Fluid and electrolyte emergencies in critically ill patients


- Slides: 57
Fluid and electrolyte emergencies in critically ill patients � Dr. V. P. CHANDRASEKARAN HOD, Dept. of Emergency & Critical Care Medicine, VMKVMC , Salem
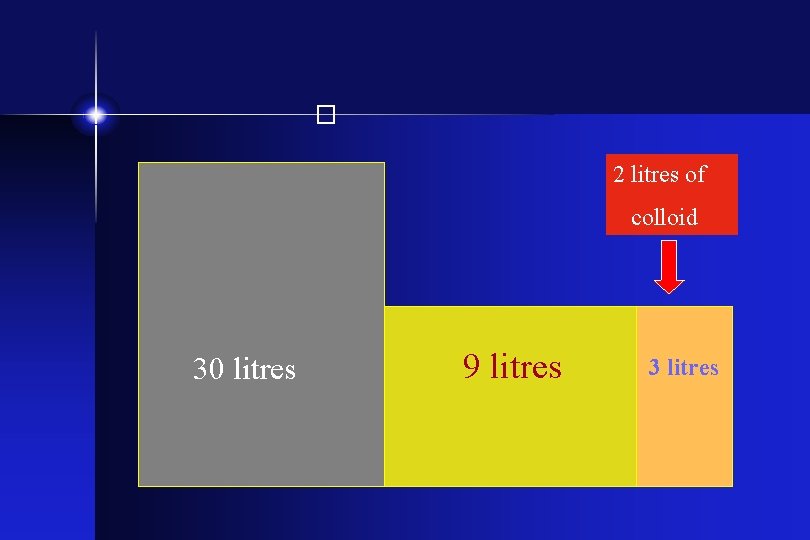
Introduction � • Total body water (60%) • Two third is intracellular fluid (40%) • One third is extra cellular fluid (20%) - Interstitial fluid (15%) - Intravascular fluid (5%)
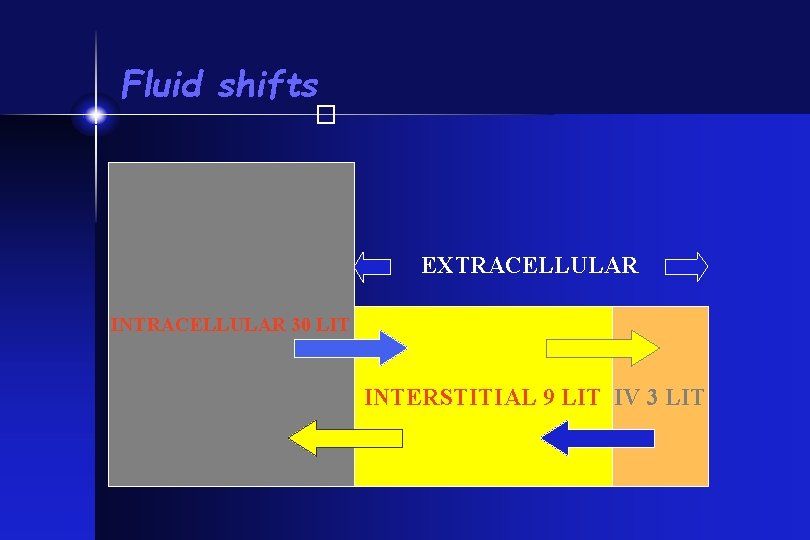
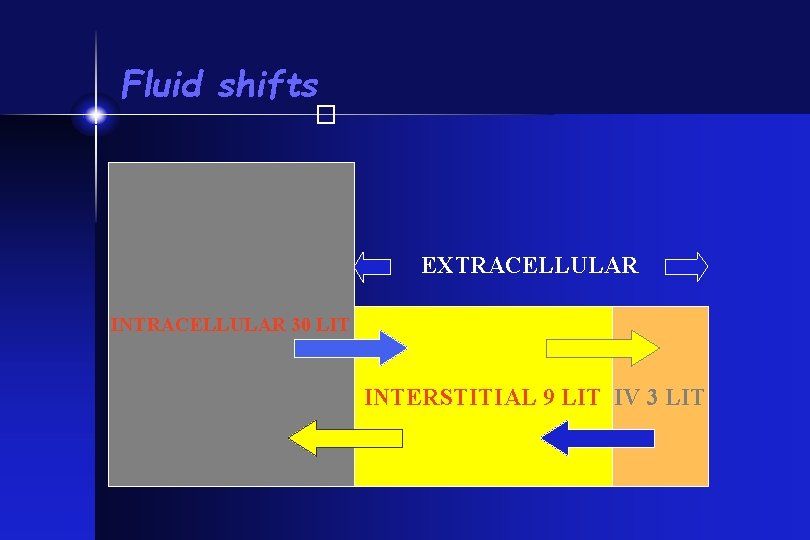
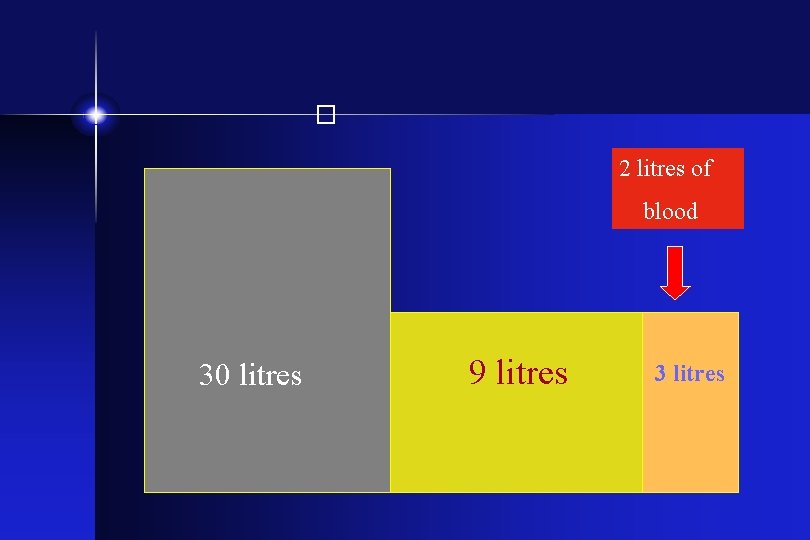
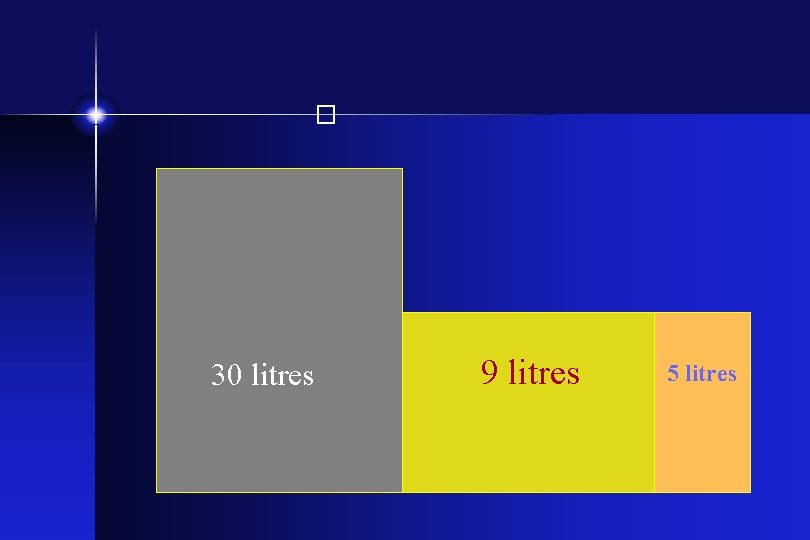
Fluid shifts � EXTRACELLULAR INTRACELLULAR 30 LIT INTERSTITIAL 9 LIT IV 3 LIT
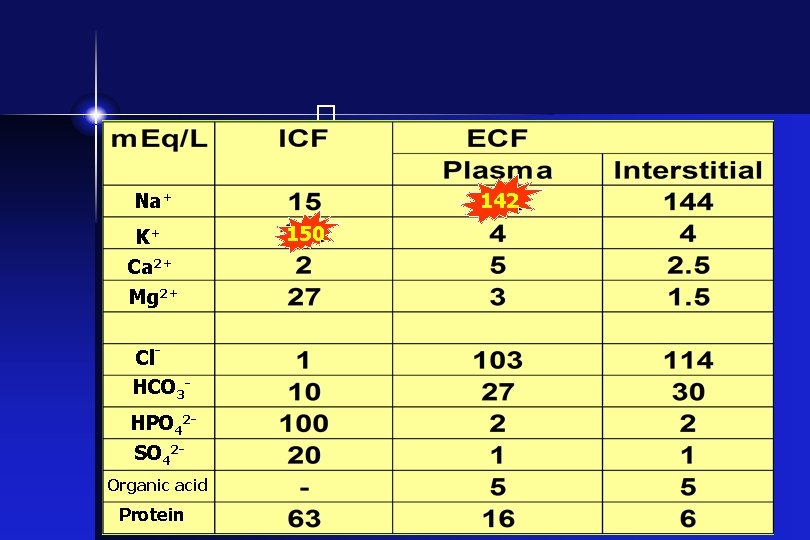
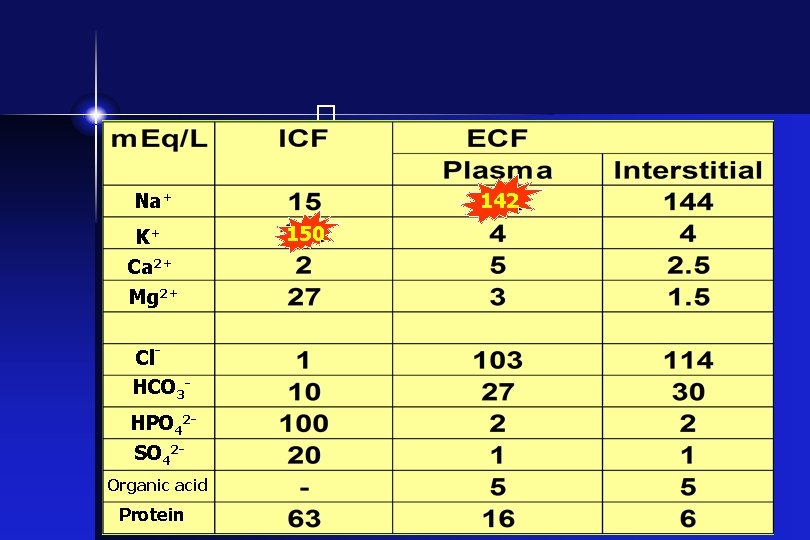
� 142 Na+ K+ Ca 2+ Mg 2+ Cl. HCO 3 HPO 42 SO 42 Organic acid Protein 150
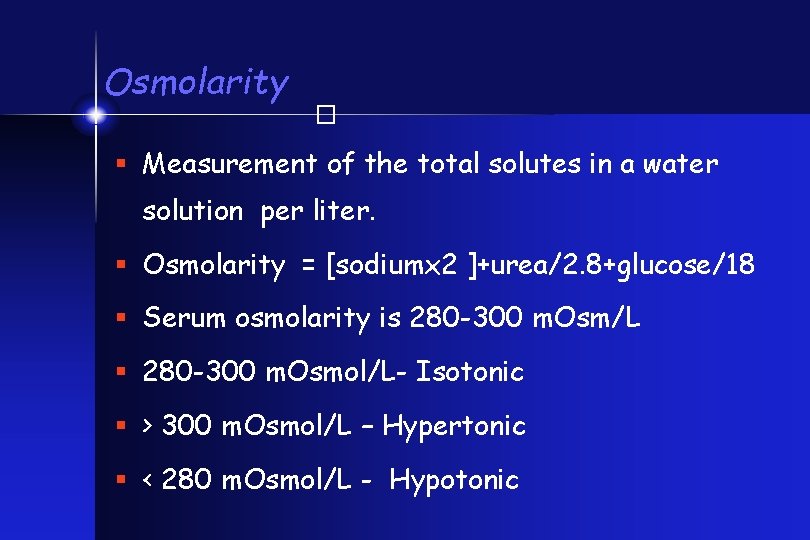
� Osmolarity § Measurement of the total solutes in a water solution per liter. § Osmolarity = [sodiumx 2 ]+urea/2. 8+glucose/18 § Serum osmolarity is 280 -300 m. Osm/L § 280 -300 m. Osmol/L- Isotonic § > 300 m. Osmol/L – Hypertonic § < 280 m. Osmol/L - Hypotonic
