Urinary Incontinence in Women Dr Hazem AlMandeel Associate







- Slides: 35

Urinary Incontinence in Women Dr. Hazem Al-Mandeel Associate Professor Department of Obstetrics and Gynecology College of Medicine, King Saud University
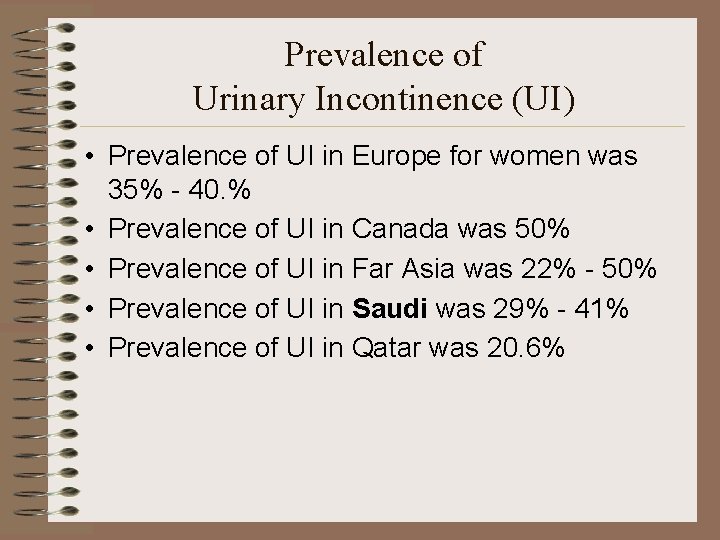
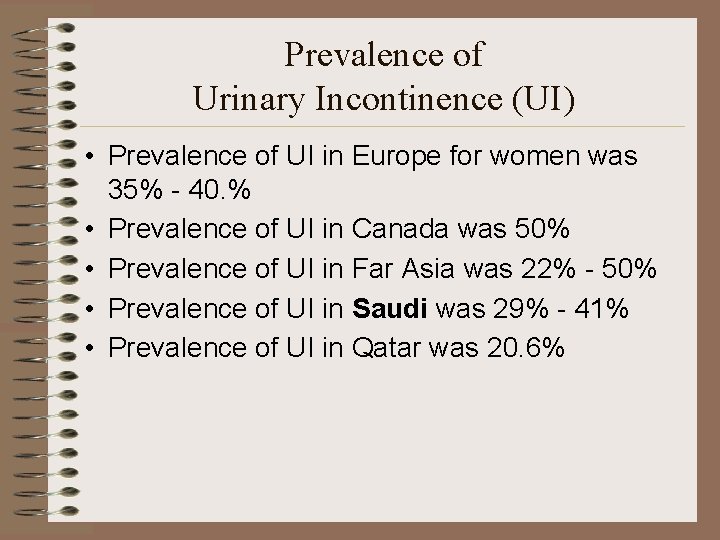
Prevalence of Urinary Incontinence (UI) • Prevalence of UI in Europe for women was 35% - 40. % • Prevalence of UI in Canada was 50% • Prevalence of UI in Far Asia was 22% - 50% • Prevalence of UI in Saudi was 29% - 41% • Prevalence of UI in Qatar was 20. 6%
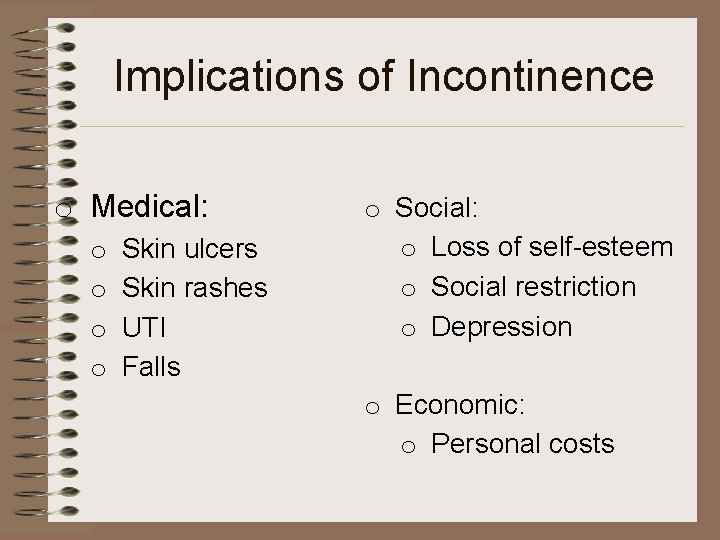
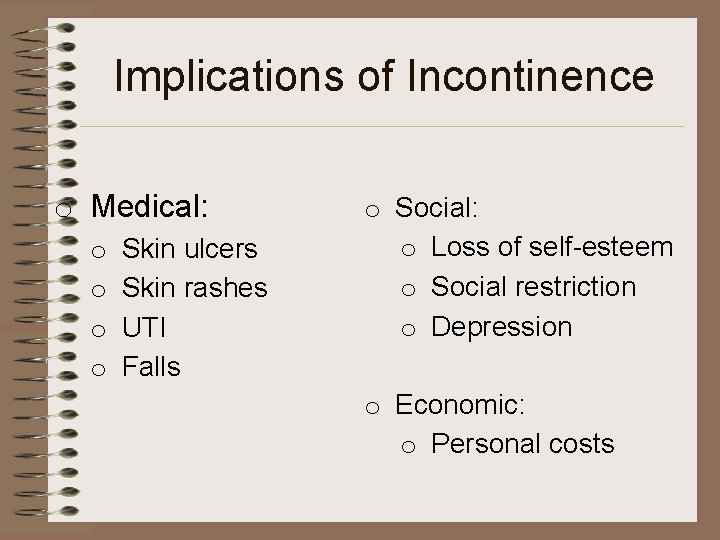
Implications of Incontinence o Medical: o o Skin ulcers Skin rashes UTI Falls o Social: o Loss of self-esteem o Social restriction o Depression o Economic: o Personal costs
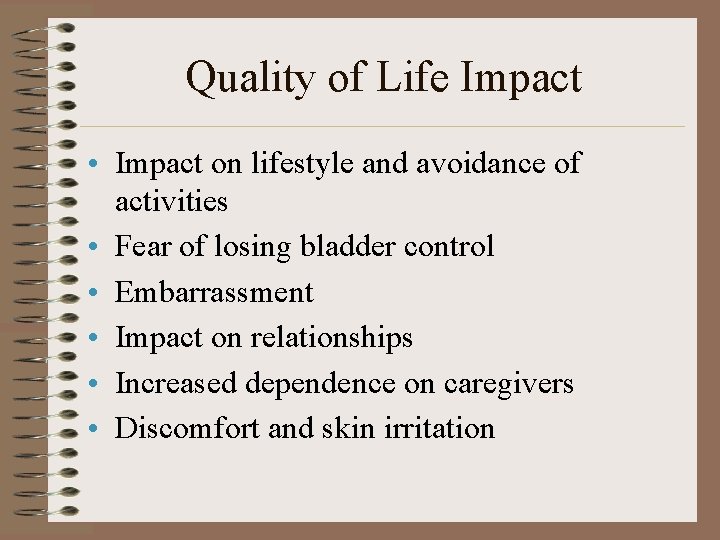
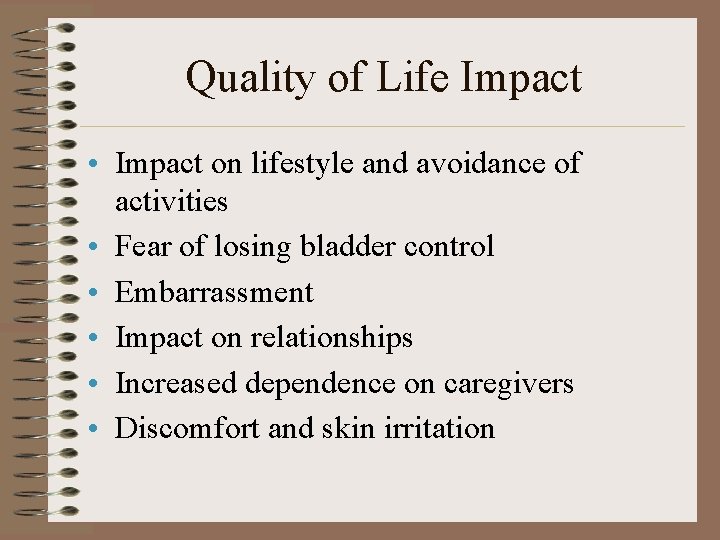
Quality of Life Impact • Impact on lifestyle and avoidance of activities • Fear of losing bladder control • Embarrassment • Impact on relationships • Increased dependence on caregivers • Discomfort and skin irritation
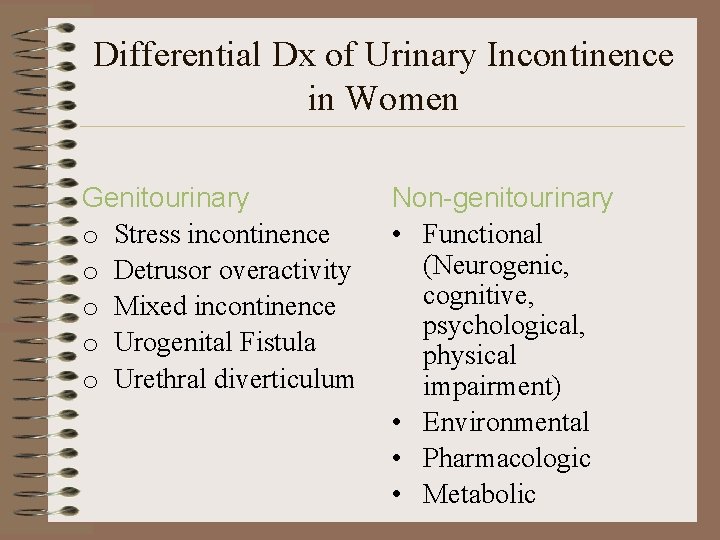
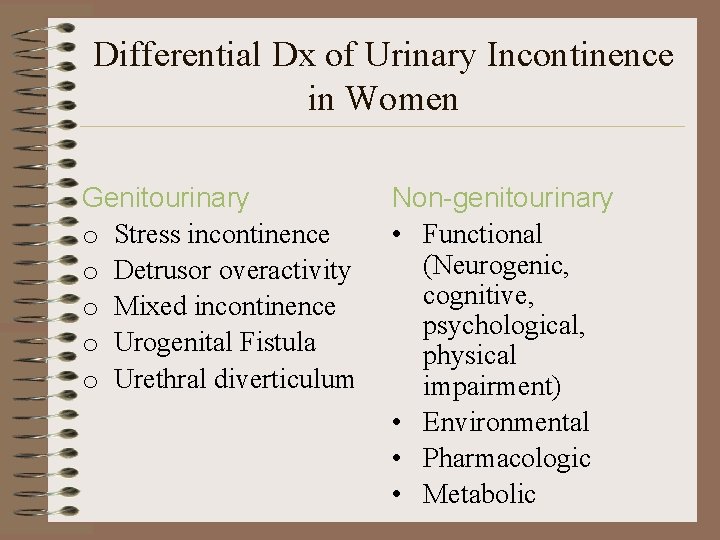
