5 1 3112021 Echocardiography in Critically ill Patients








- Slides: 41

5 1 3/11/2021
Echocardiography in Critically ill Patients Rasoul Azarfarin MD, FACC Professor of Anesthesiology Fellowship of Cardiac Anesthesia 3/11/2021 2
3/11/2021 3

Critically ill and hemodynamically unstable patients (Extra-cardiac and Cardiac causes) • • • ARDS Sepsis Cardiac Tamponade Acute Cor-pulmonale Acute bleeding ant hypovolemia Pulmonary thrombo-embolism (PTE) Acute LV and RV failure (e. i. AMI) Lethal Arrhythmias Cardiac Arrest 3/11/2021 4
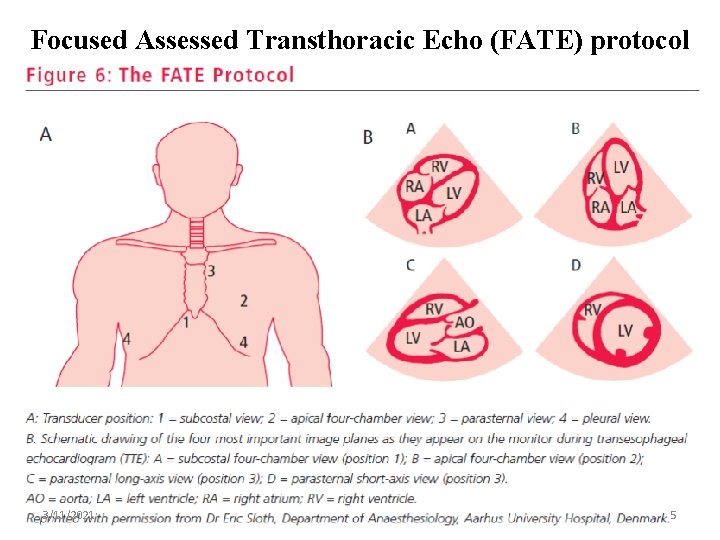
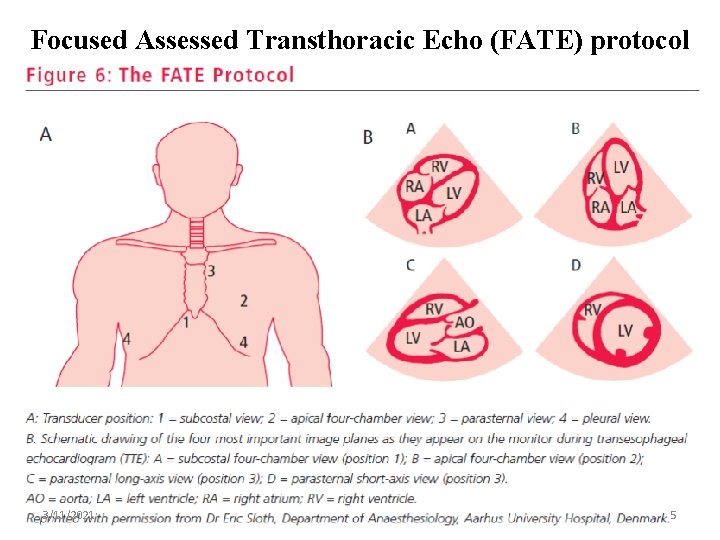
Focused Assessed Transthoracic Echo (FATE) protocol 3/11/2021 5
Diagnosis of “low cardiac output” state • Intensivist must differentiate Extra-Cardiac vs. Cardiac causes. • “Low cardiac output” stat not limited only to BP or CVP measurements. • Physician should evaluate the direct and indirect evidence of “Low-Cardiac Output” such as oliguria, cold and pale skin, … • The best way is a objective measurement of CO “Echocardiographic Assessment of Cardiac output” 3/11/2021 6
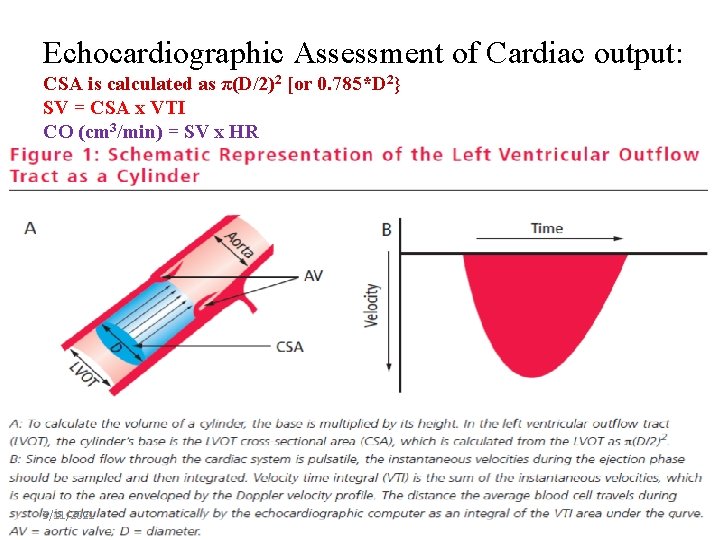
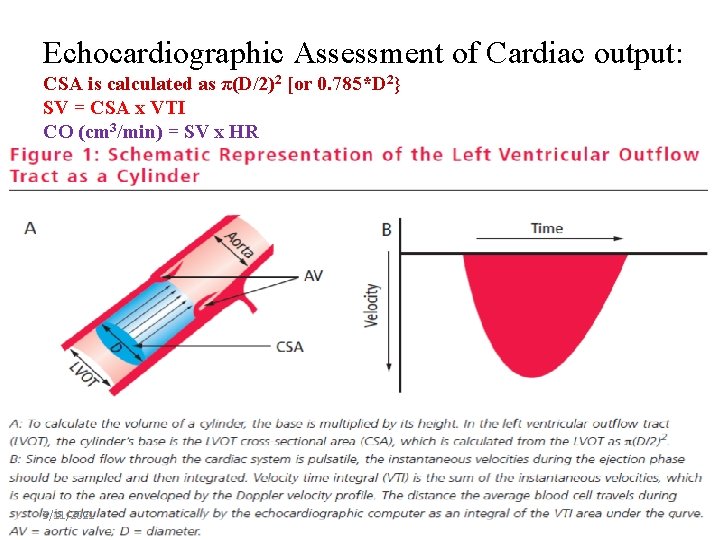
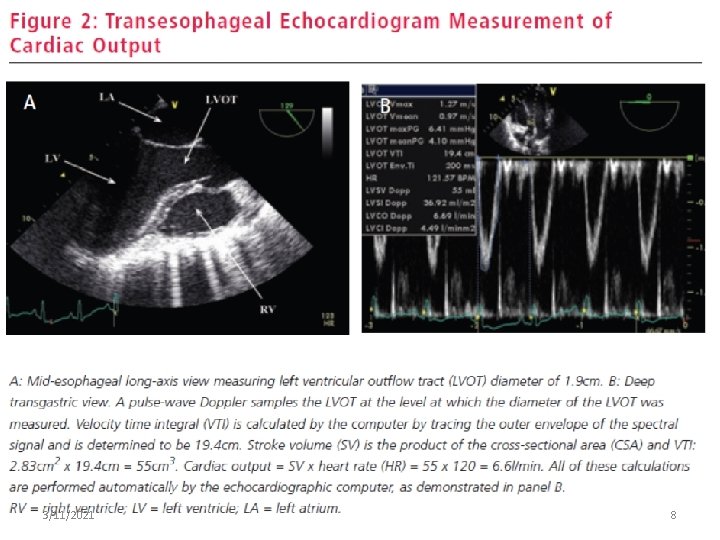
