Trauma Informed Response Suicidal Ideation and SelfInjury Amy
- Slides: 44
Trauma Informed Response: Suicidal Ideation and Self-Injury Amy Budd, IMF HERE Now Bilingual Clinical Coordinator Corey. Ann Friedrich, LCSW HERE Now Lead Mental Health Specialist
HERE Now Helping Engaging Reconnecting Educating • School based suicide prevention and early intervention program serving San Diego County schools grades 7 th through 12 th • Funded through the County of San Diego Behavioral Health Services.
HERE Now School-Based Prevention and Early Intervention Project focuses on: – Preventing suicide by educating youth, their families and the community on the risk factors – Reducing the stigma around seeking help for themselves or others – Working to support the school culture and environment and working with schools existing anti-bullying protocols and initiatives
Presentation Agenda Trauma Informed Care Self Injurious Behaviors Suicidal Ideation Safety Assessment Guide
Trauma Informed Care
What is Trauma? • Definition (NASMHPD, 2006) – Experience of violence and victimization, including: • • • Sexual Abuse Physical Abuse Severe Neglect Loss Domestic Violence Witnessing violence, terrorism or disasters – Trauma and its effects will differ from student to student
Prevalence of Trauma • 90% public mental health clients have been exposed to trauma • Vast majority of students report trauma Assume Trauma Provide Trauma-Informed Care
What is Trauma Informed Care? Trauma Informed Care (TIC) is a collaborative philosophy that acknowledges the impact of one’s life experiences and guides our interactions to promote connection, inspiration, strength, and healing.
TIC as a Philosophy • “What’s wrong with you? ” “What happened to you? ” • Seek to understand experiences Doesn’t excuse behavior, but it explains it • Symptoms (e. g. problem behaviors) – Adaptive coping behaviors & protection – Not pathology
How Does TIC Influence Education? • Safety first • Strengths-based • Collaborative • Holistic-perspective – Not simply modifying behavior
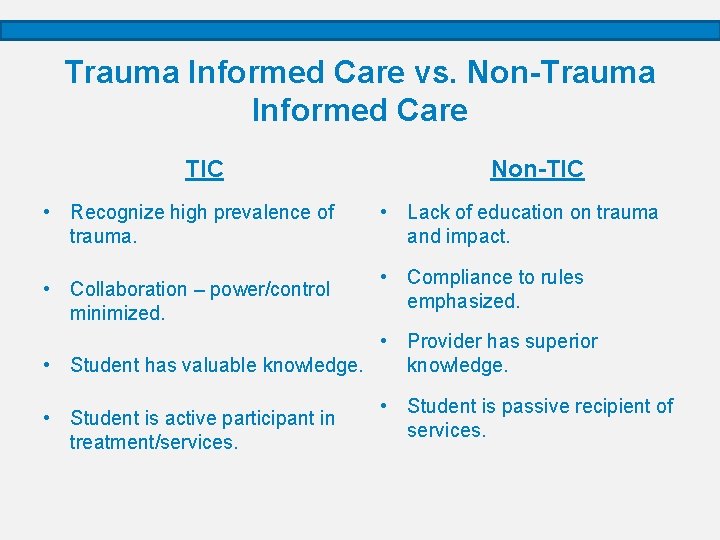
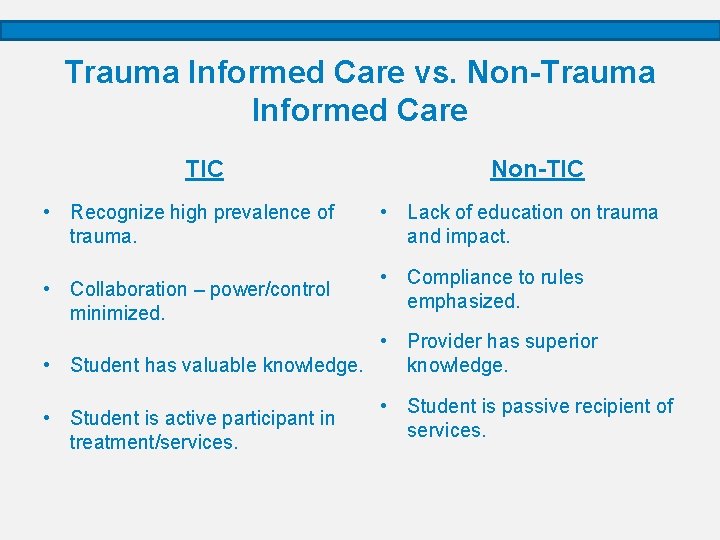
Trauma Informed Care vs. Non-Trauma Informed Care TIC • Recognize high prevalence of trauma. • Collaboration – power/control minimized. Non-TIC • Lack of education on trauma and impact. • Compliance to rules emphasized. • Provider has superior • Student has valuable knowledge. • Student is active participant in treatment/services. • Student is passive recipient of services.
