MACRA Proposed Rule What You Need to Know
- Slides: 33
MACRA Proposed Rule: What You Need to Know
Why Does This Matter? • Physicians: Impact on payment, performance measurement requirements • Hospitals: May bear cost of implementation and compliance with new payment and performance measurement system by employed physicians • Continued shift in hospital-physician relationships • Incentives to participate in alternative payment arrangements increasing interest in risk-bearing arrangements
MACRA Proposed Rule • Released on Apr. 27 • Proposes policies implementing new Physician Quality Payment Program mandated by MACRA • Affects payment in CY 2019 – Performance period of CY 2017 • Final rule expected by Nov. 1, 2016
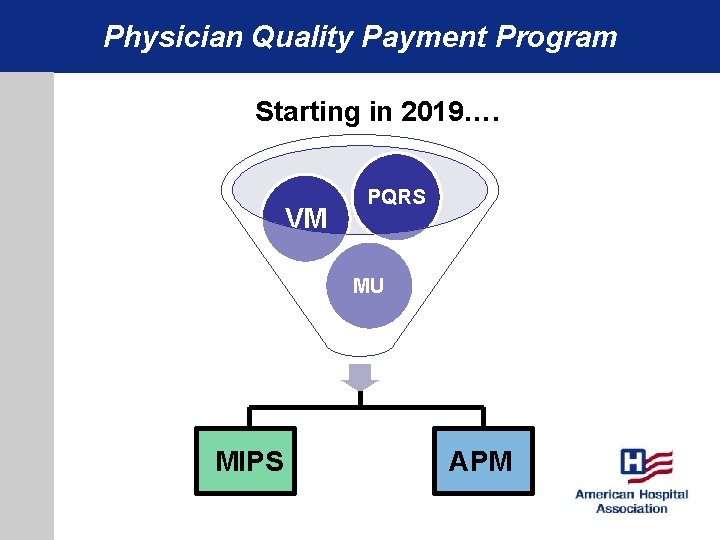
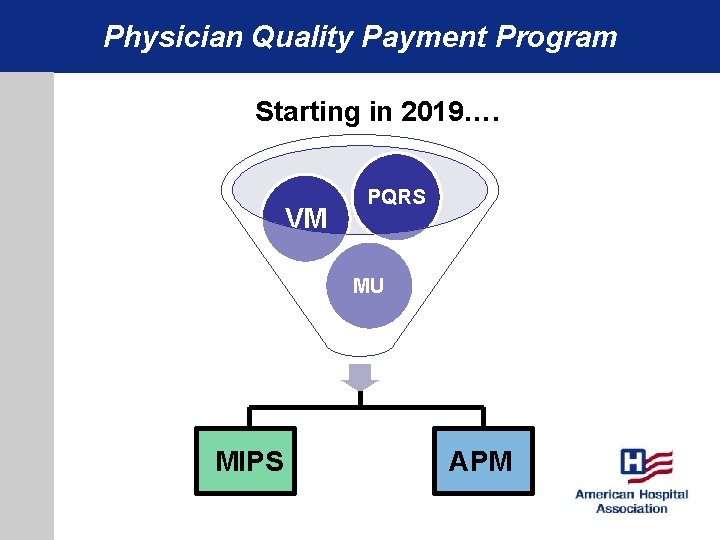
Physician Quality Payment Program Starting in 2019…. VM PQRS MU MIPS APM
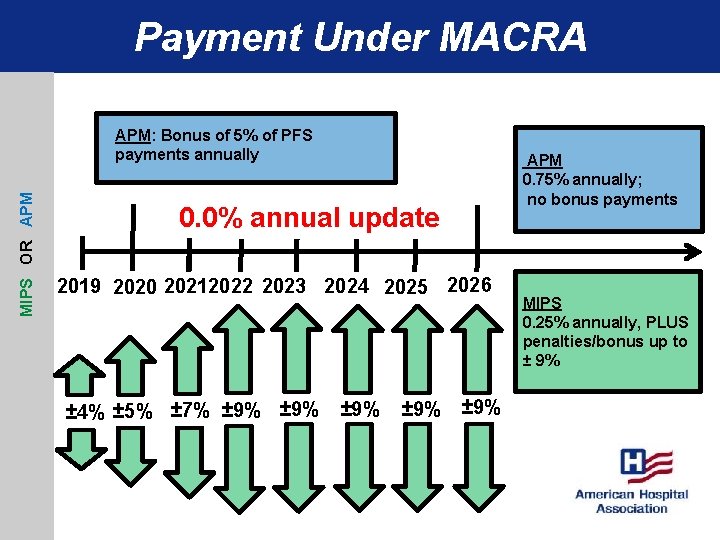
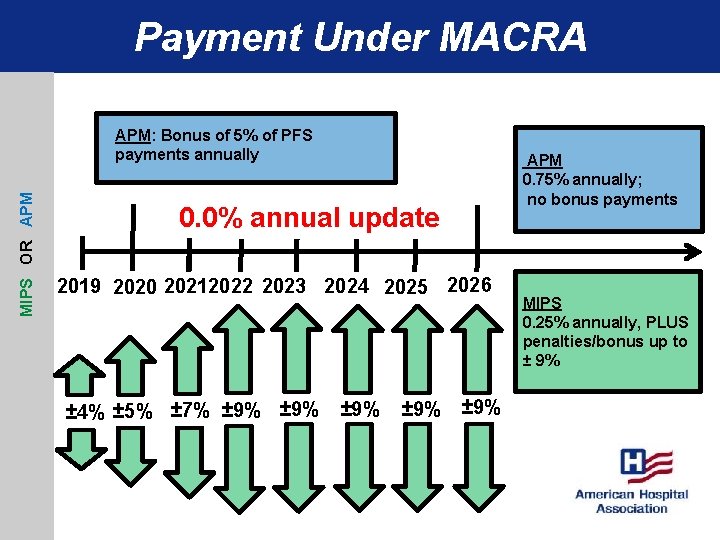
Payment Under MACRA MIPS OR APM: Bonus of 5% of PFS payments annually APM 0. 75% annually; no bonus payments 0. 0% annual update 2019 2020 20212022 2023 2024 2025 2026 ± 4% ± 5% ± 7% ± 9% ± 9% MIPS 0. 25% annually, PLUS penalties/bonus up to ± 9%
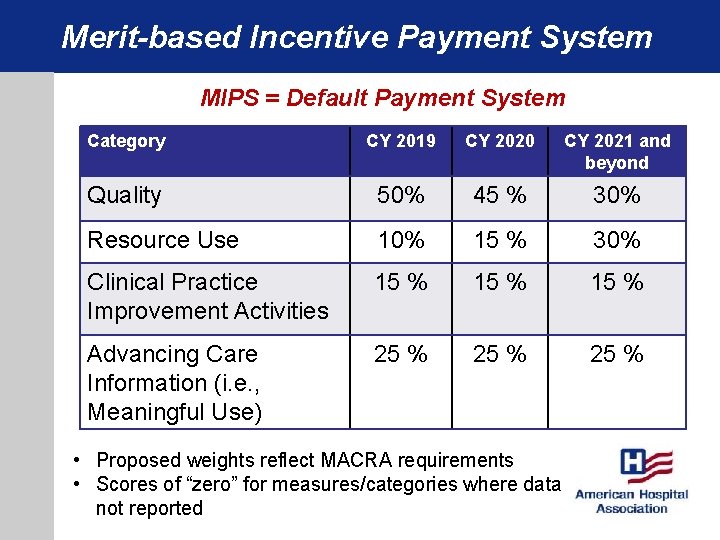
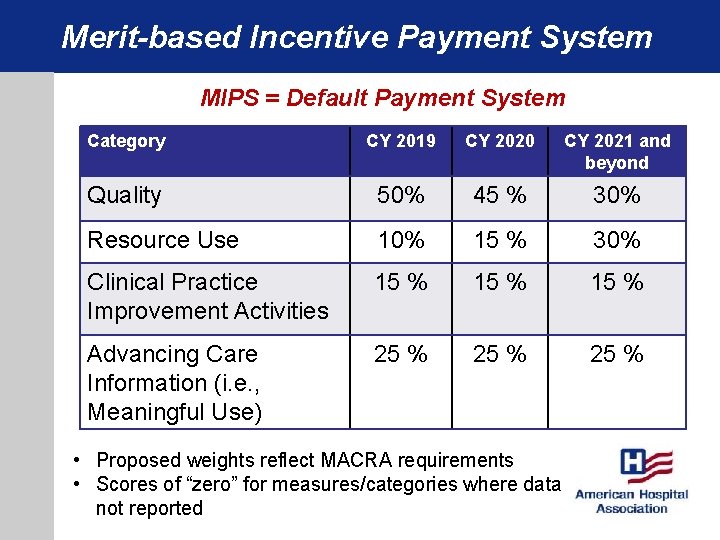
Merit-based Incentive Payment System MIPS = Default Payment System Category CY 2019 CY 2020 CY 2021 and beyond Quality 50% 45 % 30% Resource Use 10% 15 % 30% Clinical Practice Improvement Activities 15 % Advancing Care Information (i. e. , Meaningful Use) 25 % • Proposed weights reflect MACRA requirements • Scores of “zero” for measures/categories where data not reported
