The Road to 2024 Navigating MACRA MIPS 2018


- Slides: 23
The Road to 2024 Navigating MACRA / MIPS 2018 Performance Year
Who we are. . JOY RIOS REBECCA DIFRANCESCO Joy Rios is an author, subject matter expert and health IT consultant focusing on the Merit-based Incentive Payment System. She has developed several training programs and online courses on health IT subject matter. Joy holds an MBA and is a Certified Healthcare Technology Specialist with a specialty in Workflow Redesign. Rebecca Di. Francesco is a health IT and project management expert with more than 17 years experience in the healthcare industry. In addition to a Bachelor’s degree, she has earned a certificate in Improvement Advisor from the Institute of Healthcare Improvement, and is a credentialed Project Management Professional (PMP). She is also a Certified HIPAA Security Professional for Compliance Officers (CHSP), Meaningful Use (CMUP), and PQRS Healthcare Professional (CPHP). @askjoyrios

The Journey to 2024 How will you get there?
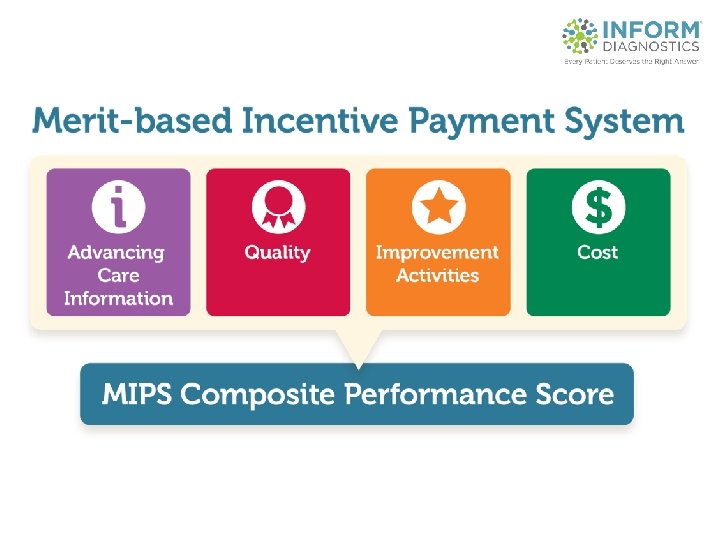
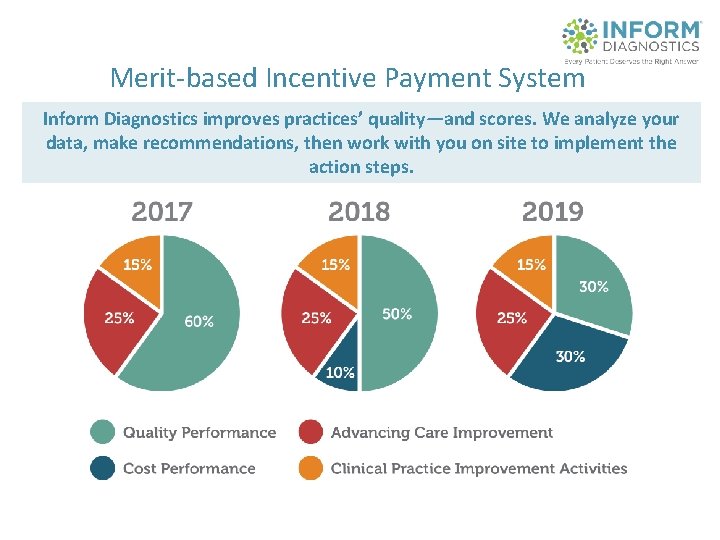
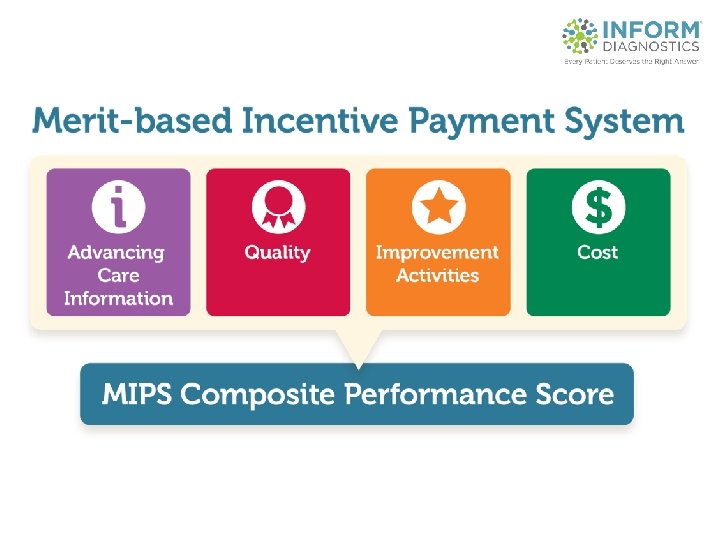
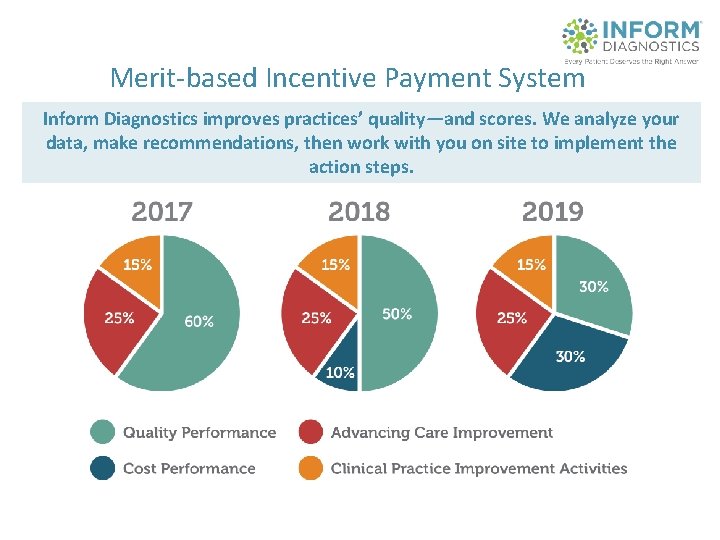
Merit-based Incentive Payment System Inform Diagnostics improves practices’ quality—and scores. We analyze your data, make recommendations, then work with you on site to implement the action steps.
