1 Neoplastic Disease KNH 411 2 Cancer Carcinogenesis


- Slides: 27
1 Neoplastic Disease KNH 411
2 Cancer Carcinogenesis - Etiology Genes may be affected by antioxidants, soy, protein, fat, kcal, alcohol high fat diets decreasing kcals in people overweight obese avoiding excess alcohol benefits of flavenoids in alcohol(non-excessive) Nutritional genomics – study of genetic variations that cause different phenotypic responses to diet
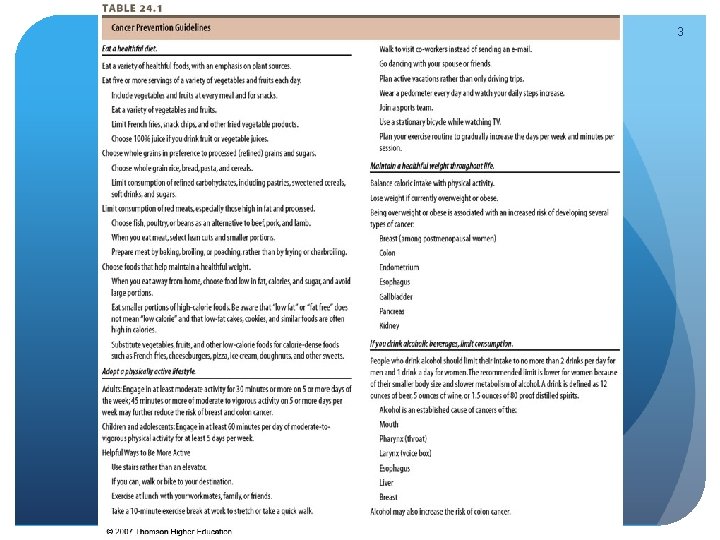
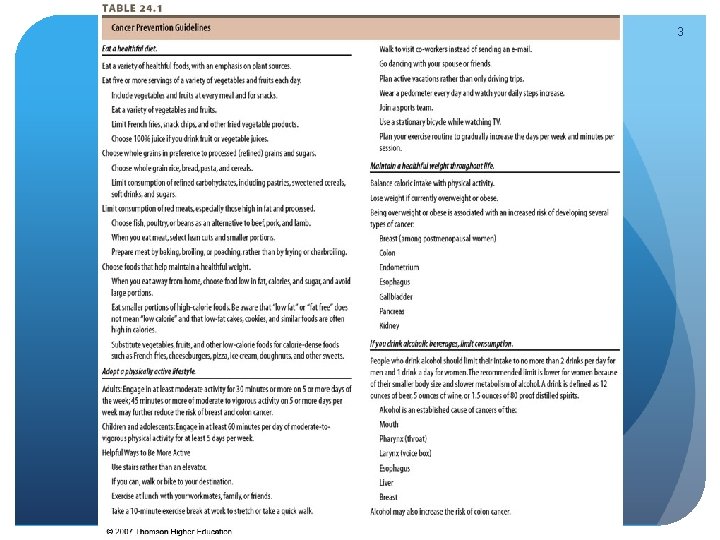
3
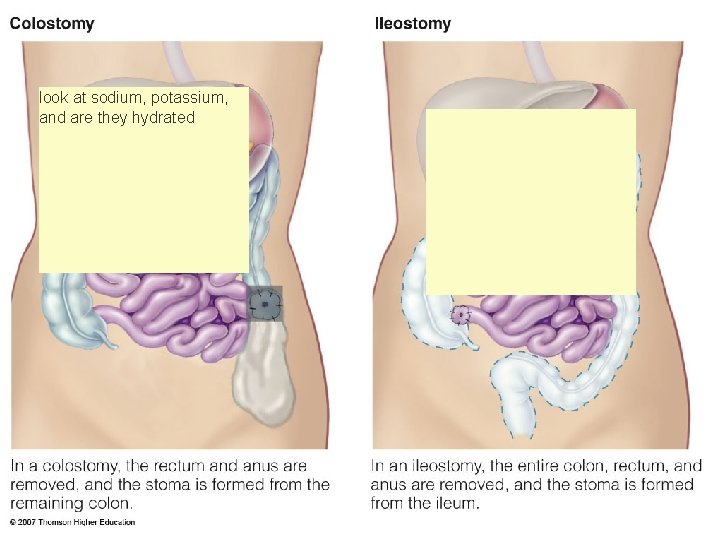
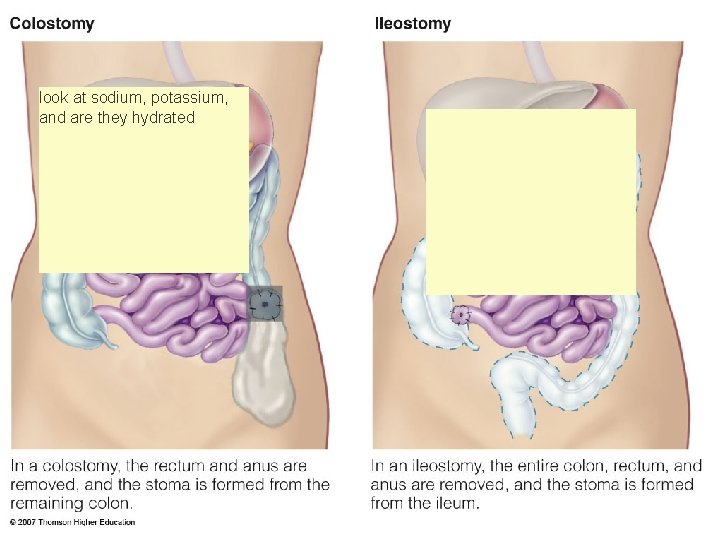
4 look at sodium, potassium, and are they hydrated © 2007 Thomson - Wadsworth
Chemotherapy Common side effects due to toxicity to rapidly dividing cells: Neutropenia--low white blood cell count; more susceptible to infections Thrombocytopenia--low platelet count; causes patients to be sluggish; need nutrient dense meals Anemia Diarrhea Mucositis--inflammation of mucus membrane; sores in mouth; be sensitive to salty/acidic foods; temperature sensitive foods Alopecia--hair loss Cardiotoxicity, neurotoxicity, nephrotoxicity--a lot of the patients will end up with cardiac, kidney, and nerve function damage 5
