Allopurinol for the treatment of essential hypertension EHTN






- Slides: 48
Allopurinol for the treatment of essential hypertension (EHTN) Farahnak Assadi, MD Emeritus Professor of Pediatrics Chief Section of Nephrology
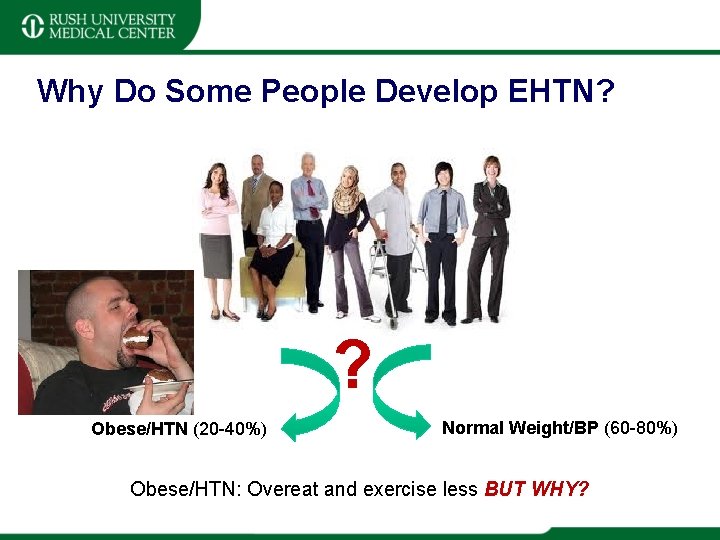
Why Do Some People Develop EHTN? ? Obese/HTN (20 -40%) Normal Weight/BP (60 -80%) Obese/HTN: Overeat and exercise less BUT WHY?
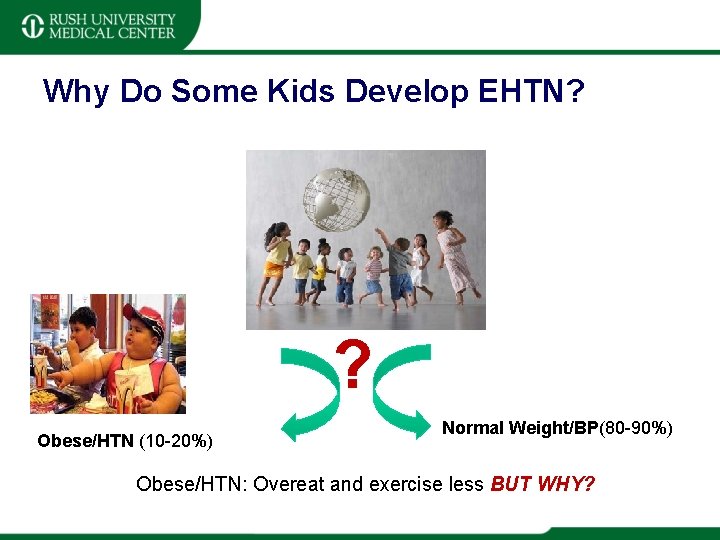
Why Do Some Kids Develop EHTN? ? Obese/HTN (10 -20%) Normal Weight/BP(80 -90%) Obese/HTN: Overeat and exercise less BUT WHY?
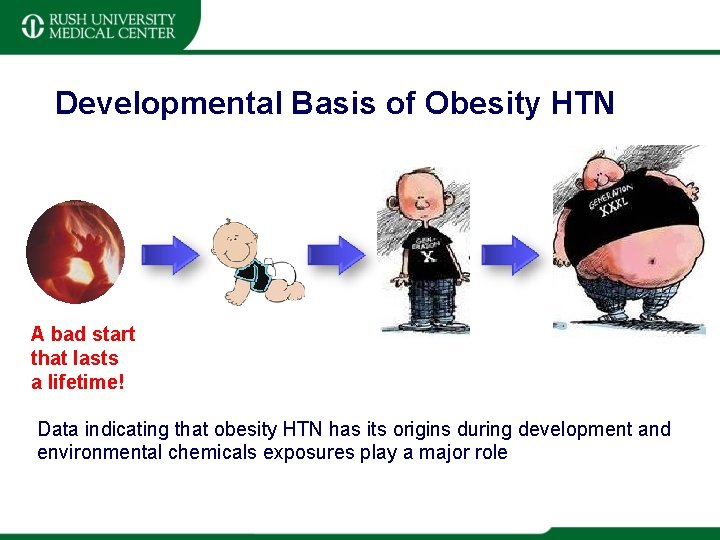
Developmental Basis of Obesity HTN A bad start that lasts a lifetime! Data indicating that obesity HTN has its origins during development and environmental chemicals exposures play a major role
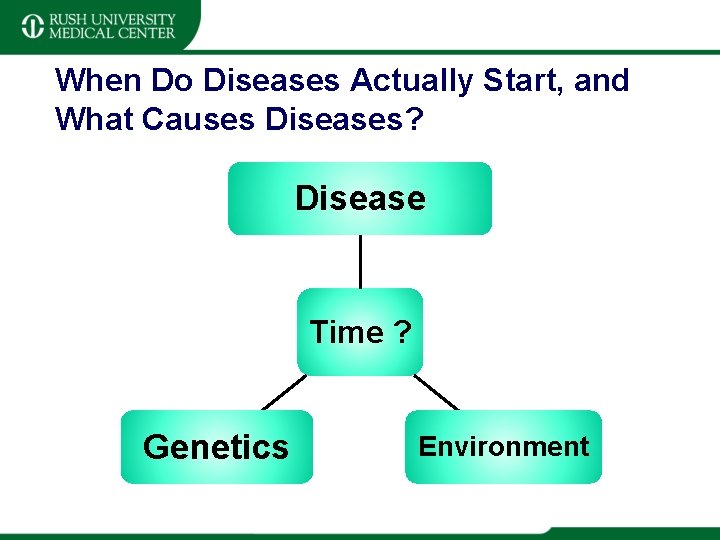
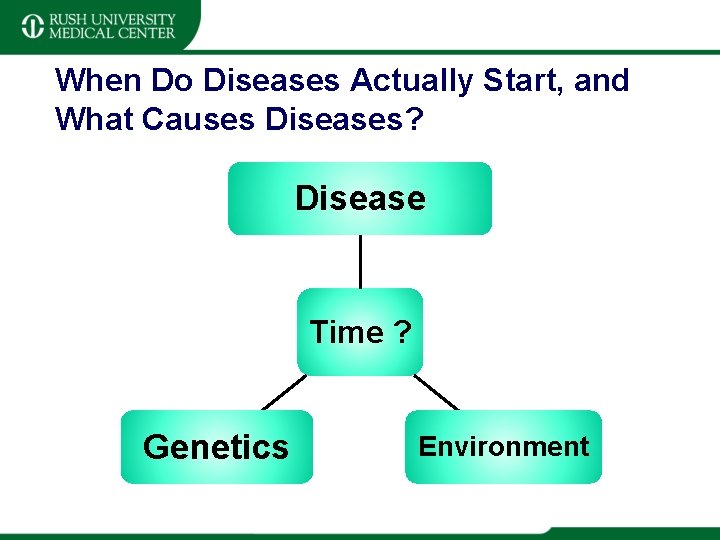
When Do Diseases Actually Start, and What Causes Diseases? Disease Time ? Genetics Environment
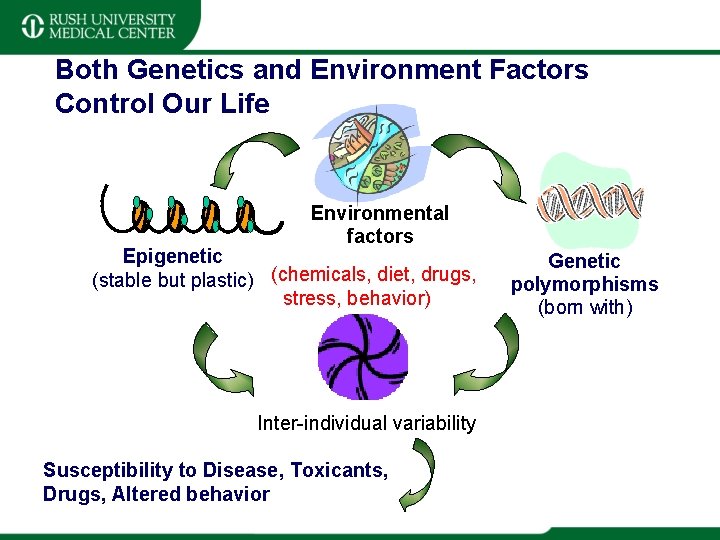
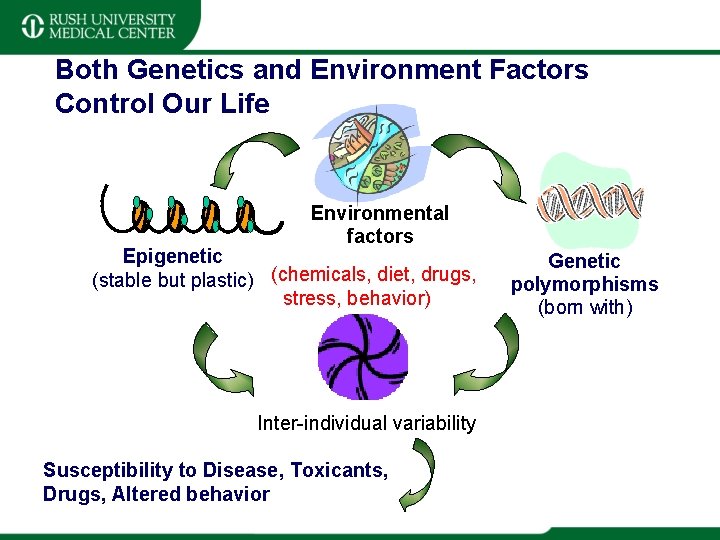
Both Genetics and Environment Factors Control Our Life Environmental factors Epigenetic (stable but plastic) (chemicals, diet, drugs, stress, behavior) Inter-individual variability Susceptibility to Disease, Toxicants, Drugs, Altered behavior Genetic polymorphisms (born with)
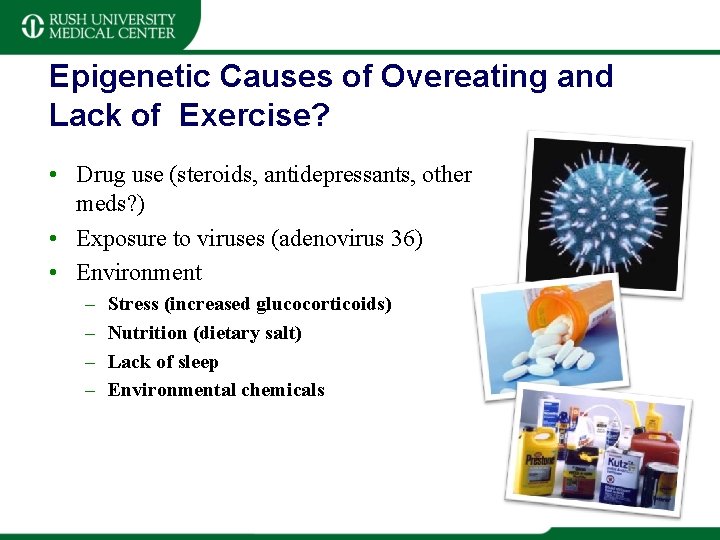
Epigenetic Causes of Overeating and Lack of Exercise? • Drug use (steroids, antidepressants, other meds? ) • Exposure to viruses (adenovirus 36) • Environment – – Stress (increased glucocorticoids) Nutrition (dietary salt) Lack of sleep Environmental chemicals
Epidemiologic studies • In Japanese the incidence of ETN approaches 50% • The mean sodium intake in Japanese is >400 mmol/day. • In Eskimo the average sodium intake is very low <50 mmol/day and EHTN is virtually nonexistent. © 2007 RUSH University Medical Center
Renal Handling of Sodium • Excessive sodium intake alone is not sufficient to cause HTN, because the sodium retention and ECF volume expansion result in increased urinary sodium excretion that eventually normalize cardiac output and BP. • Additional predisposing factors must exist that lead to the development of HTN in certain individual when the sodium intake is >60 -70 mmol/day. • Guyton AC. Hypertension 1987; 10: 1 -6 © 2007 RUSH University Medical Center
