The Radial Approach for CTO PCI Utility in














- Slides: 55
The Radial Approach for CTO PCI Utility in the Retrograde and the Antegrade Approaches Shigeru Saito, MD, FACC, FSCAI, FJCC Shonan Kamakura General Hospital
Shigeru Saito, MD I have no real or apparent conflicts of interest to report.
PCI for a CTO still remains the greatest challenge to the interventional cardiologist • Increased procedural complexity and complications • Low procedural success rate The most important point during PCI for CTO lesions is: To perform PCI successfully without causing the patients to have a worse clinical conditions than before.
Trans-radial intervention (TRI) Sometimes TRI with retrograde approach can make possible what seems to be impossible to treat by PCI.
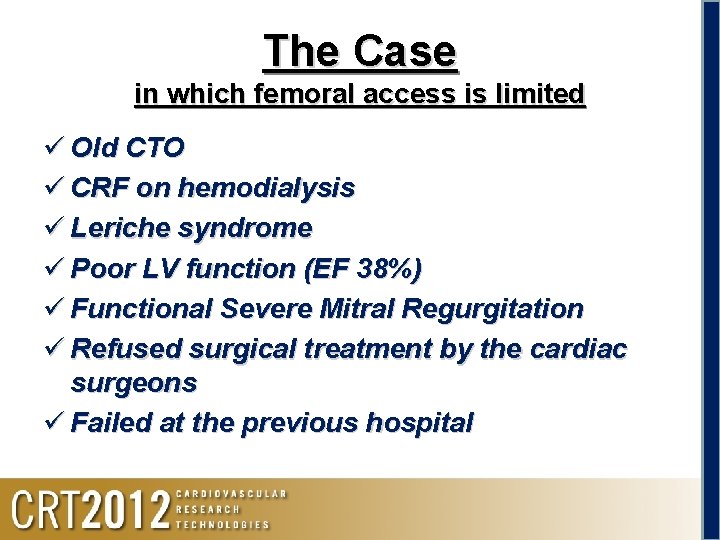
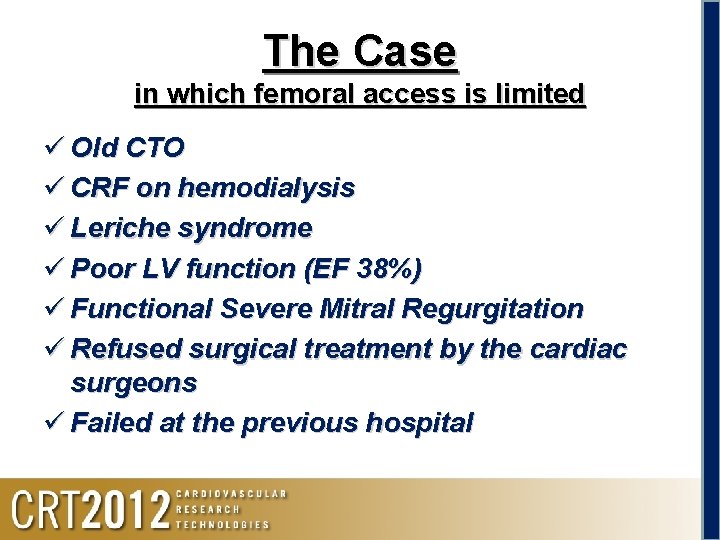
The Case in which femoral access is limited ü Old CTO ü CRF on hemodialysis ü Leriche syndrome ü Poor LV function (EF 38%) ü Functional Severe Mitral Regurgitation ü Refused surgical treatment by the cardiac surgeons ü Failed at the previous hospital
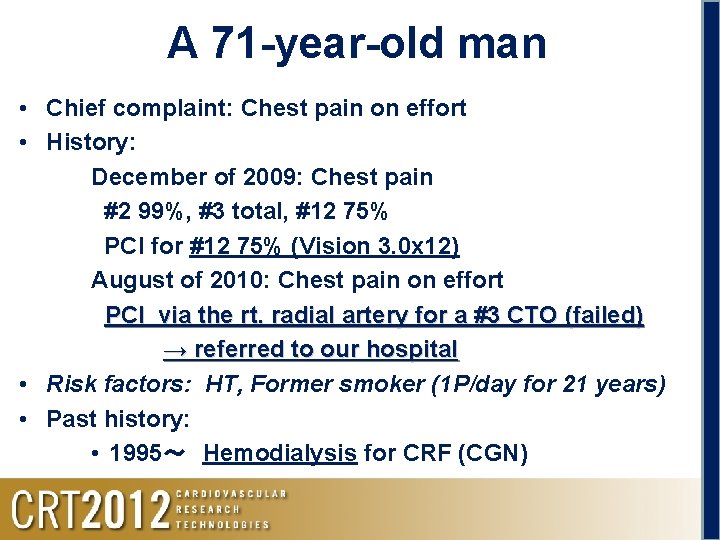