Trauma Informed Education • Importance of connection • Academic success affects mental health – Academic pressure without balance • Mental health affects academic success – Failing grades, lack of participation, low attendance
Self-Injurious Behaviors or Self-Harm
Fact or Fiction? • People who self-injure want to die. – FACT: Those who self-injure do not want to die. When they self-harm, they are NOT trying to kill themselves, but instead are trying to cope with their pain and/or strong emotions associated to trauma. – Trauma informed perspective would tell us self injury may in fact be a way of helping the individual to go on living. However, in the long-term, people who self-injure have a much higher risk of suicide, which is why it’s important to seek help. • People who self-injure only cut their skin on their wrists. – FACT: The most common form of self-injurious behavior is cutting one’s skin. However there are many creative ways students self-injure and many different areas of the body that can be affected. – Trauma informed perspective would remind us to look at the whole person, not just their self-injury i. e. we wouldn’t call a student a “cutter” or expect “cutting” to be the only form of self-injury they could be participating in.
Fact or Fiction? • Self-injury is just a fad. Ignore it and kids will grow out of it. – FICTION: Self-injury should not be minimized or referred to as a “fad”; there is no evidence that individuals spontaneously “grow out of it. ” Self-injury can involves real tissue damage and potential scarring as well as other potentially serious injuries. – Trauma informed perspective would say self-injury is indicative of serious distress that requires assessment and treatment by a mental health professional. • People who self-injure are trying to get attention. – FICTION: People who self-harm generally do so in secret. They are struggling with powerful emotions that are difficult to regulate. Self-injury is a way for the individual to cope with these feelings and should ALWAYS be viewed as a cry for help. – Trauma informed perspective would say, even if the self-injury is for attention, we should ask ourselves “what NEED is not being met? ” What is making an individual go to SUCH an extreme that they feel this is the only way to get support from a trusted adult?
What is Self-Injurious Behavior? • Self-injury refers to the intentional self-infliction of wounds, without the intent to die (Walsh, 2006). – Self-injury can include behaviors such as cutting, burning, hitting, picking, hair pulling, head banging, punching self/object, etc. • Oftentimes individuals who self-harm will frequently engage in the behavior repeatedly and in a secretive manner.
Why does this happen? Teens self-injure for many different reasons: Most are struggling with powerful emotions. Self-injury might seem like the only way to express or interrupt feelings that seem too intense to endure. Disconnection Numb Physical Pain Control Distraction Feeling Addicted Peer Pressure Other Mental Health Conditions Any of these factors may help to explain why a particular teen will self-injure. However, each teen has unique feelings and experiences that play a role. Some who self harm might not be able to explain why they do it.