Echocardiographic Assessment of Cardiac output: CSA is calculated as π(D/2)2 [or 0. 785*D 2} SV = CSA x VTI CO (cm 3/min) = SV x HR 3/11/2021 7
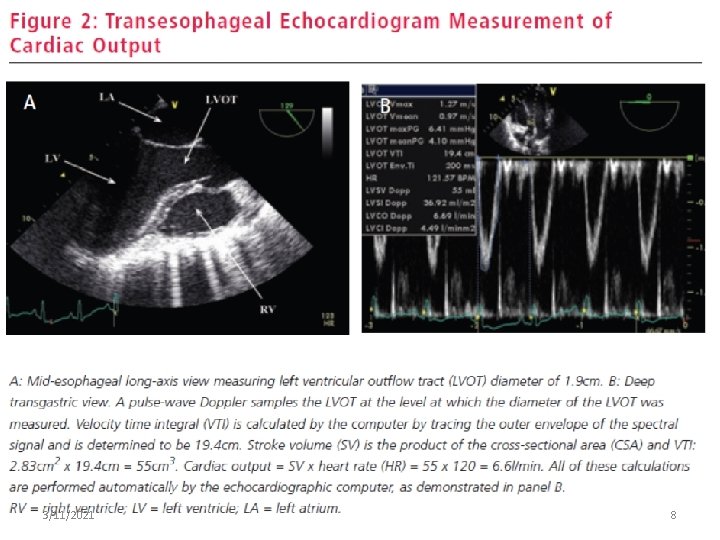
3/11/2021 8
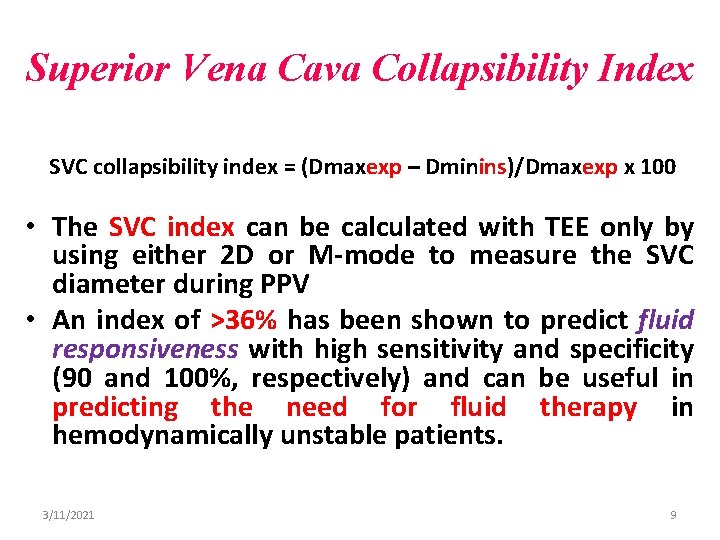
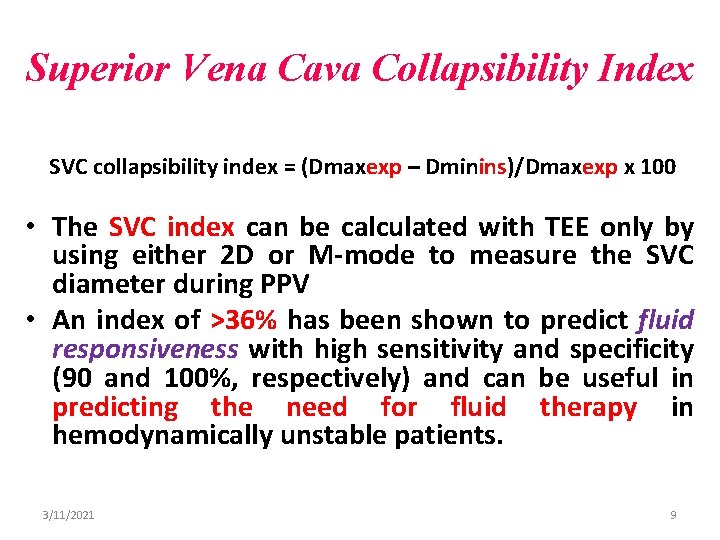
Superior Vena Cava Collapsibility Index SVC collapsibility index = (Dmaxexp – Dminins)/Dmaxexp x 100 • The SVC index can be calculated with TEE only by using either 2 D or M-mode to measure the SVC diameter during PPV • An index of >36% has been shown to predict fluid responsiveness with high sensitivity and specificity (90 and 100%, respectively) and can be useful in predicting the need for fluid therapy in hemodynamically unstable patients. 3/11/2021 9
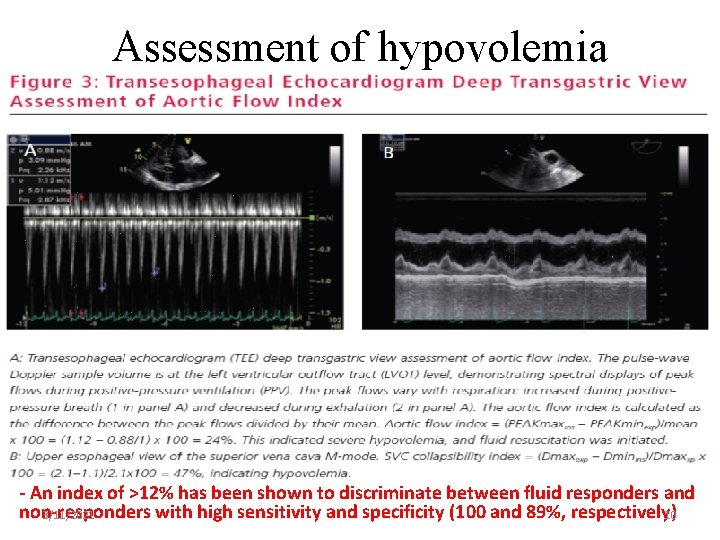
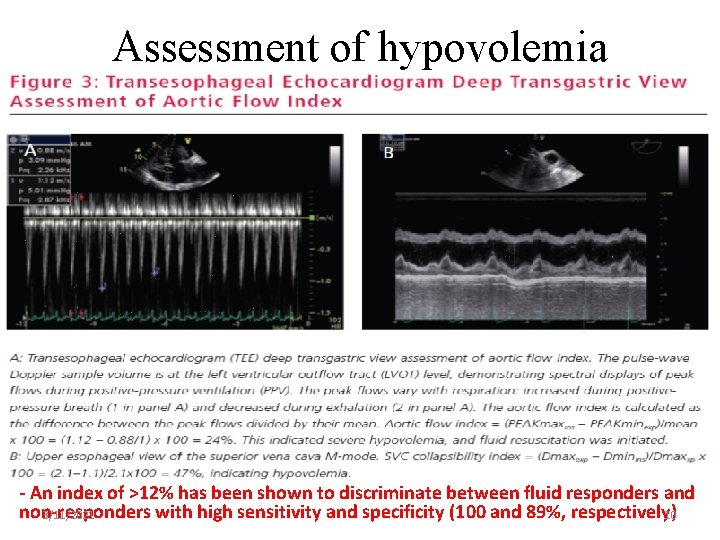
Assessment of hypovolemia - An index of >12% has been shown to discriminate between fluid responders and non-responders with high sensitivity and specificity (100 and 89%, respectively) 3/11/2021 10

3/11/2021 11
RATIONALE FOR ECHO USE IN ARDS • RV DYSFUNCTION: RECOGNITION & SUPPORT • VENTILATORY STRATEGY • DIFFERENTIAL DIAGNOSIS : ARDS vs. CARDIOGENIC PULMONARY EDEMA • NTRACARDIAC SHUNT DETECTION 3/11/2021 12

