Toxic Injuries of Lung INHALATION INJURY Definitions of




- Slides: 25
Toxic Injuries of Lung 호흡기내과 허진원

INHALATION INJURY
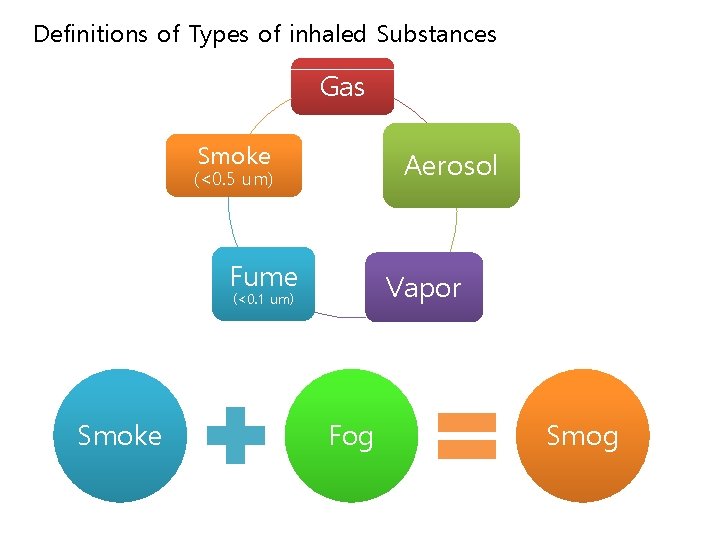
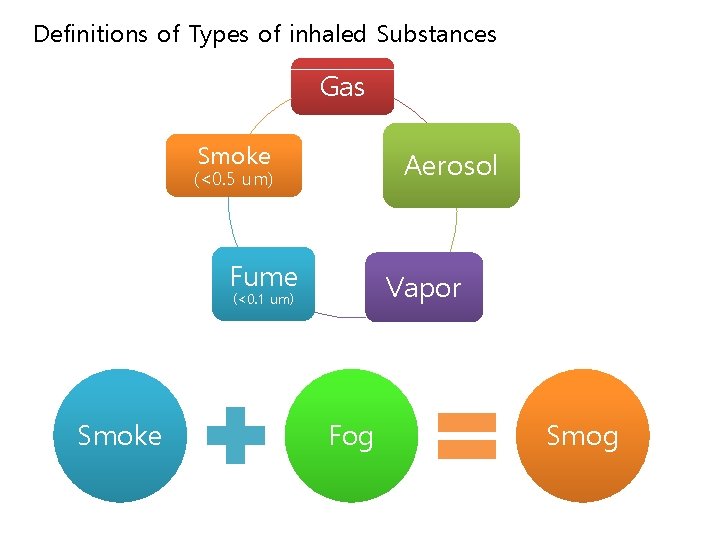
Definitions of Types of inhaled Substances Gas Smoke Aerosol (<0. 5 um) Fume Vapor (<0. 1 um) Smoke Fog Smog
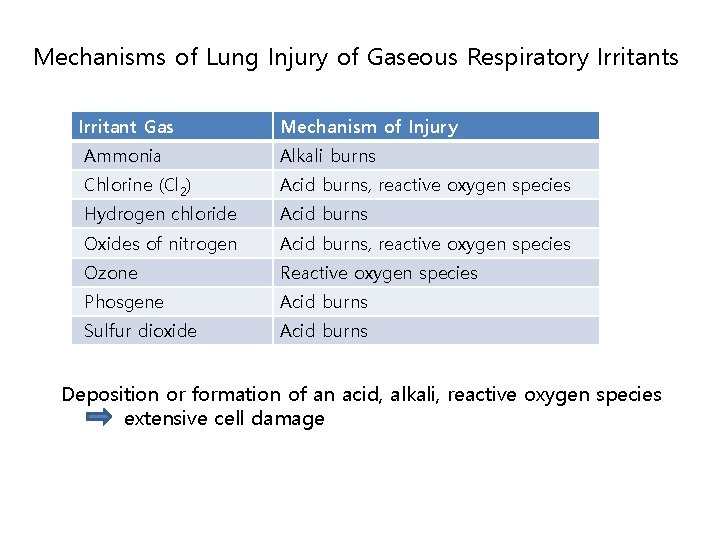
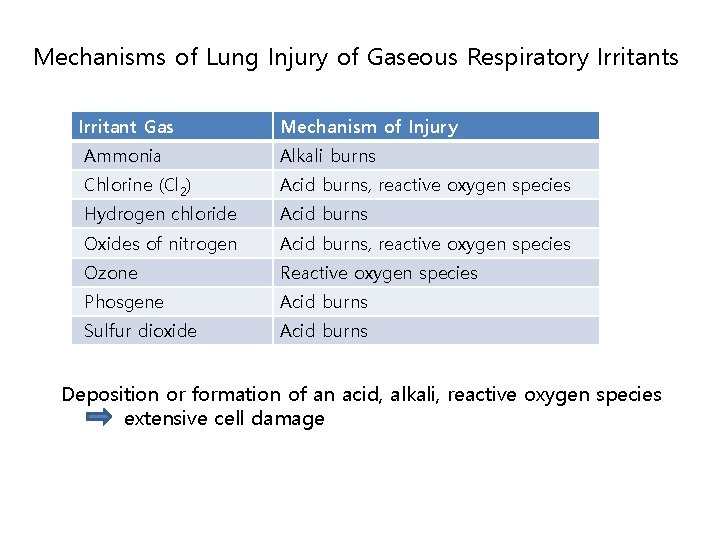
Mechanisms of Lung Injury of Gaseous Respiratory Irritants Irritant Gas Mechanism of Injury Ammonia Alkali burns Chlorine (Cl 2) Acid burns, reactive oxygen species Hydrogen chloride Acid burns Oxides of nitrogen Acid burns, reactive oxygen species Ozone Reactive oxygen species Phosgene Acid burns Sulfur dioxide Acid burns Deposition or formation of an acid, alkali, reactive oxygen species extensive cell damage
SMOG (PM 2. 5)
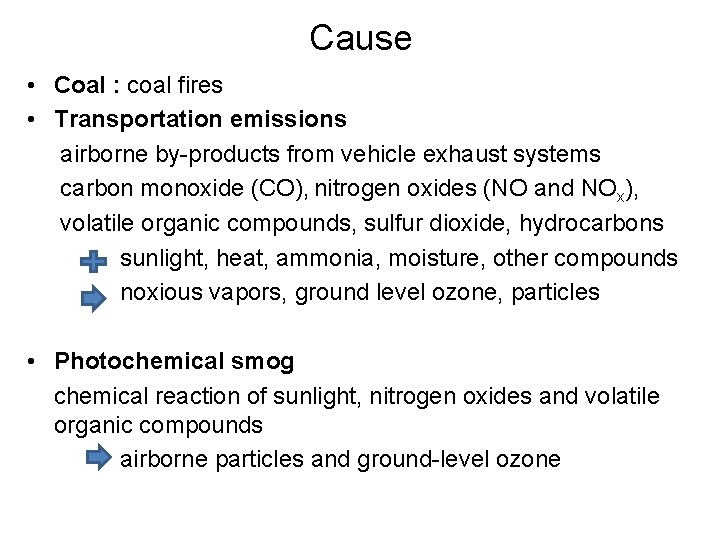
Cause • Coal : coal fires • Transportation emissions airborne by-products from vehicle exhaust systems carbon monoxide (CO), nitrogen oxides (NO and NOx), volatile organic compounds, sulfur dioxide, hydrocarbons sunlight, heat, ammonia, moisture, other compounds noxious vapors, ground level ozone, particles • Photochemical smog chemical reaction of sunlight, nitrogen oxides and volatile organic compounds airborne particles and ground-level ozone
