Transfusion dependent microcytic hypochromic anemia with low ferritin




- Slides: 21
Transfusion dependent microcytic hypochromic anemia with low ferritin Dr Babak Abdolkarimi Pediatric hematologist
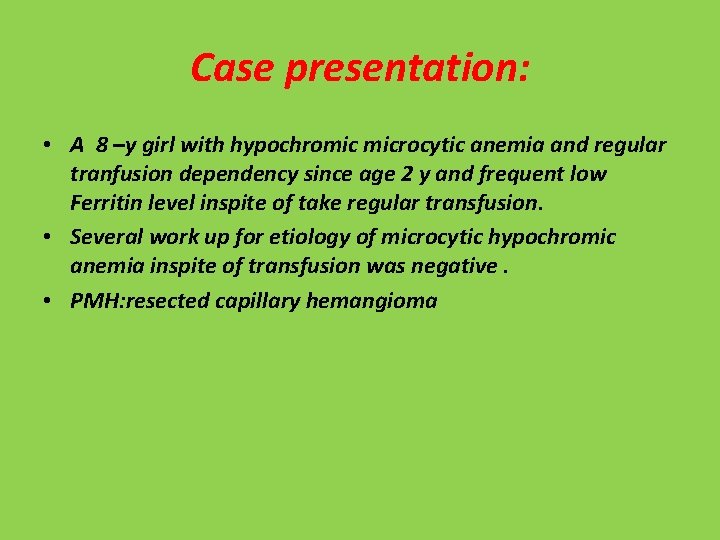
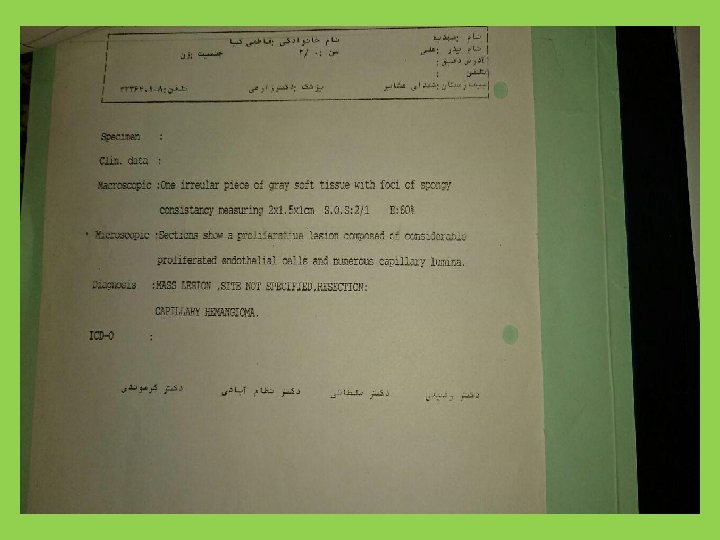
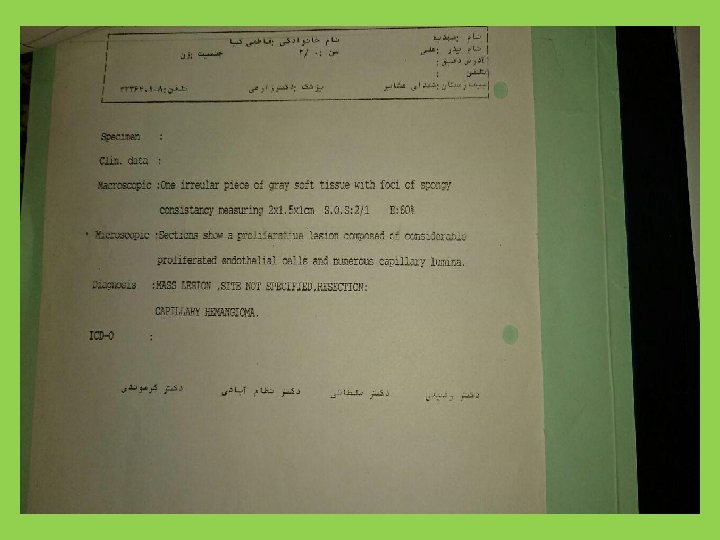
Case presentation: • A 8 –y girl with hypochromic microcytic anemia and regular tranfusion dependency since age 2 y and frequent low Ferritin level inspite of take regular transfusion. • Several work up for etiology of microcytic hypochromic anemia inspite of transfusion was negative. • PMH: resected capillary hemangioma
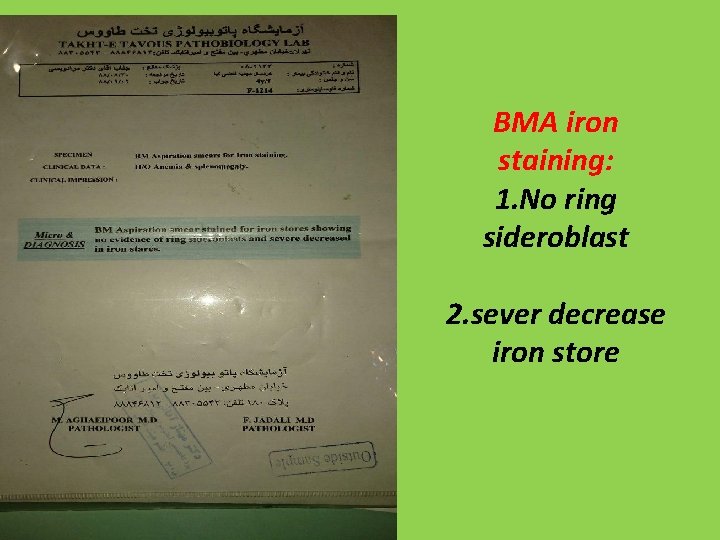
