Thoracic Aortic Aneurysms Aortic Dissection Prof Moaath AlSmady

- Slides: 43
Thoracic Aortic Aneurysms & Aortic Dissection Prof. Moaath Al-Smady. Division of Cardiothoracic/Vascular surgery – Department of Surgery University of Jordan 1
Presentation’s Outline n n n Introduction Definition Anatomy n Presentation n Diagnosis n Management n Open repair vs. EVAR n Complications Natural History Risk factors 2
Introduction n Aneurysm and dissection are the most common diseases of the aorta. n Definition : localized or diffuse aortic dilation that exceeds 50% of the normal aortic diameter n Elasticity and tensile strength from the medial layer contains elastin, collagen, smooth muscle cells, and ground substance Genetic Factors n Cystic medial degeneration leads to the final common pathway of progressive aortic expansion and eventual rupture n Atherosclerosis : coexisting process rather than the underlying cause. n The vicious cycle Laplace's law (tension = pressure ´ radius) 3
Location n Ascending n Arch n Descending n Thoracoabdominal 4
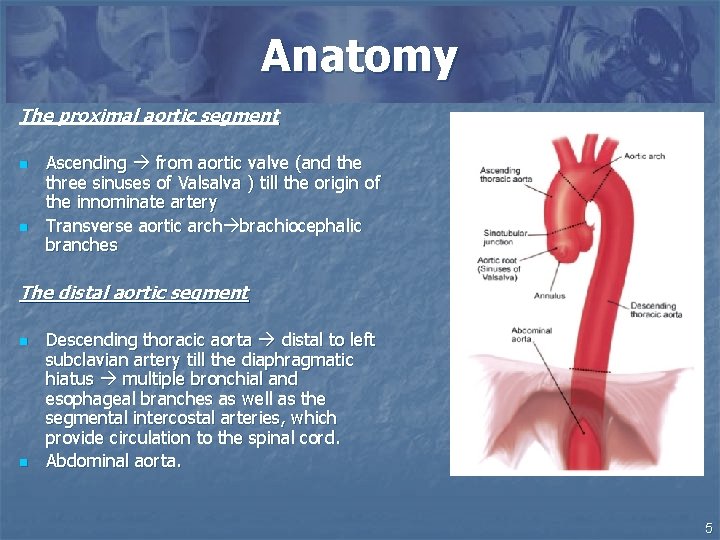
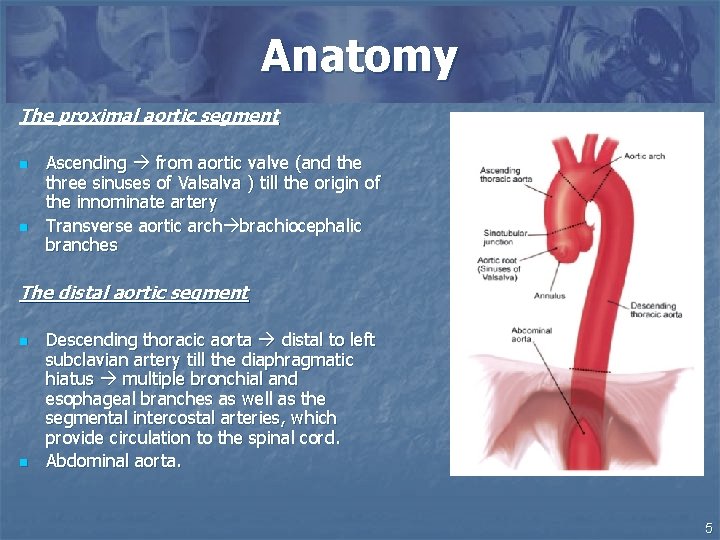
Anatomy The proximal aortic segment n n Ascending from aortic valve (and the three sinuses of Valsalva ) till the origin of the innominate artery Transverse aortic arch brachiocephalic branches The distal aortic segment n n Descending thoracic aorta distal to left subclavian artery till the diaphragmatic hiatus multiple bronchial and esophageal branches as well as the segmental intercostal arteries, which provide circulation to the spinal cord. Abdominal aorta. 5
