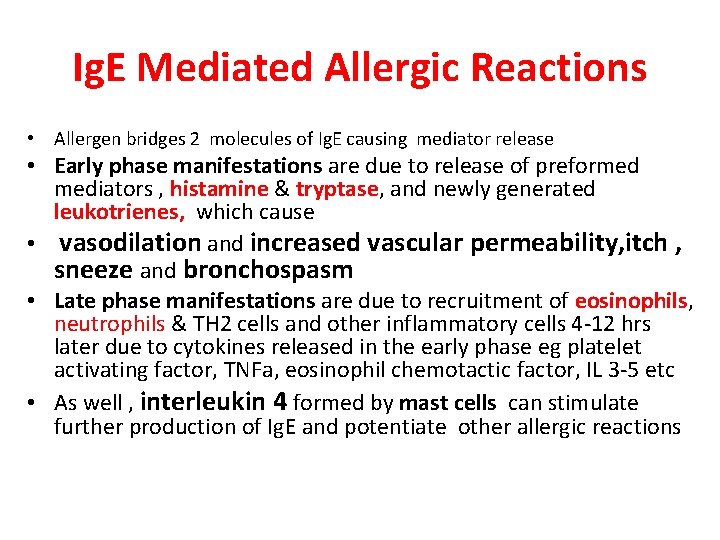
Ig. E Mediated Allergic Reactions • Allergen bridges 2 molecules of Ig. E causing mediator release • Early phase manifestations are due to release of preformed mediators , histamine & tryptase, and newly generated leukotrienes, which cause • vasodilation and increased vascular permeability, itch , sneeze and bronchospasm • Late phase manifestations are due to recruitment of eosinophils, neutrophils & TH 2 cells and other inflammatory cells 4 -12 hrs later due to cytokines released in the early phase eg platelet activating factor, TNFa, eosinophil chemotactic factor, IL 3 -5 etc • As well , interleukin 4 formed by mast cells can stimulate further production of Ig. E and potentiate other allergic reactions
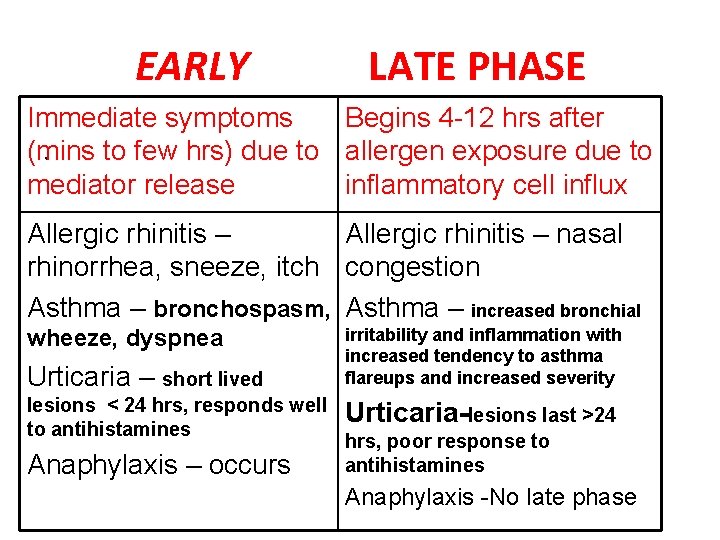
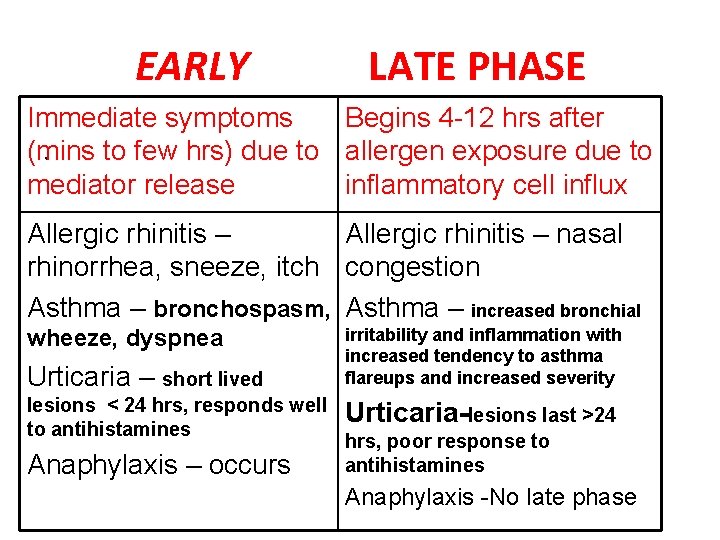
EARLY LATE PHASE Immediate symptoms Begins 4 -12 hrs after. (mins to few hrs) due to allergen exposure due to mediator release inflammatory cell influx Allergic rhinitis – nasal rhinorrhea, sneeze, itch congestion Asthma – bronchospasm, Asthma – increased bronchial wheeze, dyspnea Urticaria – short lived lesions < 24 hrs, responds well to antihistamines Anaphylaxis – occurs irritability and inflammation with increased tendency to asthma flareups and increased severity Urticaria-lesions last >24 hrs, poor response to antihistamines Anaphylaxis -No late phase
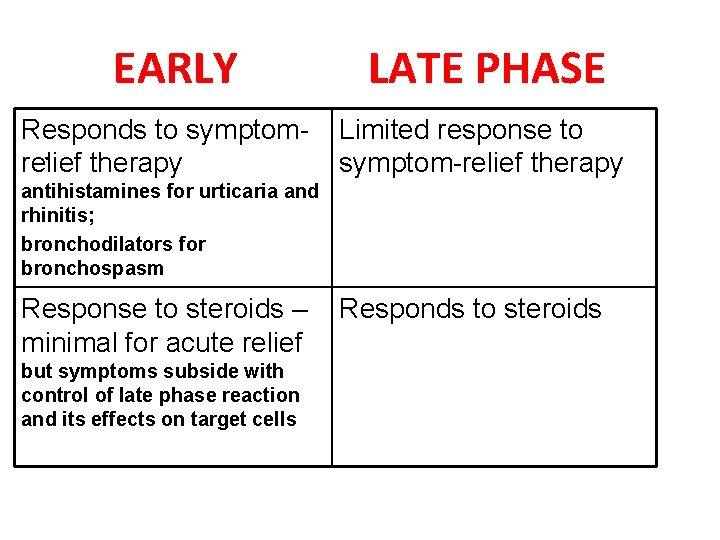
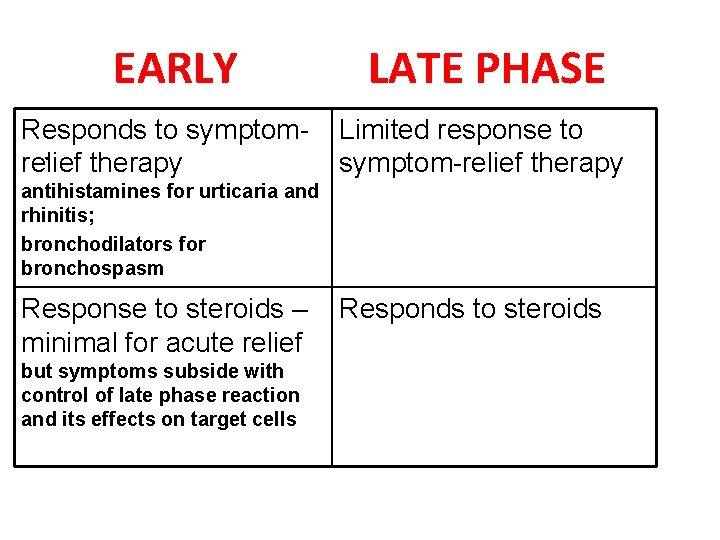