Pulmonary Hypertension in ARDS 3/11/2021 13
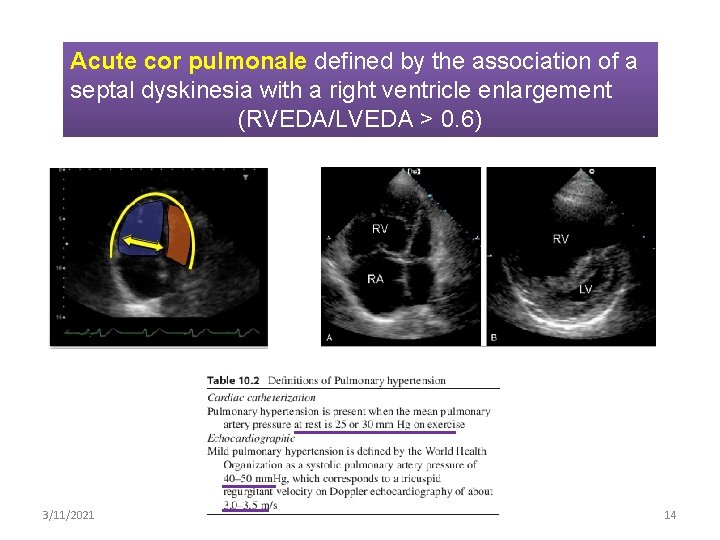
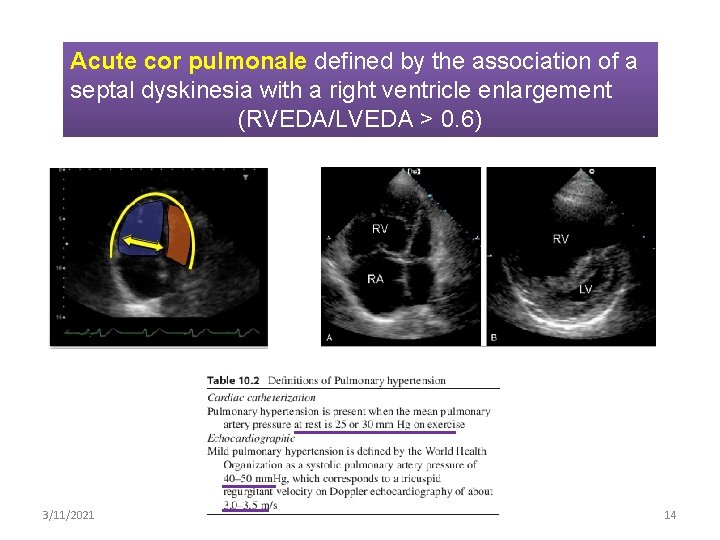
Acute cor pulmonale defined by the association of a septal dyskinesia with a right ventricle enlargement (RVEDA/LVEDA > 0. 6) 3/11/2021 14
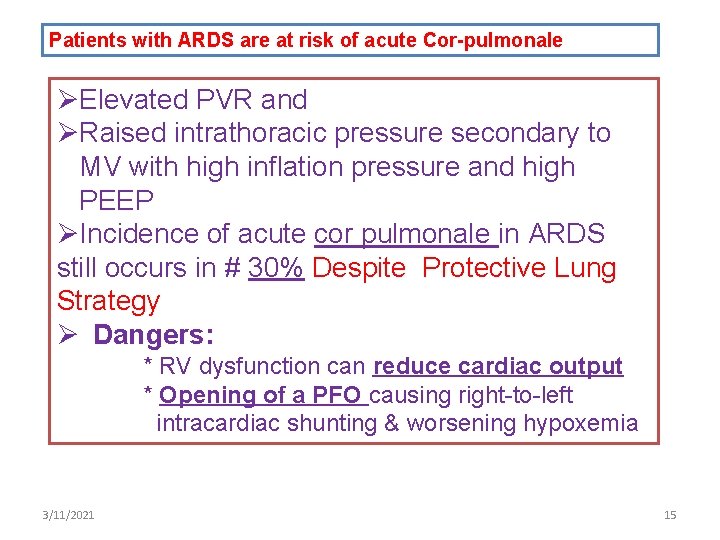
Patients with ARDS are at risk of acute Cor-pulmonale ØElevated PVR and ØRaised intrathoracic pressure secondary to MV with high inflation pressure and high PEEP ØIncidence of acute cor pulmonale in ARDS still occurs in # 30% Despite Protective Lung Strategy Ø Dangers: * RV dysfunction can reduce cardiac output * Opening of a PFO causing right-to-left intracardiac shunting & worsening hypoxemia 3/11/2021 15
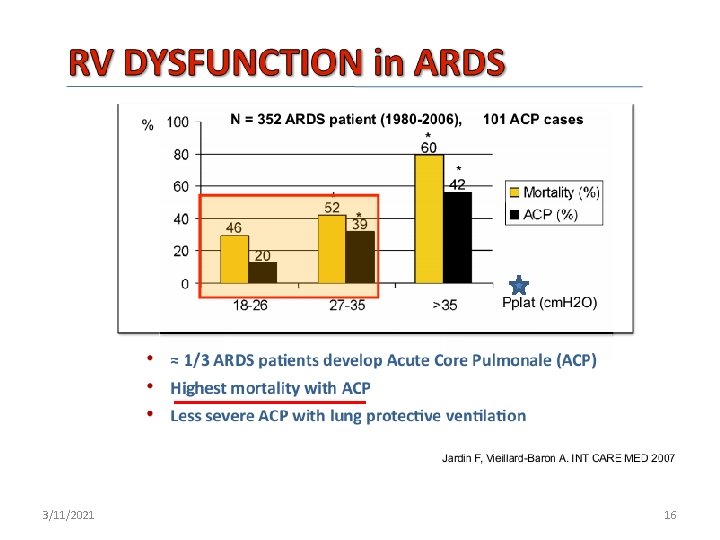
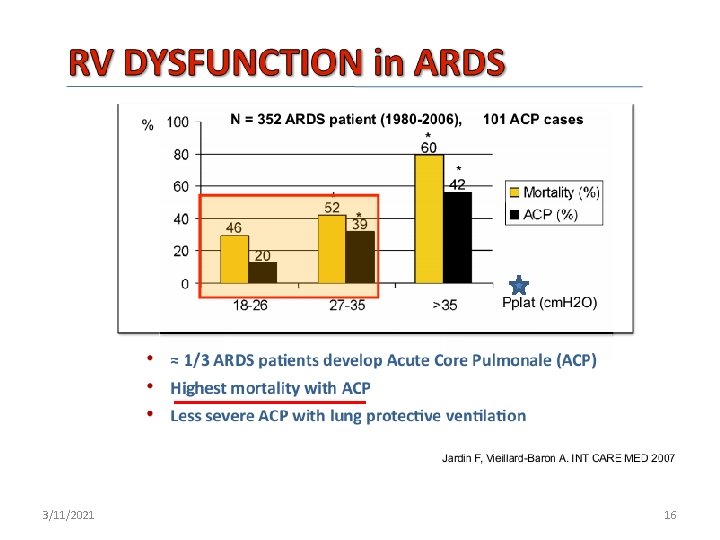
3/11/2021 16
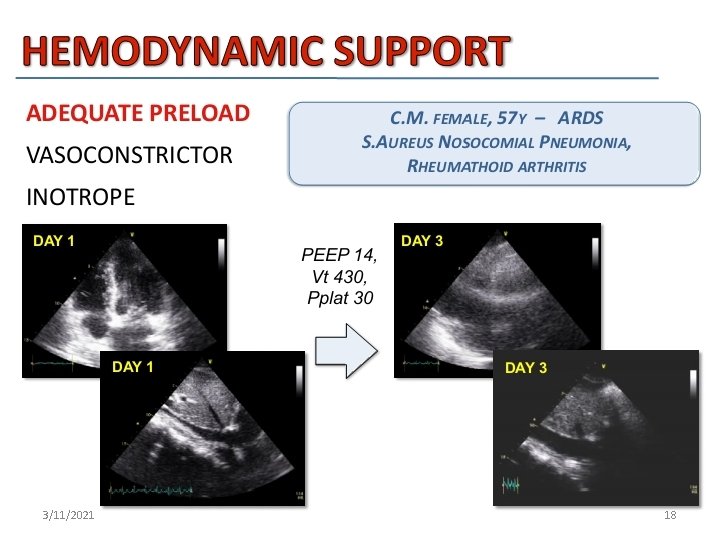
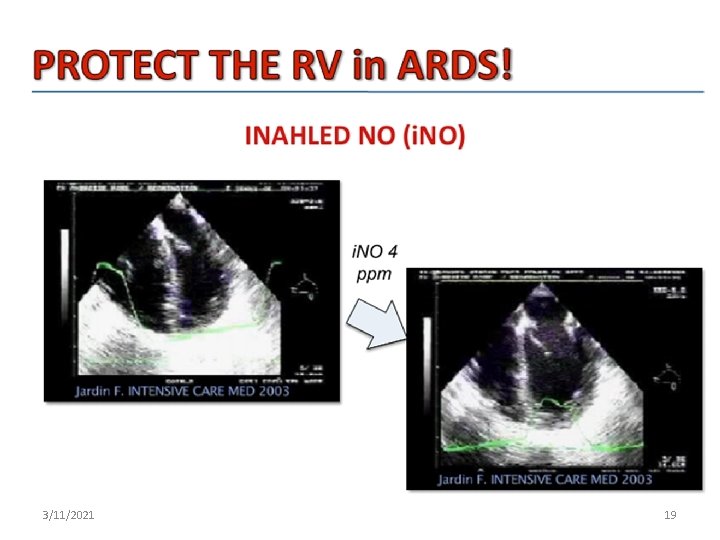
Treatment options in ARDS: Ø Adequate Preload Ø vasopressor support to augment RV perfusion pressure, Ø strategies to reduce PVR (correction of acidosis, increasing FIo 2, inhaled nitric oxide, etc. ), Ø Reducing airway pressure Ø Prone positioning may be benficial Ø Ultrasonography of the chest cavity is also useful to asses s the presence and size of pleural effusion 3/11/2021 17