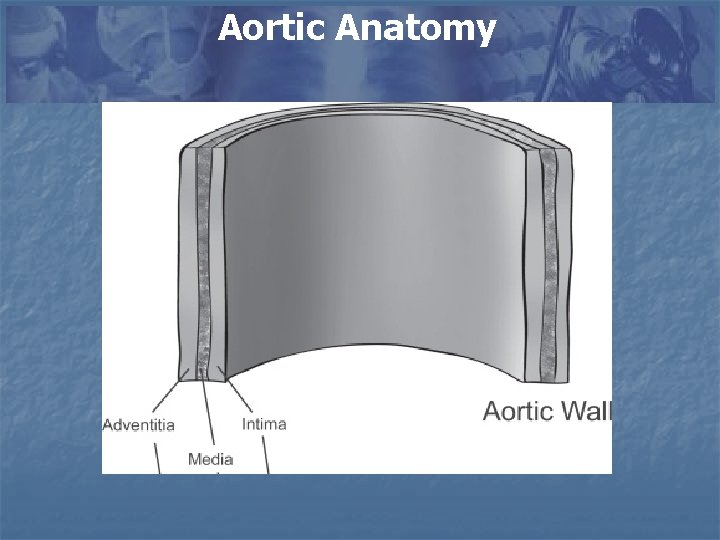
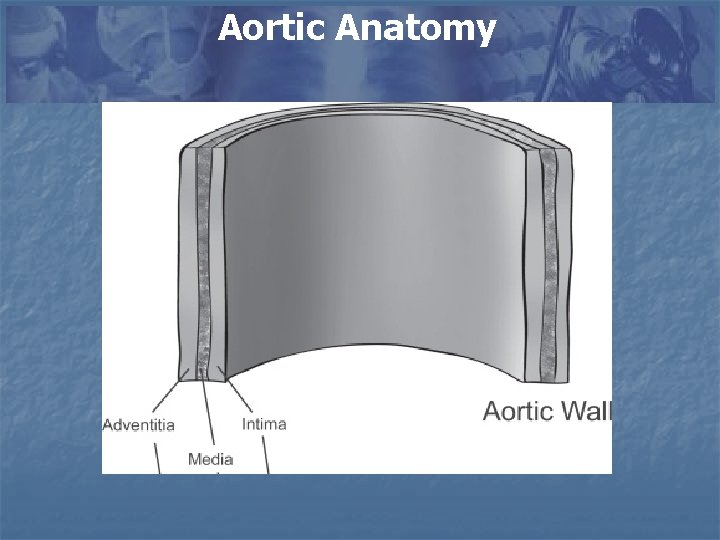
Aortic Anatomy
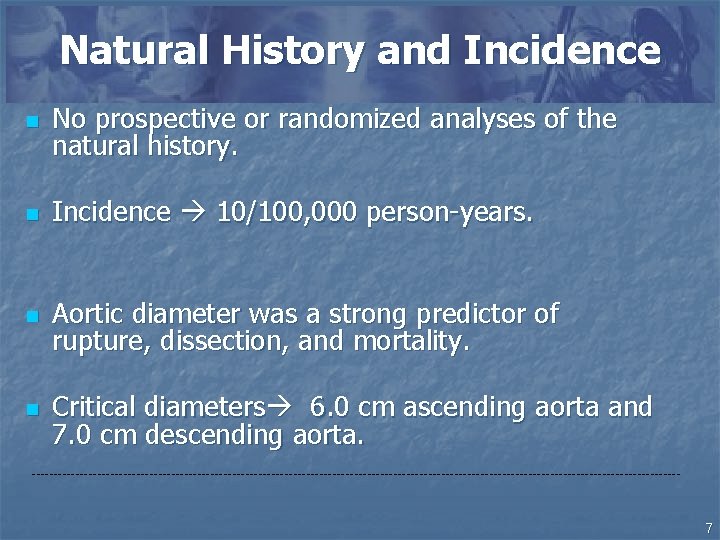
Natural History and Incidence n No prospective or randomized analyses of the natural history. n Incidence 10/100, 000 person-years. n Aortic diameter was a strong predictor of rupture, dissection, and mortality. n Critical diameters 6. 0 cm ascending aorta and 7. 0 cm descending aorta. --------------------------------------------------------------------------- 7
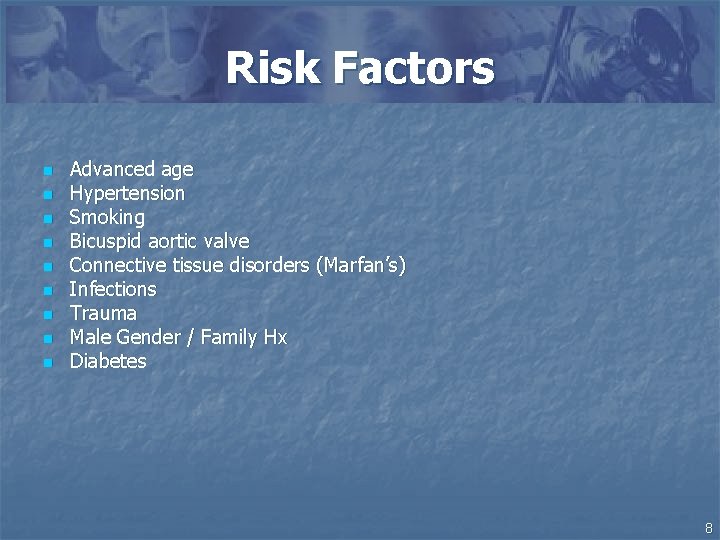
Risk Factors n n n n n Advanced age Hypertension Smoking Bicuspid aortic valve Connective tissue disorders (Marfan’s) Infections Trauma Male Gender / Family Hx Diabetes 8
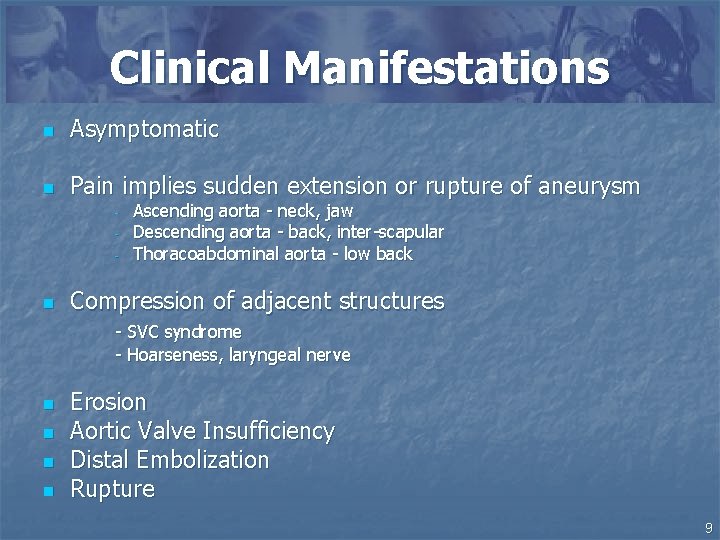
Clinical Manifestations n Asymptomatic n Pain implies sudden extension or rupture of aneurysm - n Ascending aorta - neck, jaw Descending aorta - back, inter-scapular Thoracoabdominal aorta - low back Compression of adjacent structures - SVC syndrome - Hoarseness, laryngeal nerve n n Erosion Aortic Valve Insufficiency Distal Embolization Rupture 9
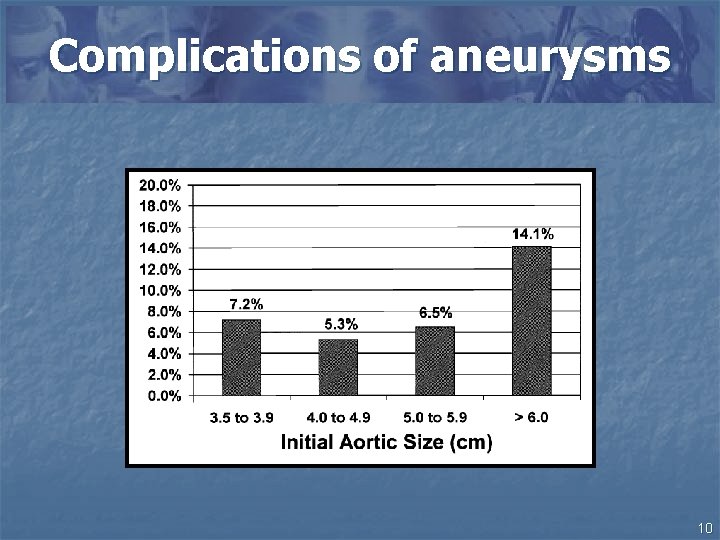
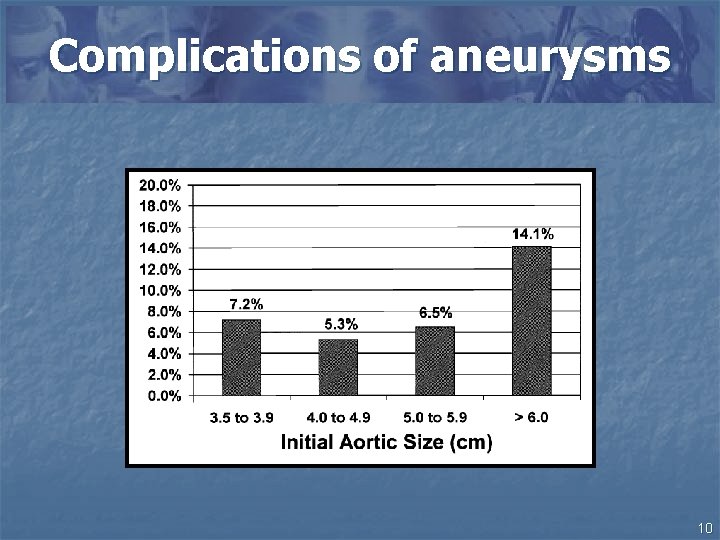
Complications of aneurysms 10
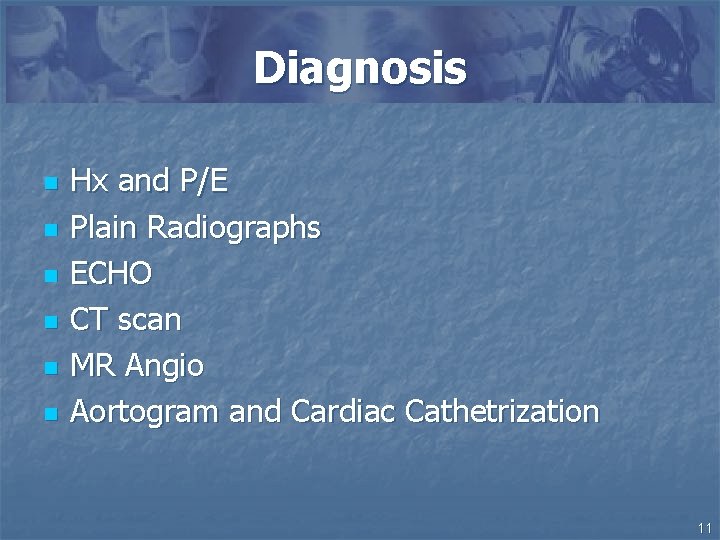