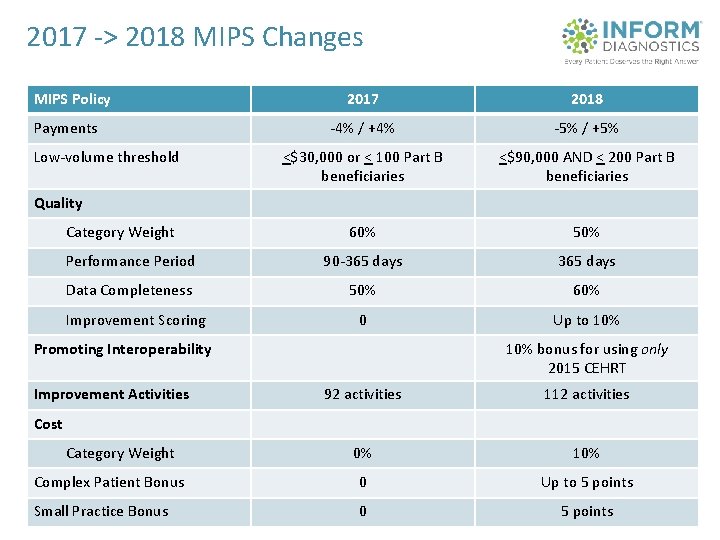
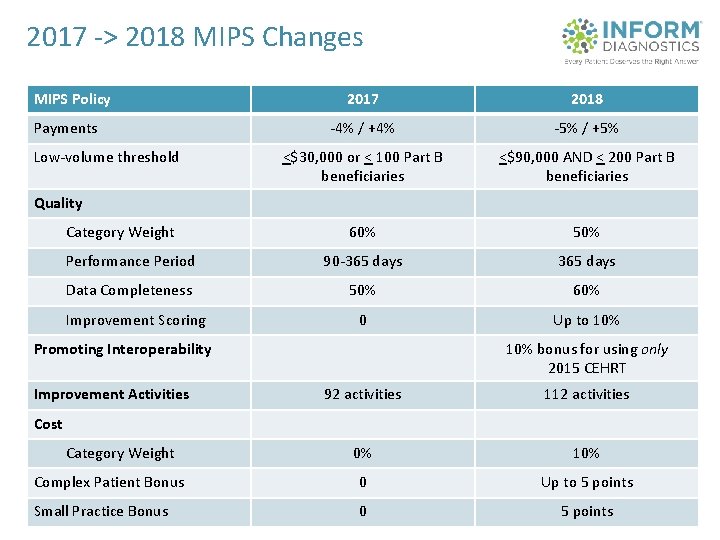
2017 -> 2018 MIPS Changes MIPS Policy 2017 2018 -4% / +4% -5% / +5% <$30, 000 or < 100 Part B beneficiaries <$90, 000 AND < 200 Part B beneficiaries 60% 50% Performance Period 90 -365 days Data Completeness 50% 60% 0 Up to 10% Payments Low-volume threshold Quality Category Weight Improvement Scoring Promoting Interoperability Improvement Activities 10% bonus for using only 2015 CEHRT 92 activities 112 activities 0% 10% Complex Patient Bonus 0 Up to 5 points Small Practice Bonus 0 5 points Cost Category Weight
