Alterations of Hematologic Function Part 2 Chapter 21

- Slides: 88
Alterations of Hematologic Function – Part 2 Chapter 21 Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Alterations of Leukocyte Function Increases or decreases in cell numbers Ø “-cytosis” or “-philia” refer to an increase in number. Ø “-openia” refers to a decrease in number. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Alterations of Leukocyte Function Leukocytosis – higher than normal leukocyte count. Ø Leukocytosis is a normal protective physiologic response to physiologic stressors, including infection. Leukopenia – lower than normal leukocyte count. Ø Leukopenia is not normal and not beneficial. Ø A low white count predisposes a patient to infections. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
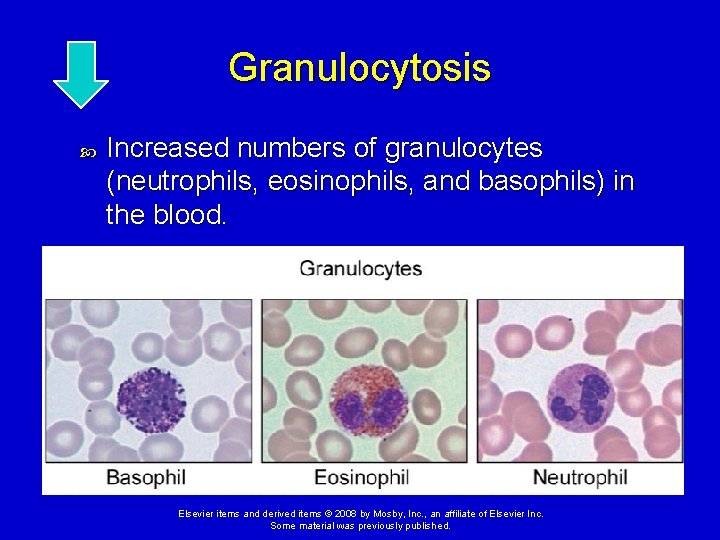
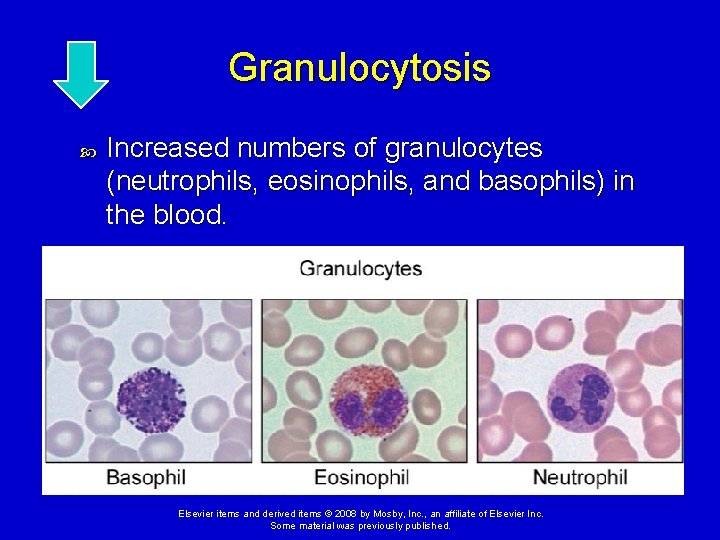
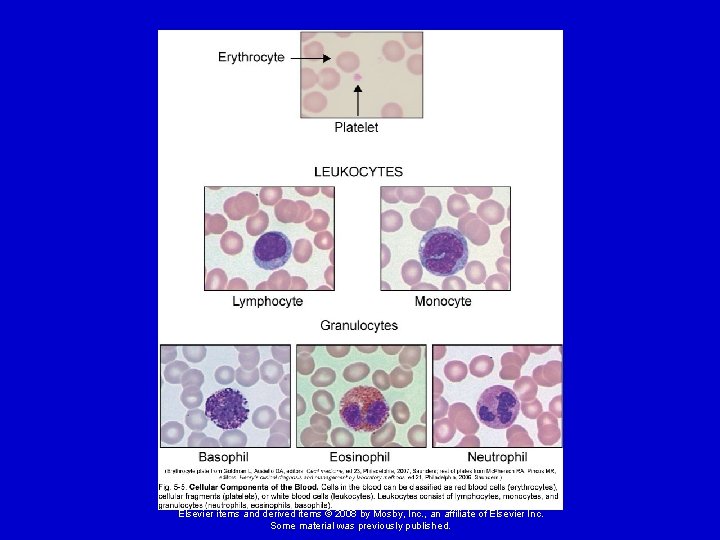
Granulocytosis Increased numbers of granulocytes (neutrophils, eosinophils, and basophils) in the blood. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
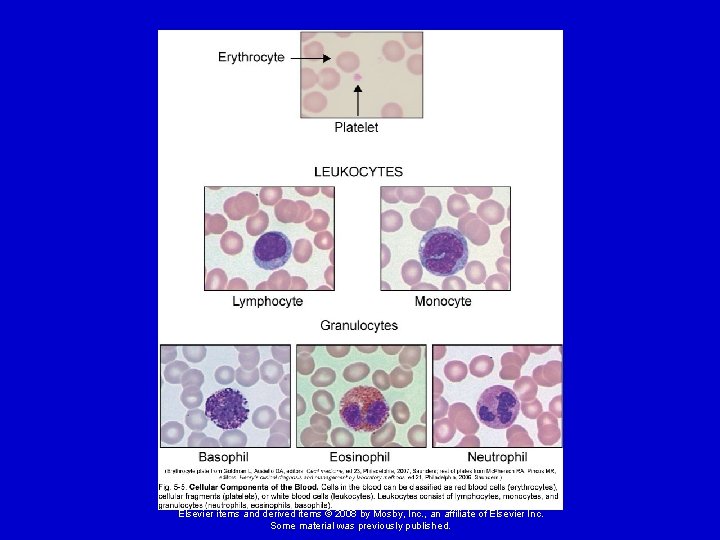
Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Neutrophilia Neutrophilia is evident in the first stages of an infection or inflammation (count >7, 500/mm 3). If the need for neutrophils increases beyond the supply, immature neutrophils (banded neutrophils) are released into the blood. This premature release is detected in the manual WBC differential and is termed a shift-to-the-left. When the population returns to normal, it is termed a shift-to-the-right. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Neutropenia Reduction in circulating neutrophils less than 2000/mm 3. Causes: Ø Prolonged severe infection Ø Decreased production Ø Reduced survival Ø Abnormal neutrophil distribution and sequestration Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Granulocytopenia (Agranulocytosis) Very low numbers of granulocytes with neutrophil counts below 500/mm 3. Greatly increases risk of infection. Causes of granulocytopenia: Ø Interference with hematopoiesis Ø Immune mechanisms Ø Chemotherapy destruction Ø Ionizing radiation Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Eosinophilia Hypersensitivity reactions trigger the release of eosinophilic chemotactic factor of anaphylaxis from mast cells. Occurs in allergic disorders and parasitic invasions. Skip to Lymphocytosis Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Eosinopenia Usually caused by migration of cells to inflammatory sites. Other causes - surgery, shock, trauma, burns, or mental distress. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Basophils Basophilia Ø Basophils account for only 0% to 1% of the circulating WBCs Ø Basophilia occurs in response to inflammation and hypersensitivity reactions. Basopenia Ø Occurs in acute infections, hyperthyroidism, and long-term steroid therapy. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Monocytes Monocytosis Ø Poor correlation with disease. Ø Usually occurs with neutropenia in later stages of infections. Ø Monocytes are needed to phagocytize organisms and debris. Monocytopenia Ø Very little known about this condition. Ø Associated with hairy cell leukemia and prednisone therapy. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Lymphocytes Lymphocytosis Ø Acute viral infections Lymphocytopenia Ø Immune deficiencies, drug destruction, viral destruction Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
