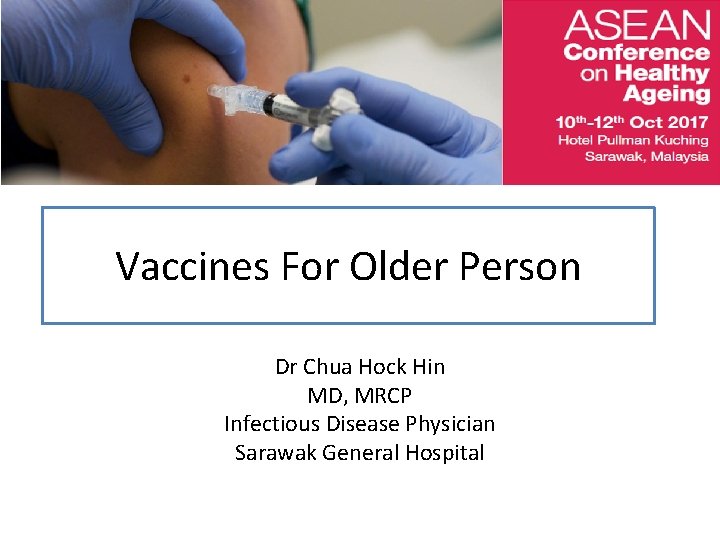
Vaccines For Older Person Dr Chua Hock Hin



















- Slides: 56
Vaccines For Older Person Dr Chua Hock Hin MD, MRCP Infectious Disease Physician Sarawak General Hospital
Outline Of This Talk • 1. What is the aim of vaccination in elderly patients ? • 2. What is the burden of disease in elderly patients? • 3. Immuno-senescence : How it impacts on the elderly ? • 4. Few common VPDs.

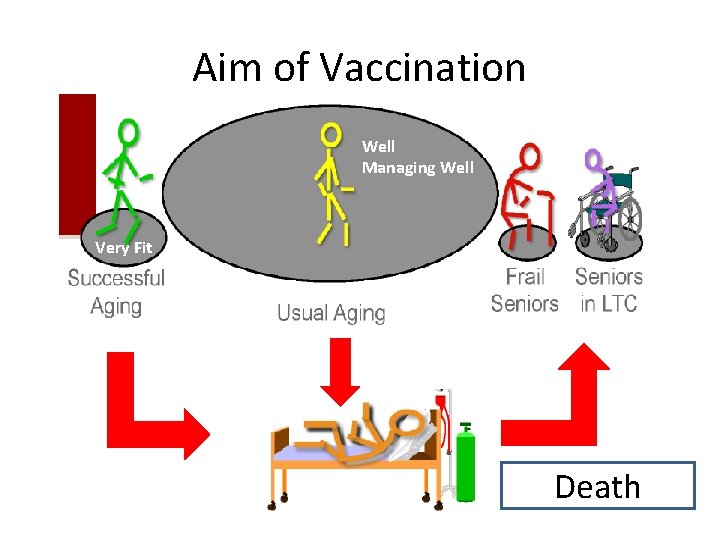
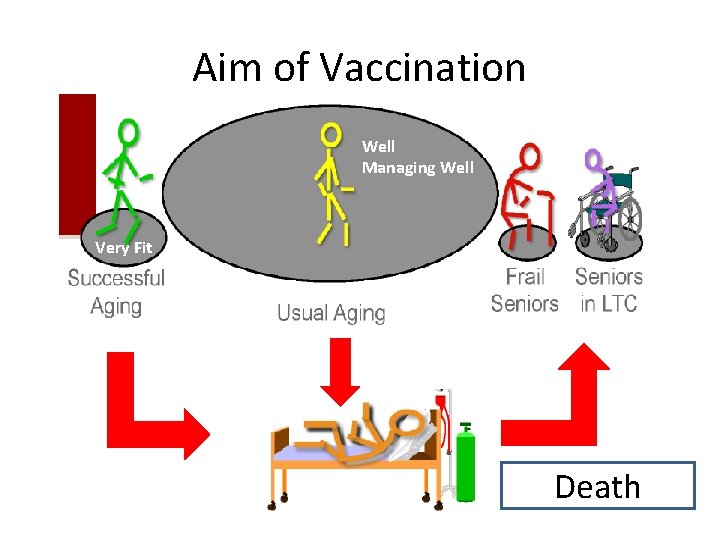
Aim of Vaccination Well Managing Well Very Fit Death
Aim of Vaccination Death
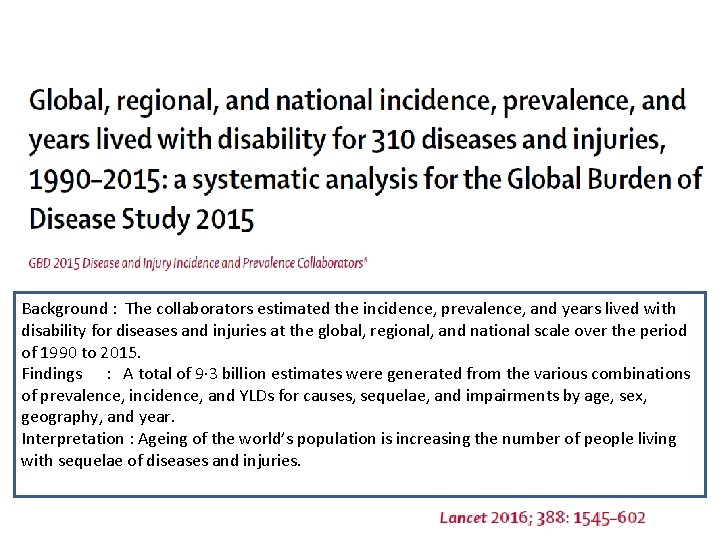
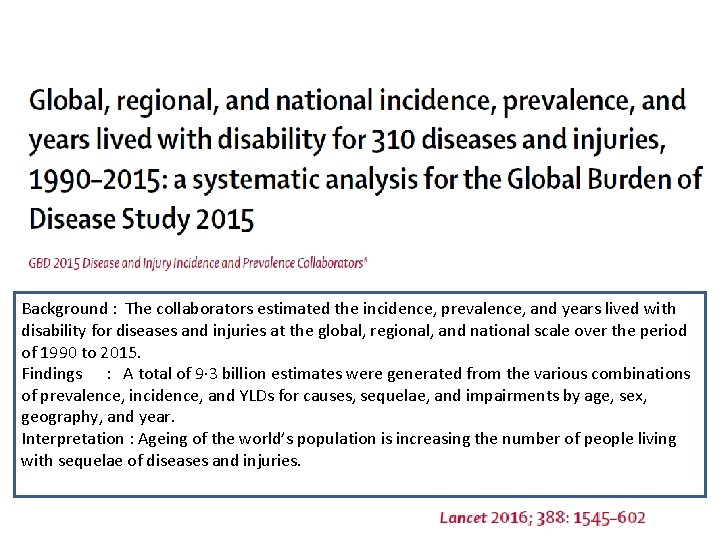
Background : The collaborators estimated the incidence, prevalence, and years lived with disability for diseases and injuries at the global, regional, and national scale over the period of 1990 to 2015. Findings : A total of 9· 3 billion estimates were generated from the various combinations of prevalence, incidence, and YLDs for causes, sequelae, and impairments by age, sex, geography, and year. Interpretation : Ageing of the world’s population is increasing the number of people living with sequelae of diseases and injuries.