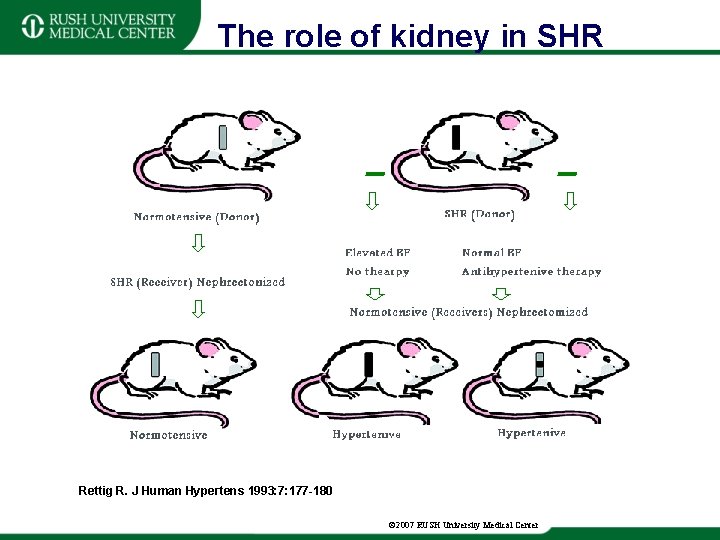
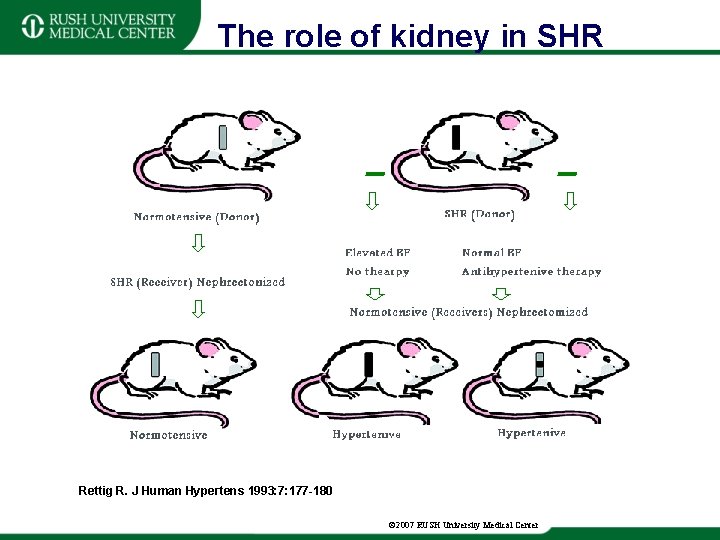
The role of kidney in SHR Rettig R. J Human Hypertens 1993: 7: 177 -180 © 2007 RUSH University Medical Center
Role of kidney in Human EHTN • In patients with ESRD due to EHTN, bilateral nephrectomy and a well-functioning allograft from a normotensive cadaver, cures EHTN • Incidence of EHTN in recipients of cadaver kidneys correlates with the incidence of EHTN in the family of donors • • Curttis jj et al. N Engl J Med 1983; 309: 1009=1015 Guidi E, et al. Nephron 1985; 41: 14 -21 © 2007 RUSH University Medical Center
Genes Causing EHTN • Aldosterone synthesis gene (CYp 11 B 2) mutations. • Angiotensin II type 1 receptor gene (ATI) polymorphism. • Endothelial nitric oxide synthesis gene (e. NOS) mutations. • G-protein β 3 subunit gene (GNβ 3) variant. • • Caulfield M et al N Engl J Med 1994; 330: 1629 -1633 Benjafield AV et al. Hypertens. 1998; 32: 1094 -1097 Siffert W, et al. Nat Genetics 1998; 18: 45 -48 Davies E, et al. Hypertens. 1999; 33: 703 -707
Impaired natriuresis: a prerequisite in EHTN • • Increase ECF volume Na/K ATPase inhibition Increase ICF sodium concentration Increase ICF calcium concentration Vasoconstriction Increase systemic vascular resistance Development of EHTN Blaustein MP. Hypertension 1984; 6: 445 -453 © 2007 RUSH University Medical Center
Pathogenesis of EHTN • There is a genetically predetermined impairment in the renal ability to excrete sodium or “impaired natriuretic capacity. ” • The prevalence of EHTN among offspring has been reported to be 46% if both parents are hypertensive, and 28% if one parent is hypertensive, and only 3% if neither parent is hypertensive. Ayman D. Arch Intern Med 1934; 53: 792 -802 © 2007 RUSH University Medical Center
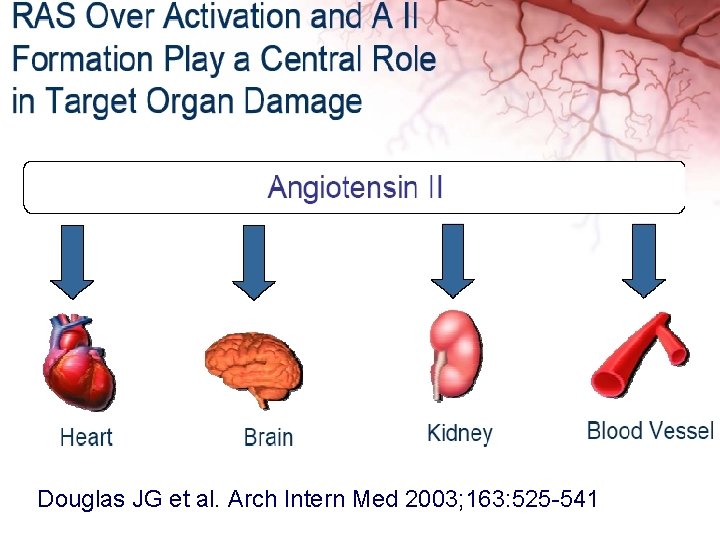
Essential hypertension(EHTN) • EHTN is a public Health problem worldwide and its burden on our health care system is becoming enormous. • Many children with obesity are not aware that they have HTN. • Over activity of renin-angiotensin system (RAS) is the main cause of primary HTN. • RAS over activity can lead to myocardial hypertrophy, CVD and CKD and stoke. © 2007 RUSH University Medical Center