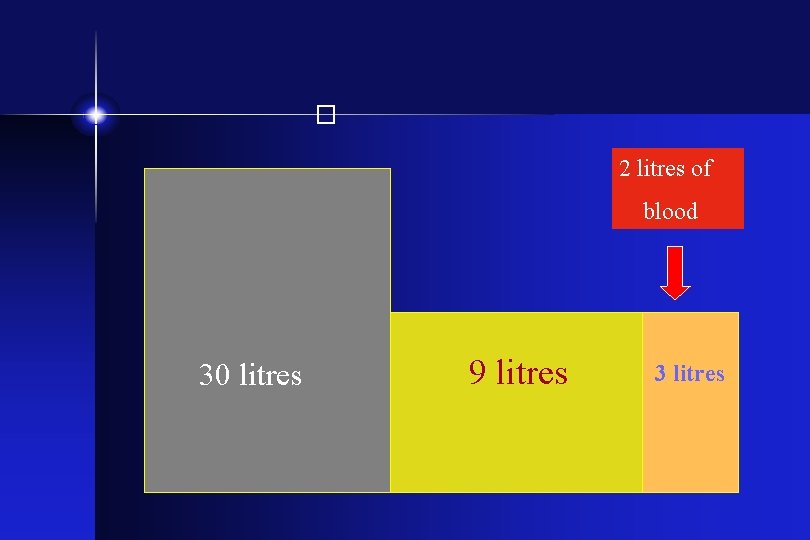
� 2 litres of blood 30 litres 9 litres 3 litres
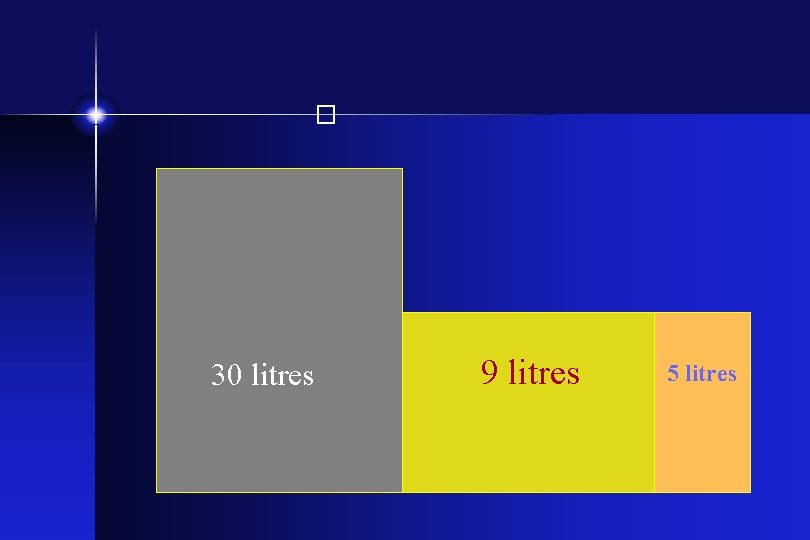
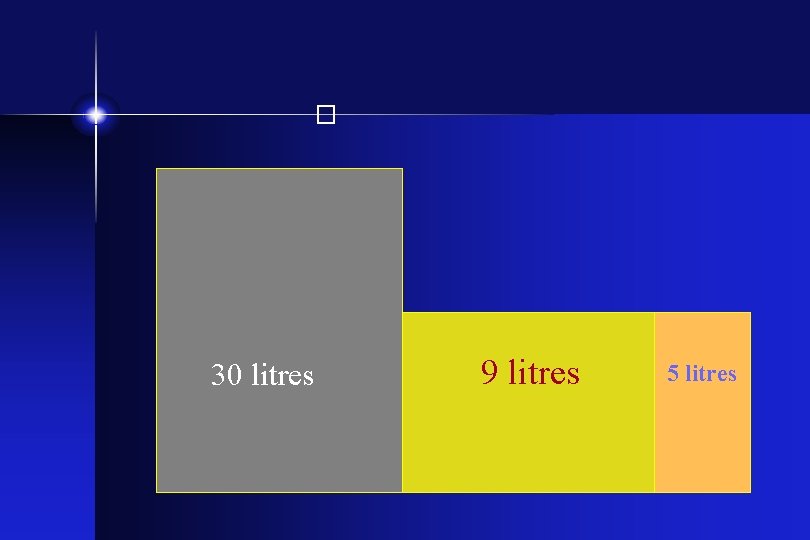
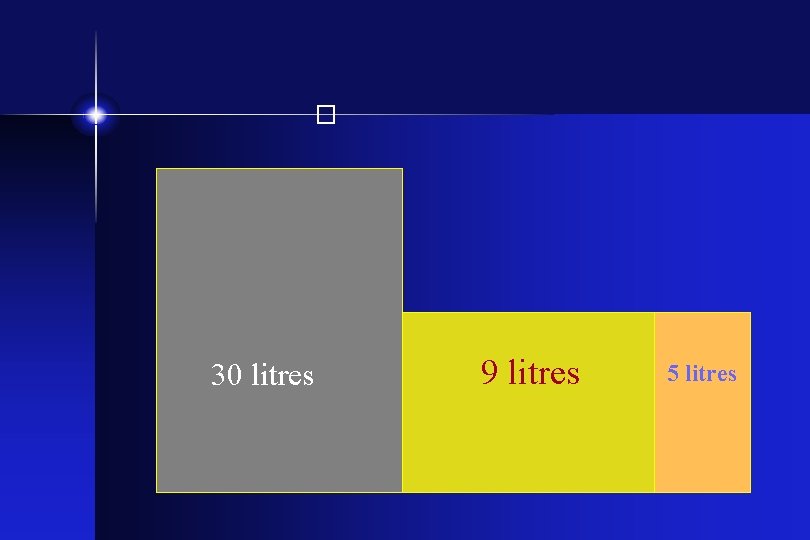
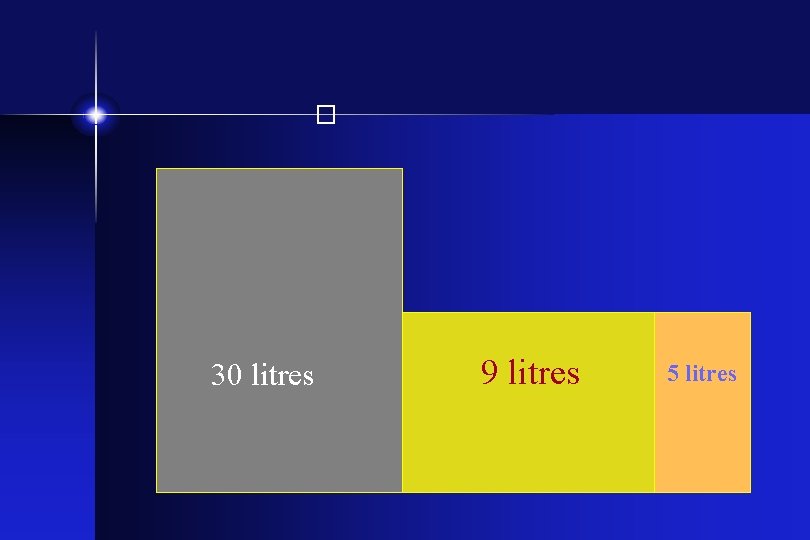
� 30 litres 9 litres 5 litres
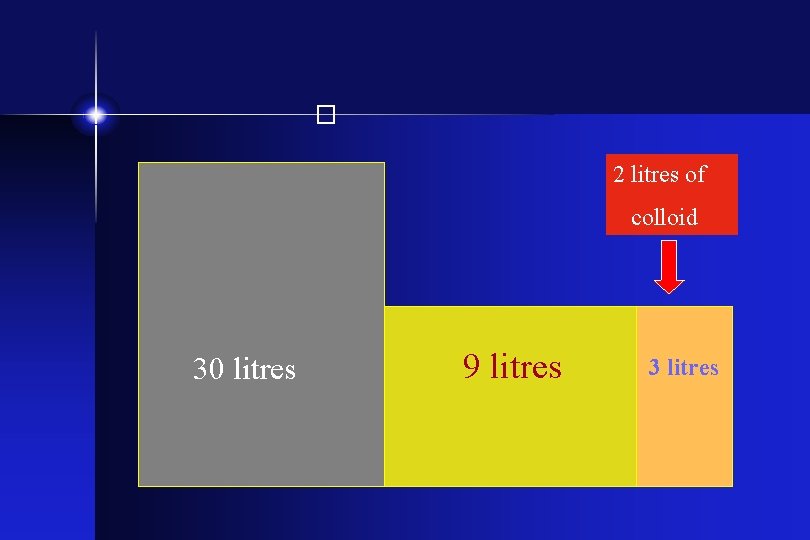
� 2 litres of colloid 30 litres 9 litres 3 litres
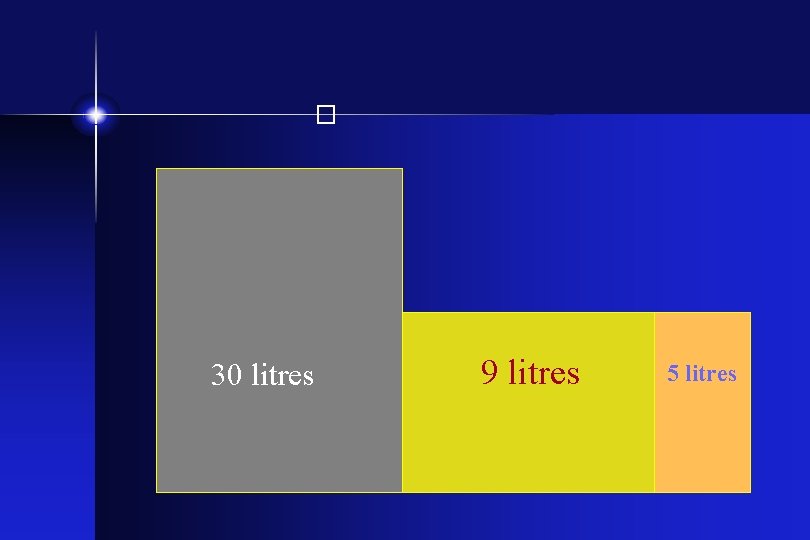
� 30 litres 9 litres 5 litres
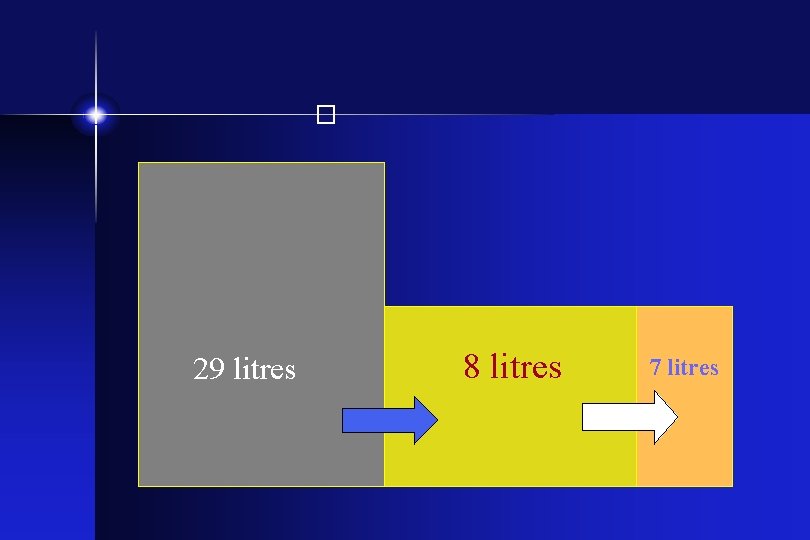
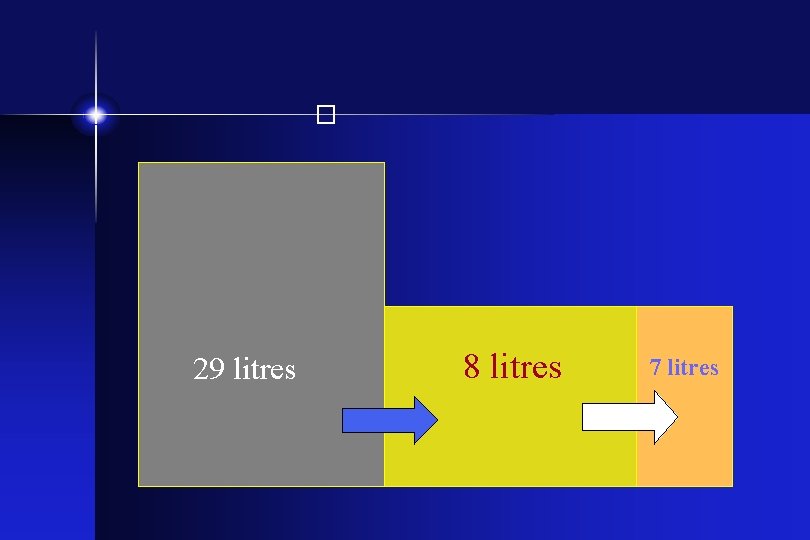
� 29 litres 8 litres 7 litres

� 2 litres of 0. 9% saline 30 litres 9 litres 3 litres
� 30 litres 9 litres 5 litres
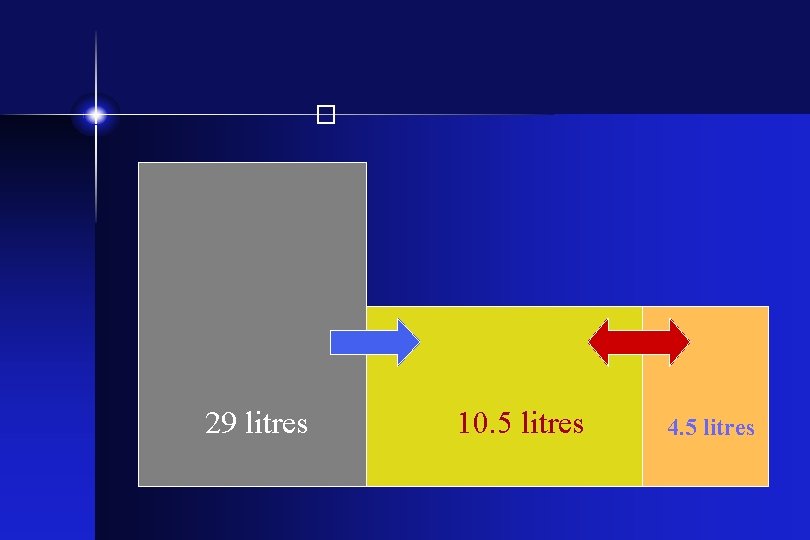
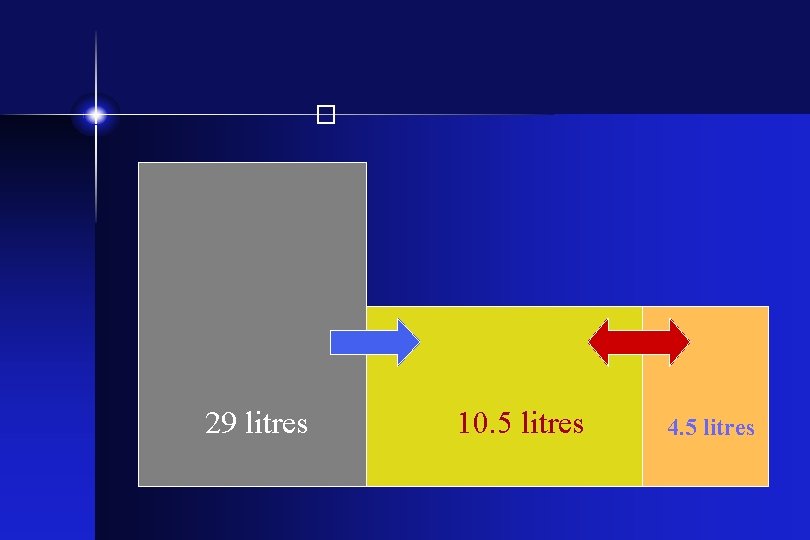
� 29 litres 10. 5 litres 4. 5 litres
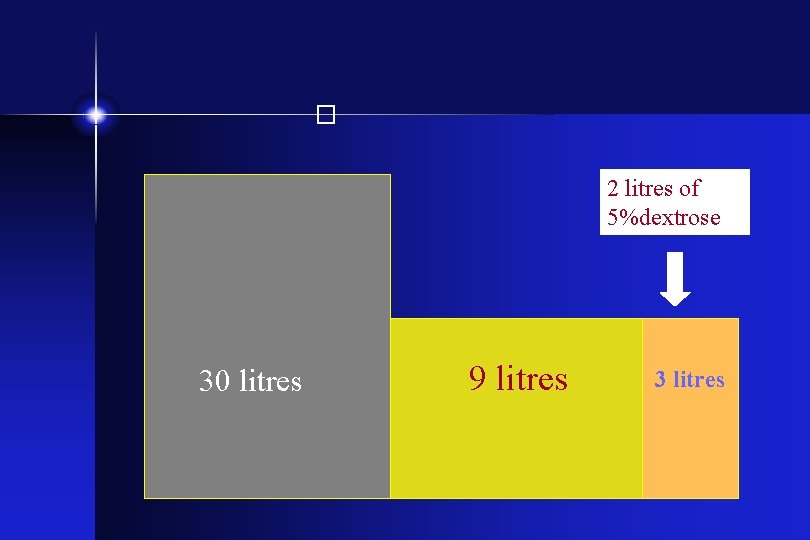
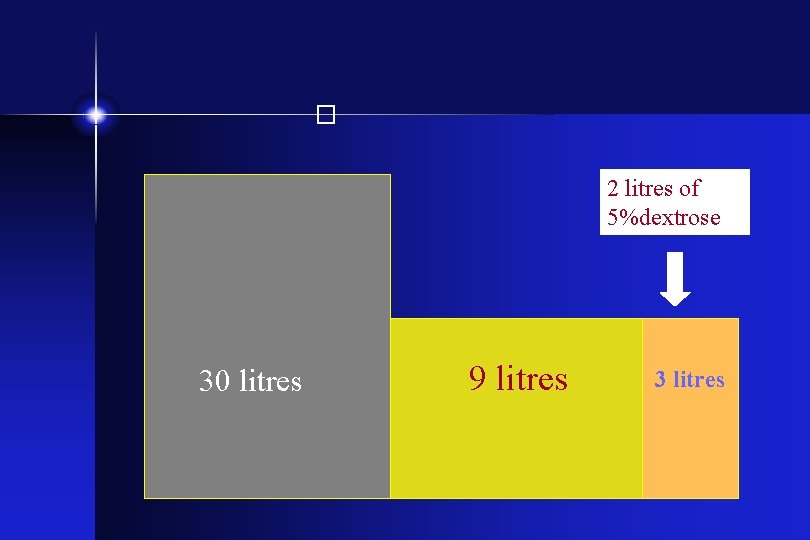
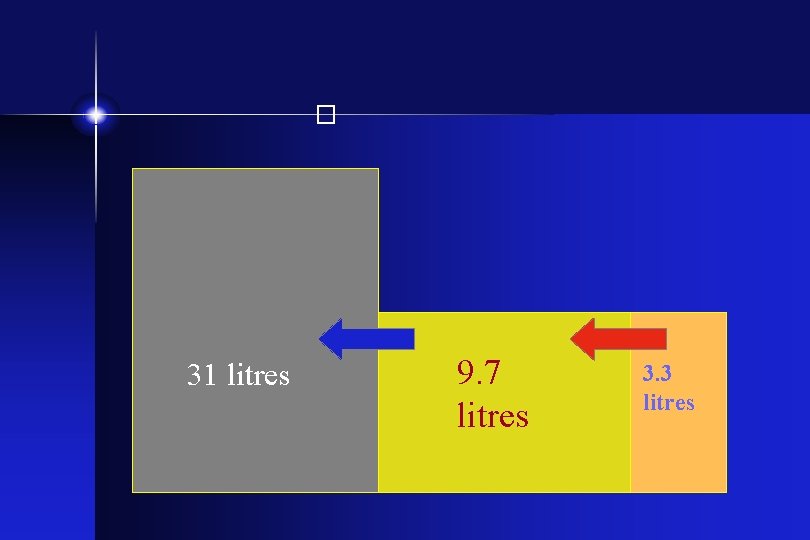
� 2 litres of 5%dextrose 30 litres 9 litres 3 litres
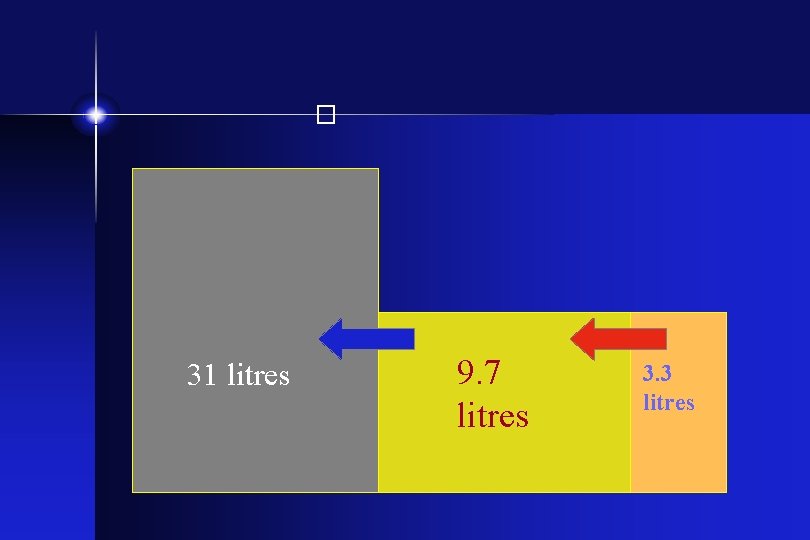
� 31 litres 9. 7 litres 3. 3 litres
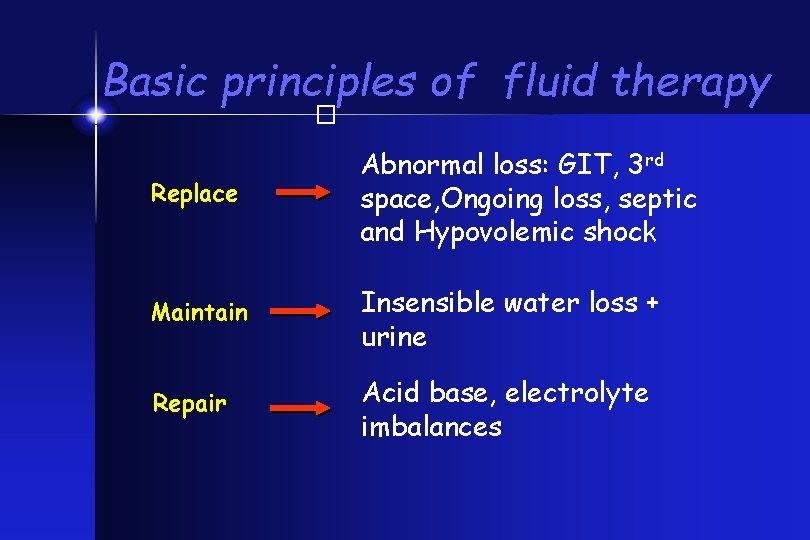
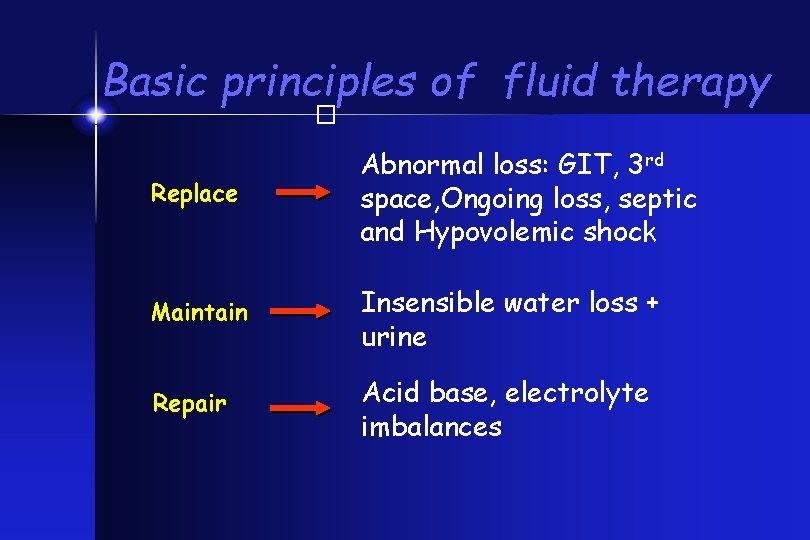