Differential Dx of Urinary Incontinence in Women Genitourinary o Stress incontinence o Detrusor overactivity o Mixed incontinence o Urogenital Fistula o Urethral diverticulum Non-genitourinary • Functional (Neurogenic, cognitive, psychological, physical impairment) • Environmental • Pharmacologic • Metabolic
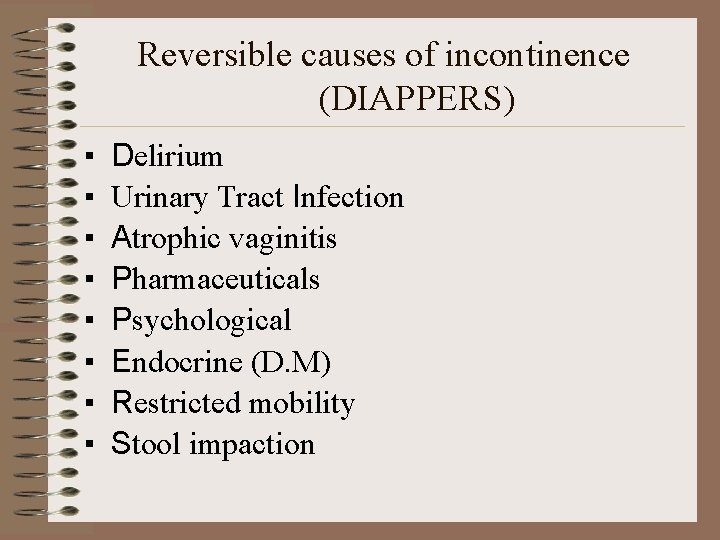
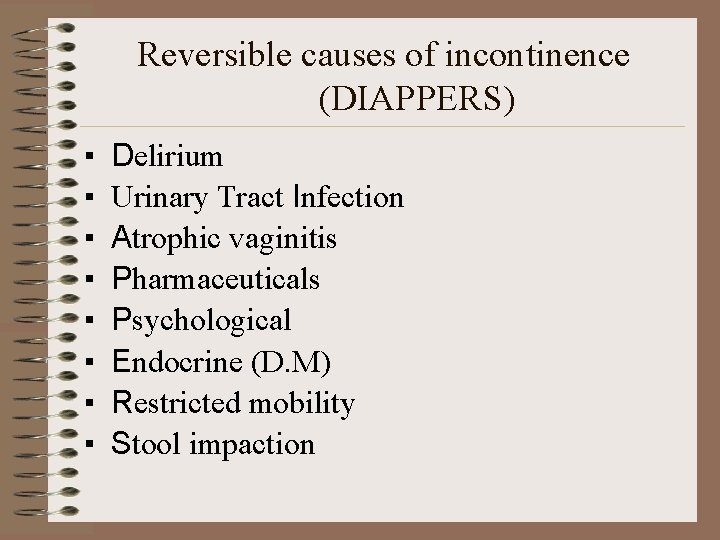
Reversible causes of incontinence (DIAPPERS) ▪ ▪ ▪ ▪ Delirium Urinary Tract Infection Atrophic vaginitis Pharmaceuticals Psychological Endocrine (D. M) Restricted mobility Stool impaction
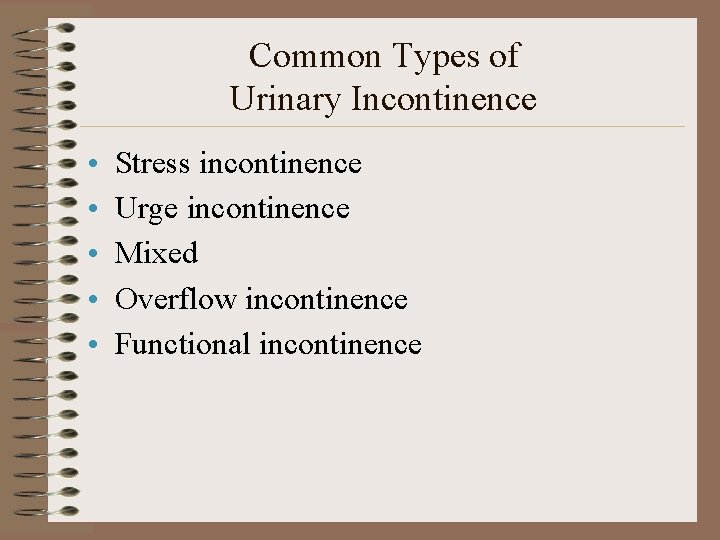
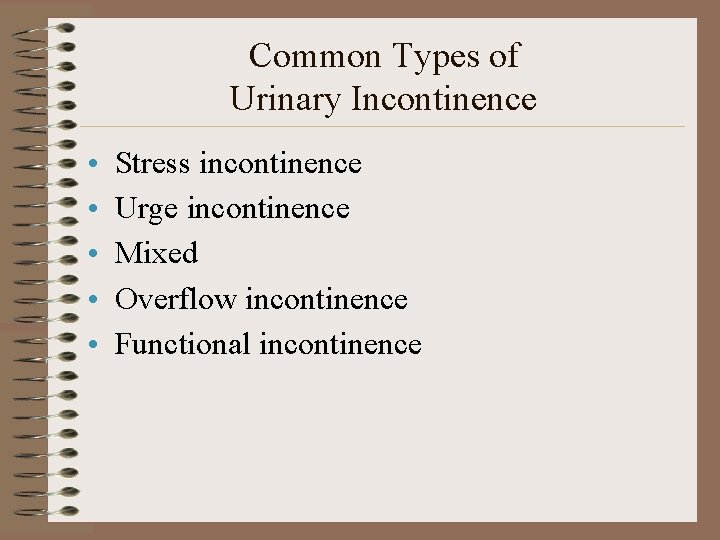
Common Types of Urinary Incontinence • • • Stress incontinence Urge incontinence Mixed Overflow incontinence Functional incontinence
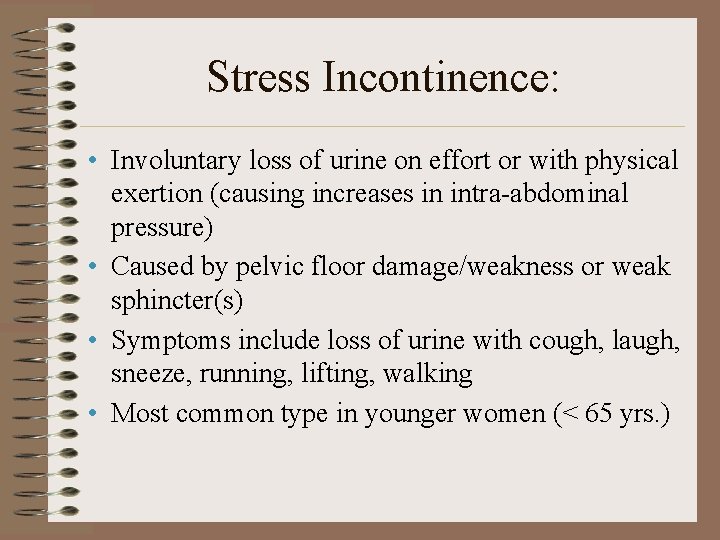
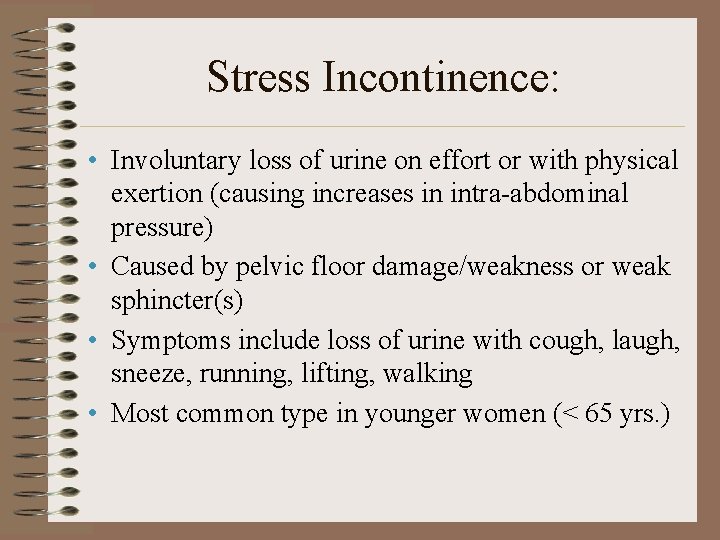
Stress Incontinence: • Involuntary loss of urine on effort or with physical exertion (causing increases in intra-abdominal pressure) • Caused by pelvic floor damage/weakness or weak sphincter(s) • Symptoms include loss of urine with cough, laugh, sneeze, running, lifting, walking • Most common type in younger women (< 65 yrs. )
