What do you need informed care trauma informed

- Slides: 47
What do you need informed care & trauma informed care in 2017? Diane K. Whitney MD, FRCPC, BCETS Assistant Professor NOSM, University of Toronto & Adjunct Professor Western University Community Based Practice Thunder Bay
Disclosure Slide – Slide 1 �Speaker: Diane K. Whitney MD, FRCPC, BCETS �Relationship with commercial interests: � Grant / Research Support: None � Speaker Bureau / Honoraria: Sunovion, Eli Lilly, Shire � Consulting Fee: None � Other: None
Disclosure Slide – Slide 2 �This program has received financial support from no organization. �This program has received in-kind support from in the form of no organization. �Potential for conflict(s) of interest: �Dr. Whitney will be speaking regarding medication used for PTSD treatment and where appropriate she will indicate if it is off-label use.
Learning Objectives: At the end of this presentation, participants will be able to: 1. Understand trauma informed care and how it is relevant to your practice setting. 2. Understand what is new in trauma treatment 3. Relevance of trauma diagnosis for responders & military veterans 4. Apply this to case vignettes – you referred!
Trauma Informed Care • What you need to know –Impact on Physical & Mental Health • ACE Study –www. acestudy. org • A Standard for Practice / Settings
Psychiatric Patients & Abuse �At least 70% of psychiatric patients have a history of some type of abuse �Sexual abuse is common-30 to 40% of women and 15% of men in general population �Verbal abuse particularly “put downs” have a particular negative impact �Trauma has negative impact on personal, social & emotional development & self image i. e. developmental trauma
ACE STUDY How stressful or traumatic experiences during childhood effect adult health
ACE Study -Introduction �Adverse Childhood Experiences (ACE) Study �To find how stressful or traumatic experiences during childhood affect adult health �Clear relationship between ACES Score with poor physical & mental health as well as premature death in adults �Linked to increased suicide attempts & depression �Relevant to North Western Ontario
ACE Study �Adverse Childhood Experiences (ACE) Study involving 17, 000 Kaiser Permanente patients from routine health surveys �To find how stressful or traumatic experiences during childhood affect adult health �Cumulative score related to adverse childhood event scale �Clear relationship between ACES Score with poor physical & mental health as well as premature death in adults
ACE SCORES � 63% of study participants had at least one category of childhood trauma & over 20% had 3 or more categories �ACE events tend to cluster together �Obesity used as shield against unwanted sexual attention or form of defense against physical attack �Many had been sexually &/or physically abused as children
ACE SCORES �See questions �You might be surprised by the scores of some of your patients �Caution about using scale as handout
ACE Study: Depression & Suicide �ACE score at least 7 increased suicide attempts: �Child/adolescent suicide attempts by 51 fold �Adult suicide attempts by 30 fold �Emotional abuse exhibited the strongest relationship to depressive symptoms in men & women �“Names do hurt”
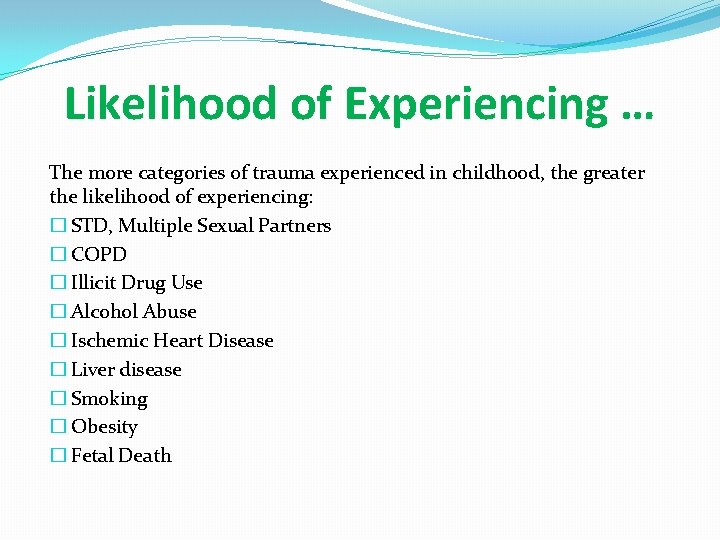
Likelihood of Experiencing … The more categories of trauma experienced in childhood, the greater the likelihood of experiencing: � STD, Multiple Sexual Partners � COPD � Illicit Drug Use � Alcohol Abuse � Ischemic Heart Disease � Liver disease � Smoking � Obesity � Fetal Death
Trauma Informed Care What does it really mean? ?