Bipartisan Budget Act of 2018 • Extended “Transition Years” through 2021 – Cost to be weighted 10 -30% – No MIPS payment adjustment for Part B drugs – CMS to establish threshold • April 27, 2018 – Advancing Care Information (ACI) is renamed to Promoting Interoperability (PI)
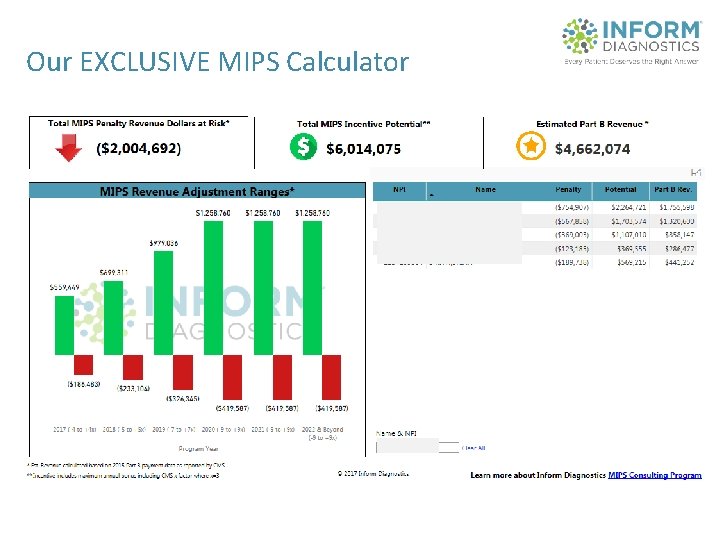
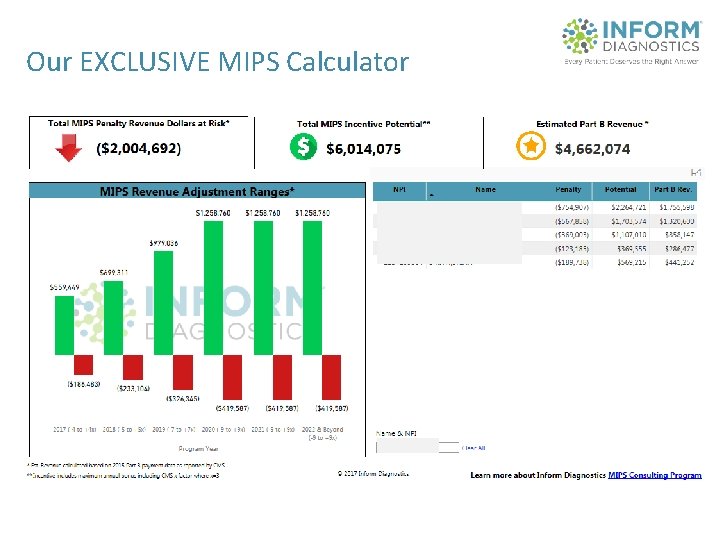
Our EXCLUSIVE MIPS Calculator
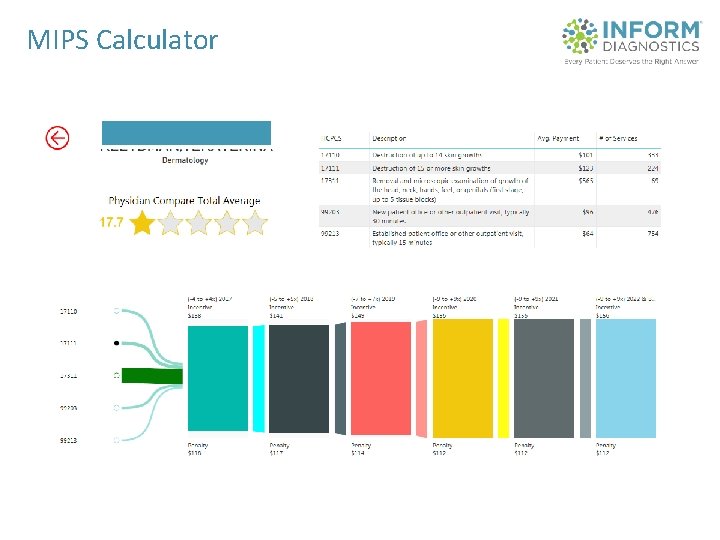
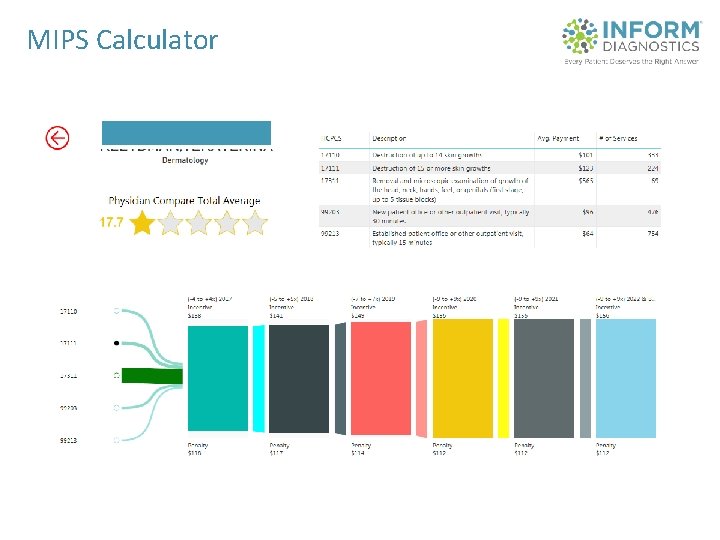
MIPS Calculator
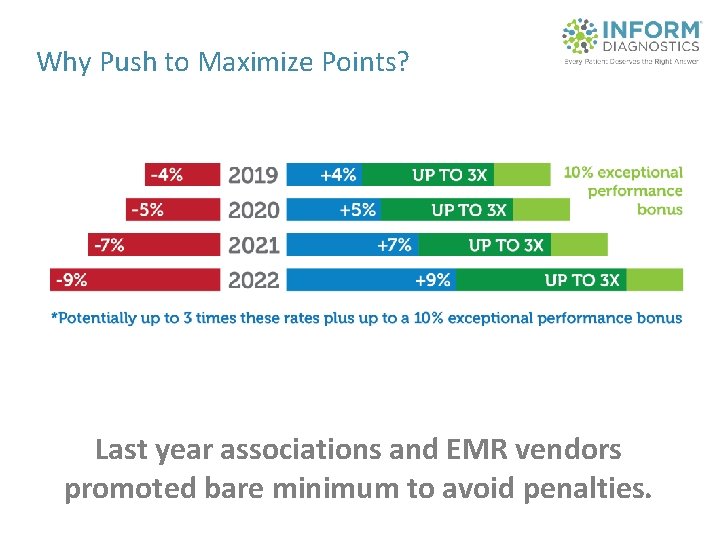
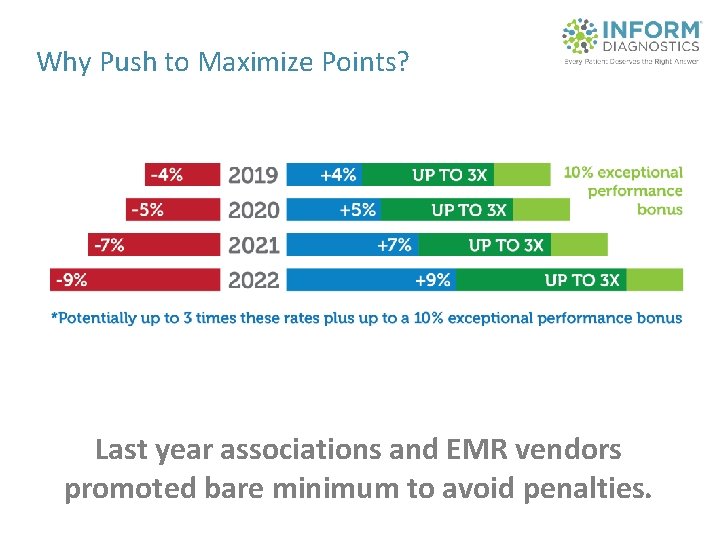
Why Push to Maximize Points? Last year associations and EMR vendors promoted bare minimum to avoid penalties.