ACTIVITY 1. 2. 3. 4. Bacterial infection. Allergic reaction. Viral infection. Parasitic infection. a. Eosinophilia b. Granulocytosis c. Lymphocytosis Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
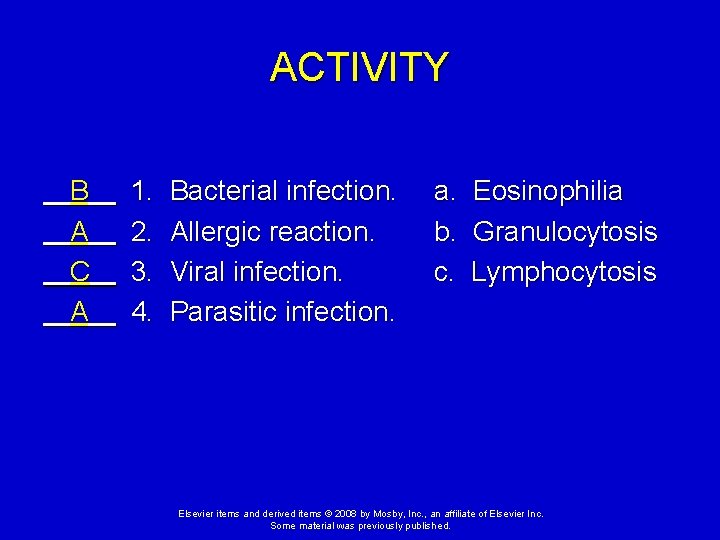
ACTIVITY B A C A 1. 2. 3. 4. Bacterial infection. Allergic reaction. Viral infection. Parasitic infection. a. Eosinophilia b. Granulocytosis c. Lymphocytosis Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Infectious Mononucleosis Acute, self-limiting infection of B-lymphocytes. Caused by the Epstein-Barr virus (EBV). Transmitted in saliva through personal contact. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Infectious Mononucleosis Manifestations: Ø Initially - fever, sore throat, swollen cervical lymph nodes, headache, fatigue, joint aches, increased lymphocyte count, and atypical (activated) lymphocytes. Ø Later – generalized lymph node enlargement, enlargement of liver and spleen (hepatomegaly and splenomegaly). Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Infectious Mononucleosis Serious complications are infrequent (<5%). Ø Splenic rupture is the most common cause of death. Diagnostic test - monospot qualitative test for heterophilic antibodies Treatment - for relief of symptoms Ø Bed rest, limit physical activity to avoid rupture of spleen. Usually self-limiting with fatigue lasting for 1 -2 months after other symptoms resolve. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
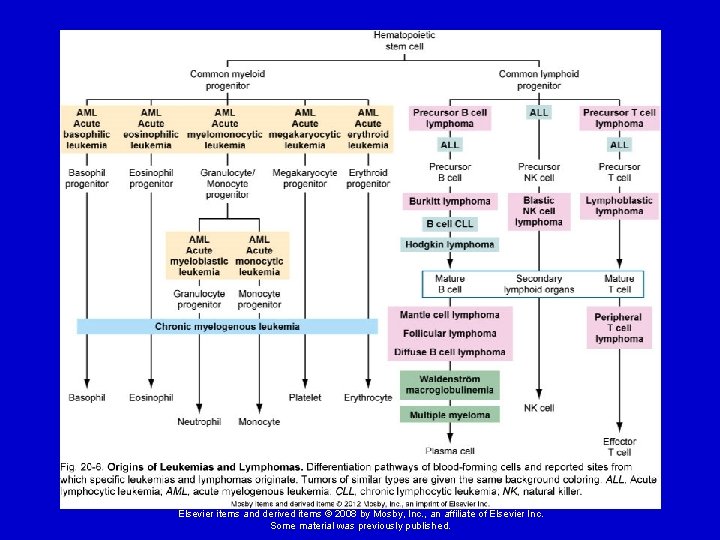
Qualitative Alterations of Leukocytes Leukemia - neoplastic proliferation of leukocyte precursor cells in the bone marrow. Ø Results in dysfunctional progeny cells. Ø Interferes with the production of other blood cells in the marrow. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
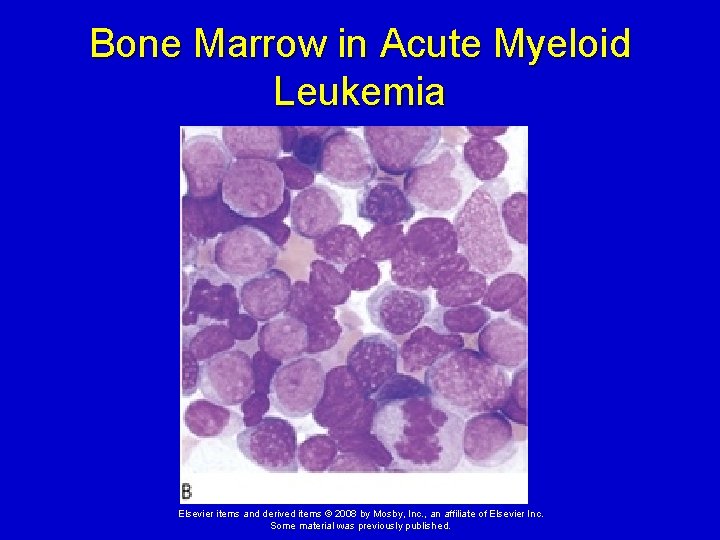
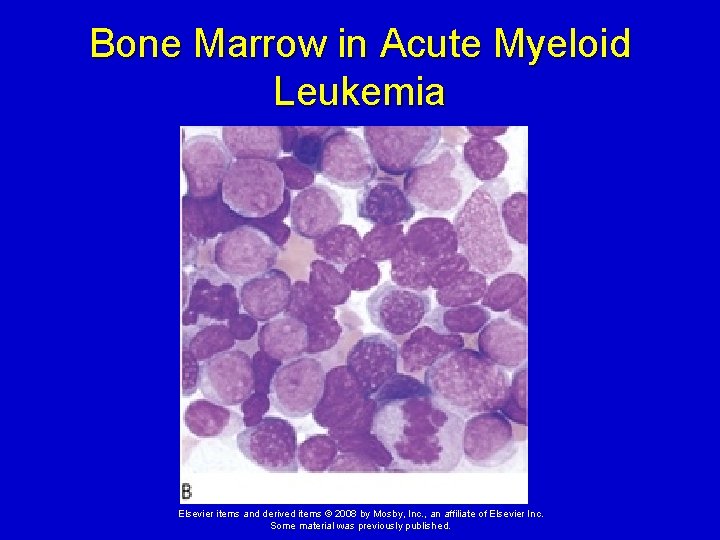
Bone Marrow in Acute Myeloid Leukemia Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Leukemias Pathophysiology: Mutations in a leukocyte precursor cell cause unregulated cellular proliferation. Believed to occur in individuals with an inherited chromosomal vulnerability to mutagens such as radiation, toxins, or chemotherapeutic agents. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Leukemias Pathophysiology (cont. ) There is a blockage of the normal differentiation of the cell so that it continues to divide (“immortal cell”); not an increase in the rate of cell division. These cells accumulate in the marrow, crowding out the other marrow cells and eventually spilling out into the peripheral blood. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Leukemias Pathophysiology (cont. ) Leukemic cells are not capable of normal white blood cell function; this, combined with decreased production of erythrocytes and platelets, leads to the common complications of leukemia: Ø Infection, anemia, and bleeding. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Leukemias Risk factors for leukemia: Family history of leukemia Certain hereditary abnormalities, including Down syndrome Some immune deficiencies Environmental factors like cigarette smoke, benzene, and ionizing radiation Viral infections - HIV, hepatitis C, and HTLV-1 Drugs that suppress bone marrow, including many chemotherapy agents Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
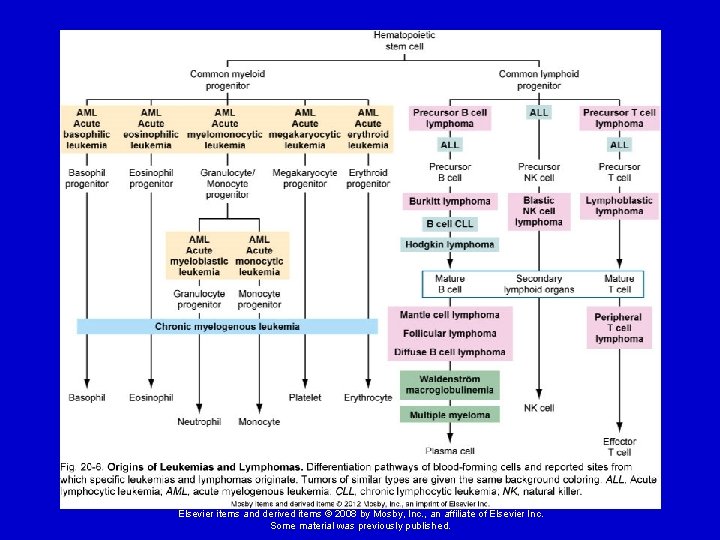
Leukemias Classifications: Acute - presence of undifferentiated or immature cells, usually blast cells Chronic - predominant cell is mature but does not function normally Myelogenous - arise from precursors of the granulocytes Lymphocytic - arise from precursors of lymphocytes Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
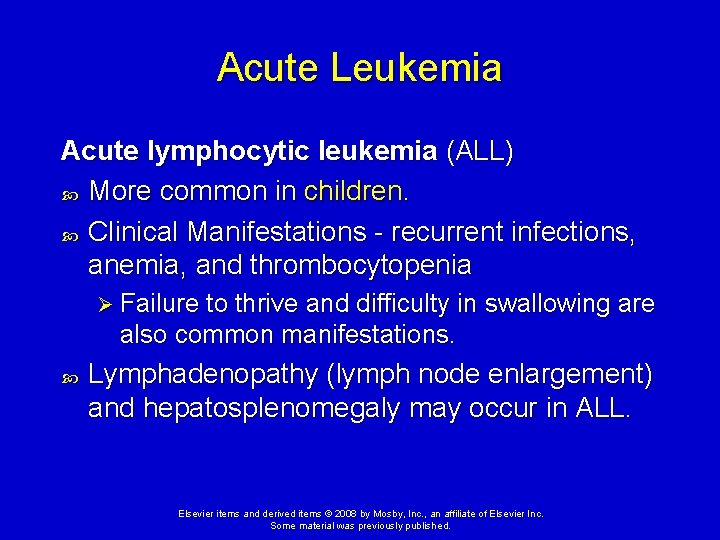
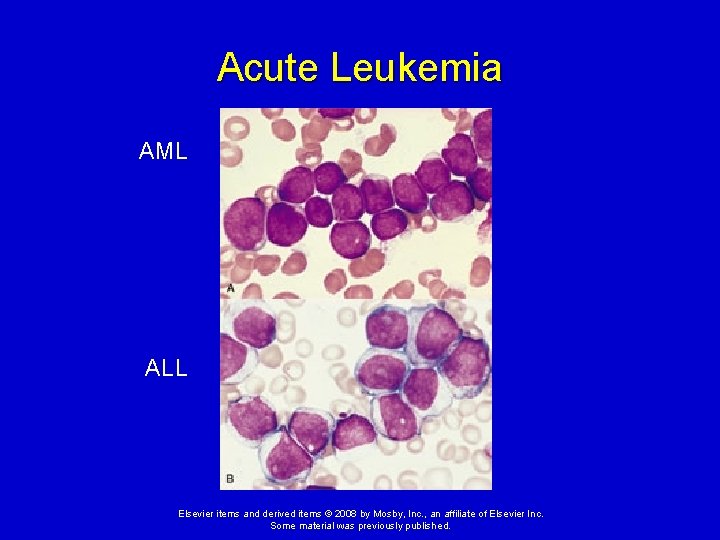
Acute Leukemia Acute lymphocytic leukemia (ALL) More common in children. Clinical Manifestations - recurrent infections, anemia, and thrombocytopenia Ø Failure to thrive and difficulty in swallowing are also common manifestations. Lymphadenopathy (lymph node enlargement) and hepatosplenomegaly may occur in ALL. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
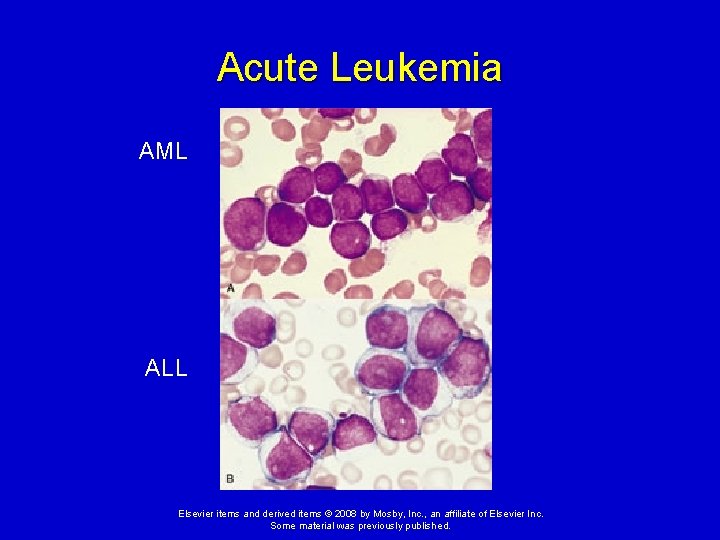
Acute Leukemia AML ALL Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
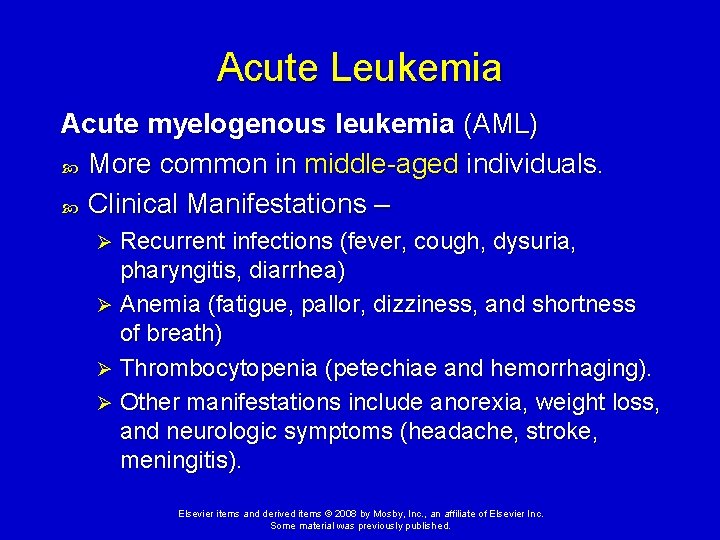
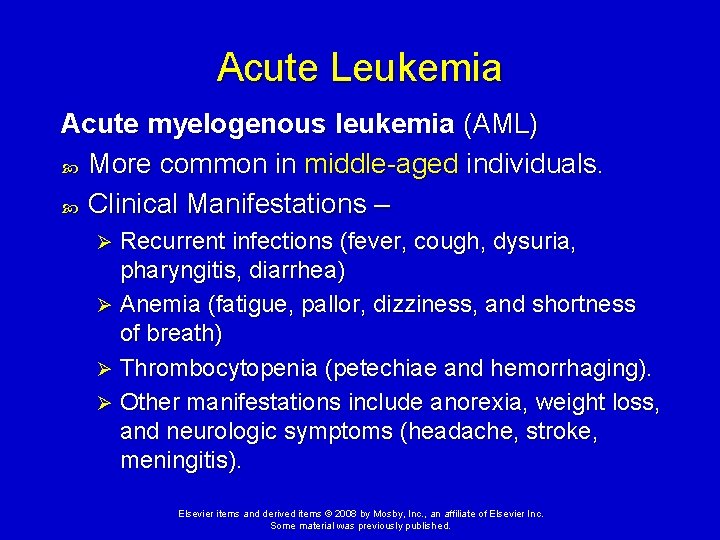
Acute Leukemia Acute myelogenous leukemia (AML) More common in middle-aged individuals. Clinical Manifestations – Recurrent infections (fever, cough, dysuria, pharyngitis, diarrhea) Ø Anemia (fatigue, pallor, dizziness, and shortness of breath) Ø Thrombocytopenia (petechiae and hemorrhaging). Ø Other manifestations include anorexia, weight loss, and neurologic symptoms (headache, stroke, meningitis). Ø Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Acute Leukemia Treatment of acute leukemia includes: Chemotherapy Bone marrow transplantation (if chemotherapy is not effective) In ALL, chemotherapy results in cure in the majority of children. Ø In AML, relapse is common and requires consideration for bone marrow transplantation. Ø Supportive care, including red blood cell transfusions, platelet transfusions, and antibiotics. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
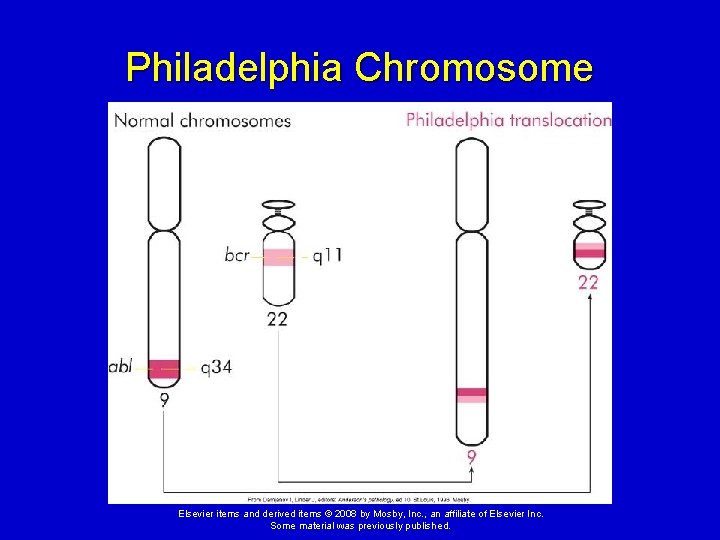
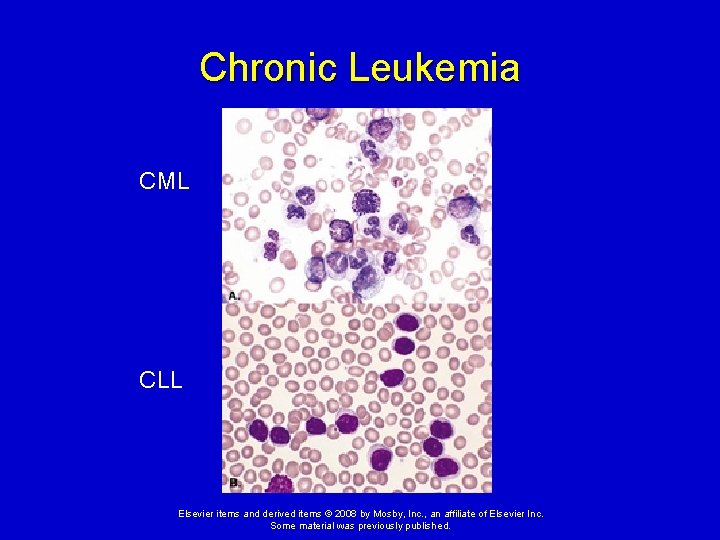
Chronic Leukemia Chronic myelogenous leukemia (CML) More common in middle-aged to older adults. Commonly associated with a specific chromosomal translocation called the Philadelphia chromosome which contains a BRC-ABL gene fusion. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
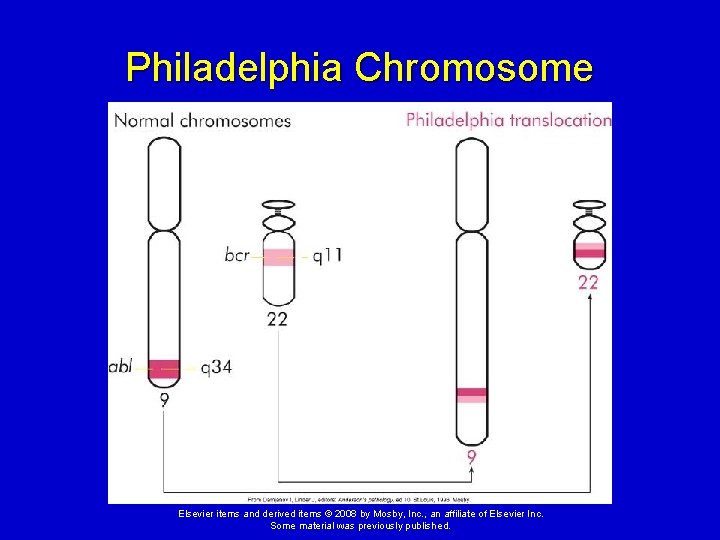
Philadelphia Chromosome Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
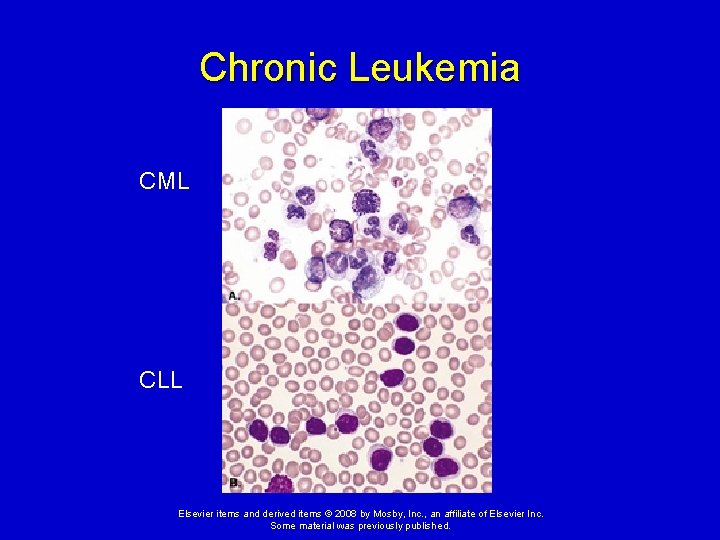