Health Effect • harmful for senior citizens, children, and people with heart and lung conditions such as emphysema, bronchitis, and asthma. • inflame breathing passages, decrease the lungs' working capacity, cause shortness of breath, pain when inhaling deeply, wheezing, and coughing • Hospital admissions and respiratory deaths often increase during periods when ozone levels are high
SMOKE INHALATION AND THERMAL INJURY
Pathogenesis Smoke inhalation injury affects the entire respiratory tract ※ pulmonary irritants in smoke → directly toxic to respiratory epithelial or alveolar cells : aldehydes, acids, ammonia, nitrogen oxides, phosgene : Induce intense neutrophilic inflammation during 12 to 24 hours after injury : Mucosal edema and ulceration : Abnormally increased permeability of pulmonary capillaries with resultant capillary leak, and epithelial, alveolar, and immune cellular dysfunction : Bronchospasm or bronchorrhea : ARDS
Clinical manifestation 1) Thermal injury to upper airway mucosa → airway compromise (due to laryngeal edema) rapidly or during 12 to 24 hours 2) Burns to the face, mouth, and neck ; distort structures of the upper airway → airway compromise subacutely and late in the course 3) bronchospasm and bronchorrhea → cough, dyspnea, wheezing →respiratory failure 4) Accumulation of secretions, failure of mucociliary clearance and immune mechanisms, and epithelial necrosis predispose to pulmonary infection, particularly 3 to 5 days after injury 5) Late pulmonary complications; eschar formation and restriction of thoracic motion.