Warning Signs • A sense of shame and secrecy often goes along with self -injury. Most teens who self-harm hide the marks and if they're noticed, make up excuses about them. – Unexplained wounds, cuts, scars, burns, and/or bruises. • “The cat scratched me”, “I burned myself on the oven. ” – Youth refusing to show their arms or wrists. – Covering of the arms or wrists with bracelets and long sleeves. • General signs of depression, including sadness, isolation and irritability. Note: Some teens don't try to hide cuts and might even call attention to them. This is cry for HELP! Adapted from: Kidshealth. org
What can Staff do to help? • Ask questions - avoid becoming angry or being judgmental. – Great opportunity to use your trauma informed perspective. • Seek additional support from mental health contacts or school administration. • Harm Reduction: this behavior has become the student’s coping mechanism so we must understand what a powerful role it plays in the student’s life and how to help them replace this with a new one. – We cannot take a coping mechanism away without replacing it with a healthy one. • Help your student identify their triggers and or pain associated with the urge to harm themselves. – Student must be aware of situations that are likely to trigger their urge to selfinjure. • Help them make a plan for what they will do instead of self harming when they are faced with their triggers. Adapted from: Kidshealth. org
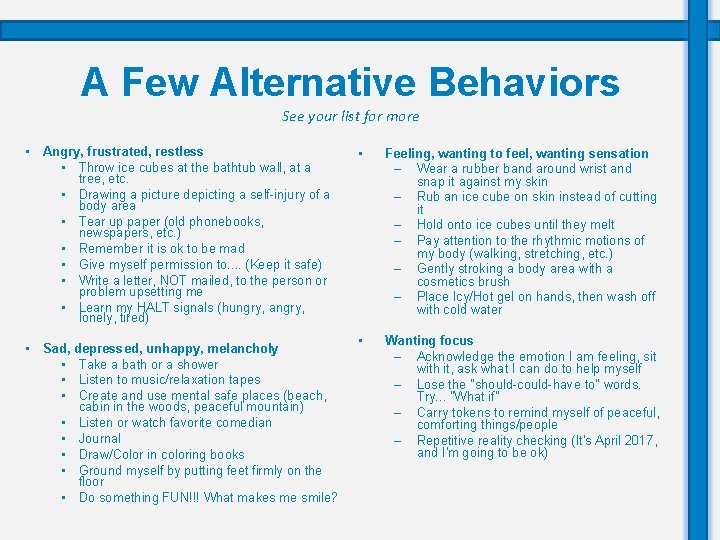
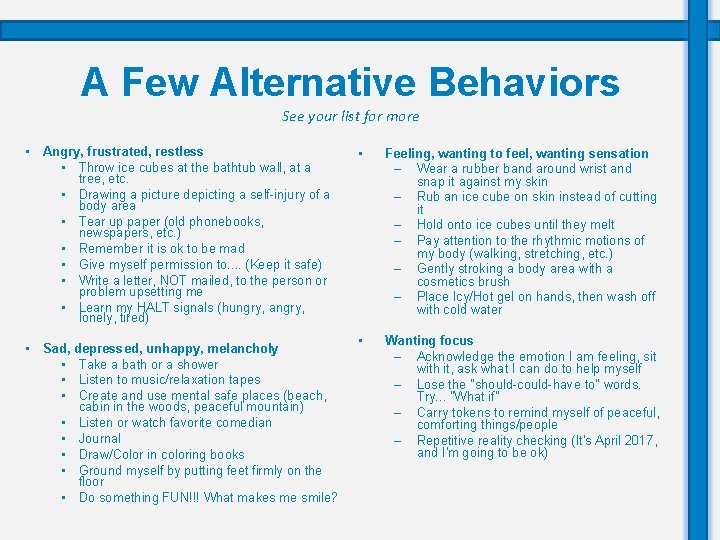
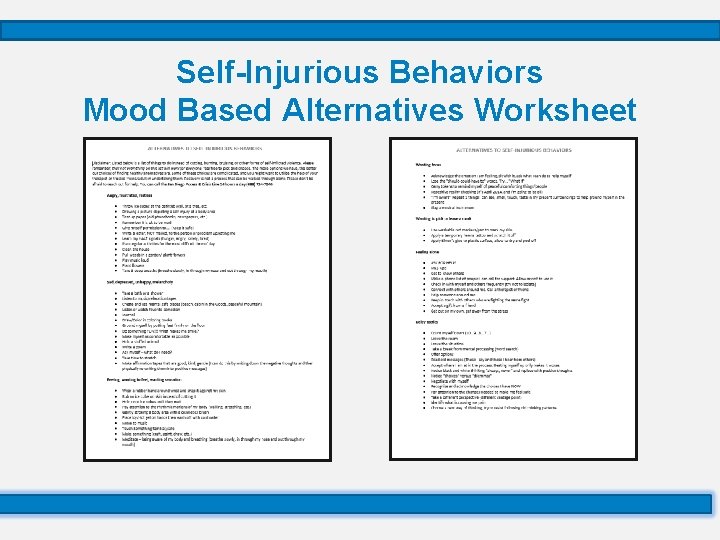
A Few Alternative Behaviors See your list for more • Angry, frustrated, restless • Throw ice cubes at the bathtub wall, at a tree, etc. • Drawing a picture depicting a self-injury of a body area • Tear up paper (old phonebooks, newspapers, etc. ) • Remember it is ok to be mad • Give myself permission to. . (Keep it safe) • Write a letter, NOT mailed, to the person or problem upsetting me • Learn my HALT signals (hungry, angry, lonely, tired) • Sad, depressed, unhappy, melancholy • Take a bath or a shower • Listen to music/relaxation tapes • Create and use mental safe places (beach, cabin in the woods, peaceful mountain) • Listen or watch favorite comedian • Journal • Draw/Color in coloring books • Ground myself by putting feet firmly on the floor • Do something FUN!!! What makes me smile? • Feeling, wanting to feel, wanting sensation – Wear a rubber band around wrist and snap it against my skin – Rub an ice cube on skin instead of cutting it – Hold onto ice cubes until they melt – Pay attention to the rhythmic motions of my body (walking, stretching, etc. ) – Gently stroking a body area with a cosmetics brush – Place Icy/Hot gel on hands, then wash off with cold water • Wanting focus – Acknowledge the emotion I am feeling, sit with it, ask what I can do to help myself – Lose the "should-could-have to" words. Try. . . "What if" – Carry tokens to remind myself of peaceful, comforting things/people – Repetitive reality checking (It's April 2017, and I'm going to be ok)
Suicidal Ideation
What does it mean when a child or teen is suicidal? • A student who is feeling suicidal is considering taking, or planning to take, their own life. • In many cases, young people who consider or attempt suicide do not really want to die: – Instead, they want to escape their pain and problems, but can’t see a way out or imagine things getting better. – Often a suicide attempt is a “cry for help” from a student who doesn’t know where to turn.