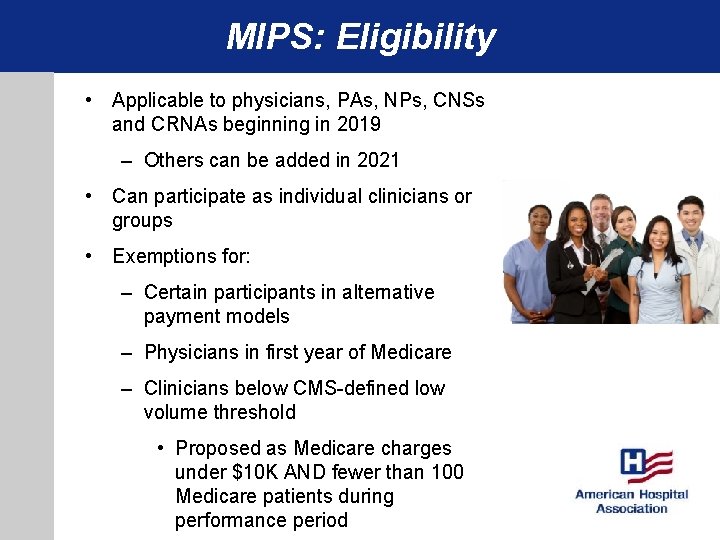
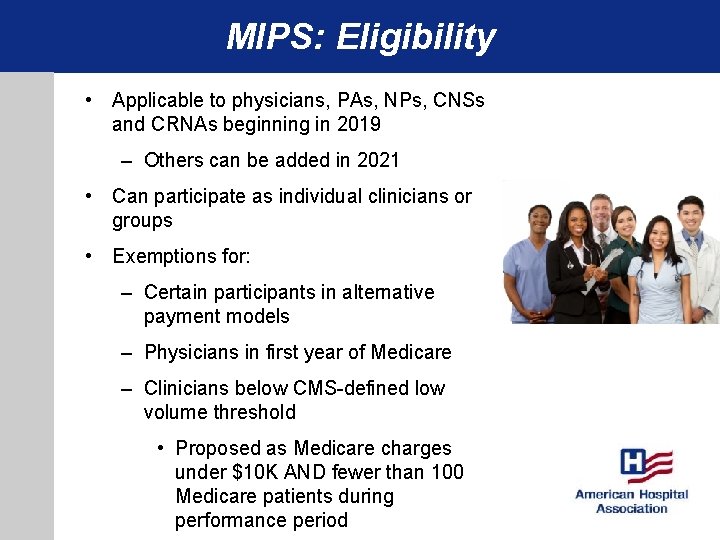
MIPS: Eligibility • Applicable to physicians, PAs, NPs, CNSs and CRNAs beginning in 2019 – Others can be added in 2021 • Can participate as individual clinicians or groups • Exemptions for: – Certain participants in alternative payment models – Physicians in first year of Medicare – Clinicians below CMS-defined low volume threshold • Proposed as Medicare charges under $10 K AND fewer than 100 Medicare patients during performance period
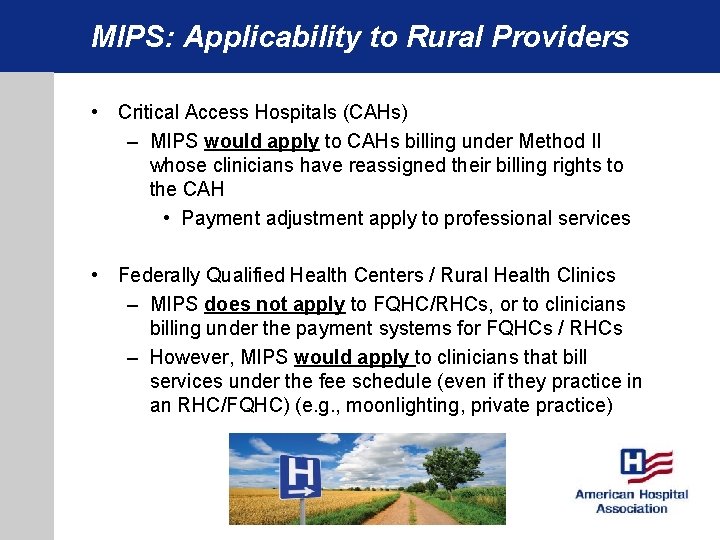
MIPS: Applicability to Rural Providers • Critical Access Hospitals (CAHs) – MIPS would apply to CAHs billing under Method II whose clinicians have reassigned their billing rights to the CAH • Payment adjustment apply to professional services • Federally Qualified Health Centers / Rural Health Clinics – MIPS does not apply to FQHC/RHCs, or to clinicians billing under the payment systems for FQHCs / RHCs – However, MIPS would apply to clinicians that bill services under the fee schedule (even if they practice in an RHC/FQHC) (e. g. , moonlighting, private practice)
MIPS: Data Reporting Mechanisms • • Must select one mechanism per category For CY 2019, report CY 2017 data Data generally due to CMS by Mar. 31, 2018 Data completeness thresholds