Chronic Leukemia CML CLL Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Chronic Leukemia Chronic lymphocytic leukemia (CLL) Occurs primarily in the elderly. Usually the result of neoplastic proliferation of a B-lymphocyte precursor. Not associated with the Philadelphia chromosome mutation. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Chronic Leukemia Clinical manifestations of chronic leukemia: Fatigue, weight loss Low-grade fever, night sweats Splenomegaly, possible abdominal discomfort Lymphadenopathy (most common in CLL) Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Chronic Leukemia Because the neoplastic cells are more differentiated than in acute leukemia, chronic leukemia tends to have a more slowly progressive course. Treatment depends on the type of leukemia and the age of the affected individual, but usually includes low-dose chemotherapy or radiation. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
ACTIVITY 1. Presence of Philadelphia chromosome. 2. Most common in children. 3. Slowly progressive; occurs mainly in elderly. 4. Rapidly progressive; occurs mainly in middle age. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
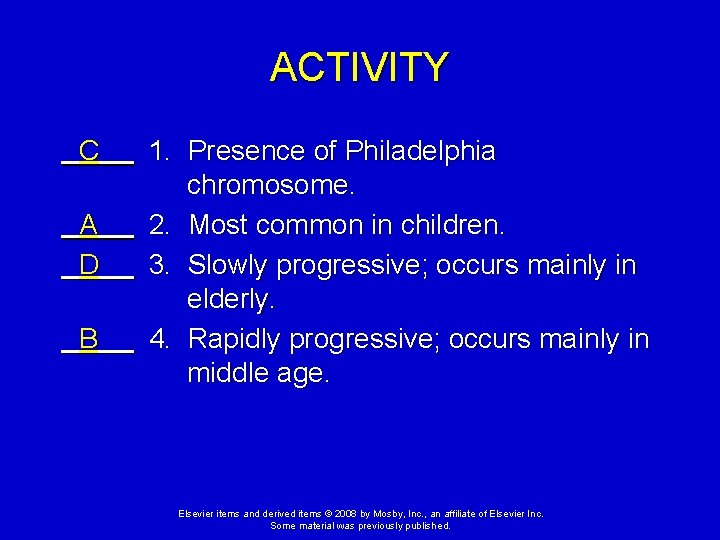
ACTIVITY C A D B 1. Presence of Philadelphia chromosome. 2. Most common in children. 3. Slowly progressive; occurs mainly in elderly. 4. Rapidly progressive; occurs mainly in middle age. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
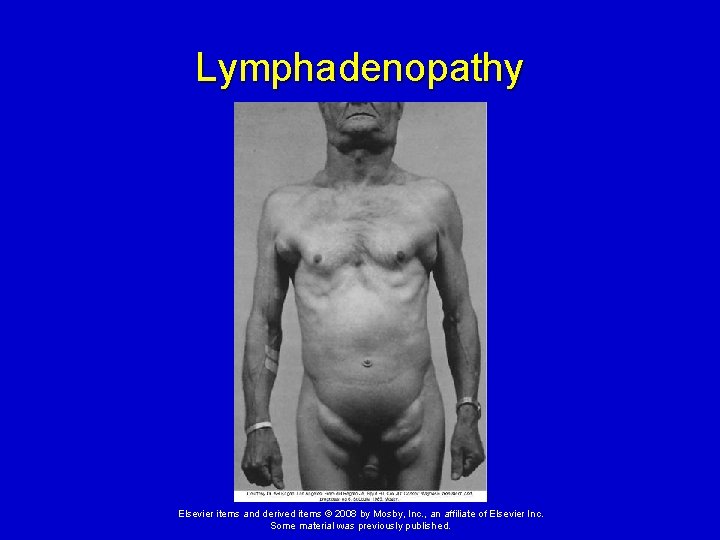
Alterations of Lymphoid Function Lymphadenopathy Enlarged lymph nodes that become palpable and tender. Local lymphadenopathy – usually due to drainage of an inflammatory lesion located near the enlarged node. General lymphadenopathy - occurs in the presence of malignant or nonmalignant disease. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
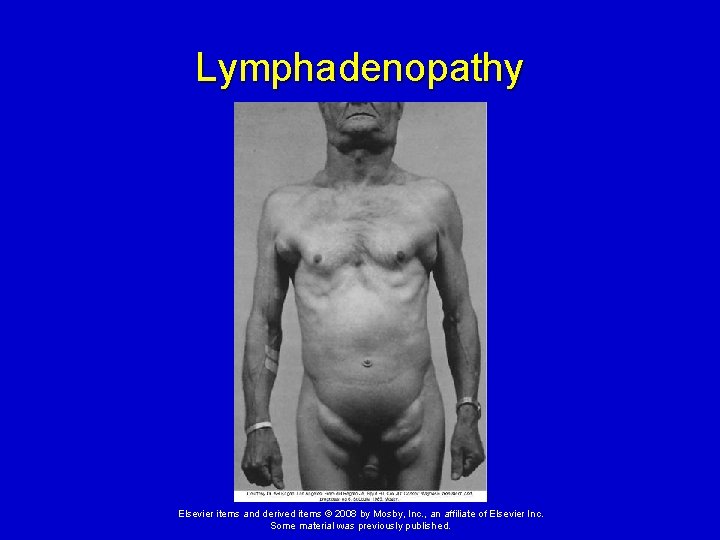
Lymphadenopathy Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Malignant Lymphomas Malignant transformation of a lymphocyte precursor, which then proliferates in lymphoid tissues. Two major categories Ø Hodgkin lymphoma Ø Non-Hodgkin lymphomas Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
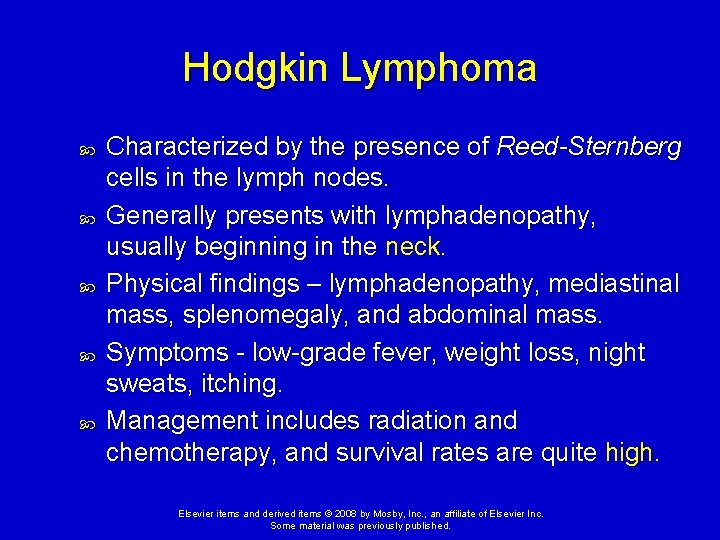
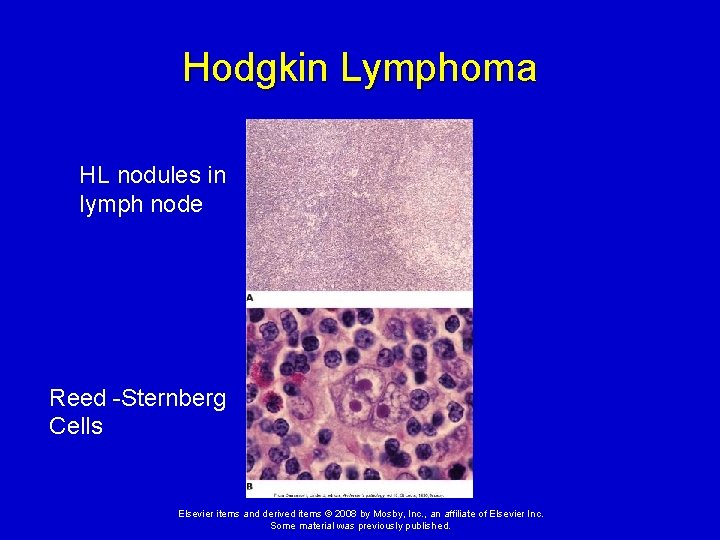
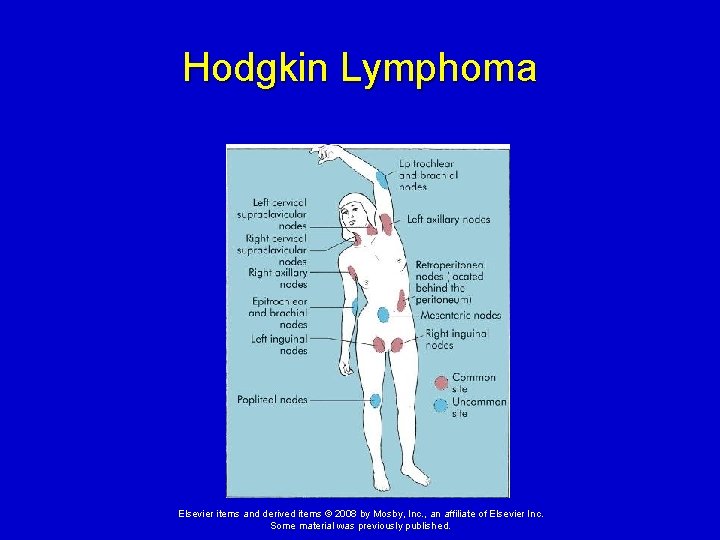
Hodgkin Lymphoma Characterized by the presence of Reed-Sternberg cells in the lymph nodes. Generally presents with lymphadenopathy, usually beginning in the neck. Physical findings – lymphadenopathy, mediastinal mass, splenomegaly, and abdominal mass. Symptoms - low-grade fever, weight loss, night sweats, itching. Management includes radiation and chemotherapy, and survival rates are quite high. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
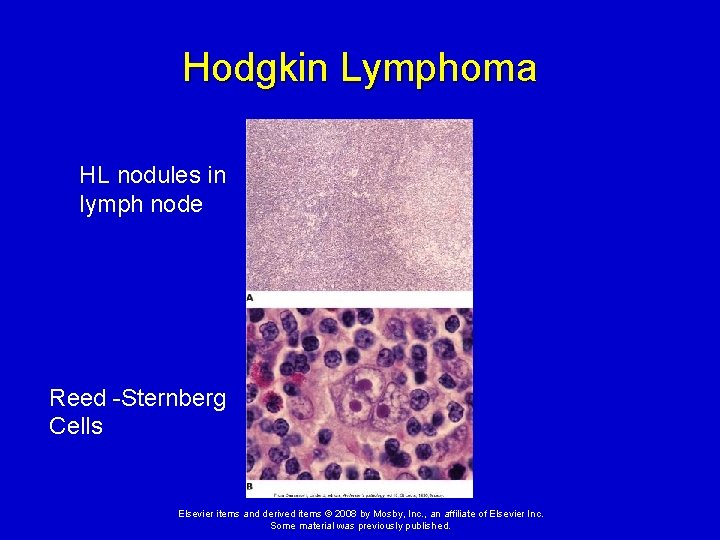
Hodgkin Lymphoma HL nodules in lymph node Reed -Sternberg Cells Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Hodgkin Lymphoma Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
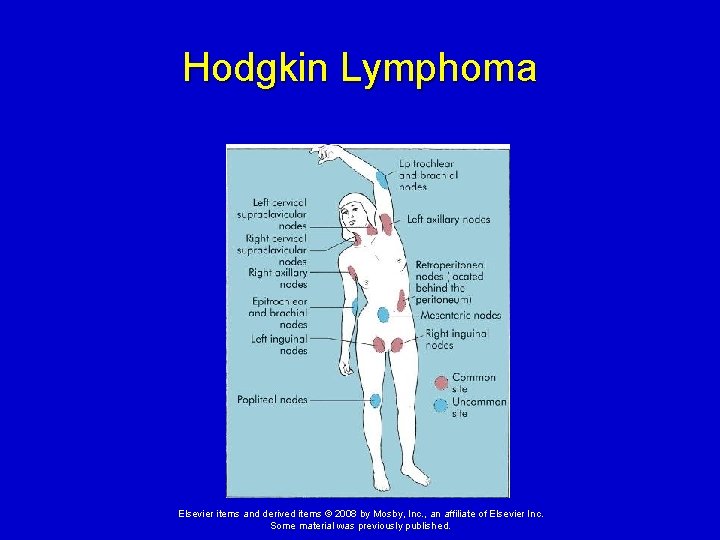