Basic principles of fluid therapy � Replace Abnormal loss: GIT, 3 rd space, Ongoing loss, septic and Hypovolemic shock Maintain Insensible water loss + urine Repair Acid base, electrolyte imbalances
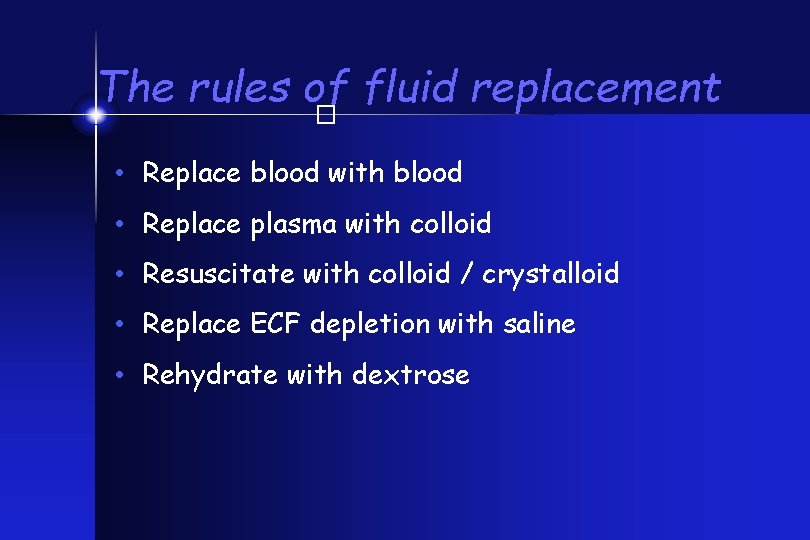
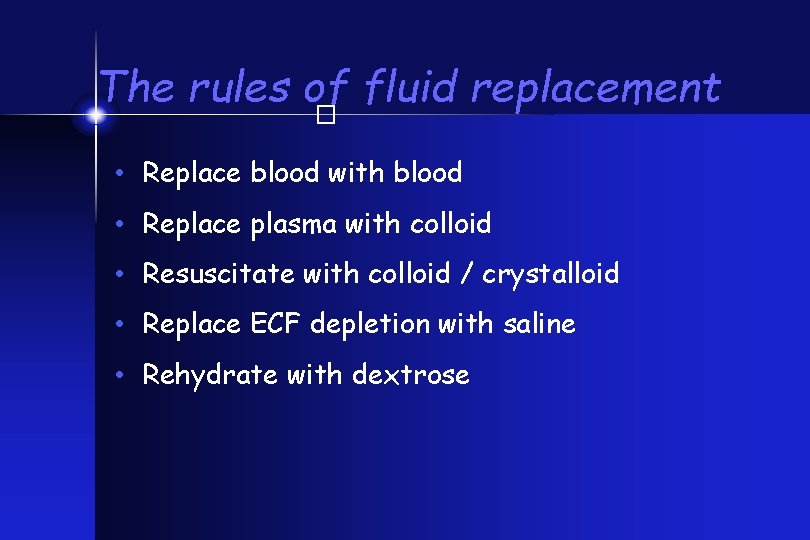
The rules of fluid replacement � • Replace blood with blood • Replace plasma with colloid • Resuscitate with colloid / crystalloid • Replace ECF depletion with saline • Rehydrate with dextrose
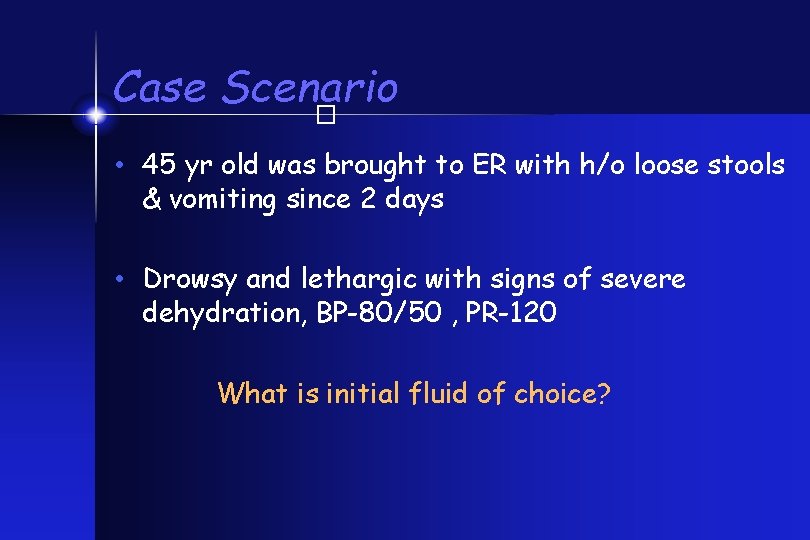
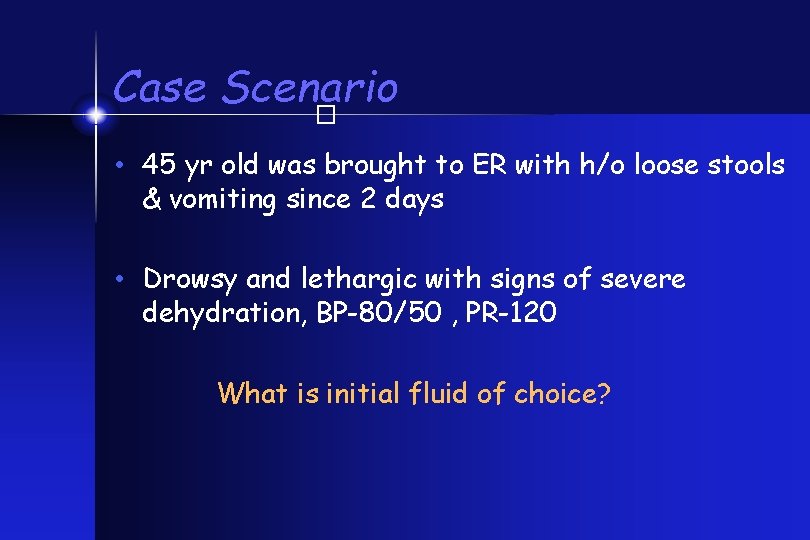
Case Scenario � • 45 yr old was brought to ER with h/o loose stools & vomiting since 2 days • Drowsy and lethargic with signs of severe dehydration, BP-80/50 , PR-120 What is initial fluid of choice?
� • Isotonic saline / Ringer’s lactate • No dextrose containing fluid initially
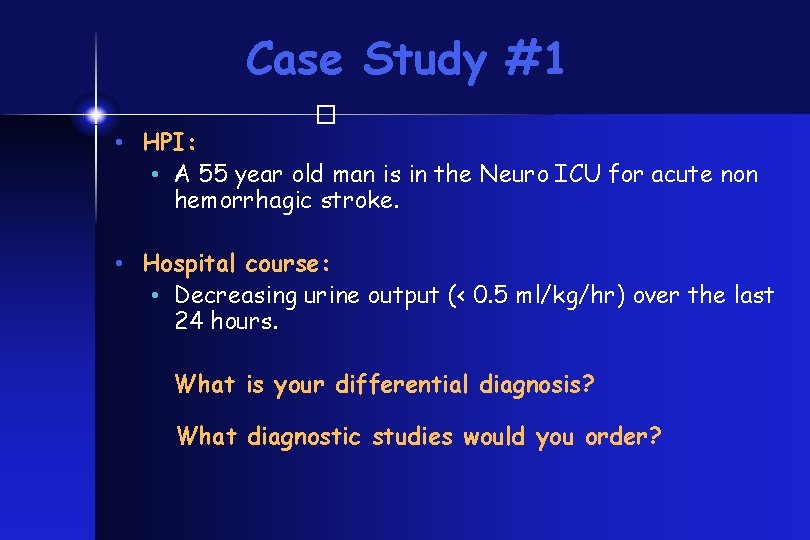
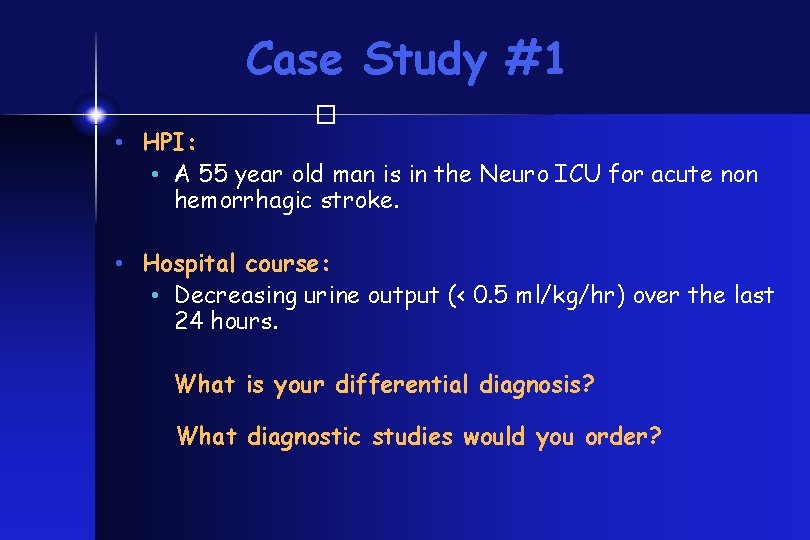
Case Study #1 � • HPI: • A 55 year old man is in the Neuro ICU for acute non hemorrhagic stroke. • Hospital course: • Decreasing urine output (< 0. 5 ml/kg/hr) over the last 24 hours. What is your differential diagnosis? What diagnostic studies would you order?