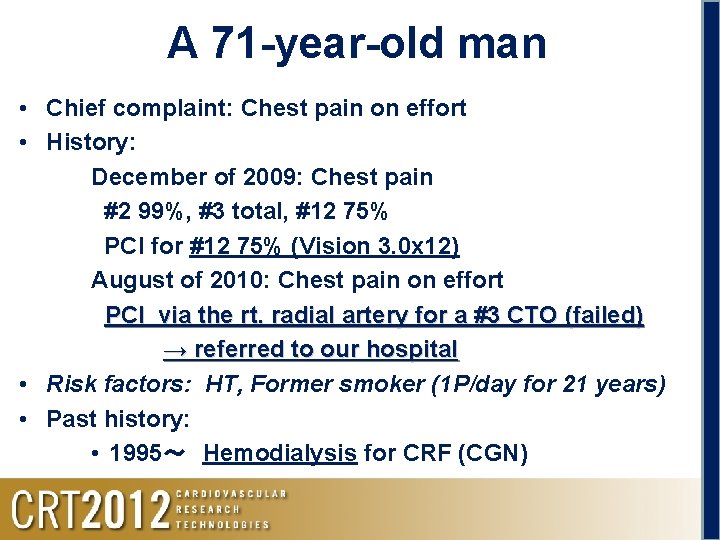
A 71 -year-old man • Chief complaint: Chest pain on effort • History: December of 2009: Chest pain #2 99%, #3 total, #12 75% PCI for #12 75% (Vision 3. 0 x 12) August of 2010: Chest pain on effort PCI via the rt. radial artery for a #3 CTO (failed) → referred to our hospital • Risk factors: HT, Former smoker (1 P/day for 21 years) • Past history: • 1995~ Hemodialysis for CRF (CGN)

