The Unhappy Hour Managing Critically Ill Patients in
![Pathophysiology of Withdrawal GABA Glutamate Upregulation Alcohol Withdrawal Crit Care Med. 2010; 38[Suppl. ]: Pathophysiology of Withdrawal GABA Glutamate Upregulation Alcohol Withdrawal Crit Care Med. 2010; 38[Suppl. ]:](https://slidetodoc.com/presentation_image_h/1f378f12a860125935f05d17348c773f/image-15.jpg)

- Slides: 44
The Unhappy Hour: Managing Critically Ill Patients in Alcohol Withdrawal Emily J. Owen, Pharm. D. , BCPS, BCCCP Surgical, Burn, Trauma ICU Clinical Pharmacist
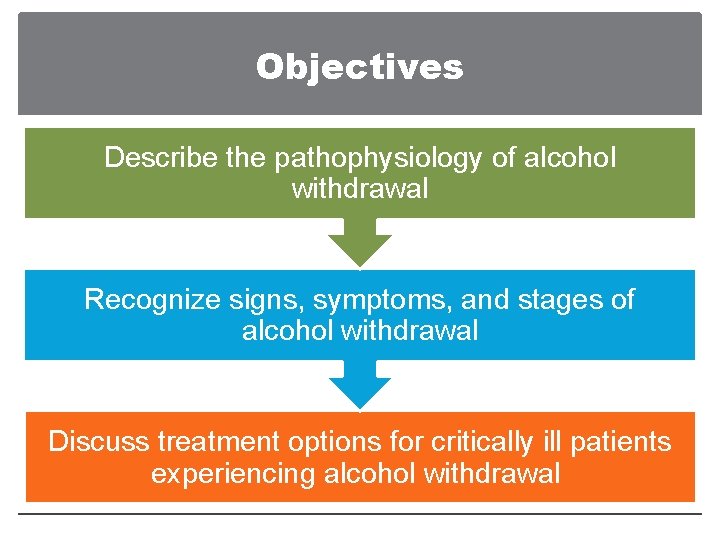
Objectives Describe the pathophysiology of alcohol withdrawal Recognize signs, symptoms, and stages of alcohol withdrawal Discuss treatment options for critically ill patients experiencing alcohol withdrawal
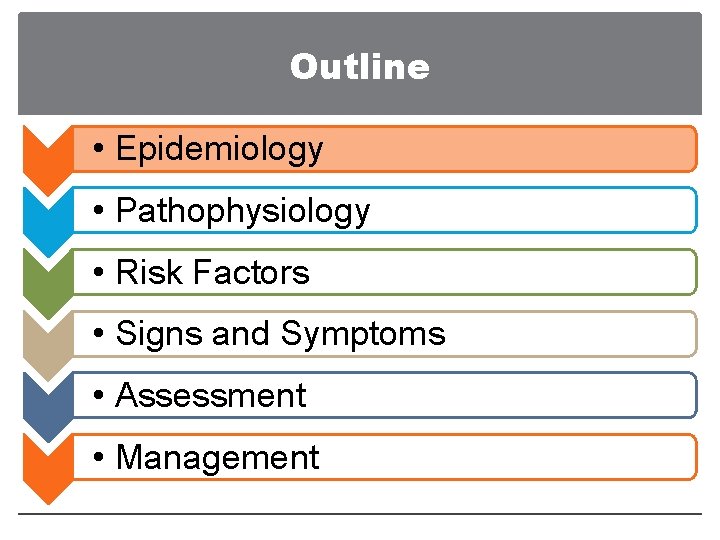
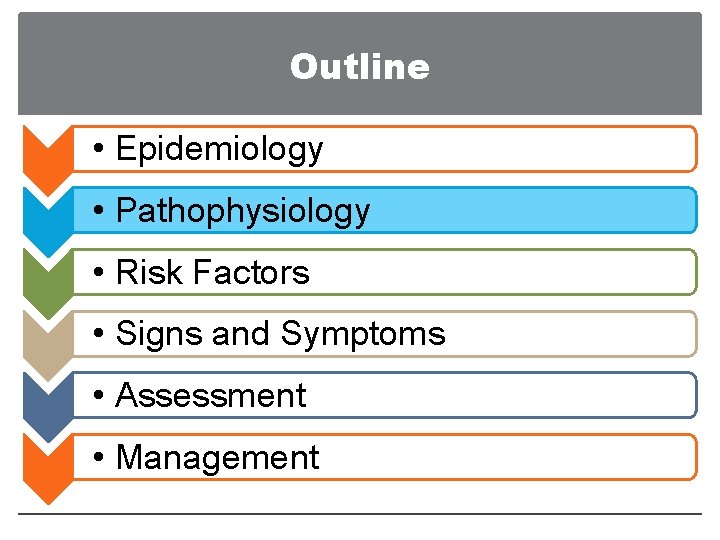
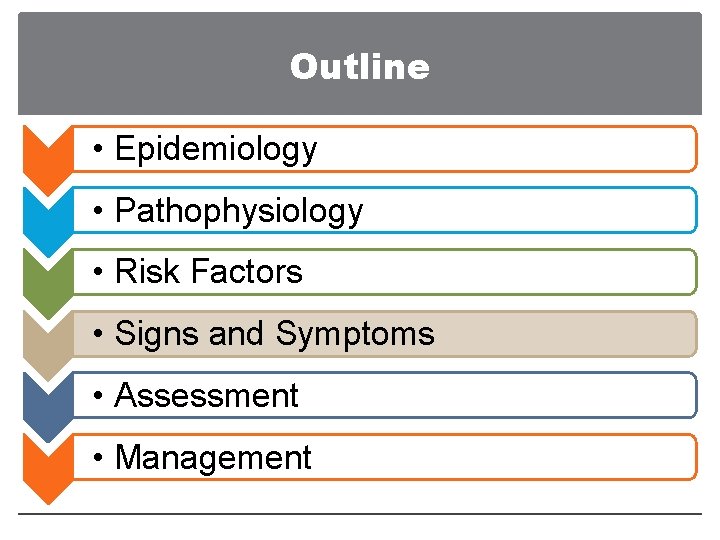
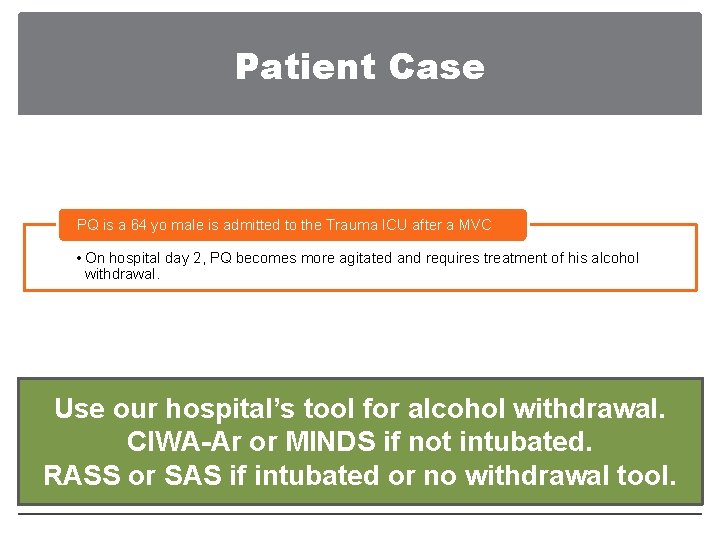
Outline • Epidemiology • Pathophysiology • Risk Factors • Signs and Symptoms • Assessment • Management
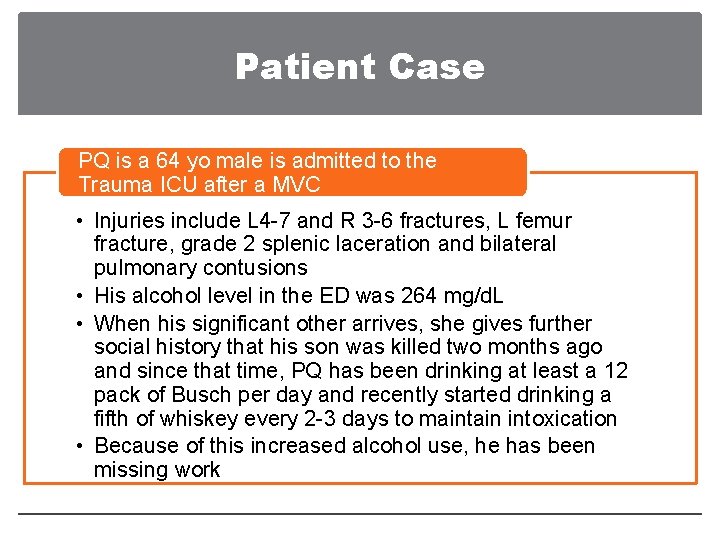
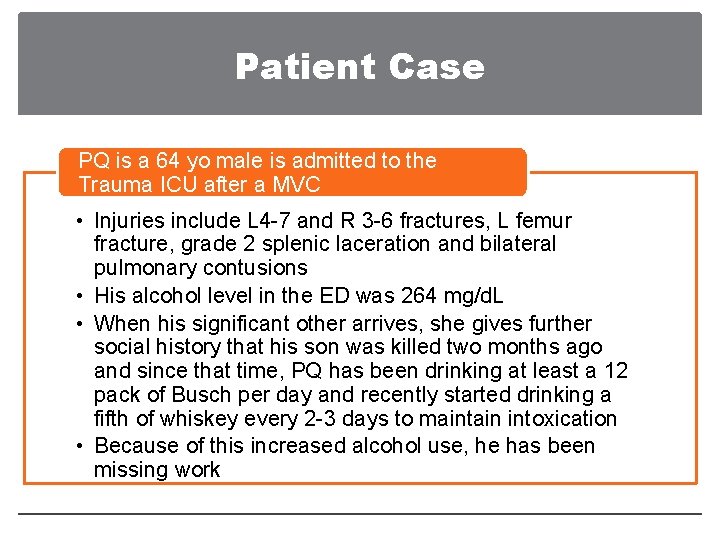
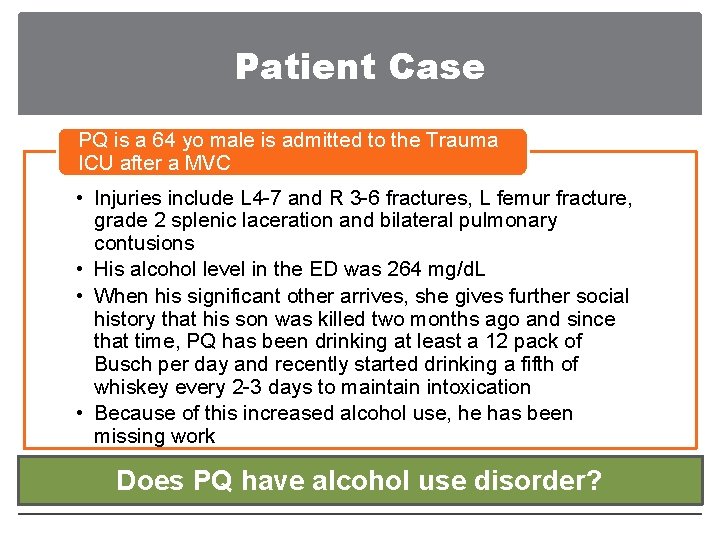
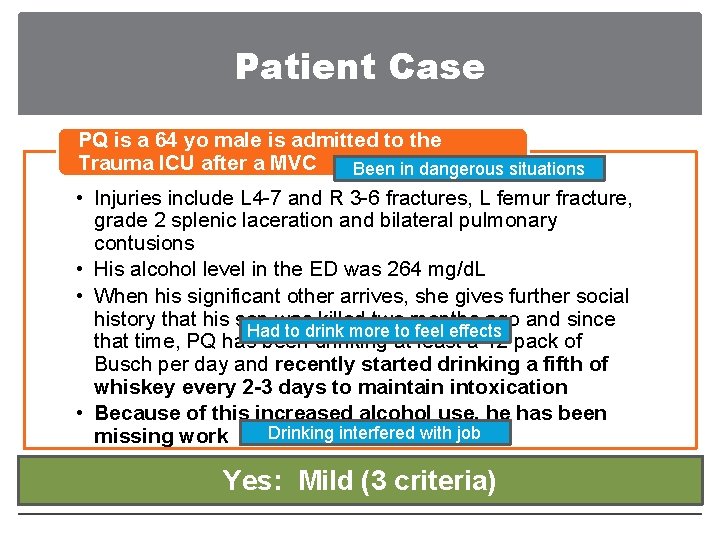
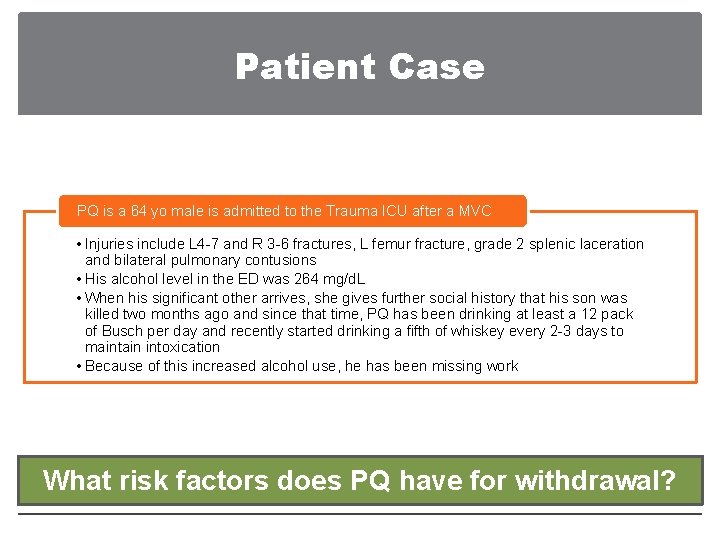
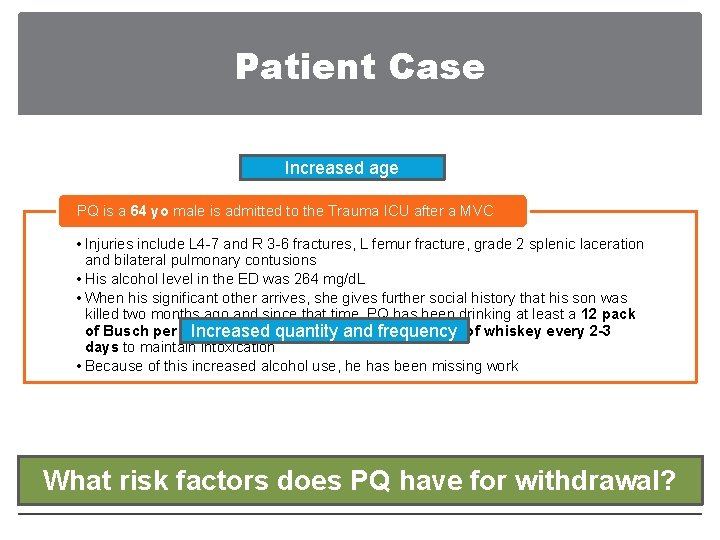
Patient Case PQ is a 64 yo male is admitted to the Trauma ICU after a MVC • Injuries include L 4 -7 and R 3 -6 fractures, L femur fracture, grade 2 splenic laceration and bilateral pulmonary contusions • His alcohol level in the ED was 264 mg/d. L • When his significant other arrives, she gives further social history that his son was killed two months ago and since that time, PQ has been drinking at least a 12 pack of Busch per day and recently started drinking a fifth of whiskey every 2 -3 days to maintain intoxication • Because of this increased alcohol use, he has been missing work
Outline • Epidemiology • Pathophysiology • Risk Factors • Signs and Symptoms • Assessment • Management
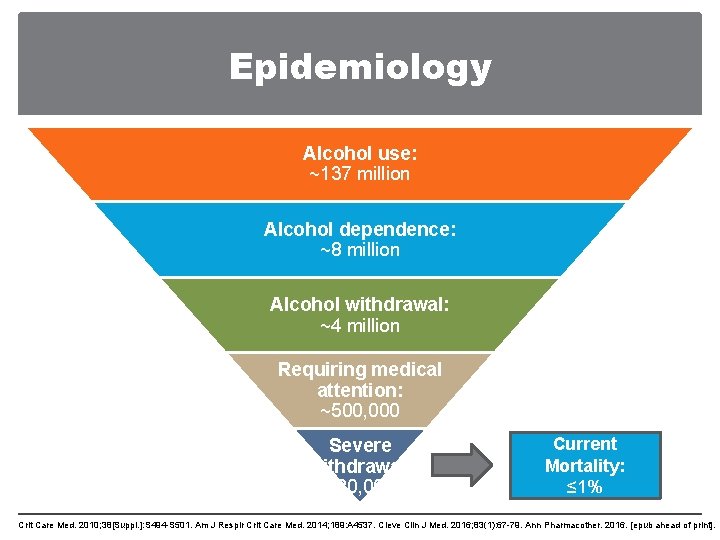
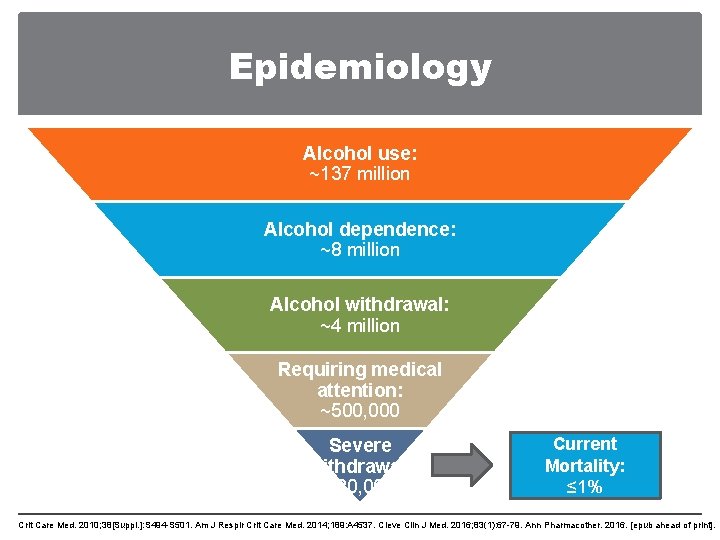
Epidemiology Alcohol use: ~137 million Alcohol dependence: ~8 million Alcohol withdrawal: ~4 million Requiring medical attention: ~500, 000 Severe withdrawal: ~20, 000 Historical Current Mortality: 15 -25% ≤ 1% Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Am J Respir Crit Care Med. 2014; 189: A 4537. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