EARLY Responds to symptom. relief therapy LATE PHASE Limited response to symptom-relief therapy antihistamines for urticaria and rhinitis; bronchodilators for bronchospasm Response to steroids – minimal for acute relief but symptoms subside with control of late phase reaction and its effects on target cells Responds to steroids
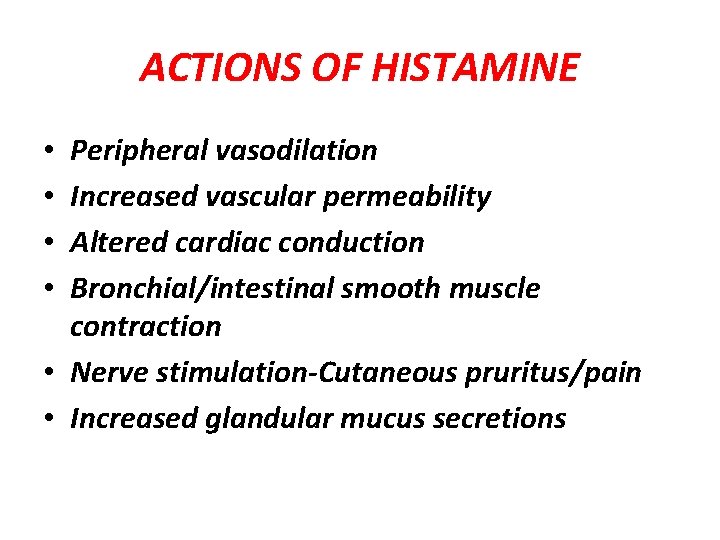
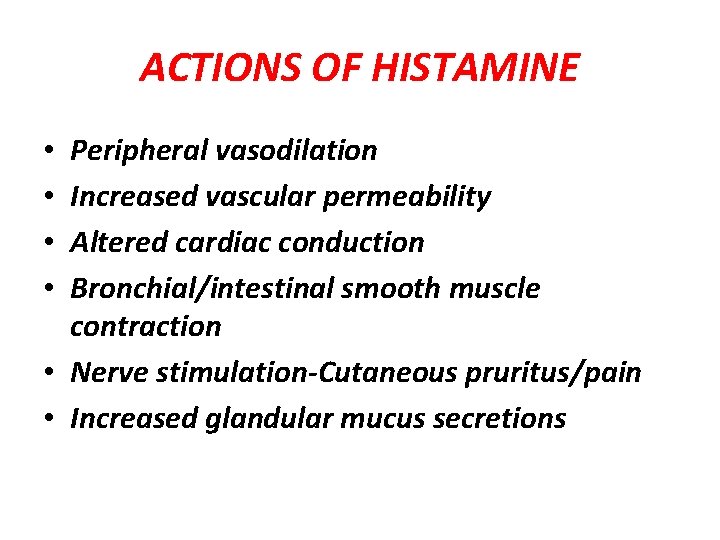
ACTIONS OF HISTAMINE Peripheral vasodilation Increased vascular permeability Altered cardiac conduction Bronchial/intestinal smooth muscle contraction • Nerve stimulation-Cutaneous pruritus/pain • Increased glandular mucus secretions • •
CLINICAL MANIFESTATIONS OF ALLERGY • Knowing the actions of histamine and other mediators , what would you predict to be the clinical effects on the body?
CLINICAL MANIFESTATIONS OF ALLERGY • Vasodilation – erythema, nasal congeston, hypotension, anaphylaxis • Increased vascular permeability – urticaria, hypotension, anaphylaxis • Smooth muscle spasm – asthma, intestinal cramps, diarrhea, anaphylaxis • Mucus secretion – allergic rhinitis, asthma • Nerve stimulation-itch, sneeze
URTICARIA Raised central white or red wheals Surrounding erythema or flare, with itch or burning Histamine mediated Varies in shape & size – circular, gyrate, linear, isolated or coalescent • Well demarcated, blanch with pressure • Predisposition to warm areas, pressure sites • Lasts hours, max 24 - 48 • •