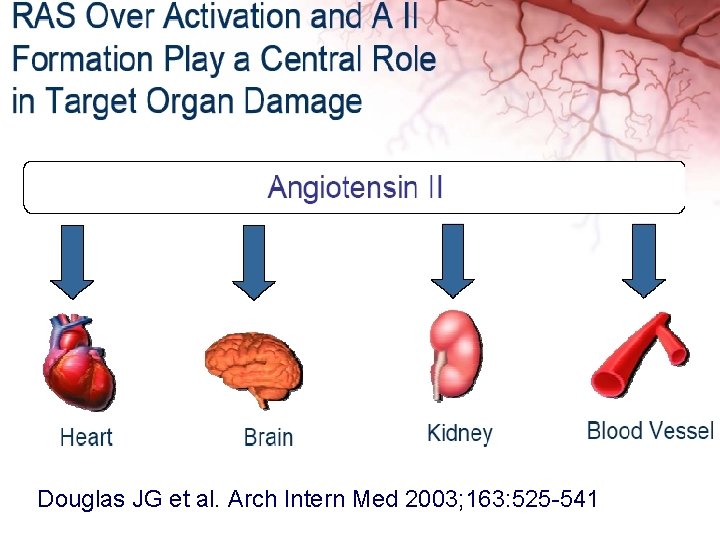
Douglas JG et al. Arch Intern Med 2003; 163: 525 -541


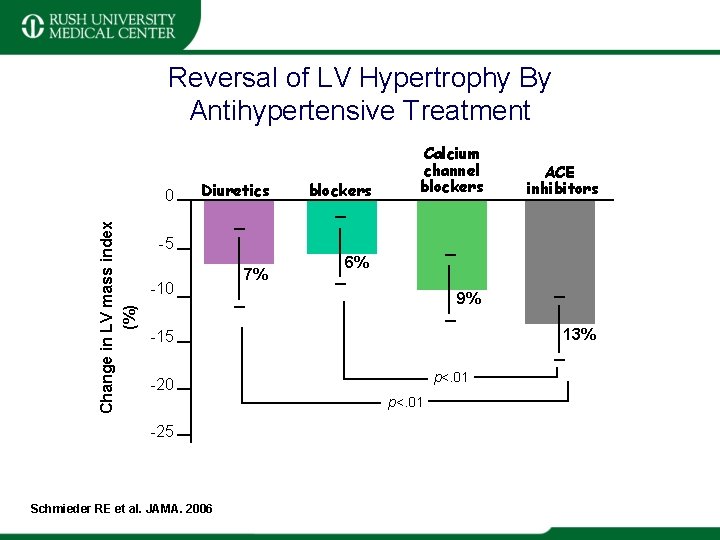
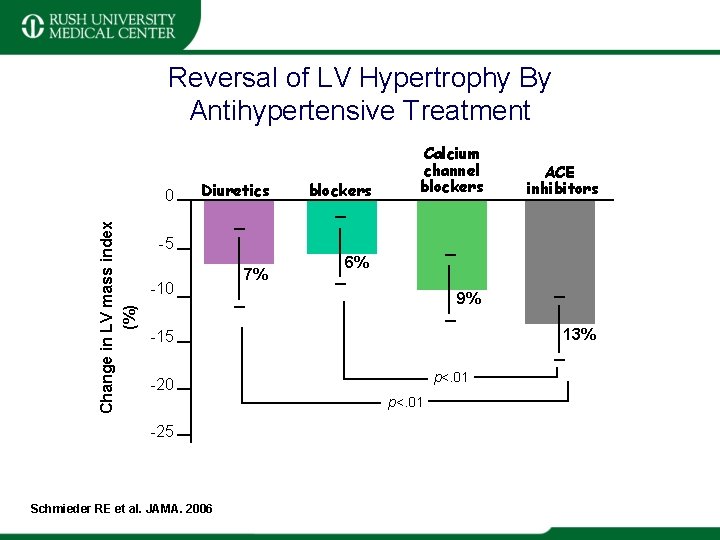
Reversal of LV Hypertrophy By Antihypertensive Treatment Change in LV mass index (%) 0 Diuretics blockers Calcium channel blockers ACE inhibitors -5 -10 7% 6% 9% 13% -15 p<. 01 -20 p<. 01 -25 Schmieder RE et al. JAMA. 2006

Uric acid and EHTN • EHTN is frequently associated with hyperuricemia in both adult and pediatric patients. • More than 60% of children with EHTN have serum uric acid (UA) levels above 5. 5 mg/d. L. • UA causes HTN through the activation of the RAS, down regulation of nitric oxide, and vascular endothelial dysfunction. • Elevated UA level is a predictor of incident HTN and cardiovascular disease. • Feig DI et al. JAMA 2008; 300: 924 -932
Hypothesis • Treating EHTN with usual antihypertensive agents does not completely reduce cardiovascular risk related to uric acid (UA) levels. • Lowering serum UA levels with allopurinol may provide greater benefit than simply treating HTN with the conventional therapy.
Purpose of the study • ACE inhibition in combination with allopurinol may reduce BP more effectively than ACE inhibitor alone in hyperuricemic children with newly diagnosed EHTN.
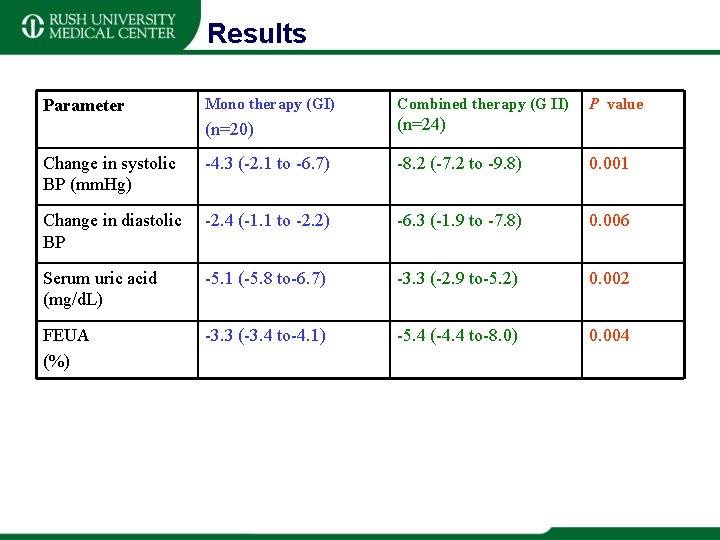
Patients • Forty- four children, aged 7 -19 years, with newly diagnosed, never treated EHTN and serum UA levels > 5. 5 mg/d. L were studied. • Patients were randomized in to two groups. Group 1 (n=20) received enalepril (0. 3 mg/kg twice daily) for 8 weeks. • Group 2 (n=24) received enalepril in combination with allopurinol (100 mg twice daily) for 8 weeks.
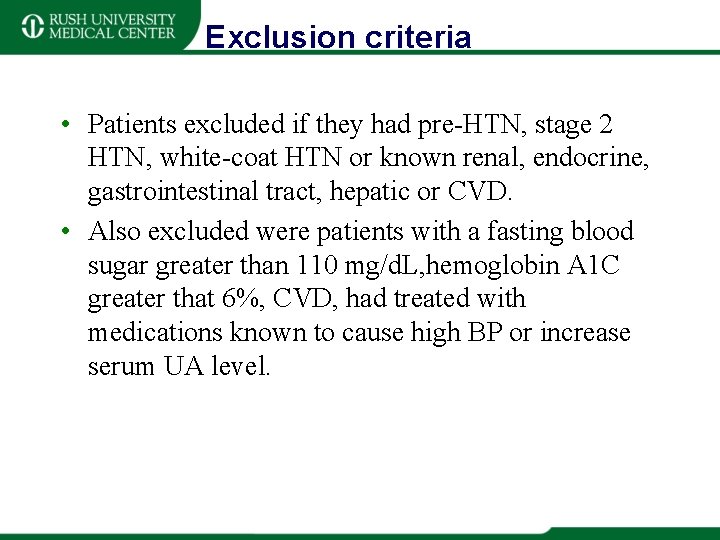
Exclusion criteria • Patients excluded if they had pre-HTN, stage 2 HTN, white-coat HTN or known renal, endocrine, gastrointestinal tract, hepatic or CVD. • Also excluded were patients with a fasting blood sugar greater than 110 mg/d. L, hemoglobin A 1 C greater that 6%, CVD, had treated with medications known to cause high BP or increase serum UA level.