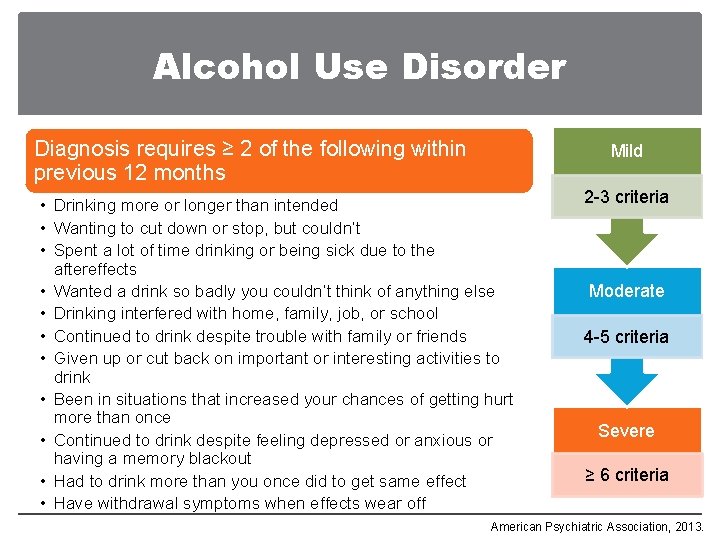
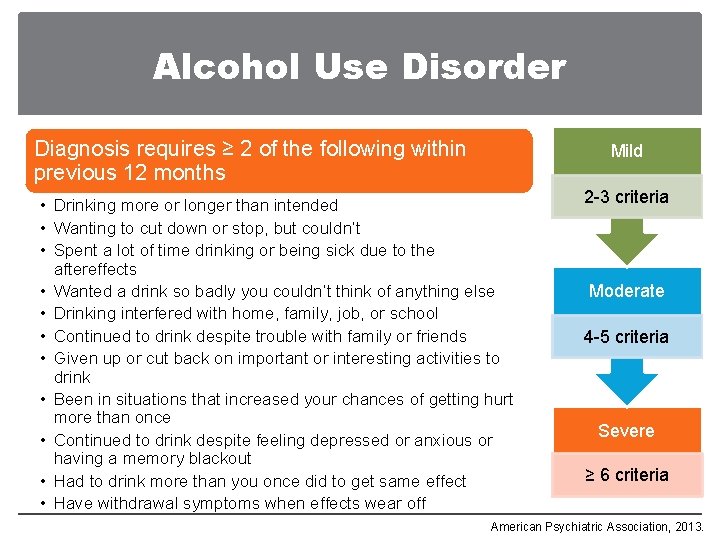
Alcohol Use Disorder Diagnosis requires ≥ 2 of the following within previous 12 months Mild • Drinking more or longer than intended • Wanting to cut down or stop, but couldn’t • Spent a lot of time drinking or being sick due to the aftereffects • Wanted a drink so badly you couldn’t think of anything else • Drinking interfered with home, family, job, or school • Continued to drink despite trouble with family or friends • Given up or cut back on important or interesting activities to drink • Been in situations that increased your chances of getting hurt more than once • Continued to drink despite feeling depressed or anxious or having a memory blackout • Had to drink more than you once did to get same effect • Have withdrawal symptoms when effects wear off 2 -3 criteria Moderate 4 -5 criteria Severe ≥ 6 criteria American Psychiatric Association, 2013.
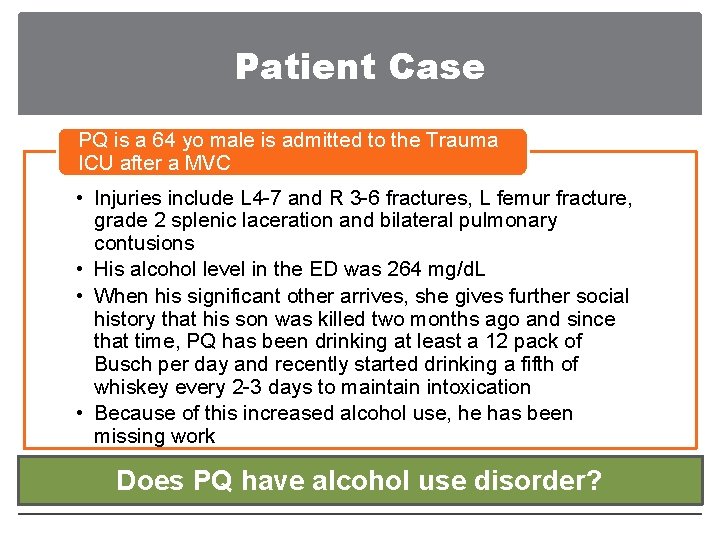
Patient Case PQ is a 64 yo male is admitted to the Trauma ICU after a MVC • Injuries include L 4 -7 and R 3 -6 fractures, L femur fracture, grade 2 splenic laceration and bilateral pulmonary contusions • His alcohol level in the ED was 264 mg/d. L • When his significant other arrives, she gives further social history that his son was killed two months ago and since that time, PQ has been drinking at least a 12 pack of Busch per day and recently started drinking a fifth of whiskey every 2 -3 days to maintain intoxication • Because of this increased alcohol use, he has been missing work Does PQ have alcohol use disorder?
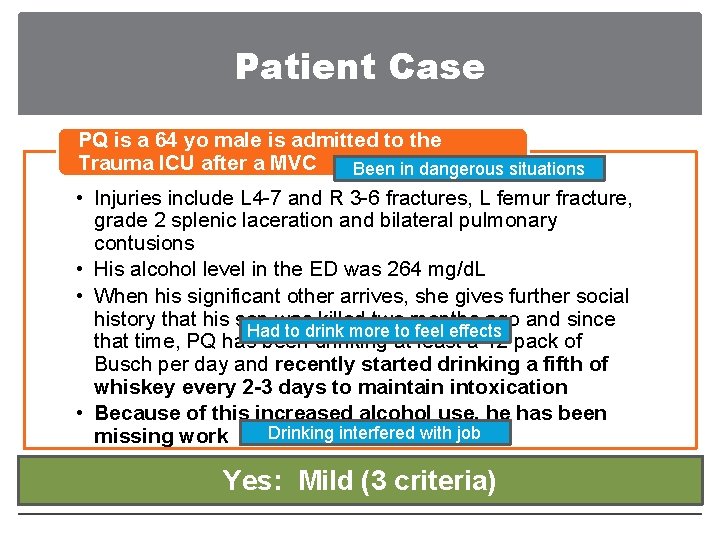
Patient Case PQ is a 64 yo male is admitted to the Trauma ICU after a MVC Been in dangerous situations • Injuries include L 4 -7 and R 3 -6 fractures, L femur fracture, grade 2 splenic laceration and bilateral pulmonary contusions • His alcohol level in the ED was 264 mg/d. L • When his significant other arrives, she gives further social history that his son was killed two months ago and since Had to drink more to feel effects that time, PQ has been drinking at least a 12 pack of Busch per day and recently started drinking a fifth of whiskey every 2 -3 days to maintain intoxication • Because of this increased alcohol use, he has been Drinking interfered with job missing work Does PQYes: have. Mild alcohol (3 criteria) use disorder?