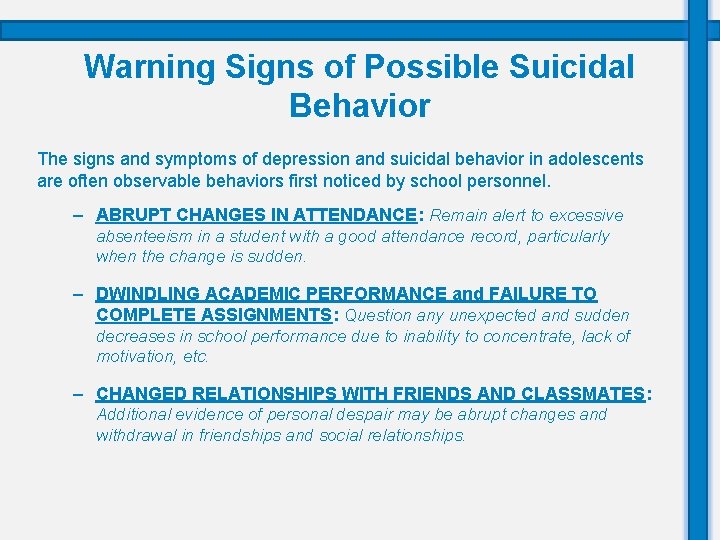
Warning Signs of Possible Suicidal Behavior The signs and symptoms of depression and suicidal behavior in adolescents are often observable behaviors first noticed by school personnel. – ABRUPT CHANGES IN ATTENDANCE: Remain alert to excessive absenteeism in a student with a good attendance record, particularly when the change is sudden. – DWINDLING ACADEMIC PERFORMANCE and FAILURE TO COMPLETE ASSIGNMENTS: Question any unexpected and sudden decreases in school performance due to inability to concentrate, lack of motivation, etc. – CHANGED RELATIONSHIPS WITH FRIENDS AND CLASSMATES: Additional evidence of personal despair may be abrupt changes and withdrawal in friendships and social relationships.
Warning Signs of Possible Suicidal Behavior – LACK OF INTEREST IN ACTIVITES AND SURROUNDINGS: One of the first signs of a potentially suicidal adolescent is general withdrawal, disengagement and apathy. – INCREASED IRRITABIITY, MOODINESS OR AGGRESSIVENESS: Depressed, stressed and potentially suicidal individuals demonstrate wide mood swings and unexpected displays of emotion. – DEATH AND SUICIDAL THEMES EVIDENT IN READING SELECTIONS AND WRITTEN ESSAYS: The selection of material centering on ideas about death or dying, the uselessness or worthlessness of life, or matters relating to persons. – PARTICIPATING IN SELF INJURY: Students who participate in self injury may not necessarily want to die. However, in the long-term, people who self-injure have a much higher risk of suicide, which is why it’s important to seek help.
Urgent Warning Signs • Saying phrases that include: – “I want to kill myself – “I want to die” – “I just want to disappear/sleep forever” • Making threats or statements: – “Don’t worry, I won’t be a problem much longer” – “If anything happens to me, I just want you to know…” • Giving away or discarding favorite possessions • Writing a suicide note • Attempting to obtain a firearm, knife or rope • Obtaining, or attempting to obtain, large quantities of medication
What is NOT helpful when working with a student who might be suicidal: • Ignoring or dismissing the issue: This sends the message that you don’t hear their message, don’t believe them, don’t take them serious or you don’t care about their pain. • Acting shocked or embarrassed • Panicking, preaching, or patronizing • Challenging, debating, or bargaining: Never challenge a suicidal person. You can’t win in a power struggle with someone who may not be thinking clearly. • Promising to keep a secret: The suicidal person is sharing his/her feelings hoping that someone will recognize the pain and help, even though they may verbally contradict this.
What is helpful: Trauma informed lens • Acknowledge: Acknowledge that you are seeing signs of depression or suicide in a student and that it is serious. – Be direct, specific, caring, and non-confrontational. – Ask the question – “Are you thinking about suicide? ” • If yes, have you thought about HOW you would do it? • If yes, do you have WHAT you need to do it? • If yes, have you thought about WHEN you would do it? • Care: Let the student know you care about them and you can help. – Listen carefully – Be genuine – “I’m concerned about you… about how you feel. ” • Tell: Follow your school protocol and tell the mental health contact. – Get help – Do NOT leave him/her alone – “You are not alone. I will help you get the support you need. ”
Safety Assessment Guide
Self-Injurious Behaviors: Questions to Ask • Have you ever used self-harm as a coping skill? – Additional ways to ask: • Have you ever hurt yourself on purpose because you were mad or upset? • Have you ever used an un-safe coping skill? • If yes, – How did you harm yourself and where on your body (if applicable) did it occur? – What did you use? – When was the last time you self-injured? – How long/often have you been in self-injuring? – Are any adults aware?