Diagnosis 1) Assessed emergently for airway patency 2) Immediate laryngoscopic evaluation of the oropharynx and supraglottic airway : head or neck burns, respiratory distress, stridor, or erythematous or edematous oral mucosa 3) Hypoxemia 4) Chest radiography : serially
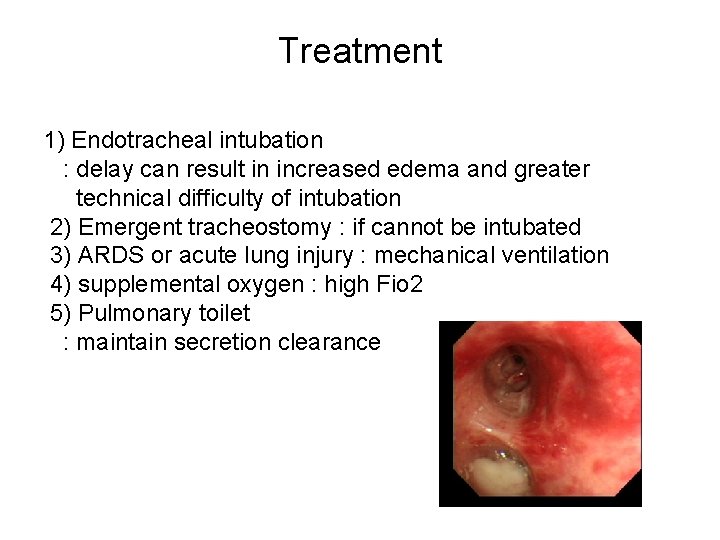
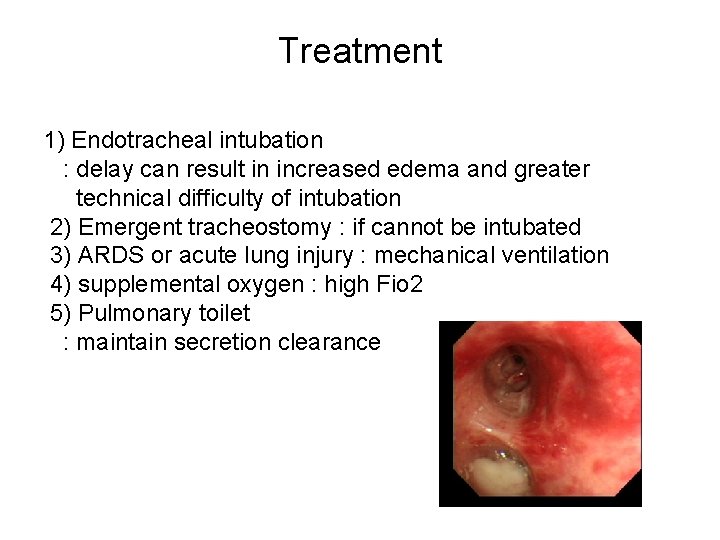
Treatment 1) Endotracheal intubation : delay can result in increased edema and greater technical difficulty of intubation 2) Emergent tracheostomy : if cannot be intubated 3) ARDS or acute lung injury : mechanical ventilation 4) supplemental oxygen : high Fio 2 5) Pulmonary toilet : maintain secretion clearance
CARBON MONOXIDE POISONING
Definition and Epidemiology 1) Carbon monoxide : a colorless, odorless gas produced by carbon-based fuels 2) CO inhalation : often coincident with smoke inhalation in fires : used in suicide attempts 3) Sources a) Endogenous production (during catabolism of Hb) : blood COHb level 0. 4 -0. 7% b) Smoking: 1 pack/day smoker → COHb level 5 -6% c) Automobile exhaust : lethal within 10 minutes in a closed space d) Heating equipment e) Fire (may reach up to 10% → COHb 75% in 1 min) : most frequent cause of immediate fire death
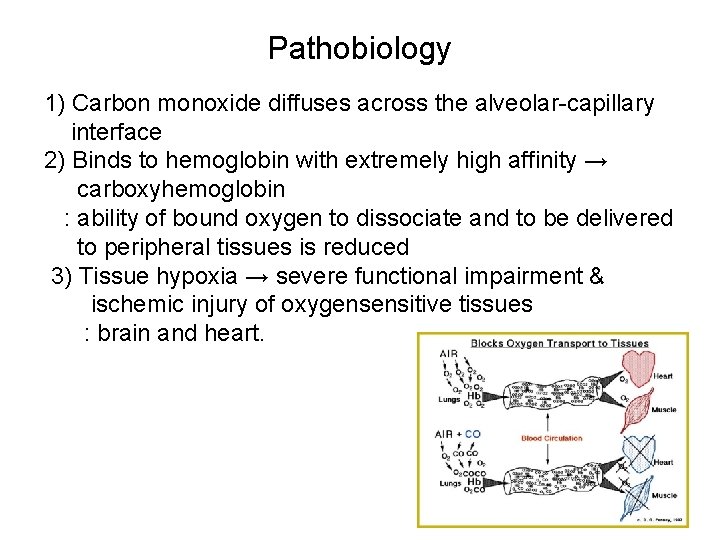
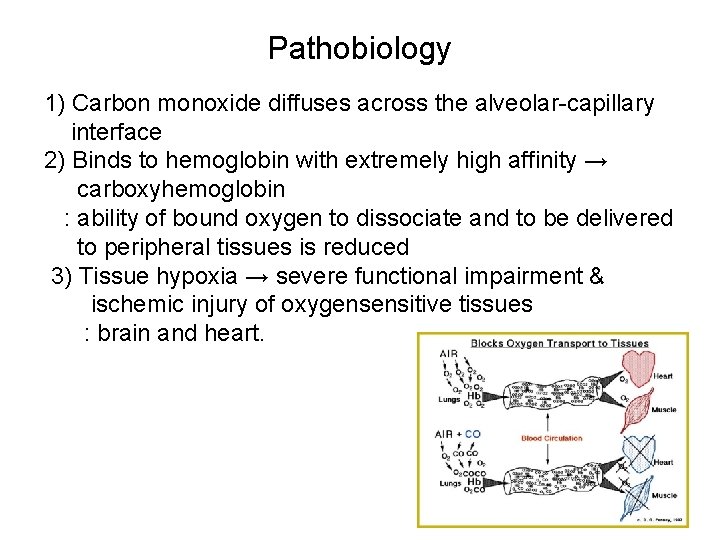
Pathobiology 1) Carbon monoxide diffuses across the alveolar-capillary interface 2) Binds to hemoglobin with extremely high affinity → carboxyhemoglobin : ability of bound oxygen to dissociate and to be delivered to peripheral tissues is reduced 3) Tissue hypoxia → severe functional impairment & ischemic injury of oxygensensitive tissues : brain and heart.