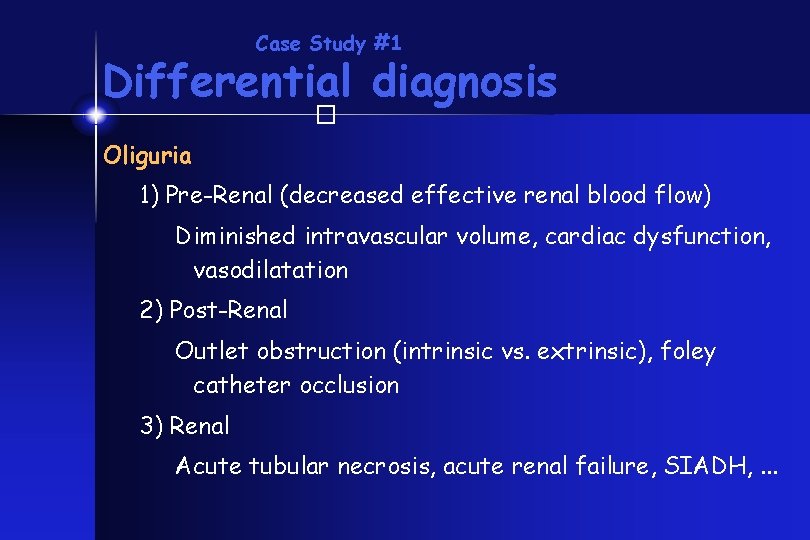
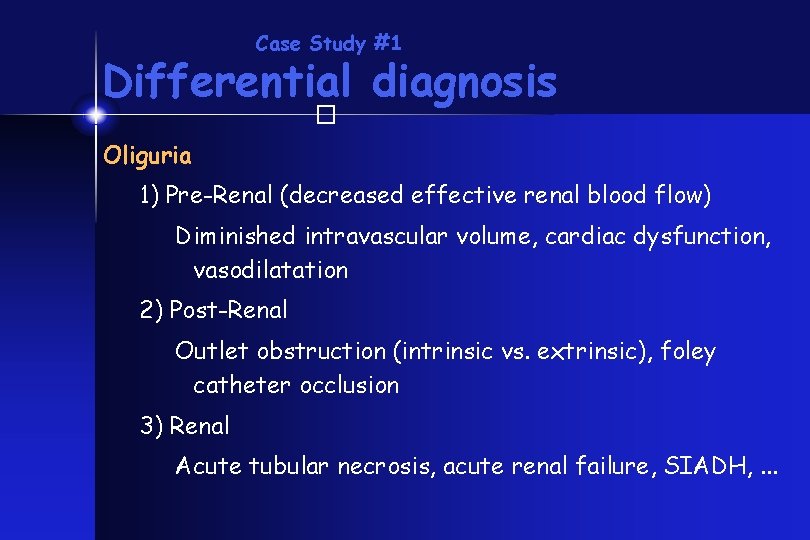
Case Study #1 Differential diagnosis � Oliguria 1) Pre-Renal (decreased effective renal blood flow) Diminished intravascular volume, cardiac dysfunction, vasodilatation 2) Post-Renal Outlet obstruction (intrinsic vs. extrinsic), foley catheter occlusion 3) Renal Acute tubular necrosis, acute renal failure, SIADH, . . .
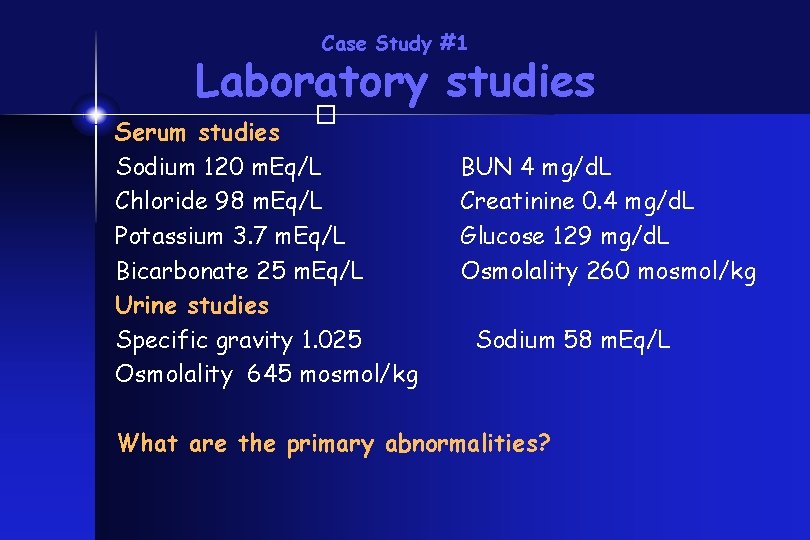
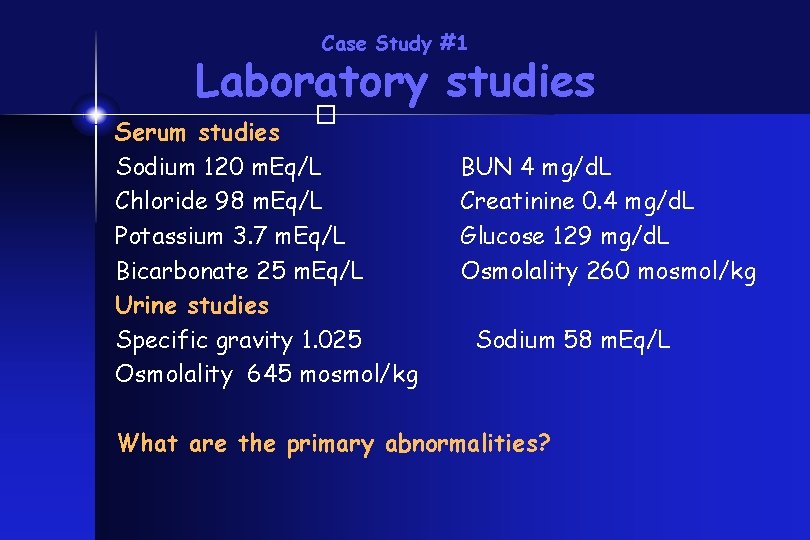
Case Study #1 Laboratory studies � Serum studies Sodium 120 m. Eq/L Chloride 98 m. Eq/L Potassium 3. 7 m. Eq/L Bicarbonate 25 m. Eq/L Urine studies Specific gravity 1. 025 Osmolality 645 mosmol/kg BUN 4 mg/d. L Creatinine 0. 4 mg/d. L Glucose 129 mg/d. L Osmolality 260 mosmol/kg Sodium 58 m. Eq/L What are the primary abnormalities?
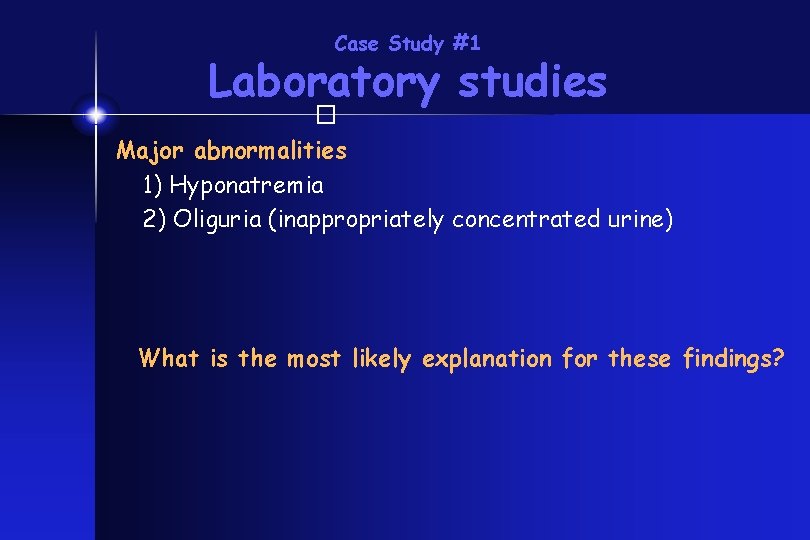
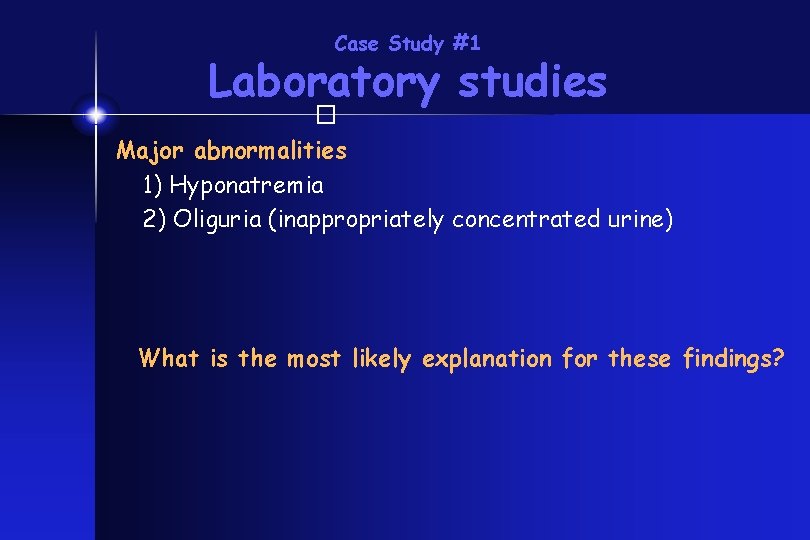
Case Study #1 Laboratory studies � Major abnormalities 1) Hyponatremia 2) Oliguria (inappropriately concentrated urine) What is the most likely explanation for these findings?
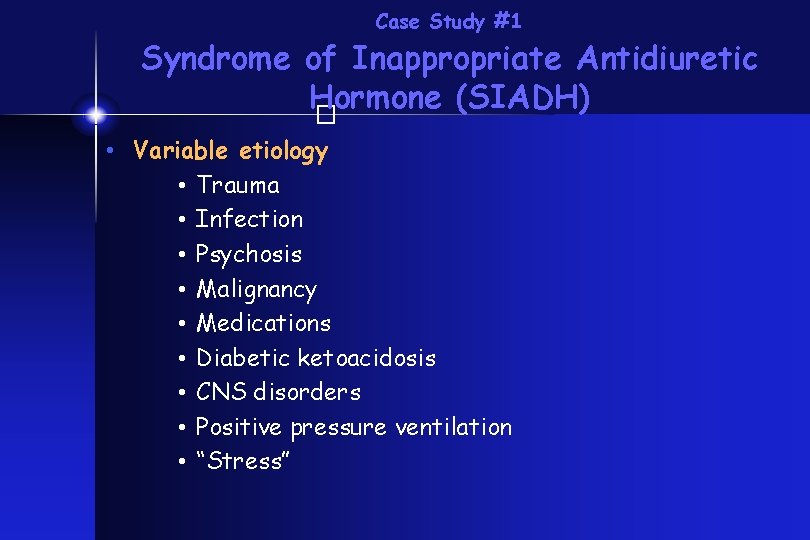
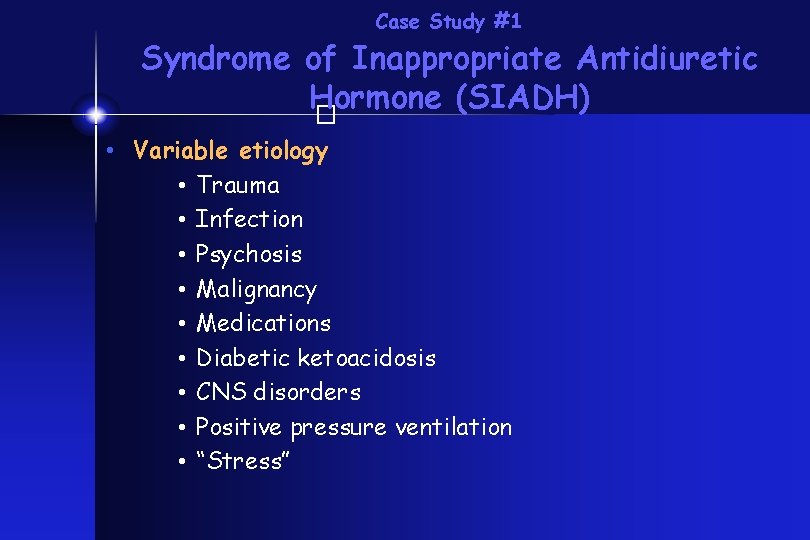
Case Study #1 Syndrome of Inappropriate Antidiuretic Hormone (SIADH) � • Variable etiology • Trauma • Infection • Psychosis • Malignancy • Medications • Diabetic ketoacidosis • CNS disorders • Positive pressure ventilation • “Stress”
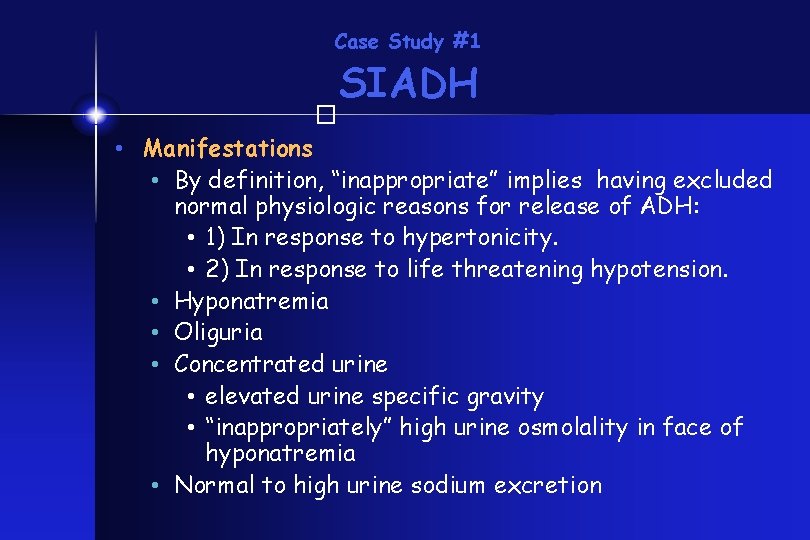
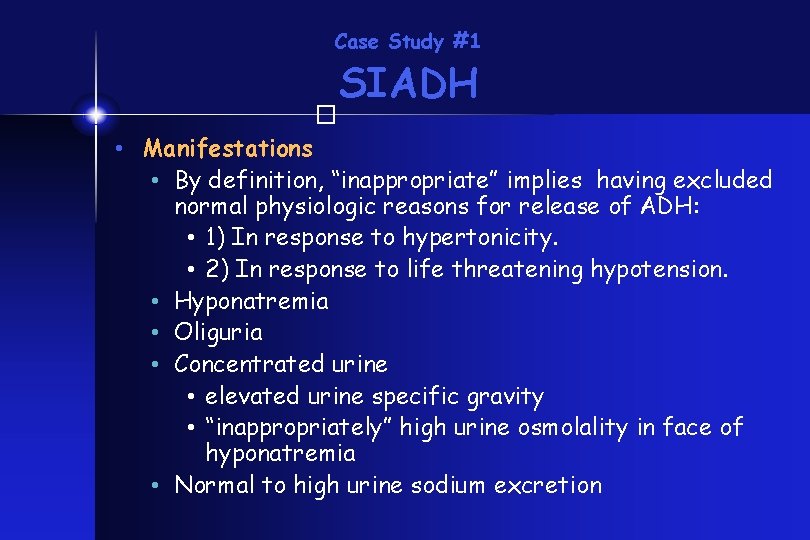
Case Study #1 SIADH � • Manifestations • By definition, “inappropriate” implies having excluded normal physiologic reasons for release of ADH: • 1) In response to hypertonicity. • 2) In response to life threatening hypotension. • Hyponatremia • Oliguria • Concentrated urine • elevated urine specific gravity • “inappropriately” high urine osmolality in face of hyponatremia • Normal to high urine sodium excretion
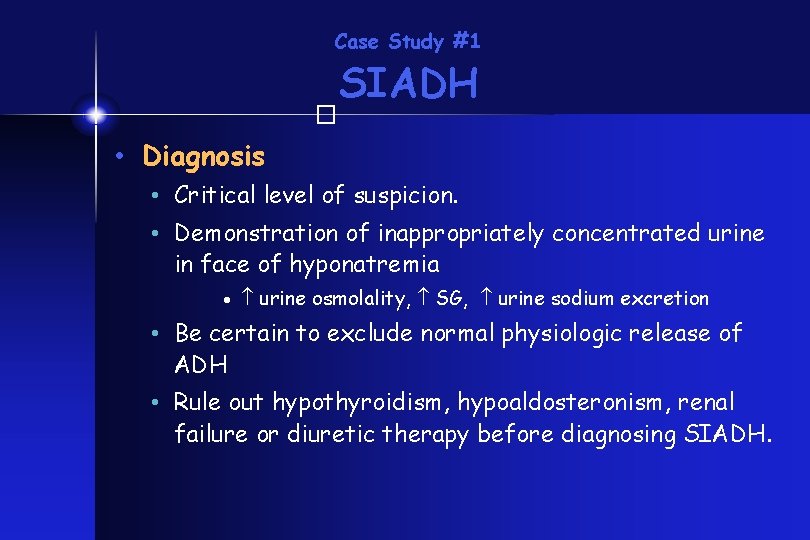
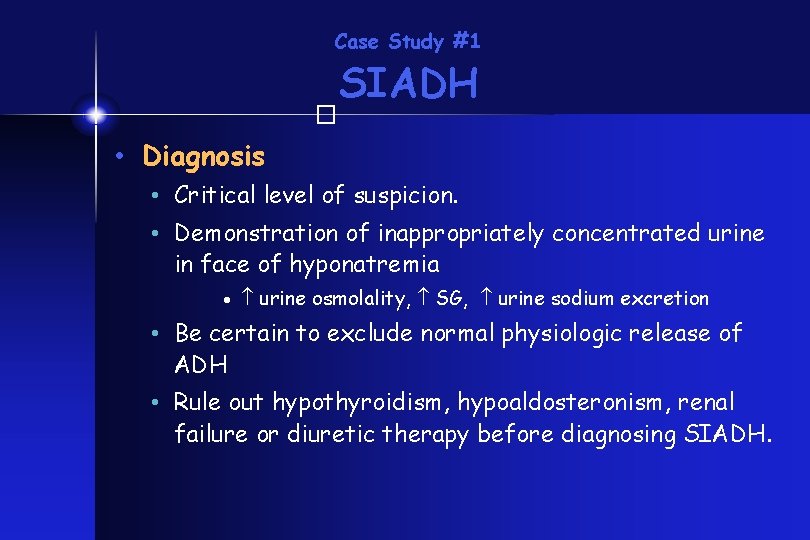