Diagnosis n n n Hx and P/E Plain Radiographs ECHO CT scan MR Angio Aortogram and Cardiac Cathetrization 11
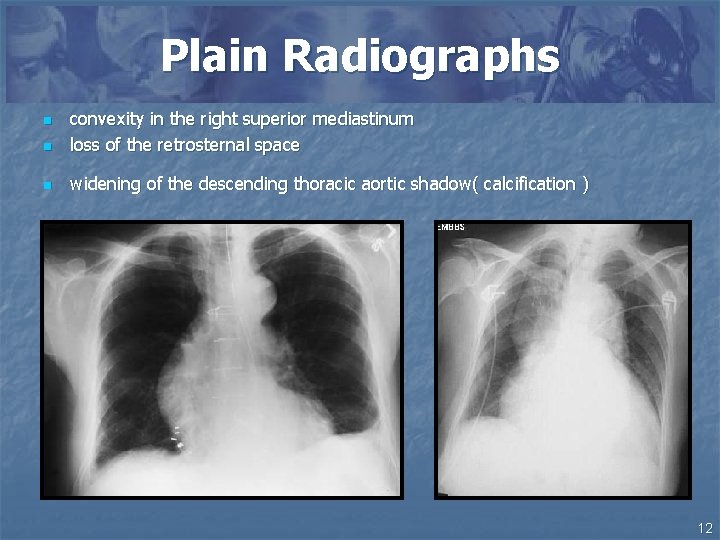
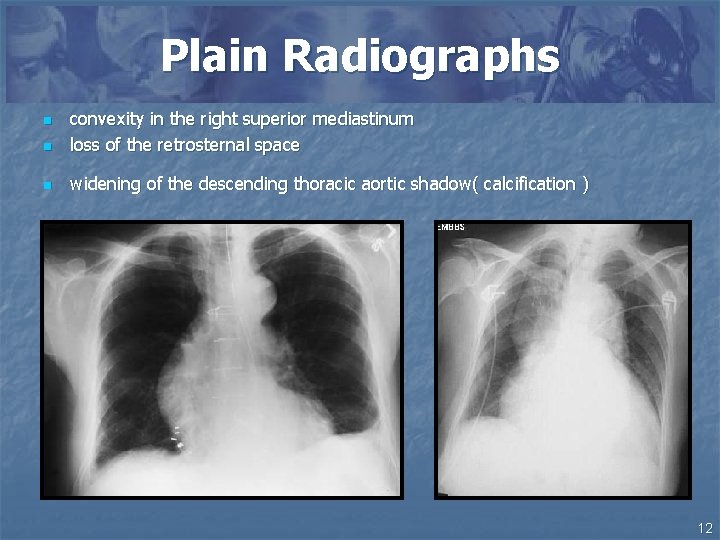
Plain Radiographs n convexity in the right superior mediastinum loss of the retrosternal space n widening of the descending thoracic aortic shadow( calcification ) n 12
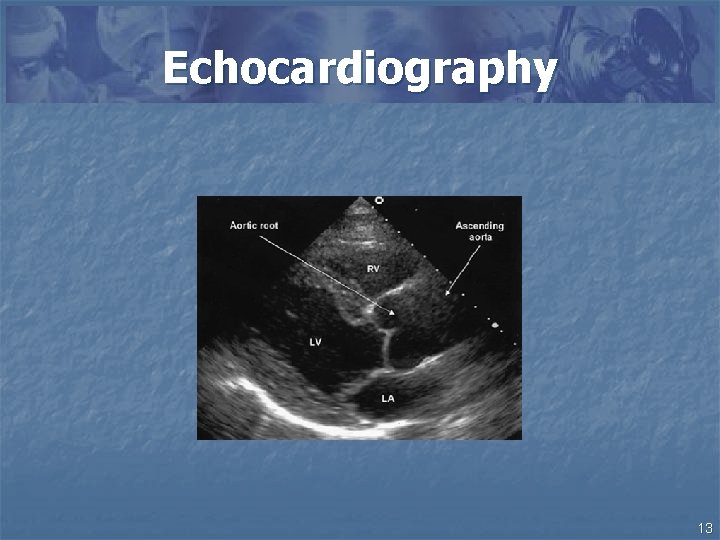
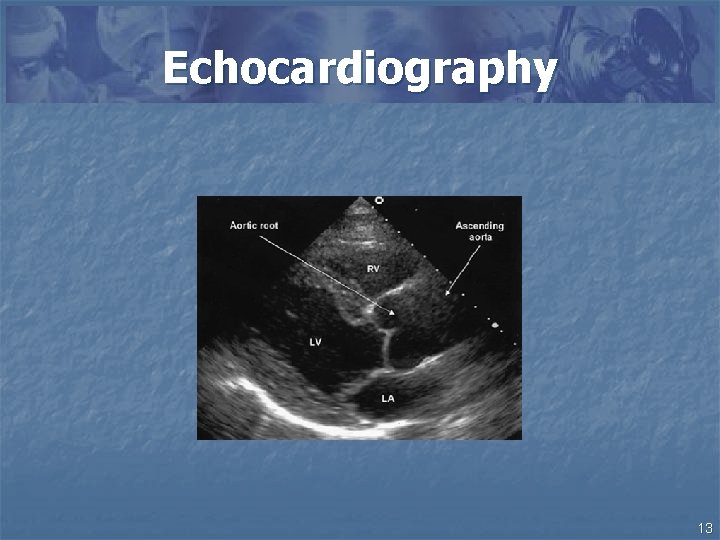
Echocardiography 13
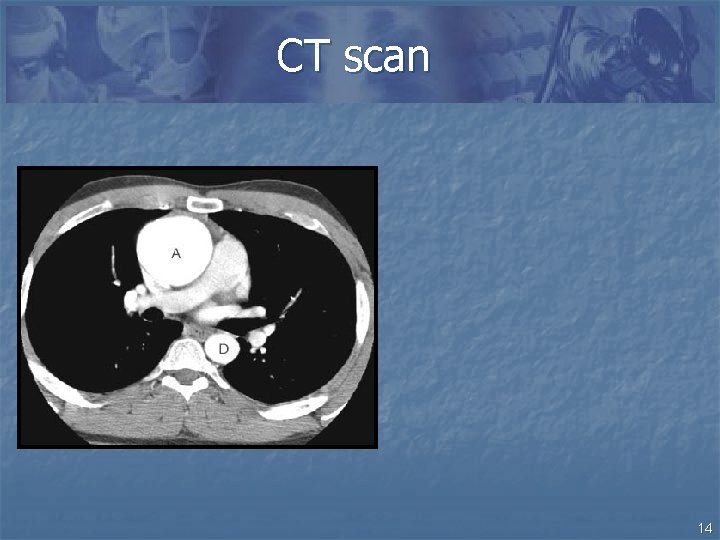
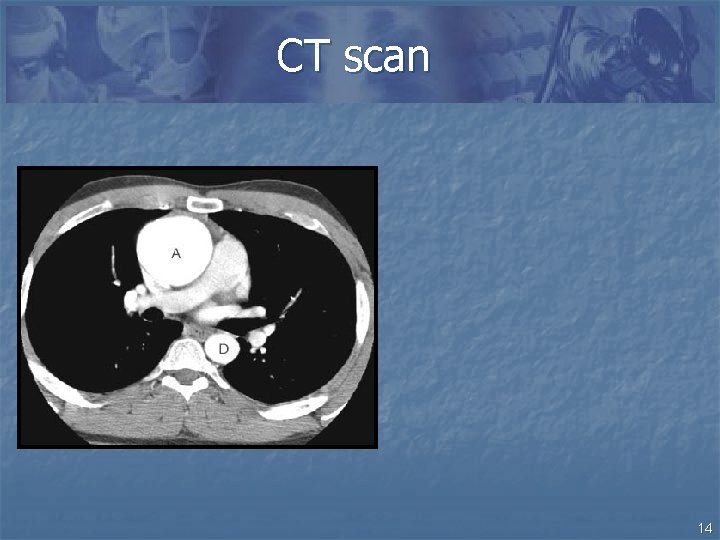
CT scan 14
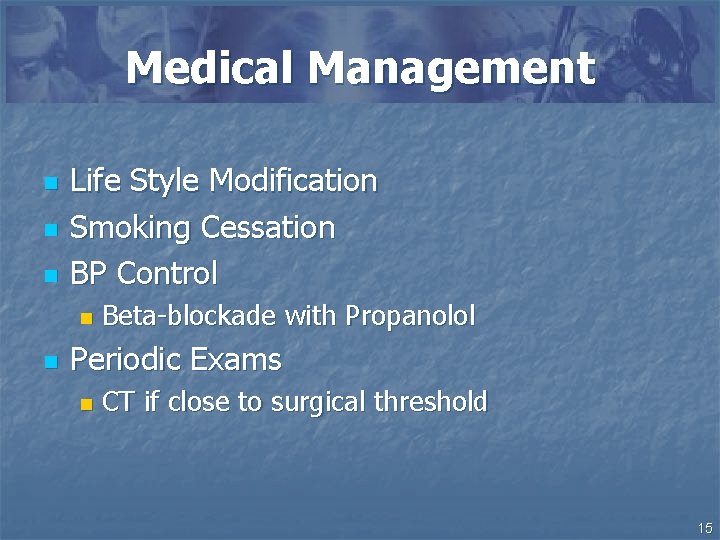
Medical Management n n n Life Style Modification Smoking Cessation BP Control n n Beta-blockade with Propanolol Periodic Exams n CT if close to surgical threshold 15
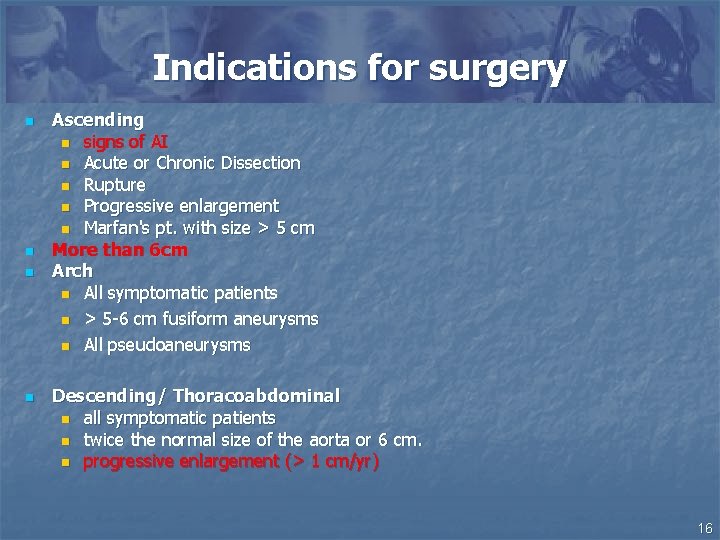
Indications for surgery n n Ascending n signs of AI n Acute or Chronic Dissection n Rupture n Progressive enlargement n Marfan's pt. with size > 5 cm More than 6 cm Arch n All symptomatic patients n > 5 -6 cm fusiform aneurysms n All pseudoaneurysms Descending/ Thoracoabdominal n all symptomatic patients n twice the normal size of the aorta or 6 cm. n progressive enlargement (> 1 cm/yr) 16
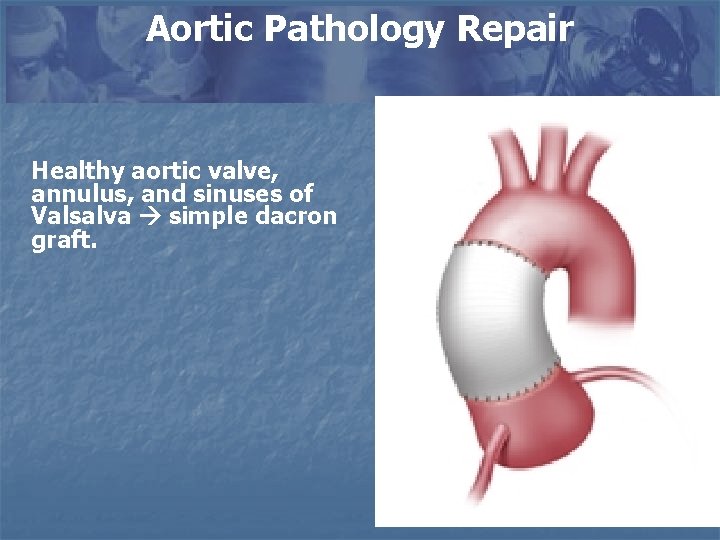
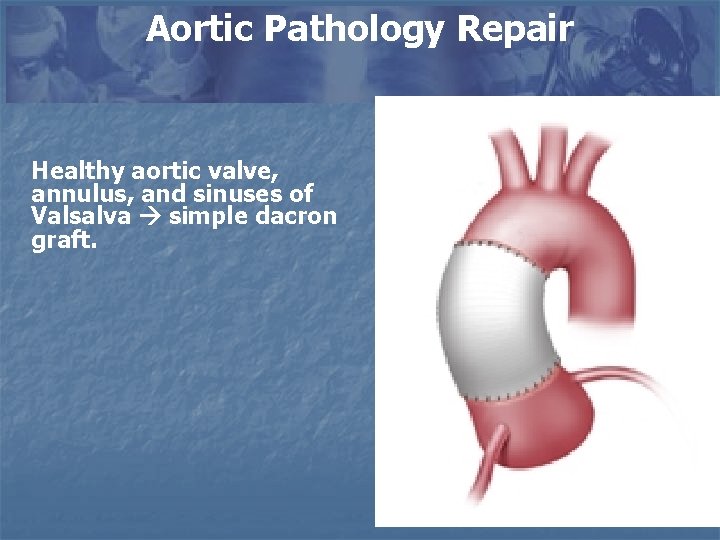
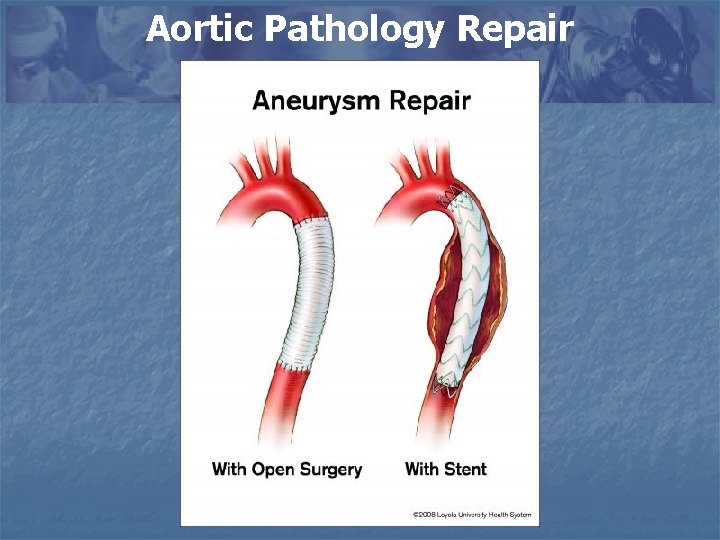
Aortic Pathology Repair Healthy aortic valve, annulus, and sinuses of Valsalva simple dacron graft.