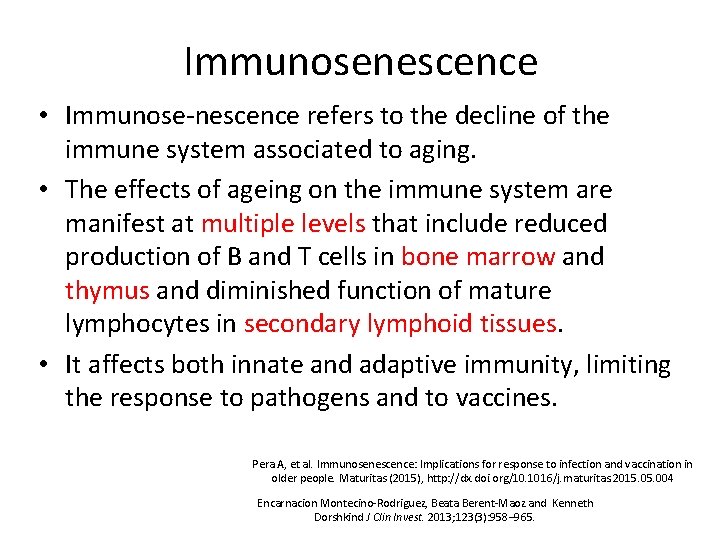
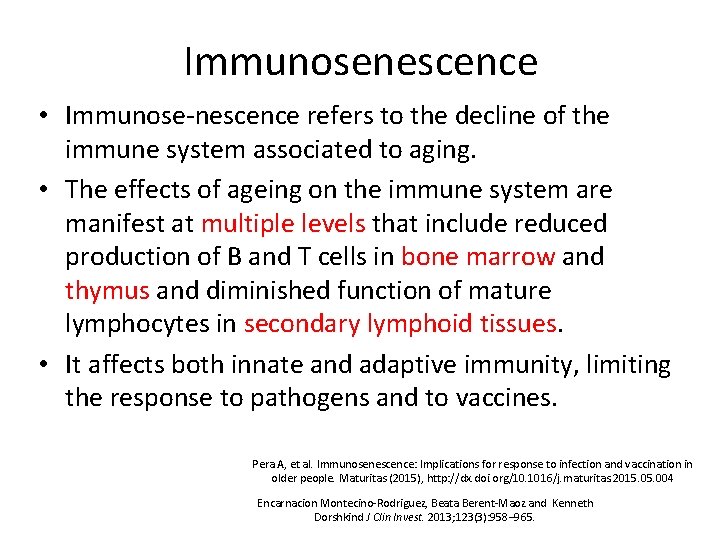
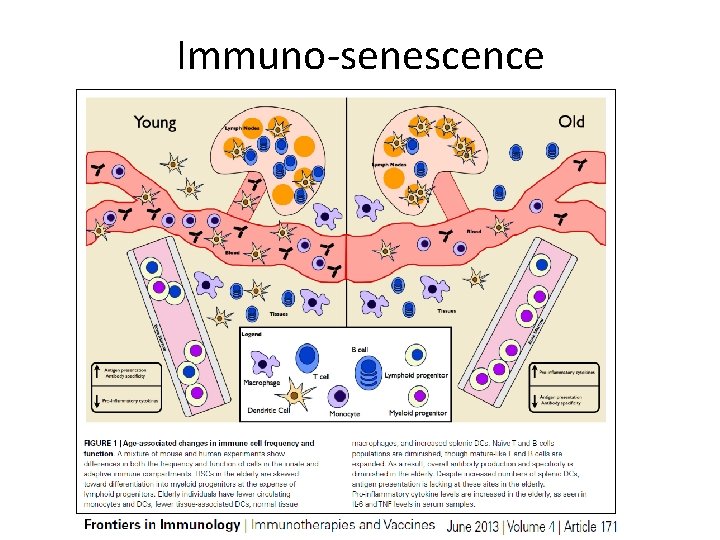
Immunosenescence • Immunose-nescence refers to the decline of the immune system associated to aging. • The effects of ageing on the immune system are manifest at multiple levels that include reduced production of B and T cells in bone marrow and thymus and diminished function of mature lymphocytes in secondary lymphoid tissues. • It affects both innate and adaptive immunity, limiting the response to pathogens and to vaccines. Pera A, et al. Immunosenescence: Implications for response to infection and vaccination in older people. Maturitas (2015), http: //dx. doi. org/10. 1016/j. maturitas. 2015. 004 Encarnacion Montecino-Rodriguez, Beata Berent-Maoz and Kenneth Dorshkind J Clin Invest. 2013; 123(3): 958– 965.
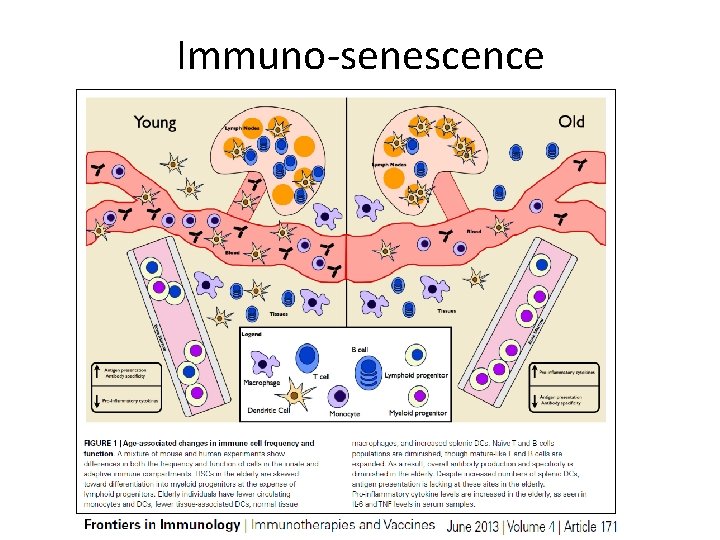
Immuno-senescence
Herpes Zoster Or Shingles

Herpes Zoster Or Shingles • Is caused by varicella zoster virus ( VZV ). • Pathogenesis : • VZV migrates from skin lesions via nerve axons and viremic spread to spinal and cranial sensory ganglia where it becomes dormant. • Later in life, VZV is reactivated ( usually within single ganglion ) to cause shingles or herpes zoster ( HZ ). • Individuals with HZ can transmit VZV to their contacts, who may develop varicella. • Household transmission rate of HZ is around 15%.