Outline • Epidemiology • Pathophysiology • Risk Factors • Signs and Symptoms • Assessment • Management
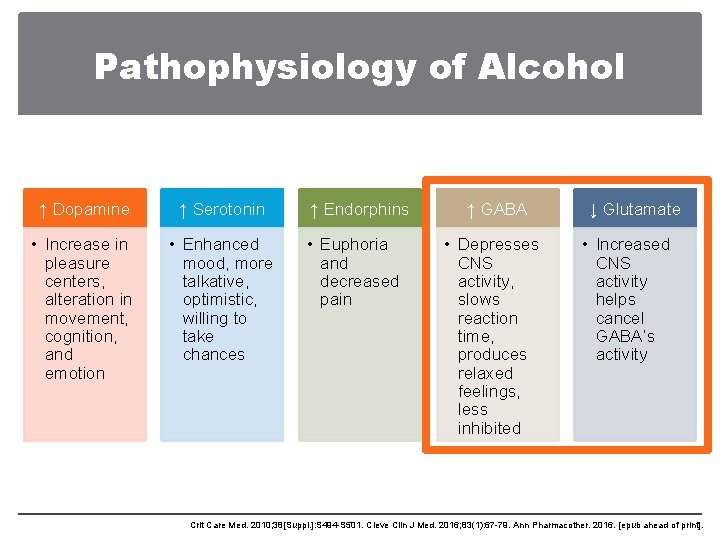
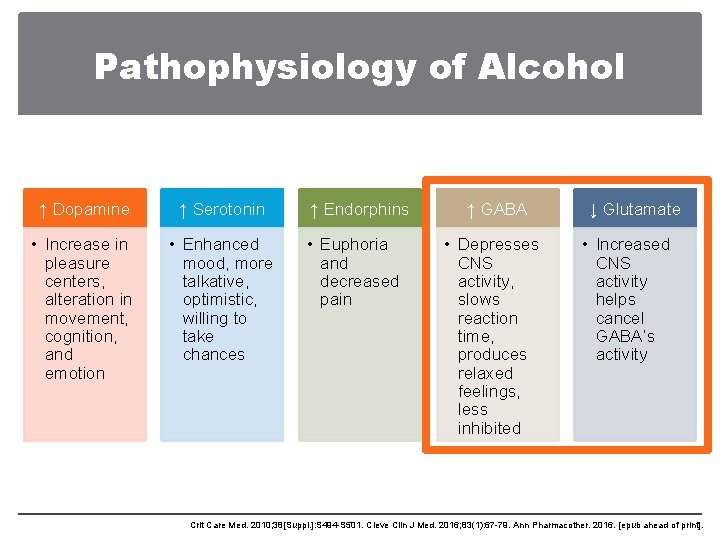
Pathophysiology of Alcohol ↑ Dopamine ↑ Serotonin ↑ Endorphins ↑ GABA • Increase in pleasure centers, alteration in movement, cognition, and emotion • Enhanced mood, more talkative, optimistic, willing to take chances • Euphoria and decreased pain • Depresses CNS activity, slows reaction time, produces relaxed feelings, less inhibited ↓ Glutamate • Increased CNS activity helps cancel GABA’s activity Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
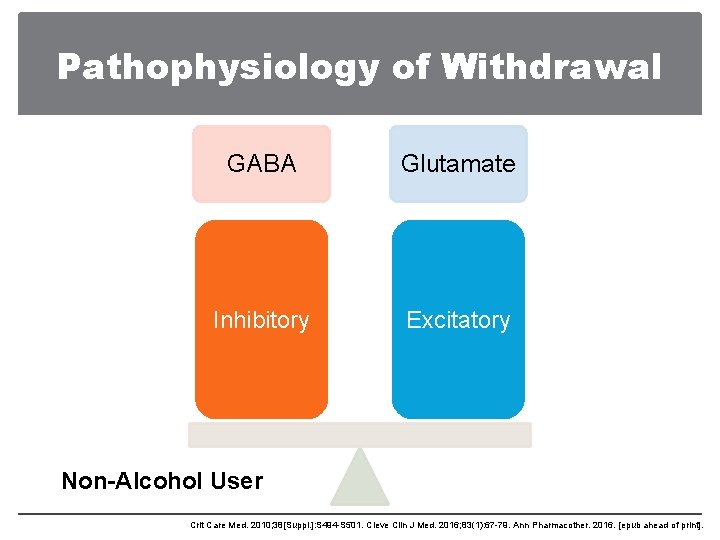
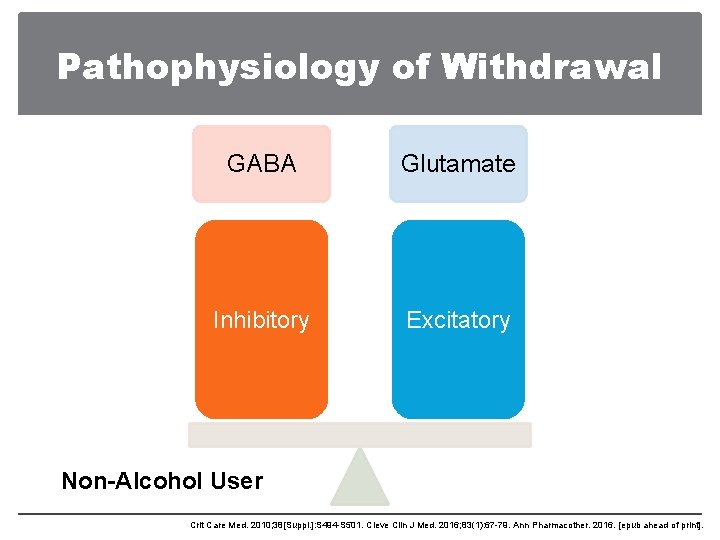
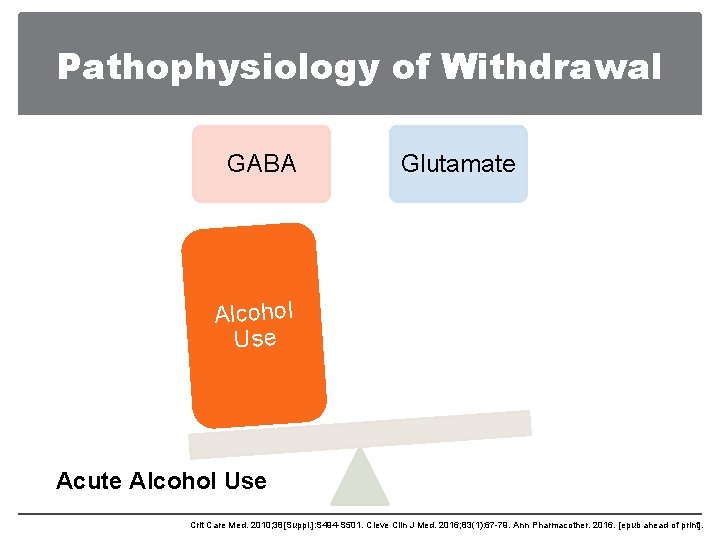
Pathophysiology of Withdrawal GABA Glutamate Inhibitory Excitatory Non-Alcohol User Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
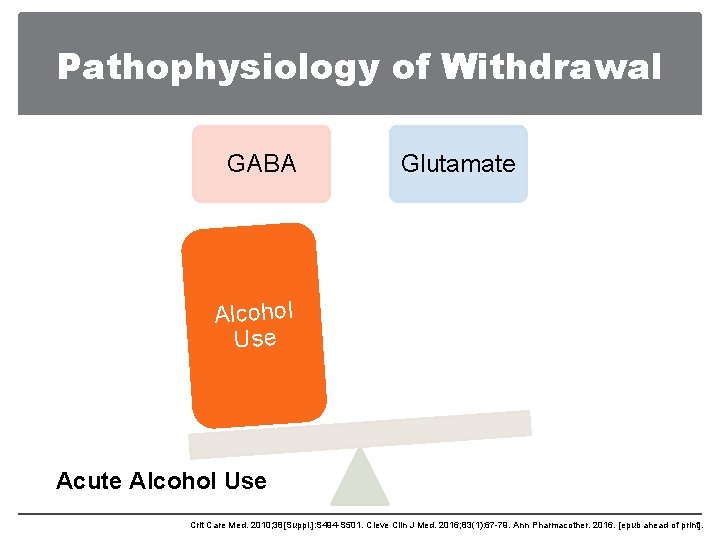
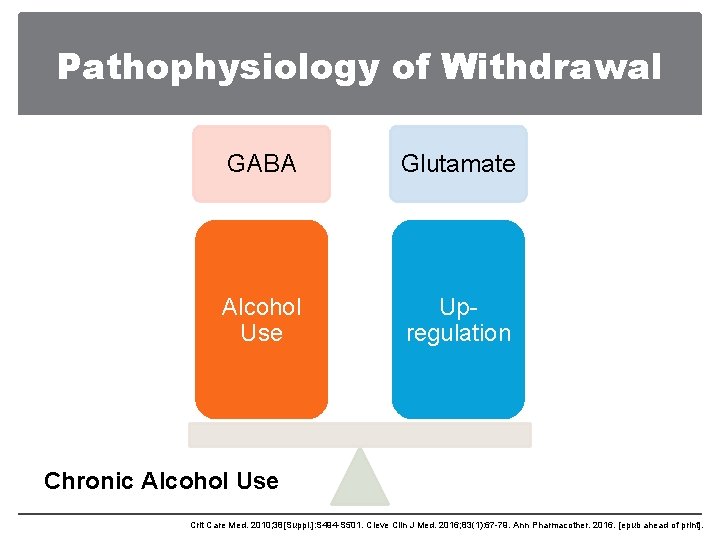
Pathophysiology of Withdrawal GABA Glutamate Alcohol Use Acute Alcohol Use Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
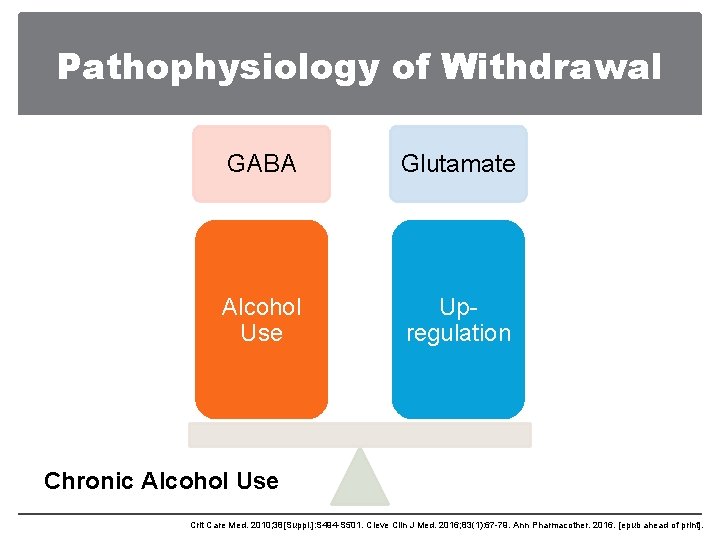
Pathophysiology of Withdrawal GABA Glutamate Alcohol Use Upregulation Chronic Alcohol Use Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
![Pathophysiology of Withdrawal GABA Glutamate Upregulation Alcohol Withdrawal Crit Care Med 2010 38Suppl Pathophysiology of Withdrawal GABA Glutamate Upregulation Alcohol Withdrawal Crit Care Med. 2010; 38[Suppl. ]:](https://slidetodoc.com/presentation_image_h/1f378f12a860125935f05d17348c773f/image-15.jpg)
Pathophysiology of Withdrawal GABA Glutamate Upregulation Alcohol Withdrawal Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
Outline • Epidemiology • Pathophysiology • Risk Factors • Signs and Symptoms • Assessment • Management

Risk Factors Increased age Increased quantity and frequency of alcohol consumption (>8 drinks per day for multiple days) Past medical history of alcohol withdrawal or delirium tremens Family history of alcohol withdrawal Binge drinking pattern Increased severity of addiction Alcoholic liver disease Delay in hospitalization Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
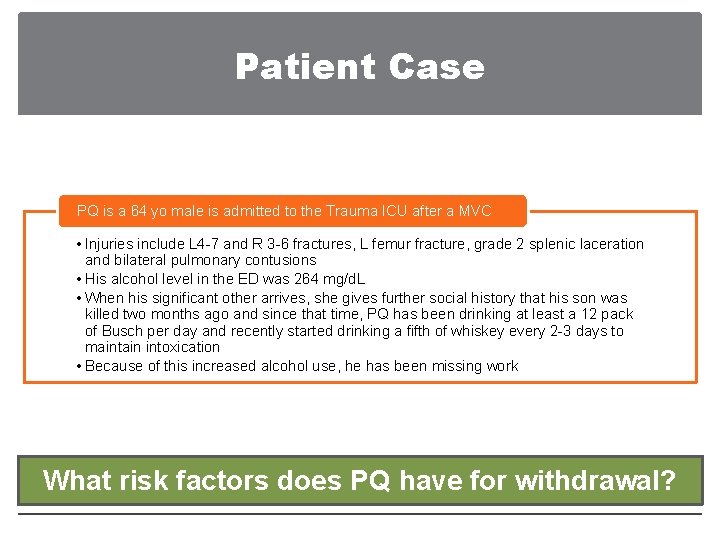
Patient Case PQ is a 64 yo male is admitted to the Trauma ICU after a MVC • Injuries include L 4 -7 and R 3 -6 fractures, L femur fracture, grade 2 splenic laceration and bilateral pulmonary contusions • His alcohol level in the ED was 264 mg/d. L • When his significant other arrives, she gives further social history that his son was killed two months ago and since that time, PQ has been drinking at least a 12 pack of Busch per day and recently started drinking a fifth of whiskey every 2 -3 days to maintain intoxication • Because of this increased alcohol use, he has been missing work What risk factors does PQ have for withdrawal?