MIPS: Quality Measure Requirements • For most reporting mechanisms, clinicians and groups would report at least 6 measures. Of the 6: – Must report 1 cross-cutting measure – 1 outcome measure (or another high priority measure if outcome is unavailable) • Can choose any 6 from list of available measures – Specialty measure sets also available • For groups of 10 or more clinicians, CMS also would calculate claims-based “population measures” – Reflect avoidable admissions and readmissions
MIPS – Resource Use Measures • CMS would continue using 2 all-condition resource use measures used in value-modifier program – Total costs per capita – Medicare spending per beneficiary for physicians • CMS also proposes to use clinical condition and procedure episode cost measures from a list of 40+ measures • Cost score = average score of all the measures that can be attributed to clinician / group – Various attribution methodologies
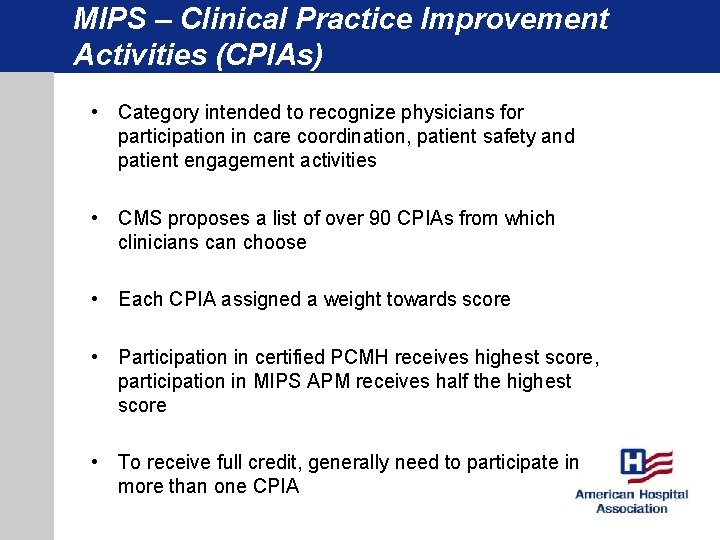
MIPS – Clinical Practice Improvement Activities (CPIAs) • Category intended to recognize physicians for participation in care coordination, patient safety and patient engagement activities • CMS proposes a list of over 90 CPIAs from which clinicians can choose • Each CPIA assigned a weight towards score • Participation in certified PCMH receives highest score, participation in MIPS APM receives half the highest score • To receive full credit, generally need to participate in more than one CPIA
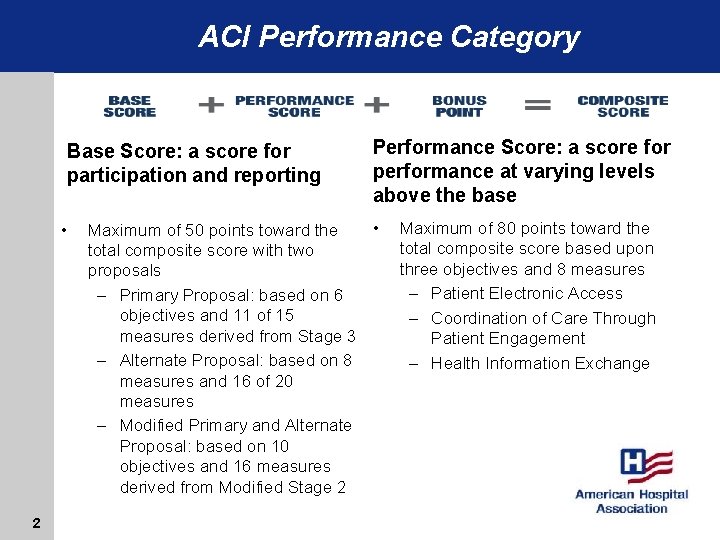
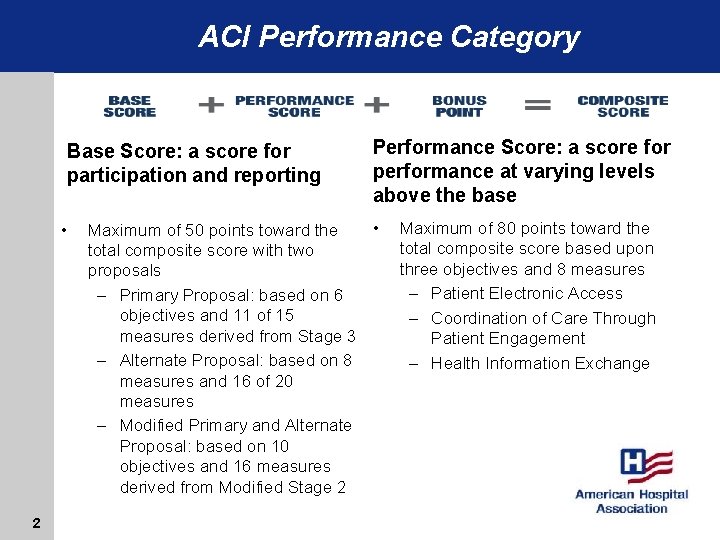
ACI Performance Category Base Score: a score for participation and reporting • 2 Performance Score: a score for performance at varying levels above the base • Maximum of 50 points toward the total composite score with two proposals – Primary Proposal: based on 6 objectives