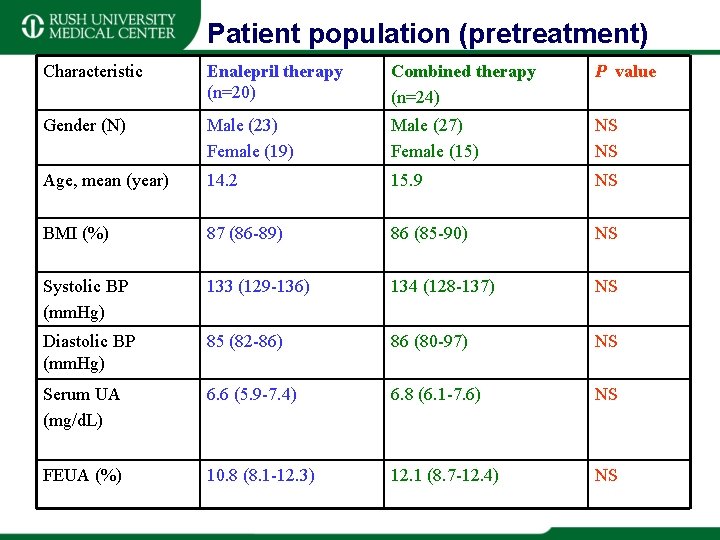
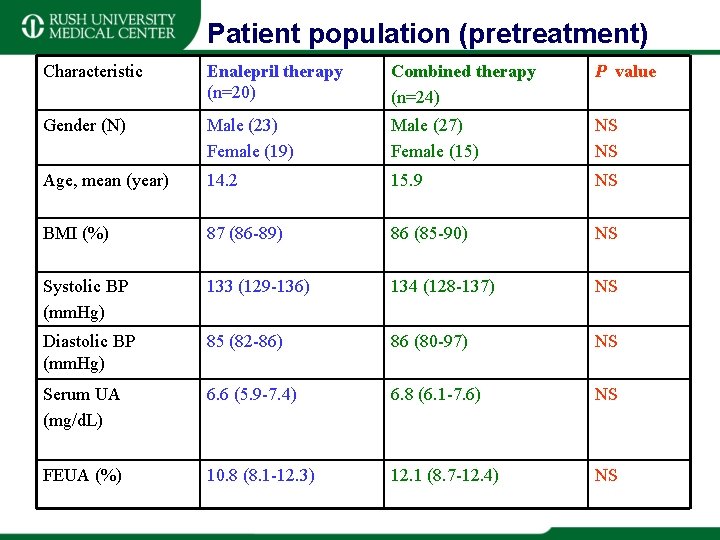
Patient population (pretreatment) Characteristic Enalepril therapy (n=20) Combined therapy (n=24) P value Gender (N) Male (23) Female (19) Male (27) Female (15) NS NS Age, mean (year) 14. 2 15. 9 NS BMI (%) 87 (86 -89) 86 (85 -90) NS Systolic BP (mm. Hg) 133 (129 -136) 134 (128 -137) NS Diastolic BP (mm. Hg) 85 (82 -86) 86 (80 -97) NS Serum UA (mg/d. L) 6. 6 (5. 9 -7. 4) 6. 8 (6. 1 -7. 6) NS FEUA (%) 10. 8 (8. 1 -12. 3) 12. 1 (8. 7 -12. 4) NS
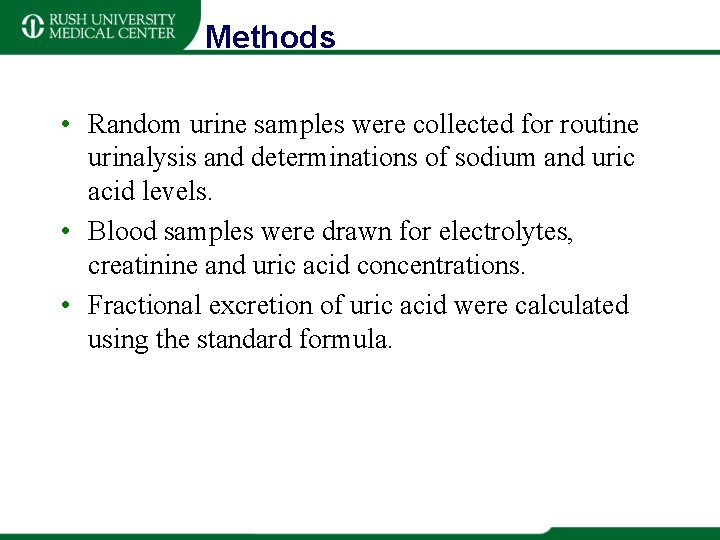
Methods • Random urine samples were collected for routine urinalysis and determinations of sodium and uric acid levels. • Blood samples were drawn for electrolytes, creatinine and uric acid concentrations. • Fractional excretion of uric acid were calculated using the standard formula.
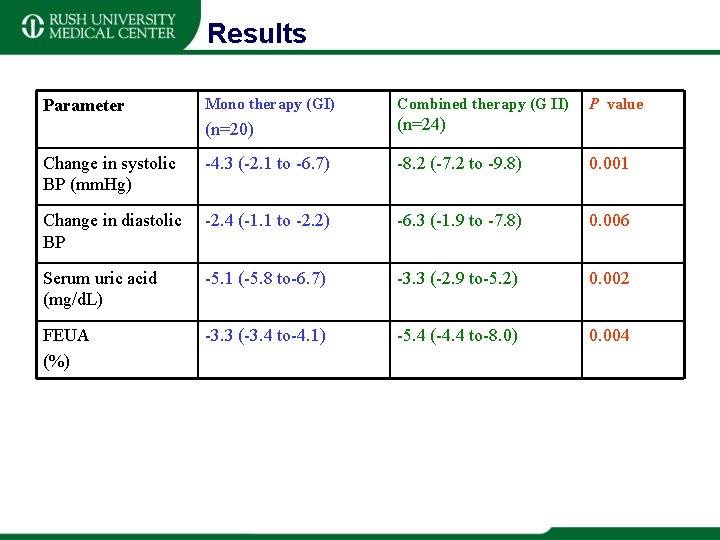
Results Mono therapy (GI) Combined therapy (G II) (n=20) (n=24) Change in systolic BP (mm. Hg) -4. 3 (-2. 1 to -6. 7) -8. 2 (-7. 2 to -9. 8) 0. 001 Change in diastolic BP -2. 4 (-1. 1 to -2. 2) -6. 3 (-1. 9 to -7. 8) 0. 006 Serum uric acid (mg/d. L) -5. 1 (-5. 8 to-6. 7) -3. 3 (-2. 9 to-5. 2) 0. 002 FEUA (%) -3. 3 (-3. 4 to-4. 1) -5. 4 (-4. 4 to-8. 0) 0. 004 Parameter P value
Conclusions • Allopurinol in combination with enalepril can reduce BP more effectively than enalepril alone in hyperuricemic children with newly diagnosed EHTN. • Strategies to lower the risk of CVD in children with EHTN should include monitoring serum uric acid level treatment regimens that lower uric acid may be indicated to decrease the incidence of CVD by reducing serum uric acid level.
Future Direction • Increased dietary intake of fructose, which is a known cause of hyperuricemia, may be contributing to the current epidemic of obesity and HTN. • Ongoing clinical trials will elucidate the role of uric acid in human HTN and will determine whether control of uuric acid may be a new way to prevent or treat EHTN.