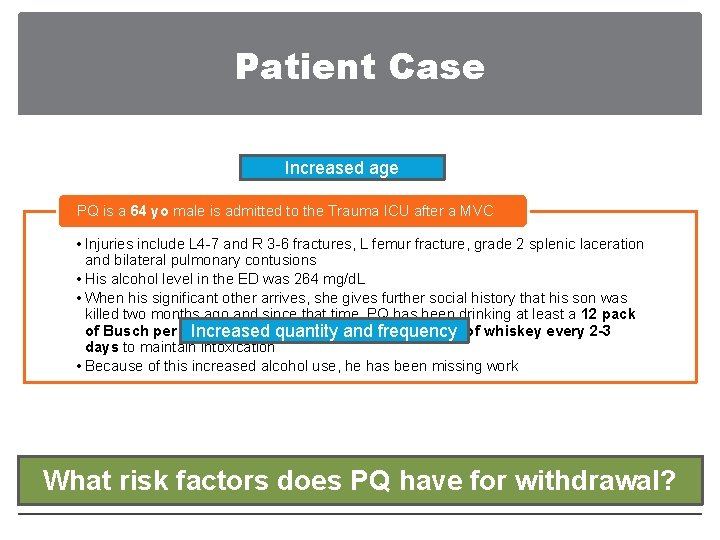
Patient Case Increased age PQ is a 64 yo male is admitted to the Trauma ICU after a MVC • Injuries include L 4 -7 and R 3 -6 fractures, L femur fracture, grade 2 splenic laceration and bilateral pulmonary contusions • His alcohol level in the ED was 264 mg/d. L • When his significant other arrives, she gives further social history that his son was killed two months ago and since that time, PQ has been drinking at least a 12 pack of Busch per day and recently started drinking a fifth of whiskey every 2 -3 Increased quantity and frequency days to maintain intoxication • Because of this increased alcohol use, he has been missing work What risk factors does PQ have for withdrawal?
Outline • Epidemiology • Pathophysiology • Risk Factors • Signs and Symptoms • Assessment • Management
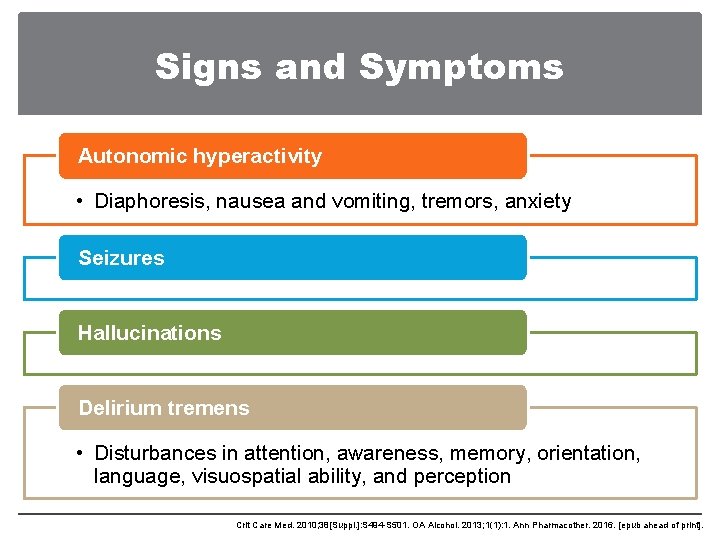
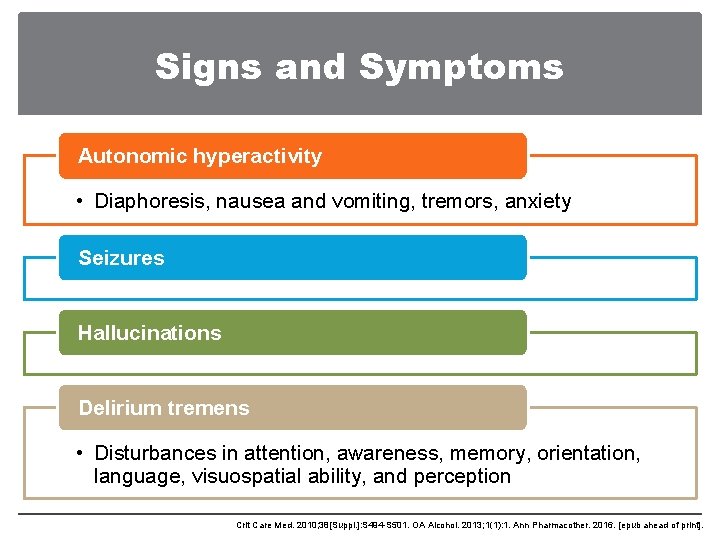
Signs and Symptoms Autonomic hyperactivity • Diaphoresis, nausea and vomiting, tremors, anxiety Seizures Hallucinations Delirium tremens • Disturbances in attention, awareness, memory, orientation, language, visuospatial ability, and perception Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. OA Alcohol. 2013; 1(1): 1. Ann Pharmacother. 2016. [epub ahead of print].
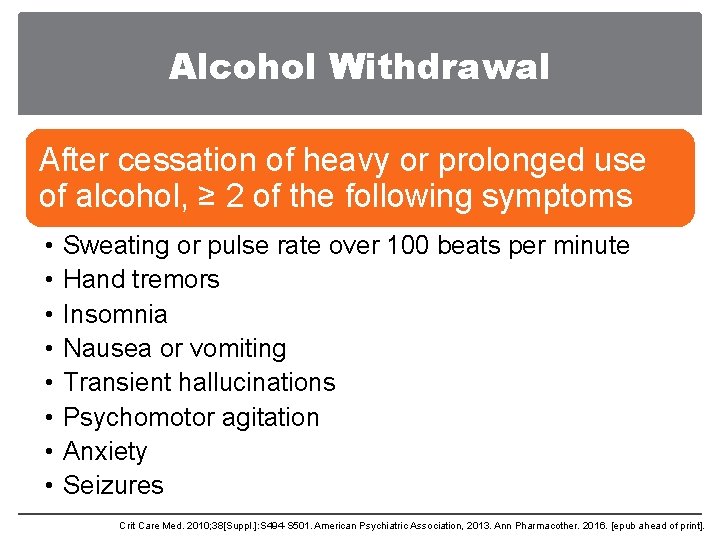
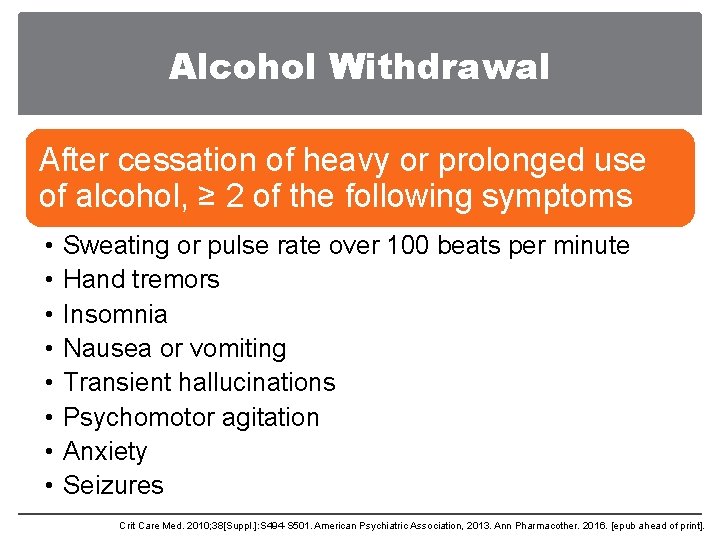
Alcohol Withdrawal After cessation of heavy or prolonged use of alcohol, ≥ 2 of the following symptoms • • Sweating or pulse rate over 100 beats per minute Hand tremors Insomnia Nausea or vomiting Transient hallucinations Psychomotor agitation Anxiety Seizures Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. American Psychiatric Association, 2013. Ann Pharmacother. 2016. [epub ahead of print].