6 Radiation delivering electromagnetic rays to destroy the cancer Side effects: Delayed wound healing Fatigue, mucositis, dysguesia, xerostomia, dysphagia, odynophagia, severe esophagitis, dehydration Radiation enteritis, fistulas, strictures, chronic malabsorption, severe diarrhea TPN may be warranted to prevent weight loss
7 Nutrition Therapy Prevent malnutrition Screening and assessment important Be aware of cancer dg and treatments most likely to cause malnutrition goal = to control symptomatic treatment with nutrition therapy
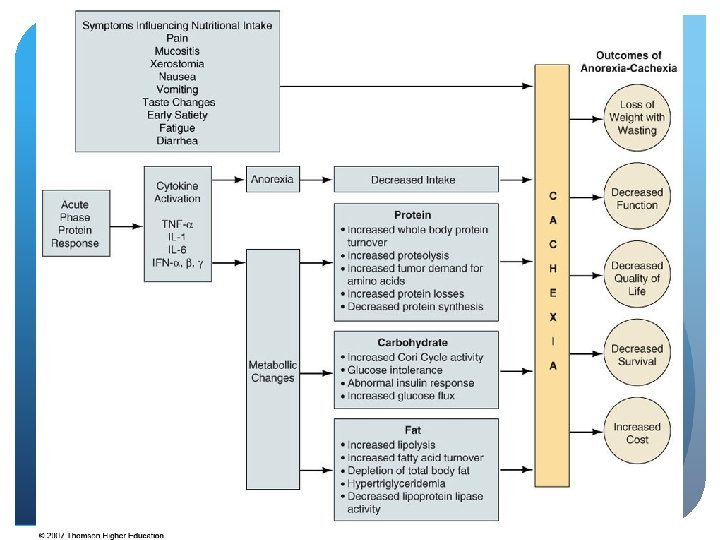
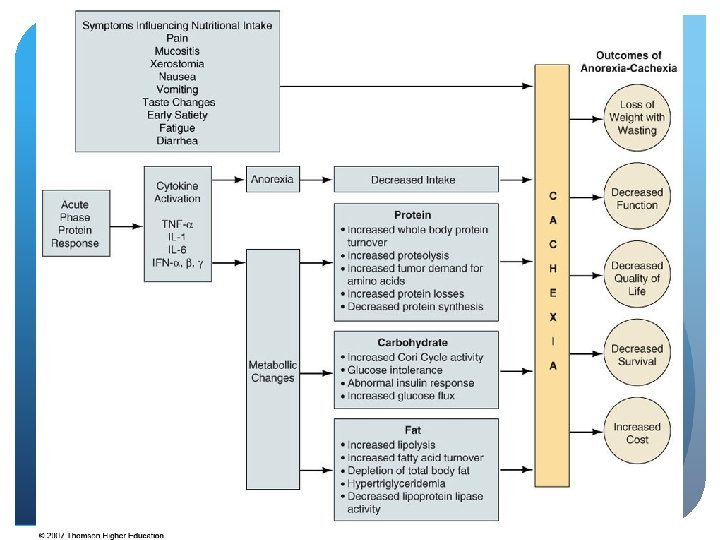
8 Nutrition Implications Cachexia – one of the most common causes of death in caner patients Metabolic alterations Tumor induces hypermetabolic catabolic state through chemical mediators Tumor specific “cachectic factors” Weight loss, anorexia, muscle wasting, fatigue, early satiety hard to alter because of the tumor Standard therapy – nutrition support
9 © 2007 Thomson - Wadsworth
10 Nutrition Implications Abnormalities in CHO, lipid, protein metabolism Normal physiologic conservation seen in starvation does not occur in presence of a malignant tumor CHO – insulin resistance, increased glucose synthesis, gluconeogenesis, increased Cori cycle activity, decreased glucose tolerance and turnover