and 11 of 15 measures derived from Stage 3 – Alternate Proposal: based on 8 measures and 16 of 20 measures – Modified Primary and Alternate Proposal: based on 10 objectives and 16 measures derived from Modified Stage 2 Maximum of 80 points toward the total composite score based upon three objectives and 8 measures – Patient Electronic Access – Coordination of Care Through Patient Engagement – Health Information Exchange
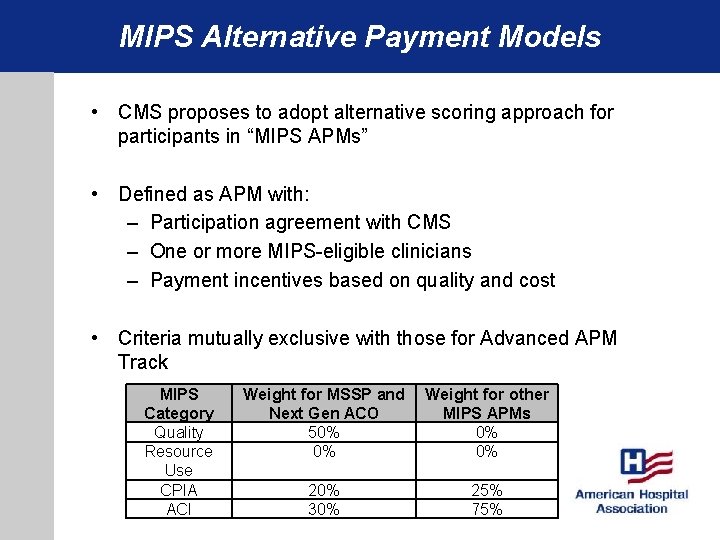
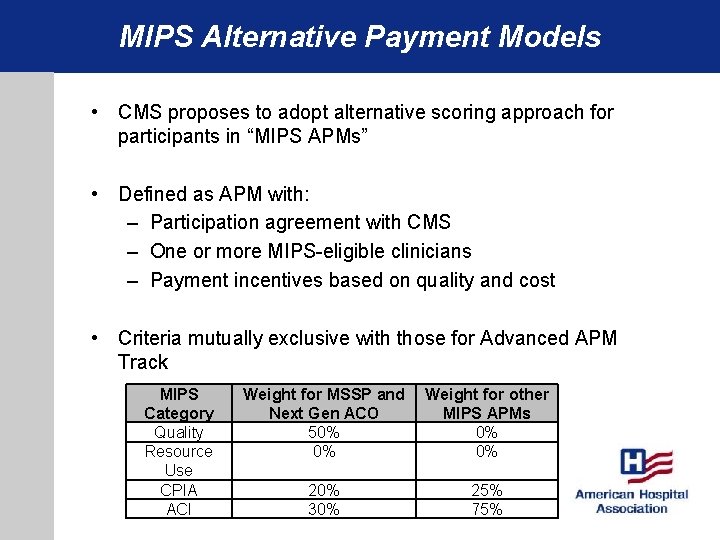
MIPS Alternative Payment Models • CMS proposes to adopt alternative scoring approach for participants in “MIPS APMs” • Defined as APM with: – Participation agreement with CMS – One or more MIPS-eligible clinicians – Payment incentives based on quality and cost • Criteria mutually exclusive with those for Advanced APM Track MIPS Category Quality Resource Use CPIA ACI Weight for MSSP and Weight for other Next Gen ACO MIPS APMs 50% 0% 20% 30% 25% 75%
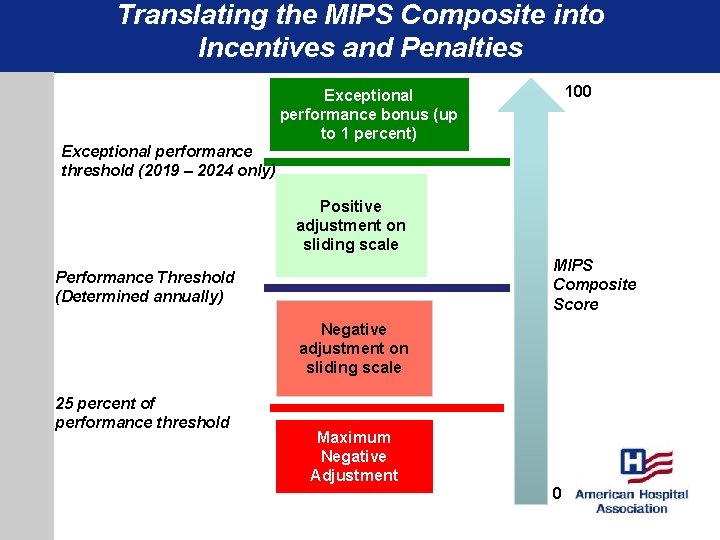
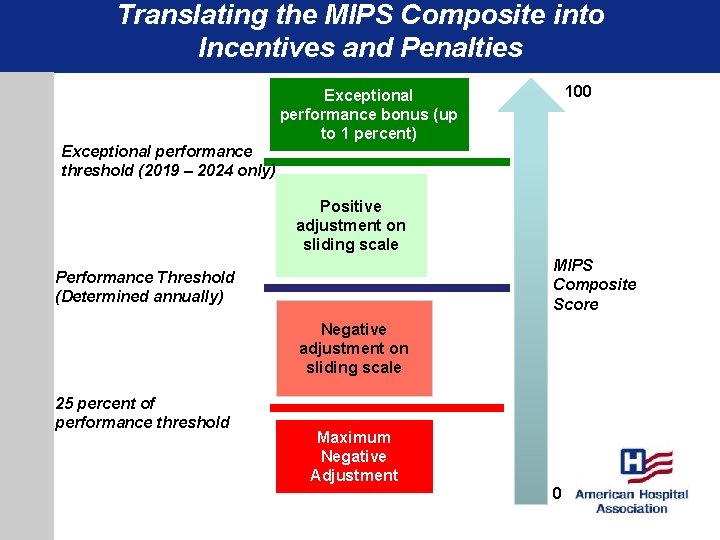
Translating the MIPS Composite into Incentives and Penalties 100 Exceptional performance bonus (up to 1 percent) Exceptional performance threshold (2019 – 2024 only) Positive adjustment on sliding scale MIPS Composite Score Performance Threshold (Determined annually) Negative adjustment on sliding scale 25 percent of performance threshold Maximum Negative Adjustment 0
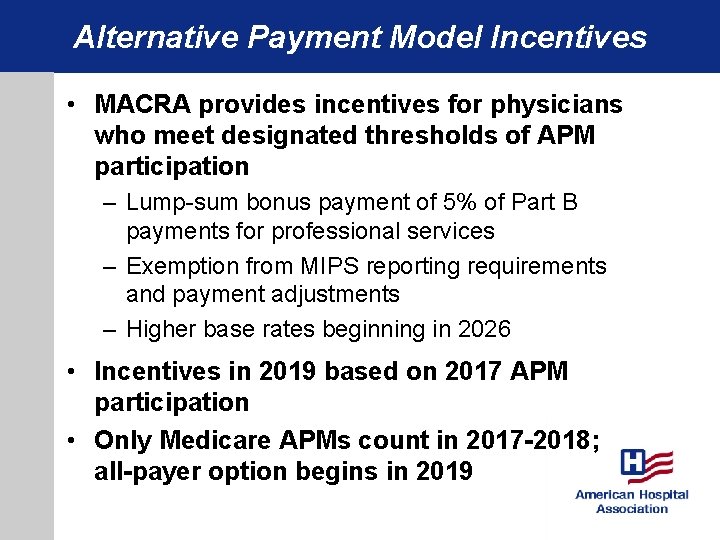