The End…. but just the beginning
© 2007 RUSH University Medical Center
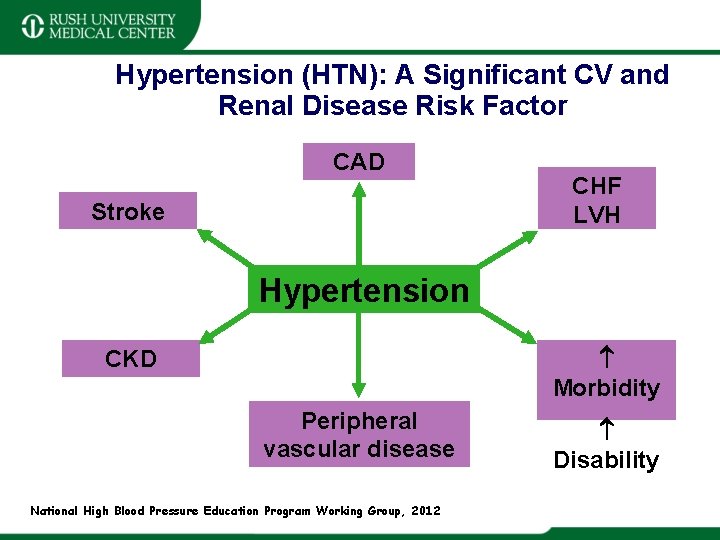
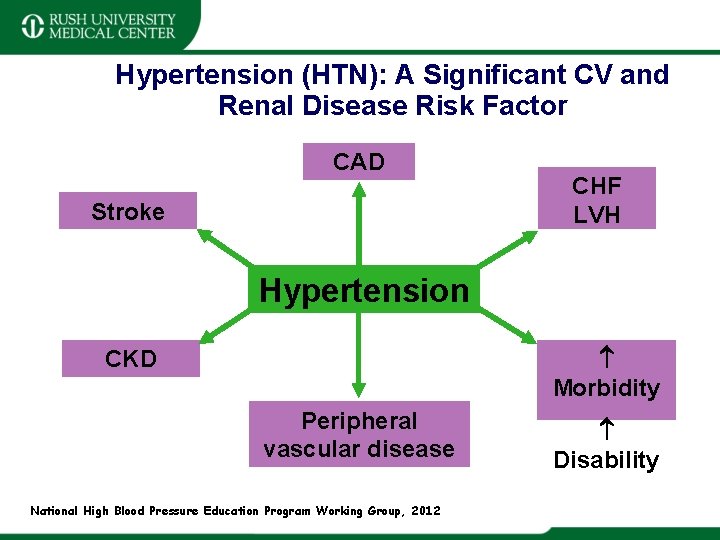
Hypertension (HTN): A Significant CV and Renal Disease Risk Factor CAD Stroke CHF LVH Hypertension Morbidity CKD Peripheral vascular disease National High Blood Pressure Education Program Working Group, 2012 Disability
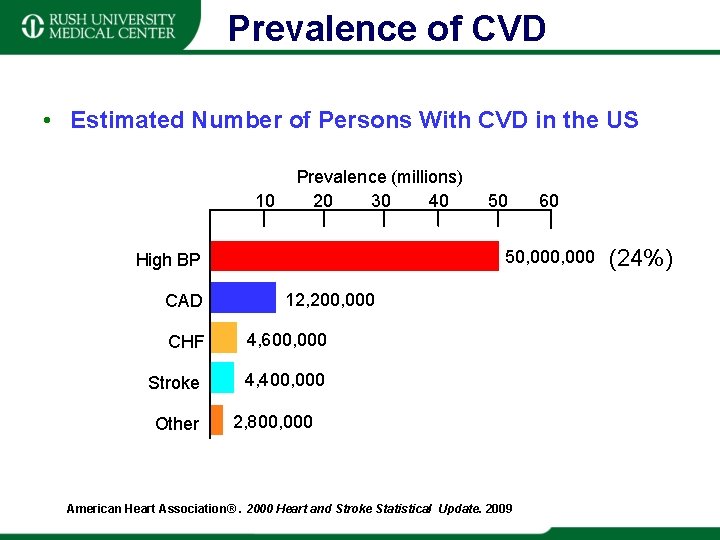
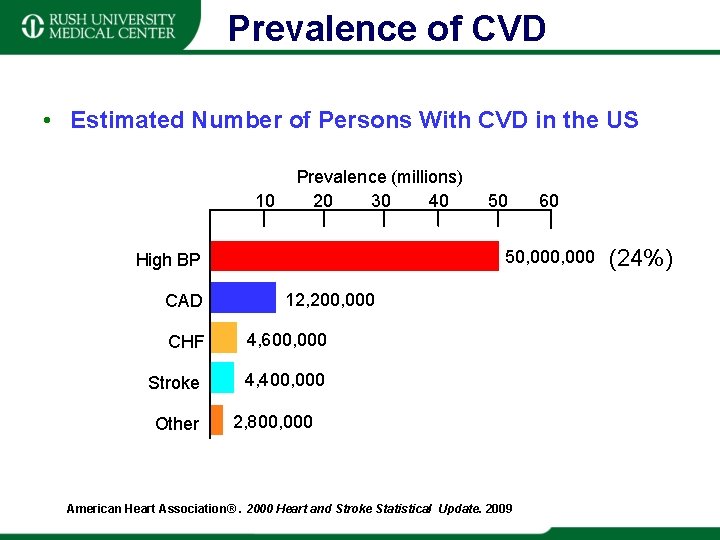
Prevalence of CVD • Estimated Number of Persons With CVD in the US 10 Prevalence (millions) 20 30 40 12, 200, 000 CHF 4, 600, 000 Stroke 4, 400, 000 Other 60 50, 000 High BP CAD 50 2, 800, 000 BP=blood pressure, CAD=coronary artery disease, CHF=congestive heart failure American Heart Association®. 2000 Heart and Stroke Statistical Update. 2009 (24%)
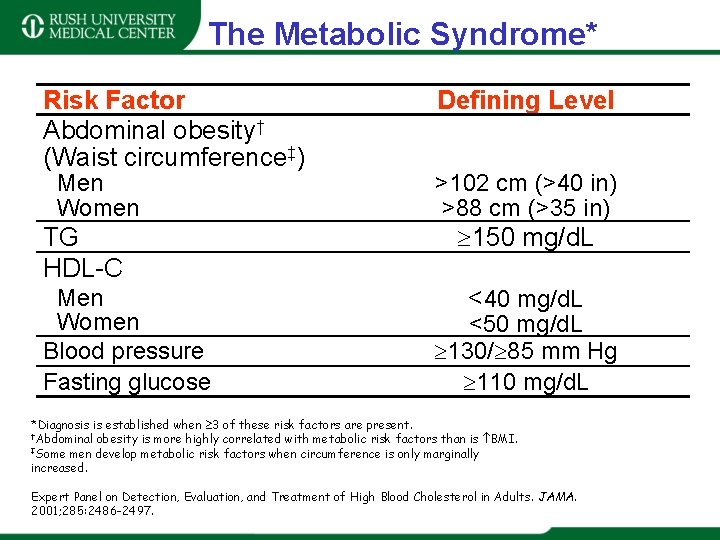
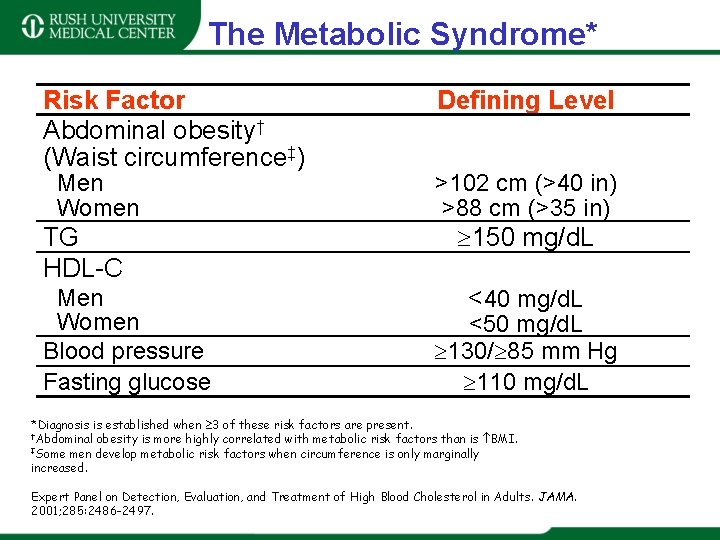
The Metabolic Syndrome* Risk Factor Abdominal obesity† (Waist circumference‡) Men Women TG HDL-C Men Women Blood pressure Fasting glucose Defining Level >102 cm (>40 in) >88 cm (>35 in) 150 mg/d. L <40 mg/d. L <50 mg/d. L 130/ 85 mm Hg 110 mg/d. L *Diagnosis is established when 3 of these risk factors are present. †Abdominal obesity is more highly correlated with metabolic risk factors than is BMI. ‡Some men develop metabolic risk factors when circumference is only marginally increased. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA. 2001; 285: 2486 -2497.