Composite valve and graft replacement 18
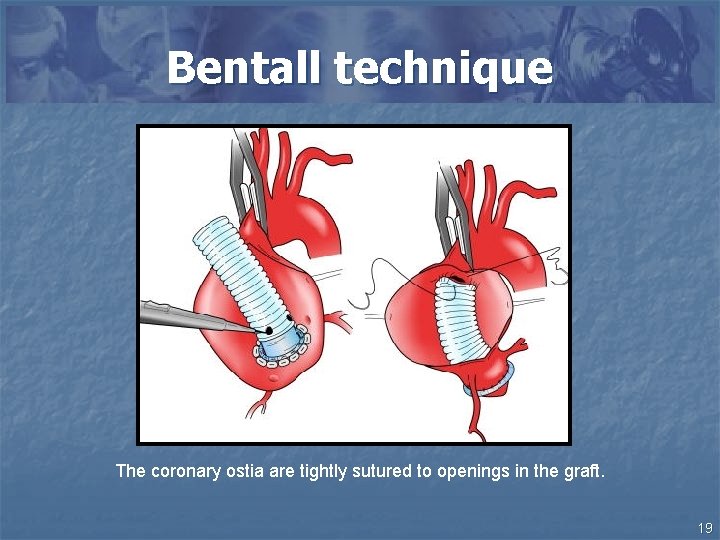
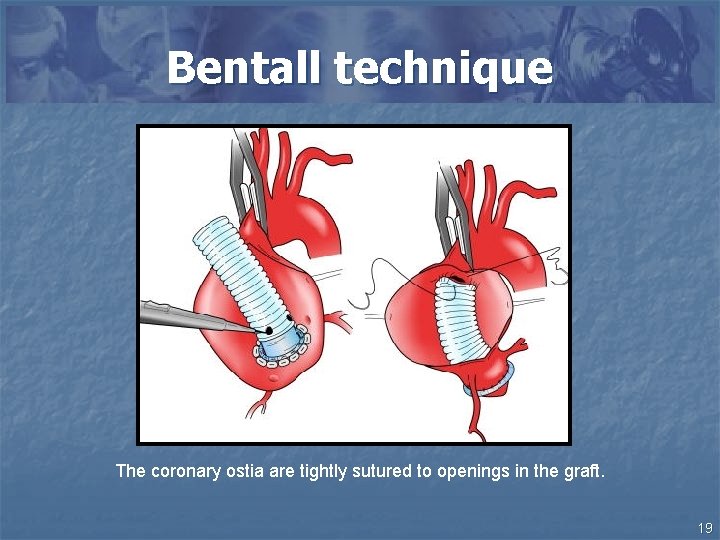
Bentall technique The coronary ostia are tightly sutured to openings in the graft. 19
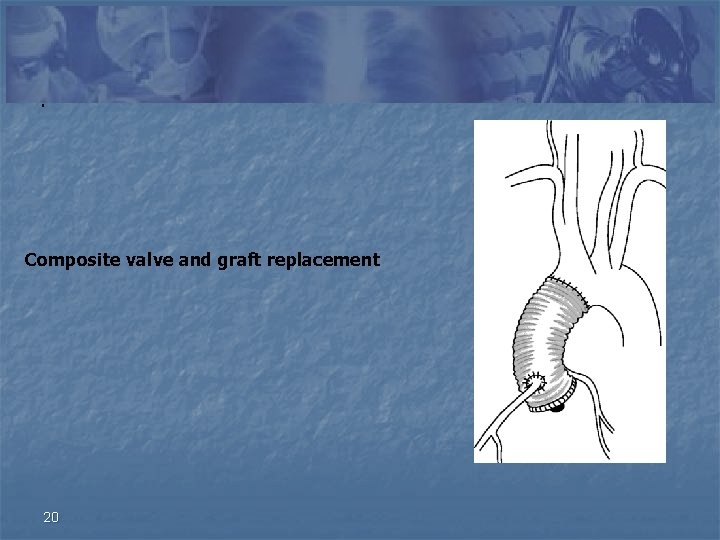
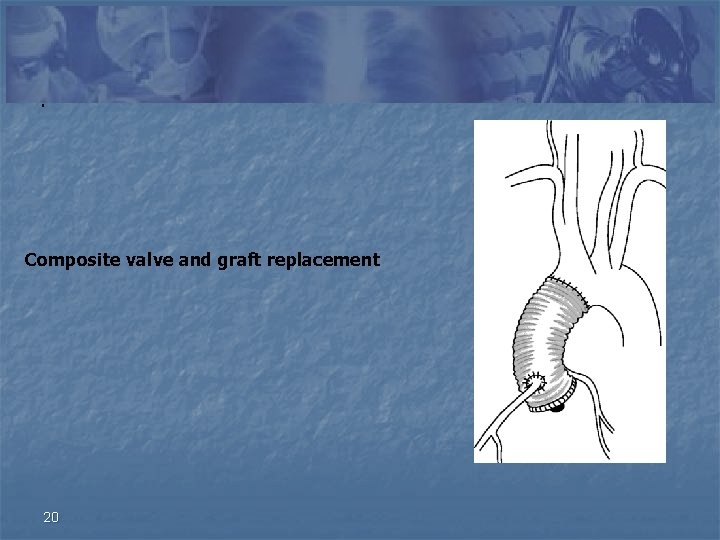
. Composite valve and graft replacement 20
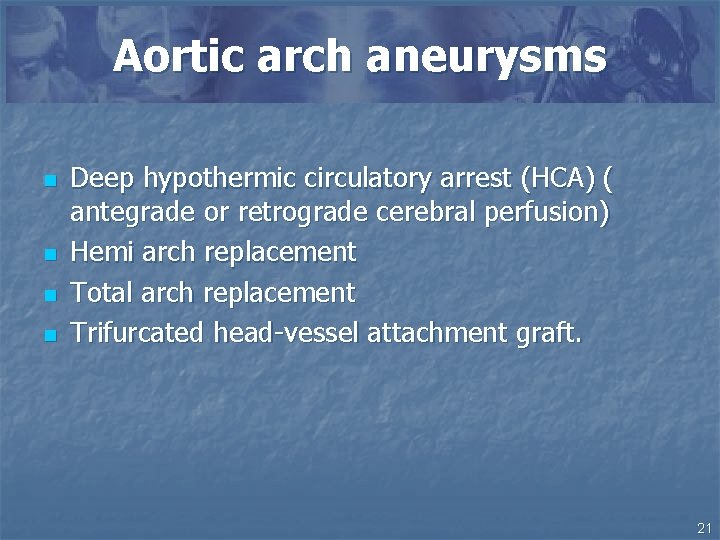
Aortic arch aneurysms n n Deep hypothermic circulatory arrest (HCA) ( antegrade or retrograde cerebral perfusion) Hemi arch replacement Total arch replacement Trifurcated head-vessel attachment graft. 21
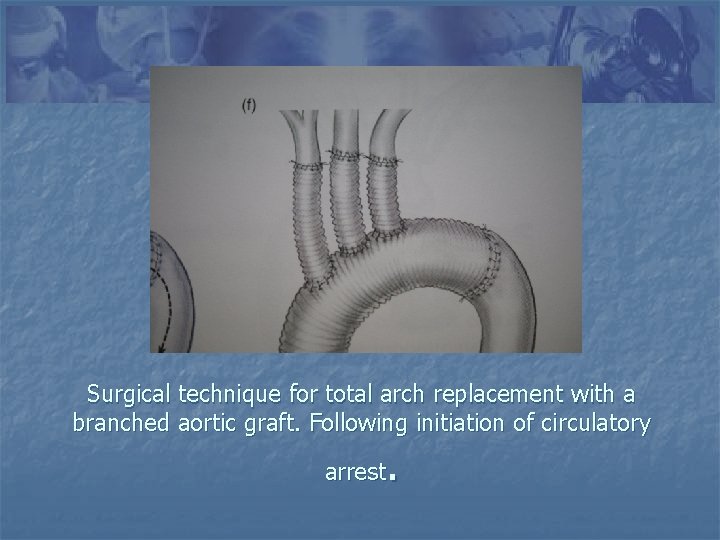
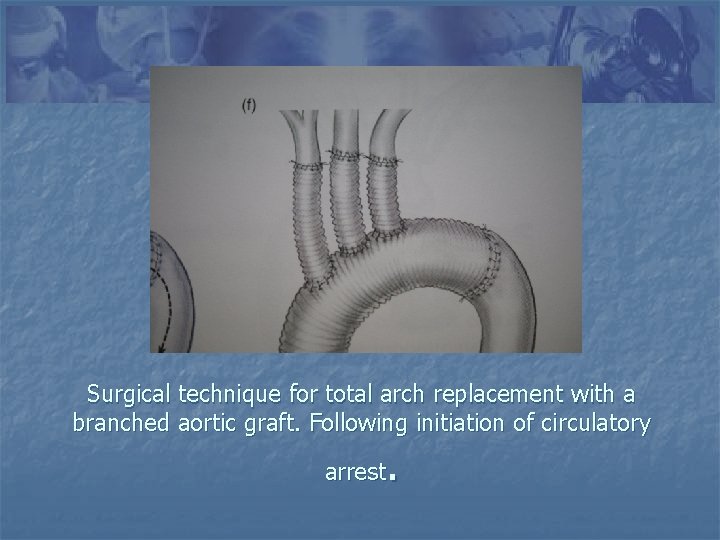
Surgical technique for total arch replacement with a branched aortic graft. Following initiation of circulatory . arrest
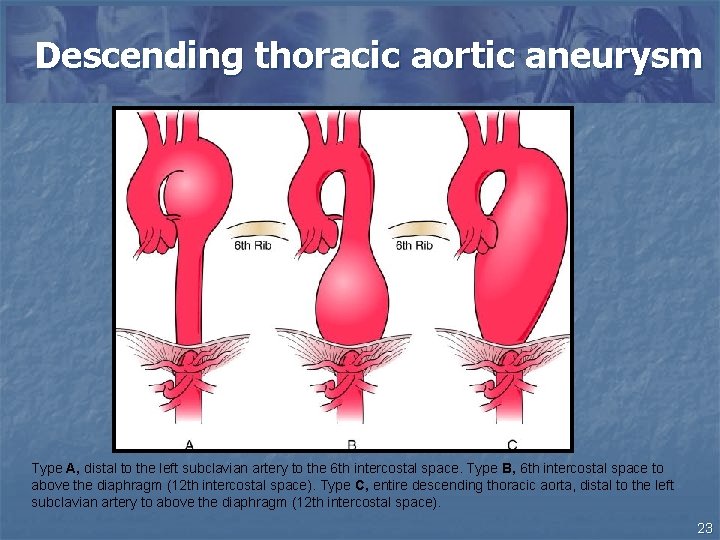
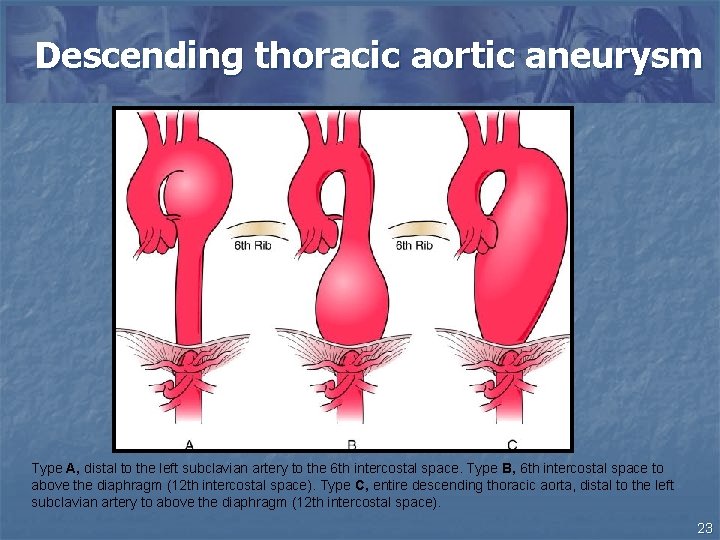
Descending thoracic aortic aneurysm Type A, distal to the left subclavian artery to the 6 th intercostal space. Type B, 6 th intercostal space to above the diaphragm (12 th intercostal space). Type C, entire descending thoracic aorta, distal to the left subclavian artery to above the diaphragm (12 th intercostal space). 23
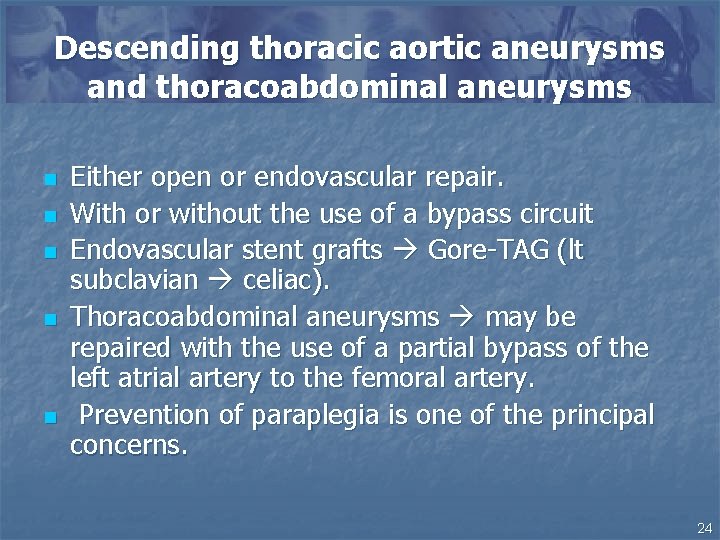
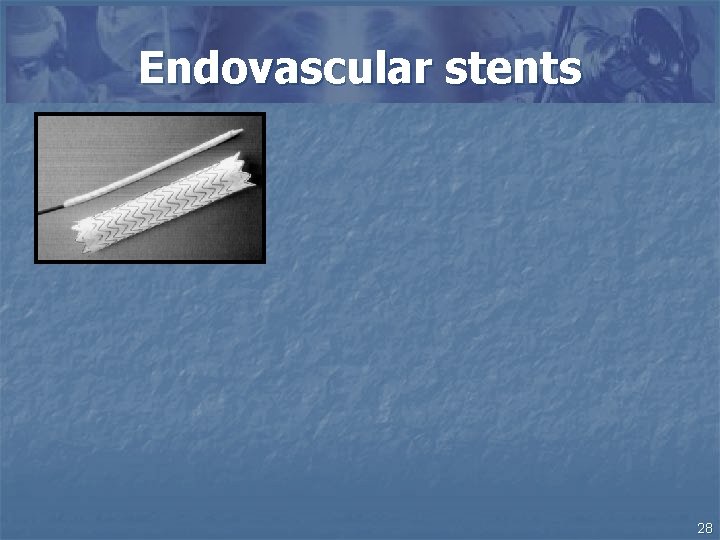