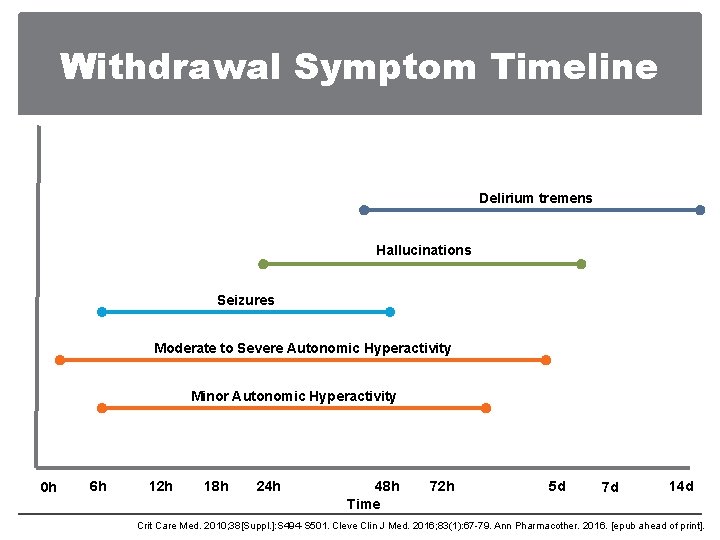
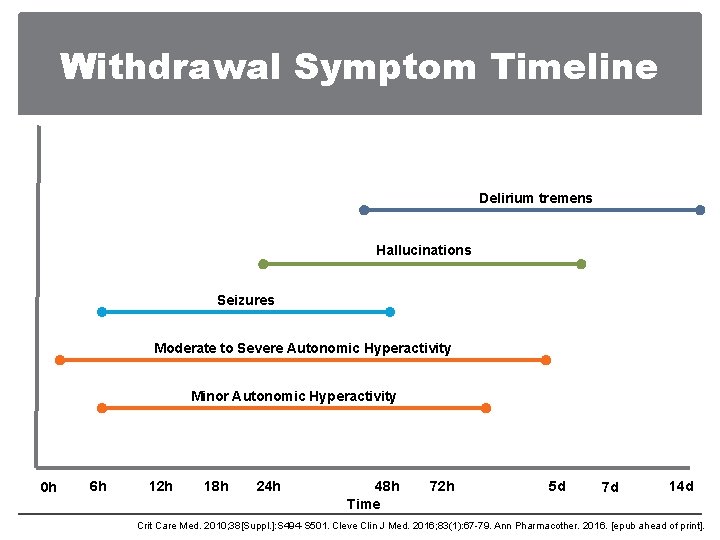
Withdrawal Symptom Timeline Delirium tremens Hallucinations Seizures Moderate to Severe Autonomic Hyperactivity Minor Autonomic Hyperactivity 0 h 6 h 12 h 18 h 24 h 48 h Time 72 h 5 d 7 d 14 d Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
Outline • Epidemiology • Pathophysiology • Risk Factors • Signs and Symptoms • Assessment • Management
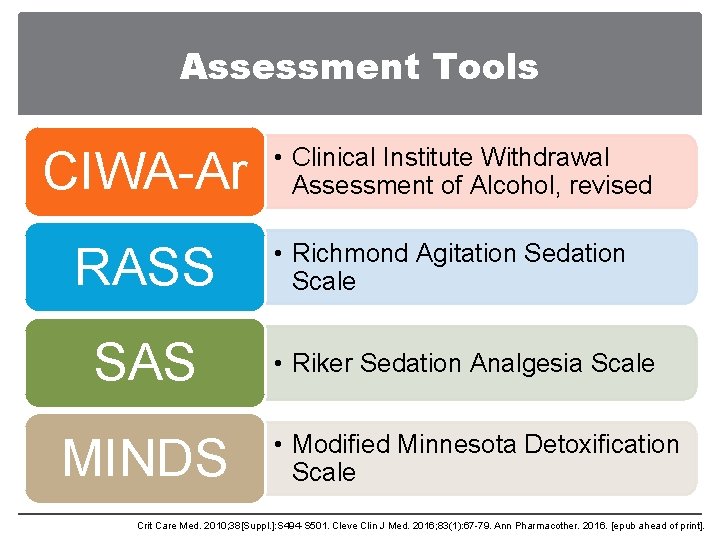
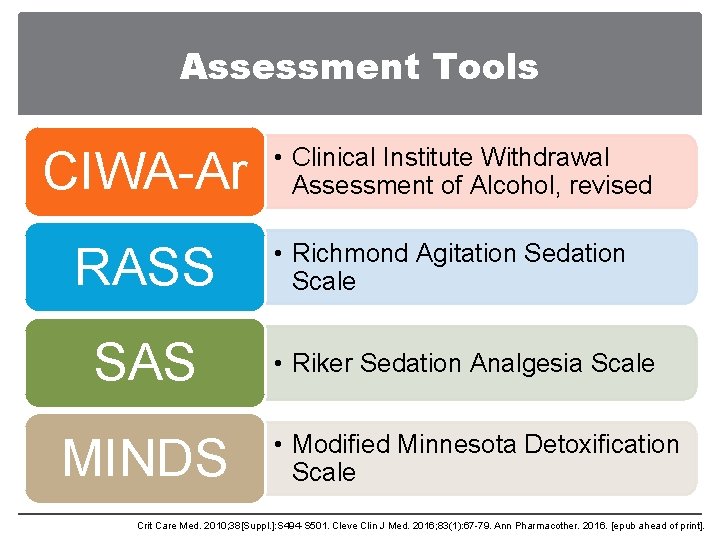
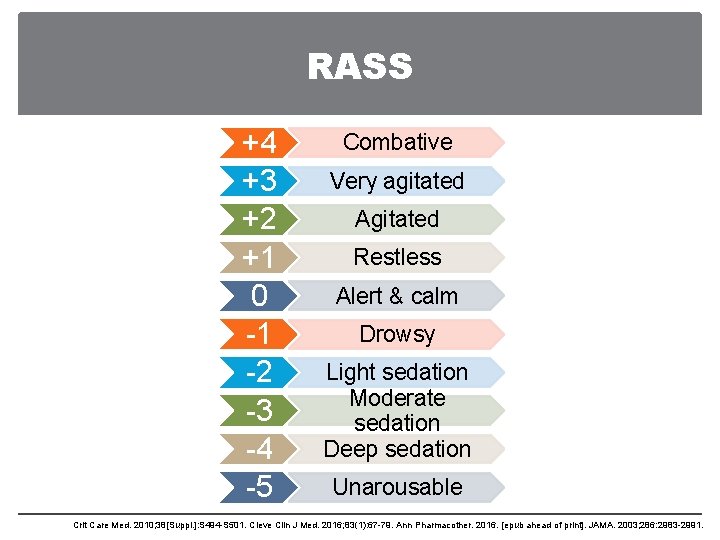
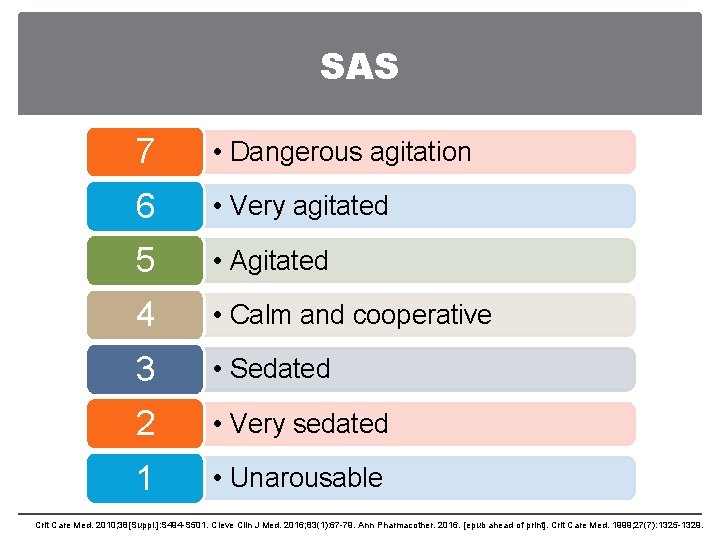
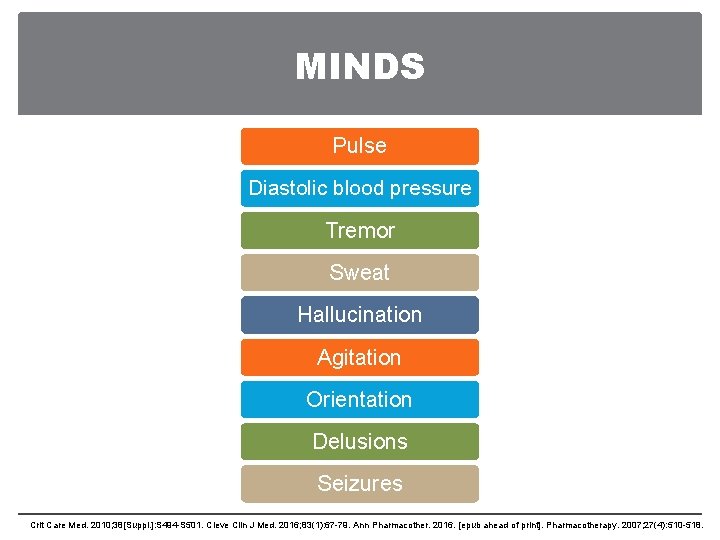
Assessment Tools CIWA-Ar RASS SAS MINDS • Clinical Institute Withdrawal Assessment of Alcohol, revised • Richmond Agitation Sedation Scale • Riker Sedation Analgesia Scale • Modified Minnesota Detoxification Scale Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
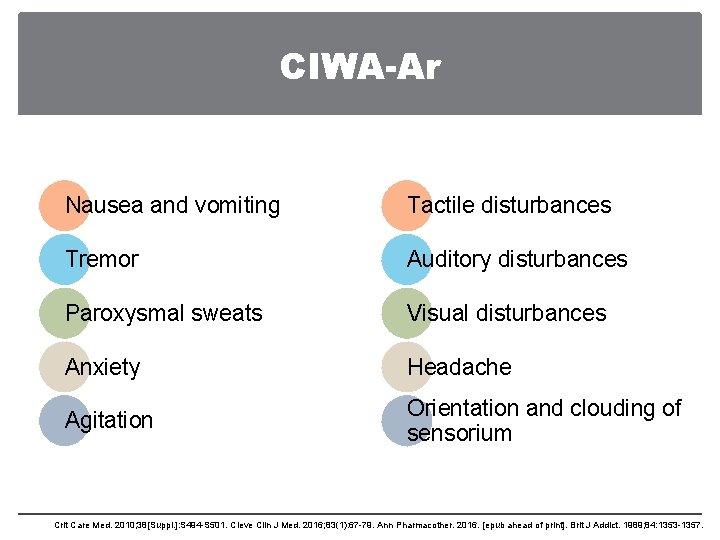
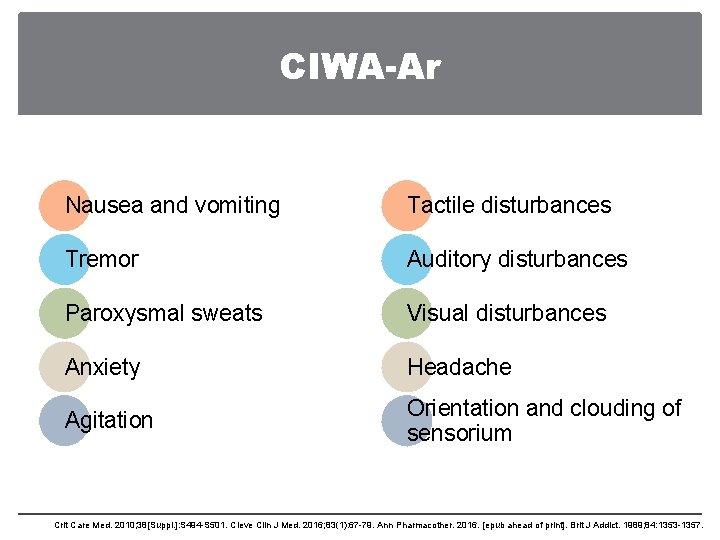
CIWA-Ar Nausea and vomiting Tactile disturbances Tremor Auditory disturbances Paroxysmal sweats Visual disturbances Anxiety Headache Agitation Orientation and clouding of sensorium Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print]. Brit J Addict. 1989; 84: 1353 -1357.
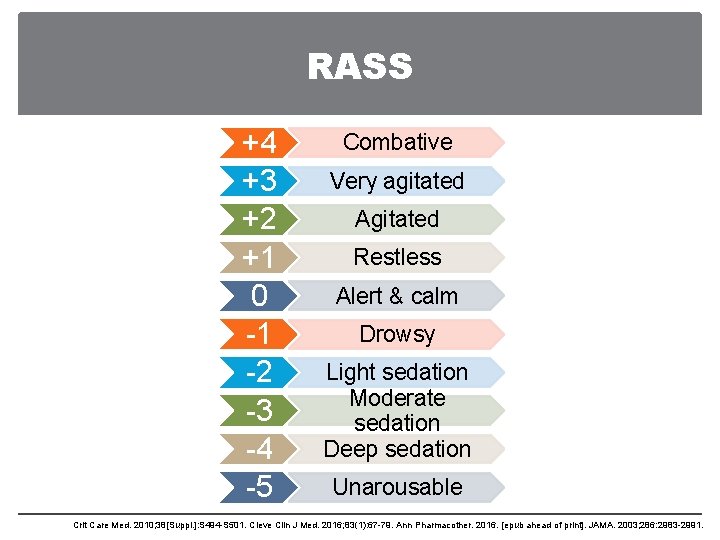
RASS +4 +3 +2 +1 0 -1 -2 -3 -4 -5 Combative Very agitated Agitated Restless Alert & calm Drowsy Light sedation Moderate sedation Deep sedation Unarousable Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print]. JAMA. 2003; 286: 2983 -2991.
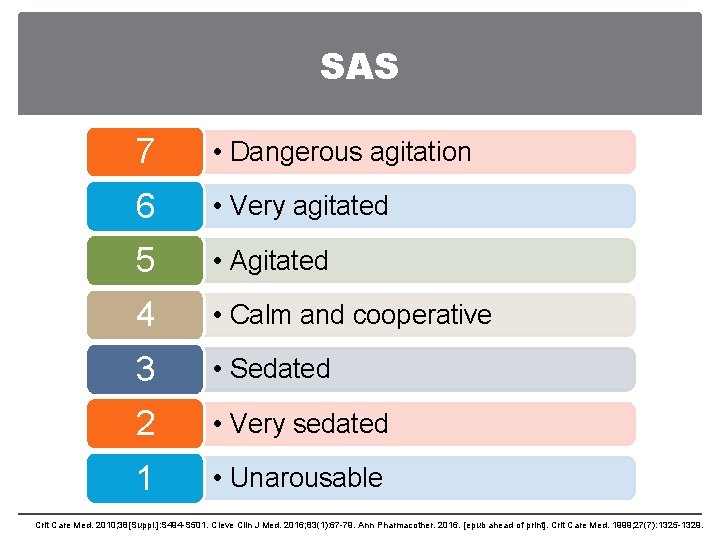
SAS 7 • Dangerous agitation 6 • Very agitated 5 • Agitated 4 • Calm and cooperative 3 • Sedated 2 • Very sedated 1 • Unarousable Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print]. Crit Care Med. 1999; 27(7): 1325 -1329.