Alternative Payment Model Incentives • MACRA provides incentives for physicians who meet designated thresholds of APM participation – Lump-sum bonus payment of 5% of Part B payments for professional services – Exemption from MIPS reporting requirements and payment adjustments – Higher base rates beginning in 2026 • Incentives in 2019 based on 2017 APM participation • Only Medicare APMs count in 2017 -2018; all-payer option begins in 2019
Qualified Professional Determination • Qualified professional = meets the criteria to qualify for APM incentives based on participation in advanced APMs • CMS proposes following general process: – Determine whether the APM meets the advanced APM criteria – Identify the APM entity – Determine whether eligible clinicians in APM entity collectively meet threshold for APM participation
Qualified Professional Determination • Qualified professional = meets the criteria to qualify for APM incentives based on participation in advanced APMs • CMS proposes following general process: – Determine whether the APM meets the advanced APM criteria – Identify the APM entity – Determine whether eligible clinicians in APM entity collectively meet threshold for APM participation
Medicare APMs are defined as: • A model tested by the CMMI, other than a health care innovation award • An ACO under the Medicare Shared Savings Program • Certain other demonstrations under federal law
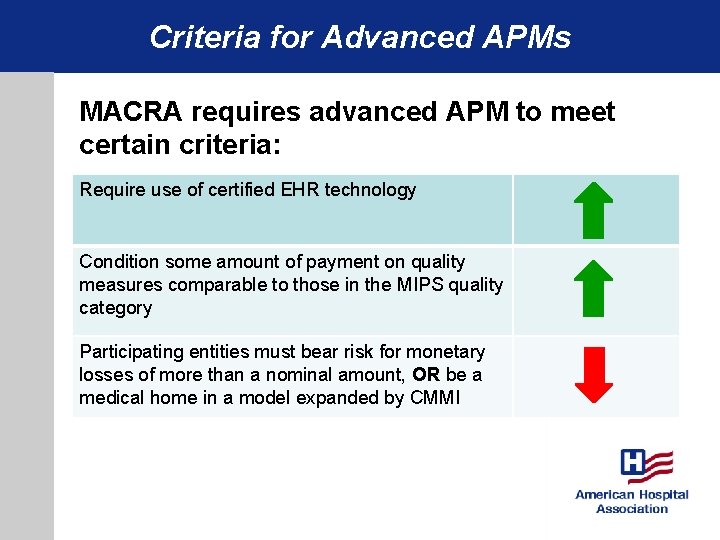
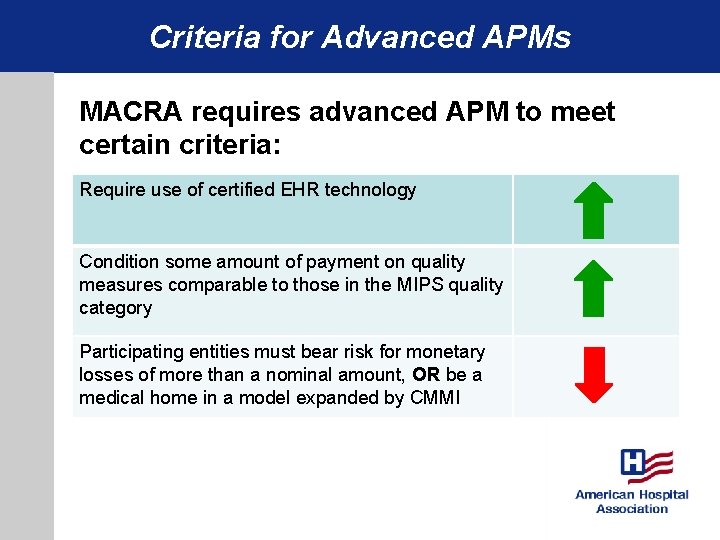
Criteria for Advanced APMs MACRA requires advanced APM to meet certain criteria: Require use of certified EHR technology Condition some amount of payment on quality measures comparable to those in the MIPS quality category Participating entities must bear risk for monetary losses of more than a nominal amount, OR be a medical home in a model expanded by CMMI