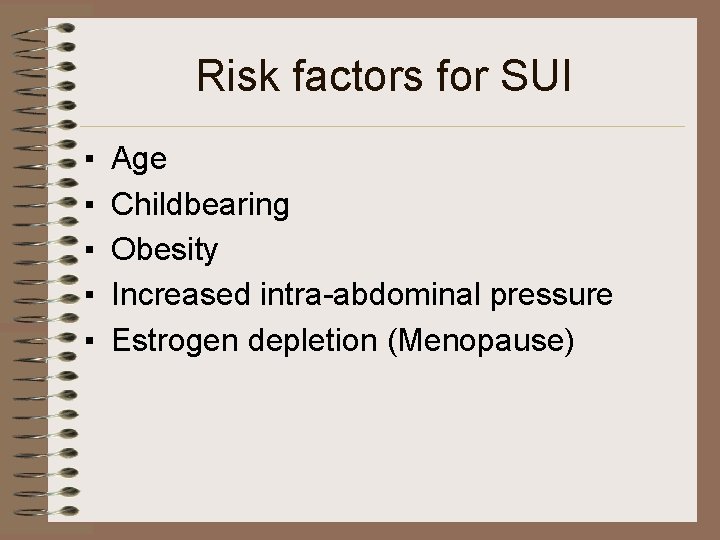
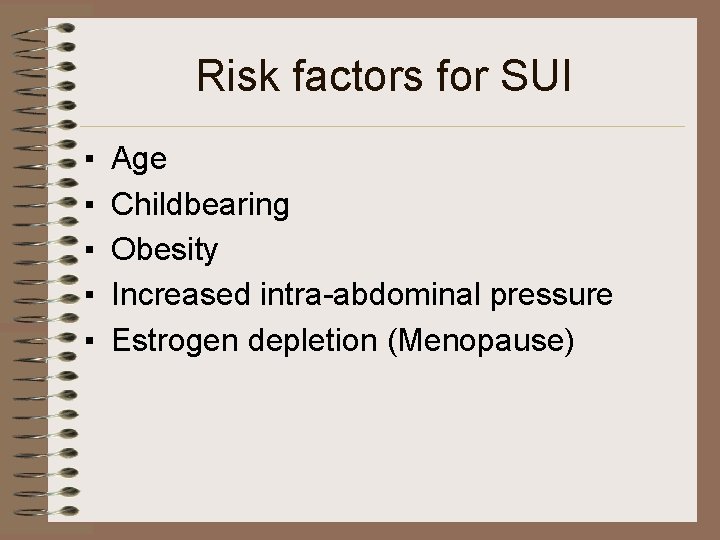
Risk factors for SUI ▪ ▪ ▪ Age Childbearing Obesity Increased intra-abdominal pressure Estrogen depletion (Menopause)

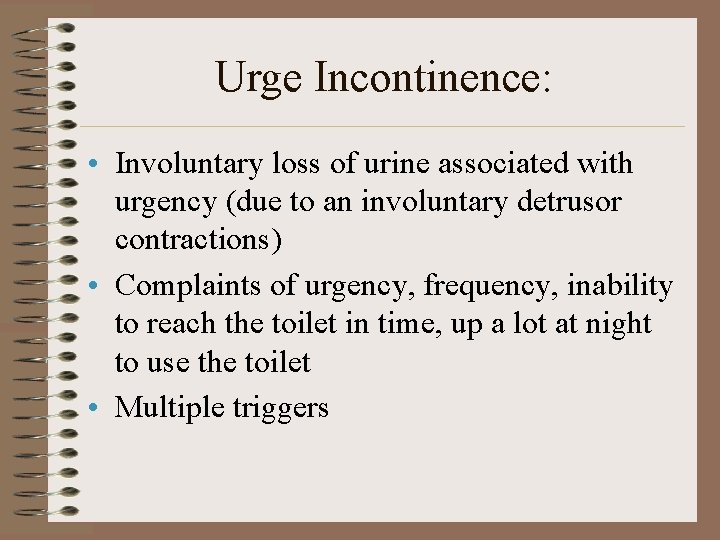
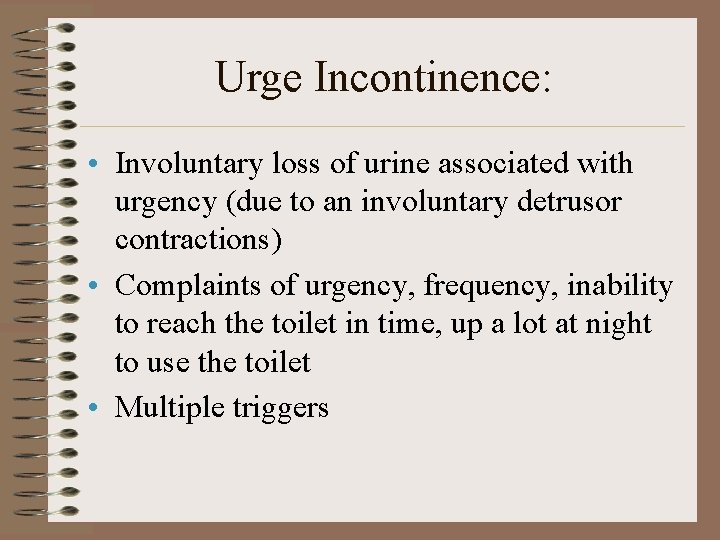
Urge Incontinence: • Involuntary loss of urine associated with urgency (due to an involuntary detrusor contractions) • Complaints of urgency, frequency, inability to reach the toilet in time, up a lot at night to use the toilet • Multiple triggers
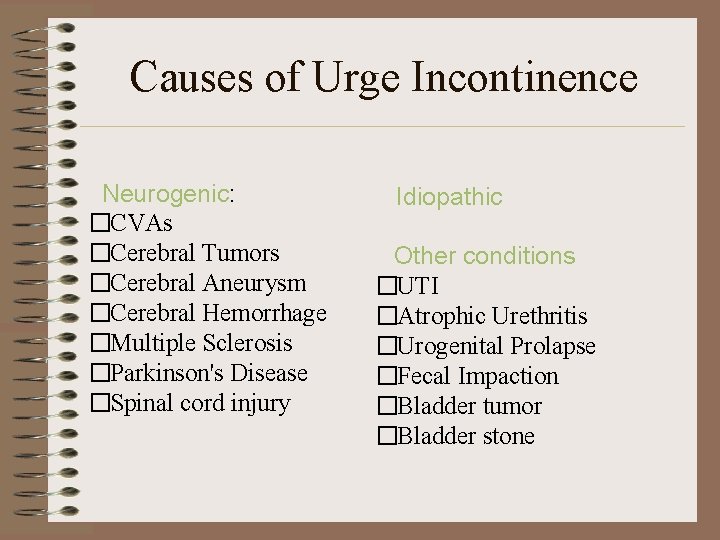
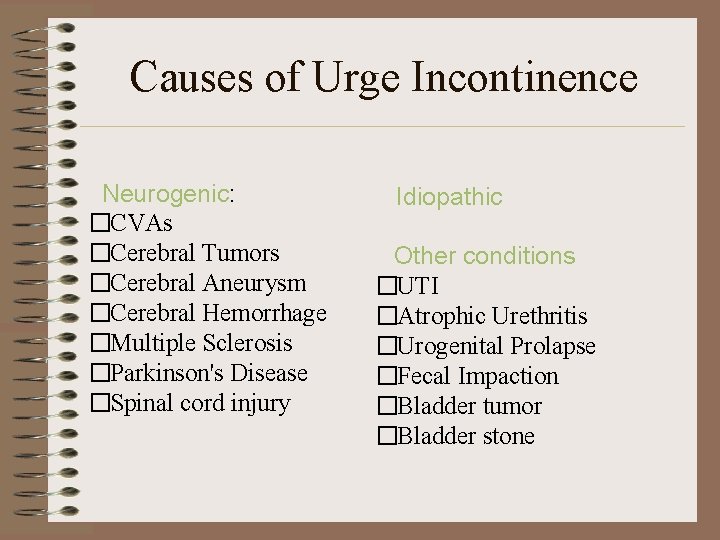
Causes of Urge Incontinence Neurogenic: �CVAs �Cerebral Tumors �Cerebral Aneurysm �Cerebral Hemorrhage �Multiple Sclerosis �Parkinson's Disease �Spinal cord injury Idiopathic Other conditions �UTI �Atrophic Urethritis �Urogenital Prolapse �Fecal Impaction �Bladder tumor �Bladder stone
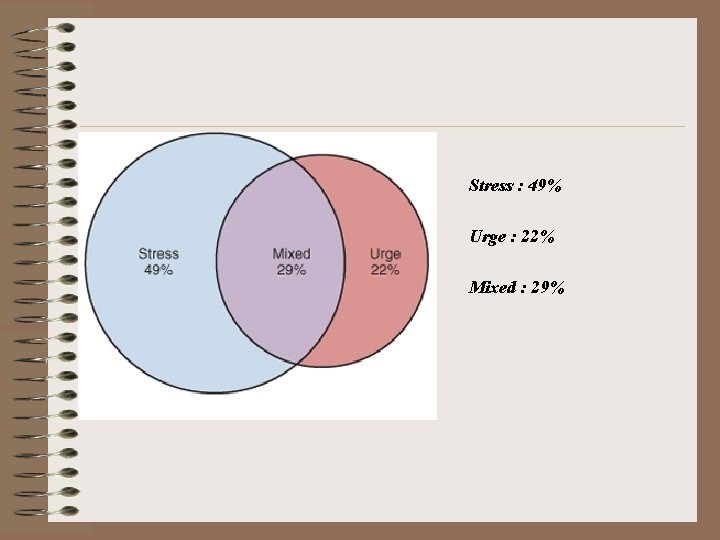
Mixed Incontinence: • Combination of stress and urge incontinence • Common presentation of mixed symptoms • Urodynamics necessary to confirm
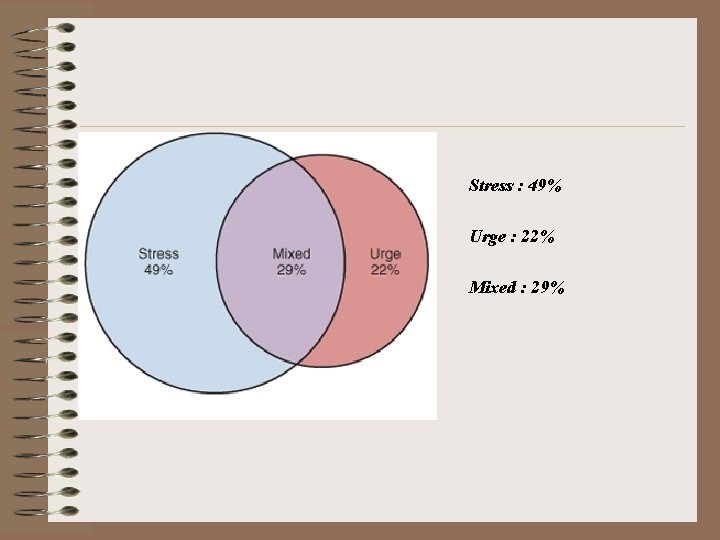
Stress : 49% Urge : 22% Mixed : 29%