Hodgkin Lymphoma Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Non-Hodgkin Lymphoma Generic term for a diverse group of lymphomas. Clinical manifestations of NHL: Ø Similar to Hodgkin lymphoma, but non- Hodgkin lymphoma progresses to include symptoms of the nasopharynx, gastrointestinal tract, bone, testes, and other soft tissues. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Non-Hodgkin Lymphoma Clinical manifestations of NHL (cont. ): Ø Tends to involve many peripheral nodes and extends into extranodal tissues. Ø Low-grade NHL is often associated with very slow disease progression and long survival times. Ø High-grade lymphomas (like those seen in AIDS) have a very poor prognosis. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
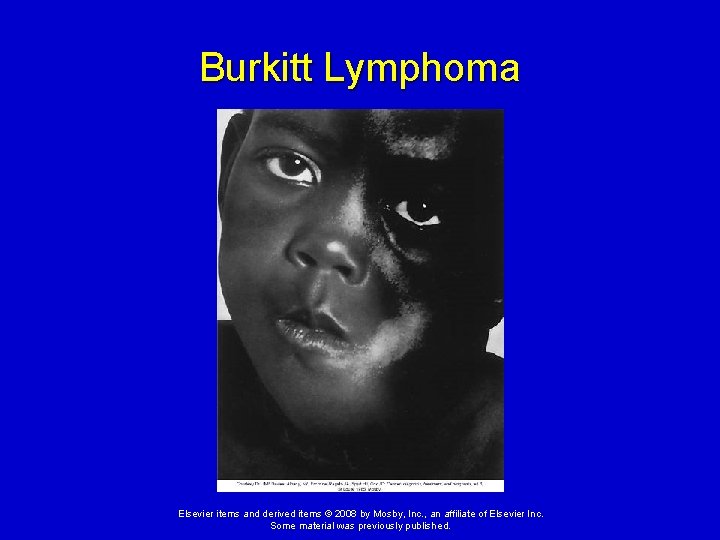
Burkitt Lymphoma B-cell tumor. Most common type of non-Hodgkin lymphoma in children. Burkitt lymphoma is a very fast-growing tumor of the jaw and facial bones. Epstein-Barr virus is associated with >90% of cases. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
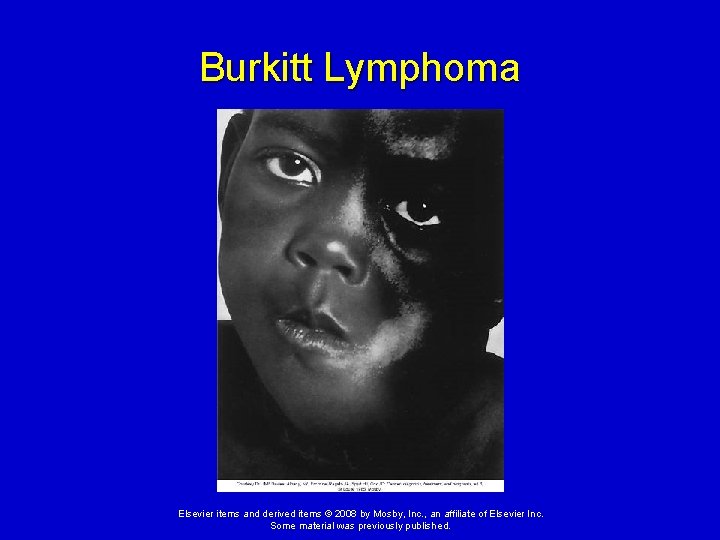
Burkitt Lymphoma Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
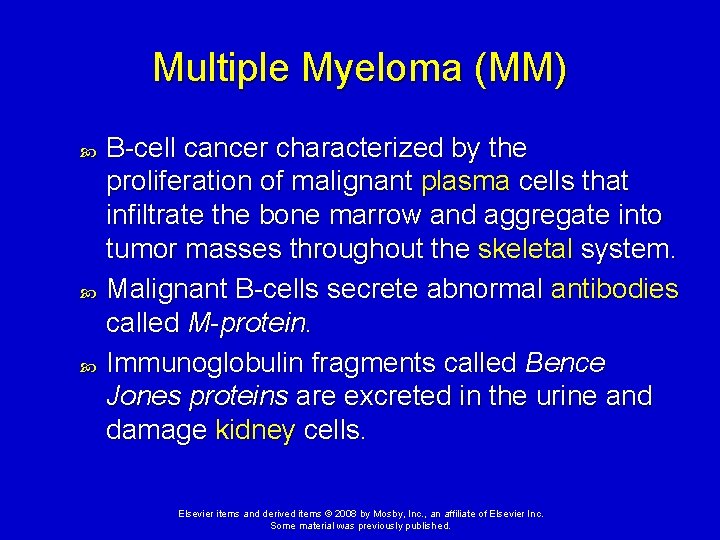
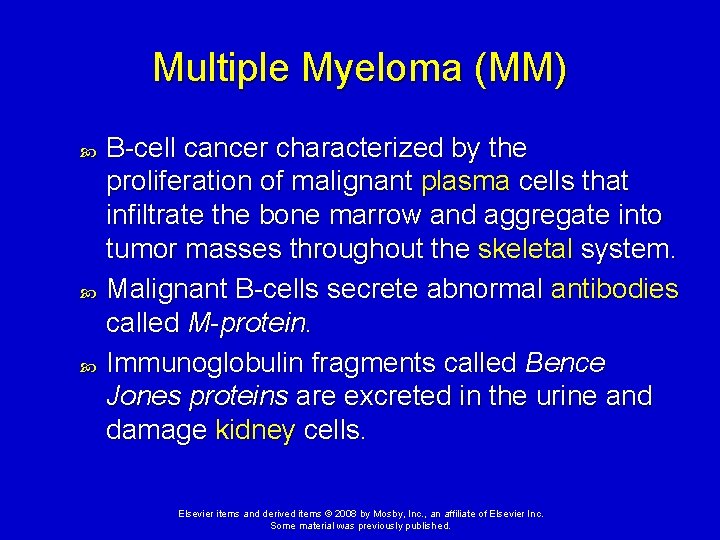
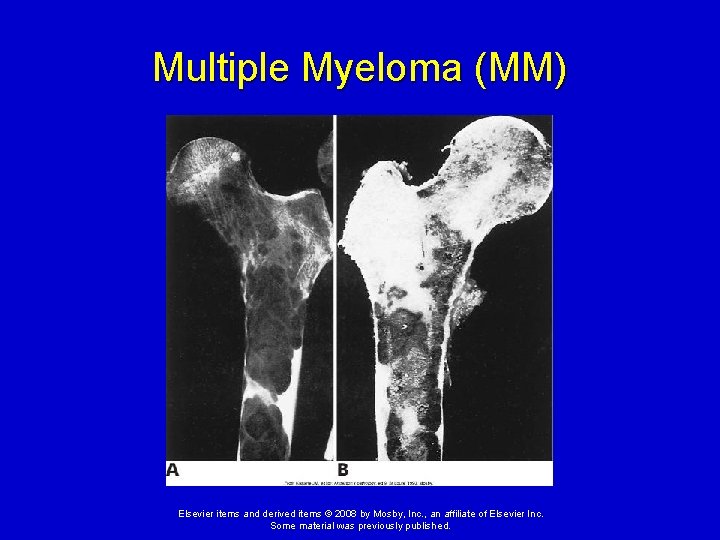
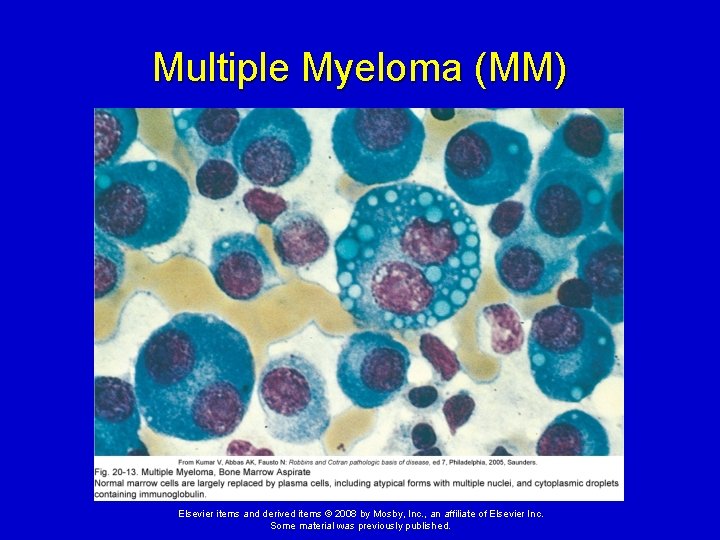
Multiple Myeloma (MM) B-cell cancer characterized by the proliferation of malignant plasma cells that infiltrate the bone marrow and aggregate into tumor masses throughout the skeletal system. Malignant B-cells secrete abnormal antibodies called M-protein. Immunoglobulin fragments called Bence Jones proteins are excreted in the urine and damage kidney cells. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
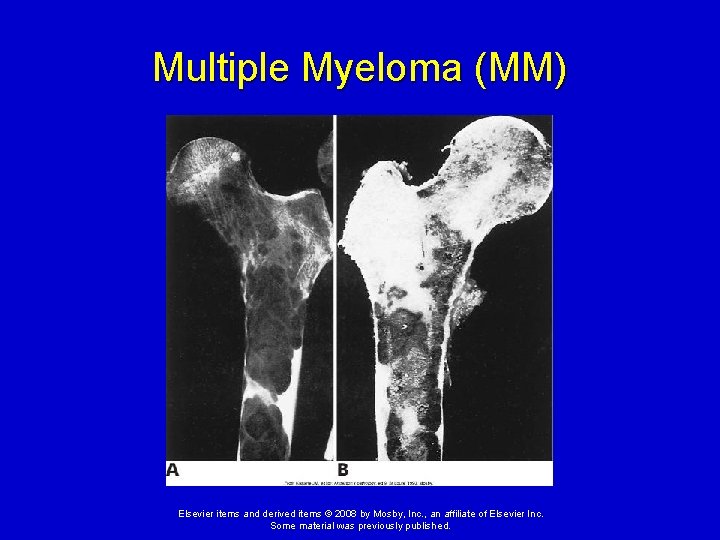
Multiple Myeloma (MM) Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
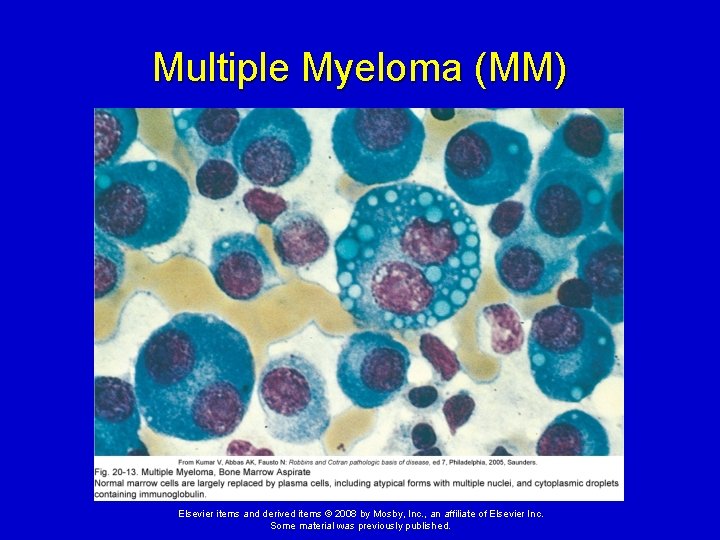
Multiple Myeloma (MM) Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
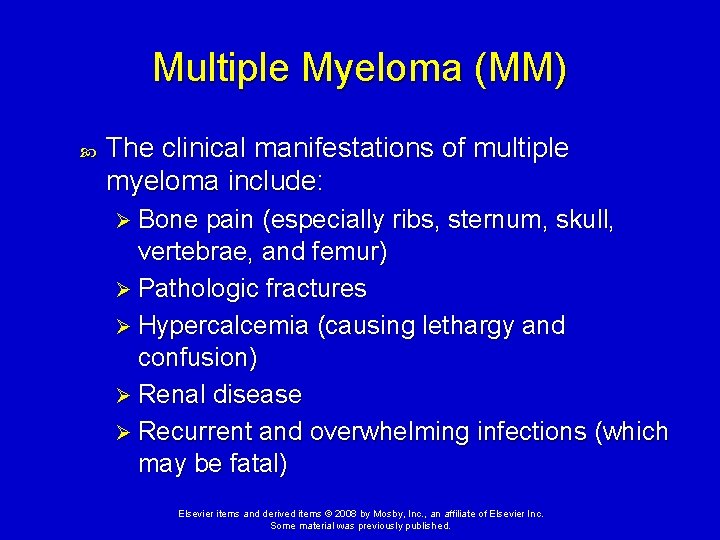
Multiple Myeloma (MM) The clinical manifestations of multiple myeloma include: Ø Bone pain (especially ribs, sternum, skull, vertebrae, and femur) Ø Pathologic fractures Ø Hypercalcemia (causing lethargy and confusion) Ø Renal disease Ø Recurrent and overwhelming infections (which may be fatal) Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Lymphoblastic Lymphoma (LL) Arises from immature T cells that become malignant in the thymus. Most commonly seen in children and adolescents. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Lymphoblastic Lymphoma (LL) Clinical manifestation: Ø Usually begins with a painless lymphadenopathy in the neck. Ø The mass in the thymus may cause chest pain and bronchial compression. Ø May infiltrate the bone marrow, liver, kidney, spleen, and brain. Ø Very aggressive. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
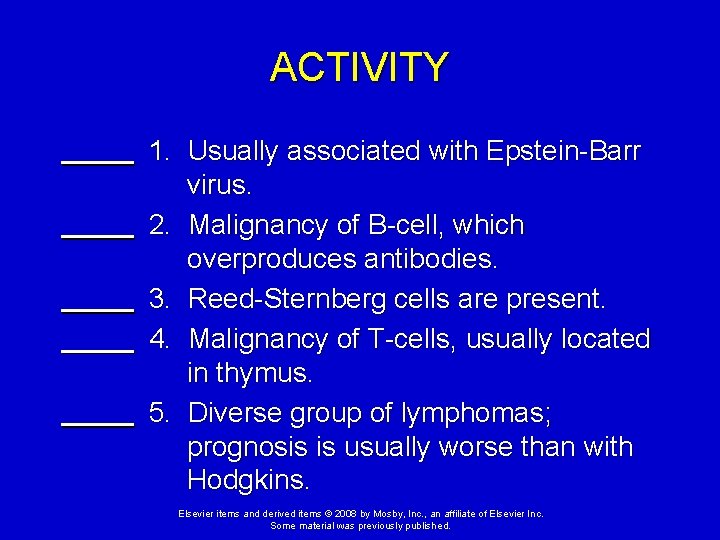
ACTIVITY 1. Usually associated with Epstein-Barr virus. 2. Malignancy of B-cell, which overproduces antibodies. 3. Reed-Sternberg cells are present. 4. Malignancy of T-cells, usually located in thymus. 5. Diverse group of lymphomas; prognosis is usually worse than with Hodgkins. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