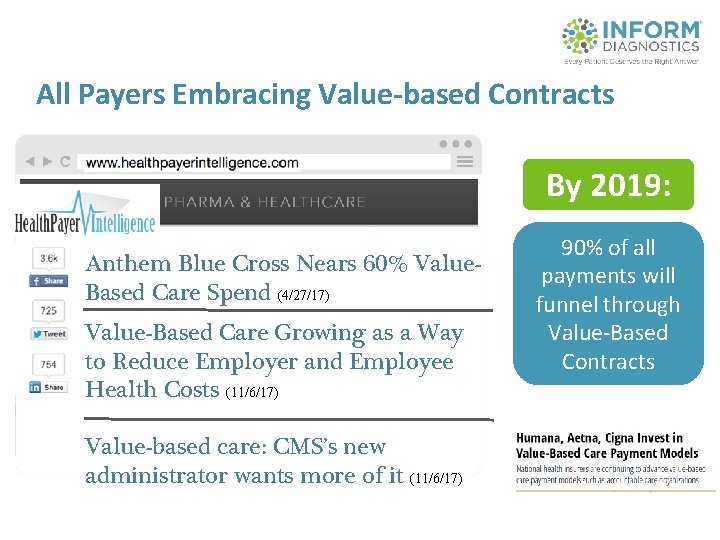
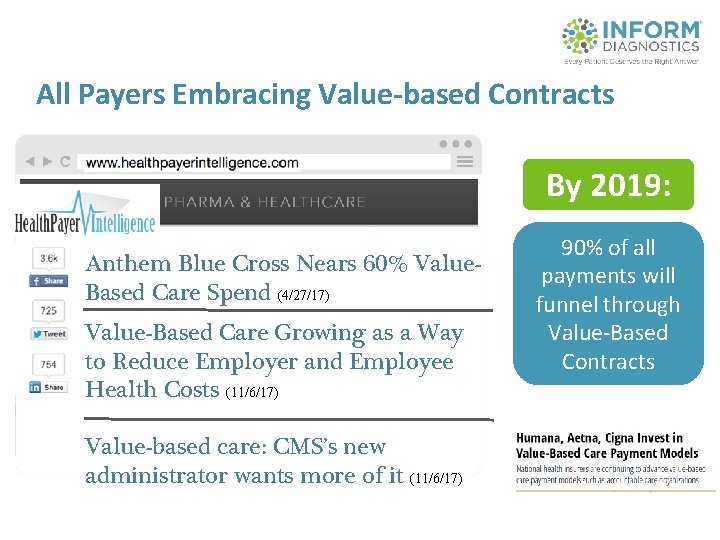
All Payers Embracing Value-based Contracts By 2019: Anthem Blue Cross Nears 60% Value. Based Care Spend (4/27/17) Value-Based Care Growing as a Way to Reduce Employer and Employee Health Costs (11/6/17) Value-based care: CMS’s new administrator wants more of it (11/6/17) 90% of all payments will funnel through Value-Based Contracts
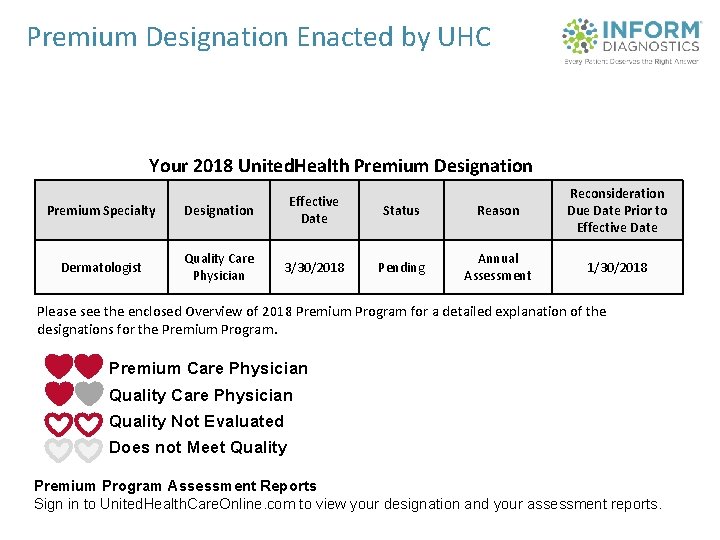
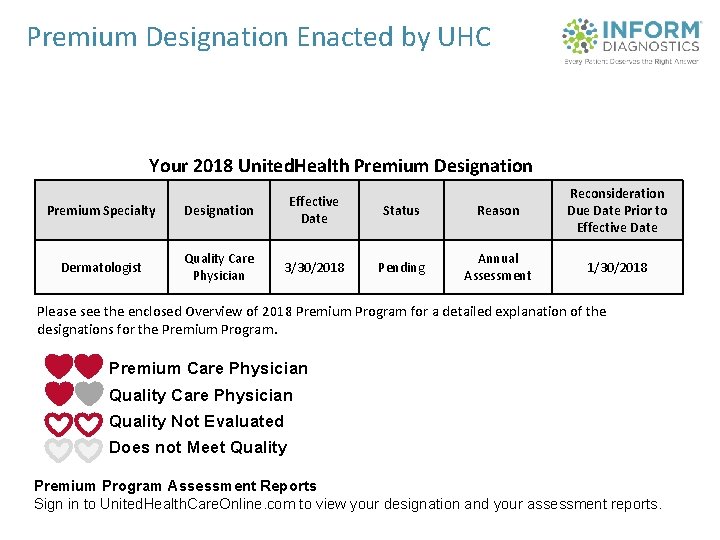
Premium Designation Enacted by UHC Your 2018 United. Health Premium Designation Premium Specialty Designation Effective Date Dermatologist Quality Care Physician 3/30/2018 Status Reason Reconsideration Due Date Prior to Effective Date Pending Annual Assessment 1/30/2018 Please see the enclosed Overview of 2018 Premium Program for a detailed explanation of the designations for the Premium Program. Premium Care Physician Quality Not Evaluated Does not Meet Quality Premium Program Assessment Reports Sign in to United. Health. Care. Online. com to view your designation and your assessment reports.
