AIRWAY MANAGEMENT IN THE ICU Rachel Garvin MD




- Slides: 45
AIRWAY MANAGEMENT IN THE ICU Rachel Garvin, MD Assistant Professor, Neurosurgery Neurocritical Care October 5, 2012
• Goals of this Lecture To give you some comfort level with airways and tips to help your patient
Topics to be covered • Why airway is so important • Why patients with neurologic injury have airway issues • Airway Anatomy • Causes of compromised airway • Airway Evaluation • Airway Adjuncts • Drugs
Why is airway management so important in the Neuro. ICU? • Hypoxemia contributes to secondary brain injury • Brain injured patients have numerous reasons to have airway compromise • You should have an understanding of basic airway management to aid in your patient’s care
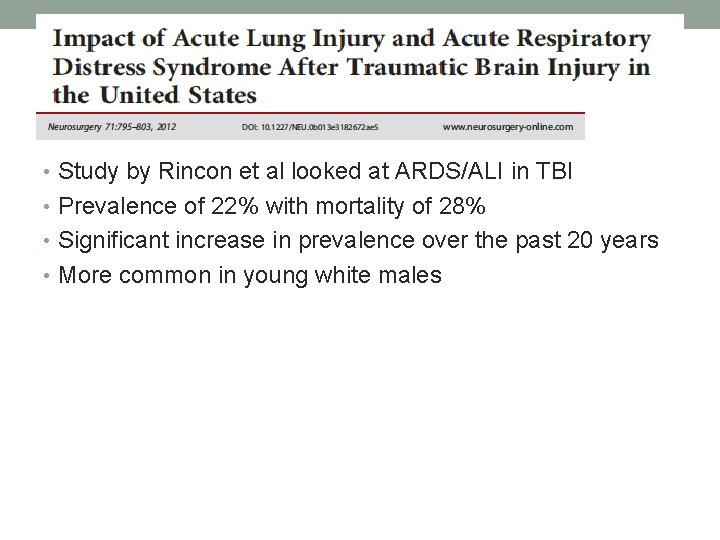
• Study by Rincon et al looked at ARDS/ALI in TBI • Prevalence of 22% with mortality of 28% • Significant increase in prevalence over the past 20 years • More common in young white males
Neural control • Corticobulbar tract • Lower CN’s • Nucleus ambiguus • Several respiratory centers • Dorsal medulla • Ventral medulla • Dorsal rostral pons • C-spine/Upper T-spine