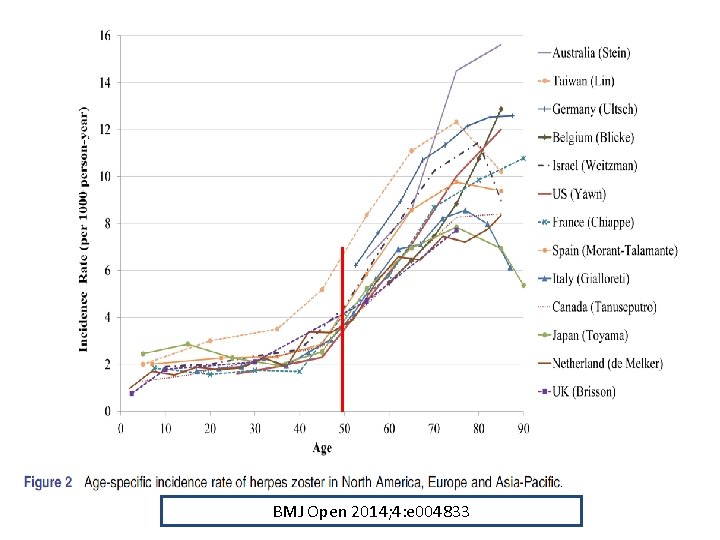
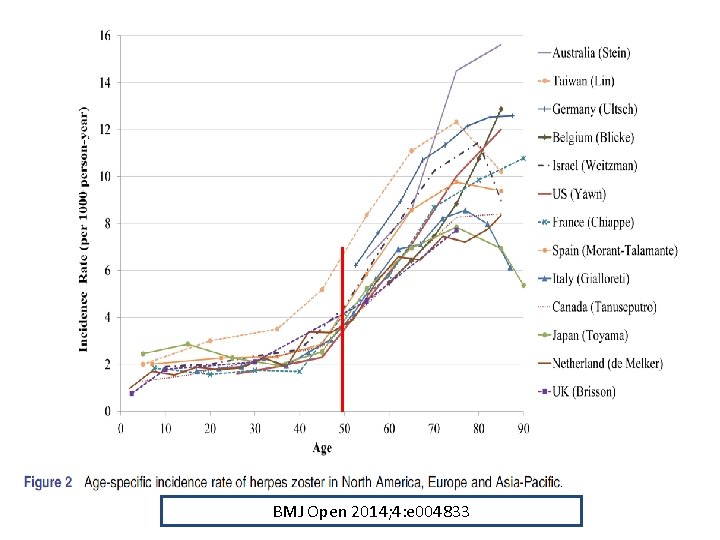
BMJ Open 2014; 4: e 004833
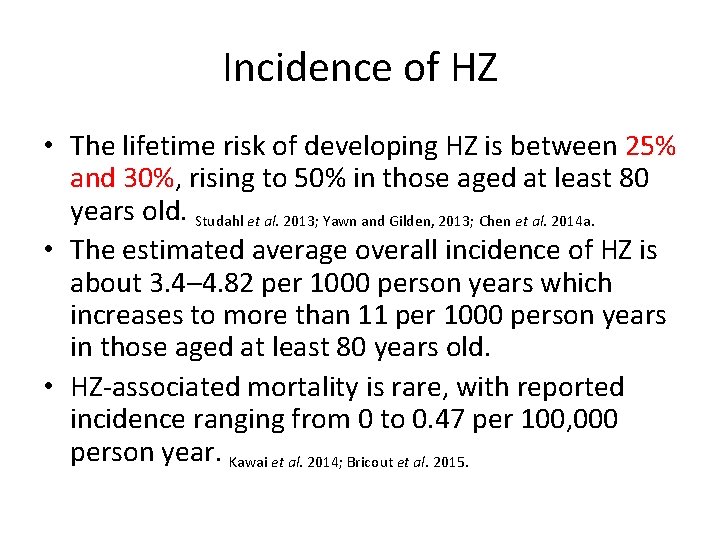
Incidence of HZ • The lifetime risk of developing HZ is between 25% and 30%, rising to 50% in those aged at least 80 years old. Studahl et al. 2013; Yawn and Gilden, 2013; Chen et al. 2014 a. • The estimated average overall incidence of HZ is about 3. 4– 4. 82 per 1000 person years which increases to more than 11 per 1000 person years in those aged at least 80 years old. • HZ-associated mortality is rare, with reported incidence ranging from 0 to 0. 47 per 100, 000 person year. Kawai et al. 2014; Bricout et al. 2015.
Post Herpetic Neuralgia ( PHN ) • Pain present for ≥ 90 days after HZ rash onset. • PHN is the most common complication of HZ. • Although the pain often resolves within a few weeks, it can last for several months or even years. • Factors associated with the development of PHN : – – – Greater severity of acute pain Older age Greater rash severity Immuno-compromised patients Restricted activities of daily living prior to HZ
Herpes Zoster Opthalmicus ( HZO ) • It accounts in 10 -20% of HZ cases. • The lifetime risk of developing HZO is approximately 1%. • Ocular complications typical of HZO can occur even when there is no visible rash. (zoster sine herpete ) • It can lead to blepharitis, kerato-conjunctivitis, iritis, scleritis, opthalmoplegia, optic neuritis and ptosis in 20 to 70% of HZO cases.

Treatment Of HZO • Oral antiviral drugs ( Acyclovir or Valacyclovir ) preferably within 72 h after rash onset. • However if > 72 hours and new lesions are present, treatment may still be useful. • Duration of treatment : 7 days ( maybe longer in older or immuno-compromised patient ). • Refer to opthalmologist for eye assessment. • Despite antiviral treatment, chronic disease can persist in 30% of patients with HZO, increasing to 70% in patients over 80 years old.
What is the impact of HZ ? • It has an adverse impact on quality of life (Qo. L) and activities of daily living. • Some patients, particularly older patients, lose their independence and require help from their families or paid caregivers. • Sleep and social activities are most severely affected. • Patients rarely recover to the same level as before the occurrence of HZ episode.
Prevention of HZ
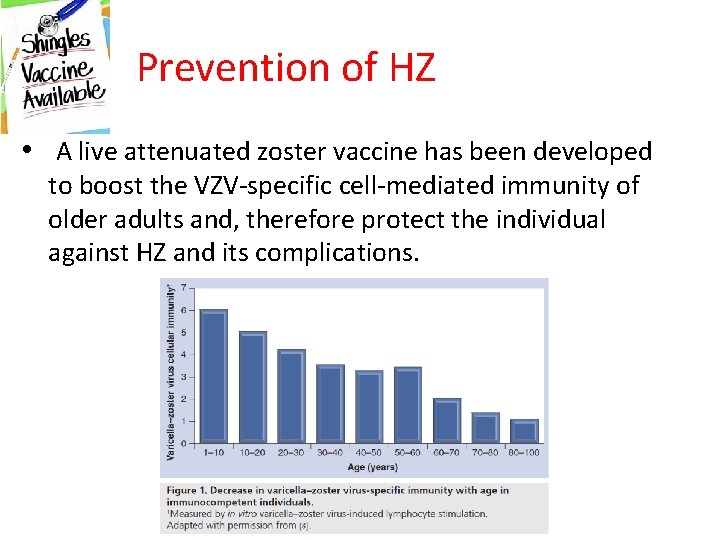
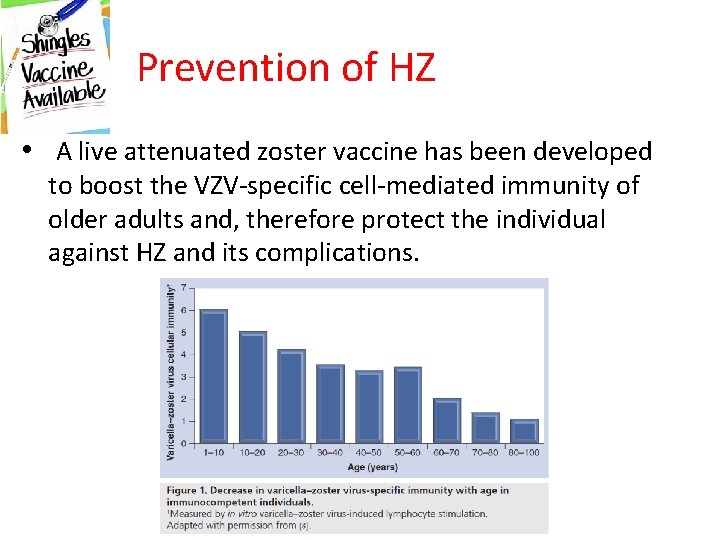
Prevention of HZ • A live attenuated zoster vaccine has been developed to boost the VZV-specific cell-mediated immunity of older adults and, therefore protect the individual against HZ and its complications.