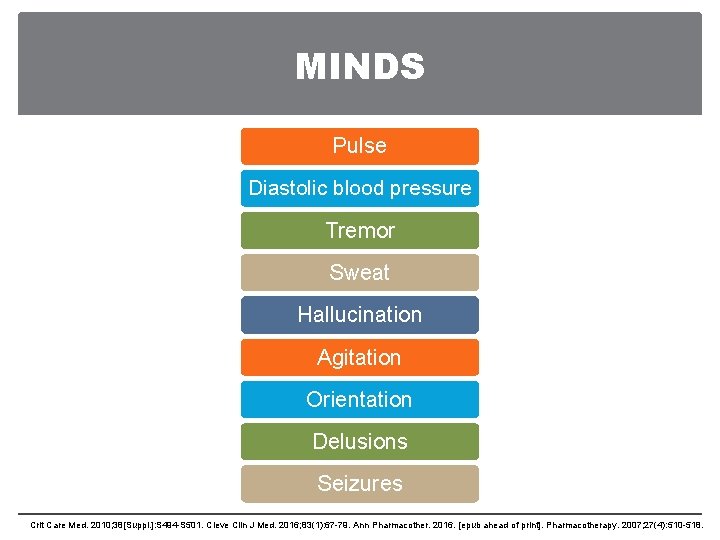
MINDS Pulse Diastolic blood pressure Tremor Sweat Hallucination Agitation Orientation Delusions Seizures Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print]. Pharmacotherapy. 2007; 27(4): 510 -518.
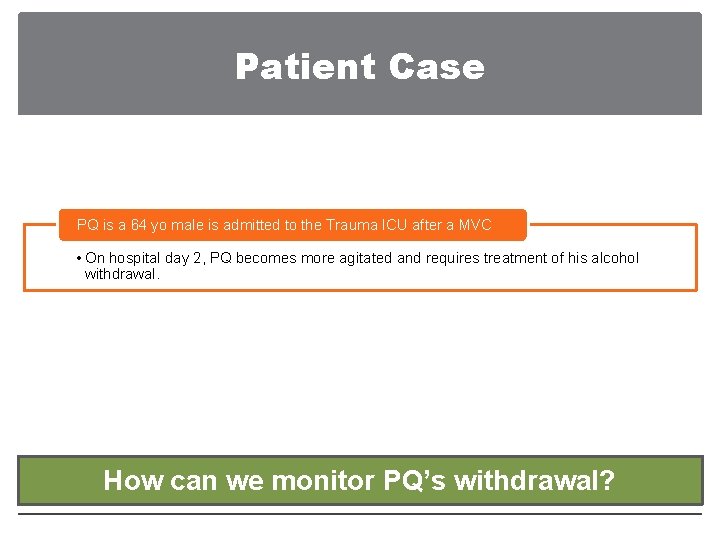
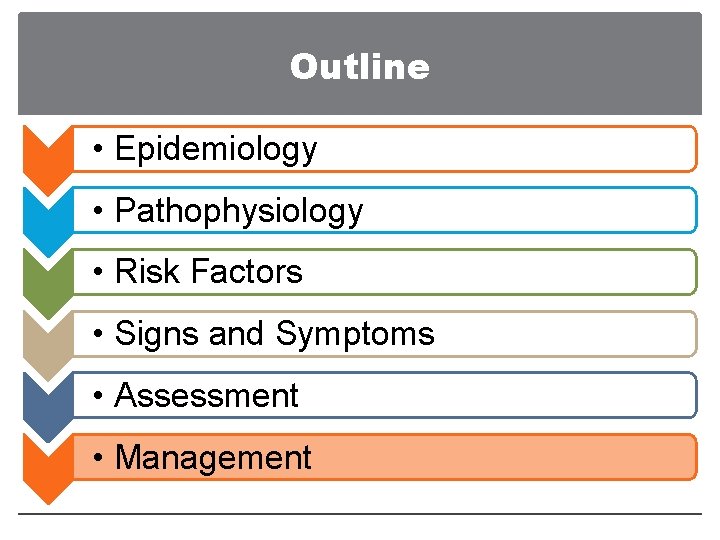
Patient Case PQ is a 64 yo male is admitted to the Trauma ICU after a MVC • On hospital day 2, PQ becomes more agitated and requires treatment of his alcohol withdrawal. How can we monitor PQ’s withdrawal?
Patient Case PQ is a 64 yo male is admitted to the Trauma ICU after a MVC • On hospital day 2, PQ becomes more agitated and requires treatment of his alcohol withdrawal. Use our hospital’s tool for alcohol withdrawal. CIWA-Ar or MINDS if not intubated. RASS or SAS if intubated or no withdrawal tool.
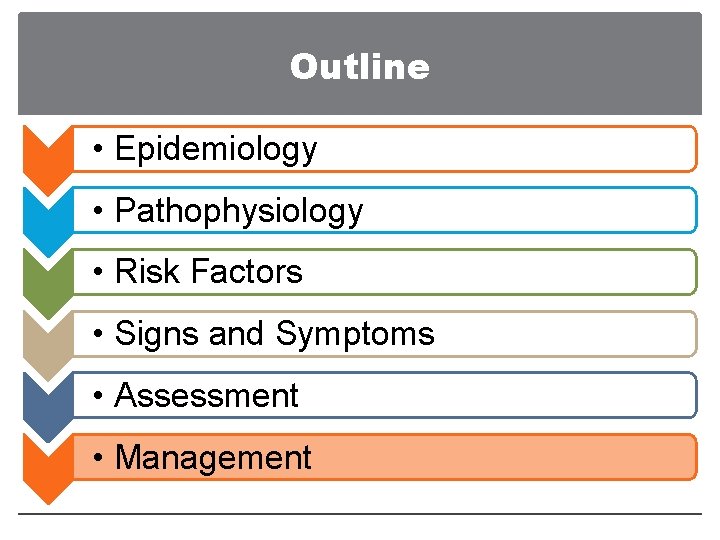
Outline • Epidemiology • Pathophysiology • Risk Factors • Signs and Symptoms • Assessment • Management
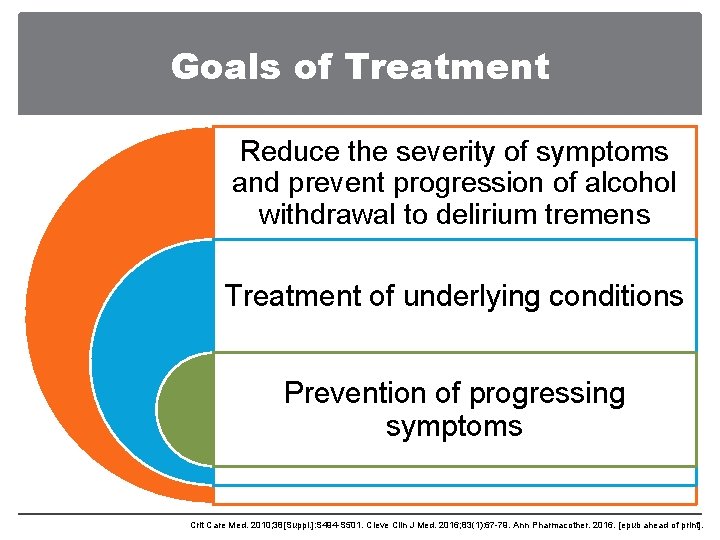
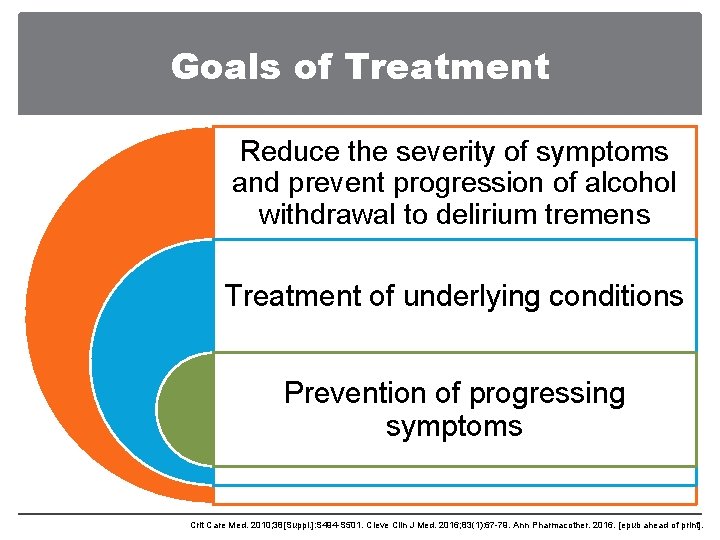
Goals of Treatment Reduce the severity of symptoms and prevent progression of alcohol withdrawal to delirium tremens Treatment of underlying conditions Prevention of progressing symptoms Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
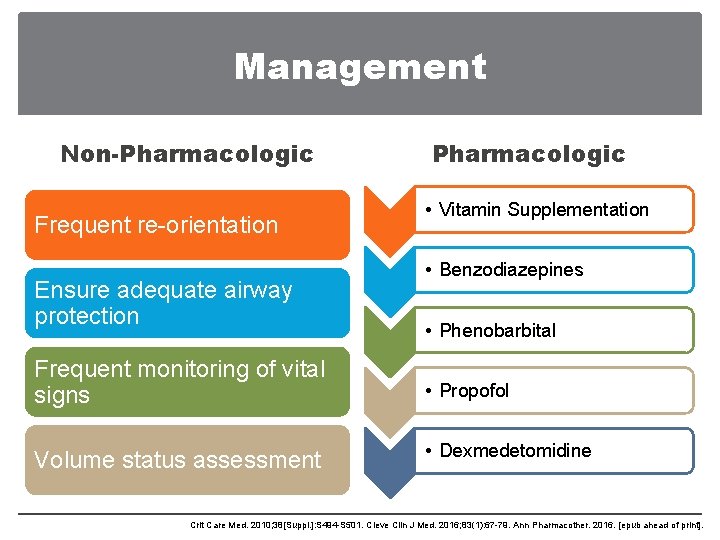
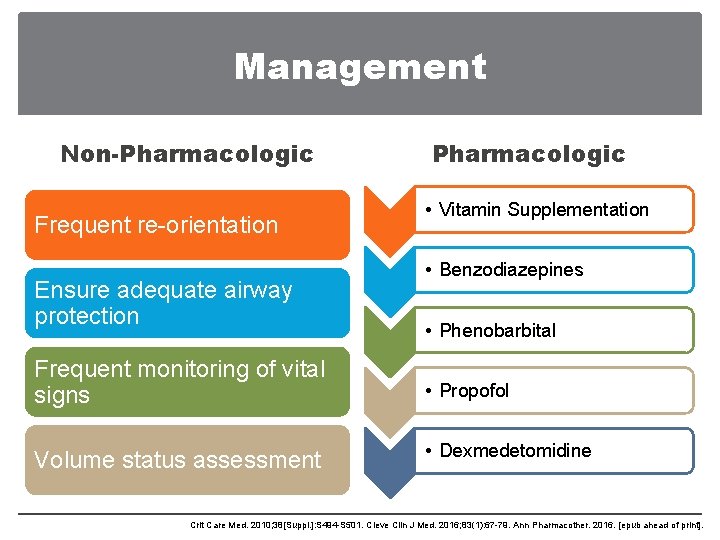
Management Non-Pharmacologic Frequent re-orientation Ensure adequate airway protection Pharmacologic • Vitamin Supplementation • Benzodiazepines • Phenobarbital Frequent monitoring of vital signs • Propofol Volume status assessment • Dexmedetomidine Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
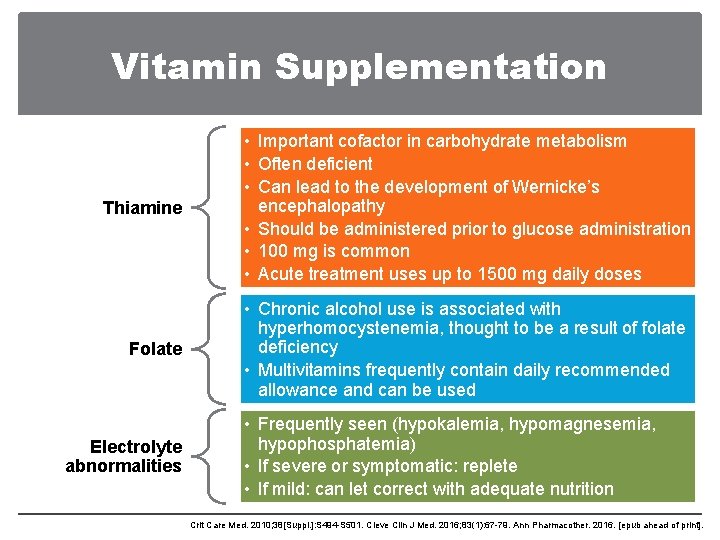
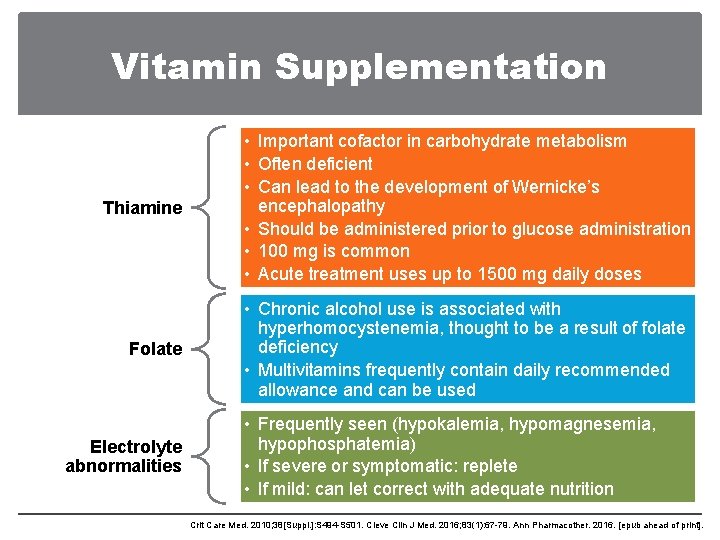
Vitamin Supplementation Thiamine • Important cofactor in carbohydrate metabolism • Often deficient • Can lead to the development of Wernicke’s encephalopathy • Should be administered prior to glucose administration • 100 mg is common • Acute treatment uses up to 1500 mg daily doses Folate • Chronic alcohol use is associated with hyperhomocystenemia, thought to be a result of folate deficiency • Multivitamins frequently contain daily recommended allowance and can be used Electrolyte abnormalities • Frequently seen (hypokalemia, hypomagnesemia, hypophosphatemia) • If severe or symptomatic: replete • If mild: can let correct with adequate nutrition Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
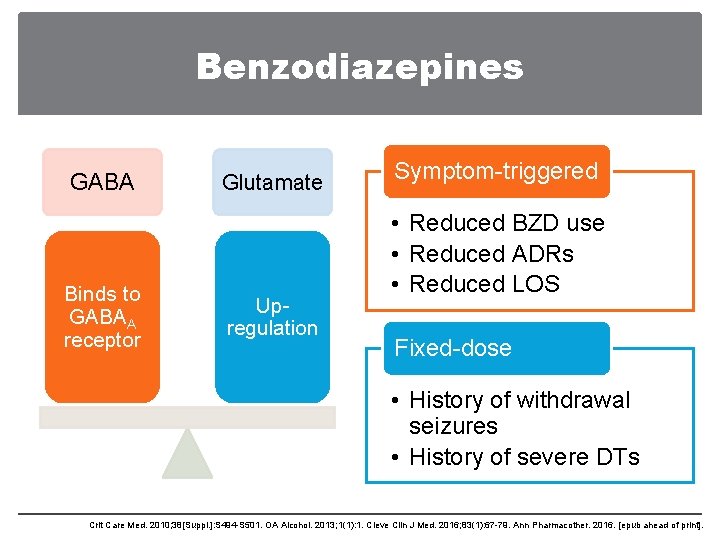
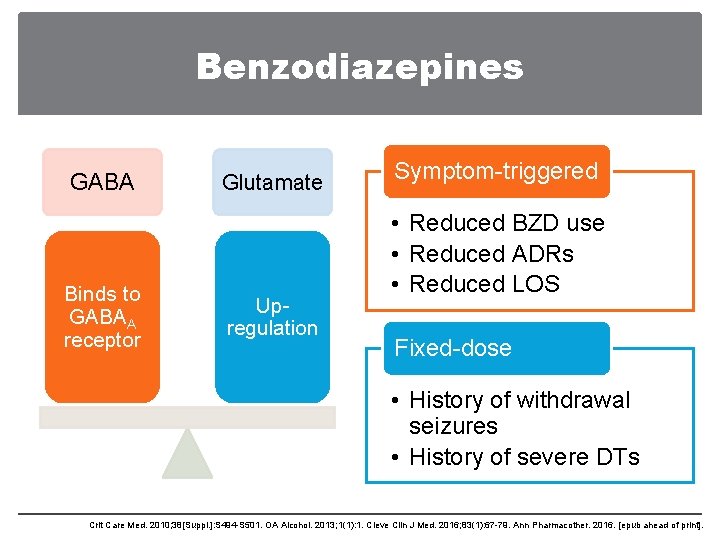
Benzodiazepines GABA Binds to GABAA receptor Glutamate Upregulation Symptom-triggered • Reduced BZD use • Reduced ADRs • Reduced LOS Fixed-dose • History of withdrawal seizures • History of severe DTs Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. OA Alcohol. 2013; 1(1): 1. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
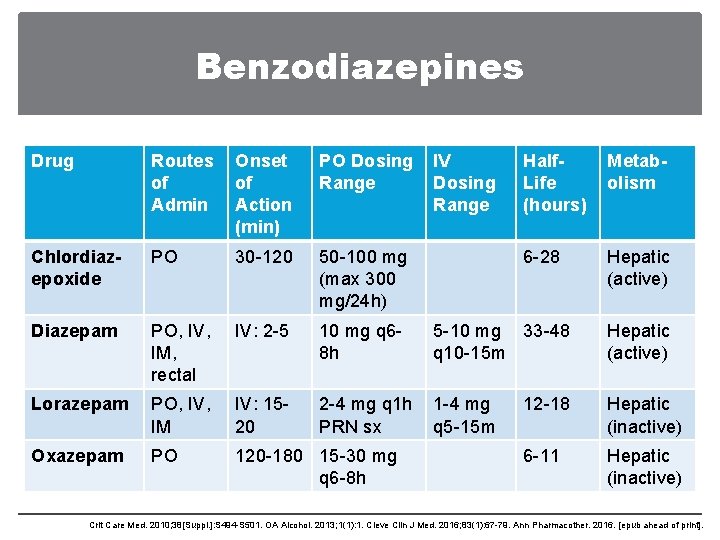