ANGIOEDEMA • Diffuse skin colored subcutaneous swelling • Pathology similar to urticaria except it occurs in deeper subcutaneous tissues • Not itchy or painful, unless in confined site • Can be histamine, bradykinin etc mediated • Can last hours or days • Not very responsive to antihistamines • Often found in 40% of urticaria cases

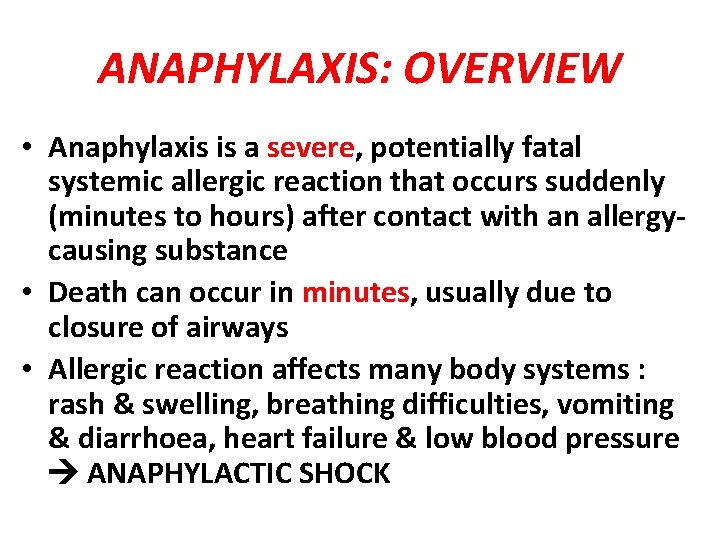
ANAPHYLAXIS: OVERVIEW • Anaphylaxis is a severe, potentially fatal systemic allergic reaction that occurs suddenly (minutes to hours) after contact with an allergycausing substance • Death can occur in minutes, usually due to closure of airways • Allergic reaction affects many body systems : rash & swelling, breathing difficulties, vomiting & diarrhoea, heart failure & low blood pressure ANAPHYLACTIC SHOCK

Anaphylaxis: Rapid recognition and treatment

Fatal anaphylaxis Minutes to cardiac arrest Median Range 55 iatrogenic 5 1 – 80 37 food 30 6 – 360 32 venom 15 4 – 120 Pumphrey RSH, Clinical and experimental allergy, 2000
Anaphylaxis: Rapid recognition and treatment
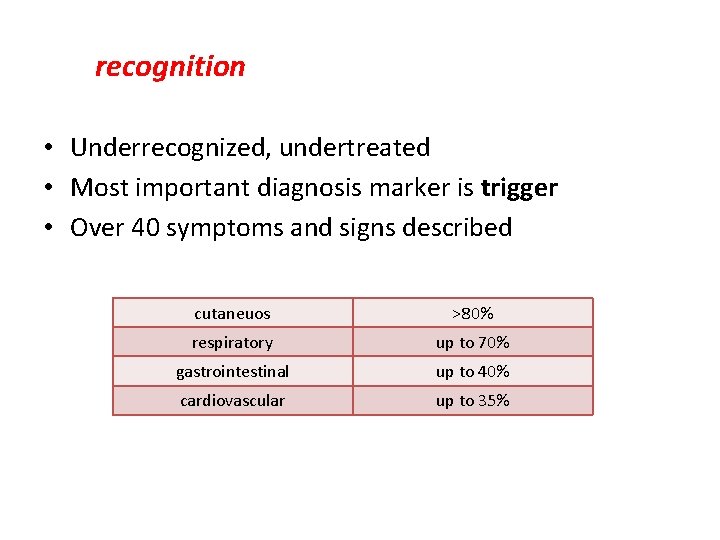
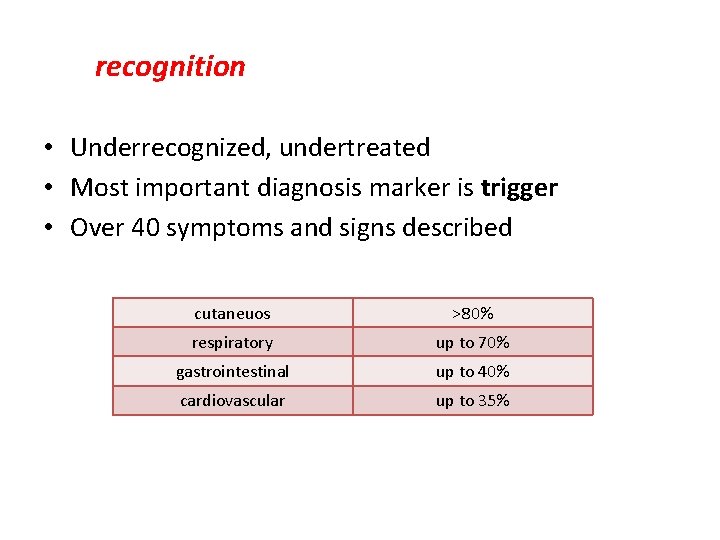
recognition • Underrecognized, undertreated • Most important diagnosis marker is trigger • Over 40 symptoms and signs described cutaneuos >80% respiratory up to 70% gastrointestinal up to 40% cardiovascular up to 35%

CLINICAL MANIFESTATIONS OF ANAPHYLAXIS • SKIN- urticaria, angioedema, pruritus, erythema • RESPIRATORY- rhinitis, conjunctivitis, cough, dyspnea, wheeze, stridor, voice change • GI – throat swelling or tightness, dysphagia, vomiting, diarrhea, cramps • CVS – hypotension, dizziness, syncope, cyanosis, secondary myocardial infarction • CNS –hypoxic seizures