Clinical Manifestations 1) Mild intoxication : nonspecific: headache, nausea, malaise, fatigue, and dizziness 2) Severe intoxications a) Neuropsychiatric symptoms : minor disturbances in attention and cognition to agitation : confusion, hallucination : seizures or frank coma 3) Physical findings : nonspecific a) tachycardia or hyperthermia b) classic “cherry-red” skin : rarely seen c) lactic acidosis, cardiac dysfunction with arrhythmia or ischemia d) pulmonary edema, rhabdomyolysis.
Diagnosis 1) A high index of suspicion is required for diagnosis 2) Arterial carboxyhemoglobin levels checked by cooximetry : all patients known to have been involved in fires, suicide attempts, or other scenarios : symptoms generally occur at carboxyhemoglobin concentrations of 10% or higher 3) Sp. O 2 at pulse oximetry : falsely normal
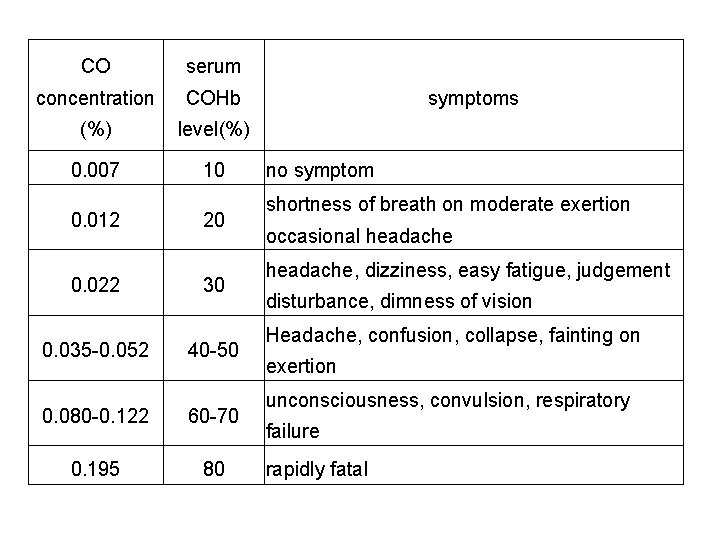
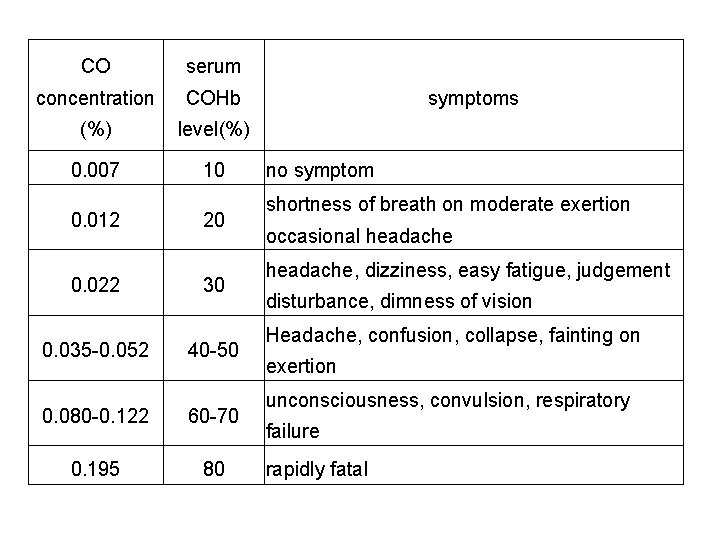
CO serum concentration COHb (%) level(%) 0. 007 10 0. 012 0. 022 0. 035 -0. 052 20 30 40 -50 0. 080 -0. 122 60 -70 0. 195 80 symptoms no symptom shortness of breath on moderate exertion occasional headache, dizziness, easy fatigue, judgement disturbance, dimness of vision Headache, confusion, collapse, fainting on exertion unconsciousness, convulsion, respiratory failure rapidly fatal
Treatment 1) CO elimination enhancement : oxygen(100%) through tight-fitting mask or endotracheal tube until COHb < 10% 2) Hyperbaric oxygen treament (HBO) a) Indication: COHb > 40% or coma or COHb > 20% in preg with fetal distress b) 3 atm for 30 min → 2 atm for 30 to 60 min c) slow decompression(∵ gas embolism) d) 3 hyperbaric oxygen treatments within 24 hrs of diagnosis reduce neurocognitive sequelae 4) Acid-base and electrolyte balance 5) Steroid and osmotic diuretics : ineffective in cytotoxic(hypoxic) cerebral edema