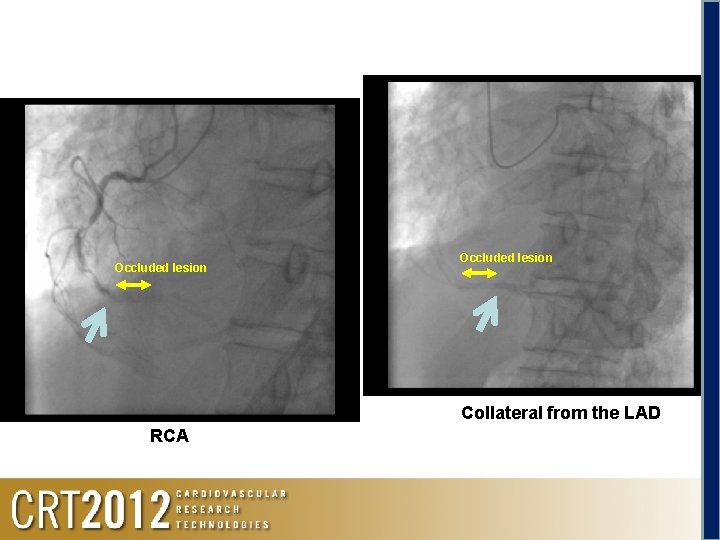
RCA

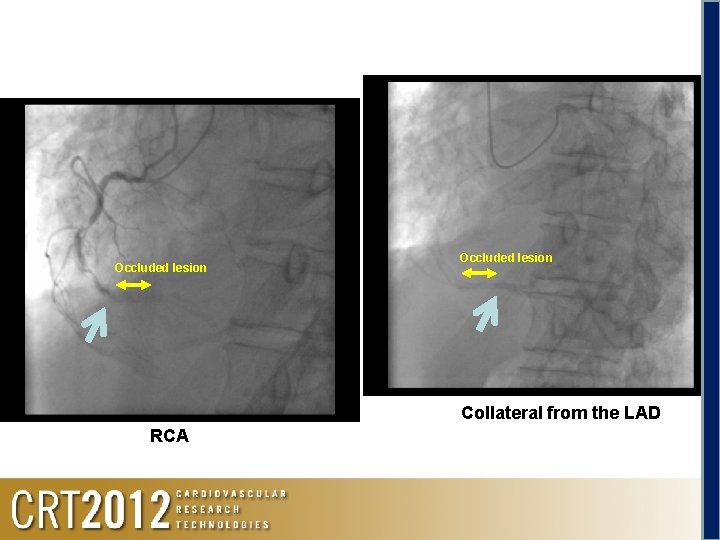
Occluded lesion Collateral from the LAD RCA

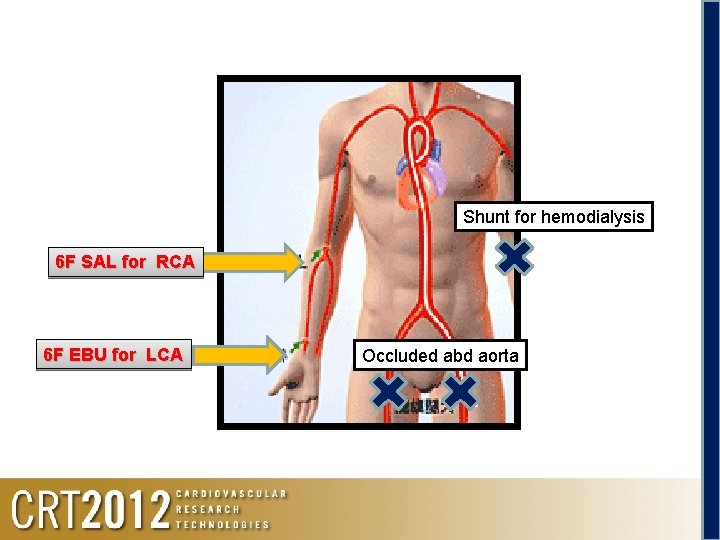
Occluded abdominal aorta Abdominal aorta occlusion
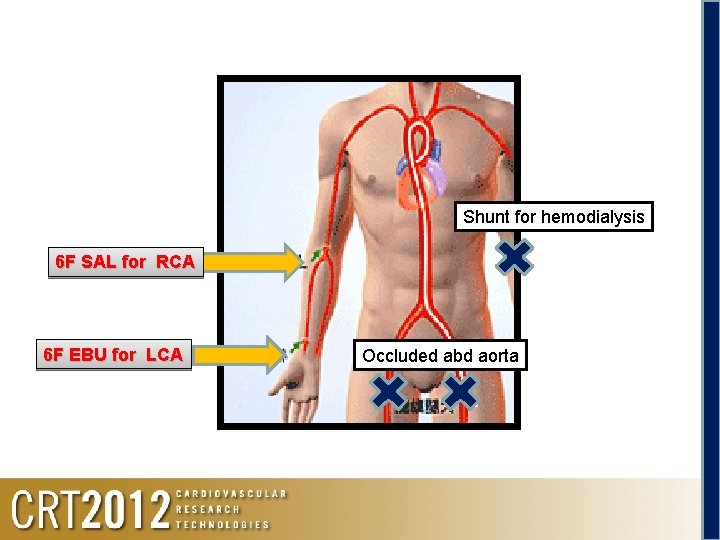
Shunt for hemodialysis 6 F SAL for RCA 6 F EBU for LCA Occluded abd aorta