Overflow Incontinence Large bladder volumes result in an intravesical pressure greater than the urethral closure pressure � Causes: o. Atonic Bladder o. Outlet Obstruction
Chronic Urinary Retention: • Outlet obstruction or bladder underactivity • May be related to previous surgery, aging, development of bad bladder habits, or neurologic disorders • Medication, such as antidepressants • May present with symptoms of stress or urge incontinence, continuous leakage, or urinary tract infection

Functional and Transient Incontinence: • • • Mostly in the elderly Urinary tract infection Restricted mobility Severe constipation Medication - diuretics, antipsychotics Psychological/cognitive deficiency
Diagnosis of Urinary Incontinence ▪ ▪ ▪ History Physical Voiding Diary PVR Urinalysis Urodynamics
Patient History: • Focus on medical, neurologic, genitourinary history • Review voiding patterns/fluid intake • Voiding diary • Review medications • Explore symptoms (duration, most bothersome, frequency, precipitants) • Assess mental status and mobility
Symptoms: • • • Frequency Nocturia Dysuria Incomplete emptying Incontinence Urgency Recurrent infections Dyspareunia Prolapse
Physical Examination: • General examination • Edema, neurologic abnormalities, mobility, cognition, dexterity • • Abdominal examination Pelvic and rectal exam - women Examination of back and lower limbs Observe urine loss with cough

Urinalysis: • Conditions associated with overactive bladder • • • Hematuria Pyuria Bacteriuria Glucosuria Proteinuria • Urine culture
Postvoid Residual Volume (PVR): • If clinically indicated accurate PVR can be done by • Catheterization • Ultrasound • PVR of <50 ml is considered adequate, repetitive PVR >200 ml is considered inadequate • Use clinical judgment when interpreting PVR results in the intermediate range (50 -199 ml)
Treatment : Stress Incontinence ◆Nonsurgical ◆Pelvic floor muscle training (Kegel) ◆Biofeedback ◆Electrical stimulation ◆Pessaries ◆Medications ◆Surgical : recreating urethral support ◆Abdominal ◆Vaginal
Kegel Exercise • • • 10 – 20 repetitions three times per day Hold contraction for 5 to 10 seconds A set can be done to suppress urgency Results take 6 – 8 weeks to manifest NOT to be done while voiding Improvement & cure rates as high as 60%
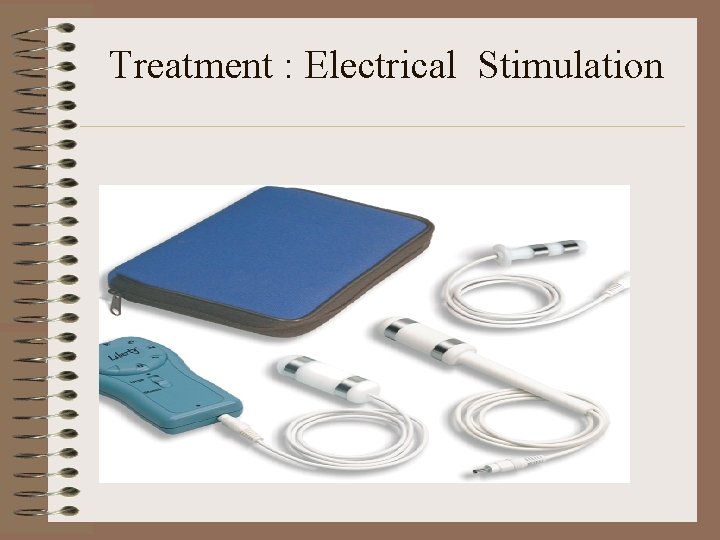
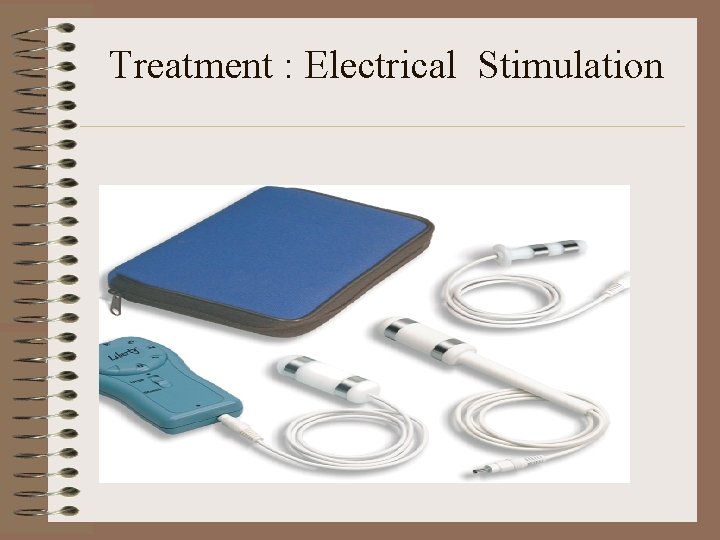
Treatment : Electrical Stimulation
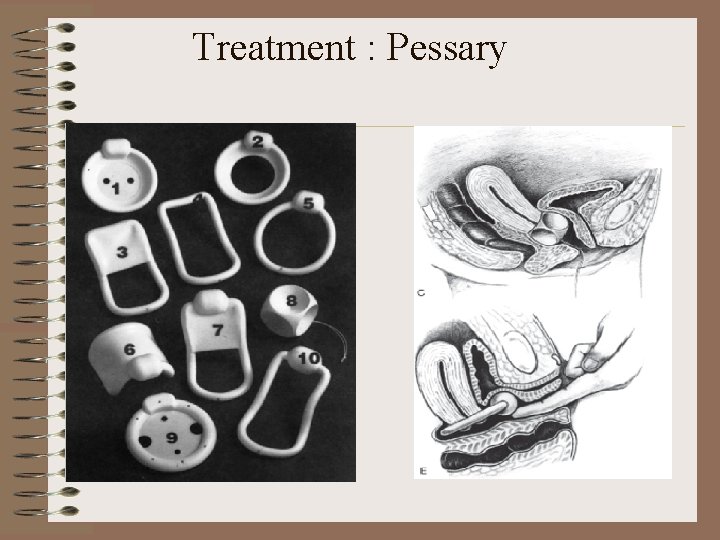
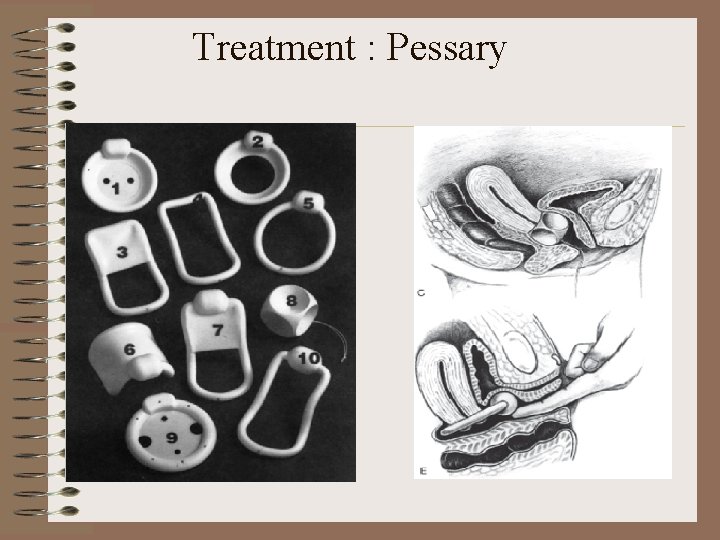
Treatment : Pessary