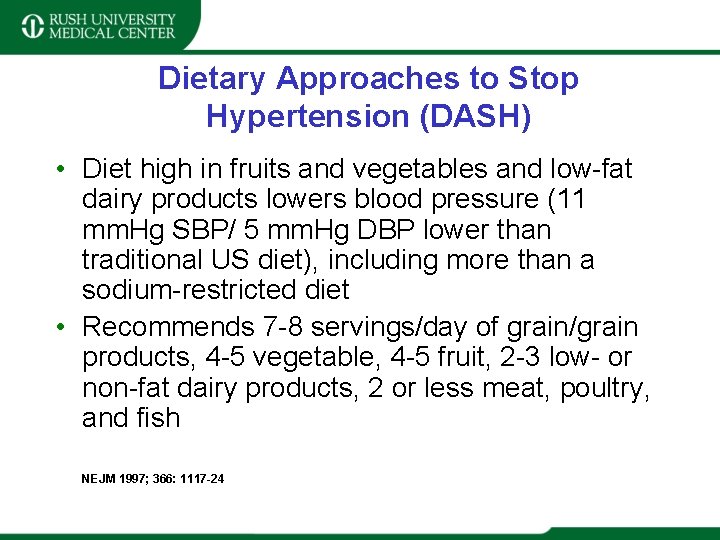
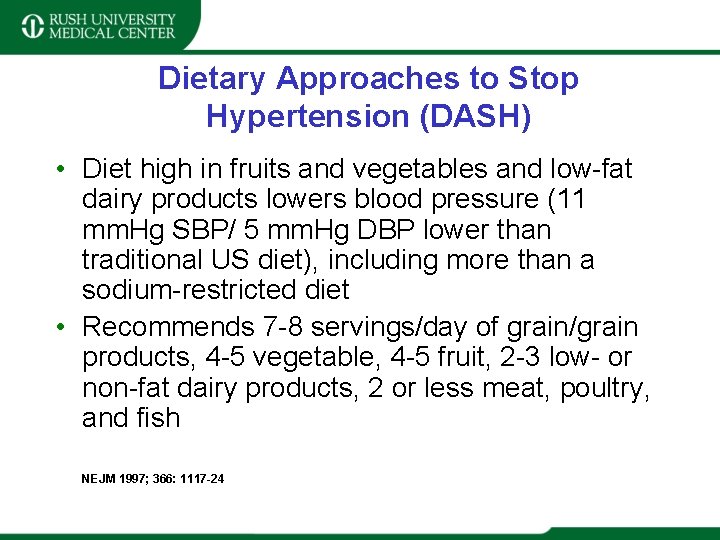
Dietary Approaches to Stop Hypertension (DASH) • Diet high in fruits and vegetables and low-fat dairy products lowers blood pressure (11 mm. Hg SBP/ 5 mm. Hg DBP lower than traditional US diet), including more than a sodium-restricted diet • Recommends 7 -8 servings/day of grain/grain products, 4 -5 vegetable, 4 -5 fruit, 2 -3 low- or non-fat dairy products, 2 or less meat, poultry, and fish NEJM 1997; 366: 1117 -24
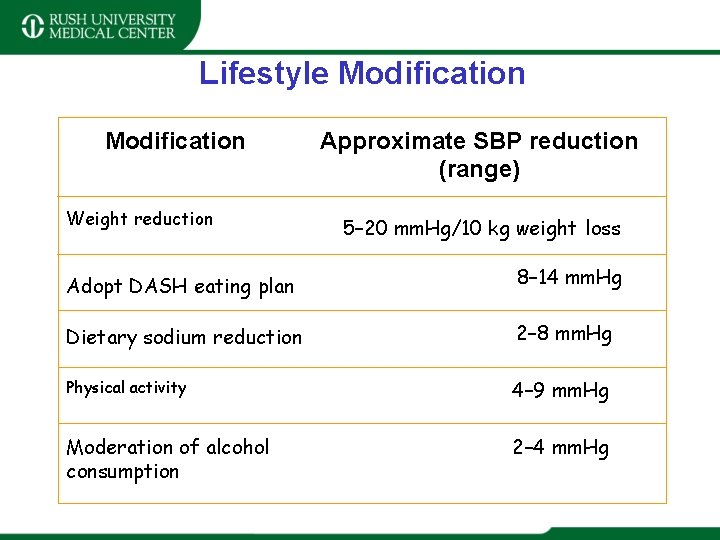
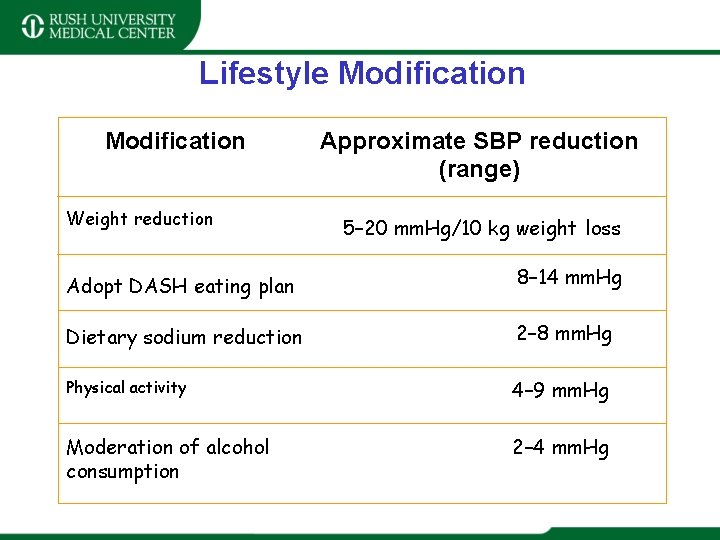
Lifestyle Modification Weight reduction Approximate SBP reduction (range) 5– 20 mm. Hg/10 kg weight loss Adopt DASH eating plan 8– 14 mm. Hg Dietary sodium reduction 2– 8 mm. Hg Physical activity 4– 9 mm. Hg Moderation of alcohol consumption 2– 4 mm. Hg
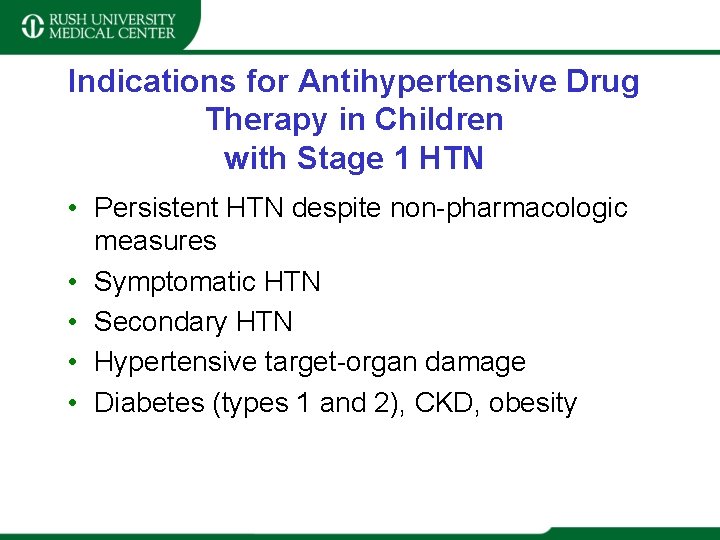
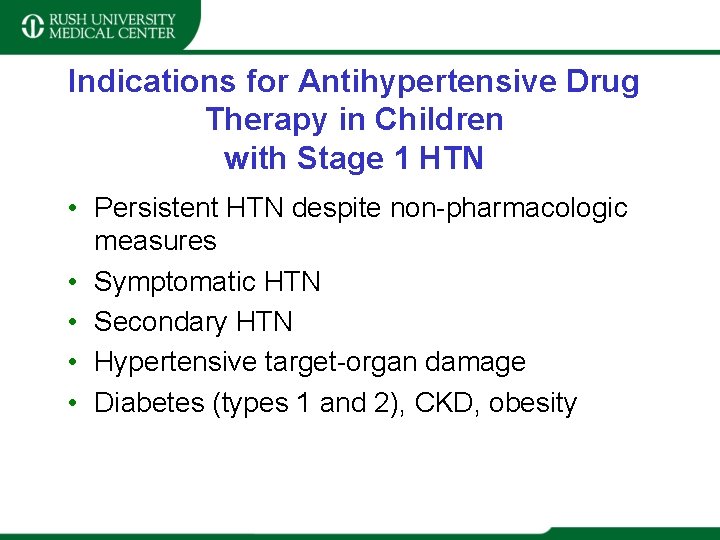
Indications for Antihypertensive Drug Therapy in Children with Stage 1 HTN • Persistent HTN despite non-pharmacologic measures • Symptomatic HTN • Secondary HTN • Hypertensive target-organ damage • Diabetes (types 1 and 2), CKD, obesity


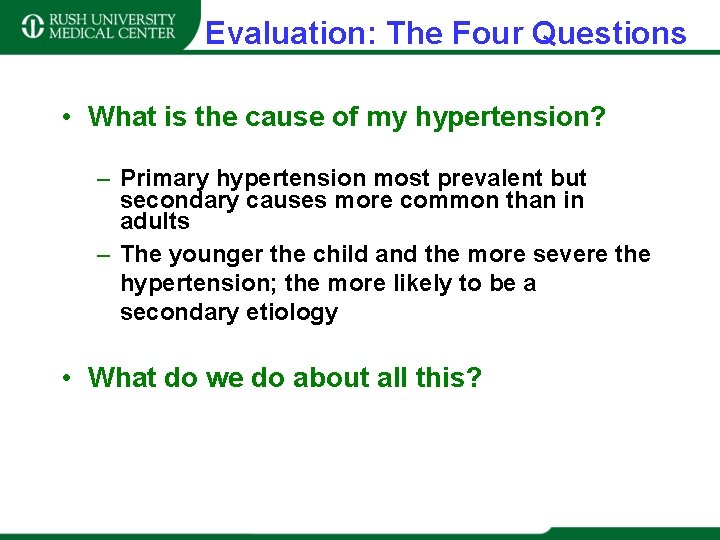
Evaluation: The Four Questions • What is the cause of my hypertension? – Primary hypertension most prevalent but secondary causes more common than in adults – The younger the child and the more severe the hypertension; the more likely to be a secondary etiology • What do we do about all this?