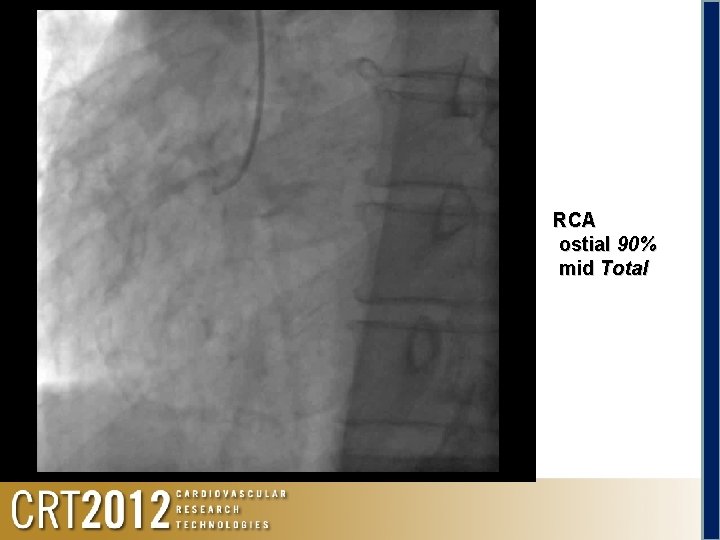
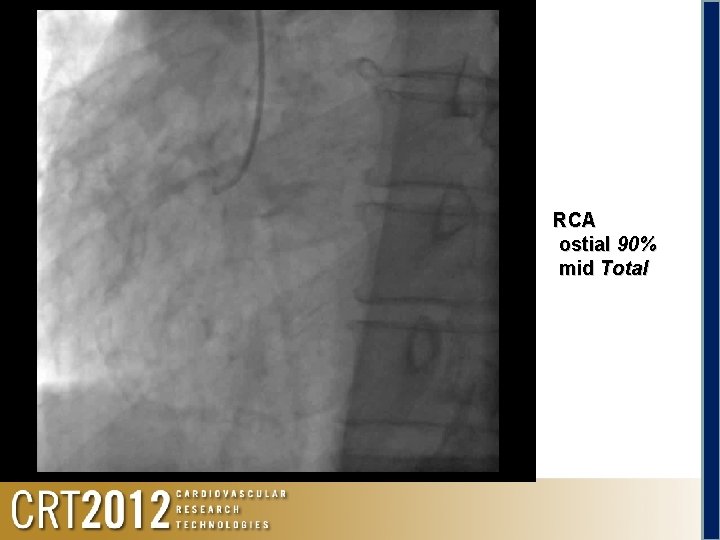
Angio RCA ostial 90% mid Total
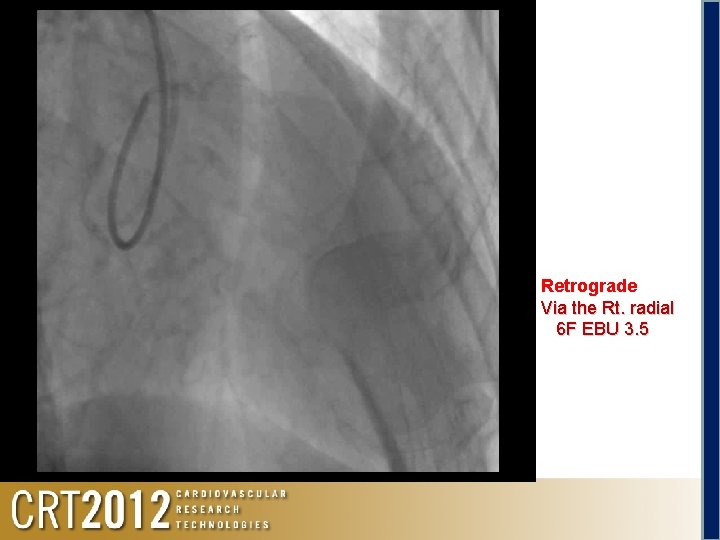
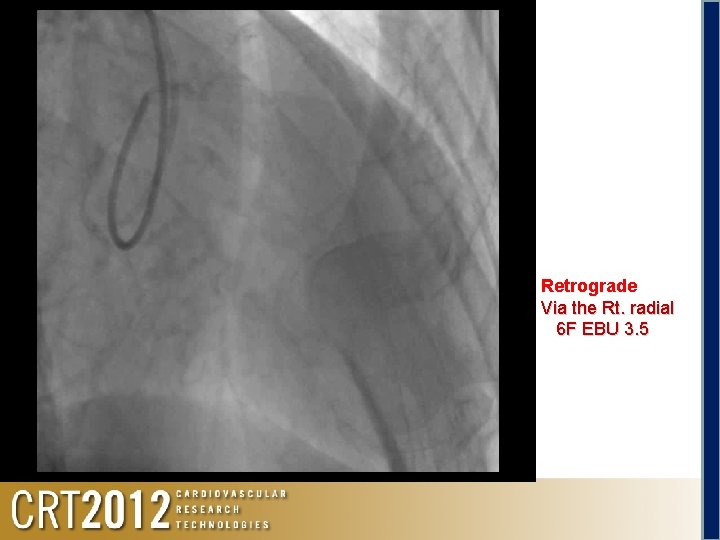
Angio LCA Retrograde Via the Rt. radial 6 F EBU 3. 5
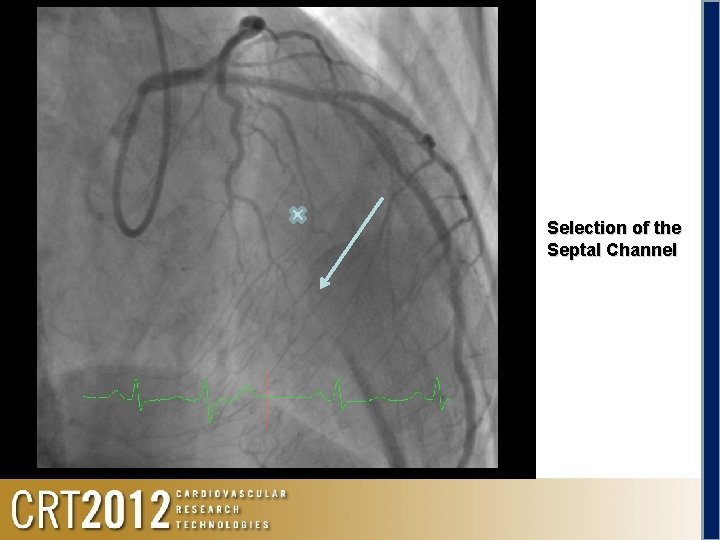
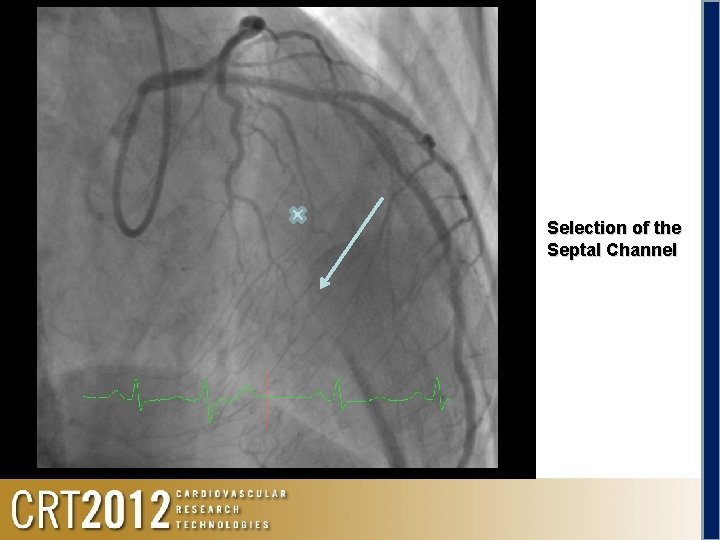
Selection of the Septal Channel