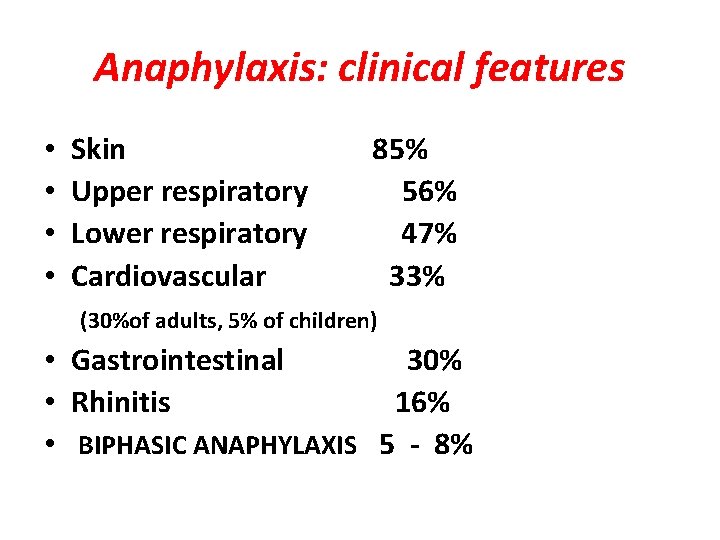
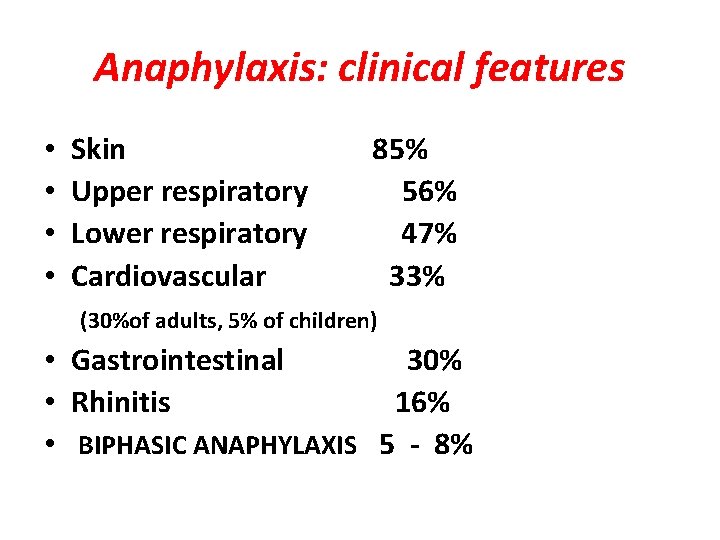
Anaphylaxis: clinical features • • Skin Upper respiratory Lower respiratory Cardiovascular 85% 56% 47% 33% (30%of adults, 5% of children) • Gastrointestinal 30% • Rhinitis 16% • BIPHASIC ANAPHYLAXIS 5 - 8%
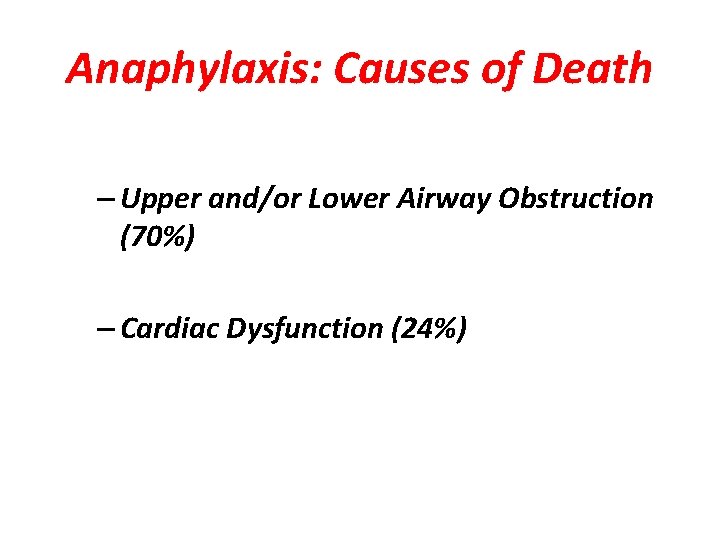
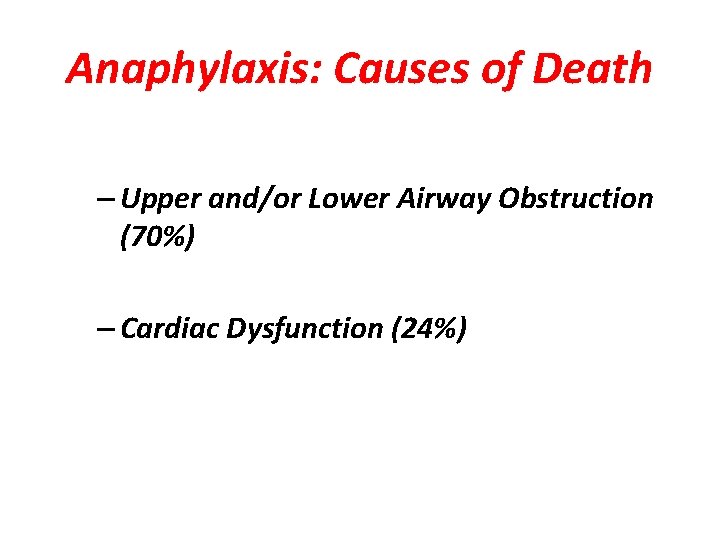
Anaphylaxis: Causes of Death – Upper and/or Lower Airway Obstruction (70%) – Cardiac Dysfunction (24%)
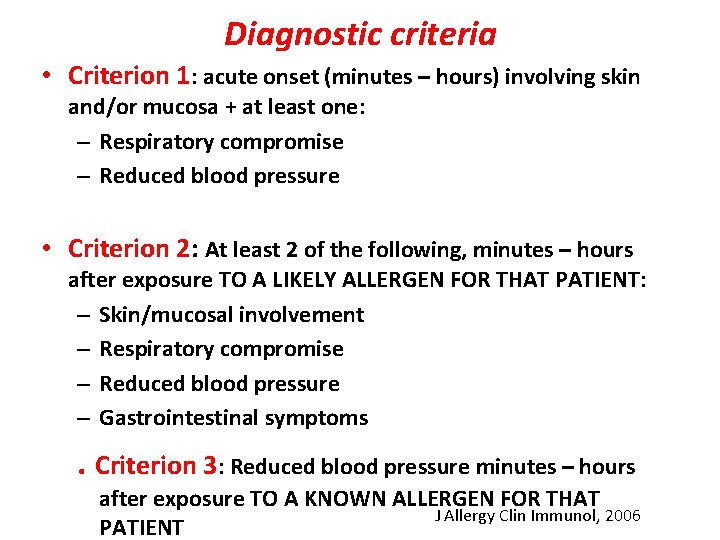
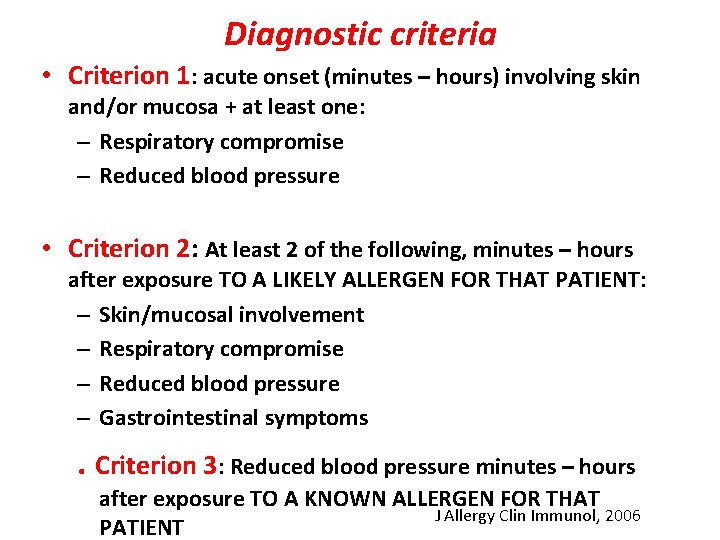
Diagnostic criteria • Criterion 1: acute onset (minutes – hours) involving skin and/or mucosa + at least one: – Respiratory compromise – Reduced blood pressure • Criterion 2: At least 2 of the following, minutes – hours after exposure TO A LIKELY ALLERGEN FOR THAT PATIENT: – Skin/mucosal involvement – Respiratory compromise – Reduced blood pressure – Gastrointestinal symptoms . Criterion 3: Reduced blood pressure minutes – hours after exposure TO A KNOWN ALLERGEN FOR THAT J Allergy Clin Immunol, 2006 PATIENT
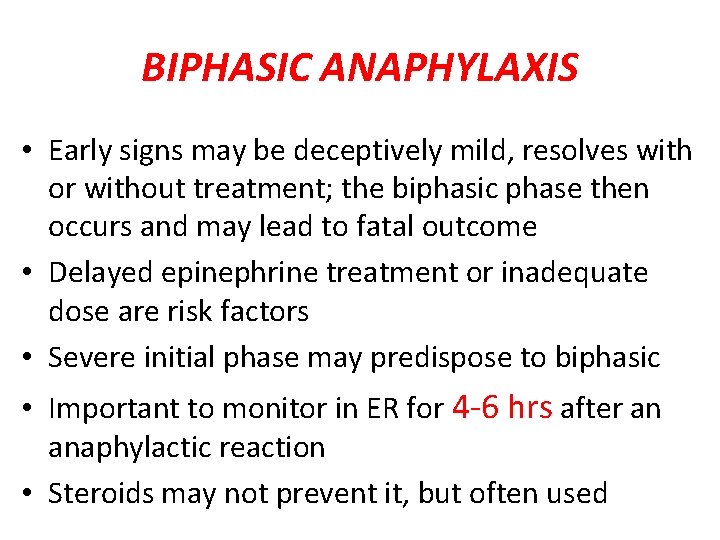
BIPHASIC ANAPHYLAXIS What is the importance?
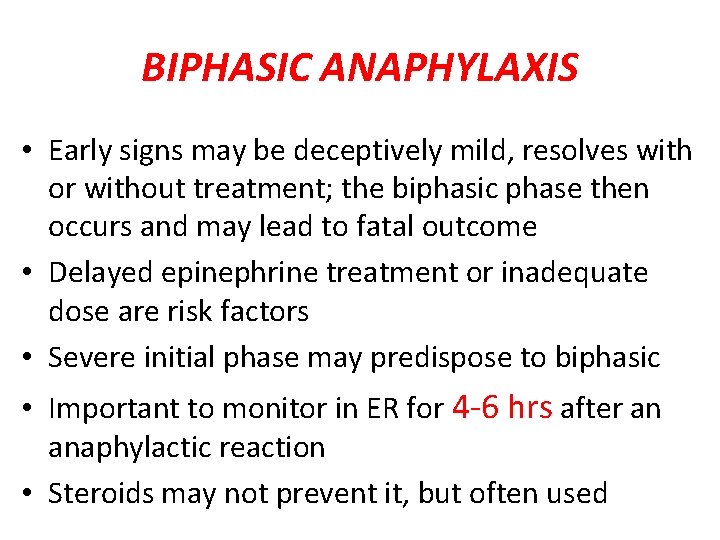
BIPHASIC ANAPHYLAXIS • Early signs may be deceptively mild, resolves with or without treatment; the biphasic phase then occurs and may lead to fatal outcome • Delayed epinephrine treatment or inadequate dose are risk factors • Severe initial phase may predispose to biphasic • Important to monitor in ER for 4 -6 hrs after an anaphylactic reaction • Steroids may not prevent it, but often used