Prognosis 1) The mortality rate : 30% in severe cases 2) 2/3 of patients who survive ; without sequelae 3) Many of the remainder will suffer from long-term neuropsychiatric symptoms : cognitive dysfunction, abnormal mood or affect, memory disturbances, and other motor or sensory abnormalities

ORAGNOPHOSPHATE POISIONING
ETIOLOGY • Malathion, parathion, dichlorvus • 피부, 폐 및 위장관을 통해 흡수

치료 • Decontamination: 피부, 위장관 세척 • 아트로핀: muscarinic effect 치료 • Pralidoxime(2 -PAM): cholinesterase 를 reactivation 시키 면서 nicotinic symptom 치료제임
 Battering intentional or unintentional
Battering intentional or unintentional What is in concrete
What is in concrete Inhalation anesthetics
Inhalation anesthetics Inhalation route
Inhalation route Widowmaker heart attack smoke inhalation
Widowmaker heart attack smoke inhalation O2 inhalation sos
O2 inhalation sos Order of inhalation
Order of inhalation Mac anesthesia minimum alveolar concentration
Mac anesthesia minimum alveolar concentration Drug form definition
Drug form definition Oxygen tent advantages and disadvantages
Oxygen tent advantages and disadvantages Sevoflurane mac value
Sevoflurane mac value Chambre d'inhalation cipla
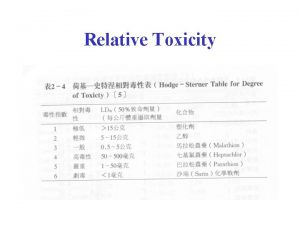
Chambre d'inhalation cipla Which is more toxic
Which is more toxic What is toxic waste
What is toxic waste The toxic tooth levy
The toxic tooth levy Toxic mentoring
Toxic mentoring Unit 4: toxins lesson 73 worksheet answers
Unit 4: toxins lesson 73 worksheet answers Polycule
Polycule Toxic relationship quiz pdf
Toxic relationship quiz pdf Toxic relatiinship
Toxic relatiinship Demulsants
Demulsants Whats bioaccumulation
Whats bioaccumulation What is the toxic trio
What is the toxic trio Be toxic
Be toxic Padilla
Padilla Toxic friendships
Toxic friendships