Self-Injury: Low Risk vs. High Risk Assessment • Language being used by student: “I want to have control”, “I wanted to be numb”, “I wanted to feel”, “takes focus away from everything else”, etc. • Low Risk Assessment – Student categorized as low risk if: • • Student has no history self injury Has thoughts about self injuring but has not identified a specific plan to harm self Does not have the means and intent to harm self Student has tried self-injury and has not found it to be helpful • High Risk Assessment – Student categorized as high risk if: • • They have a history of self-injury Extreme forms of self-injury or scarring Indifferent about the intent (coping skill versus ending their life) They have a history of related hospitalizations/ suicidal ideation/ attempts
Self-Injury: Intervention • Safety planning – Collaborate with student by making a plan for what they will do instead of self-harming when faced with their triggers. – Help your student identify their triggers and/or pain associated with the urge to harm themselves. • Student must be aware of situations that are likely to trigger their urge to self-injure. • Harm Reduction: Strategies and beliefs aimed at reducing and/or preventing negative consequences to unsafe behaviors or coping skills – This behavior plays a powerful role in the student’s life, demonstrating just how important it is to help them find those replacements. • We cannot take a coping mechanism away without replacing it with a healthy and safe one. Note: If you are unclear about the intent behind the self-injury it maybe necessary to assess for suicidal ideation. Adapted from: Kidshealth. org
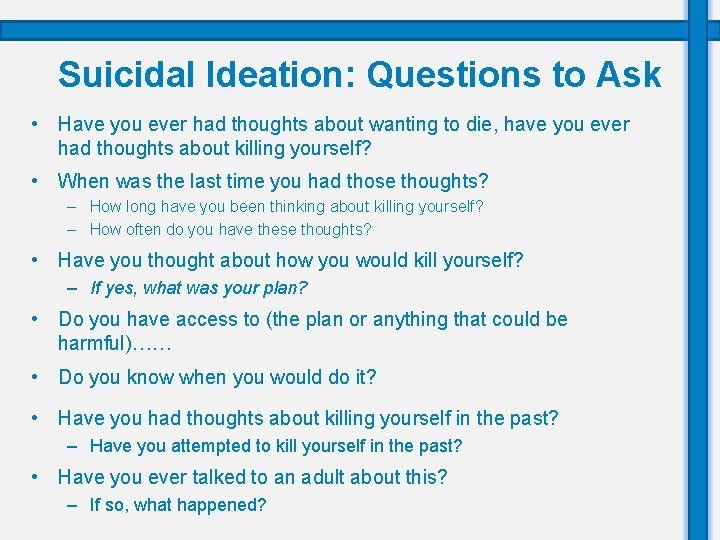
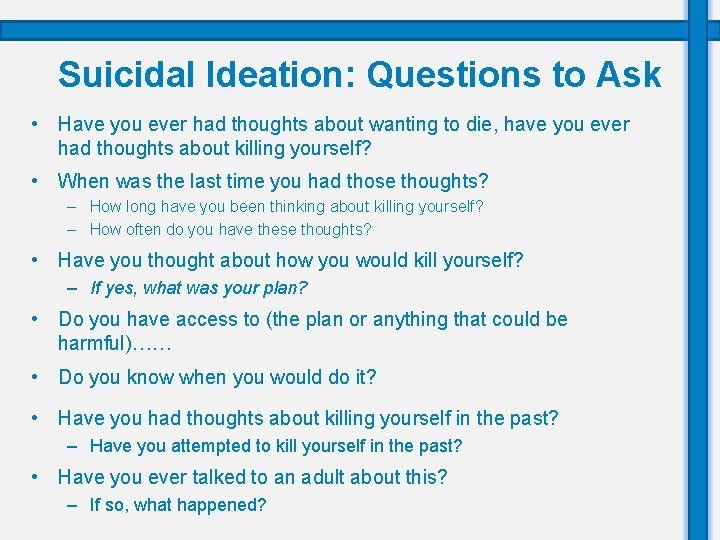
Suicidal Ideation: Questions to Ask • Have you ever had thoughts about wanting to die, have you ever had thoughts about killing yourself? • When was the last time you had those thoughts? – How long have you been thinking about killing yourself? – How often do you have these thoughts? • Have you thought about how you would kill yourself? – If yes, what was your plan? • Do you have access to (the plan or anything that could be harmful)…… • Do you know when you would do it? • Have you had thoughts about killing yourself in the past? – Have you attempted to kill yourself in the past? • Have you ever talked to an adult about this? – If so, what happened?