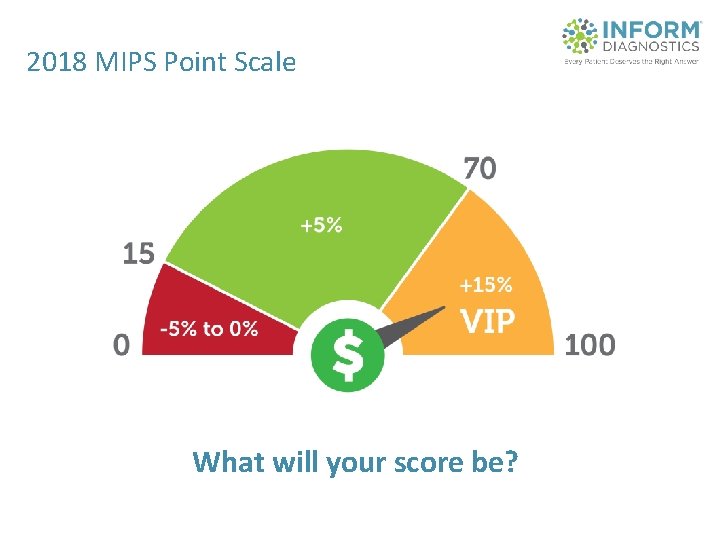
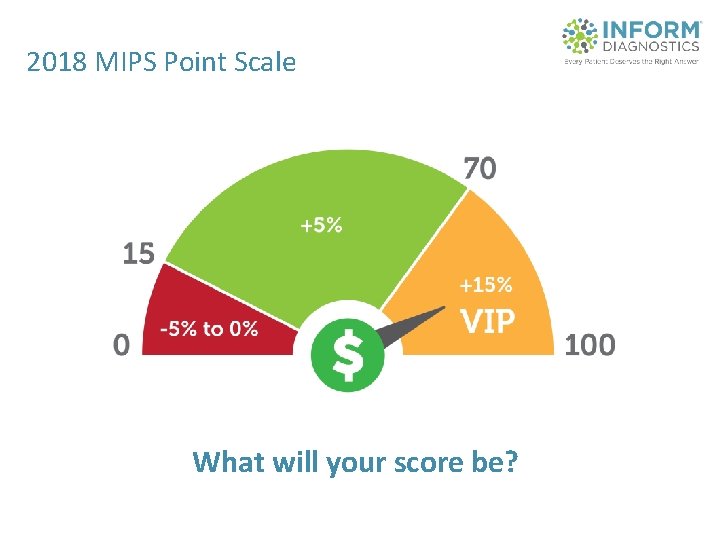
2018 MIPS Point Scale What will your score be?
Quality • Know your benchmarks • HOW you report can impact your point maximums • Data complete ness is critical 60% requirement • Full calendar year of data
Promoting Interoperability (PI) • Base Measures • Choose Where to Exert Effort • Reporting Period – 90 days
Improvement Activities • 112 choices • Choosing the right activities can add bonus points in other categories • An easy win if: – – Follow annual updates Do them and document them based on CMS recommendations Know how many your group needs Understand common pitfalls