Case Study #1 SIADH � • Diagnosis • Critical level of suspicion. • Demonstration of inappropriately concentrated urine in face of hyponatremia · urine osmolality, SG, urine sodium excretion • Be certain to exclude normal physiologic release of ADH • Rule out hypothyroidism, hypoaldosteronism, renal failure or diuretic therapy before diagnosing SIADH.
Case Study #1 SIADH � • Treatment • Fluid restriction • Avoid hypotonic fluids • Hypertonic saline / oral sodium chloride • Frusemide.
Case Study #1 The saga continues…. � Hospital course: Four hours after beginning fluid restriction, you are called because the patient is having a generalized seizure. There is no response to two doses of IV lorazepam and a loading dose of fosphenytoin What is the most likely explanation?
Case Study #1 The saga continues � Seizure 1) Worsening hyponatremia 2) Intracranial event 3) Meningitis 4) Other electrolyte disturbance 5) Medication 6) Hypertension What diagnostic studies would you order?
Case Study #1 The saga continues � Stat labs: Sodium 110 m. Eq/L What would you do now?
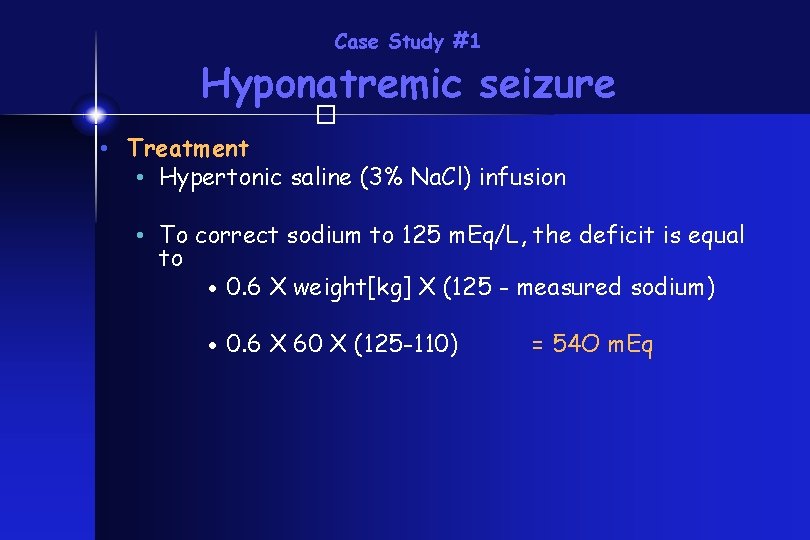
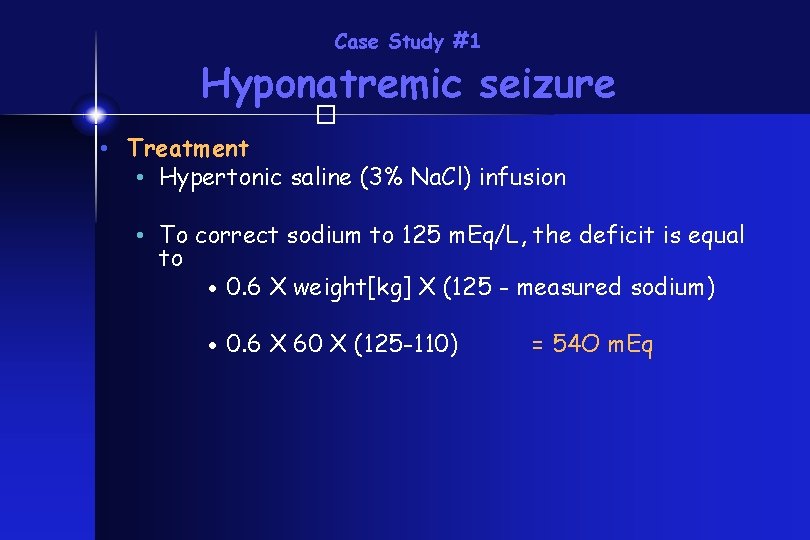
Case Study #1 Hyponatremic seizure � • Treatment • Hypertonic saline (3% Na. Cl) infusion • To correct sodium to 125 m. Eq/L, the deficit is equal to · 0. 6 X weight[kg] X (125 - measured sodium) · 0. 6 X 60 X (125 -110) = 54 O m. Eq
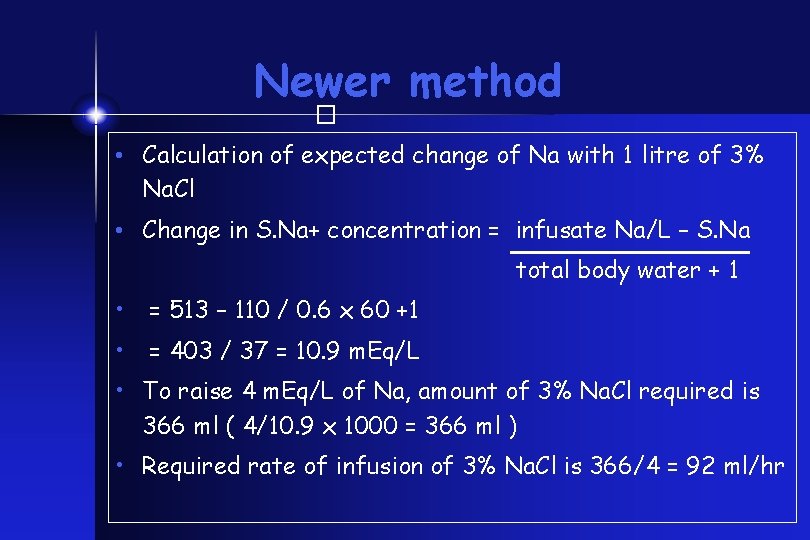
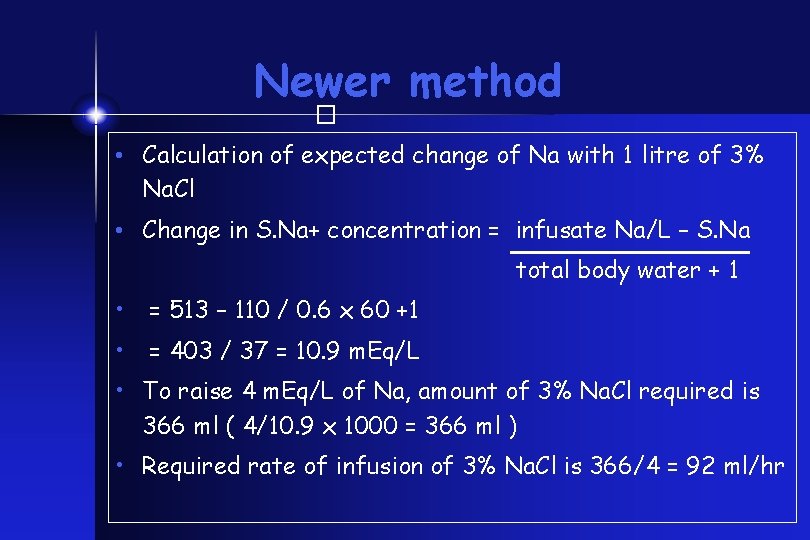
Newer method � • Calculation of expected change of Na with 1 litre of 3% Na. Cl • Change in S. Na+ concentration = infusate Na/L – S. Na total body water + 1 • = 513 – 110 / 0. 6 x 60 +1 • = 403 / 37 = 10. 9 m. Eq/L • To raise 4 m. Eq/L of Na, amount of 3% Na. Cl required is 366 ml ( 4/10. 9 x 1000 = 366 ml ) • Required rate of infusion of 3% Na. Cl is 366/4 = 92 ml/hr
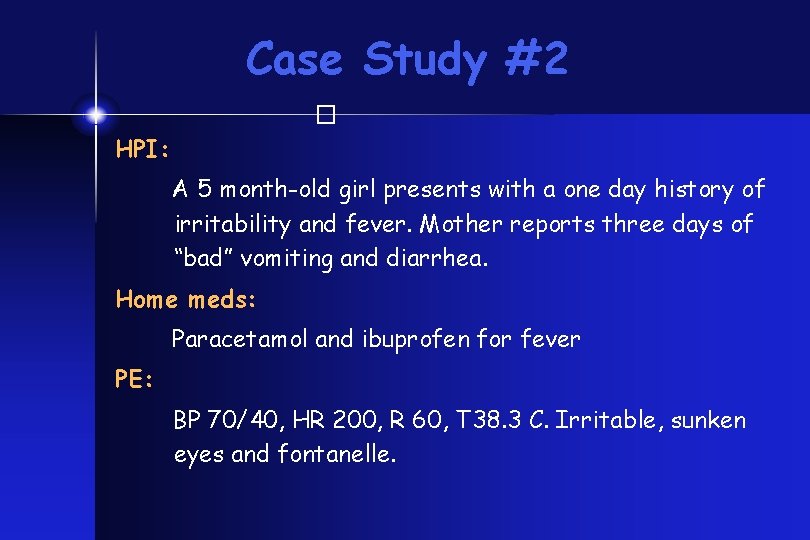
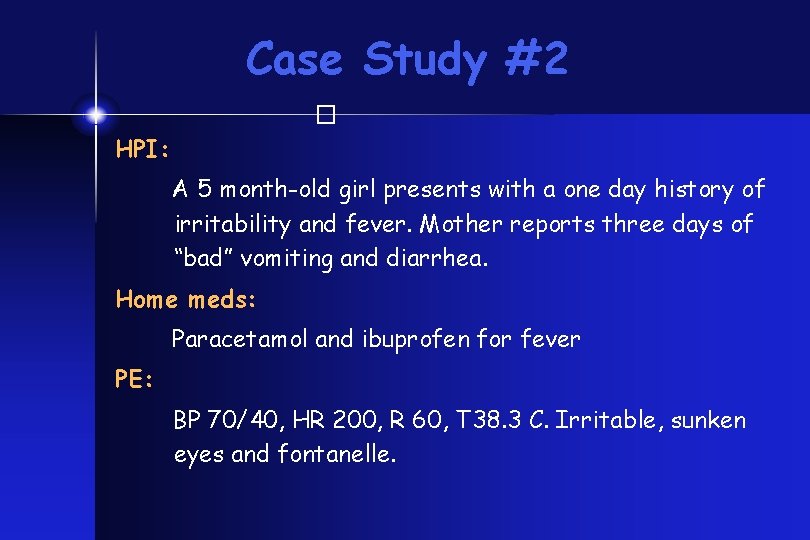
Case Study #2 � HPI: A 5 month-old girl presents with a one day history of irritability and fever. Mother reports three days of “bad” vomiting and diarrhea. Home meds: Paracetamol and ibuprofen for fever PE: BP 70/40, HR 200, R 60, T 38. 3 C. Irritable, sunken eyes and fontanelle.