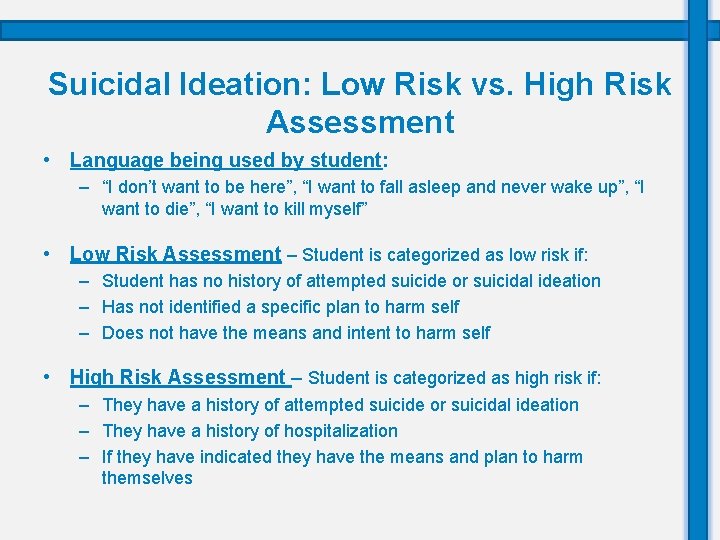
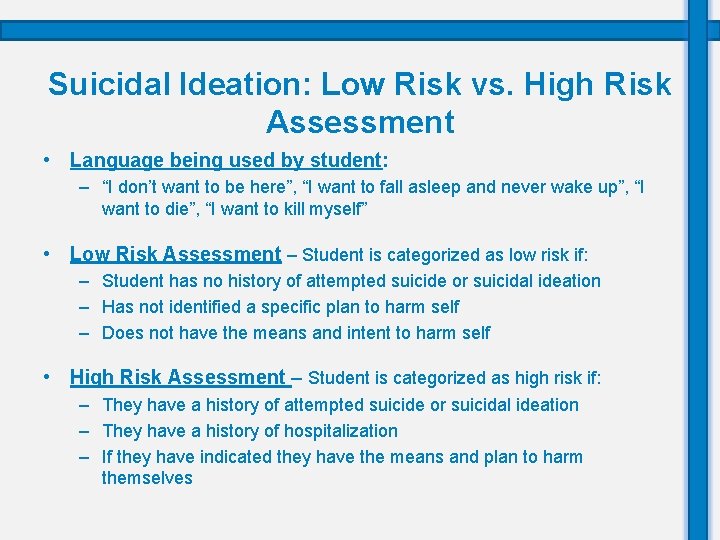
Suicidal Ideation: Low Risk vs. High Risk Assessment • Language being used by student: – “I don’t want to be here”, “I want to fall asleep and never wake up”, “I want to die”, “I want to kill myself” • Low Risk Assessment – Student is categorized as low risk if: – Student has no history of attempted suicide or suicidal ideation – Has not identified a specific plan to harm self – Does not have the means and intent to harm self • High Risk Assessment – Student is categorized as high risk if: – They have a history of attempted suicide or suicidal ideation – They have a history of hospitalization – If they have indicated they have the means and plan to harm themselves
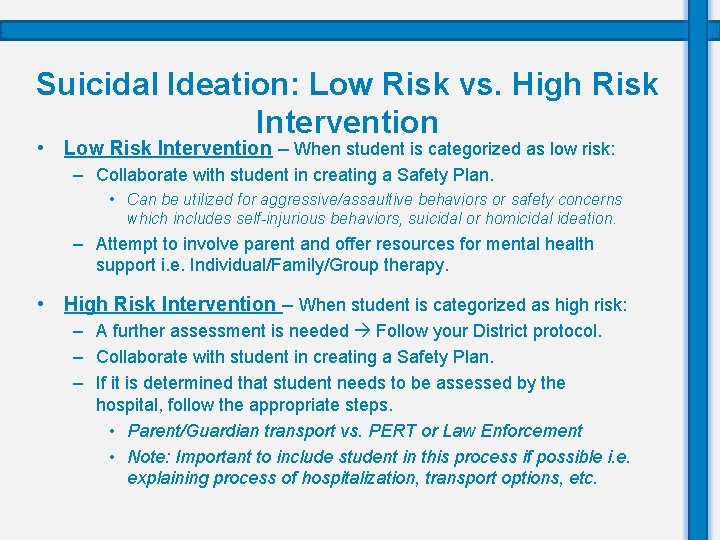
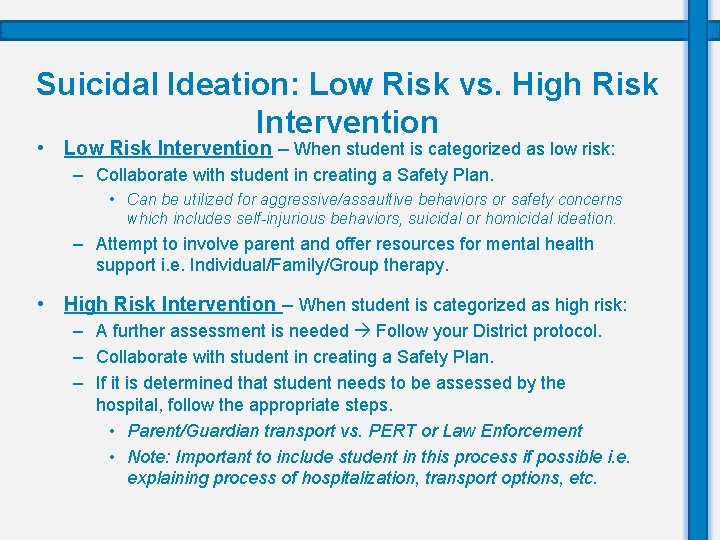
Suicidal Ideation: Low Risk vs. High Risk Intervention • Low Risk Intervention – When student is categorized as low risk: – Collaborate with student in creating a Safety Plan. • Can be utilized for aggressive/assaultive behaviors or safety concerns which includes self-injurious behaviors, suicidal or homicidal ideation. – Attempt to involve parent and offer resources for mental health support i. e. Individual/Family/Group therapy. • High Risk Intervention – When student is categorized as high risk: – A further assessment is needed Follow your District protocol. – Collaborate with student in creating a Safety Plan. – If it is determined that student needs to be assessed by the hospital, follow the appropriate steps. • Parent/Guardian transport vs. PERT or Law Enforcement • Note: Important to include student in this process if possible i. e. explaining process of hospitalization, transport options, etc.
