q Alterations in Hematologic Status Sickle Cell Anemia








- Slides: 40
q Alterations in Hematologic Status— Sickle Cell Anemia Thalassemia Major Aplastic Anemia Hemophilia Idiopathic Thrombocytopenic Purpura n NURS 317

Major functions of Bone Marrow Production of cells n Oxygenation n Nutrient distribution to cells n Immune protection n Waste collection from cells heat production n
Common Diagnostic Assessments n n n n Family History Child’s health history Physical exam Medication use Dietary pattern Lab studies: CBC w/diff, PTT, Hb, Hct, iron studies, bone marrow aspiration/bx Prepare child & family for lab tests

Sickle Cell Anemia (SCA) A global disease

Definition n n http: //www. nhlbi. nih. gov/health/dci/Di seases/Sca/SCA_What. Is. html Sickle cell anemia results from the hereditary presence of abnormal Hgb S in place of Hgb A. When Hgb S becomes deoxygenated (loses oxygen), it tends to form polymers that deform the red blood cells (RBCs) into a sickle shape. Sickled RBCs cannot pass freely through capillaries and cause blockage of small vessels. This can compromise the blood supply to various organs.
Incidence Hereditary hemoglobinopathy; autosomal recessive; 1 African Americans n Hgb S trait is found in 8 to 10% of the American black population. n n n Sickle Cell Anemia– homozygous form (Hb. SS)—most prevalent in US In Western African native blacks, up to 40% of the population carry Hgb S trait.
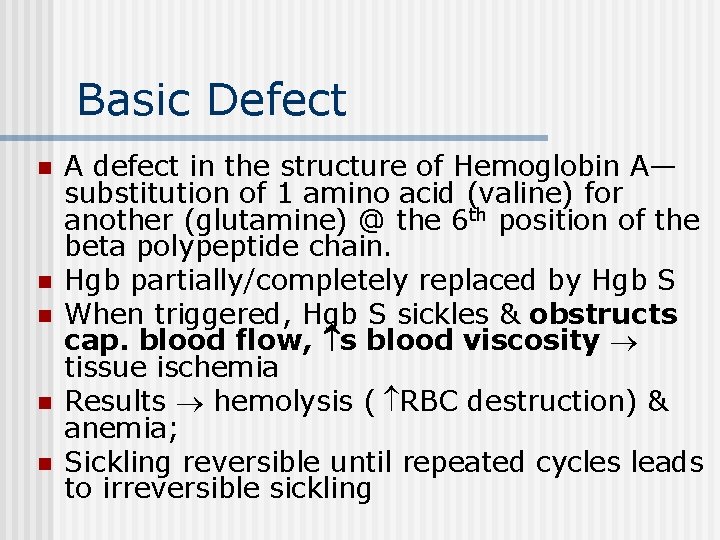
Basic Defect n n n A defect in the structure of Hemoglobin A— substitution of 1 amino acid (valine) for another (glutamine) @ the 6 th position of the beta polypeptide chain. Hgb partially/completely replaced by Hgb S When triggered, Hgb S sickles & obstructs cap. blood flow, s blood viscosity tissue ischemia Results hemolysis ( RBC destruction) & anemia; Sickling reversible until repeated cycles leads to irreversible sickling
Diagnostic Tests n n Rarely seen before 4 -6 mos. Sickledex: sickle turbidity test; finger or heel stick; results in 3 min n n Sickledex does not distinguish between sickle cell trait and sickle cell disease. Hemoglobin electrophoresis is required to distinguish between these 2 disorders. Hgb electrophoresis to “fingerprint” protein Hx, PE, CBC CXR if symptoms
Diagnostic Tests (cont’d) n Peripheral Blood Smear n The routine peripheral blood smear does not contain sickled red blood cells unless hypoxemia (inadequate levels of oxygen in the blood) or a precipitating factor (such as a red blood cell poison or drug) is present.
Diagnostic Tests (cont’d) n Electrophoresis n Both sickle cell disease (homozygous for hemoglobin S) and sickle cell trait (heterozygous for Hgb S) can be detected by this test. n This test separates different types of hemoglobin based on electrical charge. Hgb S can be differentiated from Hgb A and other types of Hgb.
Diagnostic Tests (cont’d) n Normal Results n n In hemoglobin electrophoresis, no Hgb S should be present. Normal hemoglobins in an adult are mostly Hgb A with small amounts of Hgb A 2 and Hgb F. What do abnormal results mean? n n sickle cell trait sickle cell anemia

Pathophysiology n Spleen—enlarged, if untreated, becomes fibrous & ineffective susceptibility to infection. n Liver—failure & necrosis 2 ndary to impaired circulation. Hepatomegaly and tenderness are common sx. n Kidney— perfusion 2 ndary to congestion of glomerular capillaries & tubular arterioles hematuria, inability to concentrate urine, enuresis, & possible nephrotic syndrome.