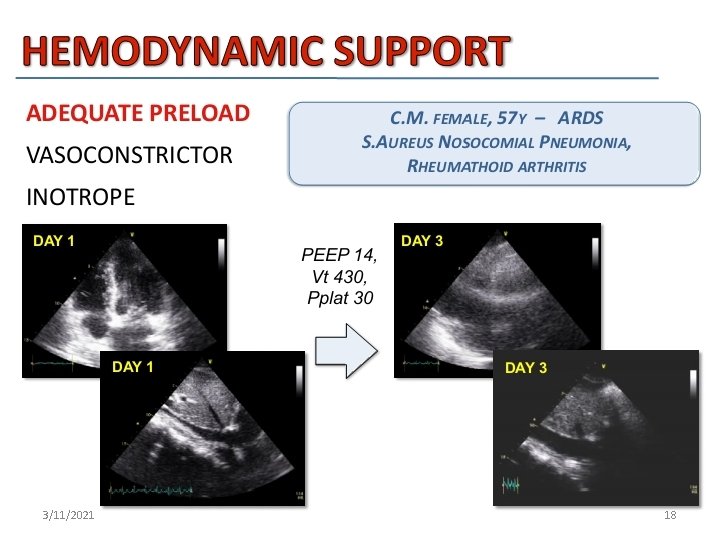
3/11/2021 18
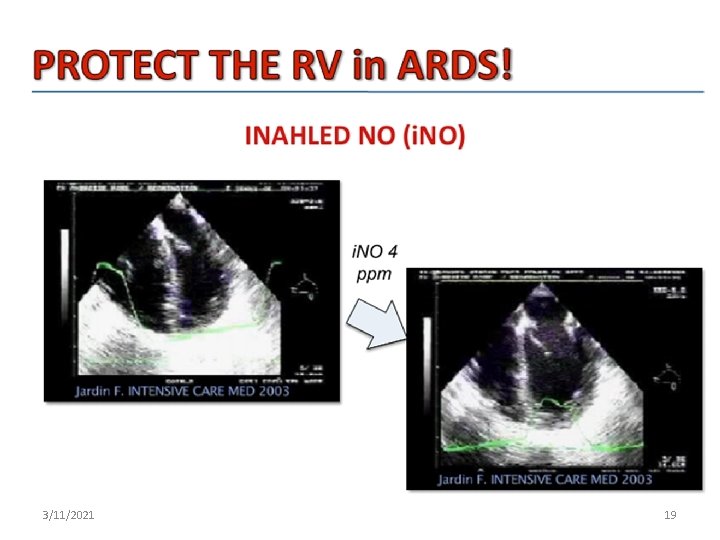
3/11/2021 19
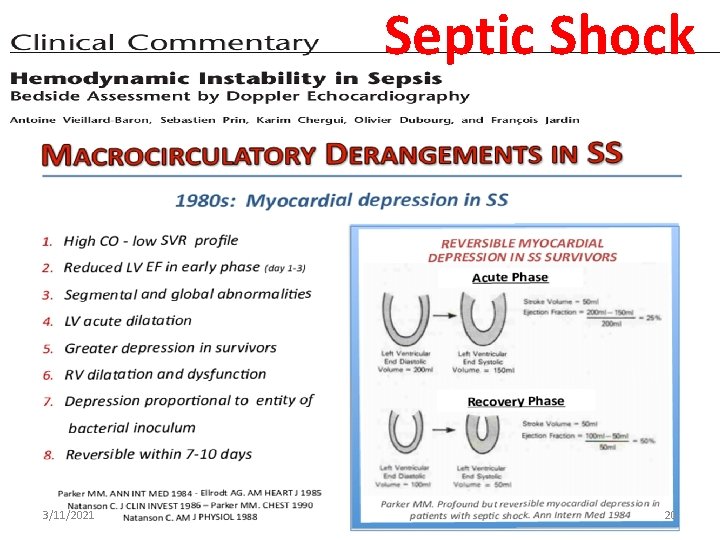
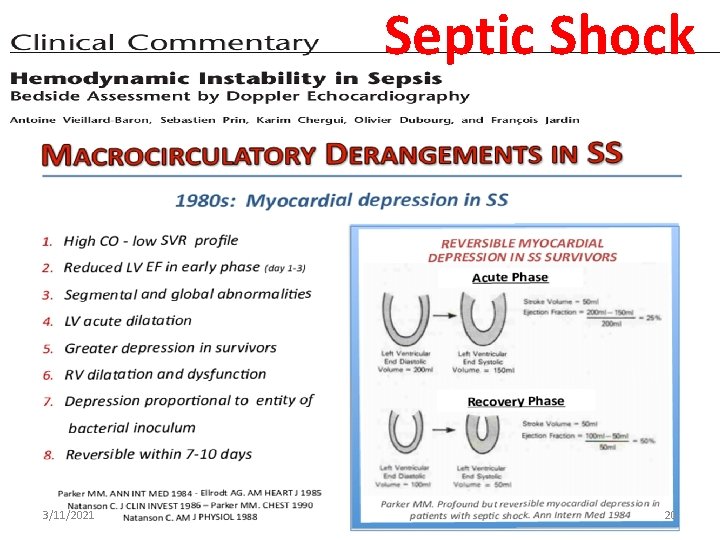
Septic Shock 3/11/2021 20

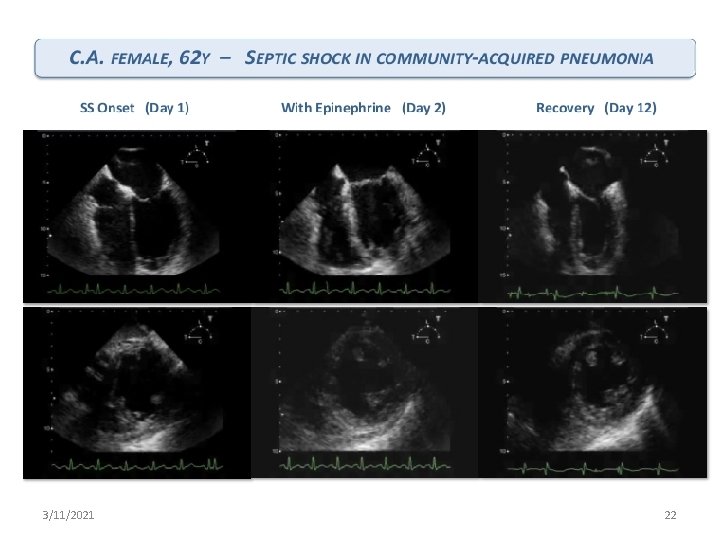
Ø Whether cardiac ventricles can acutely dilate during septic myocardial dysfunction? Ø 45 patients were studied over the first 10 days of septic shock 3/11/2021 21
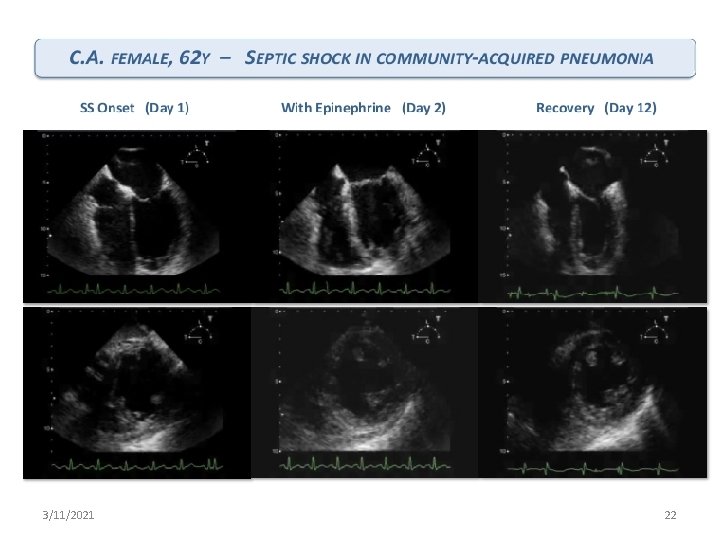
3/11/2021 22
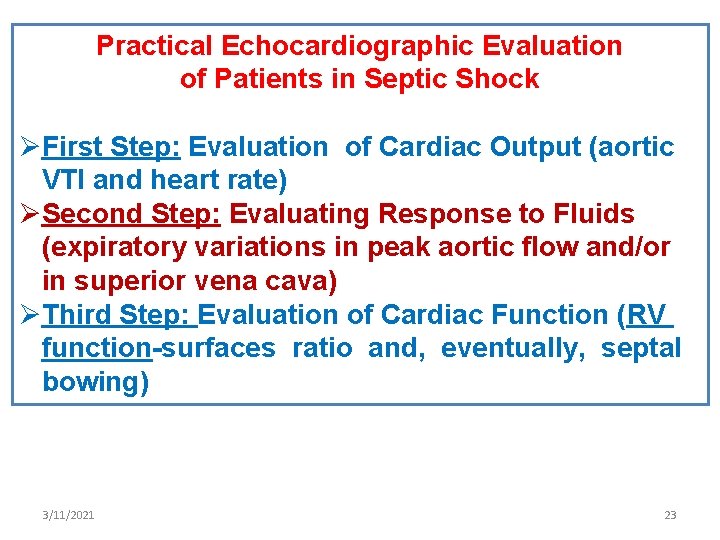
Practical Echocardiographic Evaluation of Patients in Septic Shock ØFirst Step: Evaluation of Cardiac Output (aortic VTI and heart rate) ØSecond Step: Evaluating Response to Fluids (expiratory variations in peak aortic flow and/or in superior vena cava) ØThird Step: Evaluation of Cardiac Function (RV function-surfaces ratio and, eventually, septal bowing) 3/11/2021 23
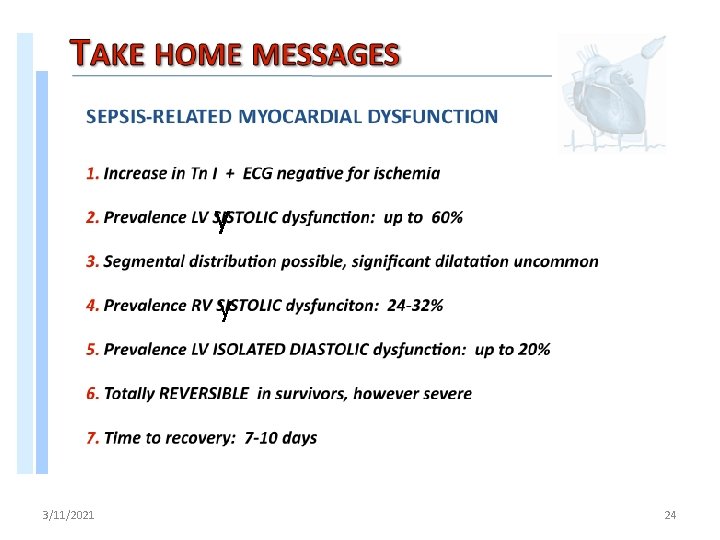
y y 3/11/2021 24
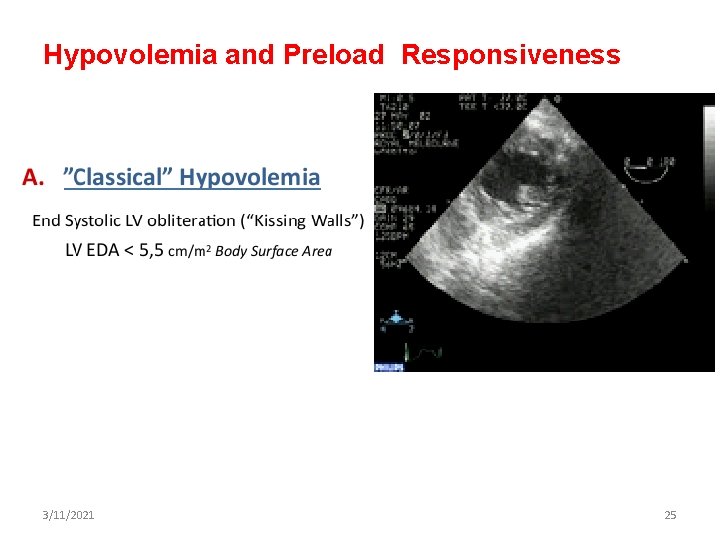
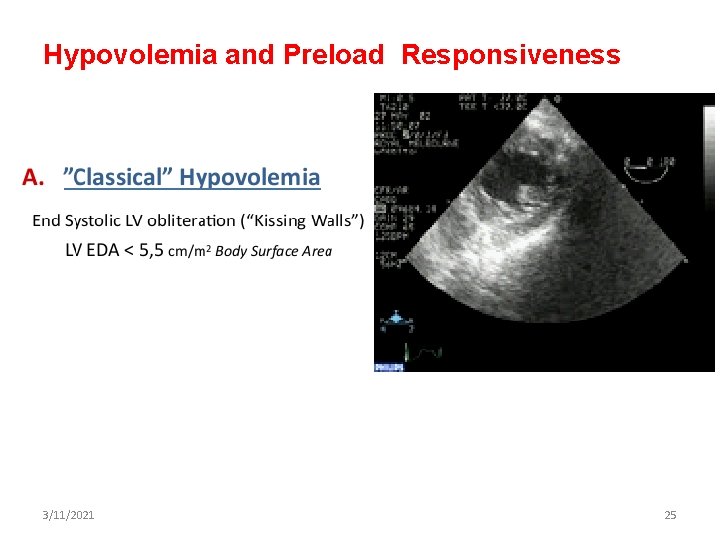
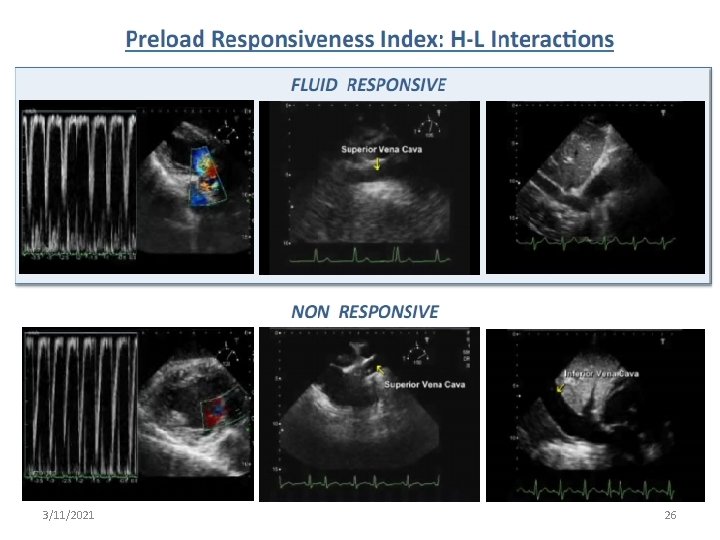
Hypovolemia and Preload Responsiveness 3/11/2021 25
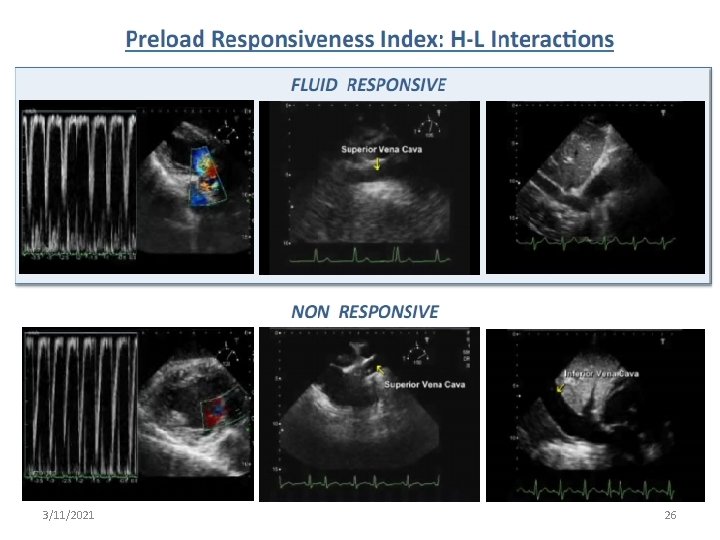
3/11/2021 26