ACTIVITY C D A E B 1. Usually associated with Epstein-Barr virus. 2. Malignancy of B-cell, which overproduces antibodies. 3. Reed-Sternberg cells are present. 4. Malignancy of T-cells, usually located in thymus. 5. Diverse group of lymphomas; prognosis is usually worse than with Hodgkins. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
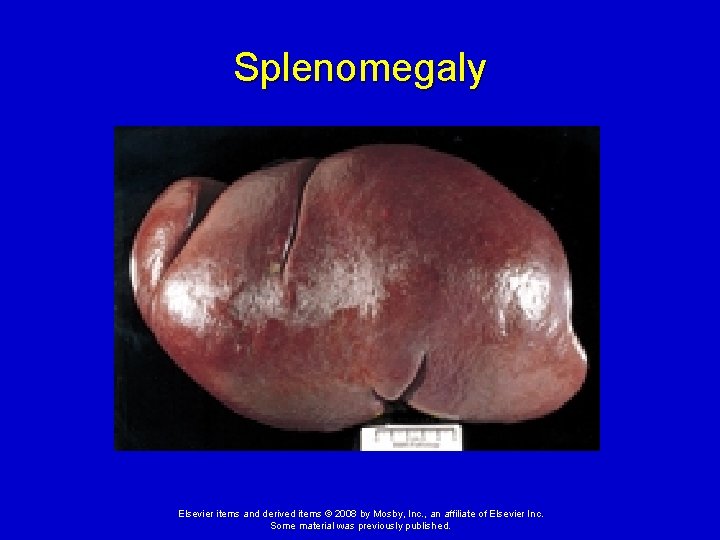
Alterations in Splenic Function Splenomegaly Ø Enlargement of the spleen. Ø May be normal or pathological. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
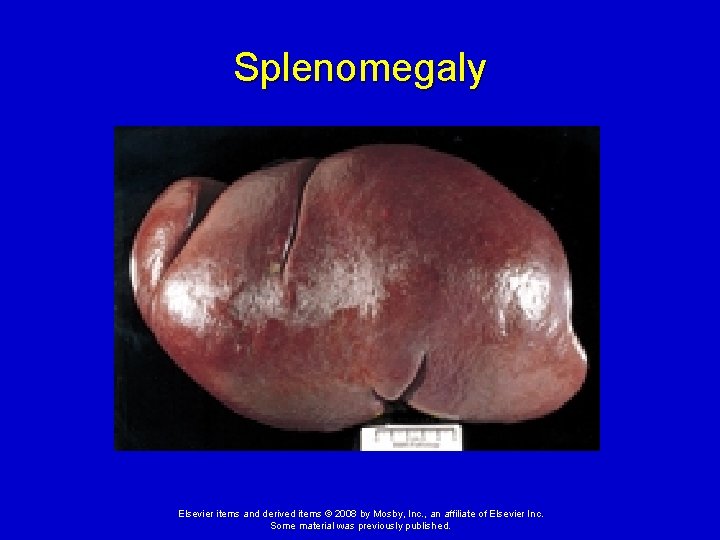
Splenomegaly Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Alterations in Splenic Function Hypersplenism - overactive splenic function. Can occur in: Ø Inflammatory or infectious conditions Ø Congestion from liver disease or heart failure Ø Leukemia and lymphoma. Can cause anemia, leukopenia, and thrombocytopenia caused by sequestration of blood components in the spleen. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disorders of Platelets Thrombocytopenia - defined as a platelet count <150, 000/mm 3, but problems occur at lower levels: <50, 000/mm 3—hemorrhage from minor trauma Ø <15, 000/mm 3—spontaneous bleeding Ø <10, 000/mm 3—severe bleeding Ø Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disorders of Platelets Causes of thrombocytopenia: Ø Hypersplenism, autoimmune disease, hypothermia, and viral or bacterial infections that cause disseminated intravascular coagulation (DIC) Ø May be congenital (rare) or acquired. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disorders of Platelets Heparin induced thrombocytopenia (HIT) An autoimmune disorder that results in intravascular aggregation of platelets and a paradoxical thrombosis in response to administration of heparin (an anticoagulant). Occurs in 1% to 5% of all individuals treated with heparin. Clinical manifestations: Deep venous thrombosis and pulmonary emboli. Ø Coronary thrombosis with myocardial ischemia may occur. Ø Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disorders of Platelets Idiopathic (immune) thrombocytopenic purpura (ITP) ITP is a form of type II hypersensitivity with antibody formation against altered platelet antigens and subsequent platelet destruction in the spleen. The acute form of ITP is more prevalent in children. Often develops after a viral infection. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disorders of Platelets Idiopathic (immune) thrombocytopenic purpura (ITP) Manifestations Ø Petechiae and purpura, progressing to major hemorrhage Treatment Ø Often self-limiting Ø Usually responds to steroid administration. Ø Splenectomy may be indicated in severe cases. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
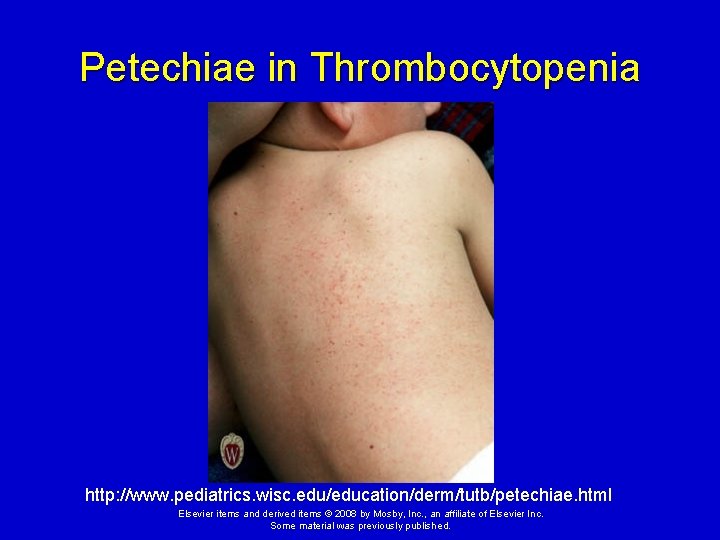
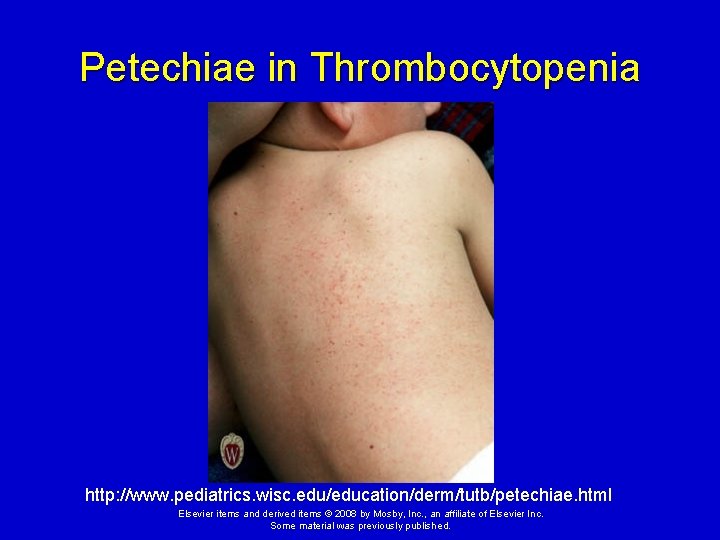
Petechiae in Thrombocytopenia http: //www. pediatrics. wisc. edu/education/derm/tutb/petechiae. html Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.

Purpura http: //www. pediatrics. wisc. edu/education/derm/tutb/85. html Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
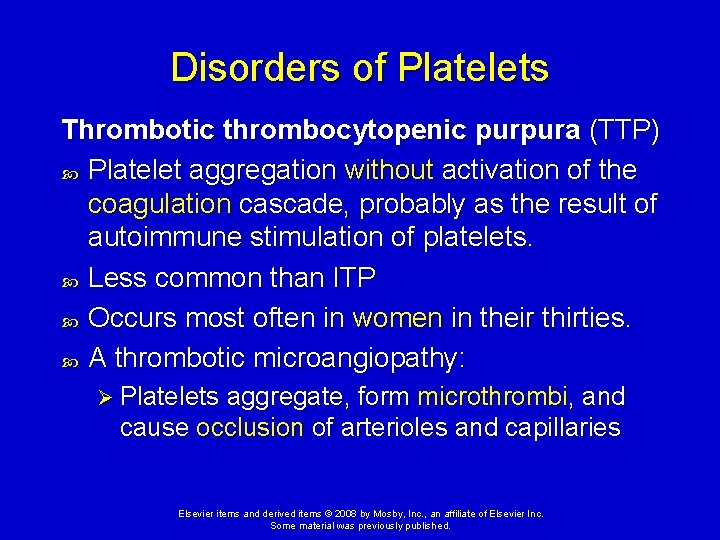