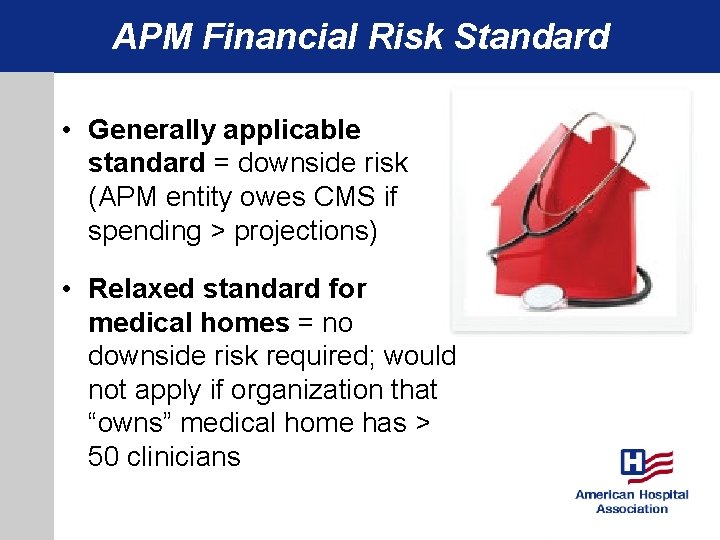
APM Financial Risk Standard • Generally applicable standard = downside risk (APM entity owes CMS if spending > projections) • Relaxed standard for medical homes = no downside risk required; would not apply if organization that “owns” medical home has > 50 clinicians
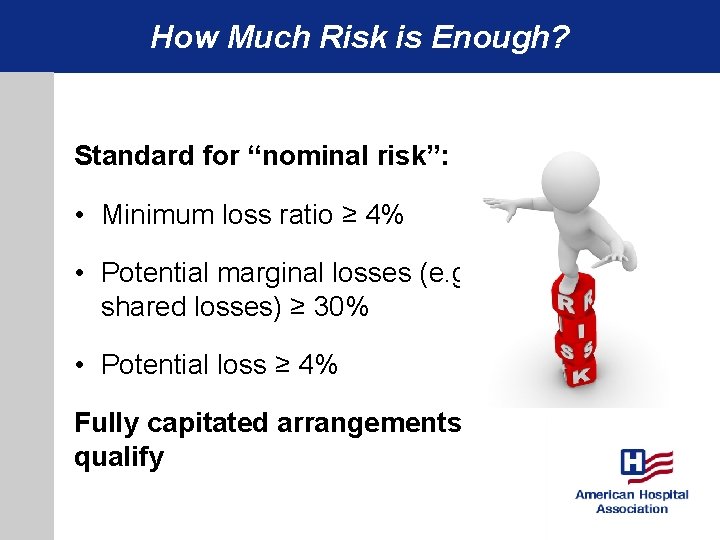
How Much Risk is Enough? Standard for “nominal risk”: • Minimum loss ratio ≥ 4% • Potential marginal losses (e. g. shared losses) ≥ 30% • Potential loss ≥ 4% Fully capitated arrangements qualify
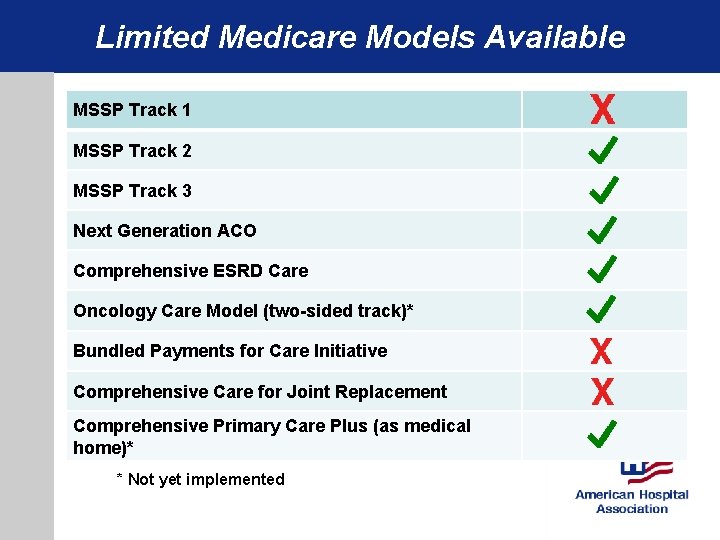
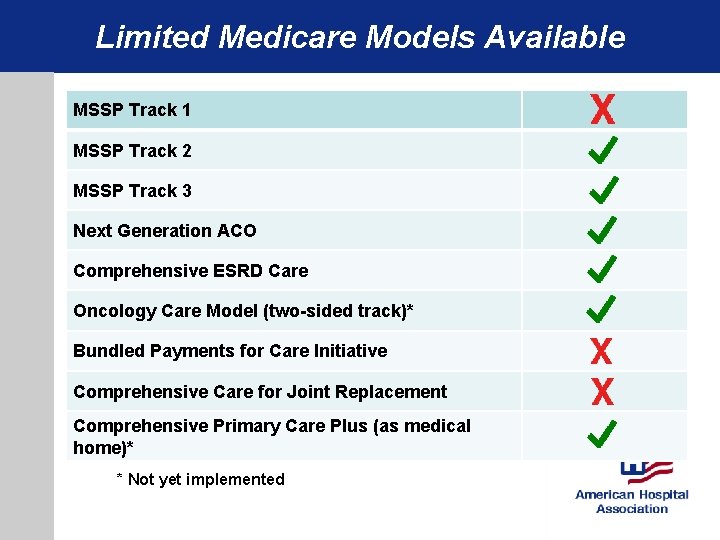
Limited Medicare Models Available MSSP Track 1 MSSP Track 2 MSSP Track 3 Next Generation ACO Comprehensive ESRD Care Oncology Care Model (two-sided track)* Bundled Payments for Care Initiative Comprehensive Care for Joint Replacement Comprehensive Primary Care Plus (as medical home)* * Not yet implemented
Qualified Professional Determination • Qualified professional = meets the criteria to qualify for APM incentives based on participation in advanced APMs • CMS proposes following general process: – Determine whether the APM meets the advanced APM criteria – Identify the APM entity – Determine whether eligible clinicians in APM entity collectively meet threshold for APM participation
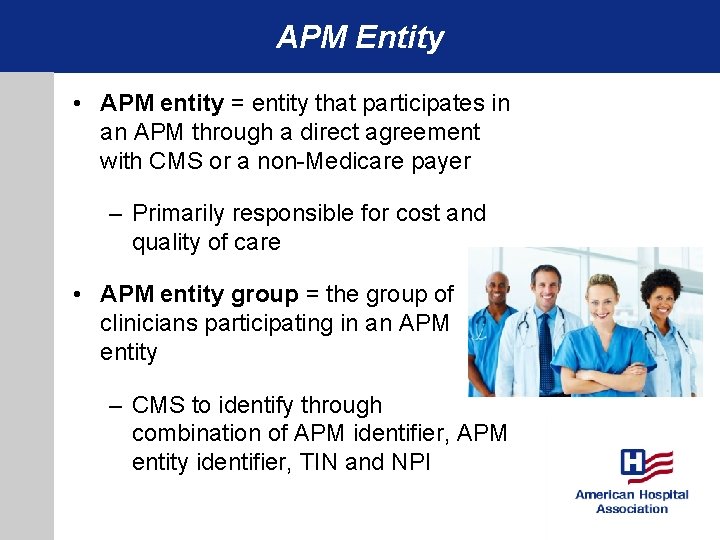