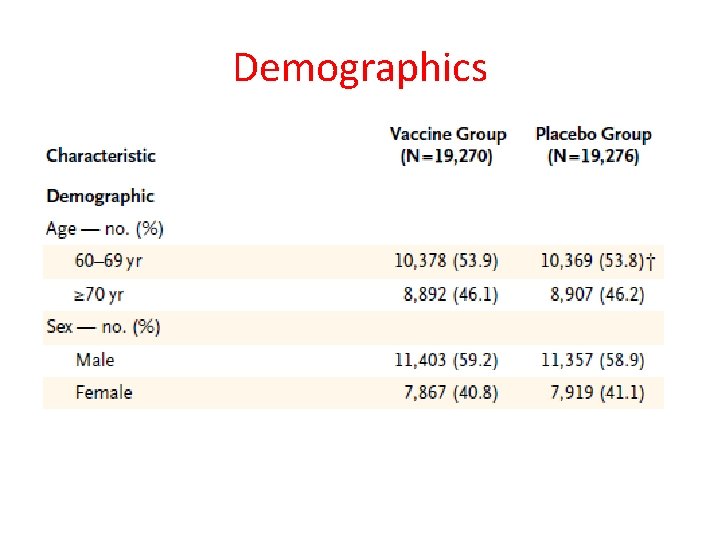
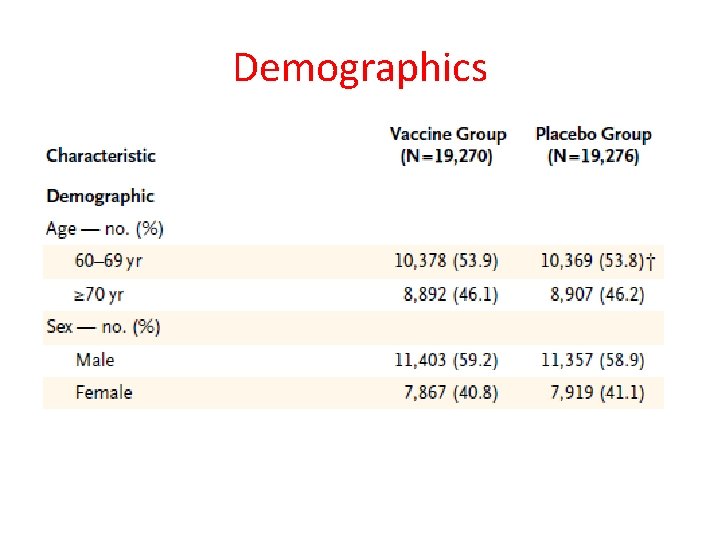
Demographics



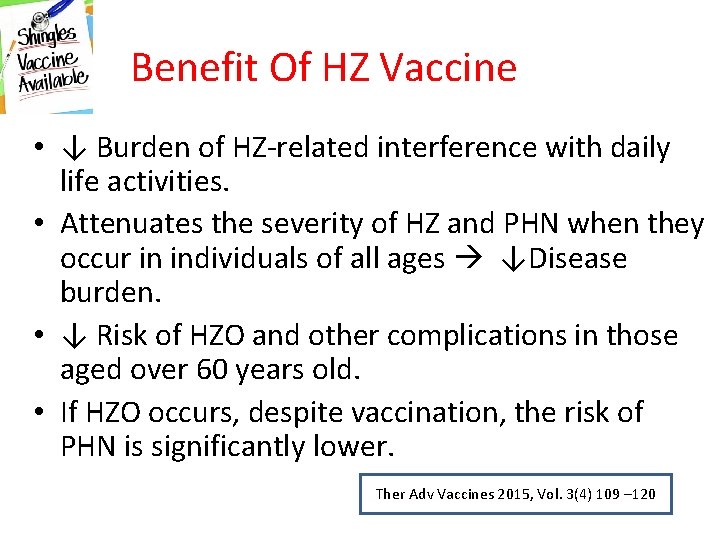
Benefit Of HZ Vaccine • ↓ Burden of HZ-related interference with daily life activities. • Attenuates the severity of HZ and PHN when they occur in individuals of all ages ↓Disease burden. • ↓ Risk of HZO and other complications in those aged over 60 years old. • If HZO occurs, despite vaccination, the risk of PHN is significantly lower. Ther Adv Vaccines 2015, Vol. 3(4) 109 – 120
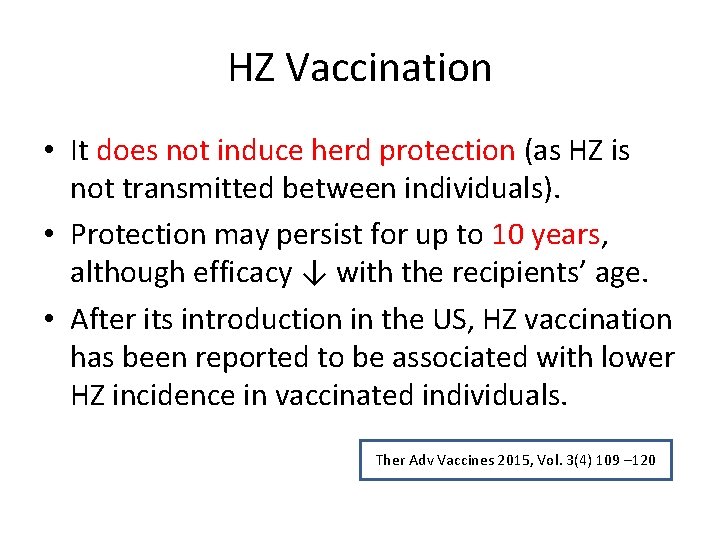
HZ Vaccination • It does not induce herd protection (as HZ is not transmitted between individuals). • Protection may persist for up to 10 years, although efficacy ↓ with the recipients’ age. • After its introduction in the US, HZ vaccination has been reported to be associated with lower HZ incidence in vaccinated individuals. Ther Adv Vaccines 2015, Vol. 3(4) 109 – 120
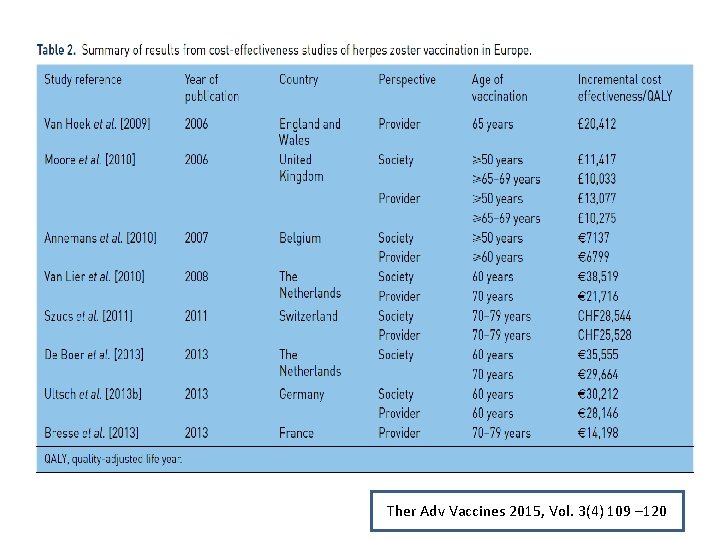
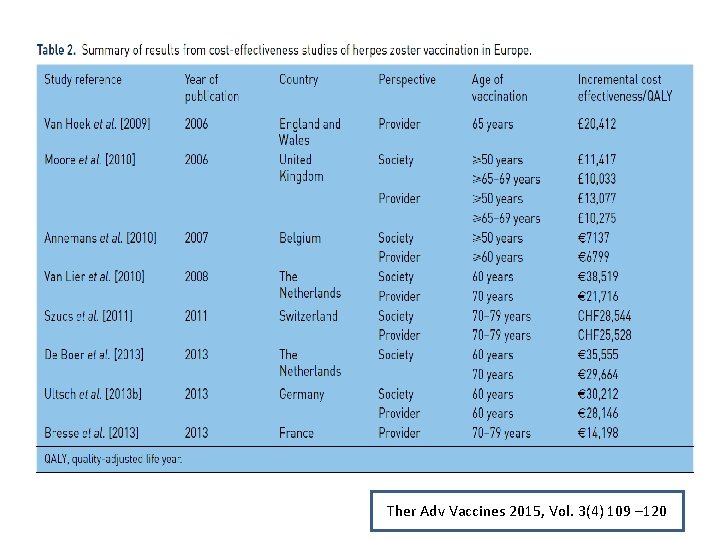
Ther Adv Vaccines 2015, Vol. 3(4) 109 – 120
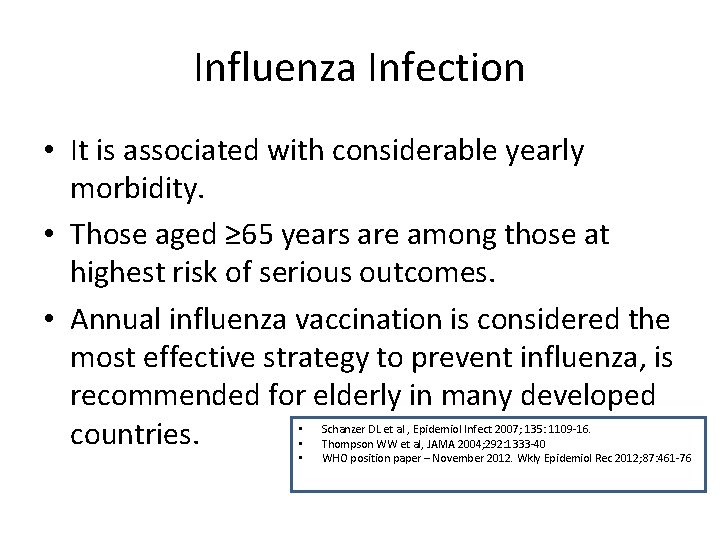
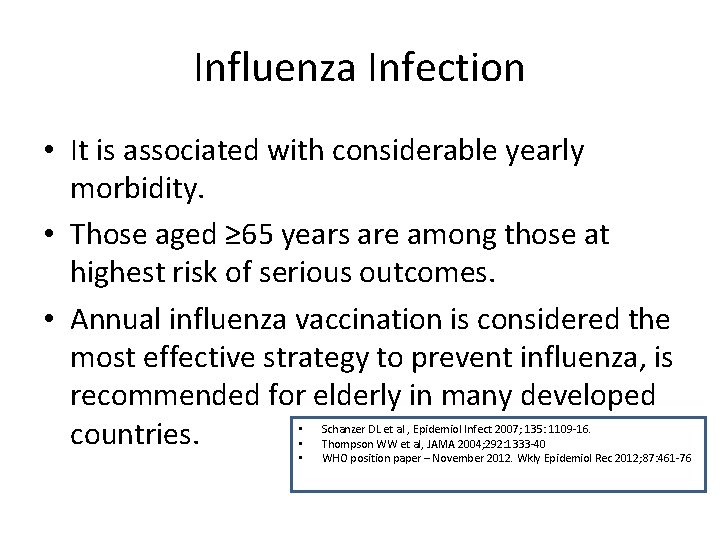
Influenza Infection • It is associated with considerable yearly morbidity. • Those aged ≥ 65 years are among those at highest risk of serious outcomes. • Annual influenza vaccination is considered the most effective strategy to prevent influenza, is recommended for elderly in many developed countries. • • • Schanzer DL et al , Epidemiol Infect 2007; 135: 1109 -16. Thompson WW et al, JAMA 2004; 292: 1333 -40 WHO position paper – November 2012. Wkly Epidemiol Rec 2012; 87: 461 -76


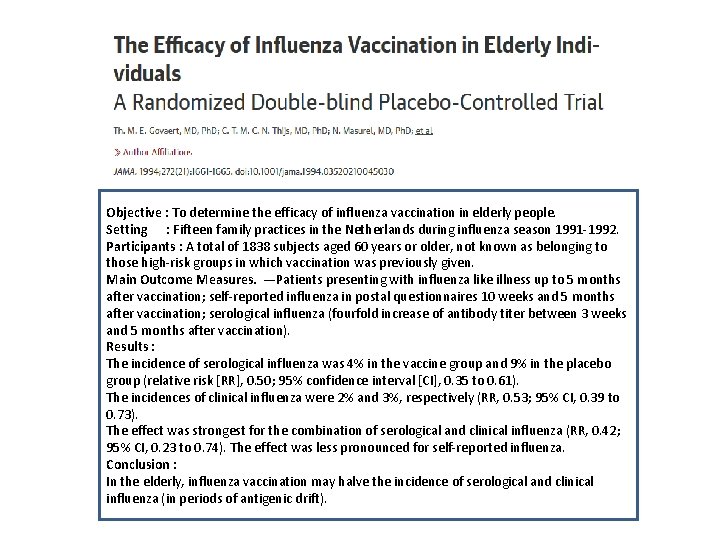
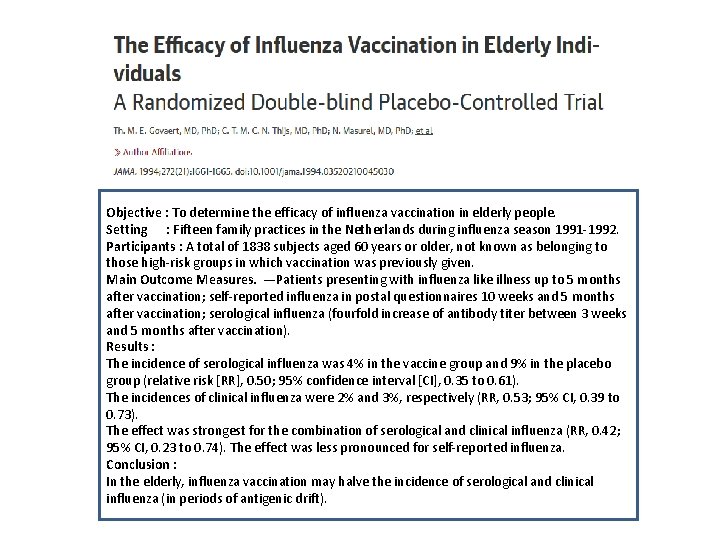
Objective : To determine the efficacy of influenza vaccination in elderly people. Setting : Fifteen family practices in the Netherlands during influenza season 1991 -1992. Participants : A total of 1838 subjects aged 60 years or older, not known as belonging to those high-risk groups in which vaccination was previously given. Main Outcome Measures. —Patients presenting