Why do neuro patients have respiratory failure? • As a result of their primary injury • Due to secondary injury • Other injuries • Development of respiratory infection • Development of ARDS
• Corral et al looked at non-neurologic complications in severe TBI patients • Respiratory infections in 68% of severe TBI patients • Mortality not increased but hospital LOS, time on mechanical ventilation increased
Why is it important to understand airway anatomy? • Airway Obstruction – where is it? • Will my rescue devices work? • What is happening in laryngospasm? • What if I need to crich someone?
Concerning Airway
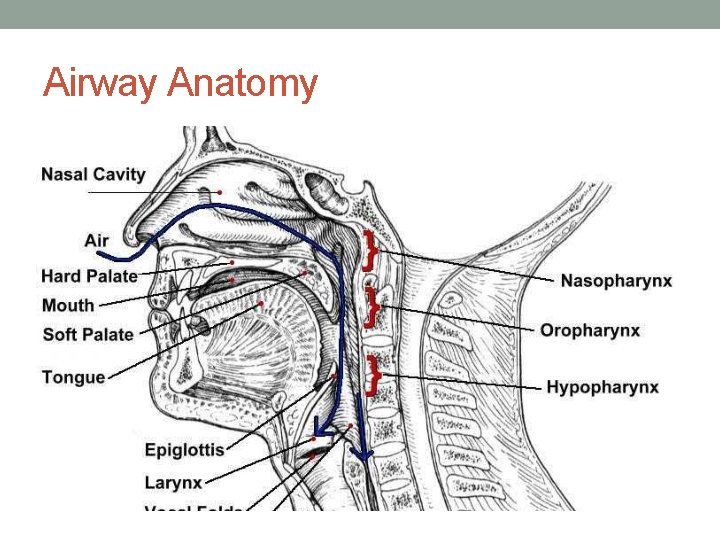
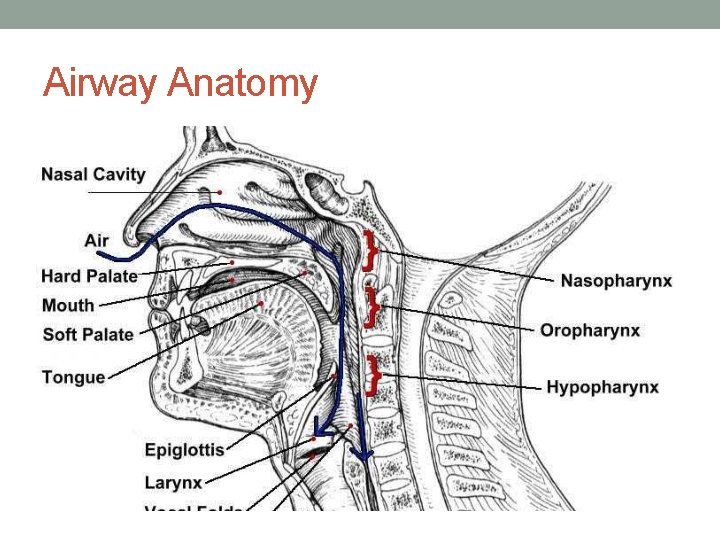
Airway Anatomy
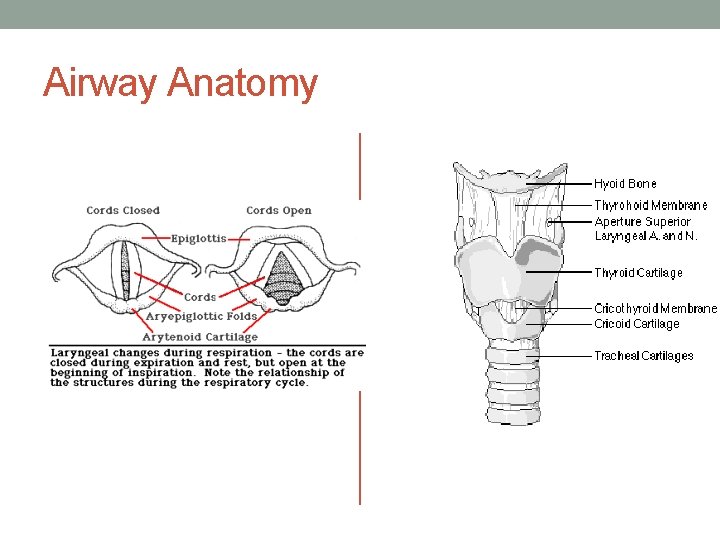
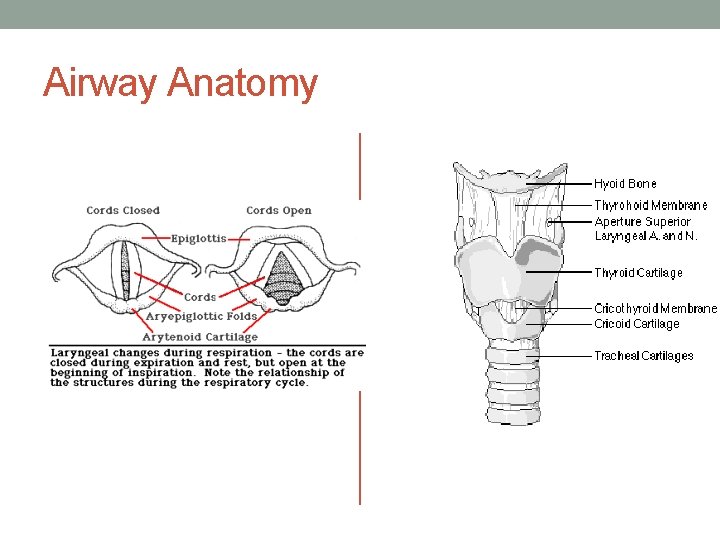
Airway Anatomy
Conditions that can compromise airway • Degree of wakefulness • Aspiration • Body habitus • Concurrent injuries • Medications • Co-morbidities
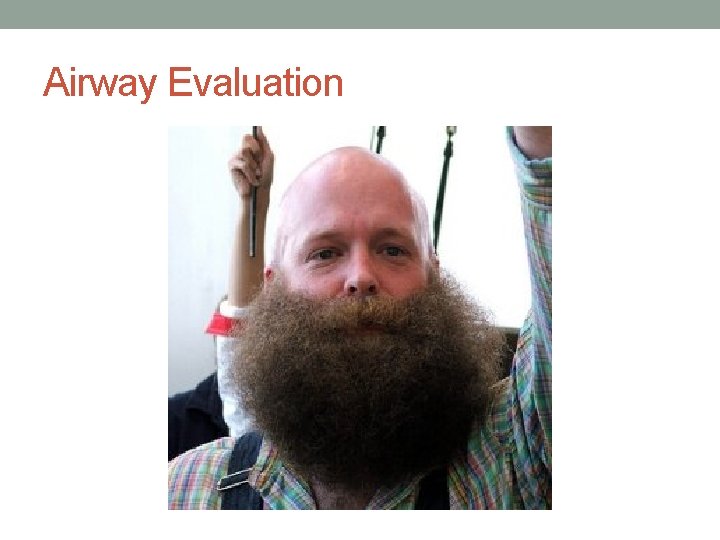
Airway Evaluation
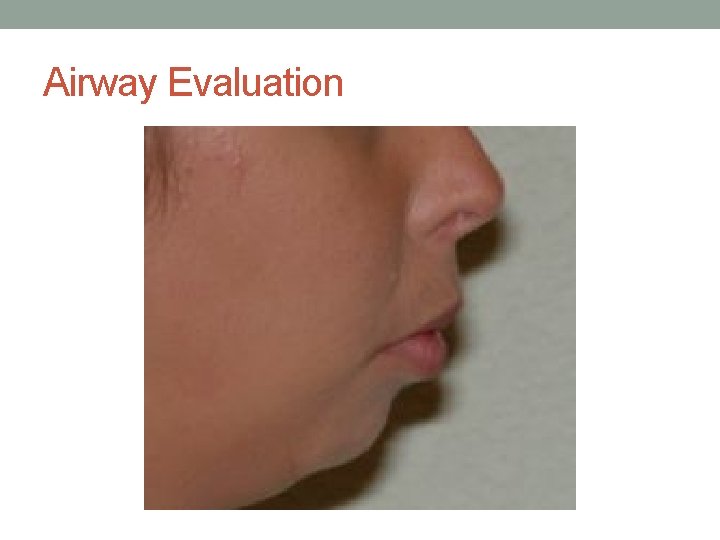
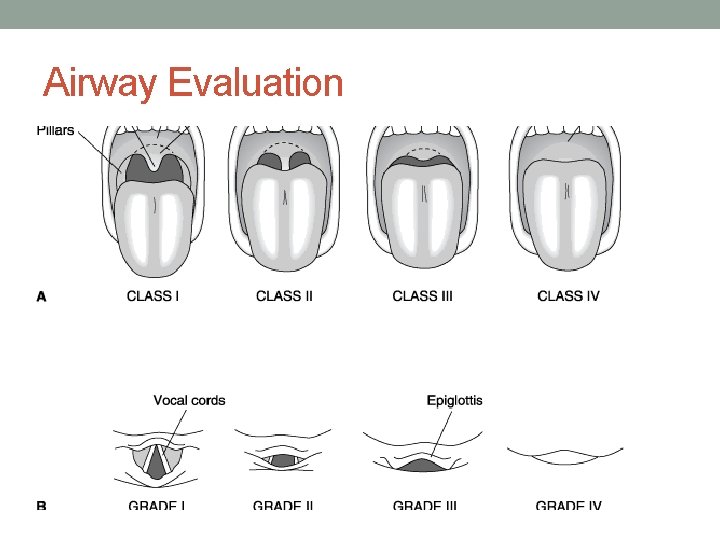
Airway Evaluation
Airway Evaluation