Descending thoracic aortic aneurysms and thoracoabdominal aneurysms n n n Either open or endovascular repair. With or without the use of a bypass circuit Endovascular stent grafts Gore-TAG (lt subclavian celiac). Thoracoabdominal aneurysms may be repaired with the use of a partial bypass of the left atrial artery to the femoral artery. Prevention of paraplegia is one of the principal concerns. 24
Surgical complications n n n n Bleeding Stroke ( arch repairs ) hypothermic circulatory arrest. Myocardial infarction Pulmonary dysfunction Renal dysfunction Paraparesis and paraplegia Endovascular stenting complications : endoleaks, stent fractures, and stent graft migration. 25
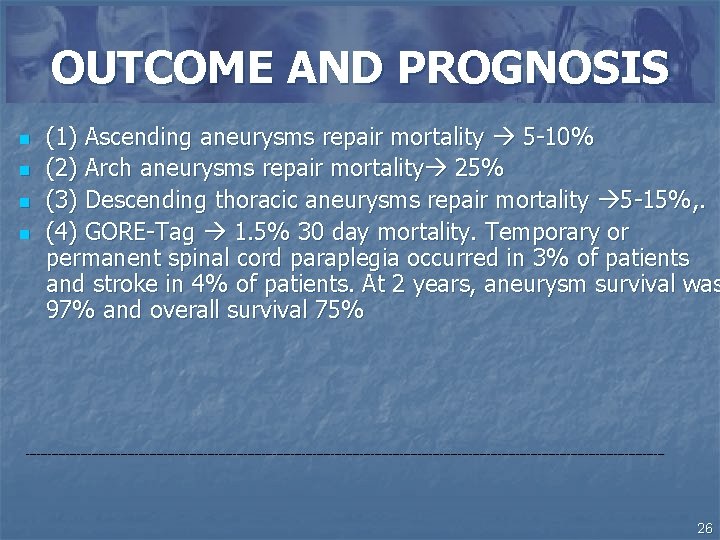
OUTCOME AND PROGNOSIS n n (1) Ascending aneurysms repair mortality 5 -10% (2) Arch aneurysms repair mortality 25% (3) Descending thoracic aneurysms repair mortality 5 -15%, . (4) GORE-Tag 1. 5% 30 day mortality. Temporary or permanent spinal cord paraplegia occurred in 3% of patients and stroke in 4% of patients. At 2 years, aneurysm survival was 97% and overall survival 75% ---------------------------------------------------------------------------------------- 26
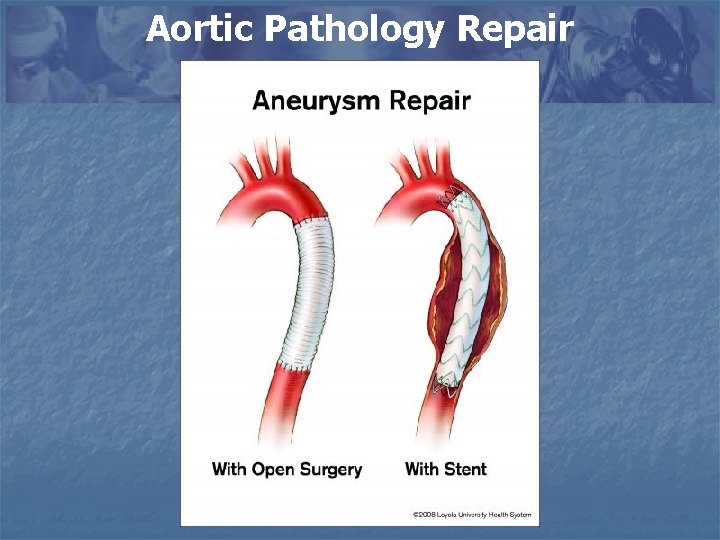
Aortic Pathology Repair
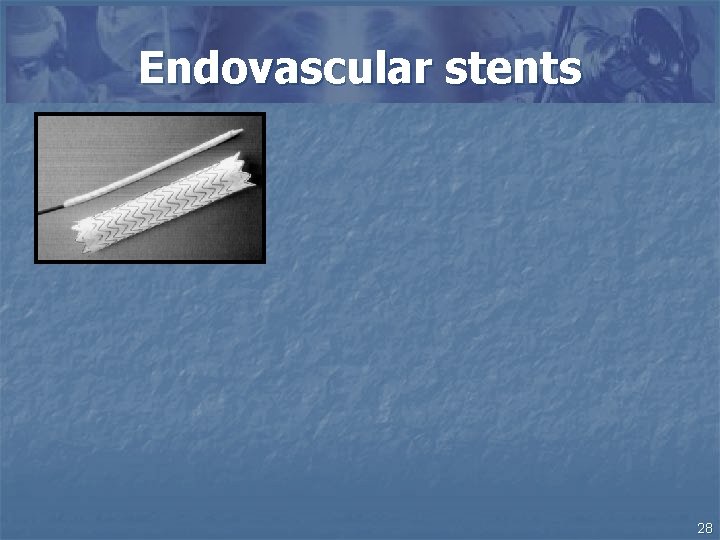
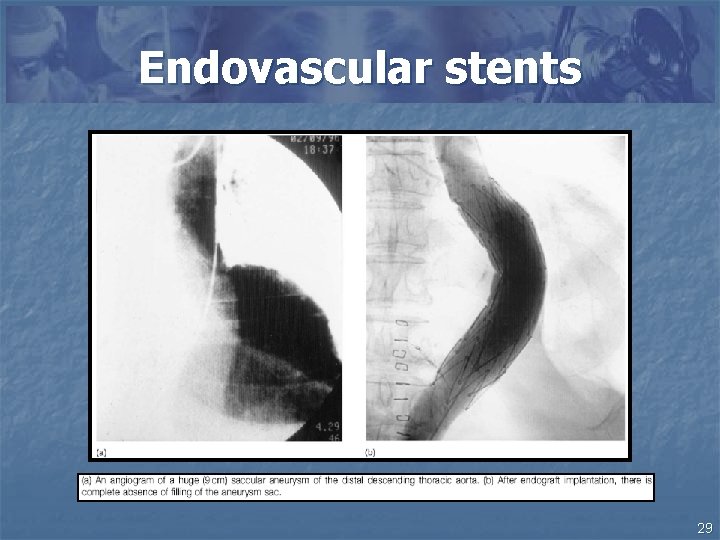
Endovascular stents 28
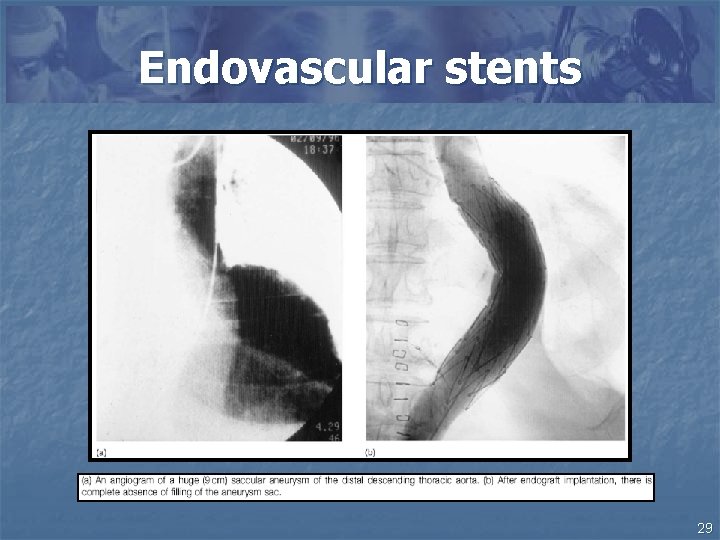
Endovascular stents 29
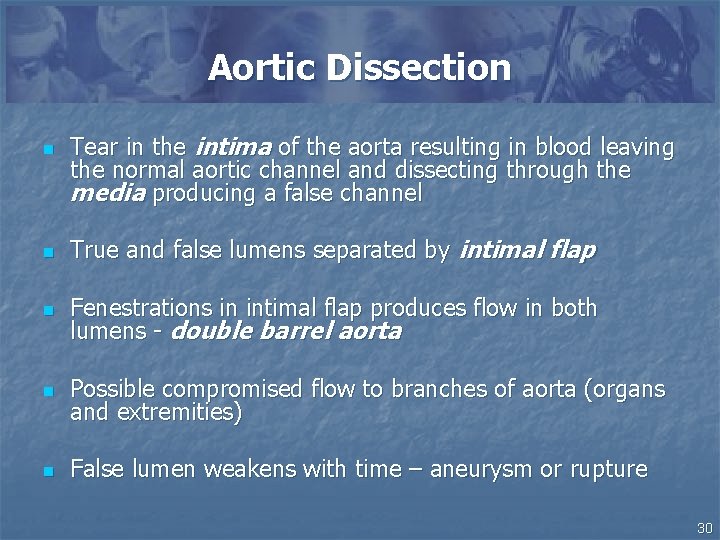
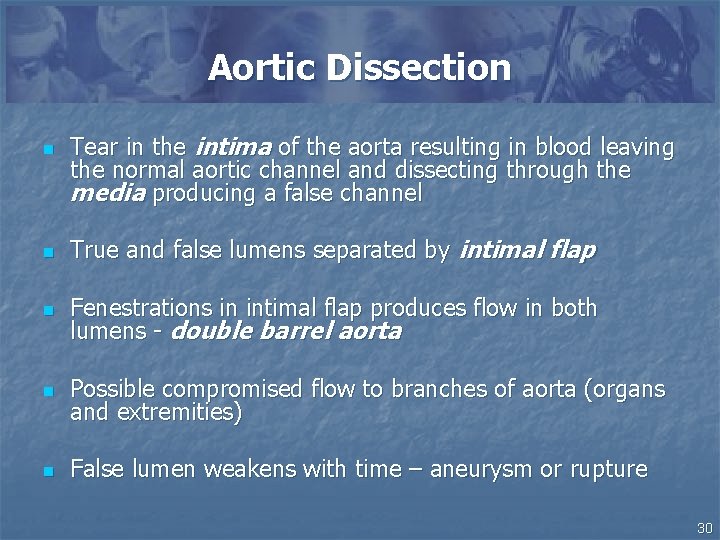