with influenza like illness up to 5 months after vaccination; self-reported influenza in postal questionnaires 10 weeks and 5 months after vaccination; serological influenza (fourfold increase of antibody titer between 3 weeks and 5 months after vaccination). Results : The incidence of serological influenza was 4% in the vaccine group and 9% in the placebo group (relative risk [RR], 0. 50; 95% confidence interval [CI], 0. 35 to 0. 61). The incidences of clinical influenza were 2% and 3%, respectively (RR, 0. 53; 95% CI, 0. 39 to 0. 73). The effect was strongest for the combination of serological and clinical influenza (RR, 0. 42; 95% CI, 0. 23 to 0. 74). The effect was less pronounced for self-reported influenza. Conclusion : In the elderly, influenza vaccination may halve the incidence of serological and clinical influenza (in periods of antigenic drift).



At the end of the day • Most seasonal influenza vaccines for elderly showed statistically significant efficacy or effectiveness, the magnitude of which, however, largely varied.
Pneumonia- The Old Enemy • Sir William Osler described, “Pneumonia remains now, as then, the most serious acute disease with which physicians have to deal; serious because it attacks the old, the feeble … persons who are not able to withstand the sudden sharp onset of the malady, ” still stands the test of time.
Pneumonia • Pneumonia is the fourth-leading cause of death globally, and Streptococcus pneumoniae is the most important causative pathogen. World Health Statistics 2014. • In developed countries, such as Japan, > 95% of deaths from pneumonia occur in the elderly (≥ 65 years old).

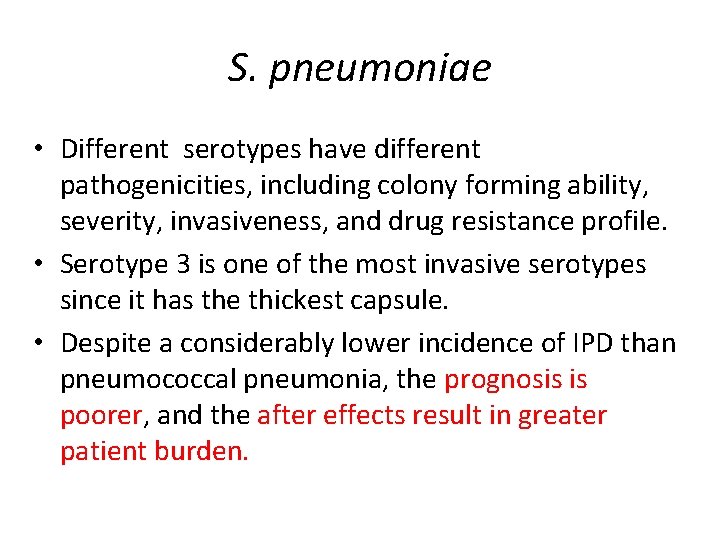
S. pneumoniae • Different serotypes have different pathogenicities, including colony forming ability, severity, invasiveness, and drug resistance profile. • Serotype 3 is one of the most invasive serotypes since it has the thickest capsule. • Despite a considerably lower incidence of IPD than pneumococcal pneumonia, the prognosis is poorer, and the after effects result in greater patient burden.