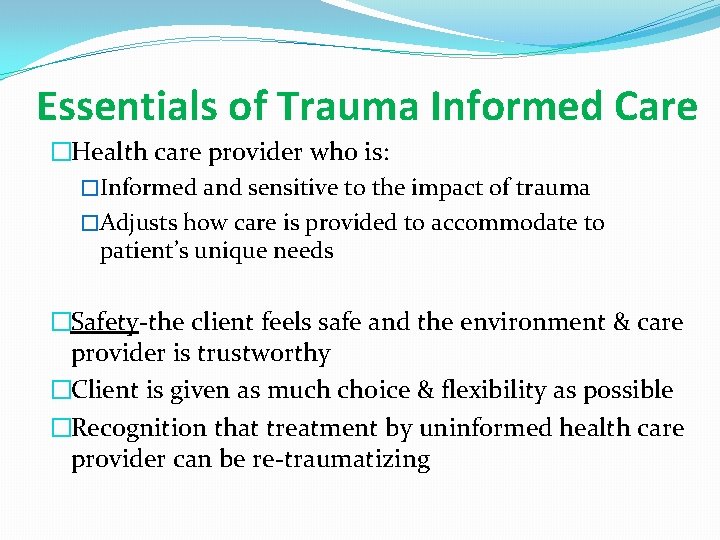
Essentials of Trauma Informed Care �Health care provider who is: �Informed and sensitive to the impact of trauma �Adjusts how care is provided to accommodate to patient’s unique needs �Safety-the client feels safe and the environment & care provider is trustworthy �Client is given as much choice & flexibility as possible �Recognition that treatment by uninformed health care provider can be re-traumatizing
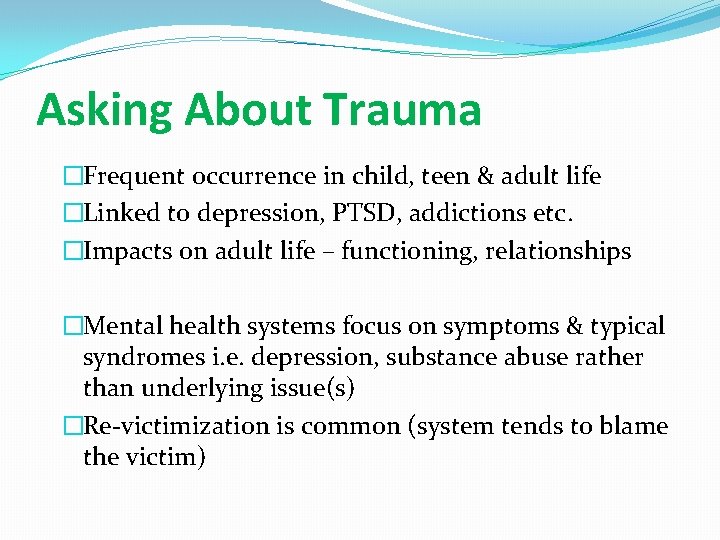
Asking About Trauma �Frequent occurrence in child, teen & adult life �Linked to depression, PTSD, addictions etc. �Impacts on adult life – functioning, relationships �Mental health systems focus on symptoms & typical syndromes i. e. depression, substance abuse rather than underlying issue(s) �Re-victimization is common (system tends to blame the victim)
Interactions with Health Care Providers �Distrust of authority figure �Fear on being abused �Fear of judgement �Need to feel “in control” �Disconnection from body �Conditioning to be passive �Feeling unworthy �Shame
Your Responsibilities �Asking the question(s) in a responsible manner �Containing the content & the emotion � Preventing “barfing on the carpet” � Acknowledging usual emotions-shame, sadness, anger & client’s strengths �Focusing on the impact of the trauma � Relationships � Emotions � Beliefs � Self Image, Self Perception �Spread discovery over time
Application in Your Environment �What are the defined guidelines / expectations for behaviour? � Safety, honesty, participation in treatment � Patient responsibility in recovery is key �Staff creating safety in treatment environment �Patients / family members not respecting safety i. e. threatening. What do you do? �What about patients who may disrupt safety environment for others?