Disorders of Platelets Thrombotic thrombocytopenic purpura (TTP) Platelet aggregation without activation of the coagulation cascade, probably as the result of autoimmune stimulation of platelets. Less common than ITP Occurs most often in women in their thirties. A thrombotic microangiopathy: Ø Platelets aggregate, form microthrombi, and cause occlusion of arterioles and capillaries Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
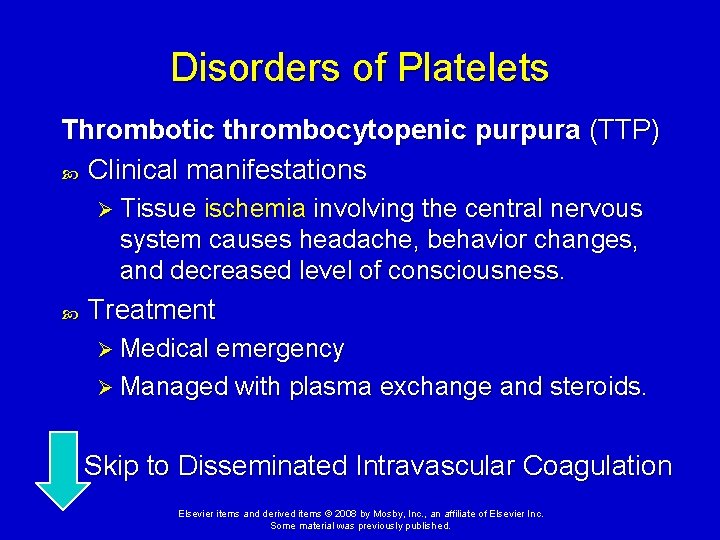
Disorders of Platelets Thrombotic thrombocytopenic purpura (TTP) Clinical manifestations Ø Tissue ischemia involving the central nervous system causes headache, behavior changes, and decreased level of consciousness. Treatment Ø Medical emergency Ø Managed with plasma exchange and steroids. Skip to Disseminated Intravascular Coagulation Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
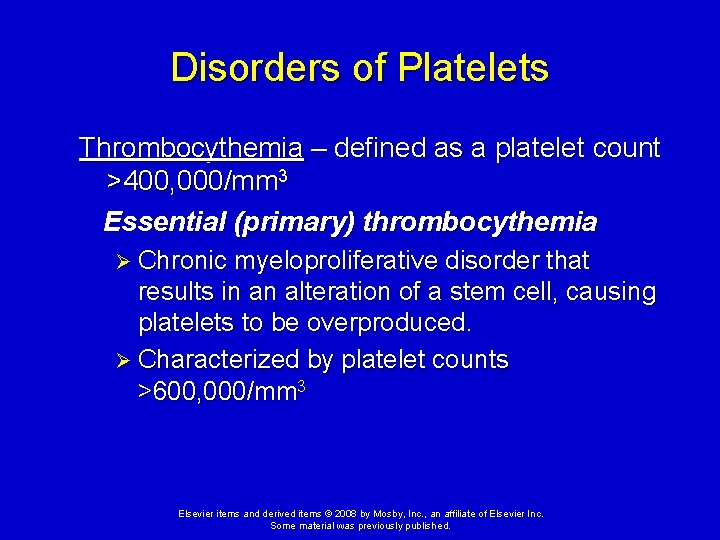
Disorders of Platelets Thrombocythemia – defined as a platelet count >400, 000/mm 3 Essential (primary) thrombocythemia Ø Chronic myeloproliferative disorder that results in an alteration of a stem cell, causing platelets to be overproduced. Ø Characterized by platelet counts >600, 000/mm 3 Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disorders of Platelets Essential (primary) thrombocythemia Clinical Manifestations Ø May be asymptomatic, or it may cause thrombosis with decreased perfusion to the extremities, myocardium, or intestines. Ø Central nervous system effects can include headache, seizures, and stroke. Ø Paradoxically, some individuals may develop mild hemorrhaging, especially into the gastrointestinal tract. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disorders of Platelets Essential (primary) thrombocythemia Treatment Ø Prevention of thrombosis and hemorrhage. Ø Management includes the administration of hydroxyurea (a myelosuppressive agent). Ø Interferon and aspirin also may be used in the treatment of the disease. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Alterations of Platelet Function Inadequate platelet function is most commonly the result of: Drugs - NSAIDs, antibiotics, cardiovascular drugs, psychotropic drugs, anesthetics, and some foods. Ø Systemic conditions - renal failure, autoimmunity disorders, and cardiopulmonary bypass. Ø Hematological alterations - leukemia, multiple myeloma, etc. Ø Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disorders of Coagulation Impaired hemostasis Vitamin K deficiency Ø Vitamin K is necessary for synthesis and regulation of prothrombin, the prothrombin factors (II, VII, X), and proteins C and S (anticoagulants) Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
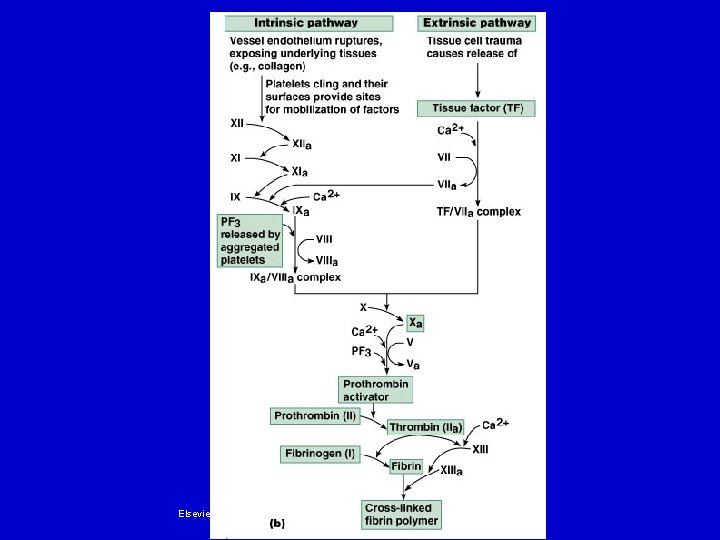
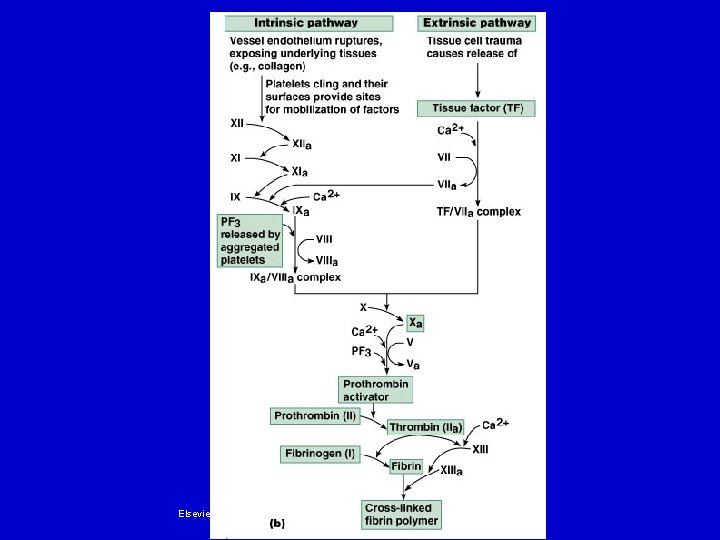
Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disorders of Coagulation Impaired hemostasis Liver disease Ø Clotting factors are made in the liver. Ø Liver disease causes a broad range of hemostasis disorders: • Defects in coagulation, fibrinolysis, and platelet number and function Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disorders of Coagulation Impaired hemostasis Inherited causes Ø Hemophilia - a group of sex-linked recessive disorders that cause insufficient production of clotting factors. Ø Von Willebrand disease - caused by a factor VIII deficiency; inherited as an autosomal dominant disorder. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disseminated Intravascular Coagulation (DIC) Complex, acquired disorder in which clotting and hemorrhage occur simultaneously. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disseminated Intravascular Coagulation (DIC) Occurs as a complication of a broad spectrum of clinical conditions, especially: Ø Sepsis Ø Trauma Ø Shock Ø Obstetrical accidents Ø Some viral infections Ø Hematologic disorders Ø Some cancers Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
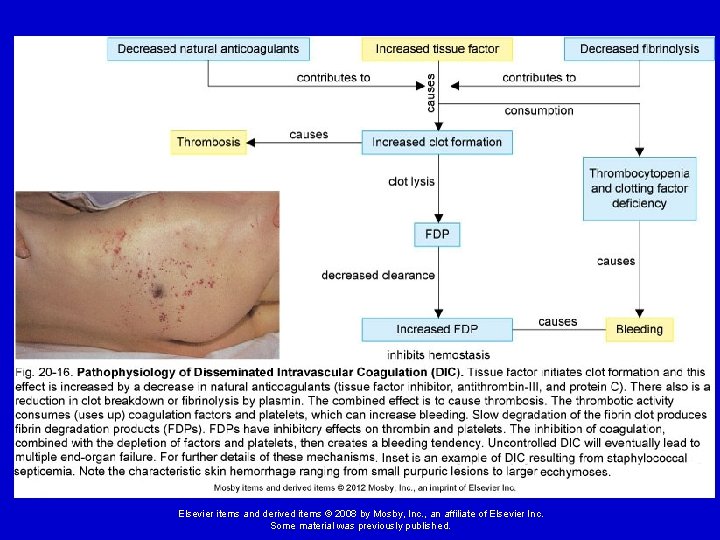
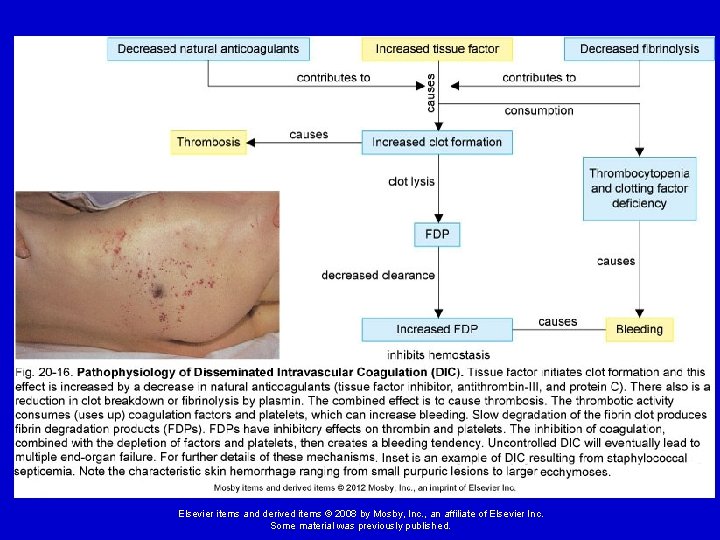
Disseminated Intravascular Coagulation (DIC) Initiated by a stimulus that causes endothelial damage and release of tissue factor (TF). High TF levels trigger systemic coagulation, which consumes clotting factors and platelets. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disseminated Intravascular Coagulation (DIC) At the same time, the clots are being broken down due to the anticoagulant effects of fibrinogen degradation products (FDPs). Ø This can lead to oozing of blood or, in severe cases, hemorrhage. The widespread thromboses created cause ischemia, infarction, and organ hypoperfusion Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Disseminated Intravascular Coagulation (DIC) Clinical signs and symptoms demonstrate wide variability: Ø Bleeding from venipuncture sites Ø Bleeding from arterial lines Ø Purpura, petechiae, and hematomas Ø Symmetric cyanosis of the fingers and toes Because of the patient’s clinical state, the disorder has a high mortality rate. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Thromboembolytic Disorders Certain conditions within the blood vessels predispose an individual to spontaneously develop thrombi. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
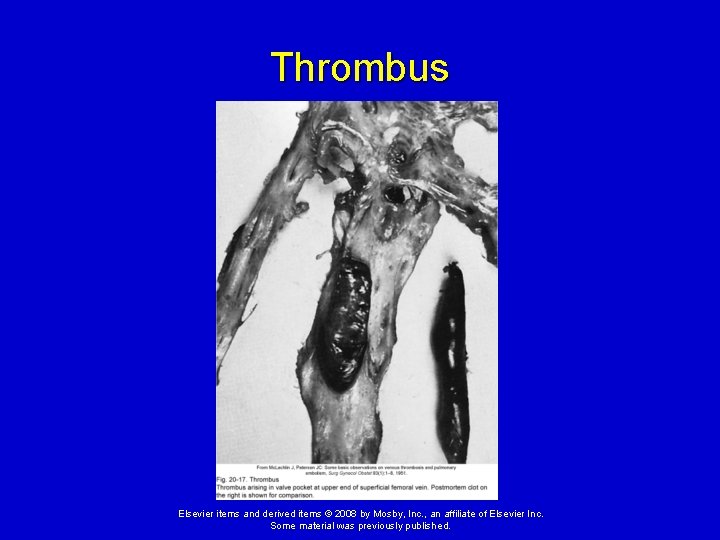
Thromboembolytic Disorders Thrombus - a clot attached to the vessel wall. Ø Eventually reduce or obstruct blood flow to tissues or organs. Ø May detach from the vessel wall and circulating within the bloodstream. Ø Frequently form in deep veins of the leg, especially in varicose veins. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
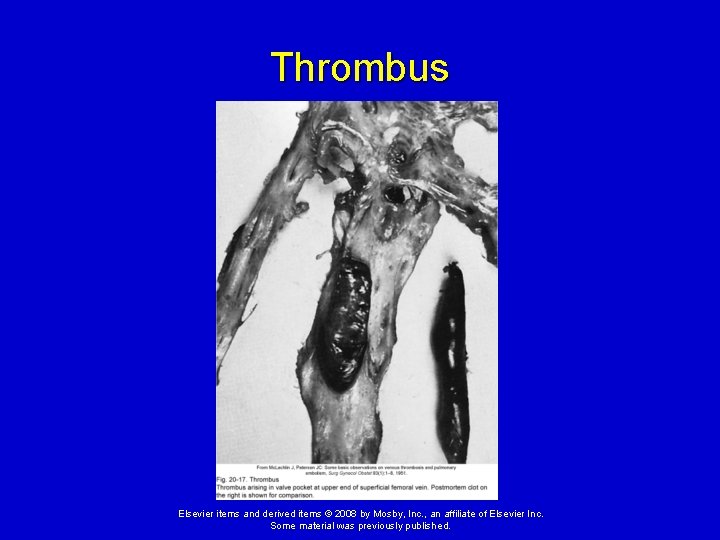
Thrombus Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Thromboembolytic Disorders Embolus - a mass that travels through the bloodstream. Ø An embolus may become lodged in smaller blood vessels, blocking blood flow into the local tissue or organ and leading to ischemia. Ø Emboli from deep leg veins often lodge in the lungs, causing a pulmonary embolism. Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.
Thromboembolytic Disorders Virchow triad - risk for developing spontaneous thrombi is related to: 1) Injury to the blood vessel endothelium 2) Stasis of blood flow 3) Hypercoagulability of the blood Elsevier items and derived items © 2008 by Mosby, Inc. , an affiliate of Elsevier Inc. Some material was previously published.