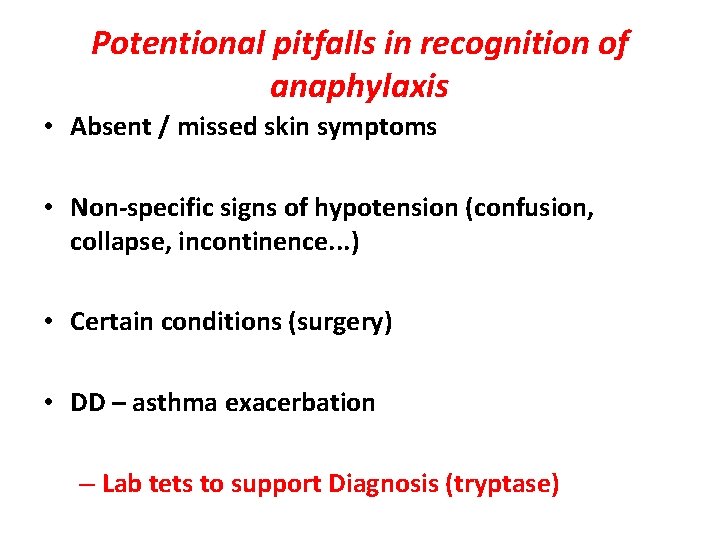
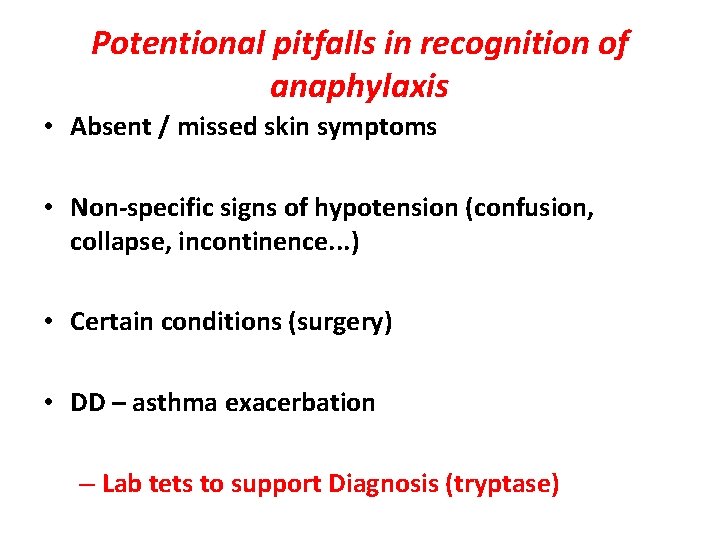
Potentional pitfalls in recognition of anaphylaxis • Absent / missed skin symptoms • Non-specific signs of hypotension (confusion, collapse, incontinence. . . ) • Certain conditions (surgery) • DD – asthma exacerbation – Lab tets to support Diagnosis (tryptase)
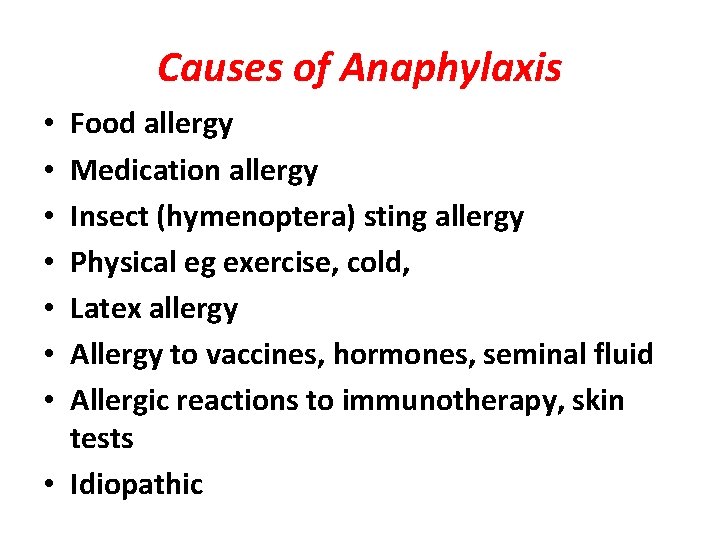
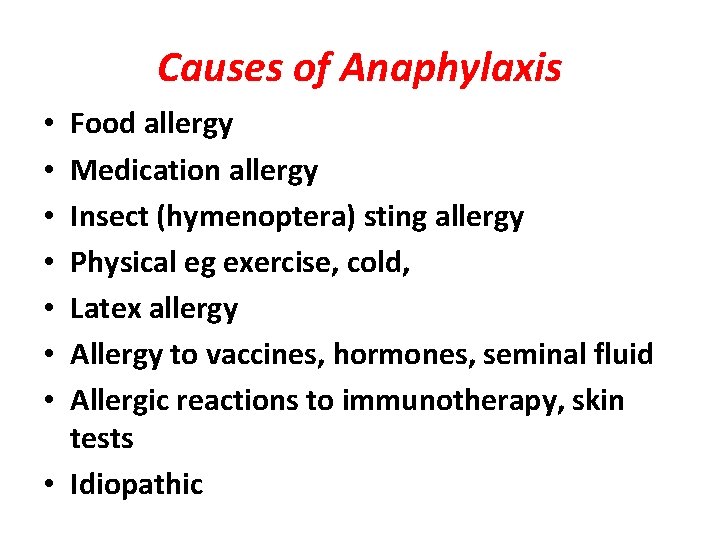
Causes of Anaphylaxis Food allergy Medication allergy Insect (hymenoptera) sting allergy Physical eg exercise, cold, Latex allergy Allergy to vaccines, hormones, seminal fluid Allergic reactions to immunotherapy, skin tests • Idiopathic • •
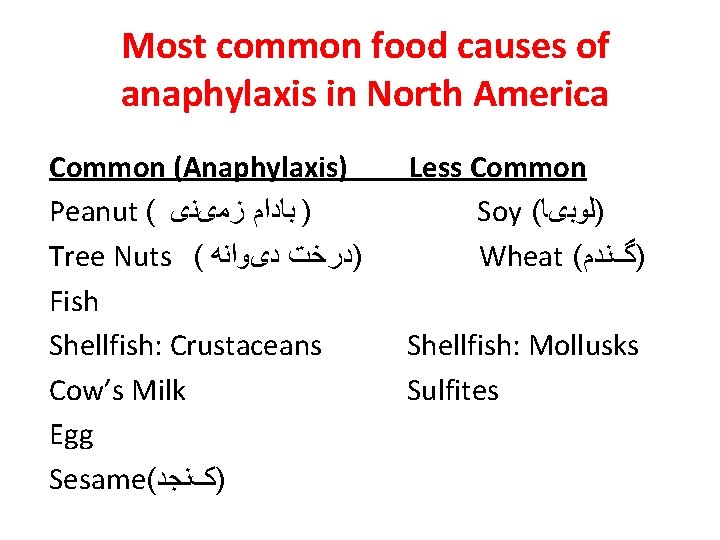
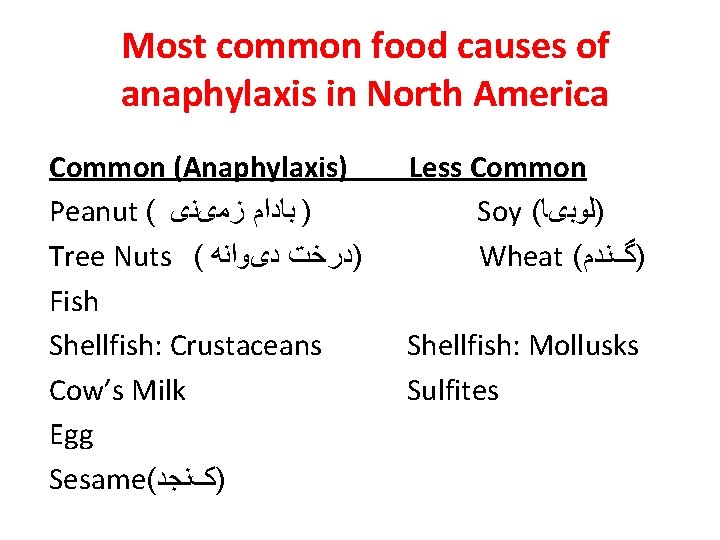
Most common food causes of anaphylaxis in North America Common (Anaphylaxis) Peanut ( ) ﺑﺎﺩﺍﻡ ﺯﻣیﻨی Tree Nuts ( )ﺩﺭﺧﺖ ﺩیﻮﺍﻧﻪ Fish Shellfish: Crustaceans Cow’s Milk Egg Sesame( )کﻨﺠﺪ Less Common Soy ( )ﻟﻮﺑیﺎ Wheat ( )گﻨﺪﻡ Shellfish: Mollusks Sulfites
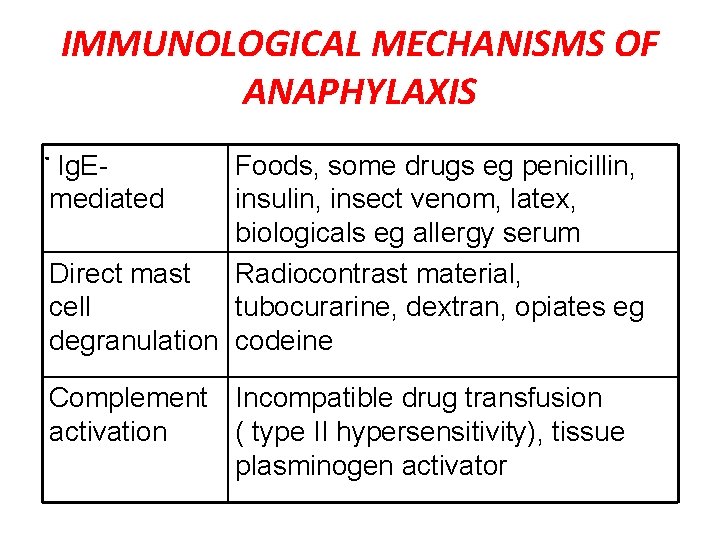
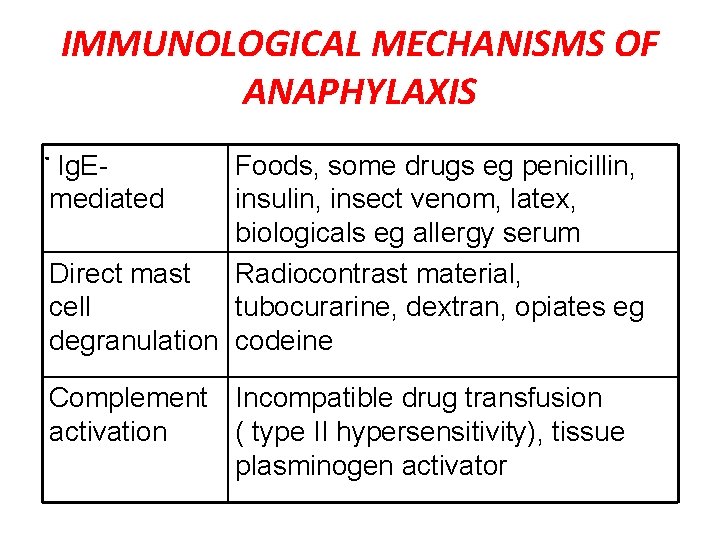
IMMUNOLOGICAL MECHANISMS OF ANAPHYLAXIS. Ig. E- Foods, some drugs eg penicillin, mediated insulin, insect venom, latex, biologicals eg allergy serum Direct mast Radiocontrast material, cell tubocurarine, dextran, opiates eg degranulation codeine Complement Incompatible drug transfusion activation ( type II hypersensitivity), tissue plasminogen activator