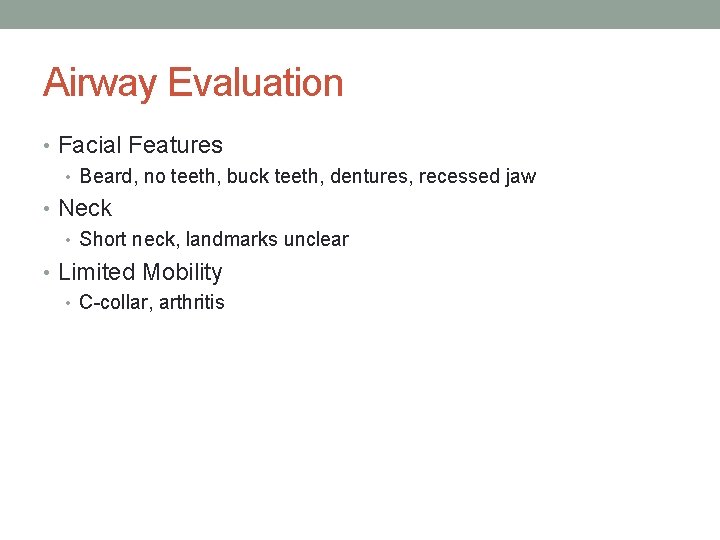
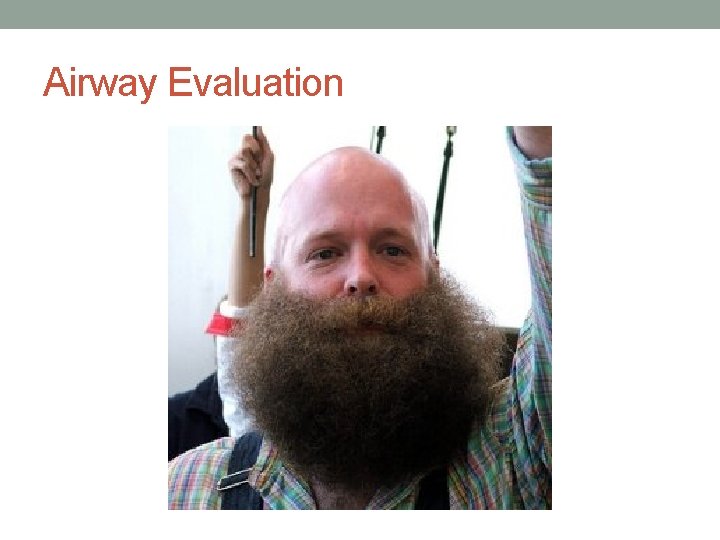
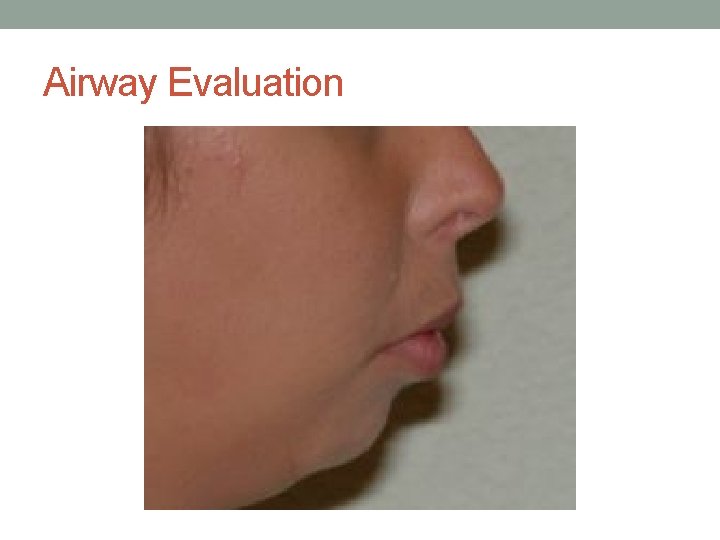
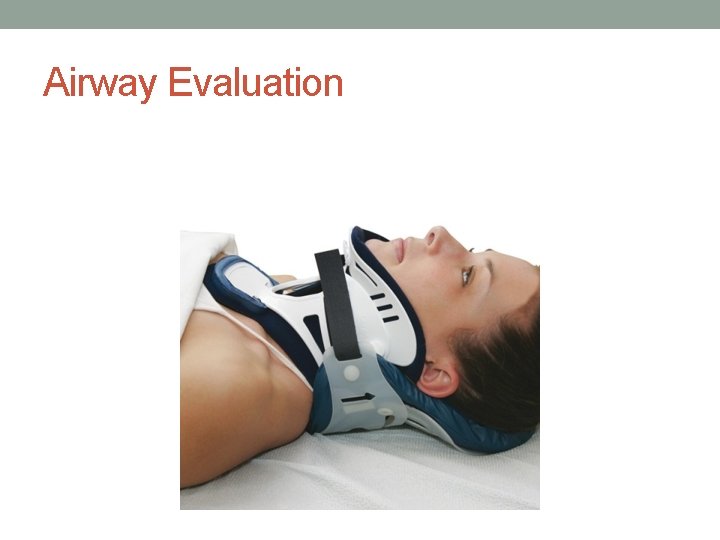
Airway Evaluation • Facial Features • Beard, no teeth, buck teeth, dentures, recessed jaw • Neck • Short neck, landmarks unclear • Limited Mobility • C-collar, arthritis
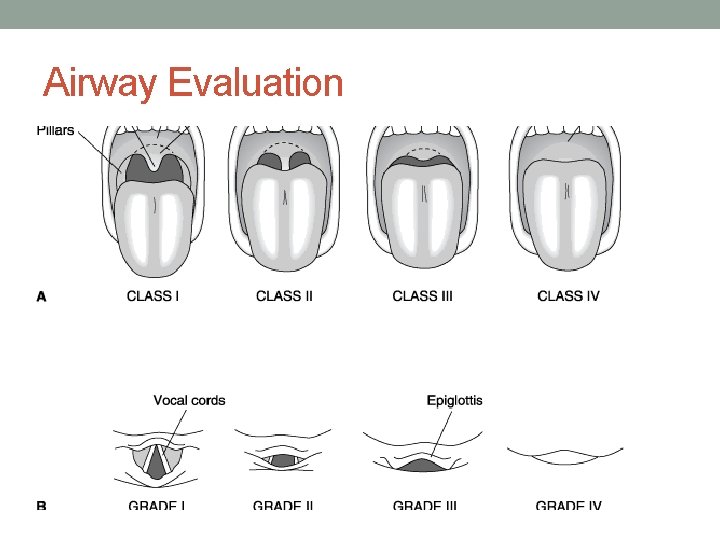
Airway Evaluation
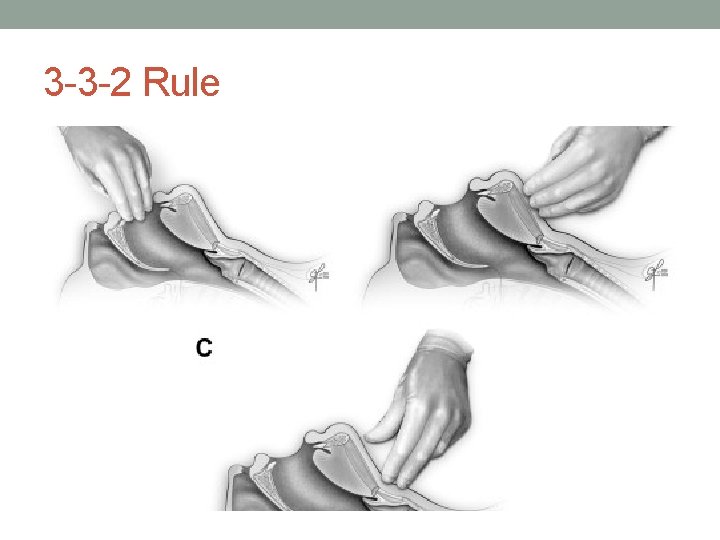
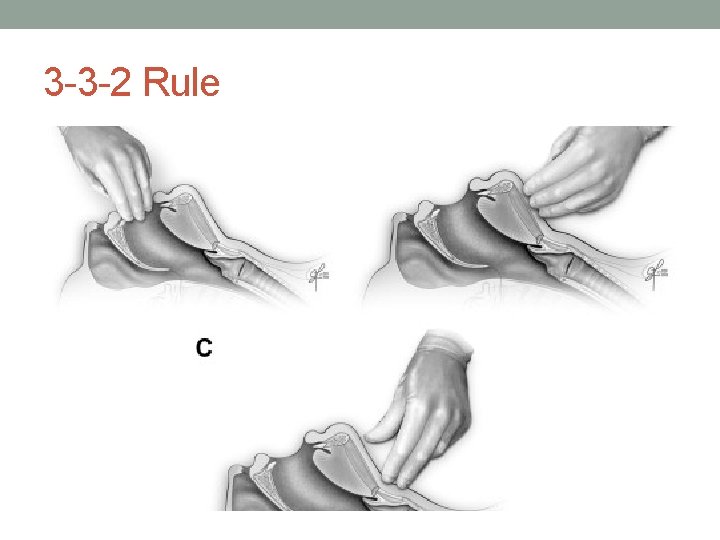
3 -3 -2 Rule
Quick Assessment: • Mouth: how much can they open it? • Tongue: how much can they protrude it? • Jaw: mobility • Neck: mobility