Safety Assessment: Additional Resources Scaling Questions Safety Plan Self-Injurious Behaviors Mood Based Alternatives Worksheet Strengths and Coping Skills Worksheet
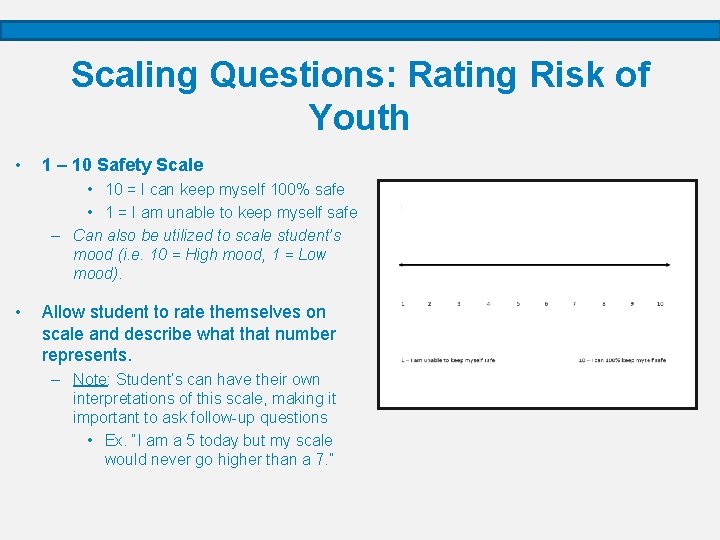
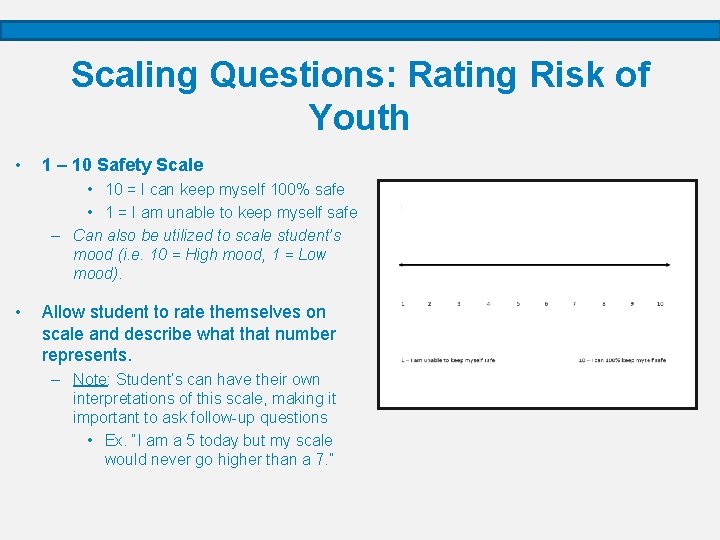
Scaling Questions: Rating Risk of Youth • 1 – 10 Safety Scale • 10 = I can keep myself 100% safe • 1 = I am unable to keep myself safe – Can also be utilized to scale student’s mood (i. e. 10 = High mood, 1 = Low mood). • Allow student to rate themselves on scale and describe what that number represents. – Note: Student’s can have their own interpretations of this scale, making it important to ask follow-up questions • Ex. “I am a 5 today but my scale would never go higher than a 7. ”
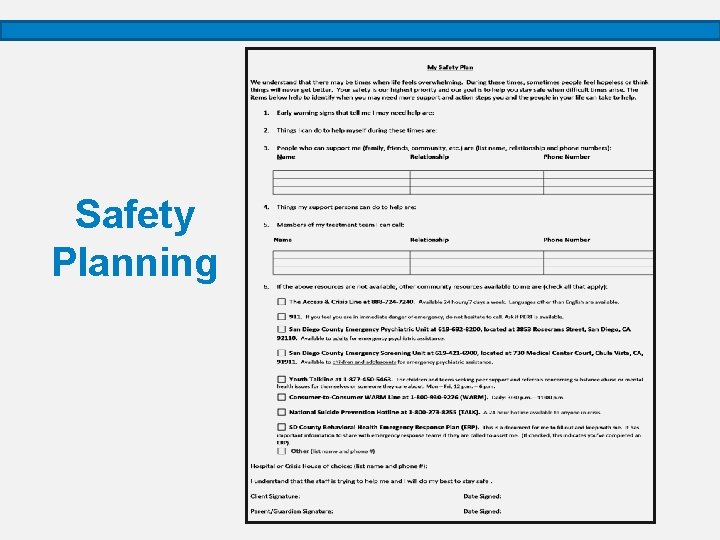
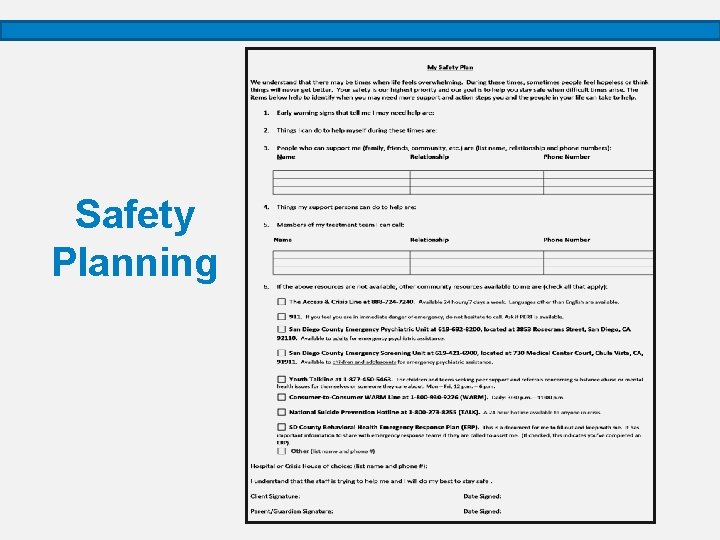
Safety Planning
When to make a Safety Plan • A safety plan can be used for almost any concerning behavior. – For example: you can use for aggressive or assaultive behaviors, safety concerns which includes self injurious behaviors, suicidal ideation, or homicidal ideation, bullying/school safety concerns, etc. – Think of safety plan as another tool in your tool box! – If completing a safety plan with a student and a parent/guardian is not involved it is very important to contact them to inform them of the plan, they may be additional support.