Pathophysiology (cont’d) n Bones— n n n Hyperplasia of bone marrow osteoporosis weakened bones lordosis and kyphosis or other skeletal deformities Chronic hypoxia possible osteomyelitis from salmonella “Hand-foot Syndrome”—occurs in children 6 mos-2 yrs. Caused by infarction of shorttubular bones. Sx: swelling & pain of soft tissue of hands & feet. Usually resolves in 2 -3 wks.
Pathophysiology (cont’d) n CNS—primarily R/T ischemia n n n MAJOR INFARCT—Stroke or CVA paralysis MINOR INFARCT—HA, aphasia, learning disability, weakness, convulsions, visual changes 2 ndary to retinopathy & retinal detachment. Heart—Decompensation & failure 2 ndary to chronic anemia CHF, pulmonary hypertension, tachycardia
Pathophysiology (cont’d) n Blood— Rate of destruction of RBC’s > rate of RBC production n RBC’s lifespan is to 10 -15 days (compared to 120 days for nml RBC) n Hgb, Hct & RBC count n Reticulocyte count, bilirubin & uric acid n
Pathphysiology (cont’d) n Other sx: n n n n Generalized weakness Anorexia Joint, back, and abdominal pain Fever Vomiting Possible leg ulcers Failure to thrive, rate of growth & development
Sickle Cell Crisis n Triggers n n n n Acute illness Dehydration Strenous exercise Hypoxic conditions Trauma Respiratory illness Results: acute pain, cell destruction, infarcts, organ damage
Types of Crises n Vaso-occlusive: PAIN, swollen joints, vomiting, fever, anorexia, dactylitis n Acute splenic sequestration: liver & spleen, HR dyspnea, weakness, pallor, shock n Aplastic crisis: weakness, pallor, dyspnea, tachycardia, shock n Hyperhemolytic— most rare form. Caused by excess RBC destruction.
Other complications n Acute chest syndrome: chest pain, cough, fever, abdominal pain. n Hydroxyurea can help prevent this. Megaloblastic anemia n Hyperhemolytic crisis n Cerebrovascular injury (stroke) n Overwhelming infections n

TREATMENT n Primary Goals: 1. Prevent Crisis (avoid sickling phenomenon)—through adequate oxygenation & hydration in every day life activities. Hydroxyurea may be used prophylactically in adolescents and older adults. Folic Acid 1 mg daily is also recommended to restore folate stores needed for erythropoiesis. 2. Treat crisis as an emergency when it occurs—determine etiology quickly and treat appropriately