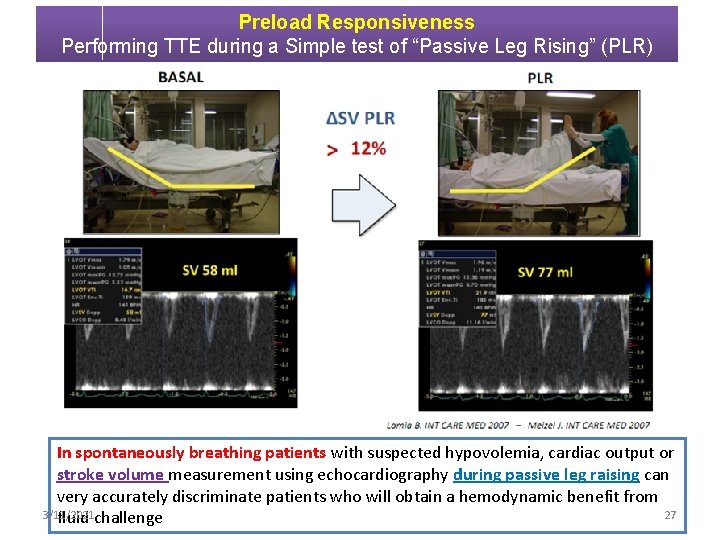
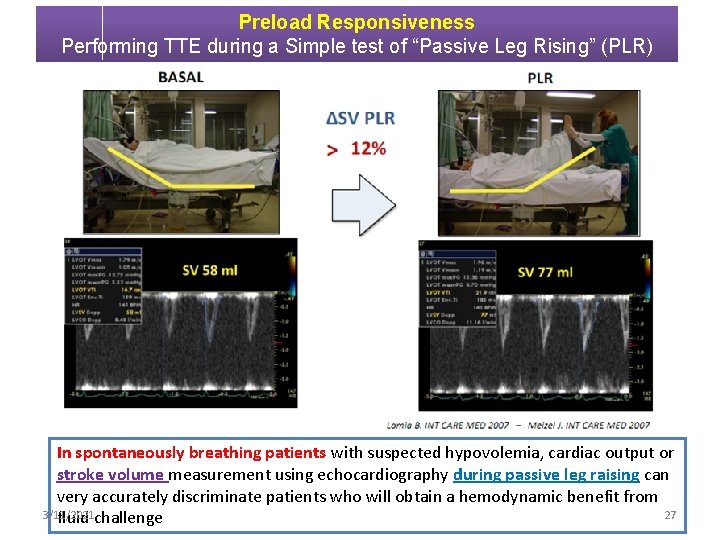
Preload Responsiveness Performing TTE during a Simple test of “Passive Leg Rising” (PLR) In spontaneously breathing patients with suspected hypovolemia, cardiac output or stroke volume measurement using echocardiography during passive leg raising can very accurately discriminate patients who will obtain a hemodynamic benefit from 3/11/2021 27 fluid challenge
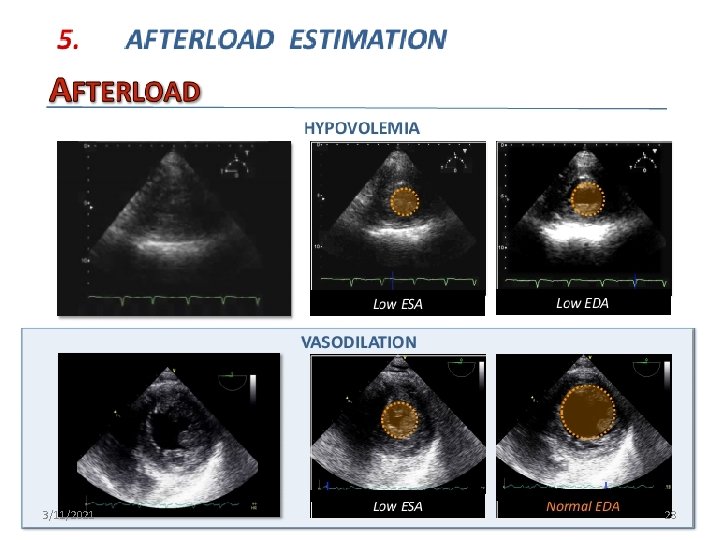
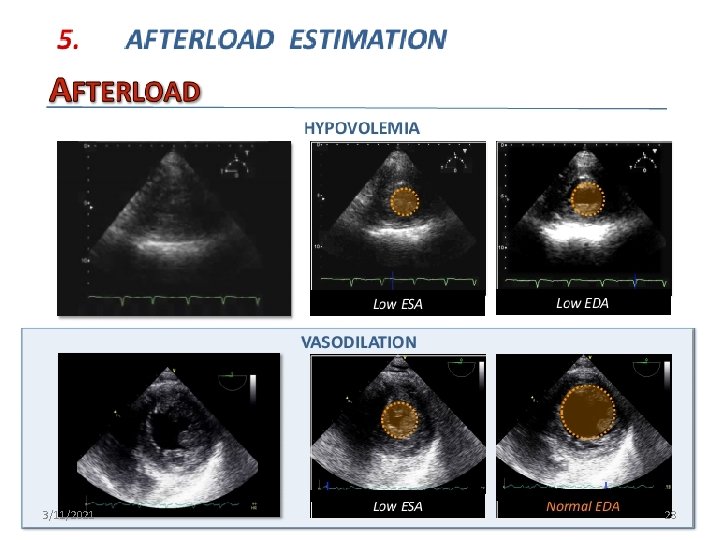
3/11/2021 28
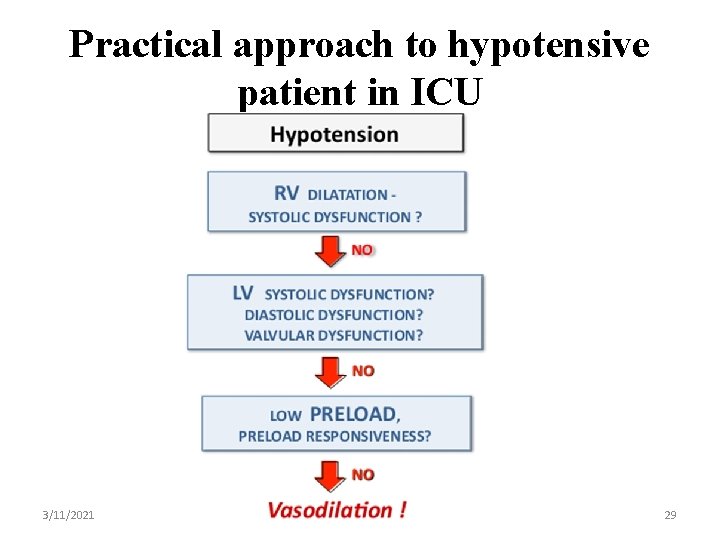
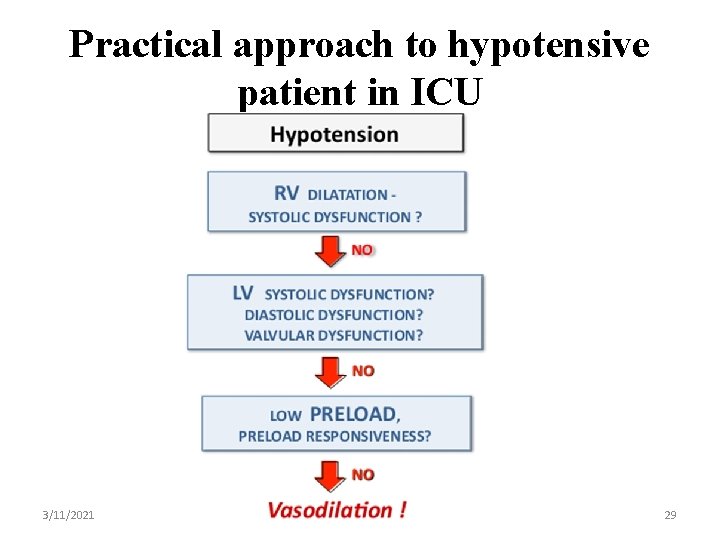
Practical approach to hypotensive patient in ICU 3/11/2021 29
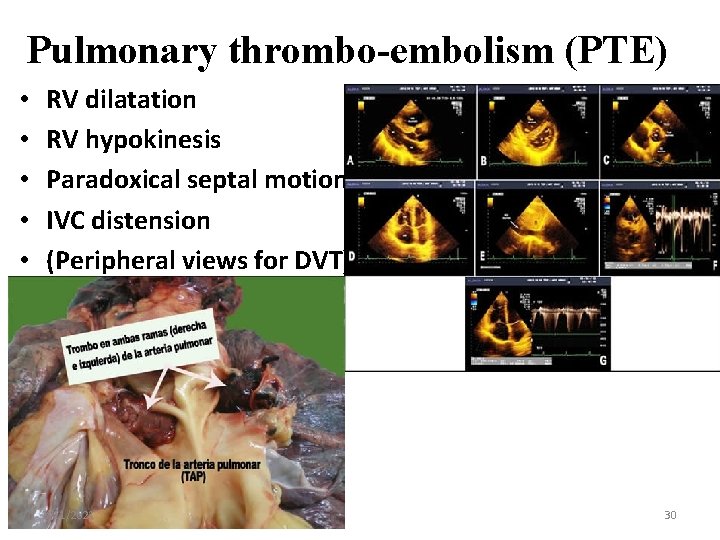
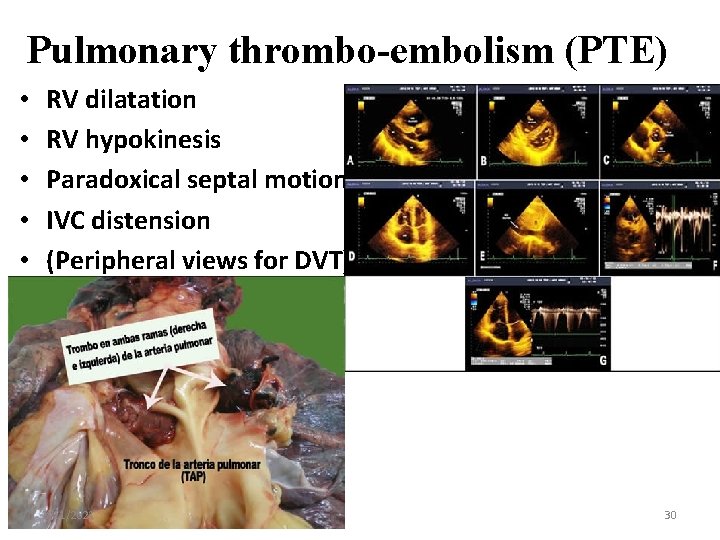
Pulmonary thrombo-embolism (PTE) • • • RV dilatation RV hypokinesis Paradoxical septal motion IVC distension (Peripheral views for DVT) 3/11/2021 30
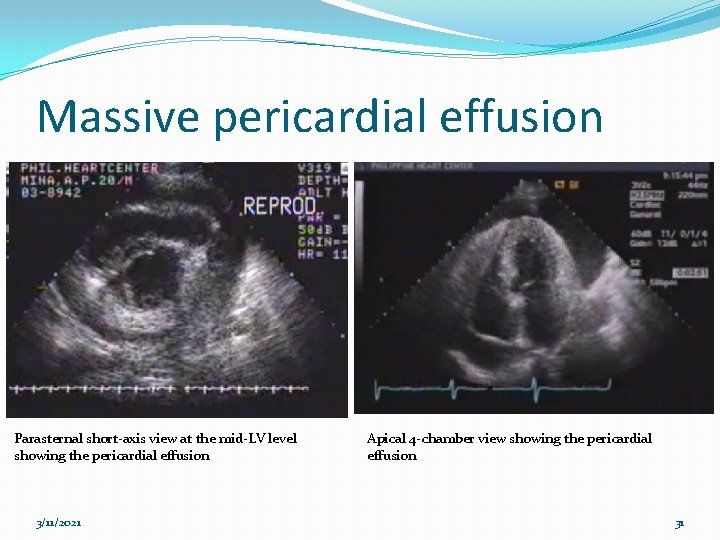
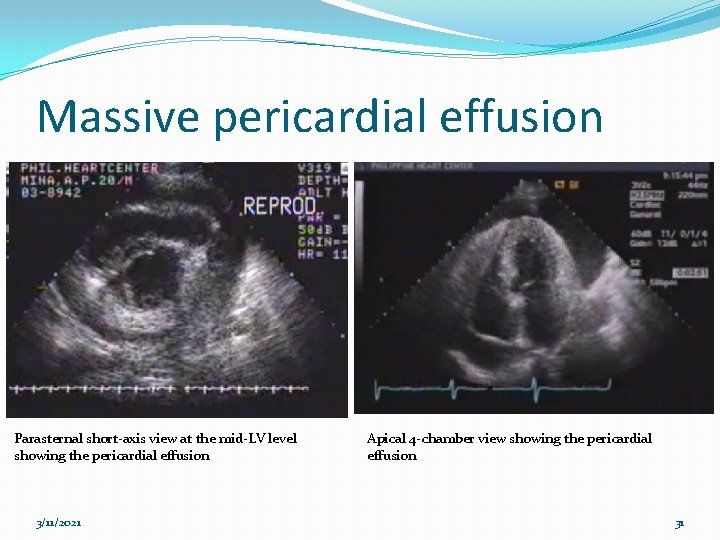
Massive pericardial effusion Parasternal short-axis view at the mid-LV level showing the pericardial effusion 3/11/2021 Apical 4 -chamber view showing the pericardial effusion 31
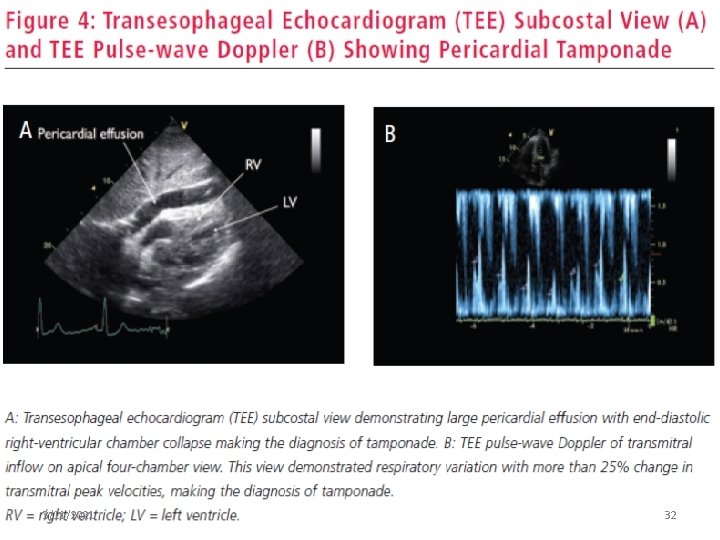