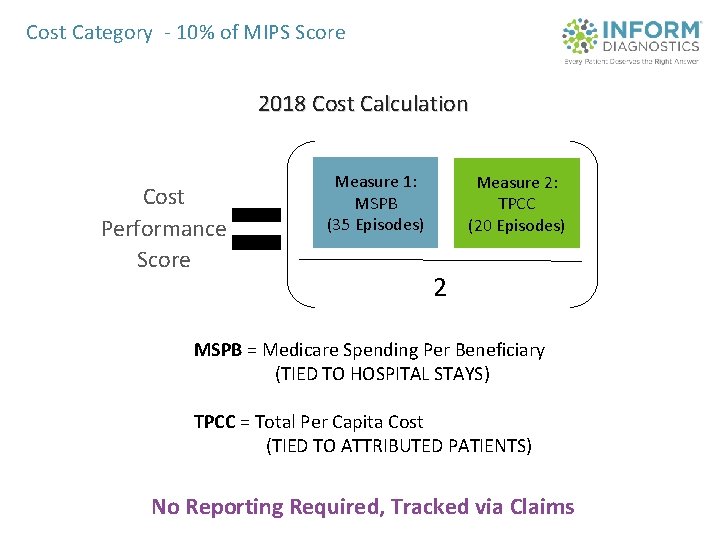
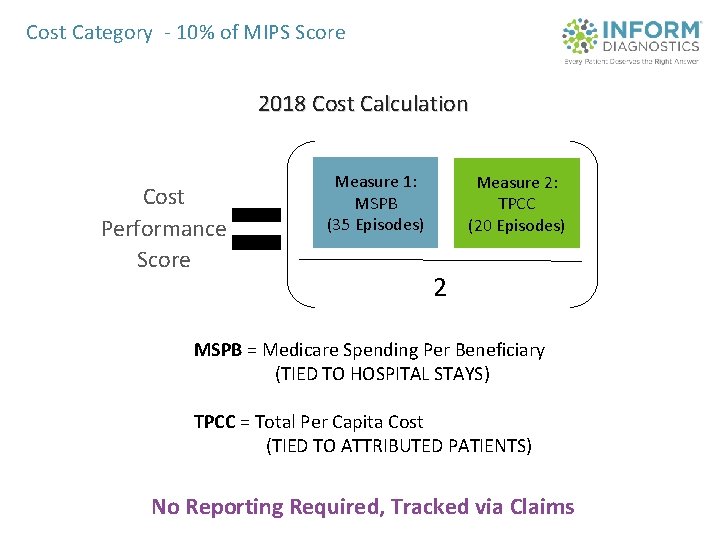
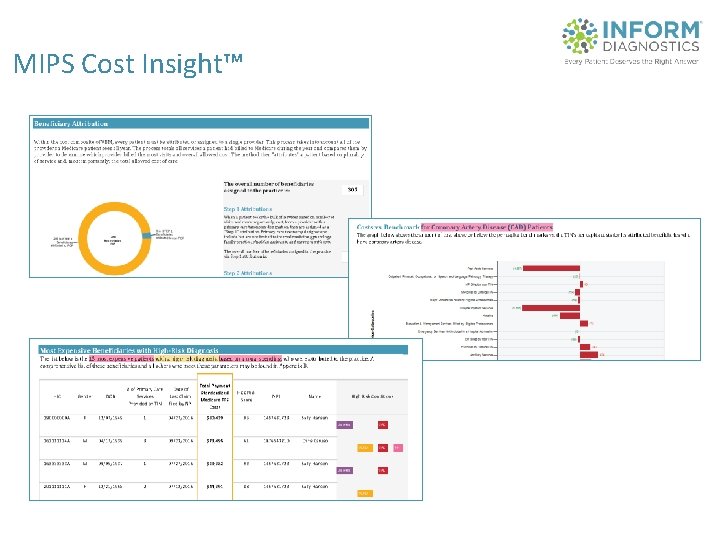
Cost Category - 10% of MIPS Score 2018 Cost Calculation Cost Performance Score Measure 1: MSPB (35 Episodes) Measure 2: TPCC (20 Episodes) 2 MSPB = Medicare Spending Per Beneficiary (TIED TO HOSPITAL STAYS) TPCC = Total Per Capita Cost (TIED TO ATTRIBUTED PATIENTS) No Reporting Required, Tracked via Claims
MIPS Cost Insight™
Ensure Comprehensive Work – – – – – MIPS Cost Insight- Quality Resource & Use Report analysis Clinical Practice Improvement Activities (CPIA) Advancing Care information (ACI) Quality guidance and submission assistance* Audit support Security Risk Assessment (SRA)* HIPAA Certification Course* Workflow guidance and support Book of Evidence Attestation assistance
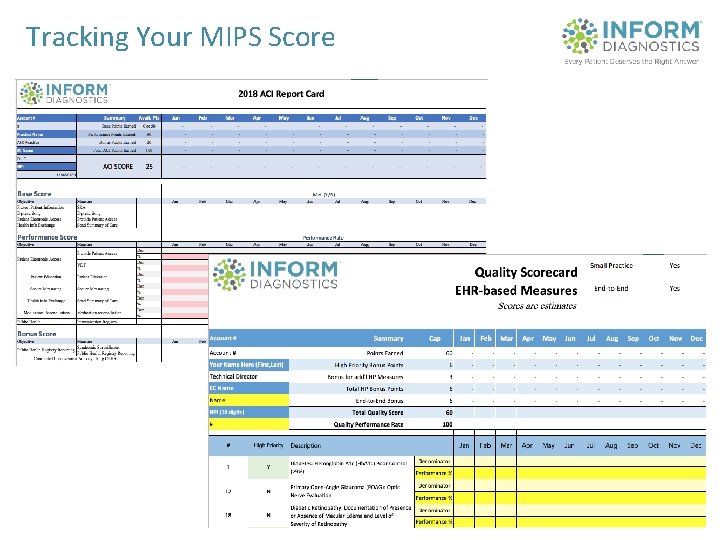
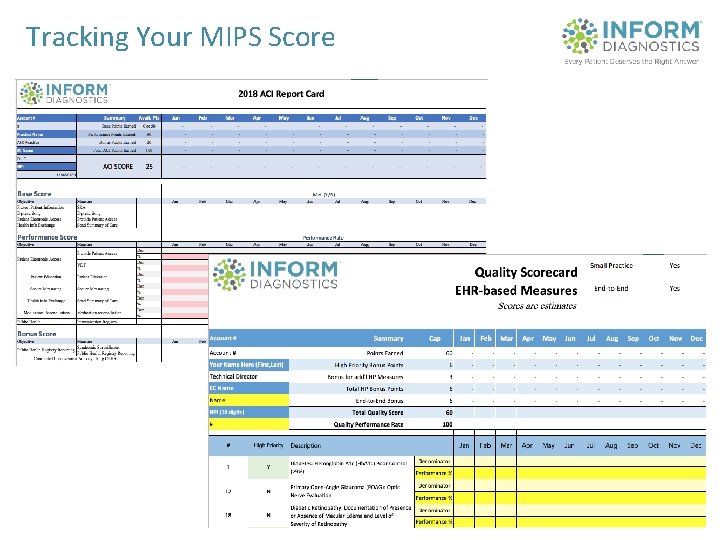
Tracking Your MIPS Score
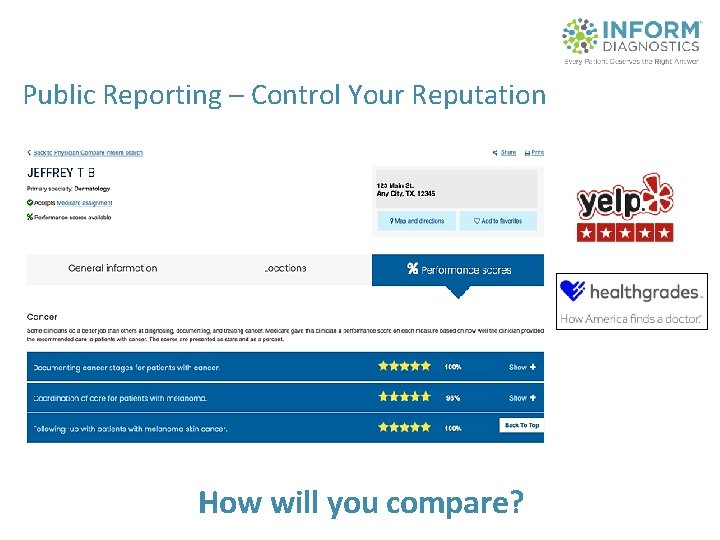
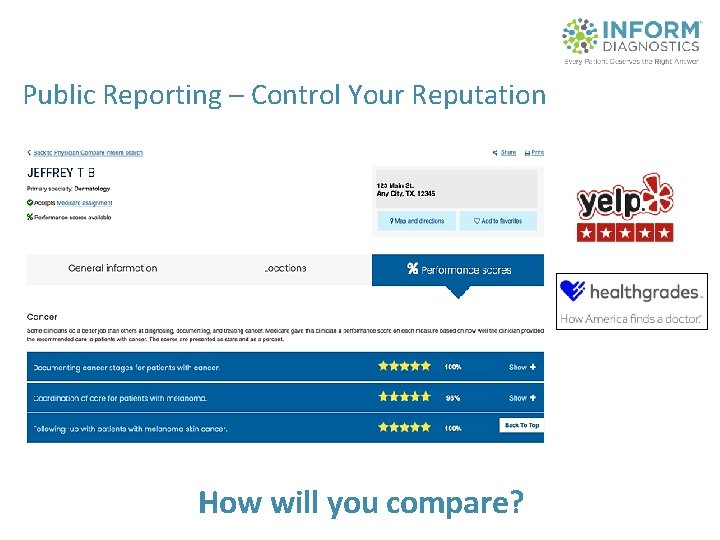
Public Reporting – Control Your Reputation How will you compare?
NJSOM - Recognition • MIPS guidance is covered in society membership! • 2017 member performance results

The Journey to 2024 How will you get there?