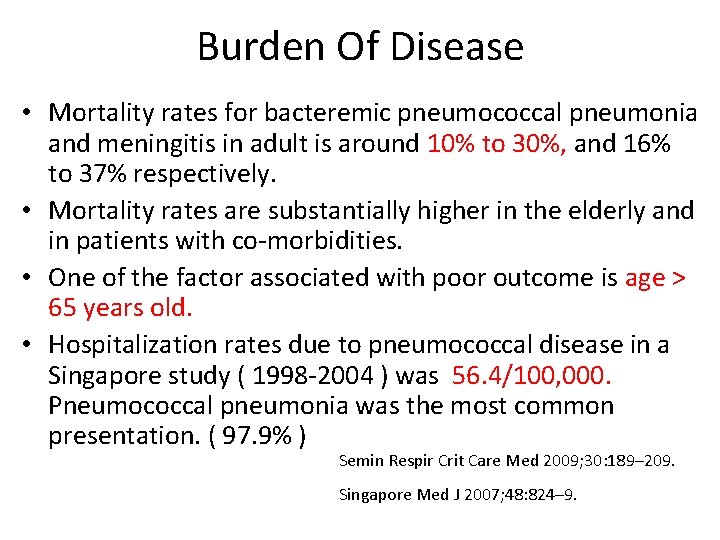
Burden Of Disease • Mortality rates for bacteremic pneumococcal pneumonia and meningitis in adult is around 10% to 30%, and 16% to 37% respectively. • Mortality rates are substantially higher in the elderly and in patients with co-morbidities. • One of the factor associated with poor outcome is age > 65 years old. • Hospitalization rates due to pneumococcal disease in a Singapore study ( 1998 -2004 ) was 56. 4/100, 000. Pneumococcal pneumonia was the most common presentation. ( 97. 9% ) Semin Respir Crit Care Med 2009; 30: 189– 209. Singapore Med J 2007; 48: 824– 9.
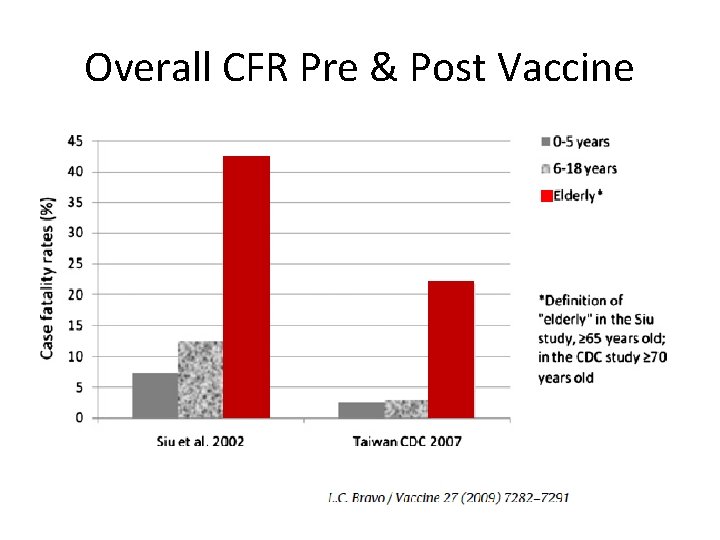
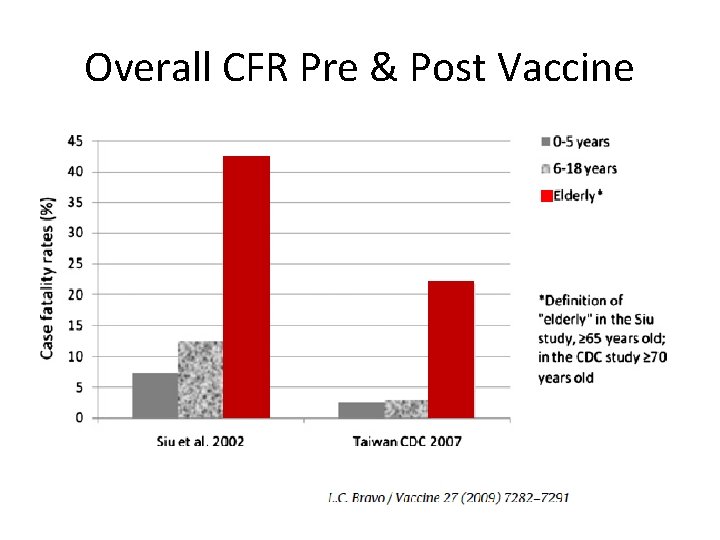
Overall CFR Pre & Post Vaccine
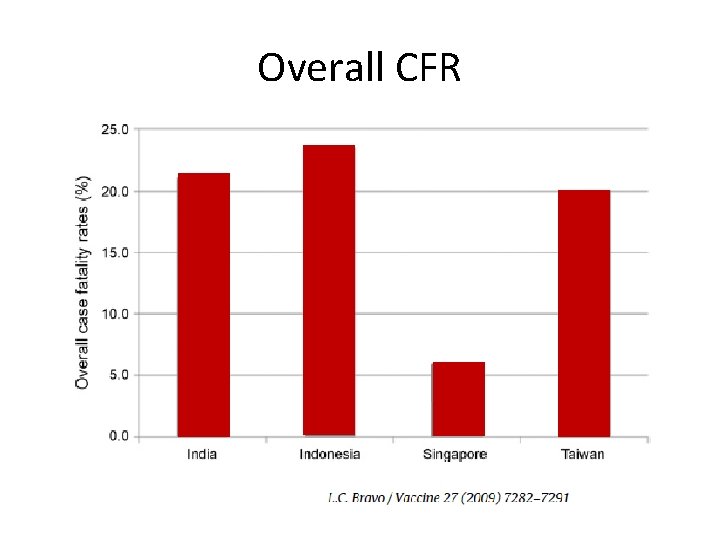
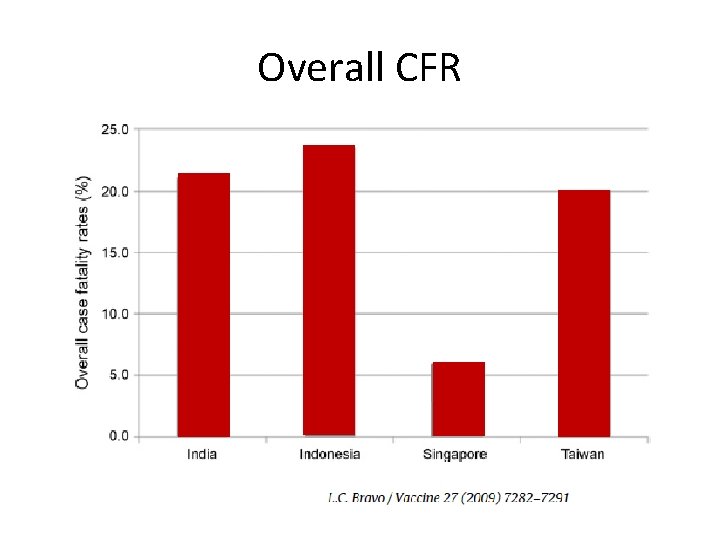
Overall CFR
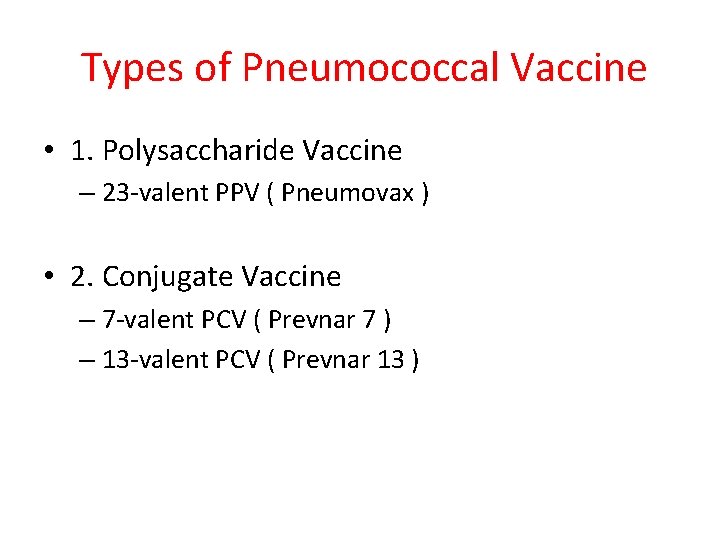
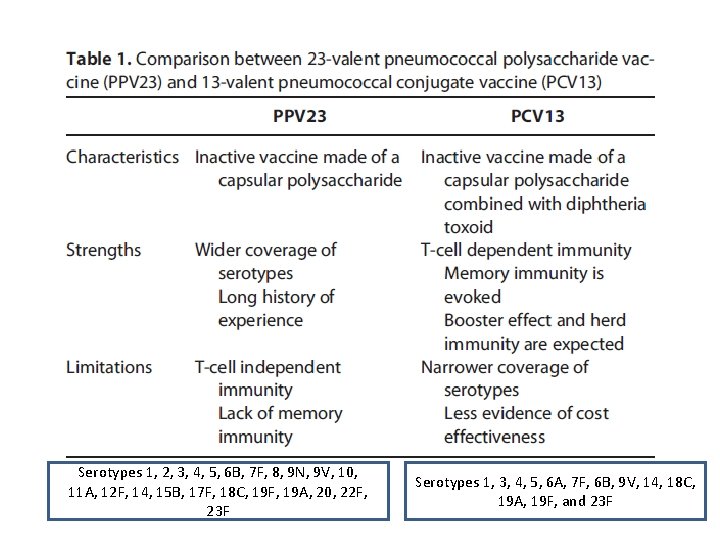