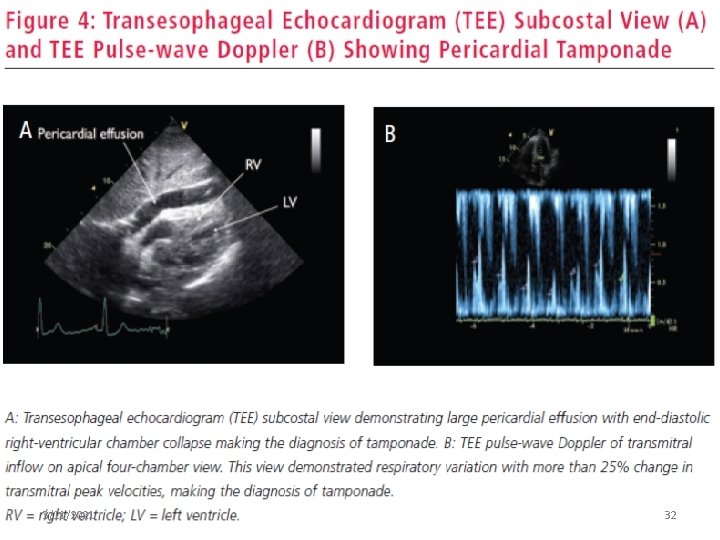
3/11/2021 32
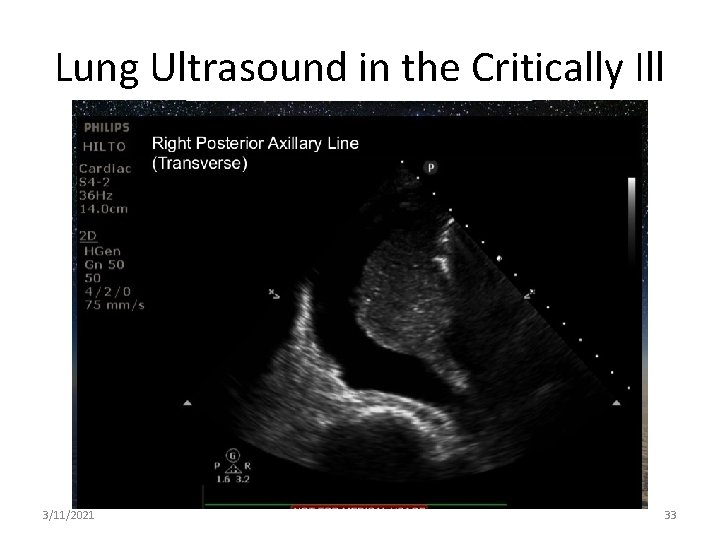
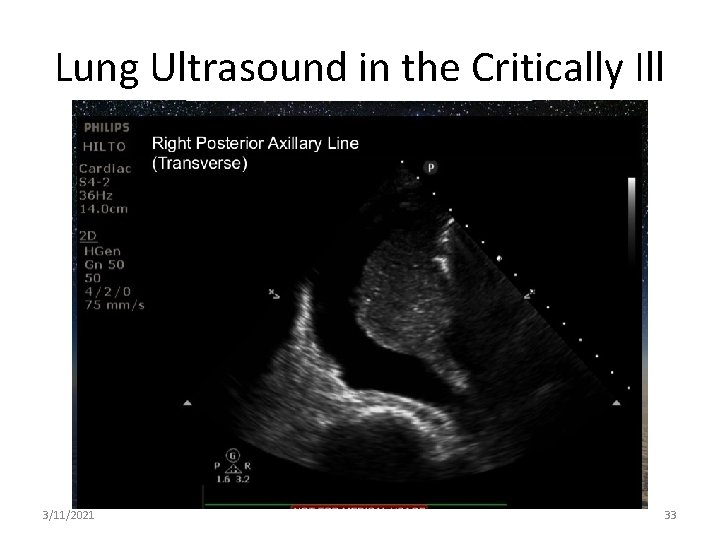
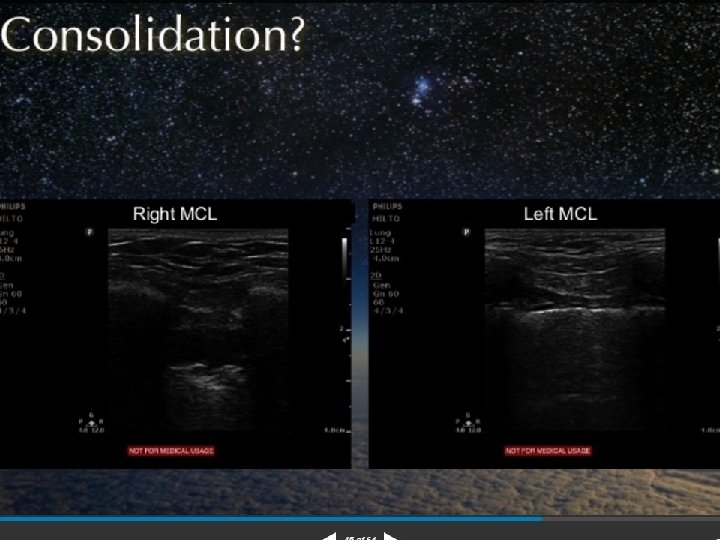
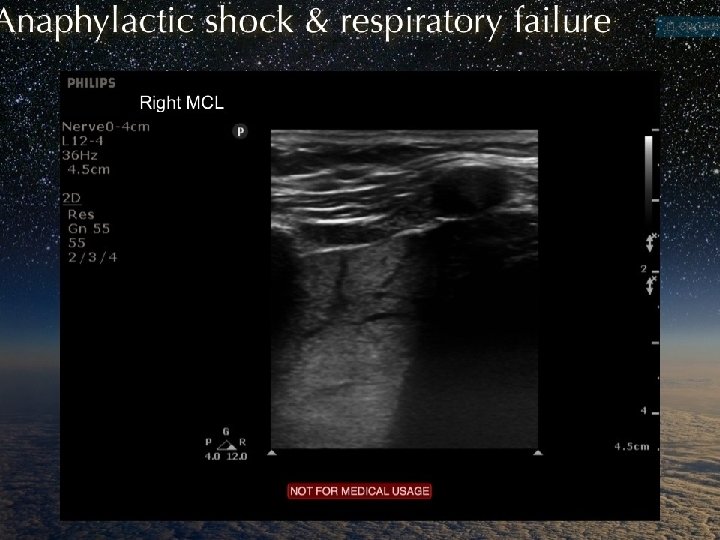
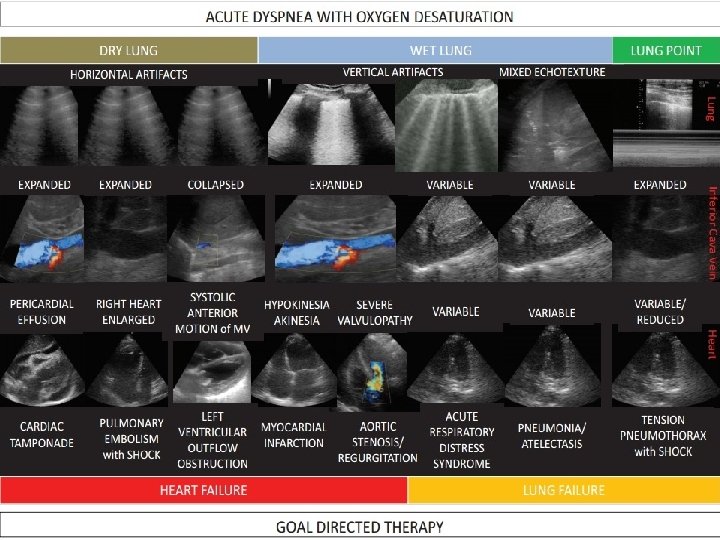
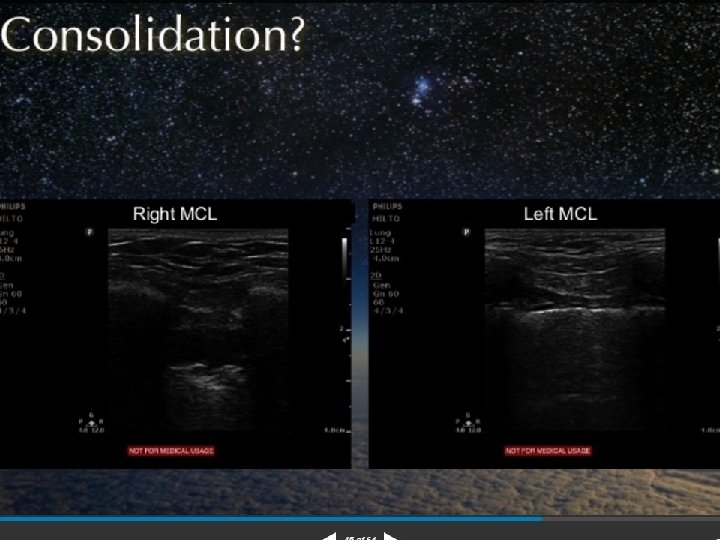
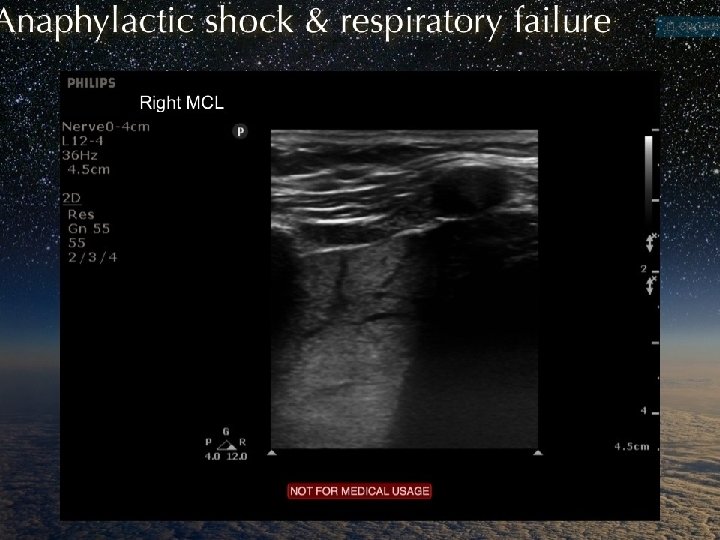
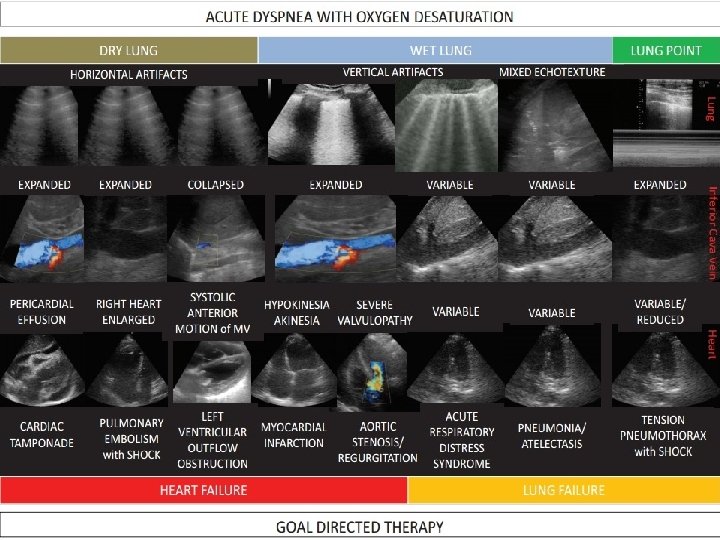
Lung Ultrasound in the Critically Ill 3/11/2021 33

3/11/2021 34
3/11/2021 35
3/11/2021 36
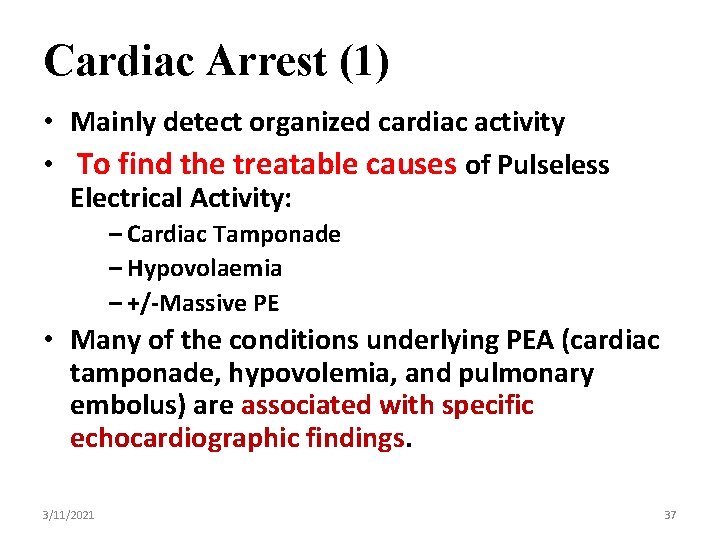
Cardiac Arrest (1) • Mainly detect organized cardiac activity • To find the treatable causes of Pulseless Electrical Activity: – Cardiac Tamponade – Hypovolaemia – +/-Massive PE • Many of the conditions underlying PEA (cardiac tamponade, hypovolemia, and pulmonary embolus) are associated with specific echocardiographic findings. 3/11/2021 37

Cardiac Arrest (2) • Is there effective myocardial contractility? – Asystole – Myocardial “twitch” – Hypokinesis – Normal • Is there a pericardial effusion? – – Perform ECHO during “quick look” and in pulse checks Pericardiocentesis • Transvenous pacemaker placement – Assessment of capture by transthoracic pacemaker – Ettin D et al: Using ultrasound to determine external pacer capture 3/11/2021 38