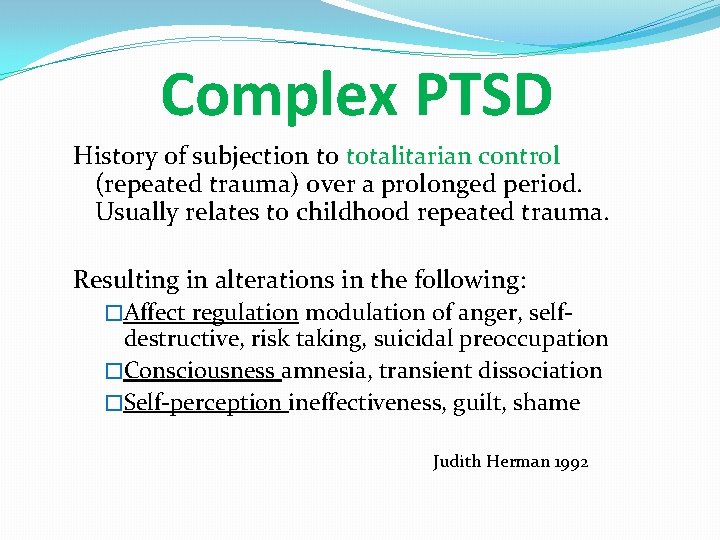
Complex PTSD Concept of Judith Herman
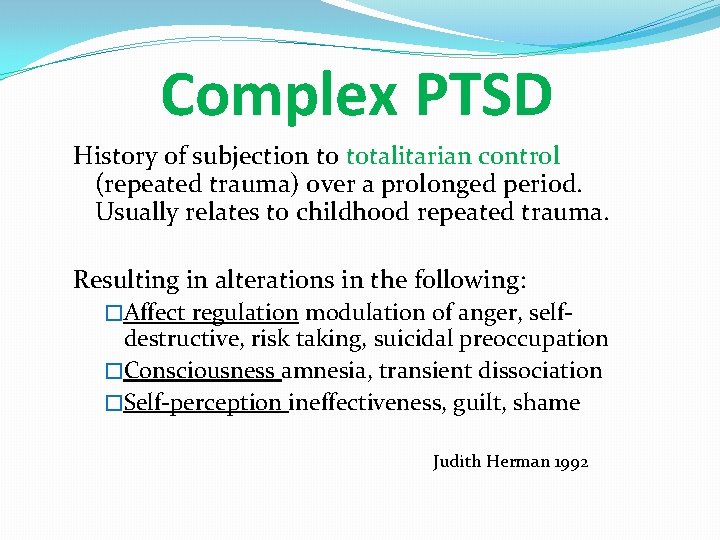
Complex PTSD History of subjection to totalitarian control (repeated trauma) over a prolonged period. Usually relates to childhood repeated trauma. Resulting in alterations in the following: �Affect regulation modulation of anger, self- destructive, risk taking, suicidal preoccupation �Consciousness amnesia, transient dissociation �Self-perception ineffectiveness, guilt, shame Judith Herman 1992
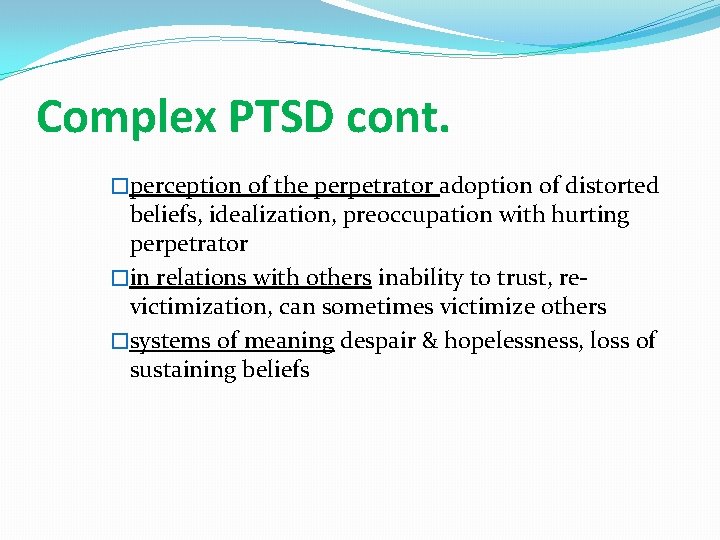
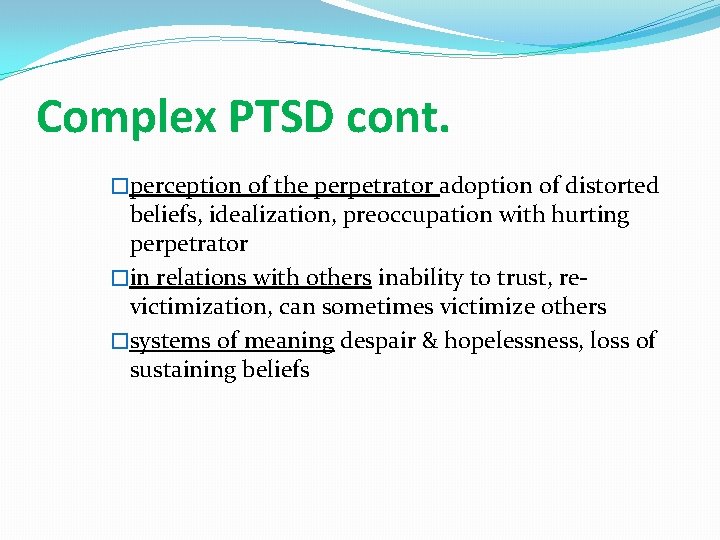
Complex PTSD cont. �perception of the perpetrator adoption of distorted beliefs, idealization, preoccupation with hurting perpetrator �in relations with others inability to trust, revictimization, can sometimes victimize others �systems of meaning despair & hopelessness, loss of sustaining beliefs
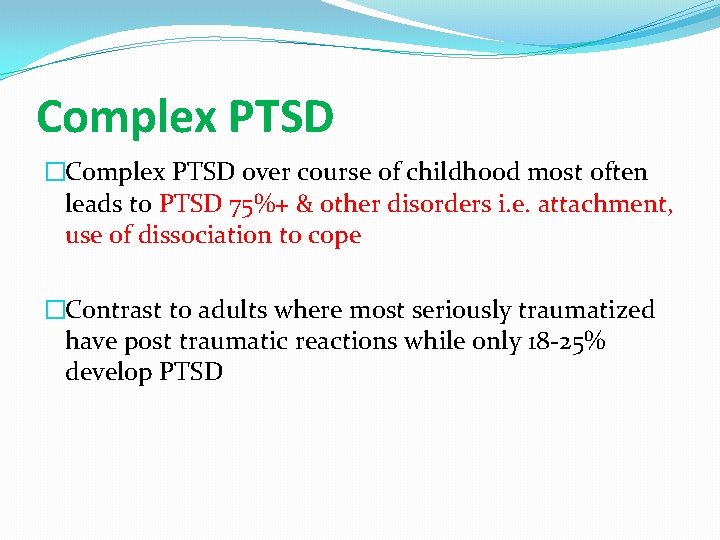
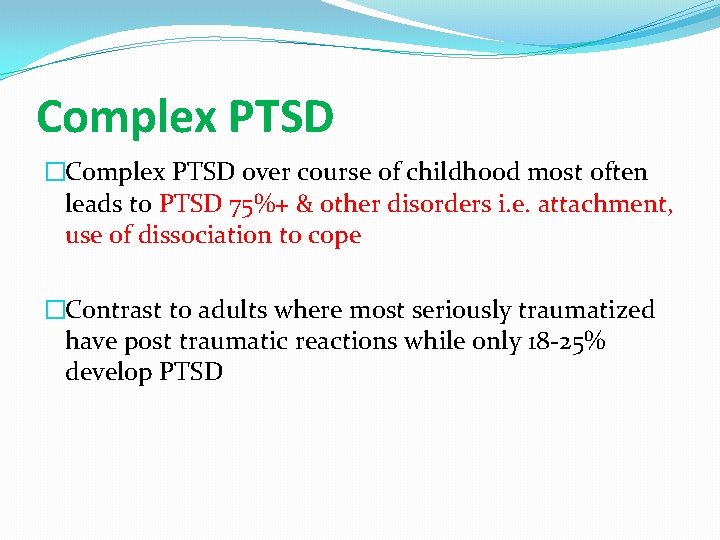
Complex PTSD �Complex PTSD over course of childhood most often leads to PTSD 75%+ & other disorders i. e. attachment, use of dissociation to cope �Contrast to adults where most seriously traumatized have post traumatic reactions while only 18 -25% develop PTSD
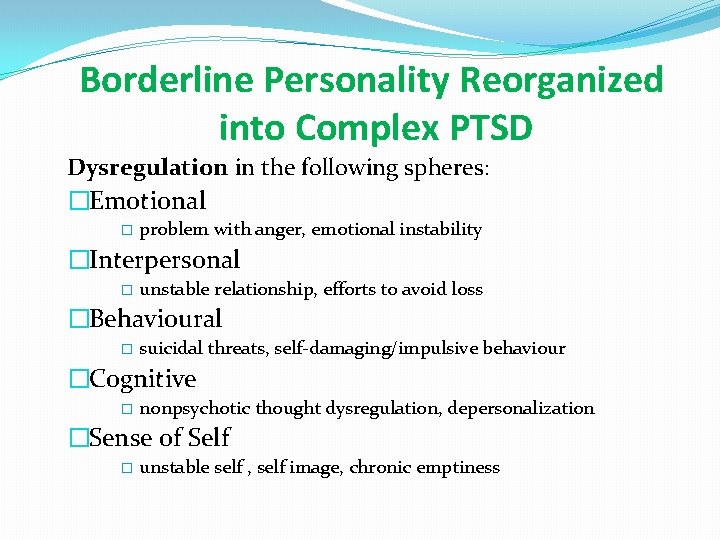
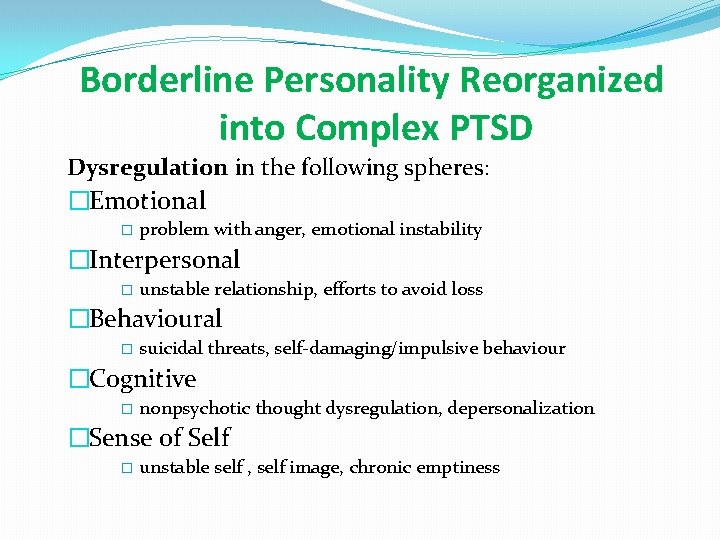