Types of Pneumococcal Vaccine • 1. Polysaccharide Vaccine – 23 -valent PPV ( Pneumovax ) • 2. Conjugate Vaccine – 7 -valent PCV ( Prevnar 7 ) – 13 -valent PCV ( Prevnar 13 )
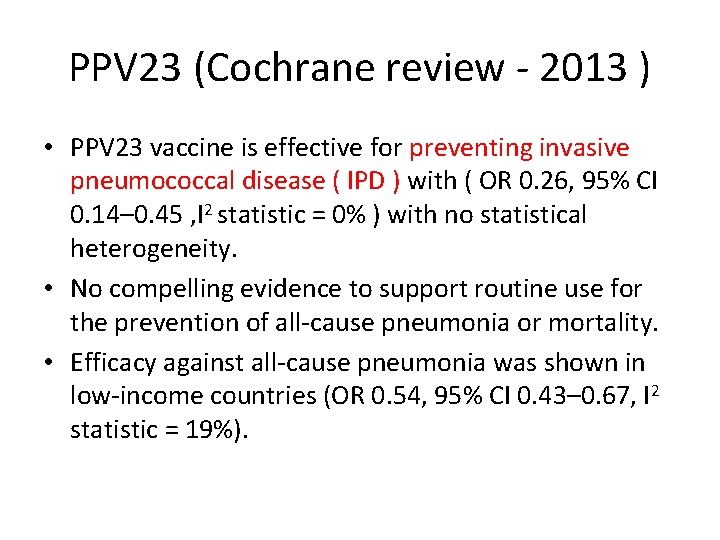
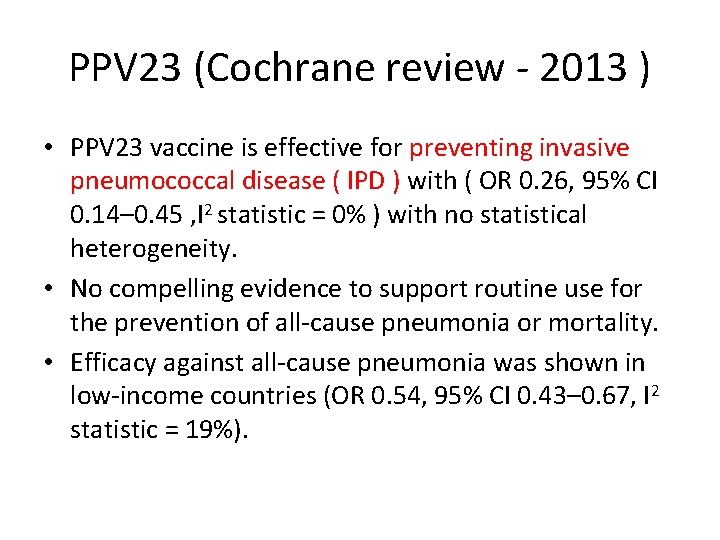
PPV 23 (Cochrane review - 2013 ) • PPV 23 vaccine is effective for preventing invasive pneumococcal disease ( IPD ) with ( OR 0. 26, 95% CI 0. 14– 0. 45 , I 2 statistic = 0% ) with no statistical heterogeneity. • No compelling evidence to support routine use for the prevention of all-cause pneumonia or mortality. • Efficacy against all-cause pneumonia was shown in low-income countries (OR 0. 54, 95% CI 0. 43– 0. 67, I 2 statistic = 19%).
CAPi. TA




Conclusion • Among older adults, PCV 13 was effective in preventing vaccine-type pneumococcal, bacteremic, and non-bacteremic communityacquired pneumonia and vaccine type invasive pneumococcal disease but not in preventing community-acquired pneumonia from any cause.