Echo during CPR • Utility of echo for in hospital cardiac arrests is for certain specialized arrests only (eg: peri -cardiac surgery, blunt and penetrating chest trauma) but not for your ‘routine ward arrest’ 3/11/2021 39
3/11/2021 40

3/11/2021 41
 Care of critically ill surgical patient
Care of critically ill surgical patient Surgical metabolism
Surgical metabolism Ivrt echo
Ivrt echo Echocardiography
Echocardiography Makalah akreditasi rumah sakit
Makalah akreditasi rumah sakit 3112021
3112021 3112021
3112021 3112021
3112021 3112021
3112021 3112021
3112021 Huntersville town billboards
Huntersville town billboards 3112021
3112021 3112021
3112021 Listening critically
Listening critically Micro critical aseptic field
Micro critical aseptic field General aseptic fields are managed critically
General aseptic fields are managed critically What is sonnet 27 about
What is sonnet 27 about Thinking critically with psychological science
Thinking critically with psychological science Illusory correlations ______.
Illusory correlations ______. Negative issues
Negative issues Critically appraised topic voorbeeld
Critically appraised topic voorbeeld Thinking critically
Thinking critically Thoughtful learning
Thoughtful learning Thinking critically with psychological science answer key
Thinking critically with psychological science answer key Thinking critically with psychological science
Thinking critically with psychological science Define critical thinking in nursing
Define critical thinking in nursing It was such a foggy day that we couldn't see the road
It was such a foggy day that we couldn't see the road Dr angel rodriguez-chevres
Dr angel rodriguez-chevres Concepts of ill health
Concepts of ill health Ill project management
Ill project management You said i am feeling ill
You said i am feeling ill This supernatural soliciting cannot be ill cannot be good
This supernatural soliciting cannot be ill cannot be good By doing nothing we learn to be ill
By doing nothing we learn to be ill 5 bad manners
5 bad manners Waiting on the lord song
Waiting on the lord song Euill
Euill What did you do on sunday?
What did you do on sunday? Ill kill him
Ill kill him Rising action of the sob sisters story
Rising action of the sob sisters story And now doth fare ill meaning in hindi
And now doth fare ill meaning in hindi Ill methodology workshop
Ill methodology workshop Scream and ill tell your mom
Scream and ill tell your mom