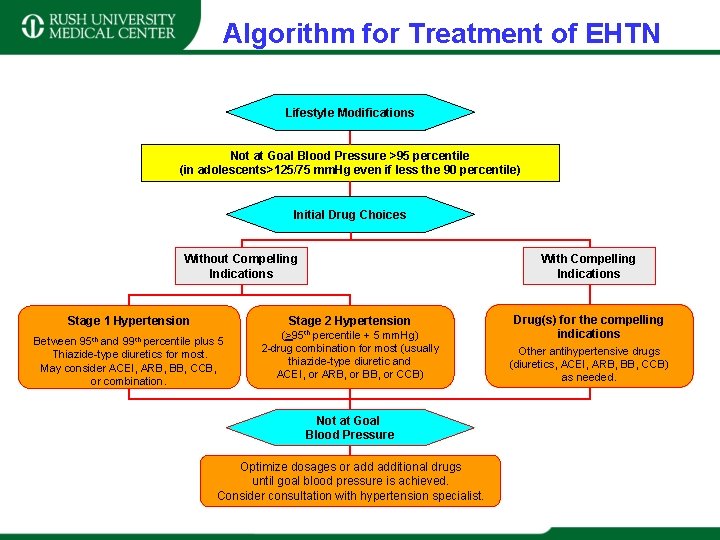
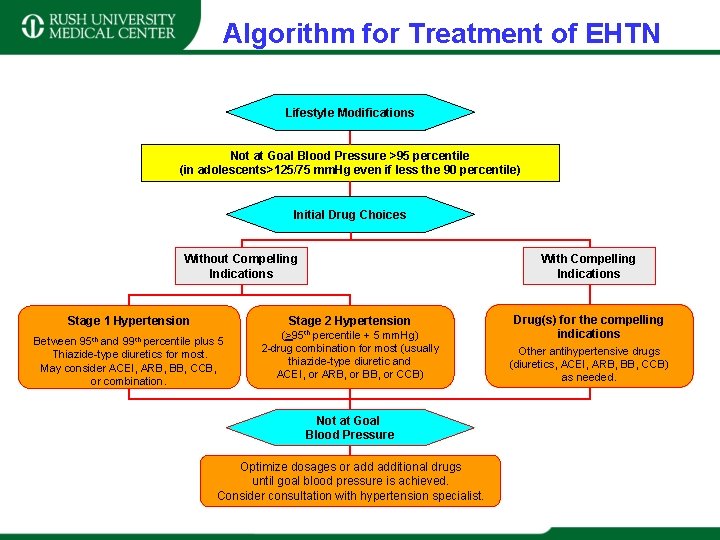
Algorithm for Treatment of EHTN Lifestyle Modifications Not at Goal Blood Pressure >95 percentile (in adolescents>125/75 mm. Hg even if less the 90 percentile) Initial Drug Choices Without Compelling Indications With Compelling Indications Stage 2 Hypertension Stage 1 Hypertension Between 95 th and 99 th percentile plus 5 Thiazide-type diuretics for most. May consider ACEI, ARB, BB, CCB, or combination. (>95 th percentile + 5 mm. Hg) 2 -drug combination for most (usually thiazide-type diuretic and ACEI, or ARB, or BB, or CCB) Not at Goal Blood Pressure Optimize dosages or additional drugs until goal blood pressure is achieved. Consider consultation with hypertension specialist. Drug(s) for the compelling indications Other antihypertensive drugs (diuretics, ACEI, ARB, BB, CCB) as needed.
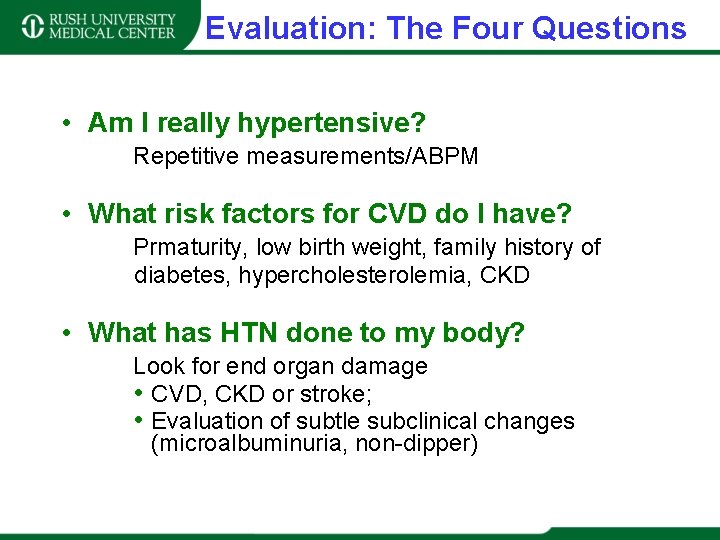
Evaluation: The Four Questions • Am I really hypertensive? Repetitive measurements/ABPM • What risk factors for CVD do I have? Prmaturity, low birth weight, family history of diabetes, hypercholesterolemia, CKD • What has HTN done to my body? Look for end organ damage • CVD, CKD or stroke; • Evaluation of subtle subclinical changes (microalbuminuria, non-dipper)
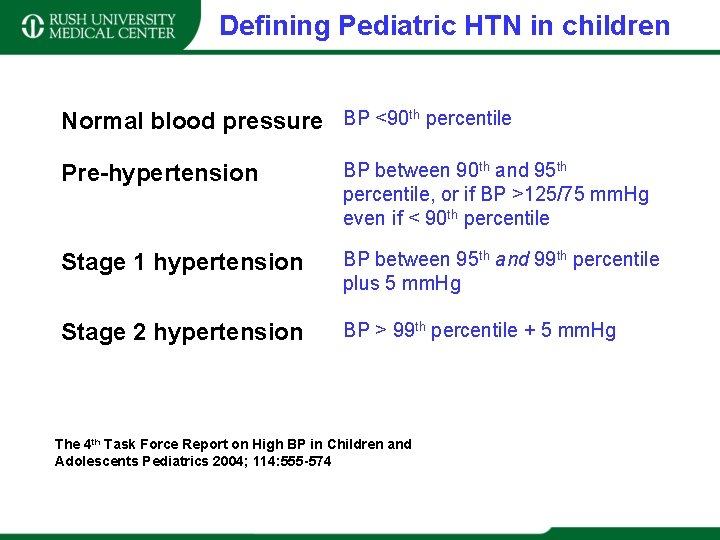
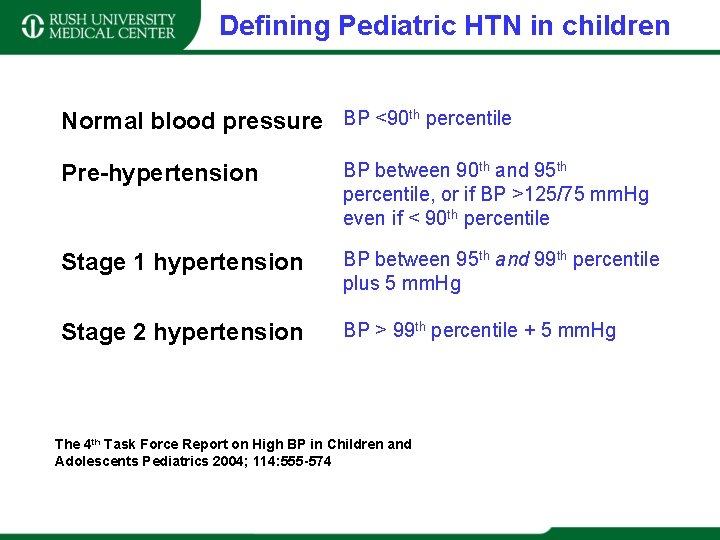
Defining Pediatric HTN in children Normal blood pressure BP <90 th percentile Pre-hypertension BP between 90 th and 95 th percentile, or if BP >125/75 mm. Hg even if < 90 th percentile Stage 1 hypertension BP between 95 th and 99 th percentile plus 5 mm. Hg Stage 2 hypertension BP > 99 th percentile + 5 mm. Hg The 4 th Task Force Report on High BP in Children and Adolescents Pediatrics 2004; 114: 555 -574 *Average SBP and DBP, on >3 occasions **Average SBP or DBP, on >3 occasions
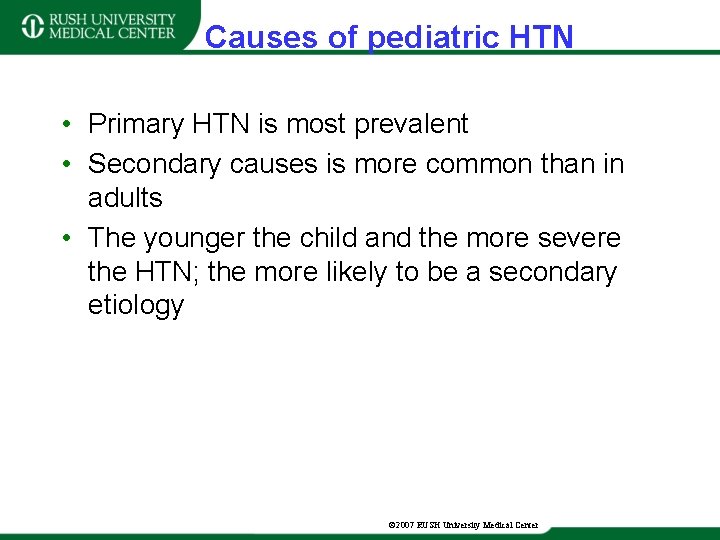
Causes of pediatric HTN • Primary HTN is most prevalent • Secondary causes is more common than in adults • The younger the child and the more severe the HTN; the more likely to be a secondary etiology © 2007 RUSH University Medical Center
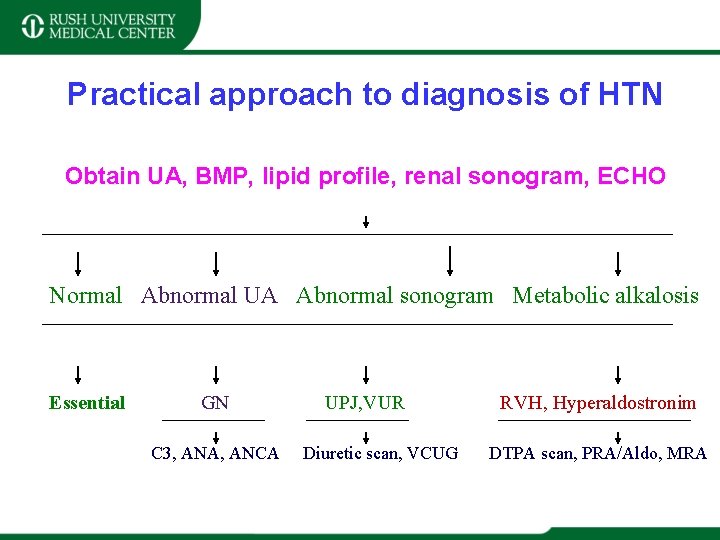
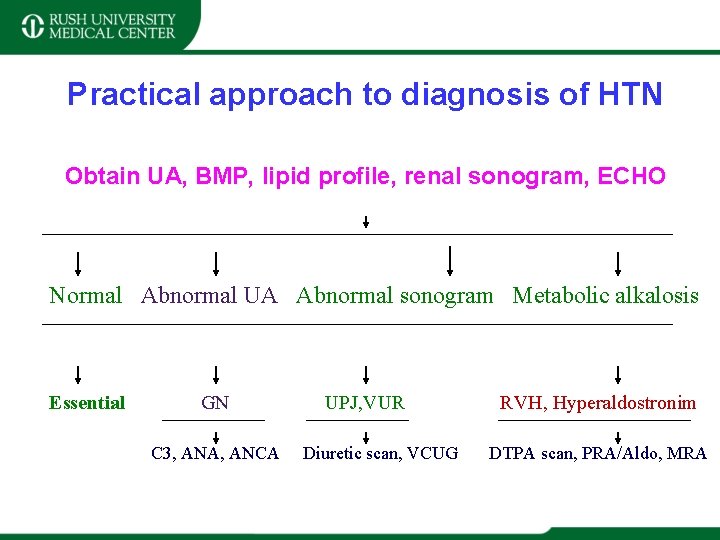
Practical approach to diagnosis of HTN Obtain UA, BMP, lipid profile, renal sonogram, ECHO Normal Abnormal UA Abnormal sonogram Metabolic alkalosis Essential GN C 3, ANA, ANCA UPJ, VUR Diuretic scan, VCUG RVH, Hyperaldostronim DTPA scan, PRA/Aldo, MRA
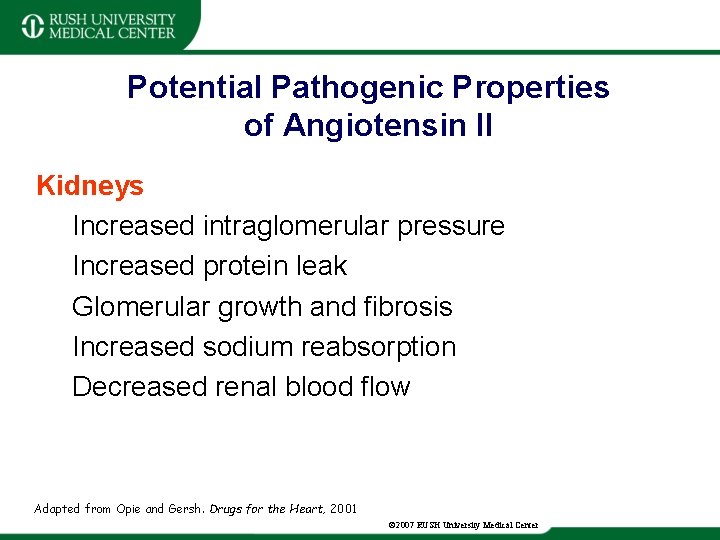