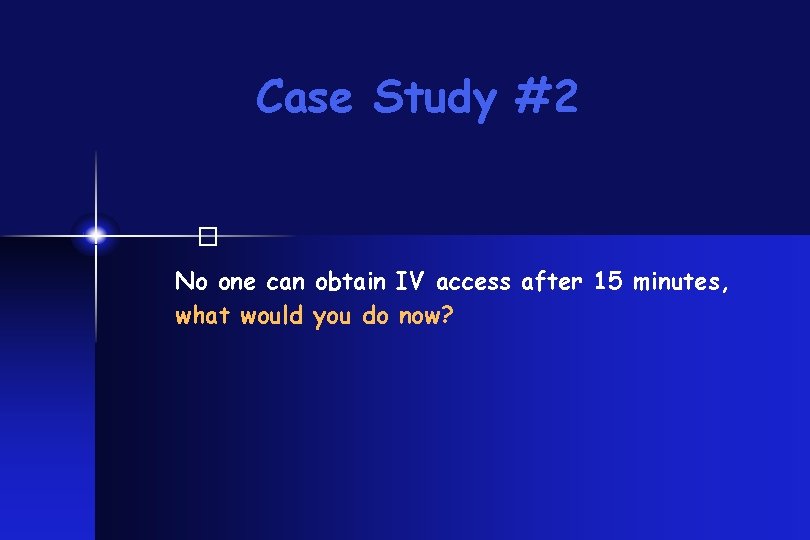
Case Study #2 � No one can obtain IV access after 15 minutes, what would you do now?
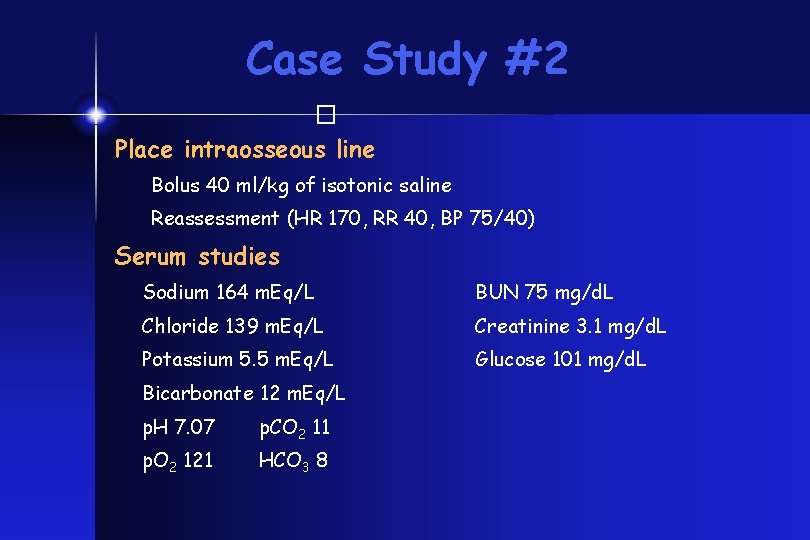
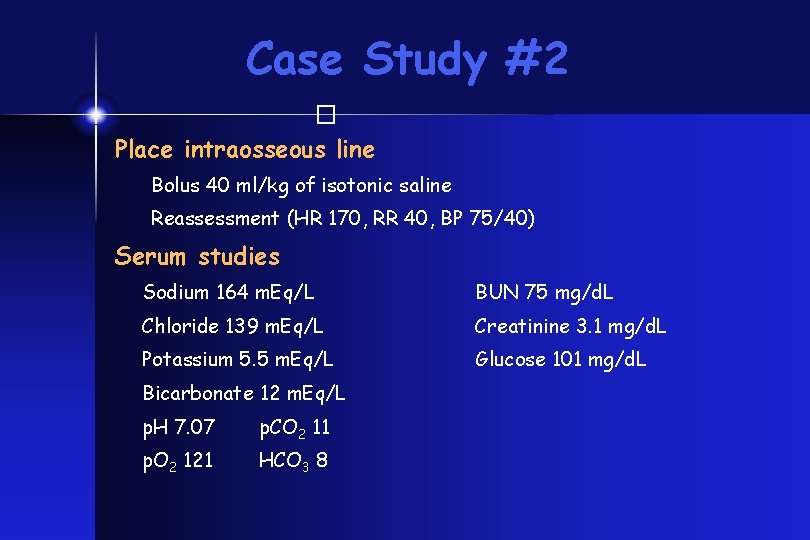
Case Study #2 � Place intraosseous line Bolus 40 ml/kg of isotonic saline Reassessment (HR 170, RR 40, BP 75/40) Serum studies Sodium 164 m. Eq/L BUN 75 mg/d. L Chloride 139 m. Eq/L Creatinine 3. 1 mg/d. L Potassium 5. 5 m. Eq/L Glucose 101 mg/d. L Bicarbonate 12 m. Eq/L p. H 7. 07 p. CO 2 11 p. O 2 121 HCO 3 8
Case Study #2 � What is the most likely explanation of this patients acidosis?
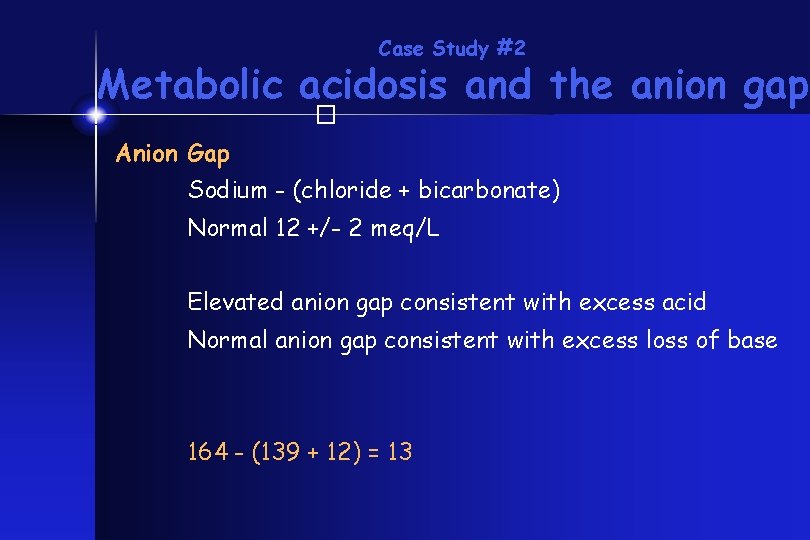
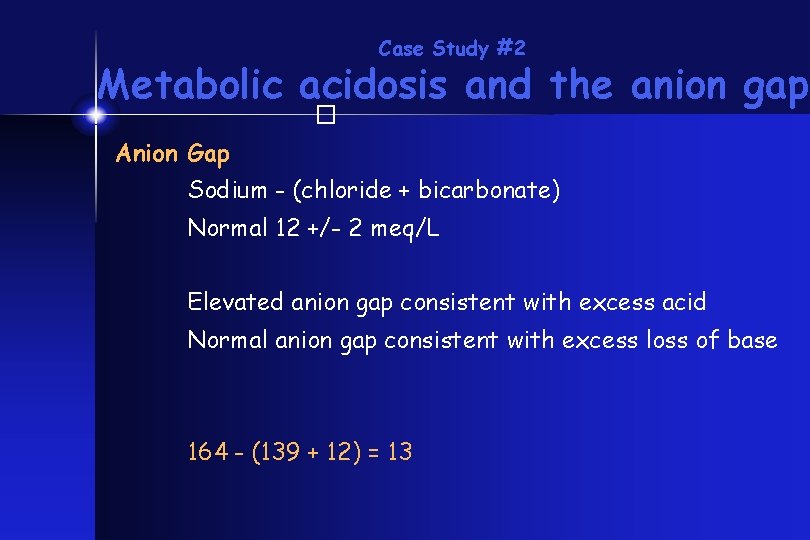
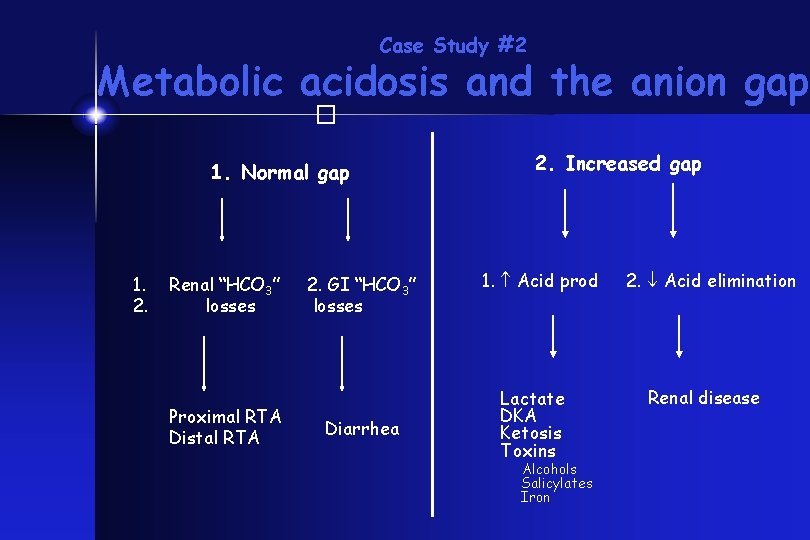
Case Study #2 Metabolic acidosis and the anion gap � Anion Gap Sodium - (chloride + bicarbonate) Normal 12 +/- 2 meq/L Elevated anion gap consistent with excess acid Normal anion gap consistent with excess loss of base 164 - (139 + 12) = 13
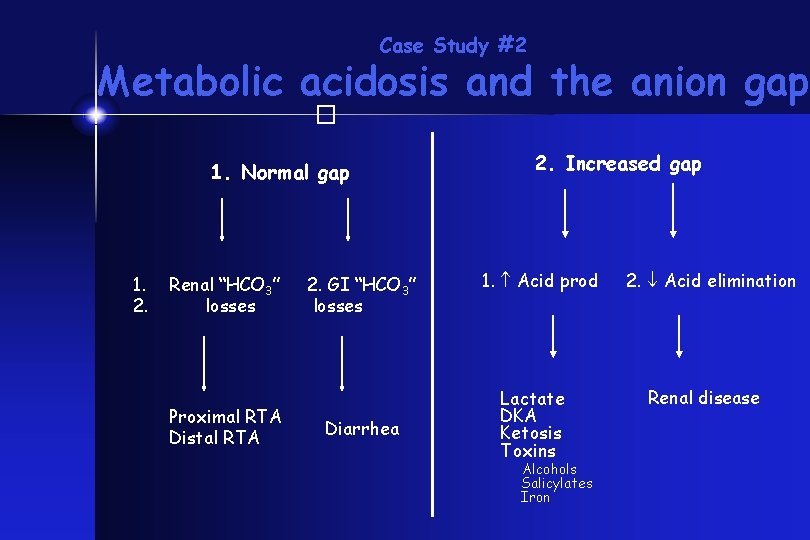
Case Study #2 Metabolic acidosis and the anion gap � 1. Normal gap 1. 2. Renal “HCO 3” losses Proximal RTA Distal RTA 2. GI “HCO 3” losses Diarrhea 2. Increased gap 1. Acid prod Lactate DKA Ketosis Toxins Alcohols Salicylates Iron 2. Acid elimination Renal disease
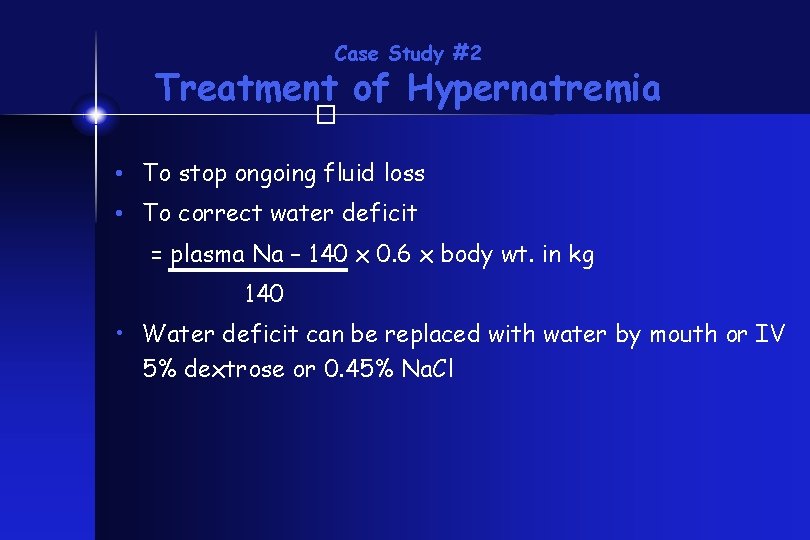
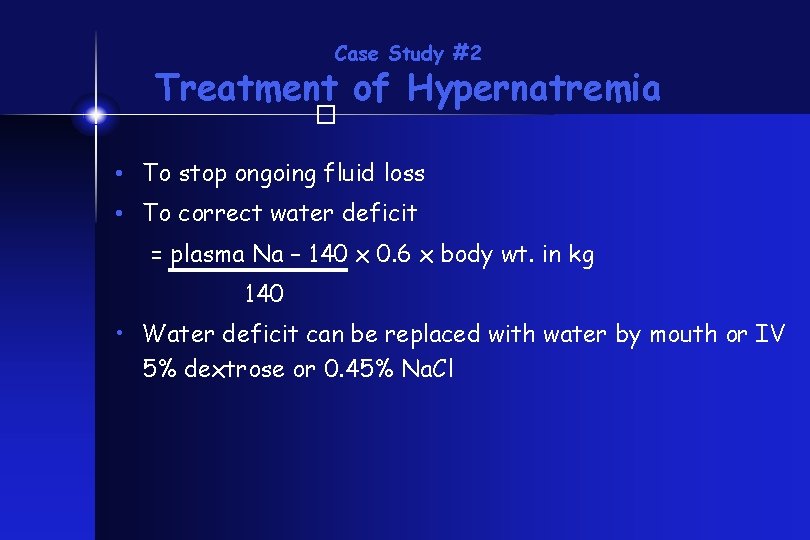
Case Study #2 Treatment of Hypernatremia � • To stop ongoing fluid loss • To correct water deficit = plasma Na – 140 x 0. 6 x body wt. in kg 140 • Water deficit can be replaced with water by mouth or IV 5% dextrose or 0. 45% Na. Cl
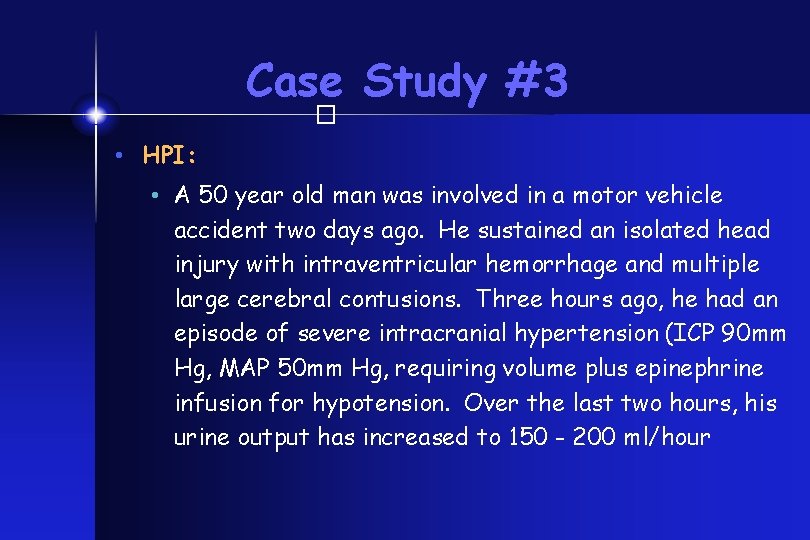
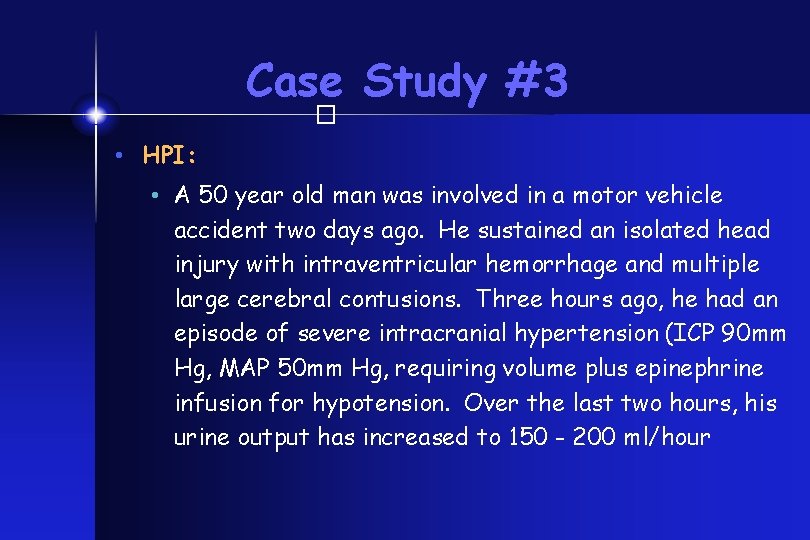
Case Study #3 � • HPI: • A 50 year old man was involved in a motor vehicle accident two days ago. He sustained an isolated head injury with intraventricular hemorrhage and multiple large cerebral contusions. Three hours ago, he had an episode of severe intracranial hypertension (ICP 90 mm Hg, MAP 50 mm Hg, requiring volume plus epinephrine infusion for hypotension. Over the last two hours, his urine output has increased to 150 - 200 ml/hour
� What is your differential diagnosis? What test would you order?