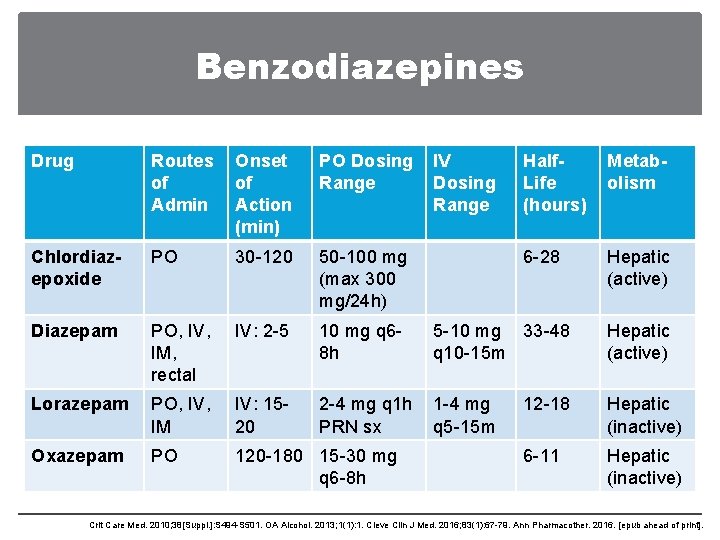
Benzodiazepines Drug Routes of Admin Onset of Action (min) PO Dosing Range IV Dosing Range Chlordiazepoxide PO 30 -120 50 -100 mg (max 300 mg/24 h) Diazepam PO, IV, IM, rectal IV: 2 -5 10 mg q 68 h Lorazepam PO, IV, IM IV: 1520 2 -4 mg q 1 h 1 -4 mg PRN sx q 5 -15 m Oxazepam PO 120 -180 15 -30 mg q 6 -8 h Half. Life (hours) Metabolism 6 -28 Hepatic (active) 5 -10 mg 33 -48 q 10 -15 m Hepatic (active) 12 -18 Hepatic (inactive) 6 -11 Hepatic (inactive) Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. OA Alcohol. 2013; 1(1): 1. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
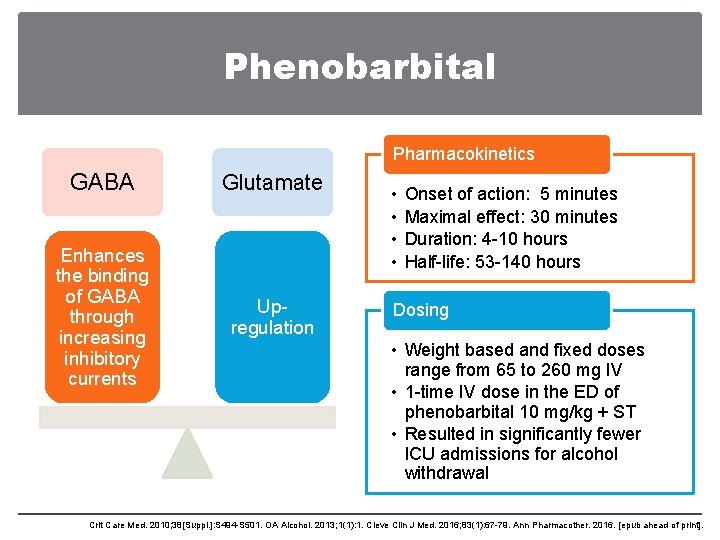
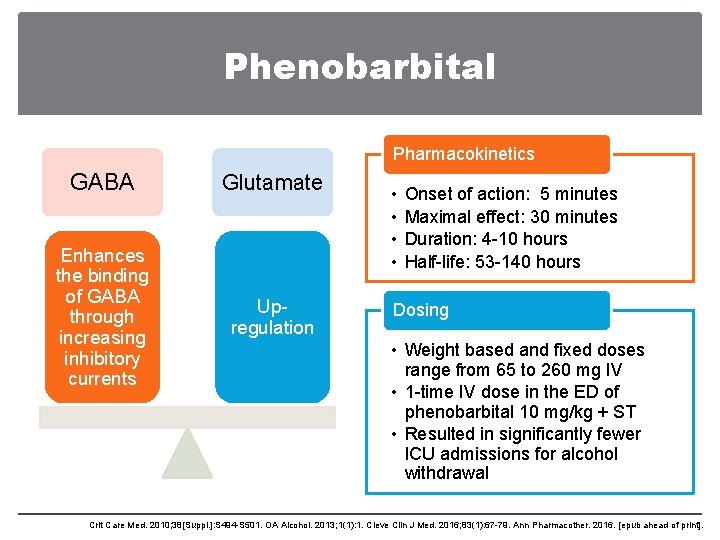
Phenobarbital Pharmacokinetics GABA Glutamate Enhances the binding of GABA through increasing inhibitory currents Upregulation • • Onset of action: 5 minutes Maximal effect: 30 minutes Duration: 4 -10 hours Half-life: 53 -140 hours Dosing • Weight based and fixed doses range from 65 to 260 mg IV • 1 -time IV dose in the ED of phenobarbital 10 mg/kg + ST • Resulted in significantly fewer ICU admissions for alcohol withdrawal Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. OA Alcohol. 2013; 1(1): 1. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
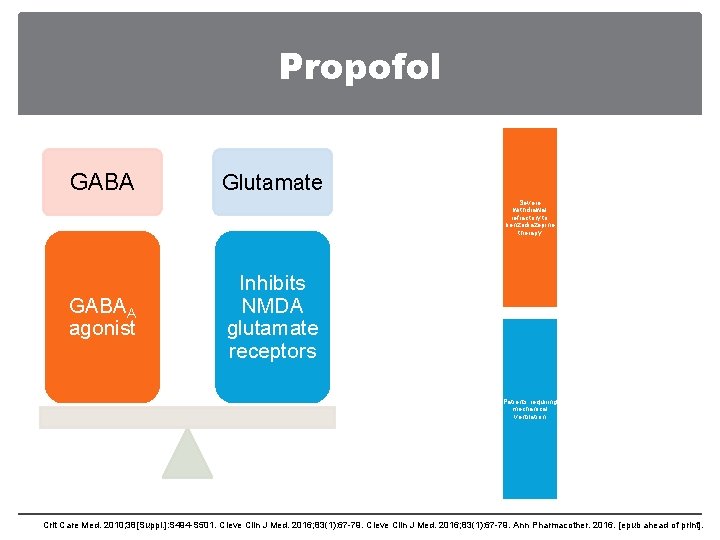
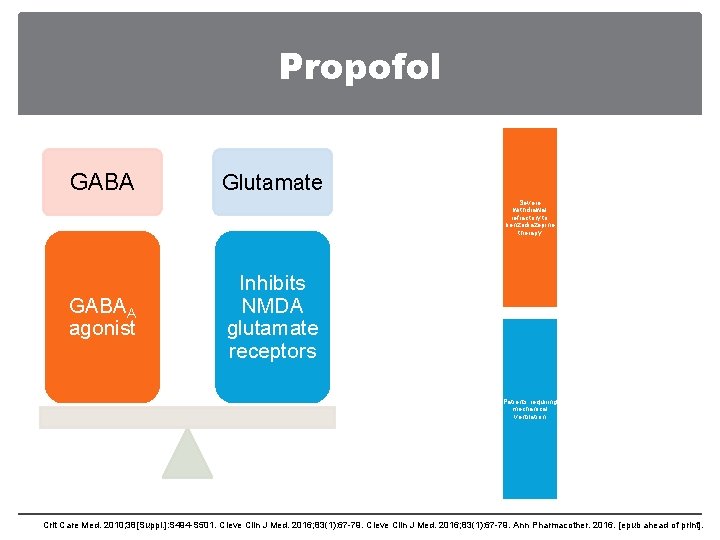
Propofol GABA Glutamate Severe withdrawal refractory to benzodiazepine therapy GABAA agonist Inhibits NMDA glutamate receptors Patients requiring mechanical ventilation Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
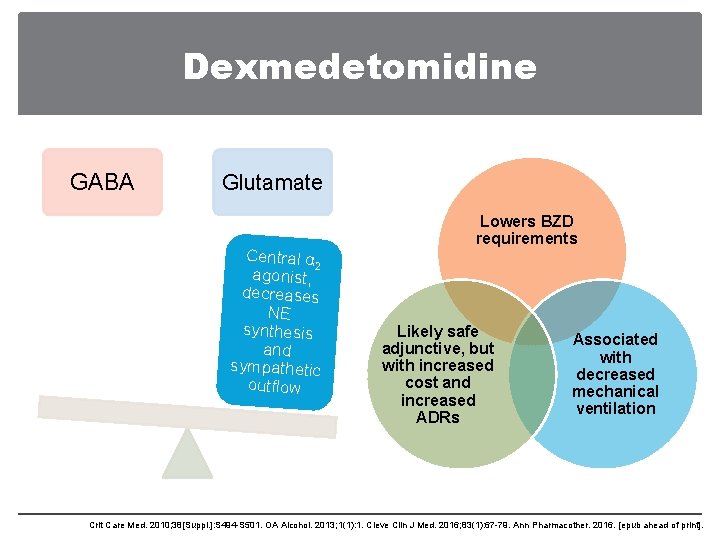
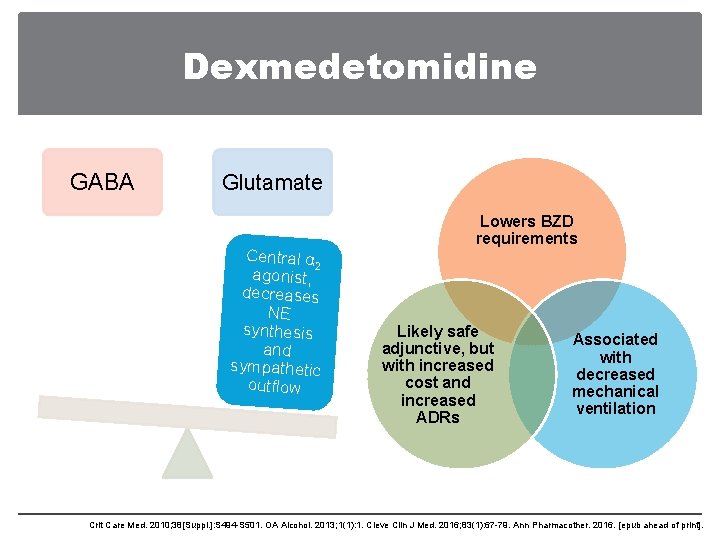
Dexmedetomidine GABA Glutamate Central α 2 agonist, decreases NE synthesis and sympathetic outflow Lowers BZD requirements Likely safe adjunctive, but with increased cost and increased ADRs Associated with decreased mechanical ventilation Crit Care Med. 2010; 38[Suppl. ]: S 494 -S 501. OA Alcohol. 2013; 1(1): 1. Cleve Clin J Med. 2016; 83(1): 67 -79. Ann Pharmacother. 2016. [epub ahead of print].
Patient Case PQ is a 64 yo male is admitted to the Trauma ICU after a MVC • On hospital day 2, PQ becomes more agitated and requires treatment of his alcohol withdrawal. How can we treat PQ’s withdrawal?
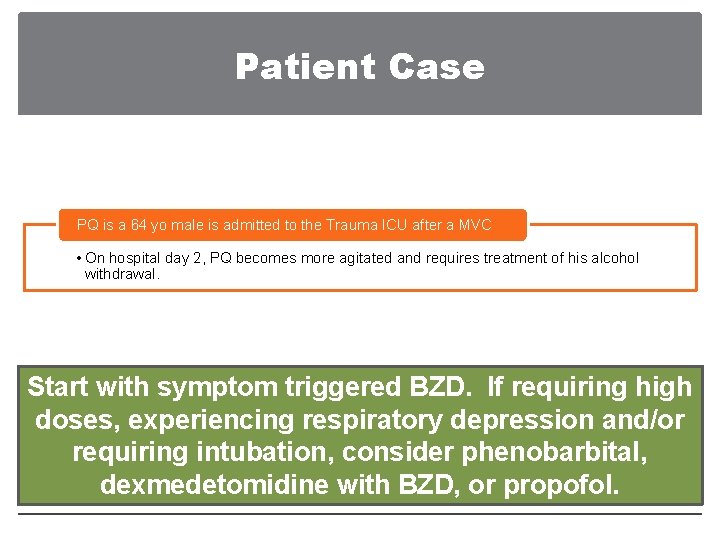
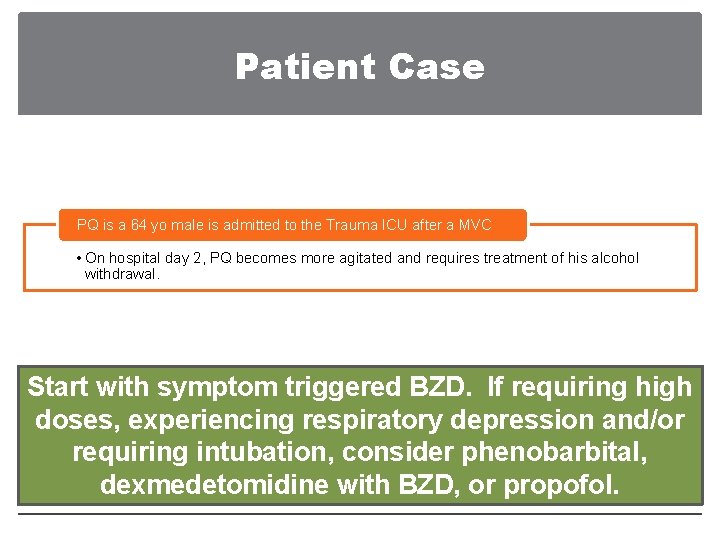
Patient Case PQ is a 64 yo male is admitted to the Trauma ICU after a MVC • On hospital day 2, PQ becomes more agitated and requires treatment of his alcohol withdrawal. Start with symptom triggered BZD. If requiring high doses, experiencing respiratory depression and/or requiring intubation, consider phenobarbital, dexmedetomidine with BZD, or propofol.
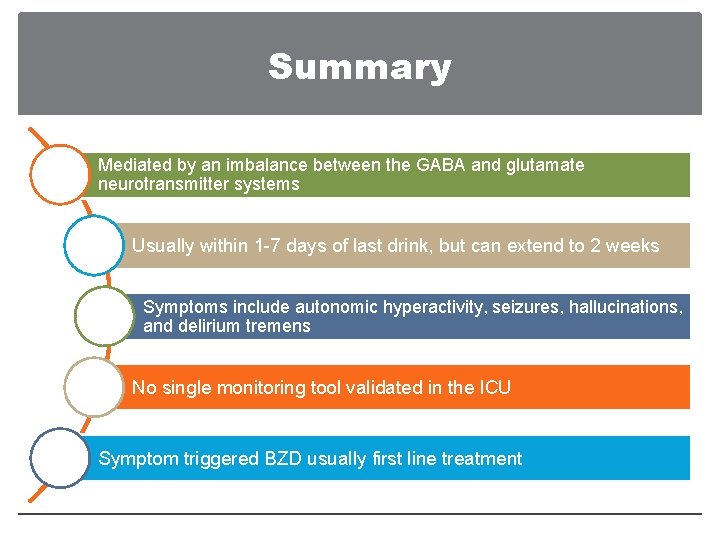
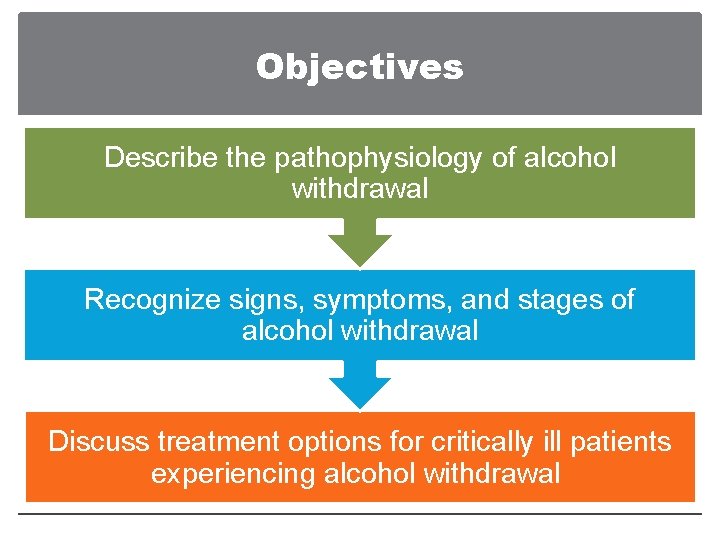
Summary Mediated by an imbalance between the GABA and glutamate neurotransmitter systems Usually within 1 -7 days of last drink, but can extend to 2 weeks Symptoms include autonomic hyperactivity, seizures, hallucinations, and delirium tremens No single monitoring tool validated in the ICU Symptom triggered BZD usually first line treatment