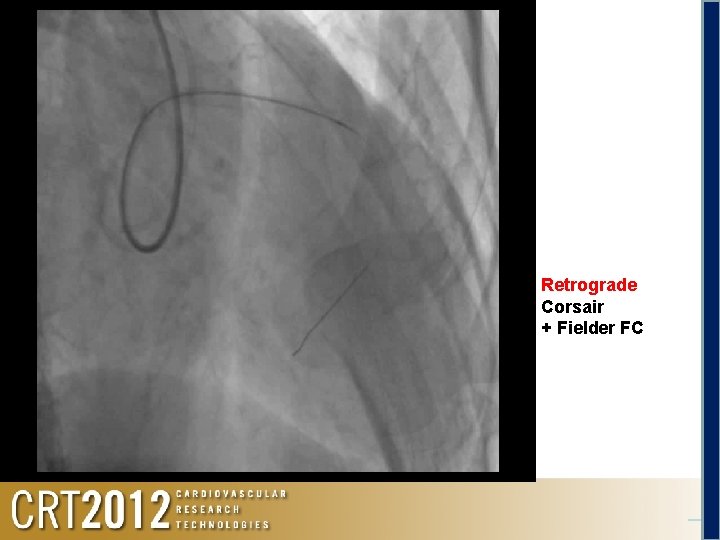
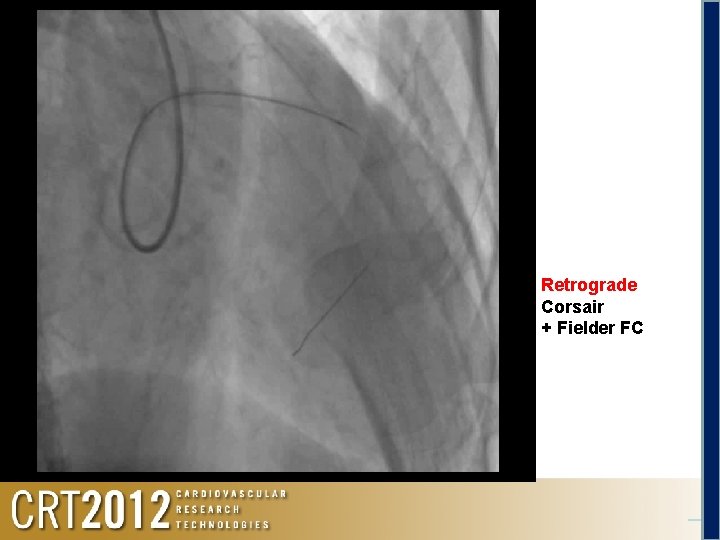
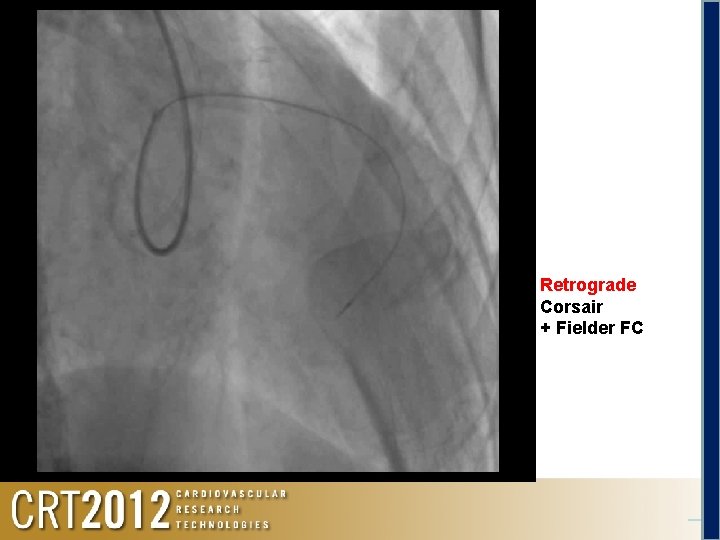
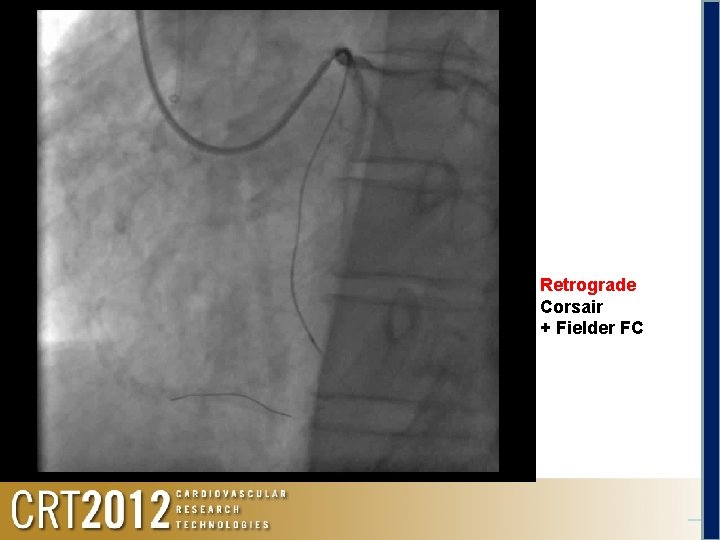
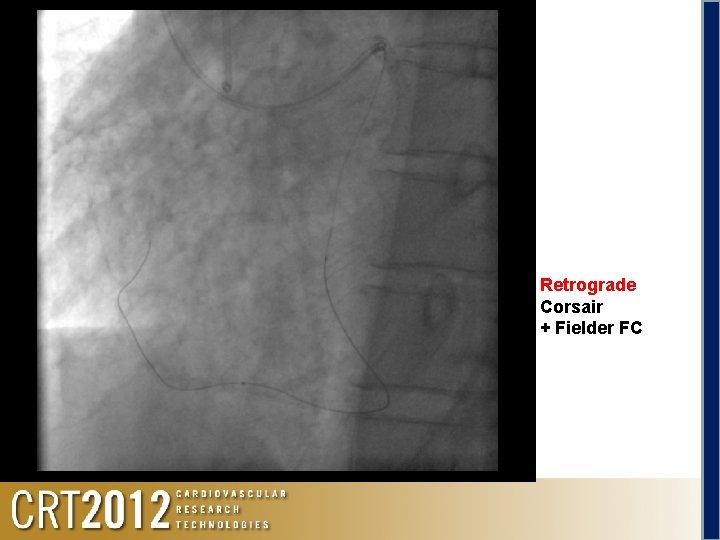
Retrograde Corsair + Fielder FC
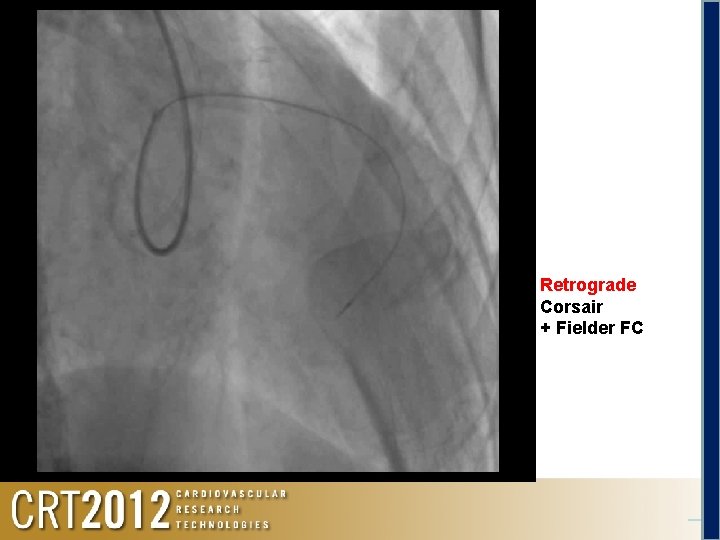
Retrograde Corsair + Fielder FC
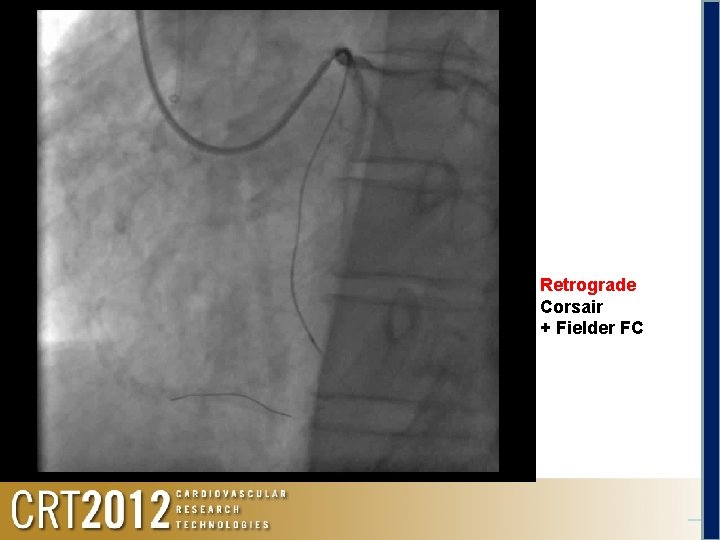
Retrograde Corsair + Fielder FC