Borderline Personality Reorganized into Complex PTSD Dysregulation in the following spheres: �Emotional � problem with anger, emotional instability �Interpersonal � unstable relationship, efforts to avoid loss �Behavioural � suicidal threats, self-damaging/impulsive behaviour �Cognitive � nonpsychotic thought dysregulation, depersonalization �Sense of Self � unstable self , self image, chronic emptiness
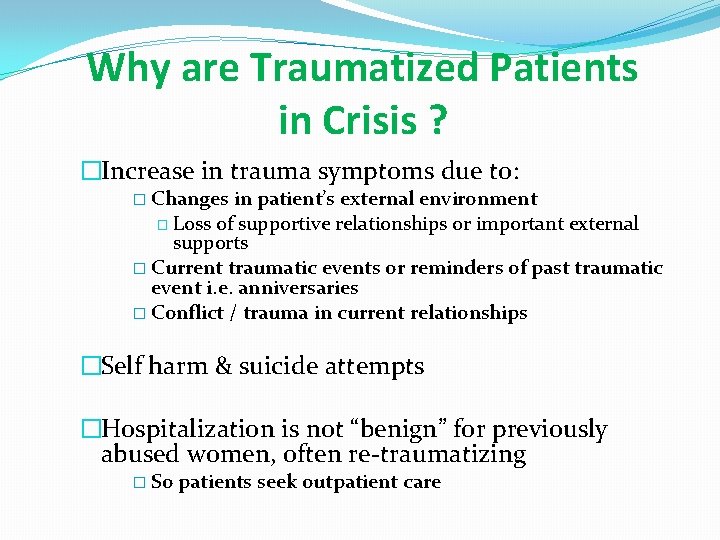
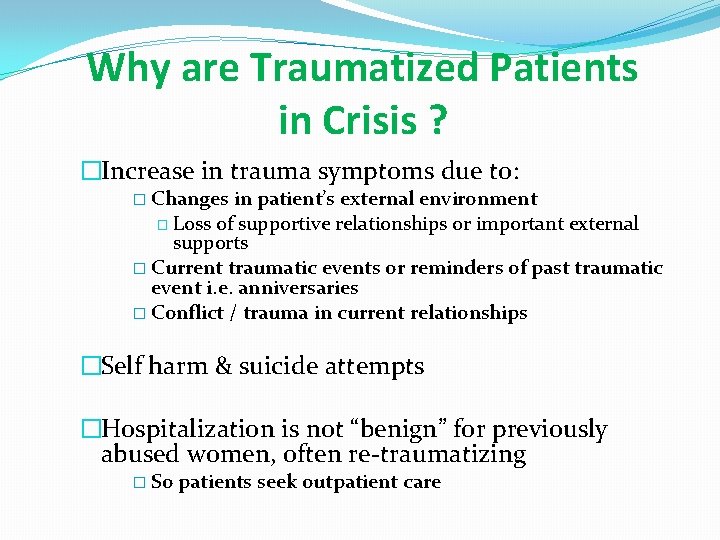
Why are Traumatized Patients in Crisis ? �Increase in trauma symptoms due to: � Changes in patient’s external environment � Loss of supportive relationships or important external supports � Current traumatic events or reminders of past traumatic event i. e. anniversaries � Conflict / trauma in current relationships �Self harm & suicide attempts �Hospitalization is not “benign” for previously abused women, often re-traumatizing � So patients seek outpatient care
Present versus Past Focus • What should treatment focus on? • Risks & Benefits of each focus
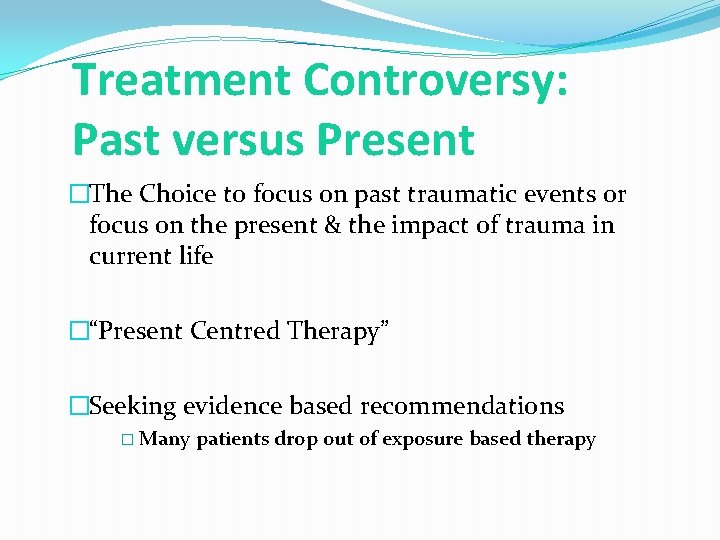
Treatment Controversy: Past versus Present �The Choice to focus on past traumatic events or focus on the present & the impact of trauma in current life �“Present Centred Therapy” �Seeking evidence based recommendations � Many patients drop out of exposure based therapy
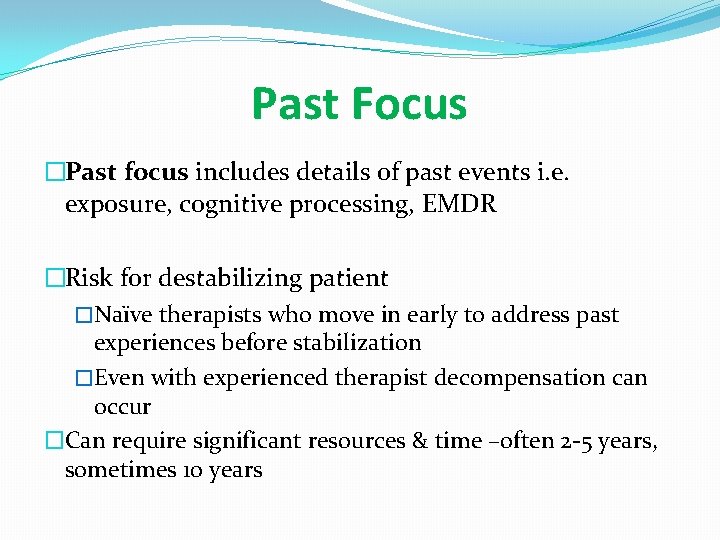
Past Focus �Past focus includes details of past events i. e. exposure, cognitive processing, EMDR �Risk for destabilizing patient �Naïve therapists who move in early to address past experiences before stabilization �Even with experienced therapist decompensation can occur �Can require significant resources & time –often 2 -5 years, sometimes 10 years