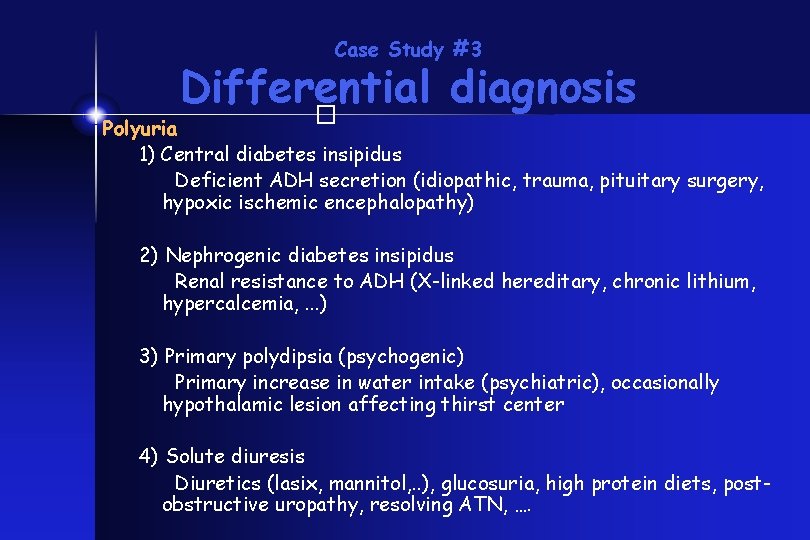
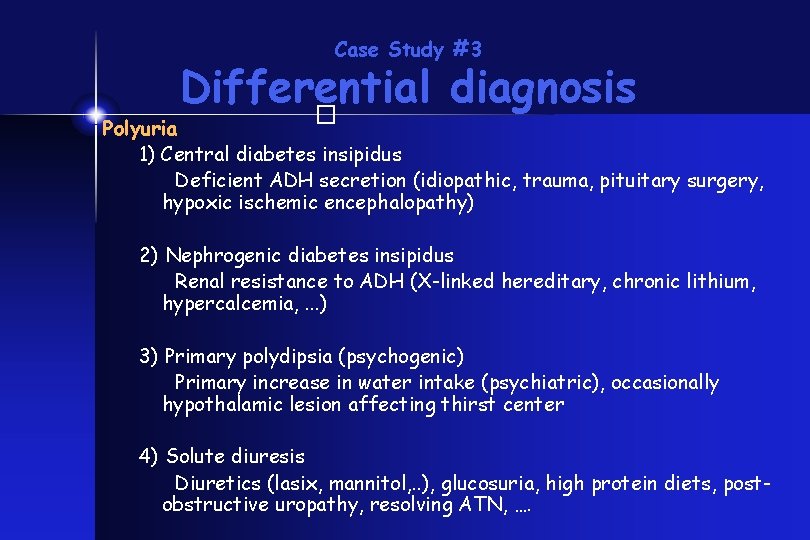
Case Study #3 Differential diagnosis � Polyuria 1) Central diabetes insipidus Deficient ADH secretion (idiopathic, trauma, pituitary surgery, hypoxic ischemic encephalopathy) 2) Nephrogenic diabetes insipidus Renal resistance to ADH (X-linked hereditary, chronic lithium, hypercalcemia, . . . ) 3) Primary polydipsia (psychogenic) Primary increase in water intake (psychiatric), occasionally hypothalamic lesion affecting thirst center 4) Solute diuresis Diuretics (lasix, mannitol, . . ), glucosuria, high protein diets, postobstructive uropathy, resolving ATN, ….
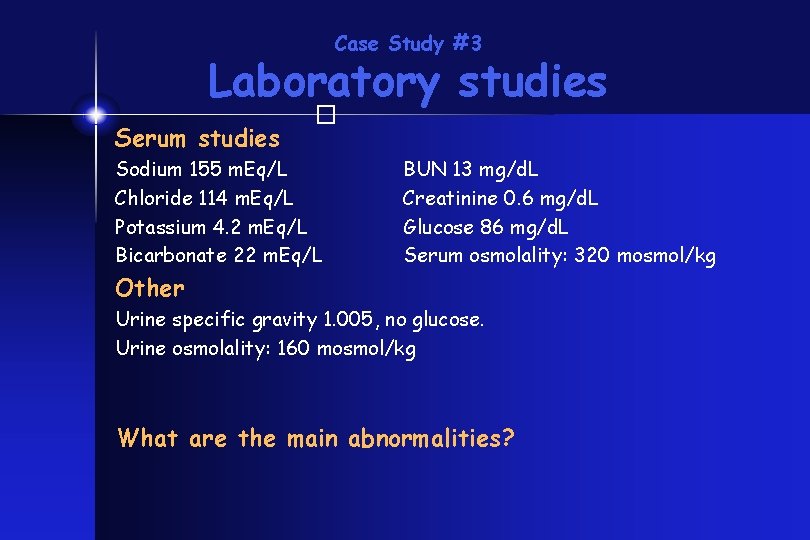
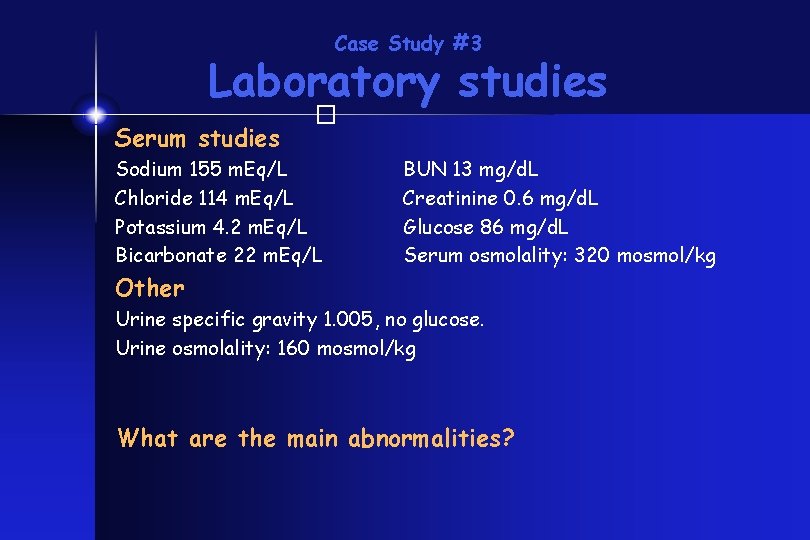
Case Study #3 Laboratory studies � Serum studies Sodium 155 m. Eq/L Chloride 114 m. Eq/L Potassium 4. 2 m. Eq/L Bicarbonate 22 m. Eq/L BUN 13 mg/d. L Creatinine 0. 6 mg/d. L Glucose 86 mg/d. L Serum osmolality: 320 mosmol/kg Other Urine specific gravity 1. 005, no glucose. Urine osmolality: 160 mosmol/kg What are the main abnormalities?
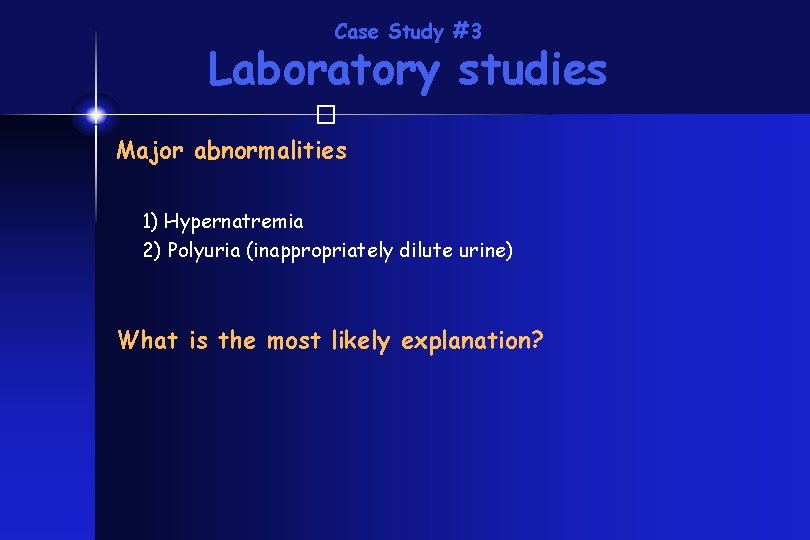
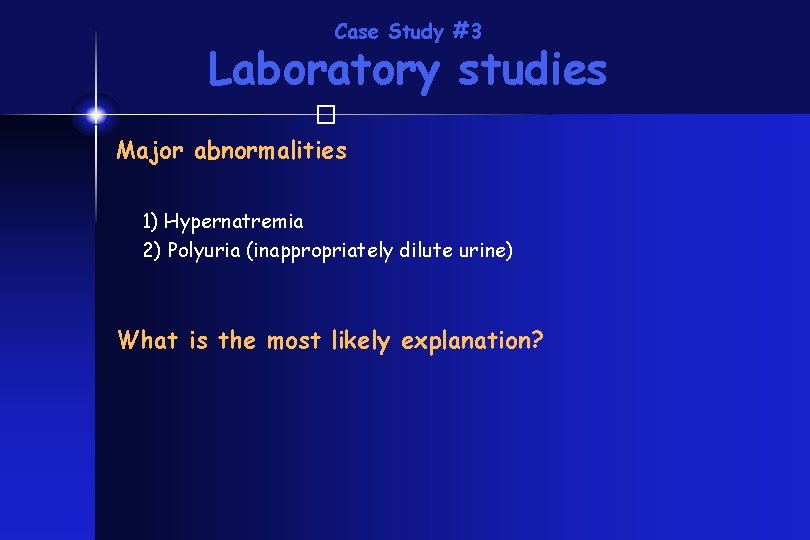
Case Study #3 Laboratory studies � Major abnormalities 1) Hypernatremia 2) Polyuria (inappropriately dilute urine) What is the most likely explanation?
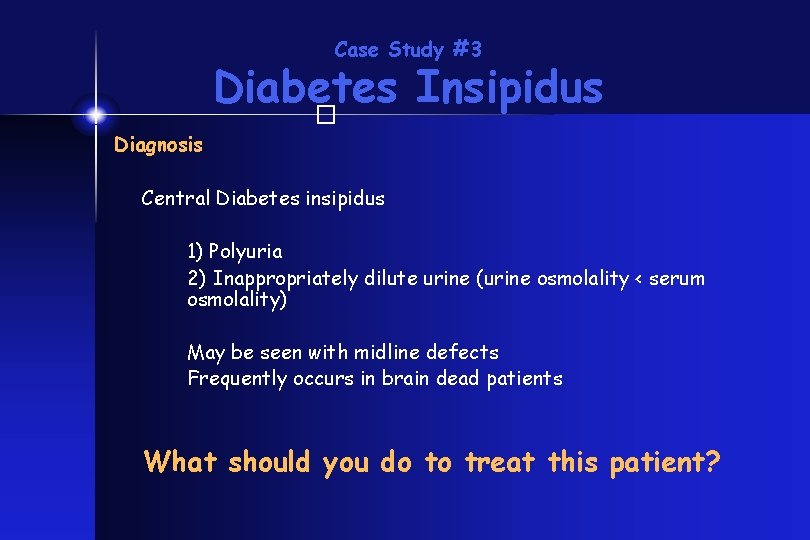
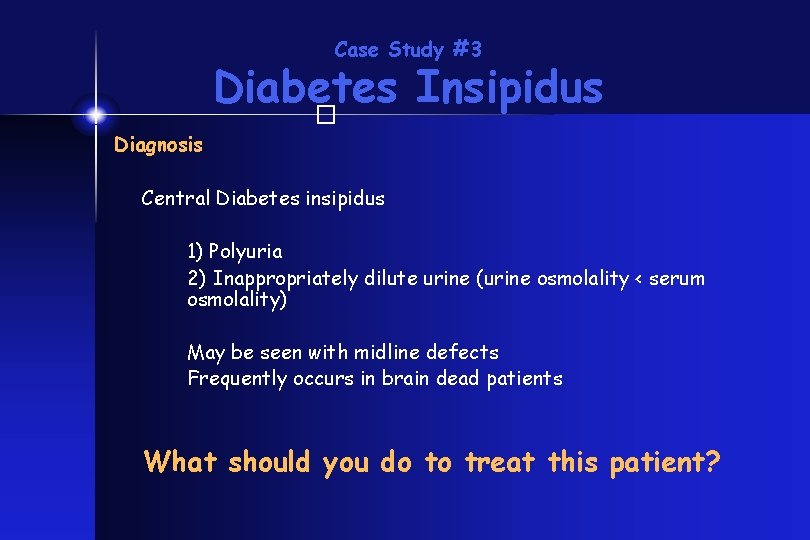
Case Study #3 Diabetes Insipidus � Diagnosis Central Diabetes insipidus 1) Polyuria 2) Inappropriately dilute urine (urine osmolality < serum osmolality) May be seen with midline defects Frequently occurs in brain dead patients What should you do to treat this patient?