Aortic Dissection n Tear in the intima of the aorta resulting in blood leaving the normal aortic channel and dissecting through the media producing a false channel n True and false lumens separated by intimal flap n Fenestrations in intimal flap produces flow in both lumens - double barrel aorta n Possible compromised flow to branches of aorta (organs and extremities) n False lumen weakens with time – aneurysm or rupture 30
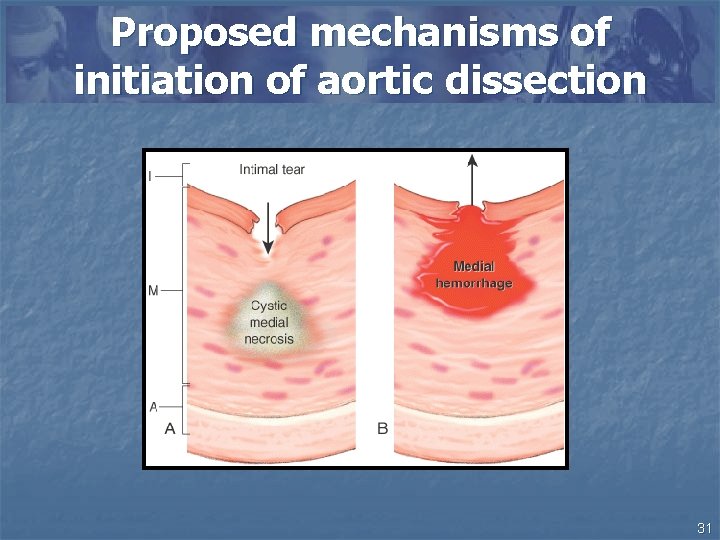
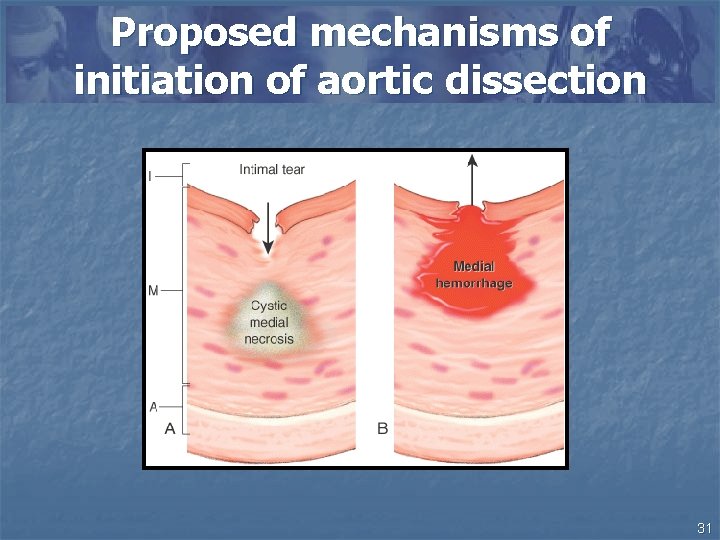
Proposed mechanisms of initiation of aortic dissection 31
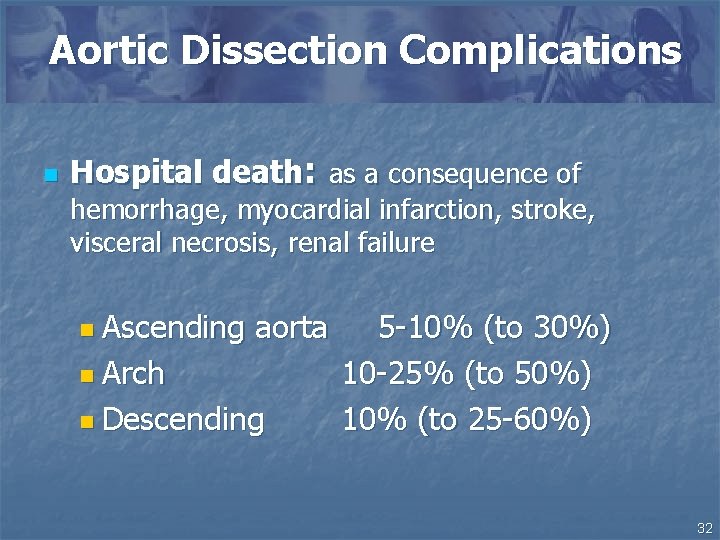
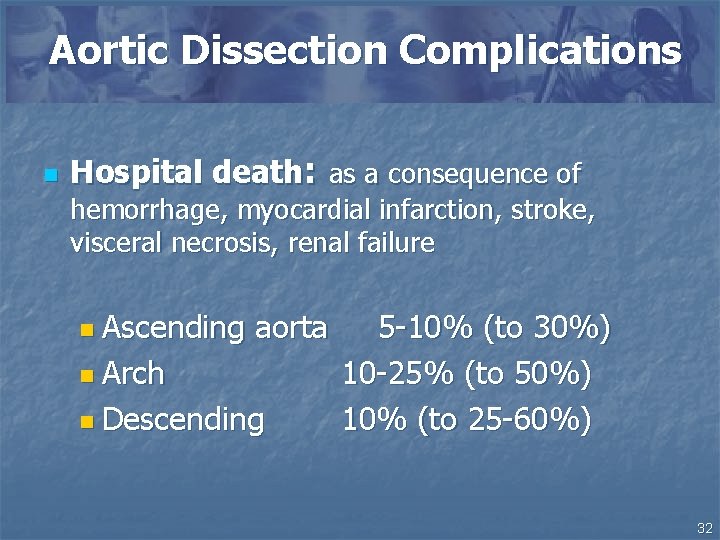
Aortic Dissection Complications n Hospital death: as a consequence of hemorrhage, myocardial infarction, stroke, visceral necrosis, renal failure n Ascending aorta n Arch n Descending 5 -10% (to 30%) 10 -25% (to 50%) 10% (to 25 -60%) 32
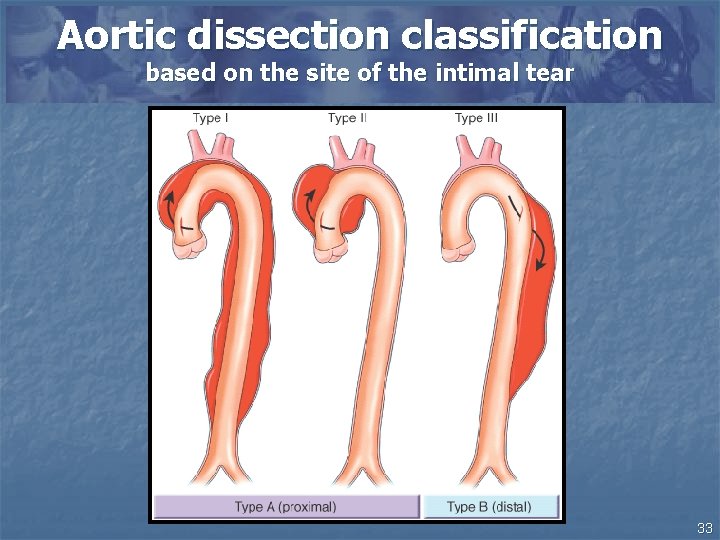
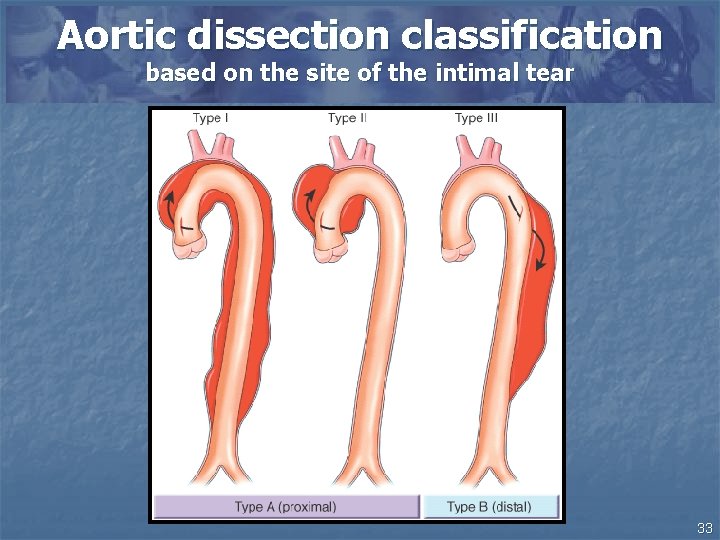
Aortic dissection classification based on the site of the intimal tear 33
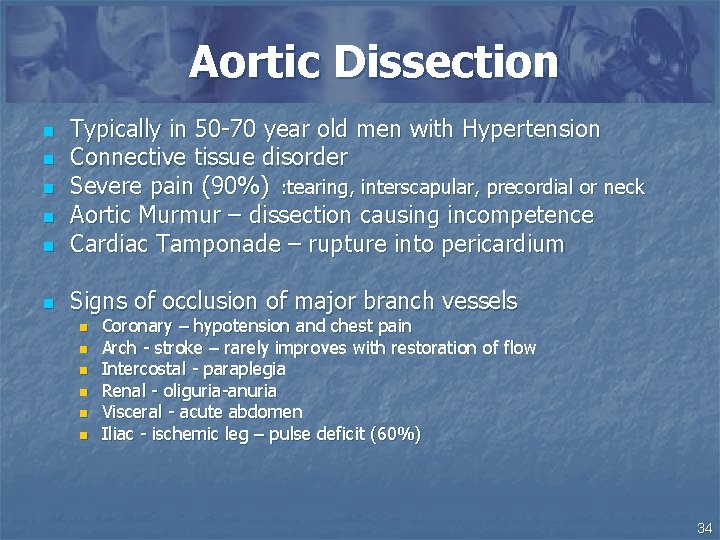
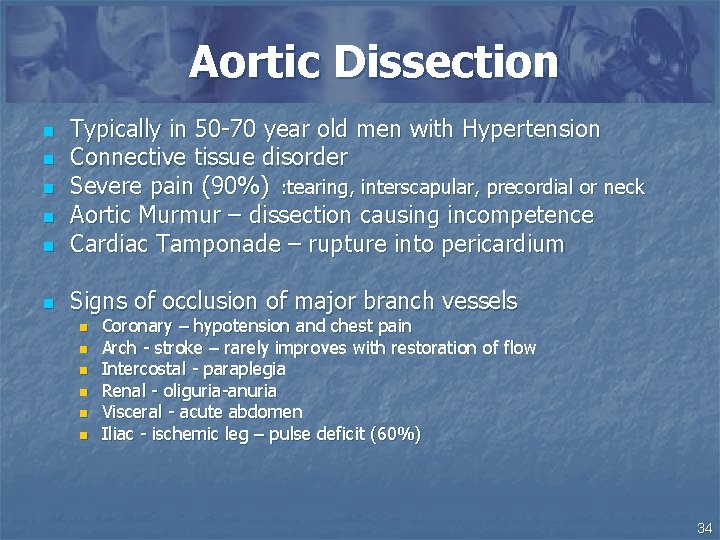
Aortic Dissection n Typically in 50 -70 year old men with Hypertension Connective tissue disorder Severe pain (90%) : tearing, interscapular, precordial or neck Aortic Murmur – dissection causing incompetence Cardiac Tamponade – rupture into pericardium n Signs of occlusion of major branch vessels n n n n n Coronary – hypotension and chest pain Arch - stroke – rarely improves with restoration of flow Intercostal - paraplegia Renal - oliguria-anuria Visceral - acute abdomen Iliac - ischemic leg – pulse deficit (60%) 34