Present Focus �Present-centred perspective focuses on altering present maladaptive relationship patterns, providing psychoeducation on client’s current life, teaching use of problem-solving strategies �Minimize maladaptive coping strategies such as substance abuse, poor partner choices etc. �Focus on positive coping strategies �Group interventions for education & coping
Implications for Primary Care �Focus should be on understanding trauma & its consequences on current life �Function & recovery should be the focus �Be cautious on over emphasizing recall & reprocessing past events �Be cautious on “putting patients off work” to deal with trauma –ongoing recovery
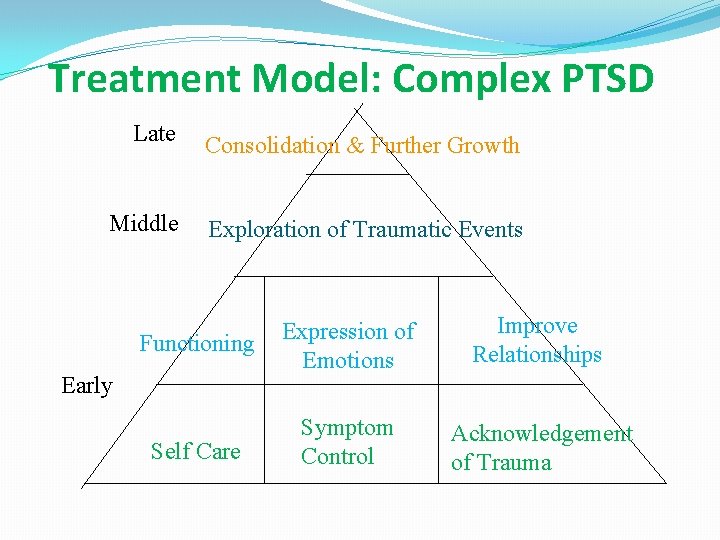
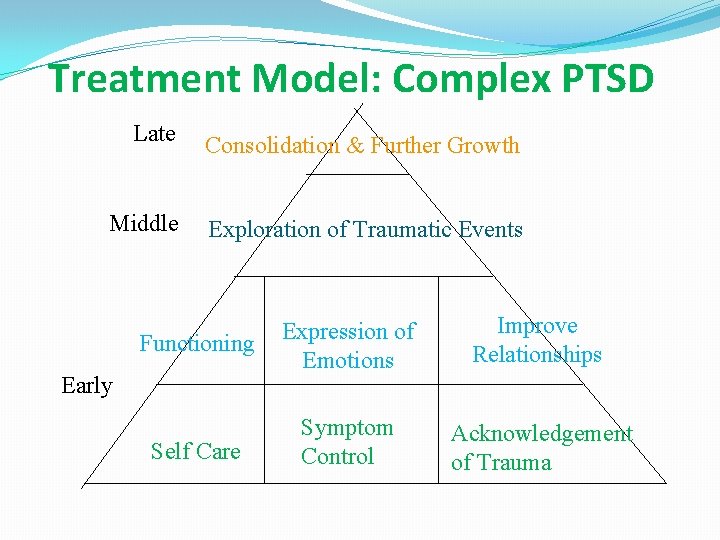
Treatment Model: Complex PTSD Late Middle Consolidation & Further Growth Exploration of Traumatic Events Functioning Expression of Emotions Improve Relationships Self Care Symptom Control Acknowledgement of Trauma Early
Self Care �Self destructive & dysfunctional behaviours need to be reframed � attempt at coping, self protective & healing efforts �Self Soothing & Relaxation Techniques to manage hyperarousal & intrusive symptoms � Mindfulness � Distress Tolerance Skills (Linehan) � distract, self soothe with senses, improve the moment
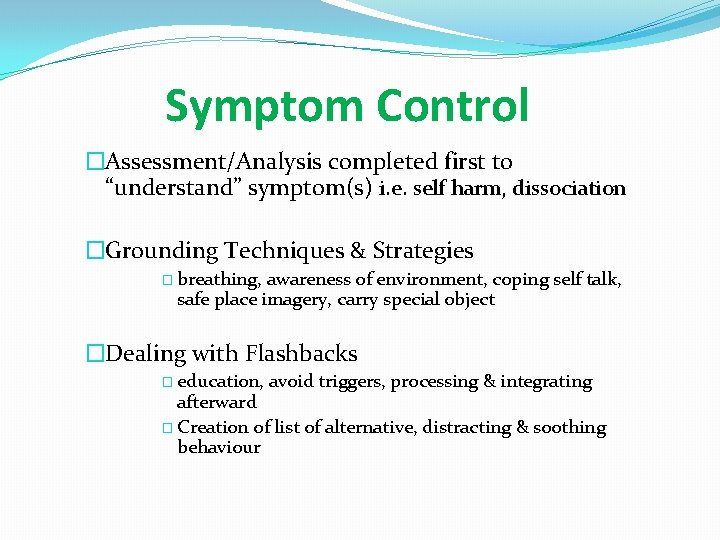
Symptom Control �Assessment/Analysis completed first to “understand” symptom(s) i. e. self harm, dissociation �Grounding Techniques & Strategies � breathing, awareness of environment, coping self talk, safe place imagery, carry special object �Dealing with Flashbacks � education, avoid triggers, processing & integrating afterward � Creation of list of alternative, distracting & soothing behaviour
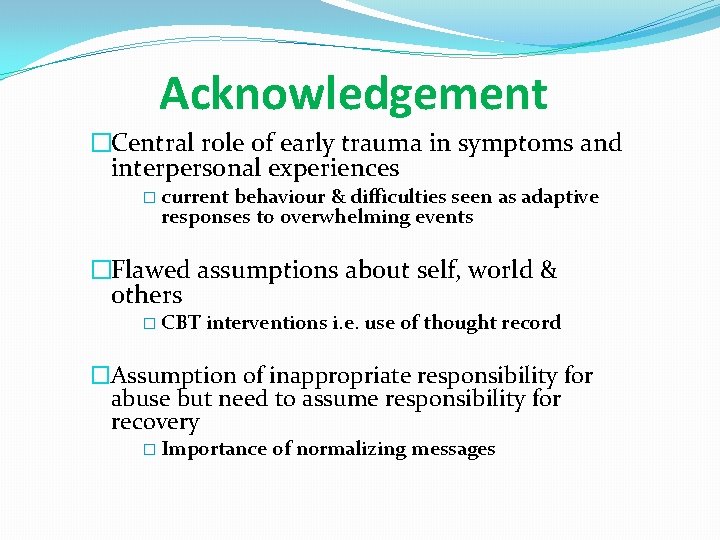