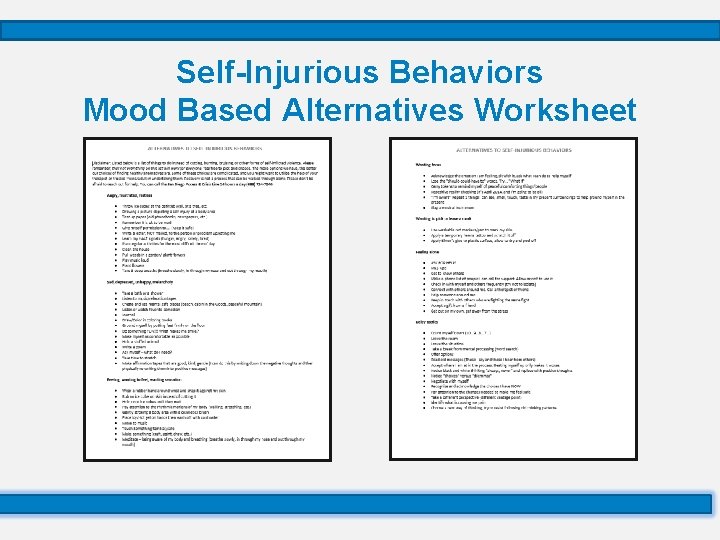
Self-Injurious Behaviors Mood Based Alternatives Worksheet
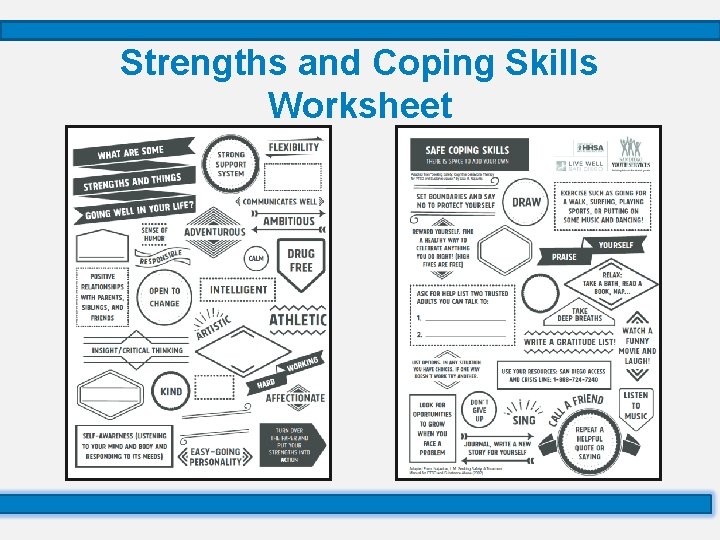
Strengths and Coping Skills Worksheet
Remember: Take Care of Yourself • You don’t need to be the expert or have all the answers! • Give yourself permission to be human. Its normal to feel anxiety or other difficult feelings. Be trauma informed with yourself. • Avoid over-involvement; it takes a team of people to help a suicidal individual. • Talk to a supportive person beforehand debrief afterwards. • Recognize that you are not responsible for another person’s choice to end their life. • Take care of yourself and practice your own safe coping skills!
Where to Get Help • San Diego Access and Crisis Line – 1 -888 -7240 – Live chat –www. Up 2 SD. org – ALL languages • Other Resources: – National Suicide Prevention Hotline: 1 -800 -273 -TALK (8255) – 211 ( San Diego non emergency resource line) http: //www. 211 sandiego. org/ – My 3 App –To create Safety Plans (Android & IPhone) – TREVOR PROJECT: LGBTQI RESOURCE 1 -866 -488 -7386 http: //www. thetrevorproject. org • Mental Health Emergencies: – Call 911 and ask for PERT Team (Psychiatric Emergency Response Team).
Questions & Discussion