APM Entity • APM entity = entity that participates in an APM through a direct agreement with CMS or a non-Medicare payer – Primarily responsible for cost and quality of care • APM entity group = the group of clinicians participating in an APM entity – CMS to identify through combination of APM identifier, APM entity identifier, TIN and NPI
Qualified Professional Determination • Qualified professional = meets the criteria to qualify for APM incentives based on participation in advanced APMs • CMS proposes following general process: – Determine whether the APM meets the advanced APM criteria – Identify the APM entity – Determine whether eligible clinicians in APM entity collectively meet threshold for APM participation
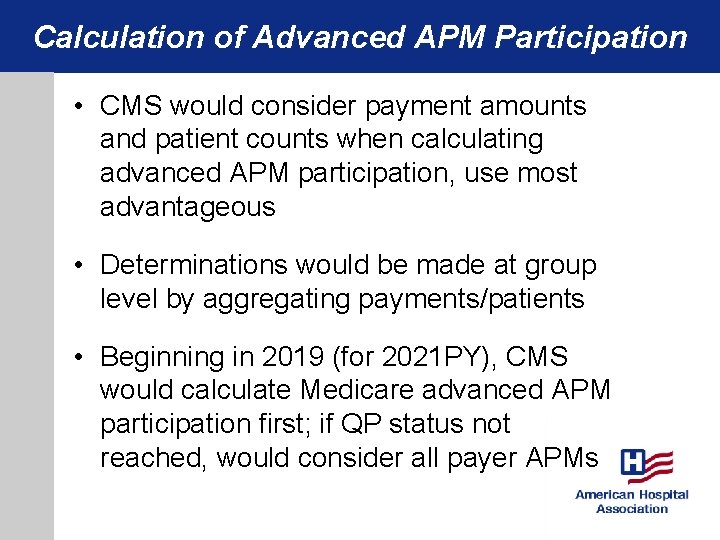
Calculation of Advanced APM Participation • CMS would consider payment amounts and patient counts when calculating advanced APM participation, use most advantageous • Determinations would be made at group level by aggregating payments/patients • Beginning in 2019 (for 2021 PY), CMS would calculate Medicare advanced APM participation first; if QP status not reached, would consider all payer APMs
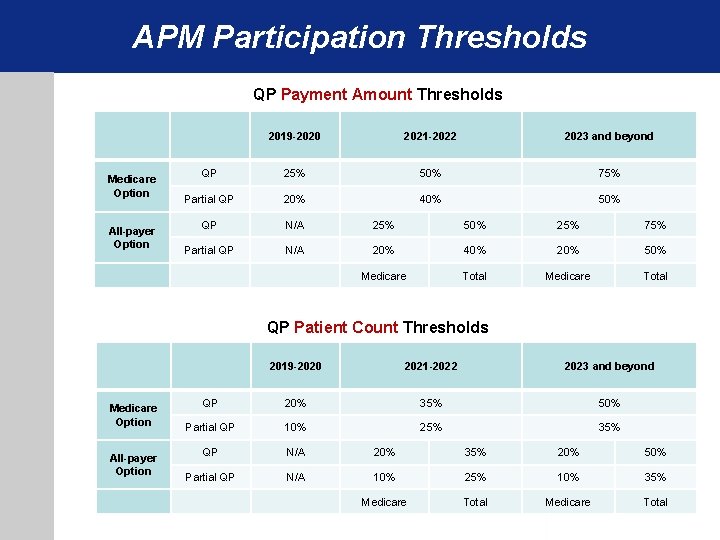
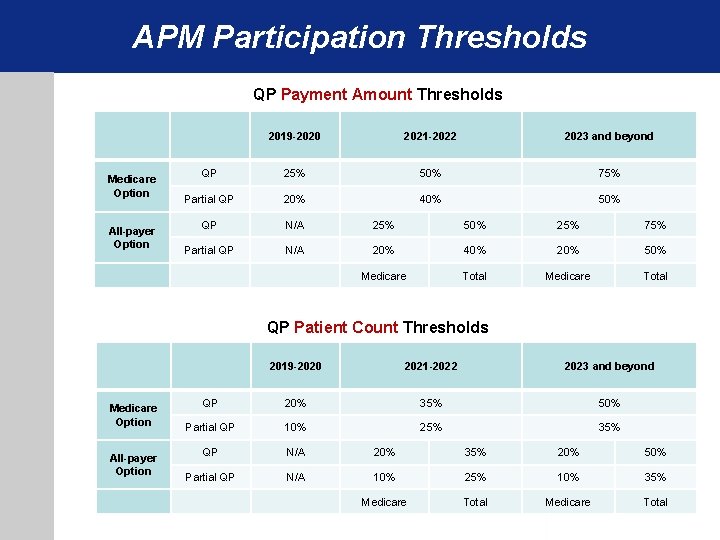
APM Participation Thresholds QP Payment Amount Thresholds Medicare Option All-payer Option 2019 -2020 2021 -2022 2023 and beyond QP 25% 50% 75% Partial QP 20% 40% 50% QP N/A 25% 50% 25% 75% Partial QP N/A 20% 40% 20% 50% Medicare Total QP Patient Count Thresholds Medicare Option All-payer Option 2019 -2020 2021 -2022 2023 and beyond QP 20% 35% 50% Partial QP 10% 25% 35% QP N/A 20% 35% 20% 50% Partial QP N/A 10% 25% 10% 35% Medicare Total
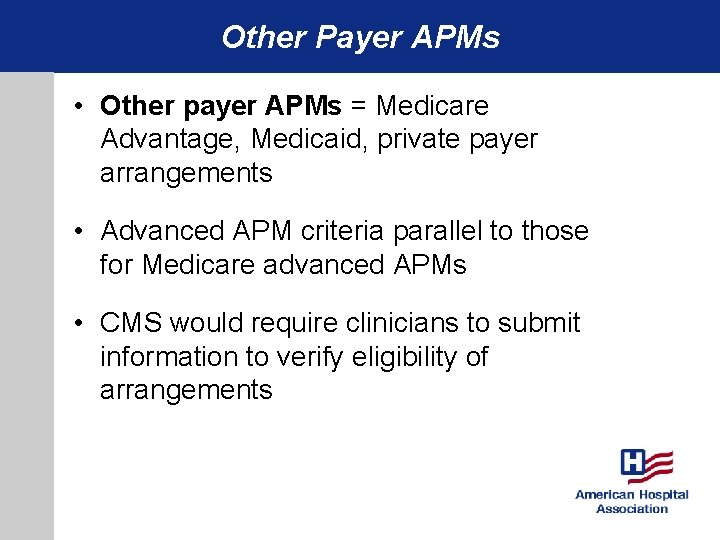