Potential Pathogenic Properties of Angiotensin II Kidneys Increased intraglomerular pressure Increased protein leak Glomerular growth and fibrosis Increased sodium reabsorption Decreased renal blood flow Adapted from Opie and Gersh. Drugs for the Heart, 2001 © 2007 RUSH University Medical Center
 Hypertensive encephalopathy
Hypertensive encephalopathy Malignant hypertention
Malignant hypertention Definition of hypertension
Definition of hypertension Malignant hypertension ppt
Malignant hypertension ppt Essential non essential fatty acids
Essential non essential fatty acids Vyvanse plm
Vyvanse plm Allopurinol nycomed
Allopurinol nycomed Allopurinol 300 gador
Allopurinol 300 gador Allopurinol ilacabak
Allopurinol ilacabak Allopurinol cost walgreens
Allopurinol cost walgreens Allopurinol buy
Allopurinol buy Allopurinol 100 mg tablet picture
Allopurinol 100 mg tablet picture Xpadder
Xpadder Allopurinol price walmart
Allopurinol price walmart Allopurinol 300 craveri
Allopurinol 300 craveri Pulmonary hypertension
Pulmonary hypertension Ocular hypertension dvla
Ocular hypertension dvla Rules of halves in hypertension
Rules of halves in hypertension Masked hypertension
Masked hypertension Presinusoidal portal hypertension
Presinusoidal portal hypertension Hypertension
Hypertension Health coaches for hypertension control
Health coaches for hypertension control Pulmonary hypertension
Pulmonary hypertension Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Bmpr gene
Bmpr gene Portal hypertension mayo clinic
Portal hypertension mayo clinic Aobp vs obpm
Aobp vs obpm Jnc 8 classification of hypertension
Jnc 8 classification of hypertension Blood pressure medication dosage chart
Blood pressure medication dosage chart Hypertension vs hypotension
Hypertension vs hypotension Isolated systolic hypertension
Isolated systolic hypertension Demadex
Demadex Jnc 7 hypertension
Jnc 7 hypertension Nursing management of portal hypertension
Nursing management of portal hypertension Hypertensive emergency
Hypertensive emergency Diagnosis hypertension
Diagnosis hypertension Htn emergency vs urgency
Htn emergency vs urgency Hypertension medical definition
Hypertension medical definition Paedp echo
Paedp echo Classification of hypertension
Classification of hypertension Equivalence hbpm
Equivalence hbpm Chd pulmonary hypertension
Chd pulmonary hypertension Hypertension artérielle
Hypertension artérielle Case scenario for hypertension
Case scenario for hypertension Conclusion of hypertension
Conclusion of hypertension Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Amas faa
Amas faa Pulmonary hypertension differential diagnosis
Pulmonary hypertension differential diagnosis Hypertension drugs
Hypertension drugs