11 Nutrition Implications Abnormalities in CHO, lipid, protein metabolism Protein - amino acids not spared, depletion of lean body mass, increased protein catabolism, or decreased protein synthesis Lipid – increased lipid metabolism, decreased lipogenesis, decreased LPL, presence of lipid-mobilizing factor (LMF)

12 Nutrition Implications Cancer treatment Nausea, vomiting Early satiety Dysgeusia Diarrhea Mucositis Xerostomia Constipation Weight loss Anemia
13 Nutrition Interventions Nutrition Assessment **SGA--subjective global assessment (basically assess who you need to see first) based on a medical and physical exam A= well nourished cancer patient B= moderately nourished patient C= severely malnourished patient scale 1 -9= if patient have 9 or more symptoms to manage, they need to be seen first Anthropometrics including height, weight, detailed weight hx, fluid retention, body composition Biochemical including serum hepatic proteins Clinical signs and symptoms
14 Nutrition Interventions Nutrition Assessment Detailed diet hx and current intake Foods tolerated, special diets, use of CAM, supplements, liquid nutritional supplement preferences
15 Nutrition Interventions Determining Nutrient Requirements Individualized Kcal to maintain weight and prevent loss Protein to prevent negative nitrogen balance and meet synthesis needs Fluid needs - 30 -35 m. L/kg Multivitamin mineral supplement < 150% DRI
16 Nutrition Interventions Nausea & Vomiting Avoid noxious odors Review medication list for potential causes Small, frequent meals Pro-kinetics CAM – acupressure, acupuncture, hypnosis, guided imagery related to delayed gastric emptying

17 Nutrition Interventions Nausea & Vomiting - Chemotherapy Small, low-fat meals morning of, avoid fried, greasy and favorite foods for several days Clear liquid diet Electrolyte-fortified beverages Non-acid fruit drinks Avoid favorite foods Avoid “creamy” liquid nutritional drinks Anti-emetics 30 -45 min. before meal inflamed GI tract
18 Nutrition Interventions Early Satiety Small, frequent nutrient-dense meals Beverages between meals and should contain nutrients Avoid high-fiber and raw vegetables Pro-kinetics
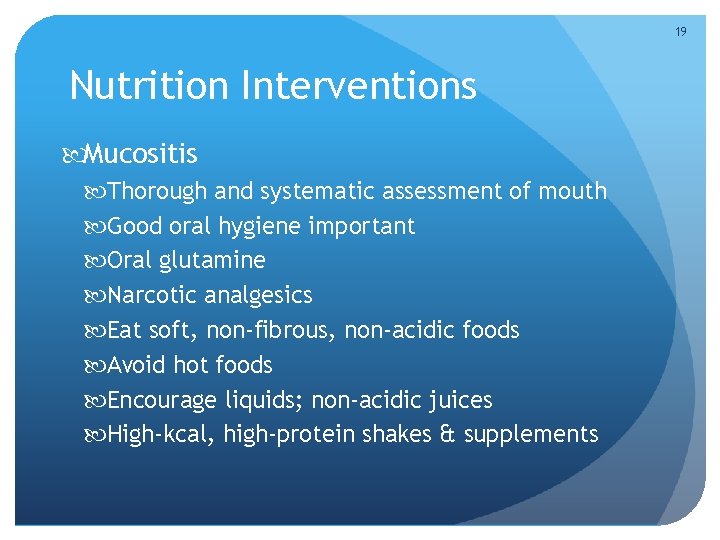
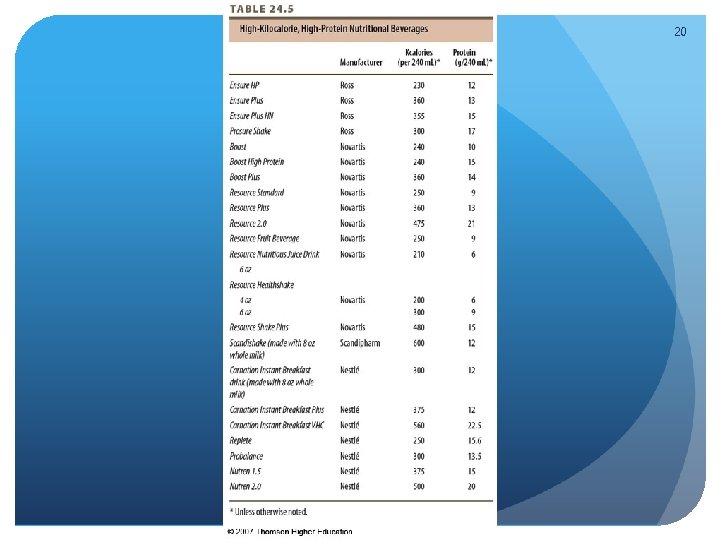
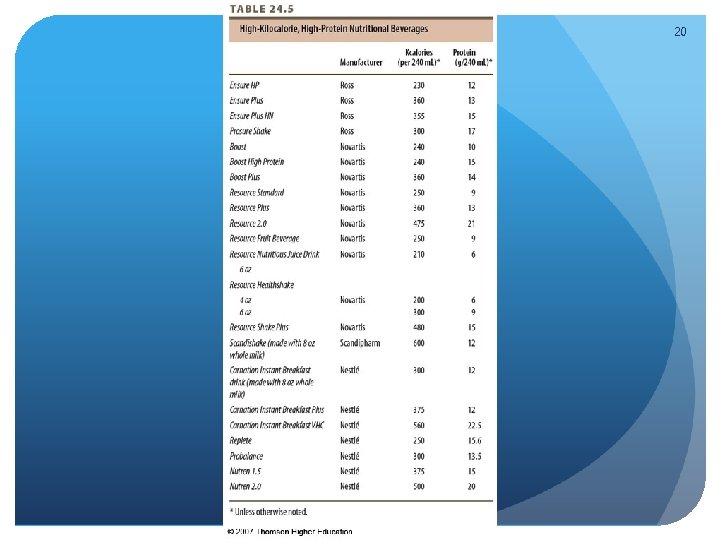
19 Nutrition Interventions Mucositis Thorough and systematic assessment of mouth Good oral hygiene important Oral glutamine Narcotic analgesics Eat soft, non-fibrous, non-acidic foods Avoid hot foods Encourage liquids; non-acidic juices High-kcal, high-protein shakes & supplements