Other Payer APMs • Other payer APMs = Medicare Advantage, Medicaid, private payer arrangements • Advanced APM criteria parallel to those for Medicare advanced APMs • CMS would require clinicians to submit information to verify eligibility of arrangements
APM Incentive Payment • Lump-sum payment = 5% of Part B professional service payments across all TINs • Based on calendar year prior to payment year • Would exclude adjustments for MIPS, VM, MU and PQRS, plus financial risk payments • Payment would be made to APM entity TIN
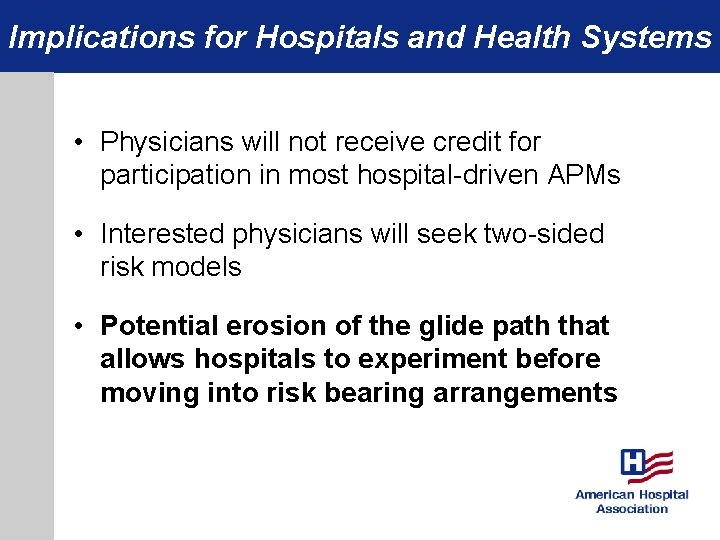
Implications for Hospitals and Health Systems • Physicians will not receive credit for participation in most hospital-driven APMs • Interested physicians will seek two-sided risk models • Potential erosion of the glide path that allows hospitals to experiment before moving into risk bearing arrangements
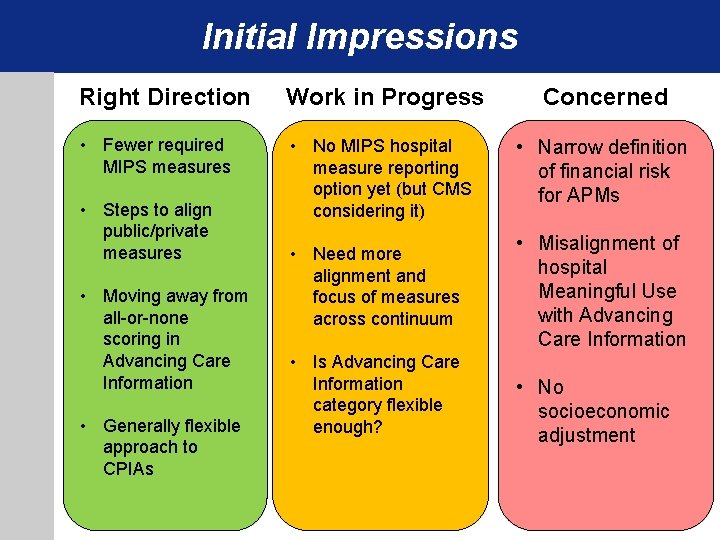
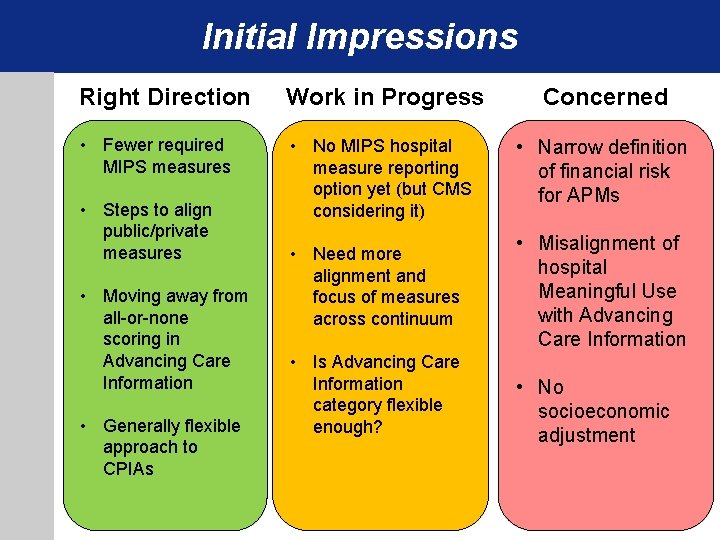
Initial Impressions Right Direction Work in Progress Concerned • Fewer required MIPS measures • No MIPS hospital measure reporting option yet (but CMS considering it) • Narrow definition of financial risk for APMs • Need more alignment and focus of measures across continuum • Misalignment of hospital Meaningful Use with Advancing Care Information • Steps to align public/private measures • Moving away from all-or-none scoring in Advancing Care Information • Generally flexible approach to CPIAs • Is Advancing Care Information category flexible enough? • No socioeconomic adjustment
MACRA Proposed Rule: What You Need to Know 8/2016