Airway Adjuncts – what you can do before calling anesthesia • Positioning • Plastic in orifices • Preoxygenate • Jaw Thrust • Check sedation

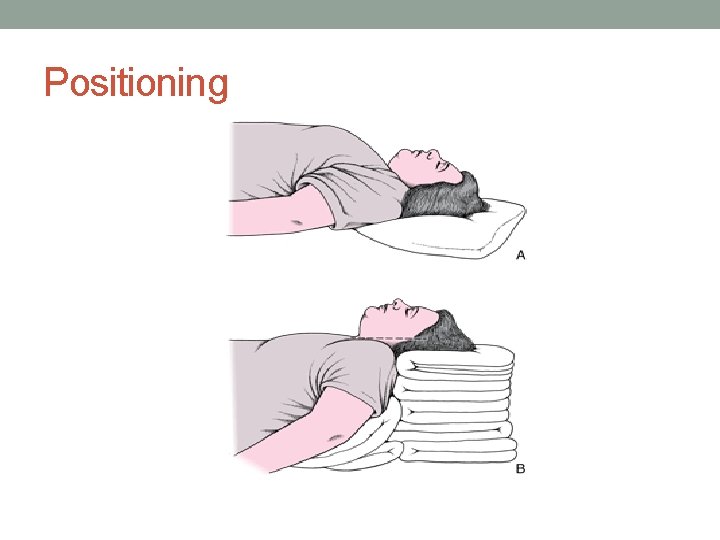
Positioning
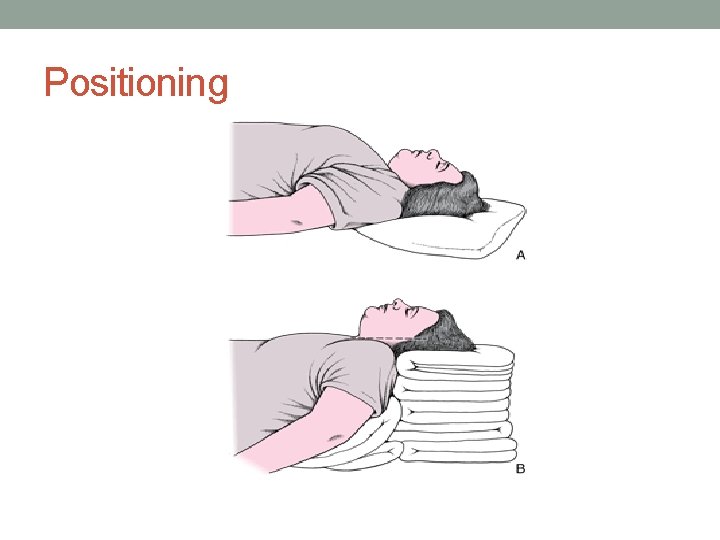
Positioning
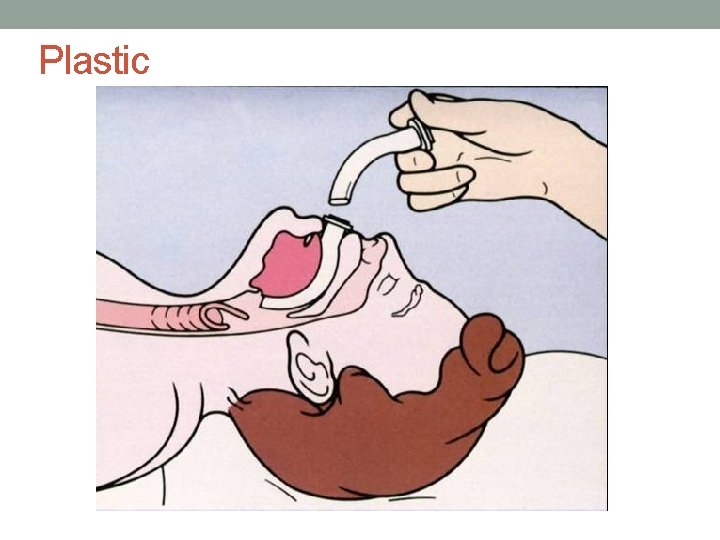
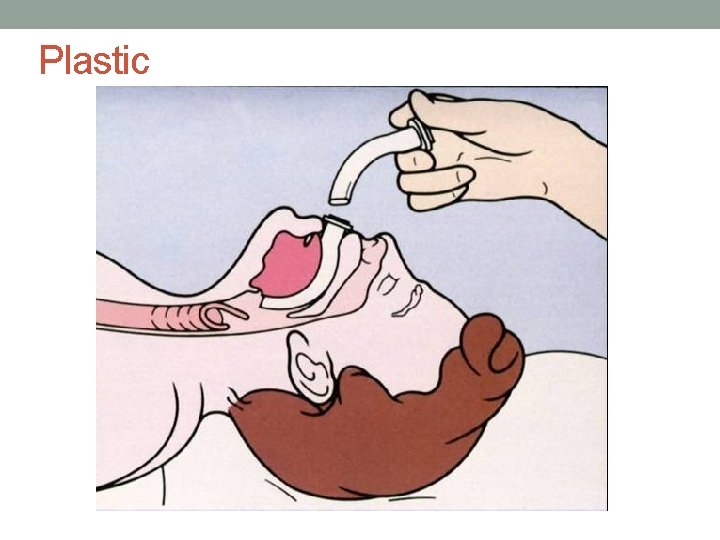
Plastic
Placing a nasal trumpet • Placed with bevel towards turbinates • Left sided goes in angled down • Right sided goes in facing upward and then turned