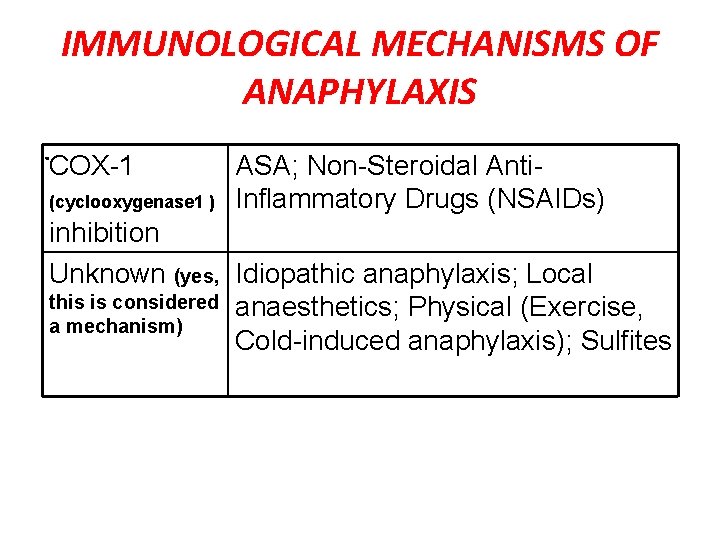
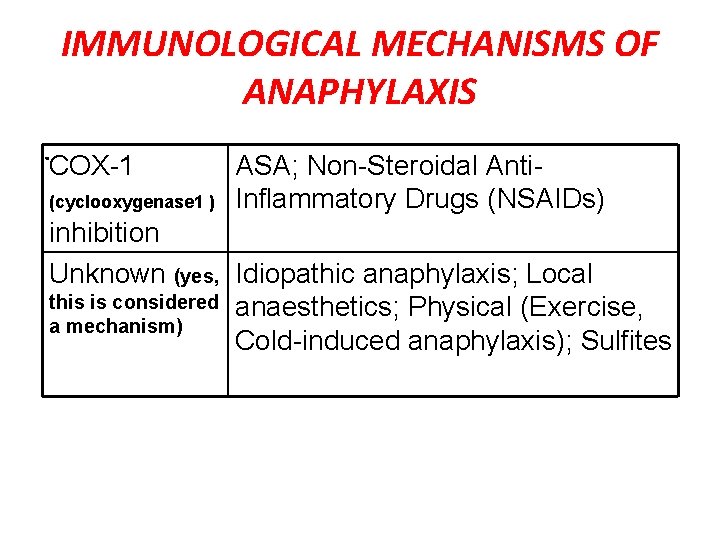
IMMUNOLOGICAL MECHANISMS OF ANAPHYLAXIS. COX-1 (cyclooxygenase 1 ) ASA; Non-Steroidal Anti. Inflammatory Drugs (NSAIDs) inhibition Unknown (yes, Idiopathic anaphylaxis; Local this is considered anaesthetics; Physical (Exercise, a mechanism) Cold-induced anaphylaxis); Sulfites

Anaphylaxis: Rapid recognition and treatment

GENERAL MANAGEMENT OF ANAPHYLAXIS • Airway • Breathing • Circulation • But use epinephrine promptly
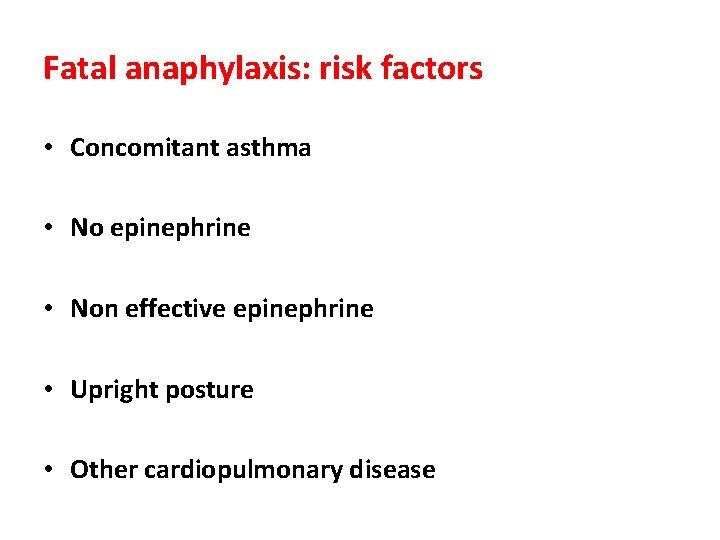
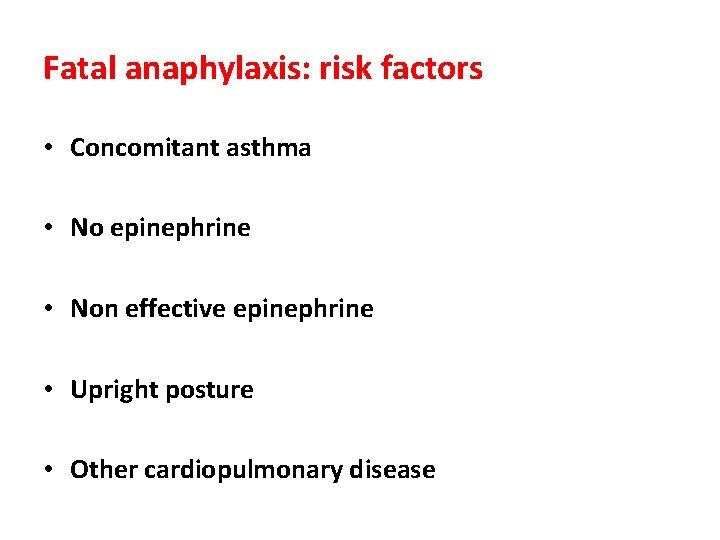
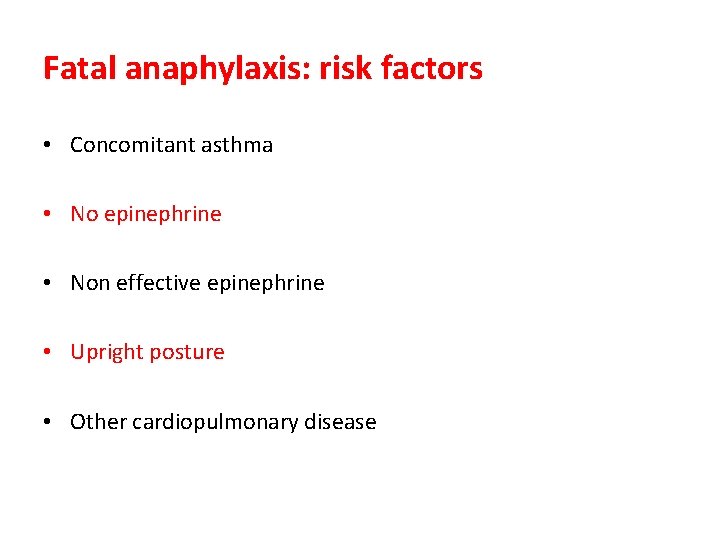
Fatal anaphylaxis: risk factors • Concomitant asthma • No epinephrine • Non effective epinephrine • Upright posture • Other cardiopulmonary disease
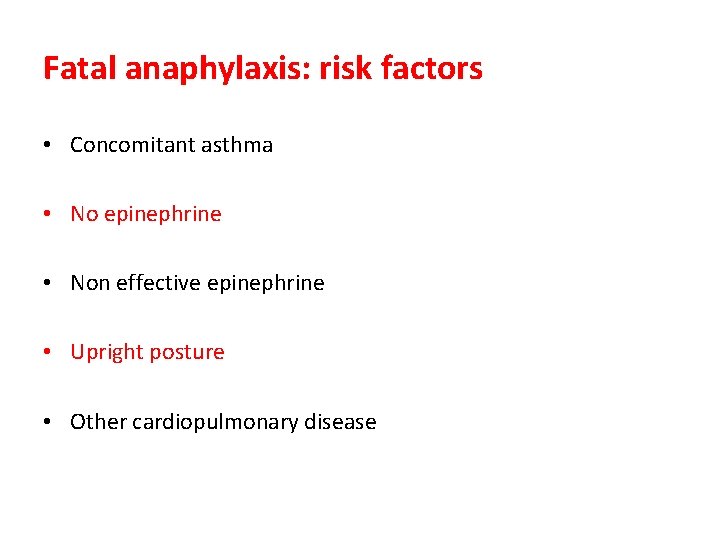
Fatal anaphylaxis: risk factors • Concomitant asthma • No epinephrine • Non effective epinephrine • Upright posture • Other cardiopulmonary disease
Initial Anaphylaxis. Treatment • Epinephrine (adrenaline) is first line treatment • Epinephrine preferably given IM • Antihistamines & bronchodilators are not first line treatment but may be given after epinephrine. • Transportation to hospital should not be delayed to administer these once epinephrine has been given.
Management of anaphylaxis: Initial • Epinephrine 0. 01 mg/kg (max 0. 5 mg) IM X 3, every 5 -20 min as needed. In severe cases epinephrine IV • H 1 antagonists eg Diphenhydramine (Benadryl) 25 -100 mg • H 2 antagonists eg cimetidine • IV fluids to maintain venous access and circulation • Oxygen • Corticosteroids