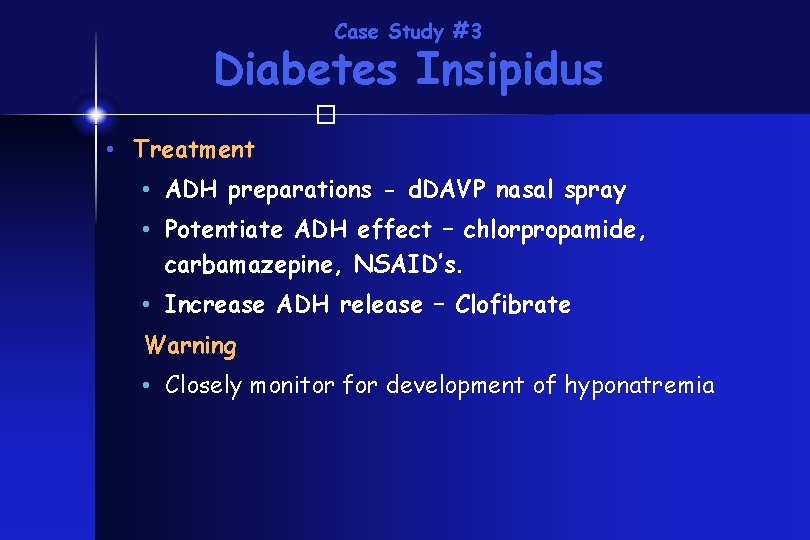
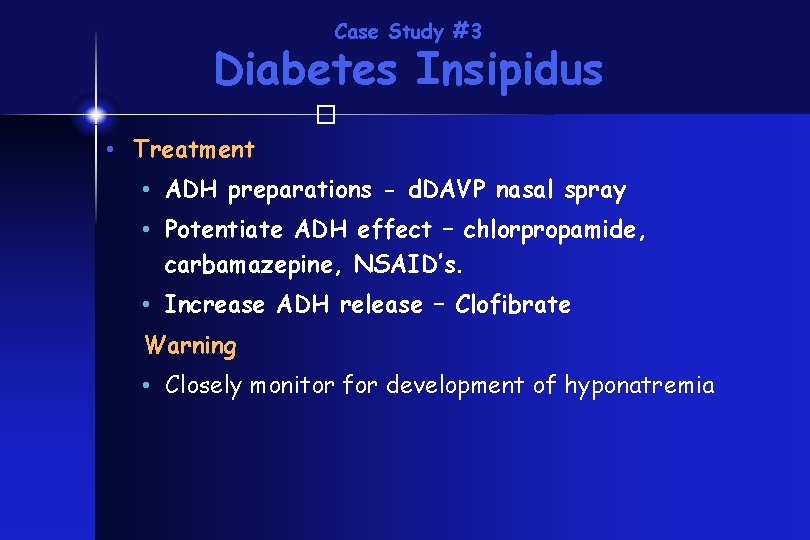
Case Study #3 Diabetes Insipidus � • Treatment • ADH preparations - d. DAVP nasal spray • Potentiate ADH effect – chlorpropamide, carbamazepine, NSAID’s. • Increase ADH release – Clofibrate Warning • Closely monitor for development of hyponatremia
Case Study #4 � • HPI: • An 35 year old lady with Chronic kidney disease presents with irritability. She is on nightly peritoneal dialysis at home. The lab calls a panic potassium value of 7. 1 meq/L. The tech says it is not hemolyzed. What do you do now?
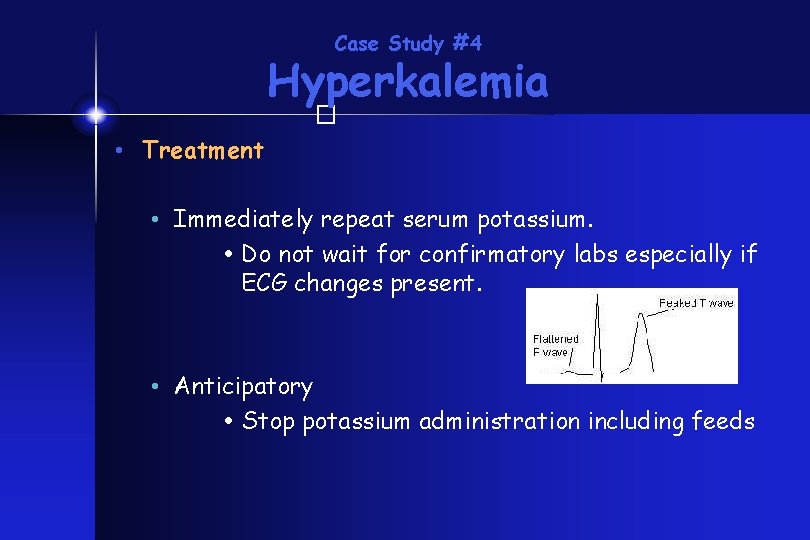
Case Study #4 Hyperkalemia � • Treatment • Immediately repeat serum potassium. Do not wait for confirmatory labs especially if ECG changes present. • Anticipatory Stop potassium administration including feeds
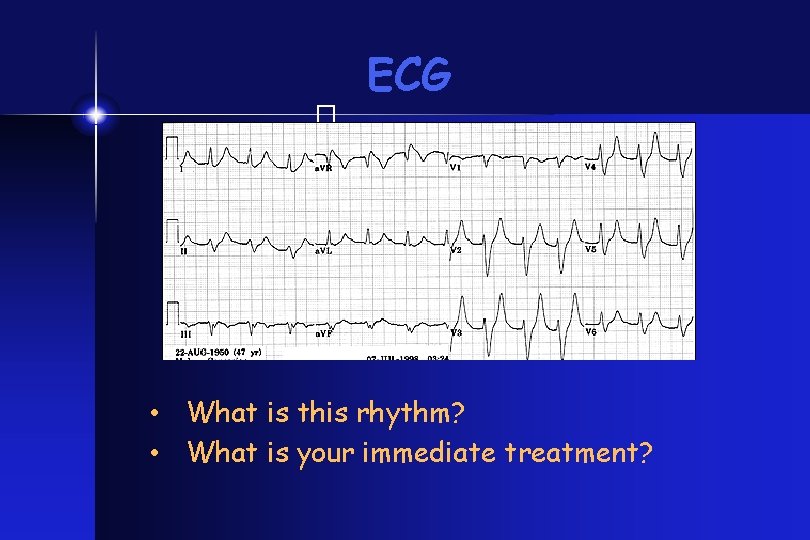
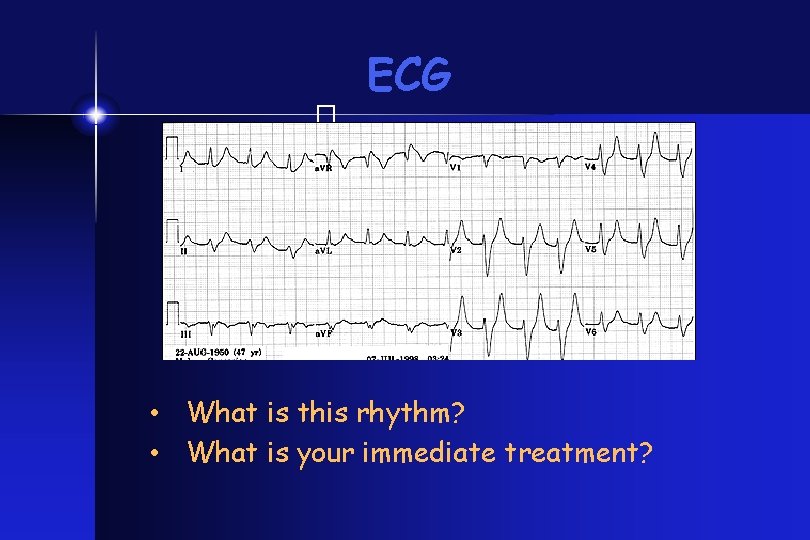
ECG � • What is this rhythm? • What is your immediate treatment?
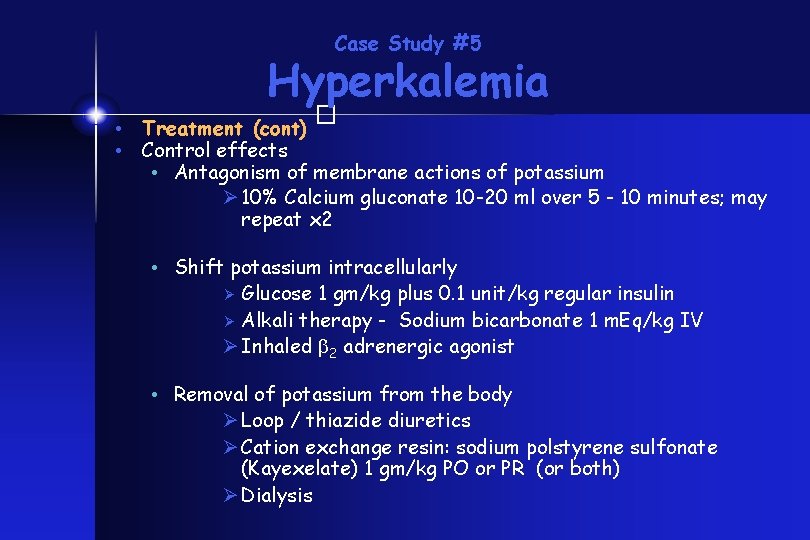
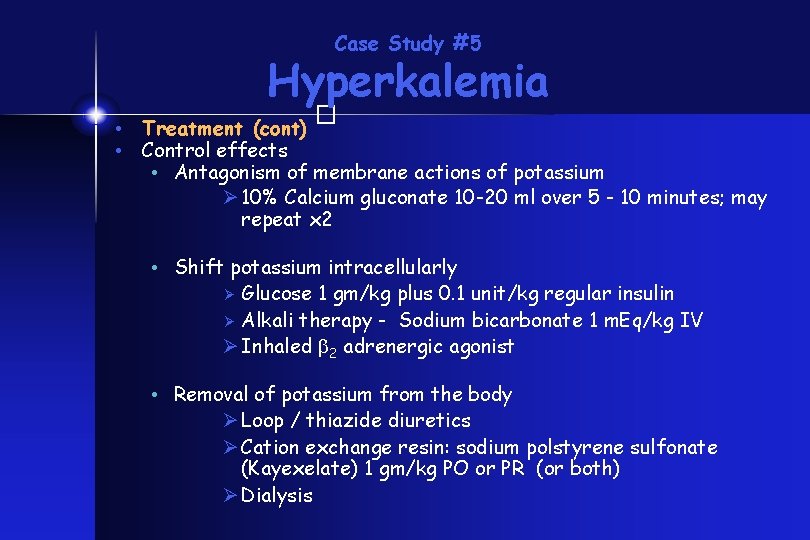
Case Study #5 Hyperkalemia � • Treatment (cont) • Control effects • Antagonism of membrane actions of potassium Ø 10% Calcium gluconate 10 -20 ml over 5 - 10 minutes; may repeat x 2 • Shift potassium intracellularly Ø Glucose 1 gm/kg plus 0. 1 unit/kg regular insulin Ø Alkali therapy - Sodium bicarbonate 1 m. Eq/kg IV Ø Inhaled 2 adrenergic agonist • Removal of potassium from the body Ø Loop / thiazide diuretics Ø Cation exchange resin: sodium polstyrene sulfonate (Kayexelate) 1 gm/kg PO or PR (or both) Ø Dialysis
Case Study #5 � • HPI: • A three year old boy is recovering from septic shock. He received 150 ml/kg in fluid boluses in the first 24 hours and has anasarca. You begin him on a frusemide infusion for diuresis. He develops severe weakness and begins to hypoventilate. You notice unifocal premature ventricular beats on his cardiac monitor.
� What is your differential diagnosis? What tests would you order?
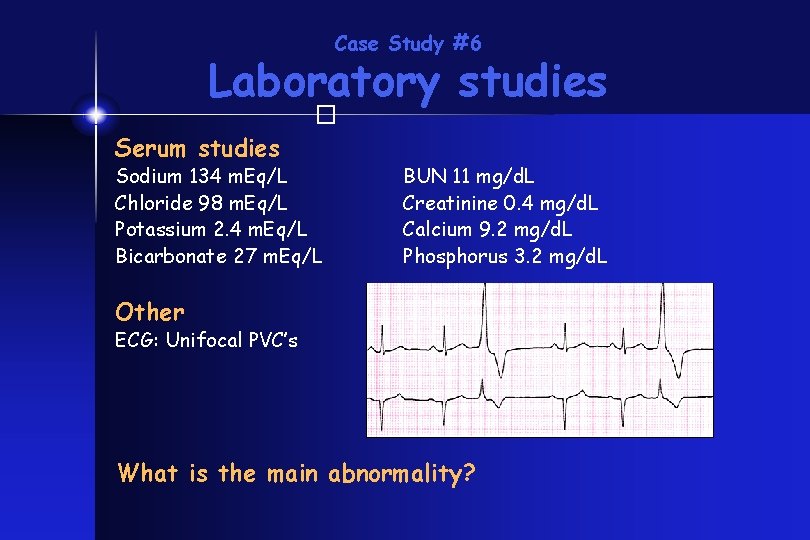
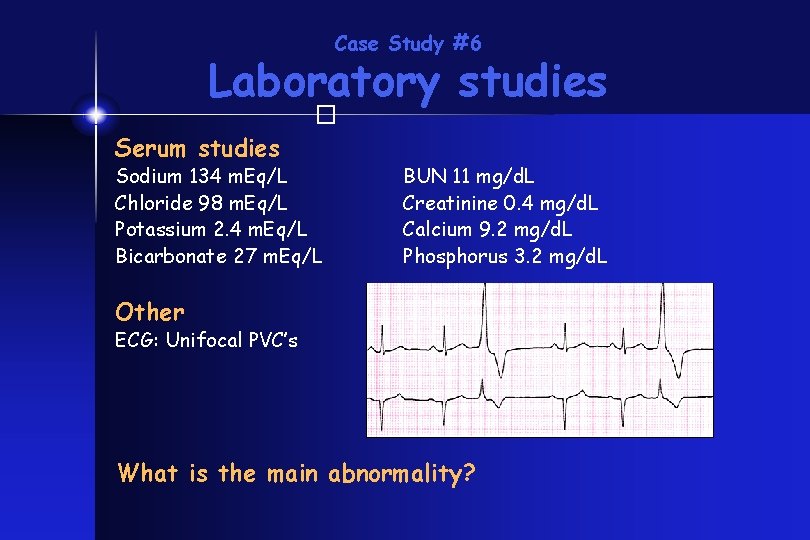
Case Study #6 Laboratory studies � Serum studies Sodium 134 m. Eq/L Chloride 98 m. Eq/L Potassium 2. 4 m. Eq/L Bicarbonate 27 m. Eq/L BUN 11 mg/d. L Creatinine 0. 4 mg/d. L Calcium 9. 2 mg/d. L Phosphorus 3. 2 mg/d. L Other ECG: Unifocal PVC’s What is the main abnormality?
Case Study #6 Laboratory studies � Major abnormality 1) Hypokalemia What would you do now?
Case Study #6 Hypokalemia � • Treatment • Oral • Safest, although solutions may cause diarrhea • IV • do not exceed 40 m. Eq/L or 10 – 20 m. Eq/hr potassium. - never give inj. Kcl directly intravenously. • Replace magnesium also if low • (25 -50 mg/kg Mg. SO 4)
Summary � • Disorders of sodium, water, and potassium regulation are common in critically ill children • Diagnostic approach must be considered carefully for each patient • Strict attention to detail is important in providing safe and effective therapy