Placing an Oral Airway • Pick the appropriate size • 3 -4 for small adult, 4 -5 medium, 5 -6 large • Insert facing upward and then rotate down • Do not use in an awake patient

Preoxygenate
Oxygen Delivery: High vs Low Flow • Nasal Cannula • Simple Face Mask • Nonrebreather Face Mask • Venti Mask Flow does NOT = Fi. O 2
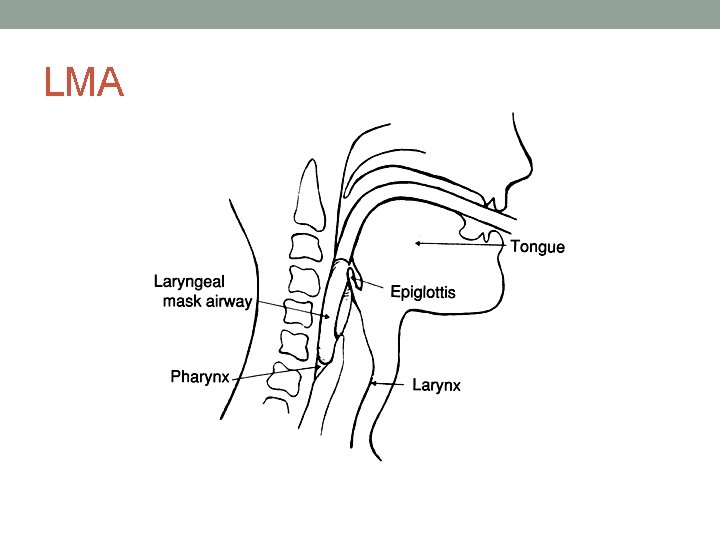
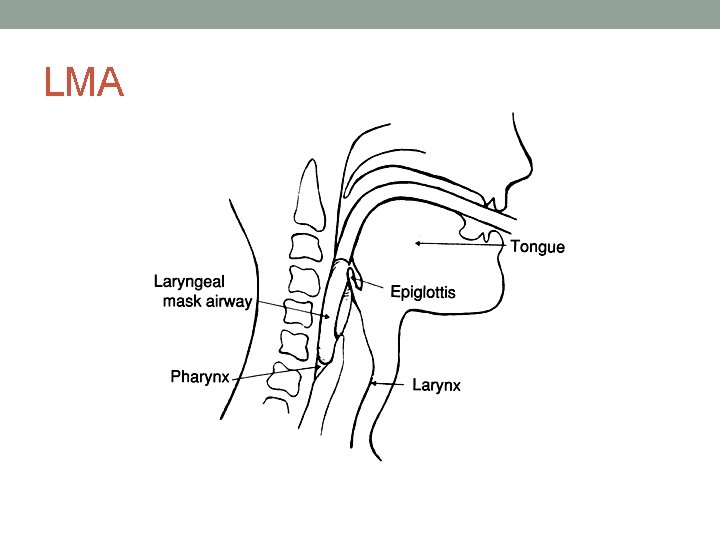
LMA

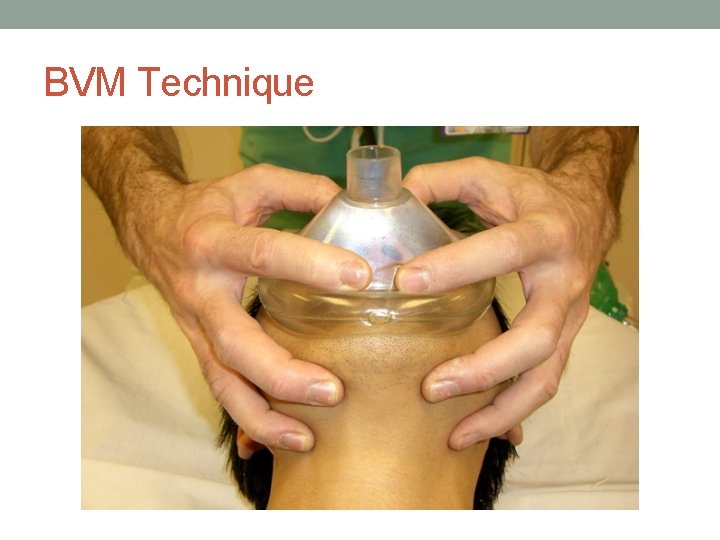
BVM Technique
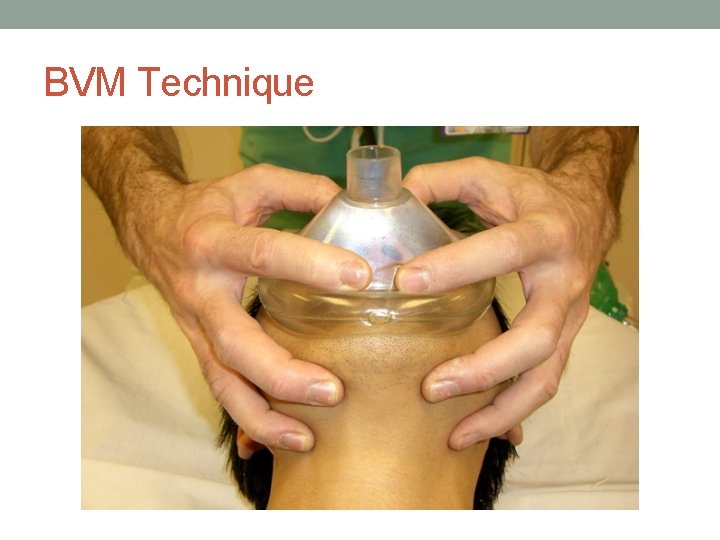
BVM Technique
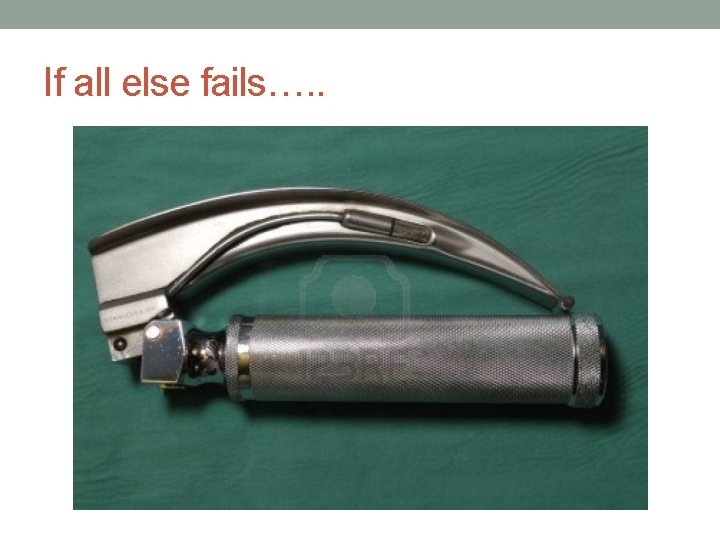
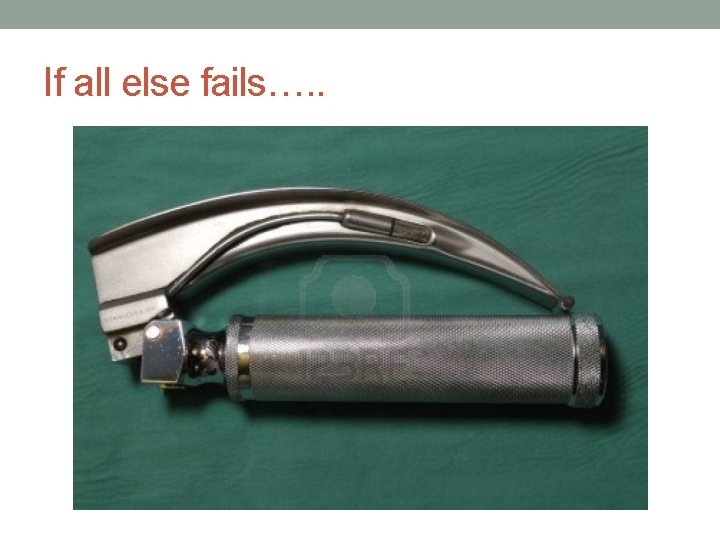
If all else fails…. .