Acknowledgement �Central role of early trauma in symptoms and interpersonal experiences � current behaviour & difficulties seen as adaptive responses to overwhelming events �Flawed assumptions about self, world & others � CBT interventions i. e. use of thought record �Assumption of inappropriate responsibility for abuse but need to assume responsibility for recovery � Importance of normalizing messages
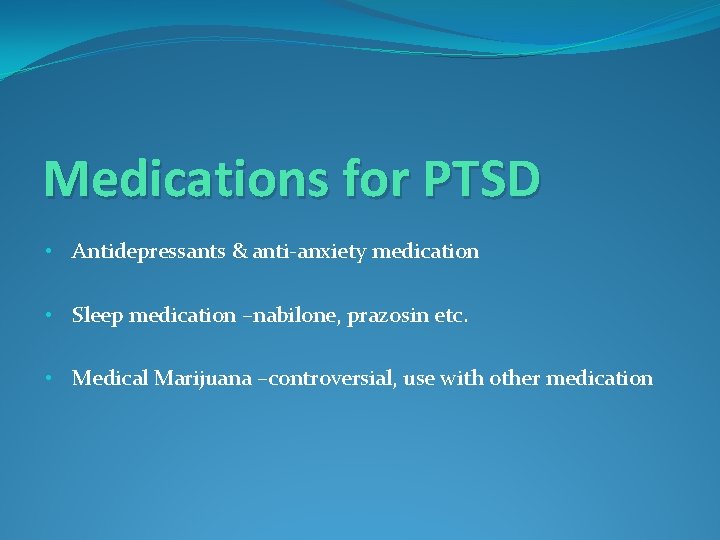
Medications for PTSD • Antidepressants & anti-anxiety medication • Sleep medication –nabilone, prazosin etc. • Medical Marijuana –controversial, use with other medication
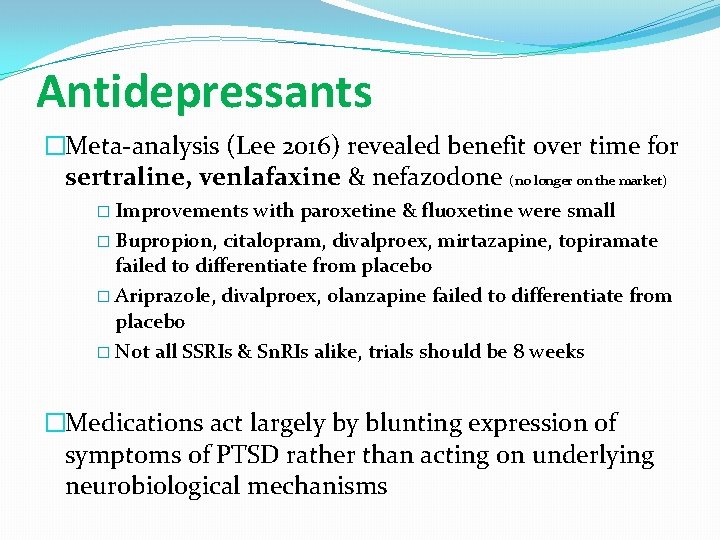
Antidepressants �Meta-analysis (Lee 2016) revealed benefit over time for sertraline, venlafaxine & nefazodone (no longer on the market) � Improvements with paroxetine & fluoxetine were small � Bupropion, citalopram, divalproex, mirtazapine, topiramate failed to differentiate from placebo � Ariprazole, divalproex, olanzapine failed to differentiate from placebo � Not all SSRIs & Sn. RIs alike, trials should be 8 weeks �Medications act largely by blunting expression of symptoms of PTSD rather than acting on underlying neurobiological mechanisms
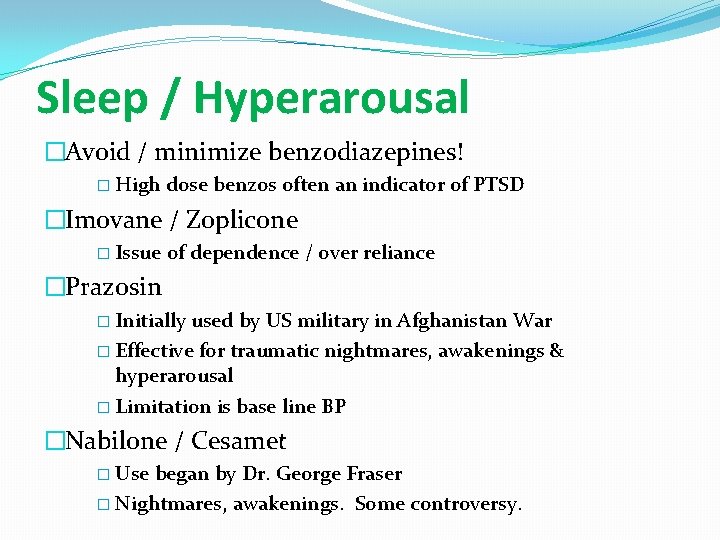
Sleep / Hyperarousal �Avoid / minimize benzodiazepines! � High dose benzos often an indicator of PTSD �Imovane / Zoplicone � Issue of dependence / over reliance �Prazosin � Initially used by US military in Afghanistan War � Effective for traumatic nightmares, awakenings & hyperarousal � Limitation is base line BP �Nabilone / Cesamet � Use began by Dr. George Fraser � Nightmares, awakenings. Some controversy.