BMA iron staining: 1. No ring sideroblast 2. sever decrease iron store
S/E(OB): Neg
Vit B 12, Folate : Nl
Celiac test: Neg
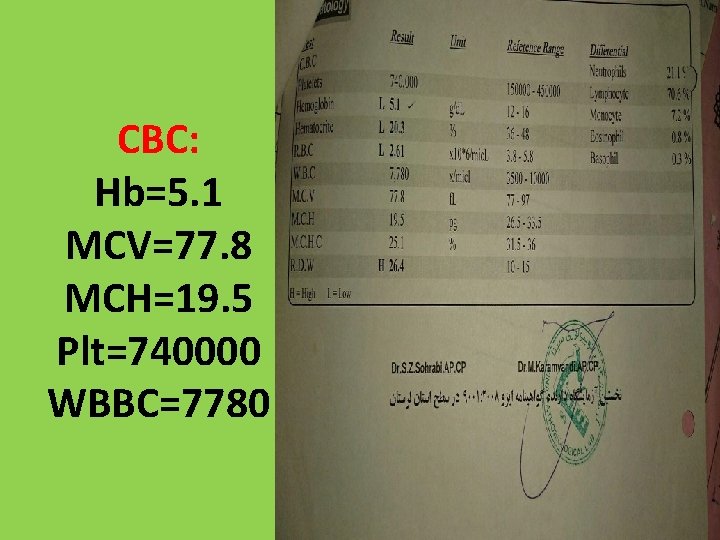
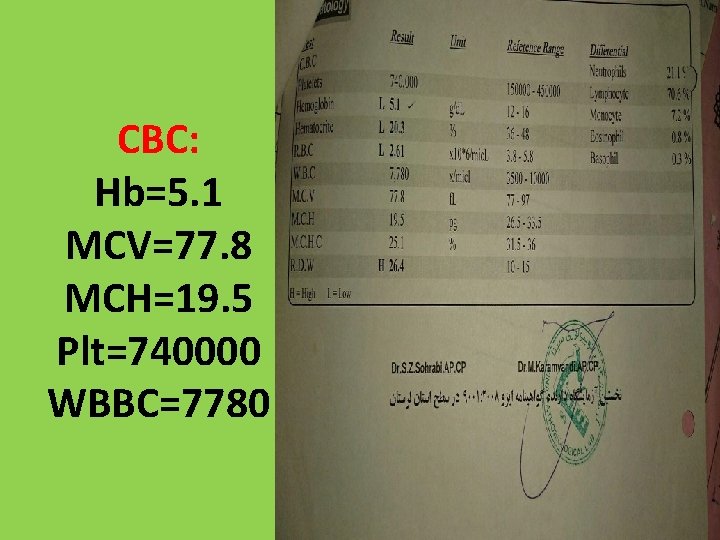
CBC: Hb=5. 1 MCV=77. 8 MCH=19. 5 Plt=740000 WBBC=7780
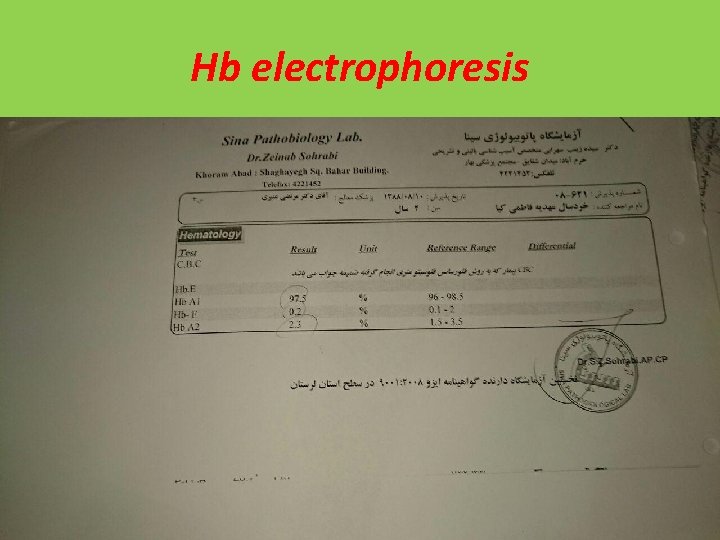
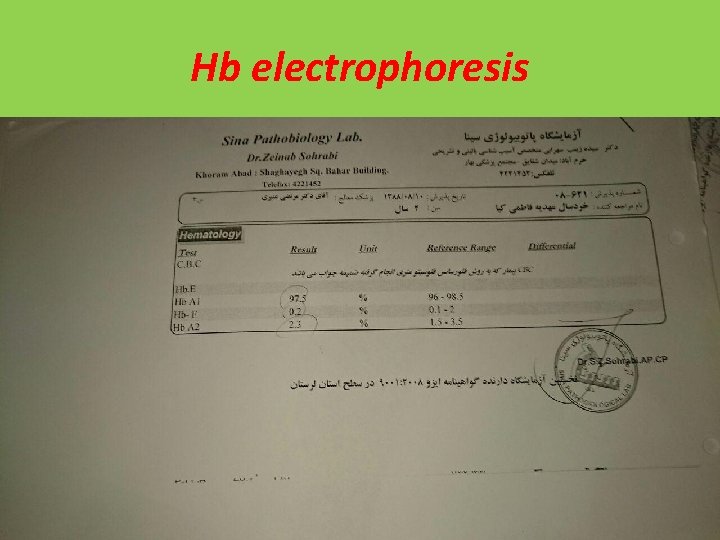
Hb electrophoresis
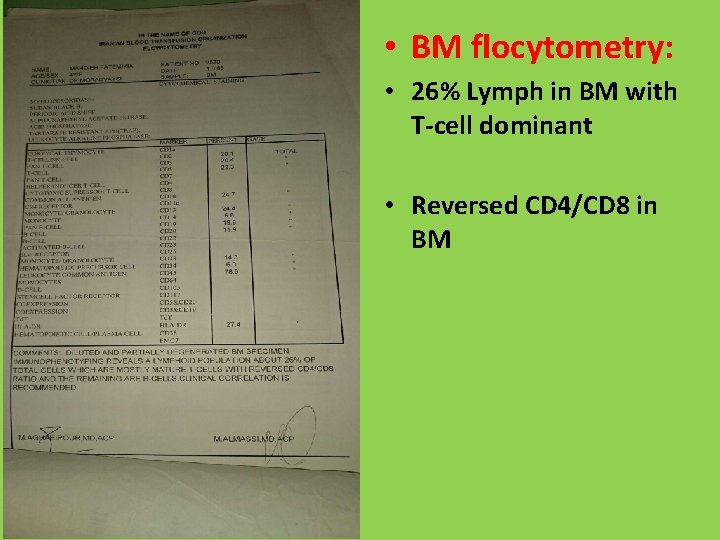
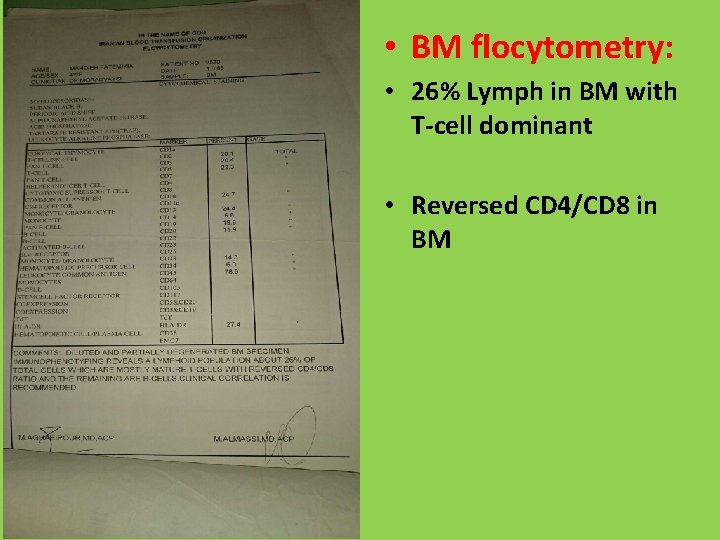
• BM flocytometry: • 26% Lymph in BM with T-cell dominant • Reversed CD 4/CD 8 in BM

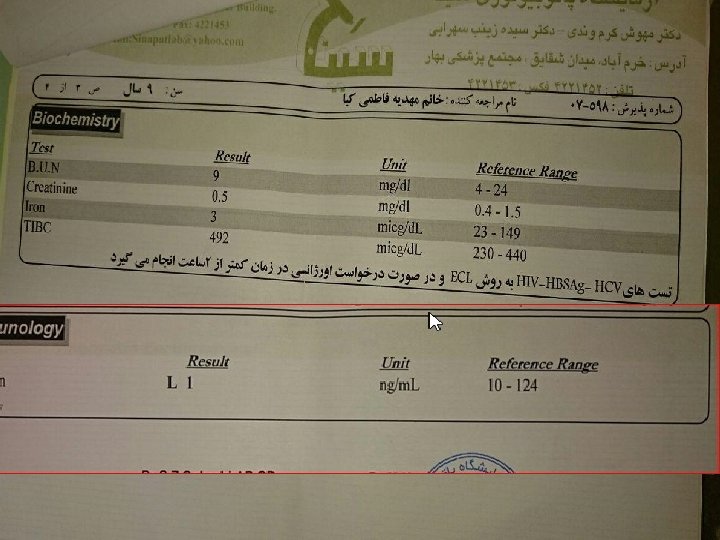
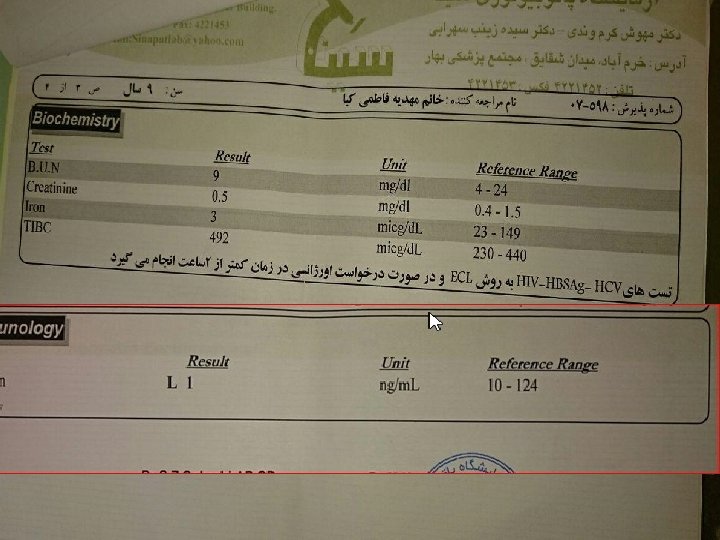
Iron profile: • Serum Iron: 3(L) • TIBC: 492(H) • Ferritin: 1(L)