20
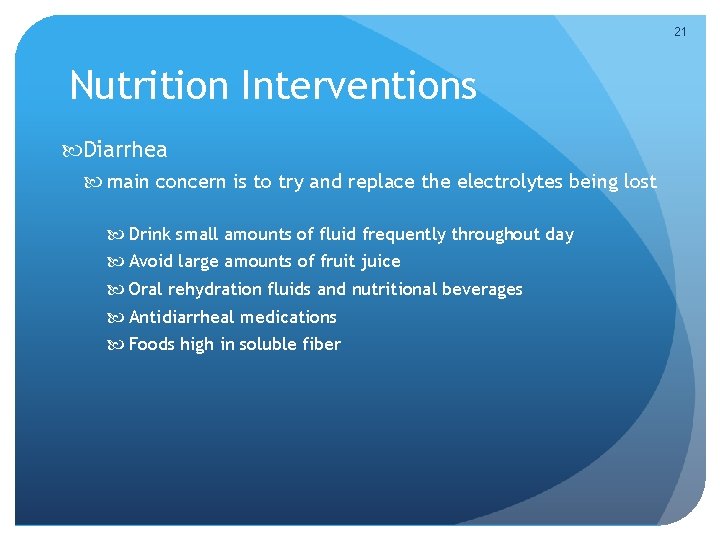
21 Nutrition Interventions Diarrhea main concern is to try and replace the electrolytes being lost Drink small amounts of fluid frequently throughout day Avoid large amounts of fruit juice Oral rehydration fluids and nutritional beverages Antidiarrheal medications Foods high in soluble fiber
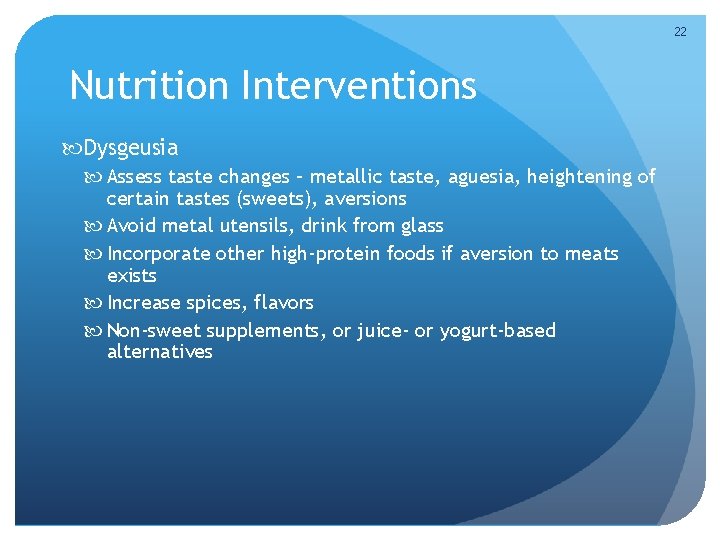
22 Nutrition Interventions Dysgeusia Assess taste changes – metallic taste, aguesia, heightening of certain tastes (sweets), aversions Avoid metal utensils, drink from glass Incorporate other high-protein foods if aversion to meats exists Increase spices, flavors Non-sweet supplements, or juice- or yogurt-based alternatives
23 Nutrition Interventions Xerostomia Artificial saliva/ mouth moisturizers Gels, lozenges, mouthwashes Sugar-free gum, sour-flavored hard candy consistency/taste/cost
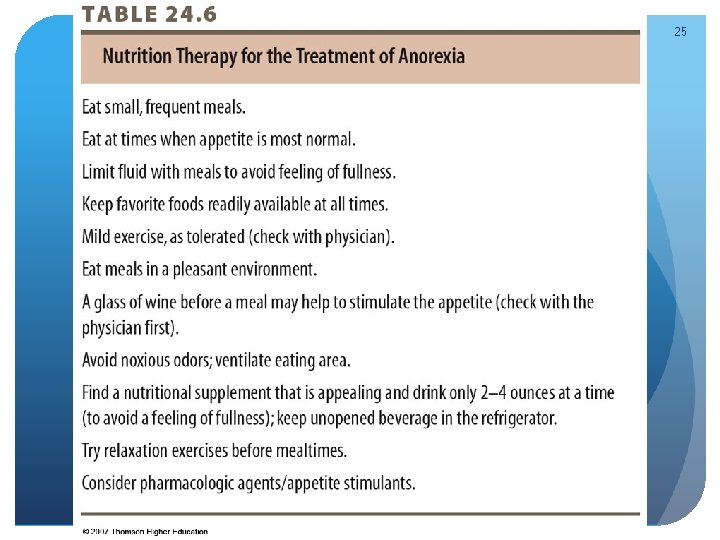
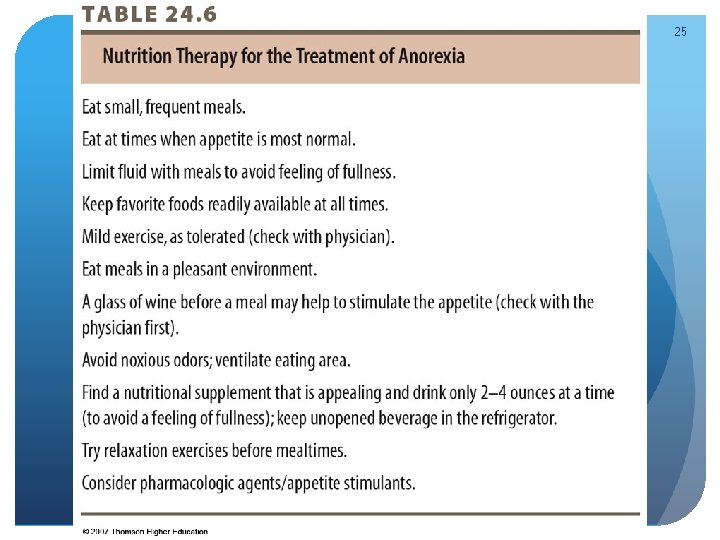
24 Nutrition Interventions Anorexia Pharmacologic agents to increase appetite Pharmacologic agents to treat weight loss Physical activity Oral supplements 50% of cancer patients will have anorexia Trying to maintain body mass
25