Nursing Management n n n n n Adequate hydration (also any electrolyte replacement if needed) Pain management Promote rest Treat any infections Blood transfusions if needed Monitor O 2 – supplement if needed Oral hygiene Maintain nutrition Family support and education--
GUIDANCE: Topics that are usually covered include: n Hours that medical staff are available and contact information to use when people with SCD or caretakers have questions n A plan for what to do and where to get care if a person has a fever, pain, or other signs of SCD complications that need immediate attention n How SCD is inherited and the risk of having a child with SCD n The importance of regular medical visits, screening tests, and evaluations n How to recognize and manage pain n How to palpate (feel) a child’s spleen. Because of the risk of splenic sequestration crisis, caretakers should learn how to palpate a child’s spleen. They should try to feel for the spleen daily and more frequently when the child is ill. If they feel that the spleen is bigger than usual, they should call the care provider. https: //www. nhlbi. nih. gov/health-topics/sca/treatment#hematopoietic
NURSING CARE n Pain Control—strive to prevent pain. n n Opioids as morphine, oxycodone, hydromorphone & methadone are preferred. Give IV or PO for severe pain round-the-clock. PCA pumps are great! Avoid Demerol (Meperidine) - ↑seizure risk Tylenol & Ibuprofen may be used after dx is made Use non-pharmacologic methods also Heat (e. g. K-pad)to affected joints may be soothing by O 2 with vasodilation.
NURSING CARE n Hydration– n n Accurate I & O essential IV/PO fluids up to 150 ml/kg/day will promote hemodilution Note color of urine—sometimes brown Prevent tissue deoxygenation n n Avoid Avoid strenuous activity environments with low O 2 concentration extremes in temp- esp. cold environment emotional stress known sources of infection
Child/Family Education How to manage & minimize crisis: avoid dehydration, cold, stress, hypoxia, acute illness, etc. n Signs of infection n Importance of immunizations n Antibiotic administration if ordered n Education & support re: long term effects n Genetic counseling n
Thalassemia Major n Autosomal recessive Defective Hgb; RBCs fragile w/short life span anemia, hemolysis n Main Tx: blood transfusions n Hemochromatosis – iron overload – occurs from hemolysis of transfused and defective RBCs n Chelation tx done to eliminate excess Fe--desferrioxamine n
Nursing Considerations Numerous blood transfusions n Assess s/s of hemosiderosis n Assess s/s infection n Folic acid supplementation n Iron chelation tx as ordered n Family support n Possible bone marrow transplant n
Aplastic Anemia n n Definition: Condition where all formed elements of the blood are depressed. Pancytopenia or Triad: Anemia (↓ RBC's) n Leukopenia (↓ WBC's) n Thrombocytopenia (↓ platelets) n
n Etiology of A. A. Primary (congenital) n Secondary (acquired) -- often secondary to drugs e. g. chemotherapy or other meds that “shut down” bone marrow function n n Diagnosis -- Bone marrow aspiration or biopsy
n Therapeutic Management -- Goal: Restore bone marrow function Immunosuppressive therapy n Bone marrow transplantation ** choice 85% survival rate n n Nursing Considerations -- Similar to child with leukemia Prepare family for diagnostic & therapeutic procedures n Preventing complications from severe pancytopenia n Emotionally supporting them in terms of a potentially fatal outcome n
Hemophilia n n n Deficiency in specific clotting factor X-linked recessive trait; 2 most common n Hemophilia A (classic) n Hemophilia B (Christmas Disease) Uncontrolled bleeding from wounds into joints, muscles, & other body tissues Spontaneous & severe uncontrolled bleeding in severe form 3 levels based on amount of factor
Common Labs Hx & PE, symptoms n PTT prolonged n Factor VIII, IX levels n Normal: PT, thrombin, bleeding time, fibrinogen, platelet count n May do liver Bx to r/o other causes n
Signs & symptoms Excessive bleeding from circumcision n Bleeding w/teething n Hemarthosis – cardinal sign n Bruises in various stages n Hematuria n Nose bleeds n Oral bleeding n
Nursing Management n Control localized bleeding: n n n n Direct pressure for extended period of time like 10 minutes Ice Elevation of affected limb Avoid injections when possible No rectal temps Monitor for bleeding (joints, urine, stool, etc) Provide pain relief Monitor neuro status if possible head bleeds
Nursing Management Administration of Factor replacement as needed n Factor VIII concentrate (Antihemophilia factor {AHF} ), or DDAVP , a synthetic form of vasopressin that is the treatment of choice in mild hemophilia & von Willebrand disease. Should increase Factor VIII activity 3 -4 fold. n
Teaching Considerations n n n n n Teach family: factor administration/storage n May have Mediport & parents know how to access & administer via central line in emergency DDAVP administration—nasal spray or injection Avoid ASA type products Avoid contact sports Medic alert tag Avoid constipation Good nutrition Good oral hygiene Genetic counseling Protective environment for infants/toddlers
Idiopathic Thrombocytopenia Purpura (ITP) n n n Excessive destruction of platelets Purpura (from petechiae under skin) Normal bone marrow Most common bleeding disorder in children 80% between 2 -5 yrs old and usually last ~ 6 m Usually after viral infection Symptoms when platelet ct < 20, 000

Therapeutic Management n IF medical tx is indicated, then may use one of the following regimens High dose glucocorticoids--IV n IVIG—expensive and takes long to administer and monitor pt n Platelet transfusion concurrently with IVIG n Anti-D antibody—controversial but may prolong survival of platelets. Can be given in 1 dose over 5 -10 minutes. n
Nursing Considerations n n n n Stress activity restriction Prevention of head injuries; instruct parents to get med eval if head or abd injury Assess for bleeding/bruising Oral care support No rectal temps – No ASA products Splenectomy if has for 1 yr and tx not successful Family support & teach on how to control bleeds
n There you have it!