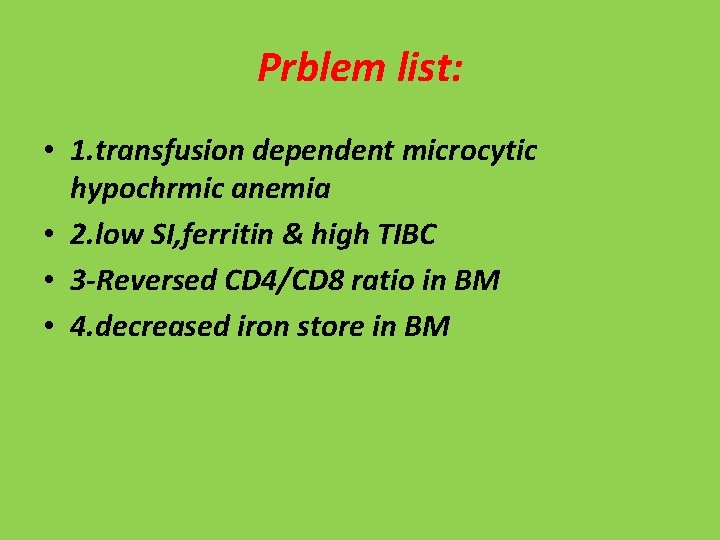
Prblem list: • 1. transfusion dependent microcytic hypochrmic anemia • 2. low SI, ferritin & high TIBC • 3 -Reversed CD 4/CD 8 ratio in BM • 4. decreased iron store in BM

What is your diagnosi?
Diffrential diagnosis • 1. congenital hypoferritinemia • 2. IRIDA • 3. ACD+IDA

hypotransferrinemia • Hypotransferrinemia though rare should be ruled out in all case of treatment refractory microcytic hypochromic anemia. • Diagnosis is confirmed by molecular genetic testing for mutation in the TF gene. Genetic counseling is available. • Treatment : infusions of FFP or purified apotransferrin that removes excess iron and replenishes