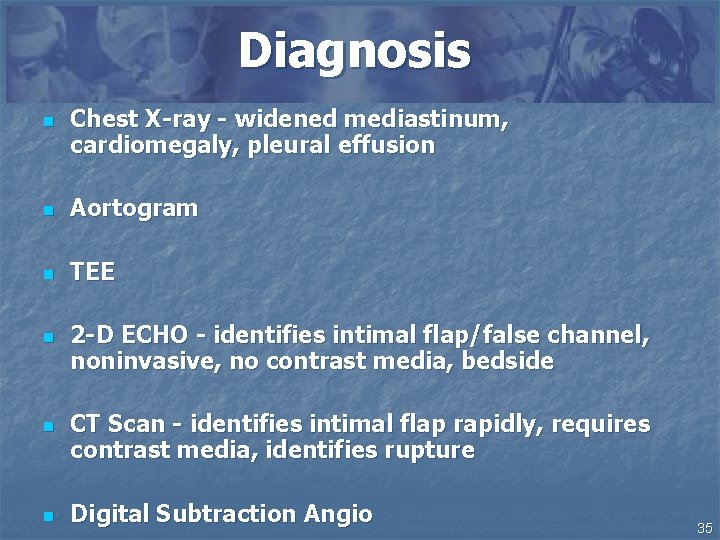
Diagnosis n Chest X-ray - widened mediastinum, cardiomegaly, pleural effusion n Aortogram n TEE n n n 2 -D ECHO - identifies intimal flap/false channel, noninvasive, no contrast media, bedside CT Scan - identifies intimal flap rapidly, requires contrast media, identifies rupture Digital Subtraction Angio 35

CXR Chest radiograph of a patient with aortic dissection. A, The patient's baseline study from 3 years prior to admission, with a normal-appearing aorta. B, The chest radiograph upon admission, which is remarkable for the interval enlargement of the aortic knob (arrow). The patient was found to have a proximal aortic dissection 36
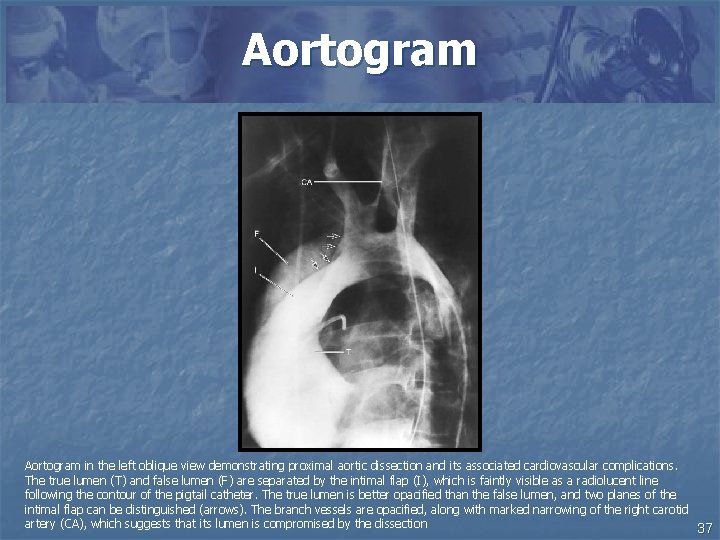
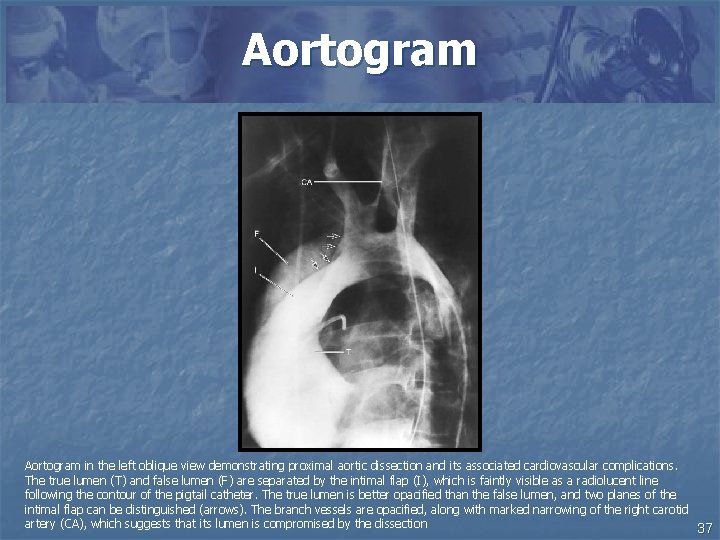
Aortogram in the left oblique view demonstrating proximal aortic dissection and its associated cardiovascular complications. The true lumen (T) and false lumen (F) are separated by the intimal flap (I), which is faintly visible as a radiolucent line following the contour of the pigtail catheter. The true lumen is better opacified than the false lumen, and two planes of the intimal flap can be distinguished (arrows). The branch vessels are opacified, along with marked narrowing of the right carotid artery (CA), which suggests that its lumen is compromised by the dissection 37
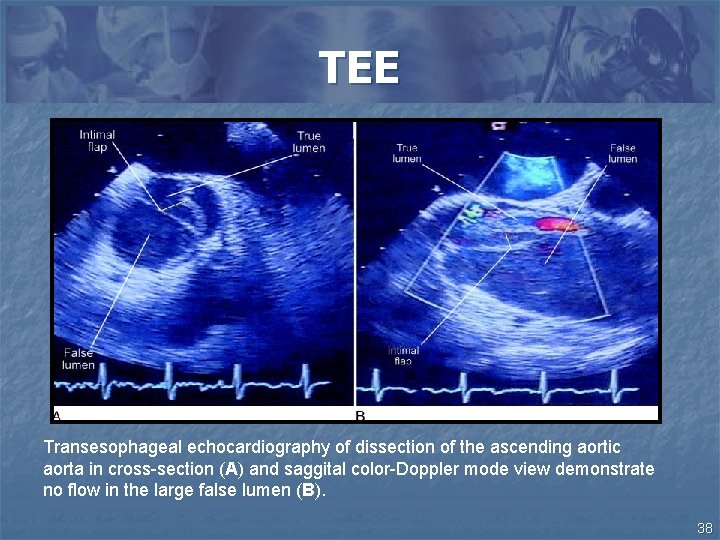
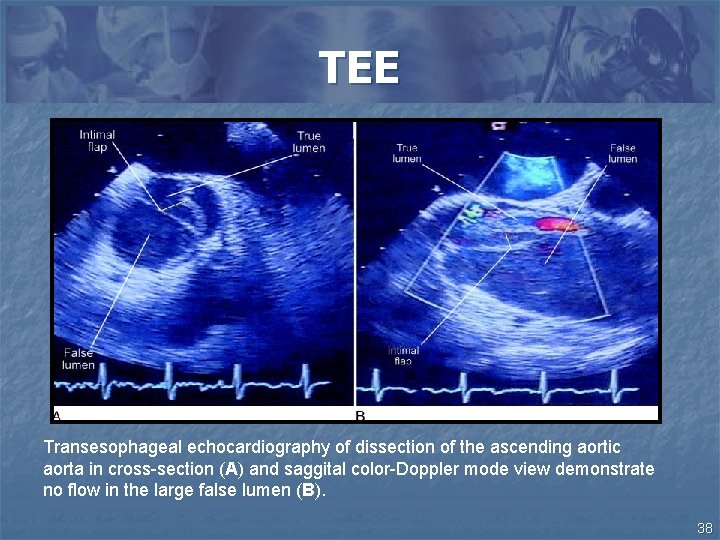