Management of anaphylaxis: Bronchospasm • Inhaled bronchodilators eg salbutamol. IV if unresponsive to inhaled • Oxygen • Intubation and ventilation if needed
Management of anaphylaxis: Laryngeal edema • Racemic epinephrine via nebulizer • Intubation or cricothyrotomy or tracheostomy
Management of anaphylaxis: Hypotension • Trendelenberg position • Volume expansion with crystalloid • Vasopressors eg dopamine, norepinephrine, metaraminol, vasopressin • Glucagon esp if on beta-blocker

Treatment of Anaphylaxis in Beta Blocked Patients • Give epinephrine initially. • If patient does not respond to epinephrine and other usual therapy: • Glucagon 1 mg IV over 2 minutes • Isoproterenol (a pure beta-agonist β 1β 2 agonist) 1 mg in 500 ml D 5 W starting at 0. 1 mcg/kg/min

EFFECTS OF EPINEPHRINE • Increases BP, reverses peripheral vasodilation , ( alpha-adrenergic activity) • Reduces urticaria and angioedema by vasoconstriction (alpha) • Bronchodilation – relaxes bronchial smooth muscle (beta-2 adrenergic activity) • Increases cardiac contractility – force and volume, increasing heart rate & BP (beta-1) • Prevents further mast cell degranulation (beta)
SIDE EFFECTS OF EPINEPHRINE • Based on the effects of epinephrine, what would you predict as the possible side effects? • What conditions or factors would you consider as higher risk for side effects of epinephrine use?