The Unhappy Hour: Managing Critically Ill Patients in Alcohol Withdrawal Emily J. Owen, Pharm. D. , BCPS, BCCCP Surgical, Burn, Trauma ICU Clinical Pharmacist
 Care of critically ill surgical patient
Care of critically ill surgical patient Nasogastrio
Nasogastrio Clock hour to credit hour conversion
Clock hour to credit hour conversion 24 hour format clock
24 hour format clock Thinking critically
Thinking critically Thinking critically with psychological science answer key
Thinking critically with psychological science answer key Negative issue
Negative issue Pico cat voorbeeld
Pico cat voorbeeld Thinking critically
Thinking critically Thoughtful learning
Thoughtful learning General aseptic fields are managed critically
General aseptic fields are managed critically Thinking critically with psychological science
Thinking critically with psychological science Critical thinking example in nursing
Critical thinking example in nursing Listening critically
Listening critically Critical aseptic field
Critical aseptic field Sonnet 27 shakespeare analysis
Sonnet 27 shakespeare analysis Thinking critically with psychological science
Thinking critically with psychological science How answer
How answer A wondering mind is an unhappy mind
A wondering mind is an unhappy mind So people are unhappy
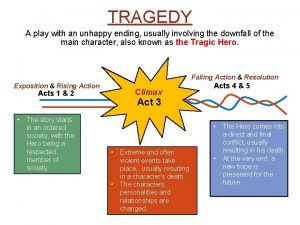
So people are unhappy Works written by shakespeare often have an unhappy ending
Works written by shakespeare often have an unhappy ending Many people are unhappy with
Many people are unhappy with I was most unhappy with the service
I was most unhappy with the service Unhappy millionaires
Unhappy millionaires Negative prefixes examples
Negative prefixes examples Story writing with outline
Story writing with outline Unhappy darling?
Unhappy darling? Out your
Out your No one is respectable or unhappy over the whole earth
No one is respectable or unhappy over the whole earth Comparative and superlative of calm
Comparative and superlative of calm King hector drank chocolate milk
King hector drank chocolate milk Wish in past
Wish in past Using manners
Using manners And now doth fare ill meaning in hindi
And now doth fare ill meaning in hindi What i did last weekend
What i did last weekend Ill methodology workshop
Ill methodology workshop Where you go ill go
Where you go ill go Rising action of the sob sisters story
Rising action of the sob sisters story An immediate and temporary care given to an injured person
An immediate and temporary care given to an injured person Ill think
Ill think Scream and ill tell your mom
Scream and ill tell your mom Second conditional
Second conditional Rapid ill
Rapid ill Mum and dad son
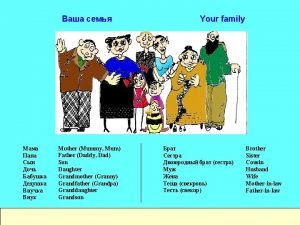
Mum and dad son Tell me and ill forget
Tell me and ill forget