TEE Transesophageal echocardiography of dissection of the ascending aortic aorta in cross-section (A) and saggital color-Doppler mode view demonstrate no flow in the large false lumen (B). 38
2 D-ECHO 39
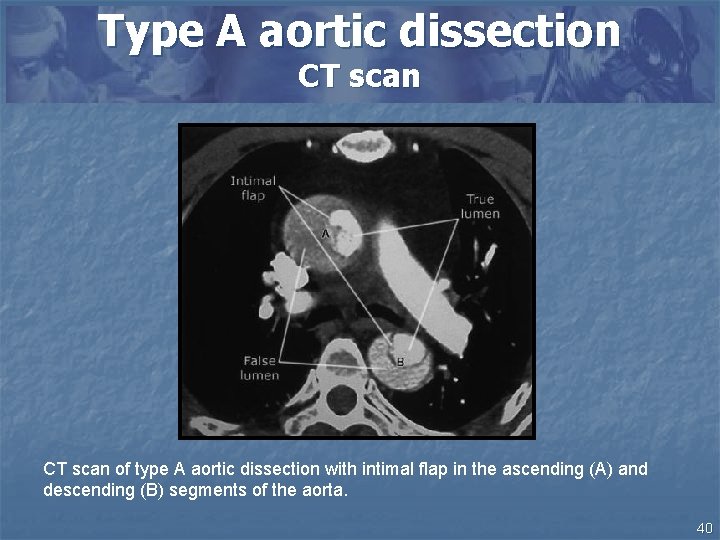
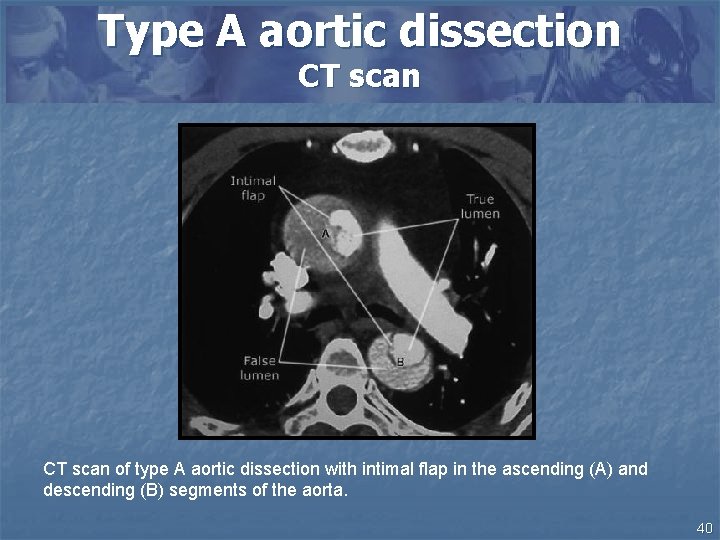
Type A aortic dissection CT scan of type A aortic dissection with intimal flap in the ascending (A) and descending (B) segments of the aorta. 40
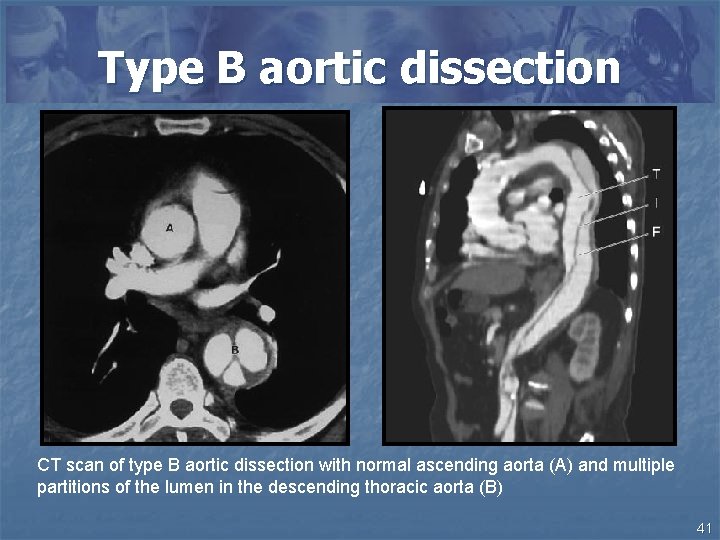
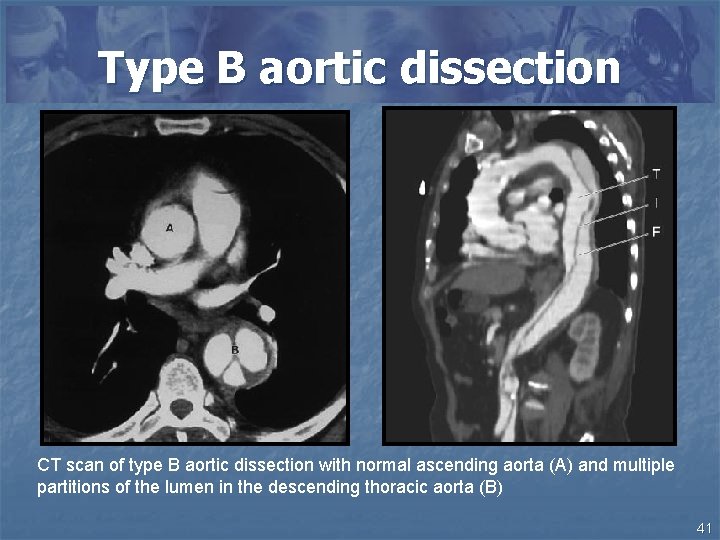
Type B aortic dissection CT scan of type B aortic dissection with normal ascending aorta (A) and multiple partitions of the lumen in the descending thoracic aorta (B) 41
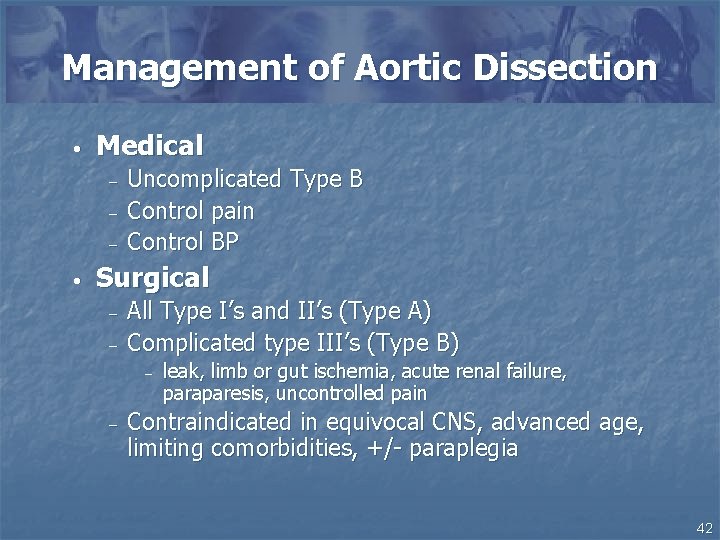
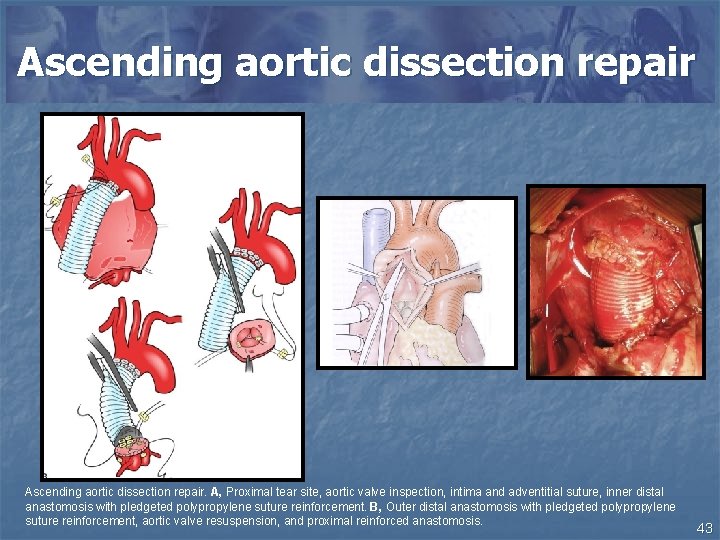
Management of Aortic Dissection • Medical – – – • Uncomplicated Type B Control pain Control BP Surgical – – All Type I’s and II’s (Type A) Complicated type III’s (Type B) – – leak, limb or gut ischemia, acute renal failure, paraparesis, uncontrolled pain Contraindicated in equivocal CNS, advanced age, limiting comorbidities, +/- paraplegia 42
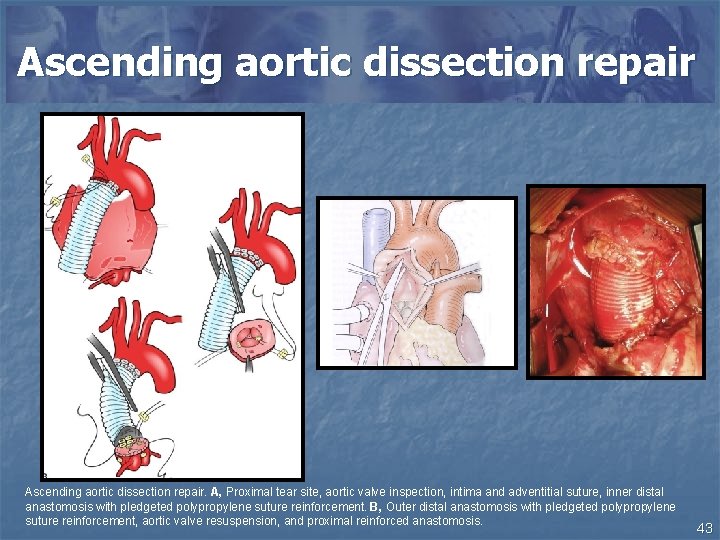
Ascending aortic dissection repair. A, Proximal tear site, aortic valve inspection, intima and adventitial suture, inner distal anastomosis with pledgeted polypropylene suture reinforcement. B, Outer distal anastomosis with pledgeted polypropylene suture reinforcement, aortic valve resuspension, and proximal reinforced anastomosis. 43