SIDE EFFECTS OF EPINEPHRINE • Increased heart rate, shakiness, dizziness, headache, anxiety, fear • Hypertension and intracranial bleed • Myocardial ischemia, infarction, arrythmia
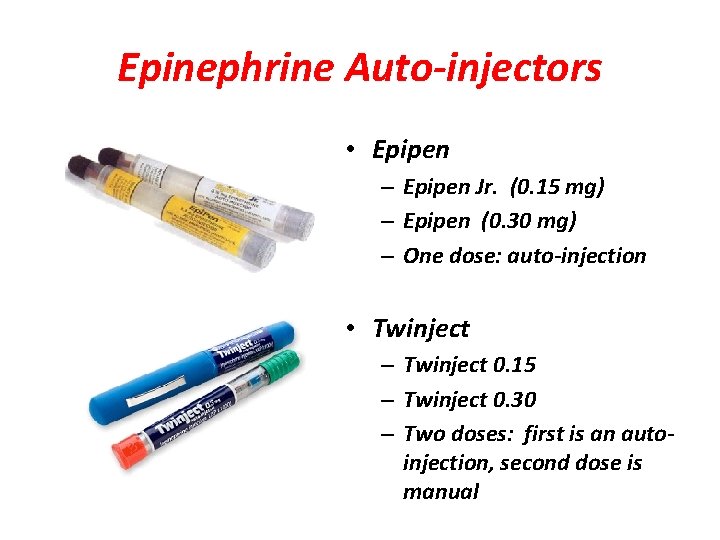
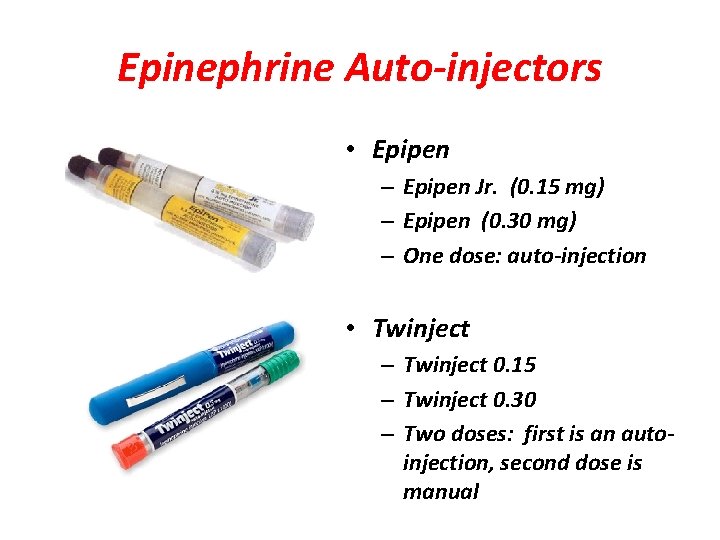
Epinephrine Auto-injectors • Epipen – Epipen Jr. (0. 15 mg) – Epipen (0. 30 mg) – One dose: auto-injection • Twinject – Twinject 0. 15 – Twinject 0. 30 – Two doses: first is an autoinjection, second dose is manual
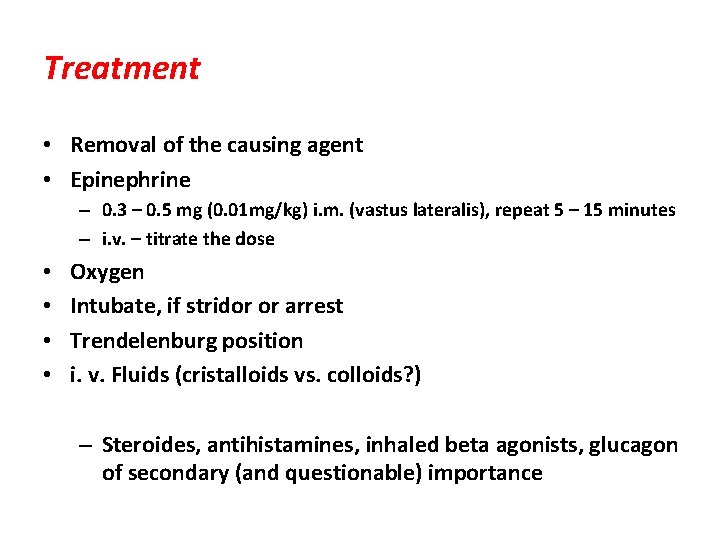
Treatment • Removal of the causing agent • Epinephrine – 0. 3 – 0. 5 mg (0. 01 mg/kg) i. m. (vastus lateralis), repeat 5 – 15 minutes – i. v. – titrate the dose • • Oxygen Intubate, if stridor or arrest Trendelenburg position i. v. Fluids (cristalloids vs. colloids? ) – Steroides, antihistamines, inhaled beta agonists, glucagon of secondary (and questionable) importance

Questions? Thank you for attention !
 Nap 6 recommendations
Nap 6 recommendations Anaphylaxis treatment
Anaphylaxis treatment Neuhaus rapid word recognition chart
Neuhaus rapid word recognition chart Causes of anaphylactic reaction
Causes of anaphylactic reaction Reaction
Reaction Anaphylactoid vs anaphylaxis
Anaphylactoid vs anaphylaxis Anaphylaxis onset
Anaphylaxis onset Dose of epinephrine in anaphylaxis
Dose of epinephrine in anaphylaxis Biphasic anaphylaxis
Biphasic anaphylaxis Anaphylaxis classification
Anaphylaxis classification Interprofessional care for anaphylaxis
Interprofessional care for anaphylaxis Anaphylaxis
Anaphylaxis Nap 6 summary
Nap 6 summary Anaphylaxis
Anaphylaxis Hypersensitivity types and examples
Hypersensitivity types and examples Brighton collaboration case definitions for vaccines
Brighton collaboration case definitions for vaccines Angioedema anaphylaxis
Angioedema anaphylaxis Anaphylaxis photos
Anaphylaxis photos Ig
Ig Anaphylaxis photos
Anaphylaxis photos Recognition and regard for oneself and one's abilities: *
Recognition and regard for oneself and one's abilities: * Policy guidelines on awards and recognition
Policy guidelines on awards and recognition Difference between recall and recognition
Difference between recall and recognition Reinforcing effort and providing recognition
Reinforcing effort and providing recognition Disadvantages of optical character recognition
Disadvantages of optical character recognition Nrl head injury recognition and referral form
Nrl head injury recognition and referral form Opportunity recognition and opportunity assessment plan
Opportunity recognition and opportunity assessment plan Va handbook 5017
Va handbook 5017 Reinforcing effort and providing recognition
Reinforcing effort and providing recognition Direction for simple recall test
Direction for simple recall test Incoterms and revenue recognition us gaap
Incoterms and revenue recognition us gaap Opportunity recognition shaping and reshaping
Opportunity recognition shaping and reshaping Praise, recognition and power are_______.
Praise, recognition and power are_______. Reinforcing effort
Reinforcing effort Shape matching and object recognition using shape contexts
Shape matching and object recognition using shape contexts Suspected cancer recognition and referral
Suspected cancer recognition and referral Suspected cancer recognition and referral
Suspected cancer recognition and referral Cm bishop pattern recognition and machine learning
Cm bishop pattern recognition and machine learning Accenture cp points value
Accenture cp points value Bolongie
Bolongie Surge and rapid response team salary
Surge and rapid response team salary Index
Index Mass customization and rapid product development
Mass customization and rapid product development Rapid prototyping techniques in software engineering
Rapid prototyping techniques in software engineering Panoramic survey telescope and rapid response system
Panoramic survey telescope and rapid response system Panoramic survey telescope and rapid response system
Panoramic survey telescope and rapid response system Rapid gui programming with python and qt
Rapid gui programming with python and qt Prototyping and rapid application development
Prototyping and rapid application development Residual chlorine
Residual chlorine Rapid application development advantages and disadvantages
Rapid application development advantages and disadvantages Rapid and accurate image super resolution
Rapid and accurate image super resolution Employee recognition proposal
Employee recognition proposal Chapter 18 revenue recognition
Chapter 18 revenue recognition Four part processing model for word recognition
Four part processing model for word recognition