What drugs do you want? • Sedatives • Paralytics
Sedatives • Etomidate • Propofol • Ketamine
Etomidate • GABA like effects • Minimal effect on BP; can lower ICP • Can reduce plasma cortisol levels • Hepatic metabolism; renally excreted • Dose 0. 3 mg/kg
Propofol • Anesthetic agent • Respiratory and CV depressant can drop BP by as much as 30% • Vasodilation and negative inotropic effect • Dose is 1 -1. 5 mg/kg
Ketamine • Anesthetic and dissociative agent • Hepatic metabolism • Can cause laryngeal spasm, hypertension • Emergence reaction give benzo with it • 1 -2 mg/kg
Paralytics • Succinylcholine • Vecuronium • Rocuronium • Cisatricurium If you don’t think you can BVM someone, don’t paralyze them!!
Succinylcholine • Only depolarizing NMB • Avoid in hyperkalemia, 24 hour post major burn, neuromuscular disease, patients with several days of ICU critical illness • Onset in 60 seconds and lasts around 5 minutes • 1 -1. 5 mg/kg
Rocuronium • Nondepolarizing • Onset about 90 seconds and last 30 -40 minutes • Lasts longer in those with hepatic impairment • Dose is 0. 6 -1 mg/kg • Effect is dose dependent
Vecuronium • Similar to rocuronium • Slower onset time (up to 4 minutes) • Lasts 40 -60 minutes • 0. 08 -0. 1 mg-kg
Conclusion • Appropriate airway management is crucial in patients with brain injury • Remember your airway anatomy and assessment in patient evaluation • Use your adjuncts to help you • Be vigilant in the drugs being given to your patients if intubation is required
Questions?
References • Corral L, Casimiro JF, Ventura JL, Marcos P, Herrero JI, Manez R. Impact of non-neurologic complications in severe traumatic brain injury outcome. Critical Care 2012; 16: R 44. • Karanjia N, Nordquist D, Stevens R, Nyquist P. A Clinical Descriuption of Extubation Failure in Patients with Primary Brain Injury. Neurocritical Care 2011; 15: 4 -12. • Rincon F, Ghosh S, Dey S, Maltenfort M, Vibbert M, Urtecho J, Mc. Bride W, Moussouttas M, Bell R, Ratliff J, Jallo J. Impact of Acute Lung Injury and Acute Respiratory Distress Syndrome After Traumatic Brain Injury in the United States. Neurosurgery 2012; 71: 795 -803. • Wong E, Yih-Yng Ng. The Difficult Airway in the Emergency Department. Int J Emerg Med, 2008: 1: 107 -111.
 Rachel garvin md
Rachel garvin md Rachel garvin md
Rachel garvin md Larangoscopy
Larangoscopy Building a learning organization by david a. garvin
Building a learning organization by david a. garvin Total quality management introduction
Total quality management introduction Debbie garvin
Debbie garvin Which of the gurus would be the father of quality control?
Which of the gurus would be the father of quality control? Effektmodifiering
Effektmodifiering Charles garvin md
Charles garvin md Airway management acls
Airway management acls Chapter 10 airway management
Chapter 10 airway management Airway management ladder
Airway management ladder Npa measurement
Npa measurement Airway abcde
Airway abcde Sandwich manuver
Sandwich manuver Stepwise approach to airway management
Stepwise approach to airway management Kebutuhan tenaga perawat
Kebutuhan tenaga perawat Escala de sedacion agitacion sas
Escala de sedacion agitacion sas Icu localization
Icu localization Icu primer sekunder tersier
Icu primer sekunder tersier Information and communications university zambia
Information and communications university zambia 5hs and 5ts
5hs and 5ts Sean forsythe
Sean forsythe Escala de consciencia
Escala de consciencia Cam icu
Cam icu Cam icu escala
Cam icu escala Kanisha belt
Kanisha belt Cam icu
Cam icu Icu unit meaning
Icu unit meaning Icu orientation
Icu orientation Critical care for dummies
Critical care for dummies Information and communications university
Information and communications university Icu acuity tool
Icu acuity tool Icu library
Icu library Icu layout and design
Icu layout and design Icu case presentation
Icu case presentation Icu case presentation
Icu case presentation Icu transliterator
Icu transliterator Icu medical b3108
Icu medical b3108 Kp icu jpm
Kp icu jpm Ideal icu setup
Ideal icu setup Chatecholamine
Chatecholamine Icu security group
Icu security group Cam icu escala
Cam icu escala Atenolol to metoprolol conversion
Atenolol to metoprolol conversion Types of iv fluid
Types of iv fluid