26 Nutrition Interventions Nutrition Support Enteral vs. parenteral Nutrition support inappropriate for those with terminal cancer or for pts. with poor prognosis for whom otherapies have been exhausted ASPEN practice guidelines for nutrition support
27 Nutrition Interventions Nutrition Support Home nutrition support May maintain quality of life Lack of appetite and food intake may be greater concern to family members, caregivers than to pt.
 Neoplastic proliferation of white blood cells
Neoplastic proliferation of white blood cells Lichen sclerosus vulvare
Lichen sclerosus vulvare Respiratory system maintain homeostasis
Respiratory system maintain homeostasis Knh
Knh Knh
Knh Cancer burden of disease
Cancer burden of disease Bharathi viswanathan
Bharathi viswanathan Opwekking 411 tekst
Opwekking 411 tekst Csce 411
Csce 411 Ncp nutrition care process
Ncp nutrition care process Comp 411
Comp 411 Seo931
Seo931 Cpsc 411
Cpsc 411 Csce 411
Csce 411 Ist 411
Ist 411 Csce 411
Csce 411 Comp 411 unc
Comp 411 unc Ist 411
Ist 411 Ist 411
Ist 411 Mgmt 411 purdue
Mgmt 411 purdue Dog breed 411
Dog breed 411 Nutritional assessment definition
Nutritional assessment definition Comp 411
Comp 411 Nutrition411
Nutrition411 Csc 411
Csc 411 411 database
411 database Comp 411
Comp 411 Spanish 411.net
Spanish 411.net