Treatments : Surgical ◆Abdominal approaches ◆Open retropubic colposuspension (Burch) ◆Pubo-vaginal sling ◆Midurethral tape procedure (e. g. TVT, TOT, TVTO, Mini Slings) ◆Periurethral Bulking Agents

Treatment Modalities for OAB • • Behavioural Modification Drug Treatment Neuromodulation (for refractory cases) Surgical Treatment (for refractory cases)

Behavioral Modification Bladder retraining Education Pelvic Floor muscle exercises Behavioral Modification Lifestyle changes Toileting programs
Bladder Retraining • Bladder Drill: – Increase intervals between voids – Aim for q 2 -3 h • Timed Voids (spinal cord) – Voiding times pre-selected e. g. . q 2 h – Interval based on avoiding leakage • Prompted Voids – Fixed time interval between voids – Third party prompt – Interval based on avoiding leakage

Lifestyle Interventions • • Elimination of bladder irritants Manage fluid intake Cessation of smoking Weight reduction Bowel regulations Use diuretics judiciously (not before bed) Reduce physical barriers to toilet (use bedside commode)
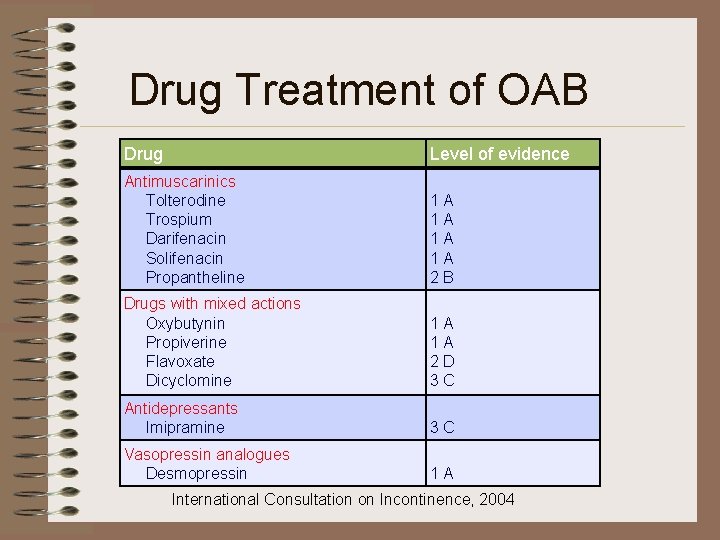
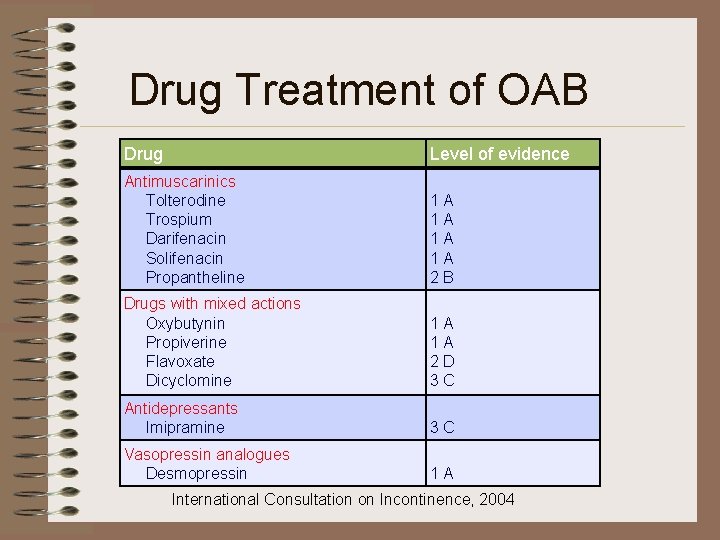