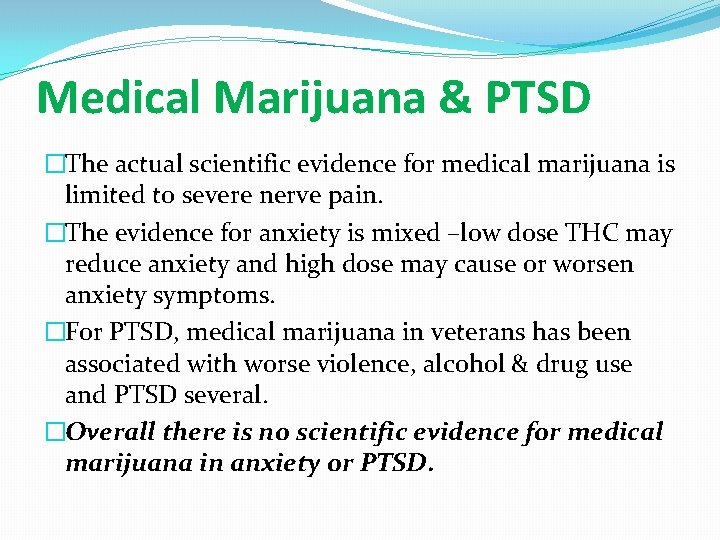
Medical Marijuana & PTSD �The actual scientific evidence for medical marijuana is limited to severe nerve pain. �The evidence for anxiety is mixed –low dose THC may reduce anxiety and high dose may cause or worsen anxiety symptoms. �For PTSD, medical marijuana in veterans has been associated with worse violence, alcohol & drug use and PTSD several. �Overall there is no scientific evidence for medical marijuana in anxiety or PTSD.

st 1 Responders & PTSD
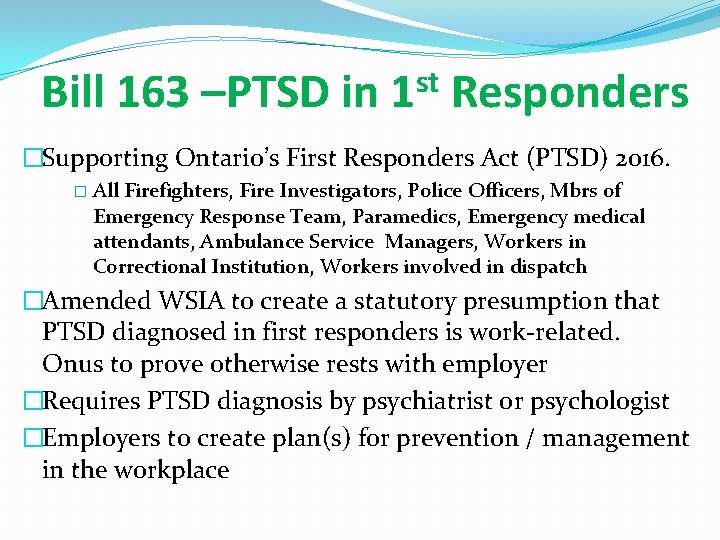
Bill 163 –PTSD in 1 st Responders �Supporting Ontario’s First Responders Act (PTSD) 2016. � All Firefighters, Fire Investigators, Police Officers, Mbrs of Emergency Response Team, Paramedics, Emergency medical attendants, Ambulance Service Managers, Workers in Correctional Institution, Workers involved in dispatch �Amended WSIA to create a statutory presumption that PTSD diagnosed in first responders is work-related. Onus to prove otherwise rests with employer �Requires PTSD diagnosis by psychiatrist or psychologist �Employers to create plan(s) for prevention / management in the workplace
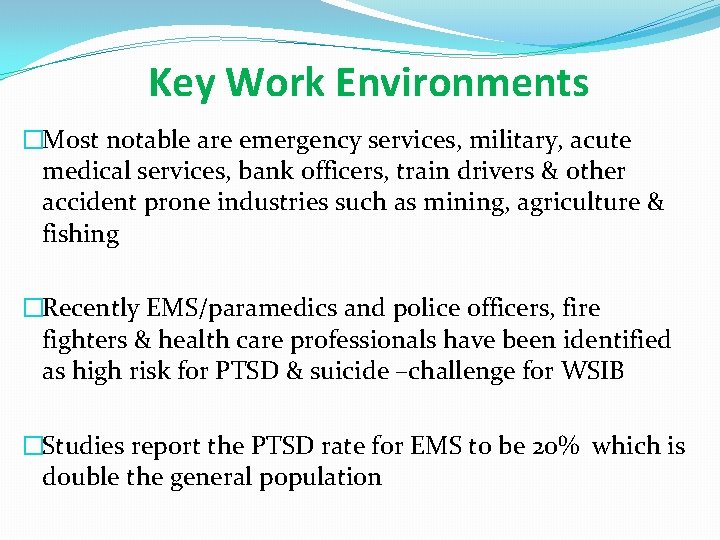
Key Work Environments �Most notable are emergency services, military, acute medical services, bank officers, train drivers & other accident prone industries such as mining, agriculture & fishing �Recently EMS/paramedics and police officers, fire fighters & health care professionals have been identified as high risk for PTSD & suicide –challenge for WSIB �Studies report the PTSD rate for EMS to be 20% which is double the general population
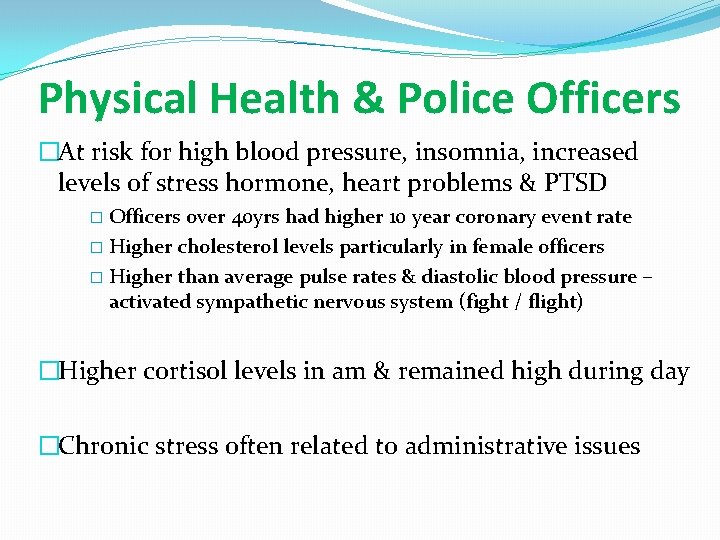
Physical Health & Police Officers �At risk for high blood pressure, insomnia, increased levels of stress hormone, heart problems & PTSD � Officers over 40 yrs had higher 10 year coronary event rate � Higher cholesterol levels particularly in female officers � Higher than average pulse rates & diastolic blood pressure – activated sympathetic nervous system (fight / flight) �Higher cortisol levels in am & remained high during day �Chronic stress often related to administrative issues