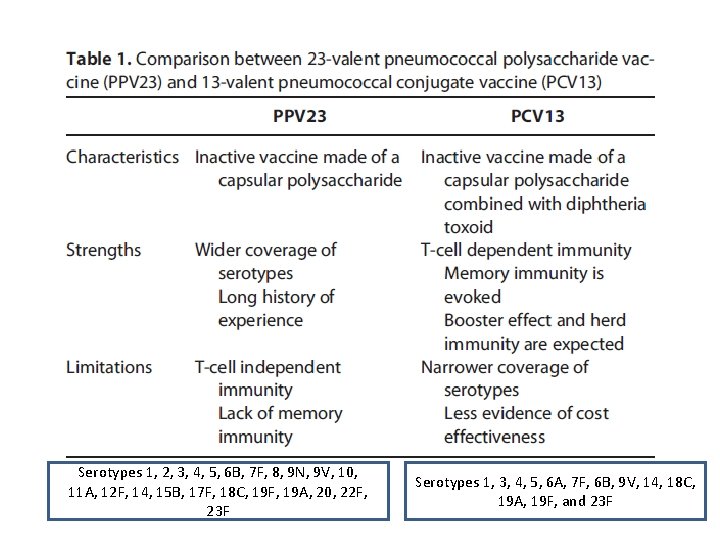
Serotypes 1, 2, 3, 4, 5, 6 B, 7 F, 8, 9 N, 9 V, 10, 11 A, 12 F, 14, 15 B, 17 F, 18 C, 19 F, 19 A, 20, 22 F, 23 F Serotypes 1, 3, 4, 5, 6 A, 7 F, 6 B, 9 V, 14, 18 C, 19 A, 19 F, and 23 F
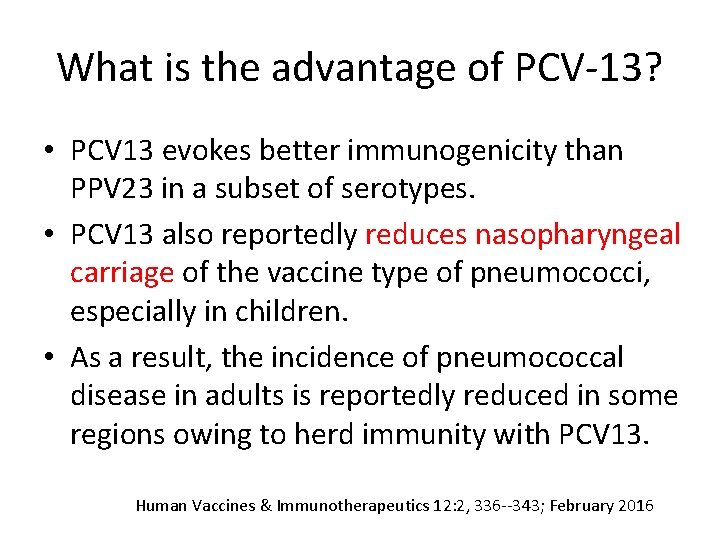
What is the advantage of PCV-13? • PCV 13 evokes better immunogenicity than PPV 23 in a subset of serotypes. • PCV 13 also reportedly reduces nasopharyngeal carriage of the vaccine type of pneumococci, especially in children. • As a result, the incidence of pneumococcal disease in adults is reportedly reduced in some regions owing to herd immunity with PCV 13. Human Vaccines & Immunotherapeutics 12: 2, 336 --343; February 2016
What is the effect of vaccination? • The pneumococcal serotype distribution have shifted from vaccine-type to non-vaccine-type serotypes since the introduction of PCVs. • The more PPV 23 and PCV 13 become prevalent both in infants and adults, the further the coverage of vaccine-type serotypes is expected to decrease in the future. Human Vaccines & Immunotherapeutics 12: 2, 336 --343; February 2016
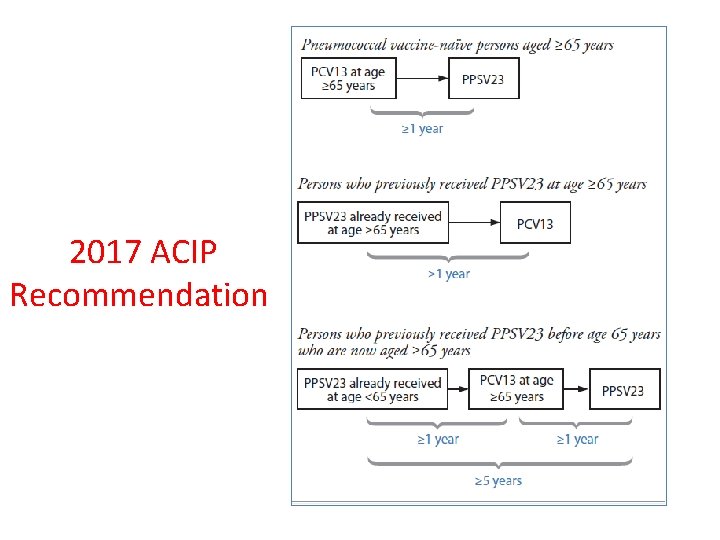
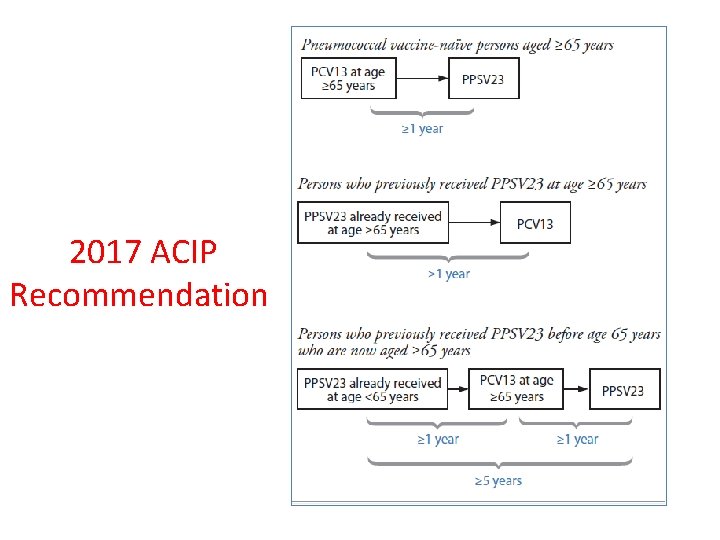
2017 ACIP Recommendation
Conclusions • Vaccine protection is not 100%. • Immuno-senescence plays a role in determining vaccine efficacy. • Considering the morbidity and mortality caused by these vaccine preventable diseases, we should opt for a better “Prevention” approach rather than “Cure” , as the later approach may proved more costly.

 Chua hock hin
Chua hock hin Life is older than the trees
Life is older than the trees Lạy chúa giêsu con tin tưởng nơi chúa
Lạy chúa giêsu con tin tưởng nơi chúa Nào cảm tạ chúa vì chúa rất nhân từ
Nào cảm tạ chúa vì chúa rất nhân từ Con yêu chúa chúa ơi
Con yêu chúa chúa ơi 1 person plural
1 person plural First person
First person Person person = new person()
Person person = new person() First person second person third person chart
First person second person third person chart Jürgen hock
Jürgen hock Dennis hock
Dennis hock 2005-1947
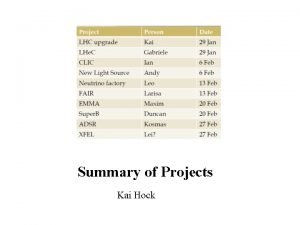
2005-1947 Kai hock
Kai hock Dee ward hock
Dee ward hock Hock aun teh
Hock aun teh Phang swee kim
Phang swee kim Dee ward hock
Dee ward hock Dee hock
Dee hock Spacing out vaccines
Spacing out vaccines Could vaccines breed viciousness
Could vaccines breed viciousness Global alliance for vaccines and immunization
Global alliance for vaccines and immunization Live vaccines mnemonic
Live vaccines mnemonic Glyphosate in vaccines
Glyphosate in vaccines Edible vaccines pros and cons
Edible vaccines pros and cons Dna vaccines pros and cons
Dna vaccines pros and cons Edible vaccines pros and cons
Edible vaccines pros and cons Hep b vaccines
Hep b vaccines Immune checkpoint inhibitors mechanism of action
Immune checkpoint inhibitors mechanism of action Hep b vaccines
Hep b vaccines Glyphosate in vaccines
Glyphosate in vaccines Brighton collaboration case definitions for vaccines
Brighton collaboration case definitions for vaccines Tubertest lecture
Tubertest lecture History of vaccines pdf
History of vaccines pdf Diseases with vaccines
Diseases with vaccines Edible vaccines in pharmacognosy
Edible vaccines in pharmacognosy Dr lim poh hin
Dr lim poh hin Gedicht ich ging im walde so für mich hin
Gedicht ich ging im walde so für mich hin Joe hin tjio y albert levan
Joe hin tjio y albert levan Pencil tracing of hull id number
Pencil tracing of hull id number Iller lech isar inn fließen zu der donau hin
Iller lech isar inn fließen zu der donau hin I hin
I hin Hin format
Hin format Lee poh hin
Lee poh hin Yong mok hin
Yong mok hin Older individuals who are blind program
Older individuals who are blind program Younger cells cuboidal older cells flattened
Younger cells cuboidal older cells flattened Sos spelling for older students
Sos spelling for older students Future medical
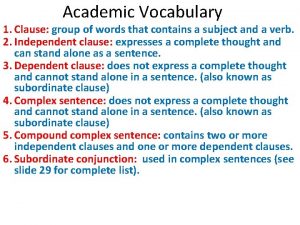
Future medical Juan continued playing although he injured his knee
Juan continued playing although he injured his knee Mental health and older adults
Mental health and older adults Older women's cohousing
Older women's cohousing Older adults mental health
Older adults mental health Downsizing and divesting older business
Downsizing and divesting older business Ajayan is ten years older than vijayan
Ajayan is ten years older than vijayan Mental health and older adults
Mental health and older adults Taller and younger shorter and older
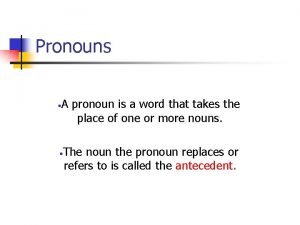
Taller and younger shorter and older Nouns for sister
Nouns for sister