Drug Treatment of OAB Drug Level of evidence Antimuscarinics Tolterodine Trospium Darifenacin Solifenacin Propantheline 1 A 1 A 2 B Drugs with mixed actions Oxybutynin Propiverine Flavoxate Dicyclomine 1 A 1 A 2 D 3 C Antidepressants Imipramine 3 C Vasopressin analogues Desmopressin 1 A International Consultation on Incontinence, 2004
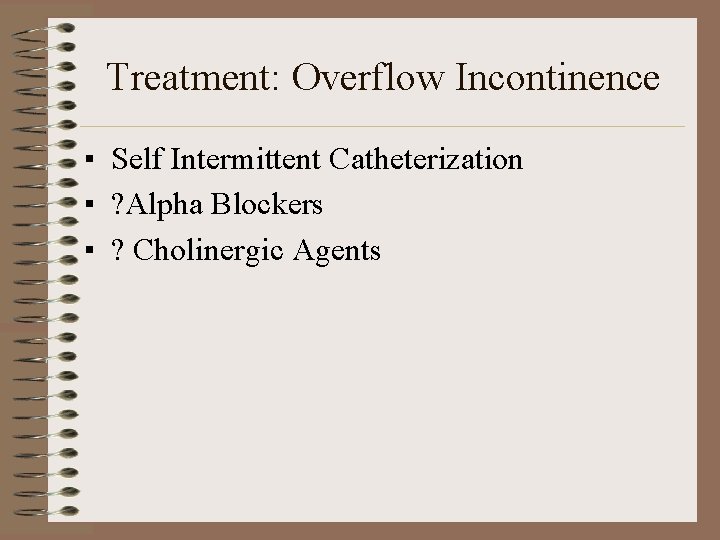
Treatment: Overflow Incontinence ▪ Self Intermittent Catheterization ▪ ? Alpha Blockers ▪ ? Cholinergic Agents
Treatment: Mixed Incontinence Treat the component which is most troubling to the patient
 Acfi domains
Acfi domains Acupuncture for incontinence
Acupuncture for incontinence Sacral reflex
Sacral reflex Coital incontinence
Coital incontinence برنامهxx
برنامهxx Bcs professional membership
Bcs professional membership Associate degree duo gift
Associate degree duo gift Ruckus accredited partner
Ruckus accredited partner Imeche associate membership
Imeche associate membership Safety associate
Safety associate Lonestar nursing application deadline
Lonestar nursing application deadline Michelin aad program
Michelin aad program Name something you associate with superman
Name something you associate with superman Associate's degree in the netherlands
Associate's degree in the netherlands Associate program
Associate program Associate degree rmit
Associate degree rmit Promotion from assistant to associate professor
Promotion from assistant to associate professor What is an associate director
What is an associate director Ultra vires meaning
Ultra vires meaning What is incose
What is incose To associate
To associate Associate warden
Associate warden Lahc associate's degree
Lahc associate's degree Child development program director permit
Child development program director permit Berstoff gearbox repair
Berstoff gearbox repair Associate consultant in capgemini
Associate consultant in capgemini Adobe audition certification
Adobe audition certification Tecniche associate al pensiero computazionale:
Tecniche associate al pensiero computazionale: Harper college associate degrees
Harper college associate degrees Marine corps league uniform regulations
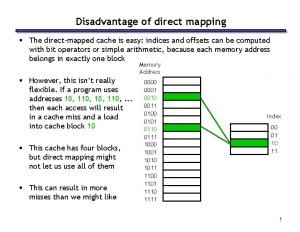
Marine corps league uniform regulations Direct mapping cache
Direct mapping cache Hea associate fellowship
Hea associate fellowship Associate degree startdag
Associate degree startdag Critical reading active process of discovery
Critical reading active process of discovery Rcog associate
Rcog associate Jeannie watkins
Jeannie watkins