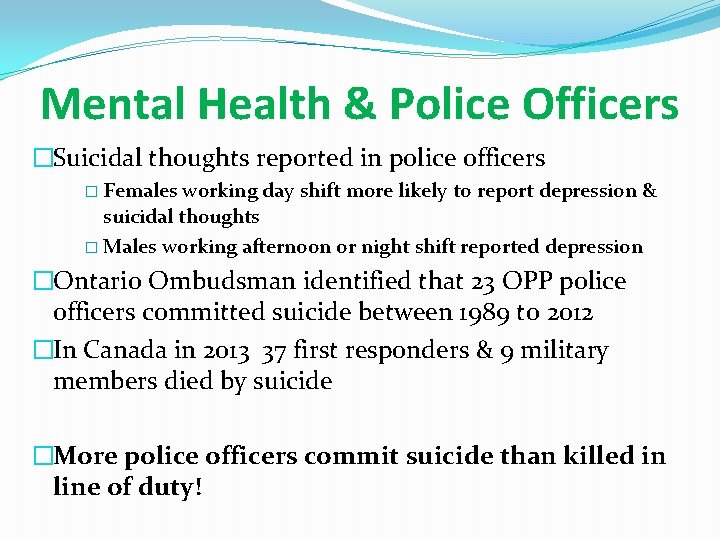
Mental Health & Police Officers �Suicidal thoughts reported in police officers � Females working day shift more likely to report depression & suicidal thoughts � Males working afternoon or night shift reported depression �Ontario Ombudsman identified that 23 OPP police officers committed suicide between 1989 to 2012 �In Canada in 2013 37 first responders & 9 military members died by suicide �More police officers commit suicide than killed in line of duty!
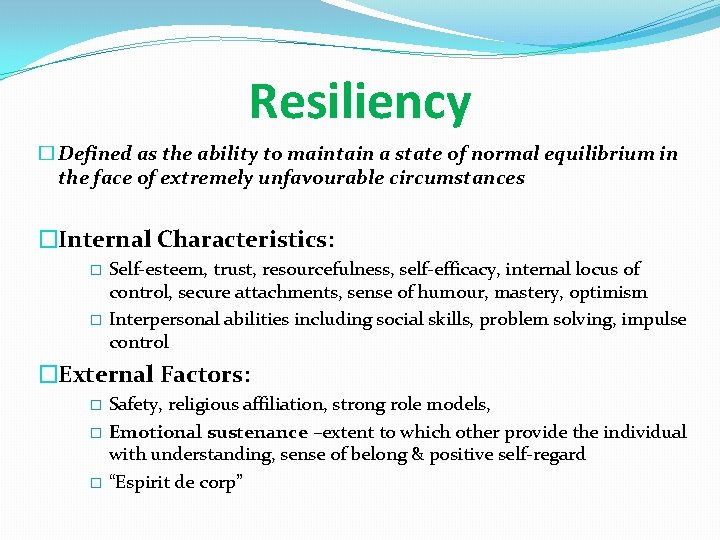
Resiliency � Defined as the ability to maintain a state of normal equilibrium in the face of extremely unfavourable circumstances �Internal Characteristics: Self-esteem, trust, resourcefulness, self-efficacy, internal locus of control, secure attachments, sense of humour, mastery, optimism � Interpersonal abilities including social skills, problem solving, impulse control � �External Factors: Safety, religious affiliation, strong role models, � Emotional sustenance –extent to which other provide the individual with understanding, sense of belong & positive self-regard � “Espirit de corp” �
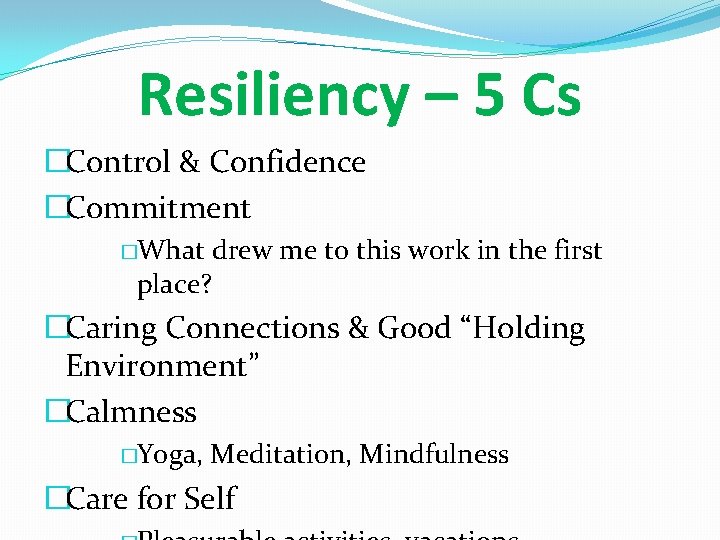
Resiliency – 5 Cs �Control & Confidence �Commitment �What drew me to this work in the first place? �Caring Connections & Good “Holding Environment” �Calmness �Yoga, Meditation, Mindfulness �Care for Self
Resources Complex PTSD (Australian) website - www. outofthestorm Books for Patients: Life After Trauma 2 nd Edition by Dena Rosenthal & Mary Beth Williams. Guildford Press 2010. Cost $20 Amazon. The PTSD Workbook-Simple, Effective Techniques for Overcoming Traumatic Stress Symtpoms 3 rd edition by Mary Beth Williams & Soili Poijula. Guildford Press 2016. Cost $30 Amazon. Complex PTSD From Surviving to Thriving: A guide & map for recovery from childhood trauma by Peter Walker. Azure Coyote Press. 2013. Cost $30 Amazon.
Questions / Discussion