the TF levels. • Monthly phlebotomy or iron chelation may be done in severe iron overload. • Treatment is life-long and regular follow-up is recommended • patients need to be in long-term follow-up to monitor the effectiveness of therapy and manage iron overload.
• The diagnosis of atransferrinemia or hypotransferrinemia may be suspected in cases with moderate to severe anemia, low (serum iron, transferrin saturation, TIBC, TF level) but with high serum ferritin. • BMA: erythroid hyperplasia with decreased iron stores. • Hepatomegaly, due to hemosiderosis and fibrosis may be noted in some cases.
IRIDA • Iron-refractory iron deficiency anemia (IRIDA) autosomal recessive disorder • IDA unresponsive to oral iron treatment but partially responsive to parenteral iron therapy • mutations in the gene TMPRSS 6, which encodes a transmembrane serine protease (also known as matriptase-2) expressed by the liver.
• inappropriately elevated levels of Hepcidin, • (a circulating hormone produced by the liver that inhibits both iron absorption from the intestine and iron release from macrophage stores. ) • TMPRSS 6 normally acts to downregulate hepcidin expression by cleaving hemojuvelin, a membranebound protein that promotes hepcidin signaling in hepatocytes. • In IRIDA, recent studies elucidating the underlying pathophysiology are presented.