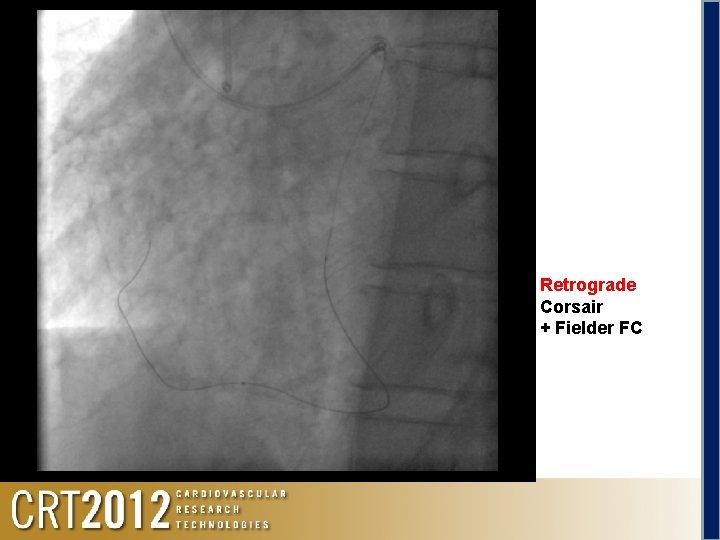
Retrograde Corsair + Fielder FC
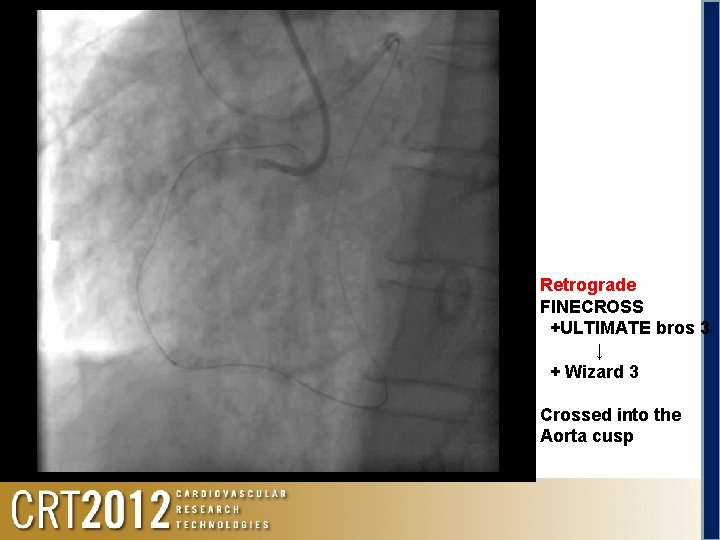
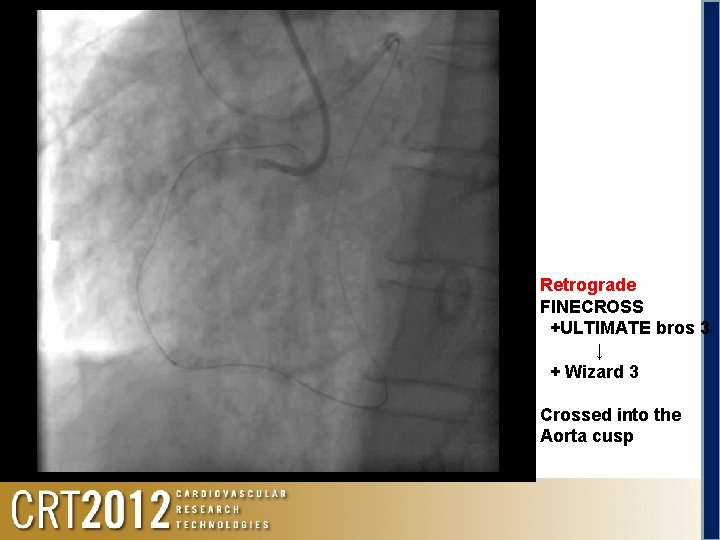
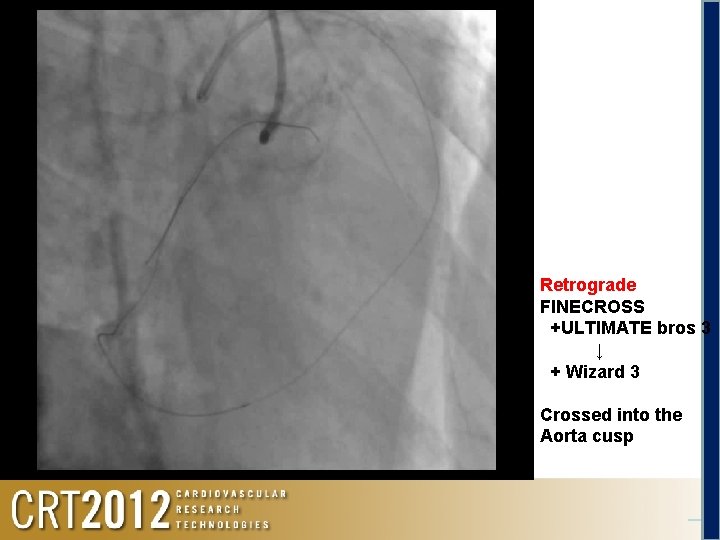
Retrograde FINECROSS +ULTIMATE bros 3 ↓ + Wizard 3 Crossed into the Aorta cusp
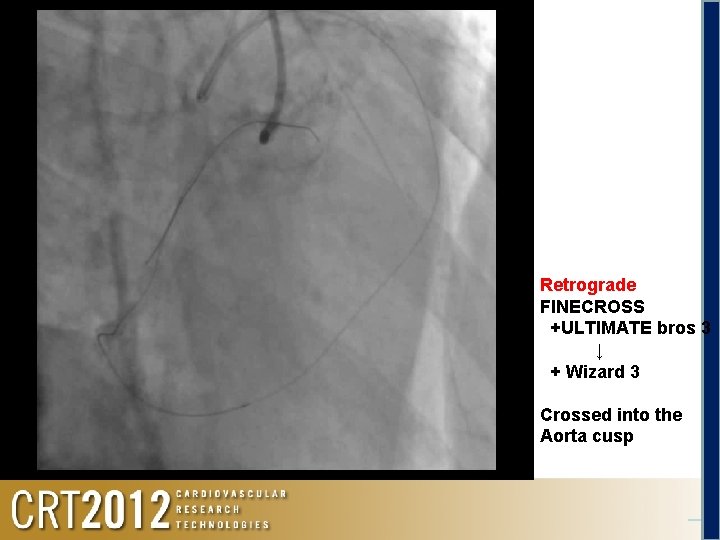
Retrograde FINECROSS +ULTIMATE bros 3 ↓ + Wizard 3 Crossed into the Aorta cusp
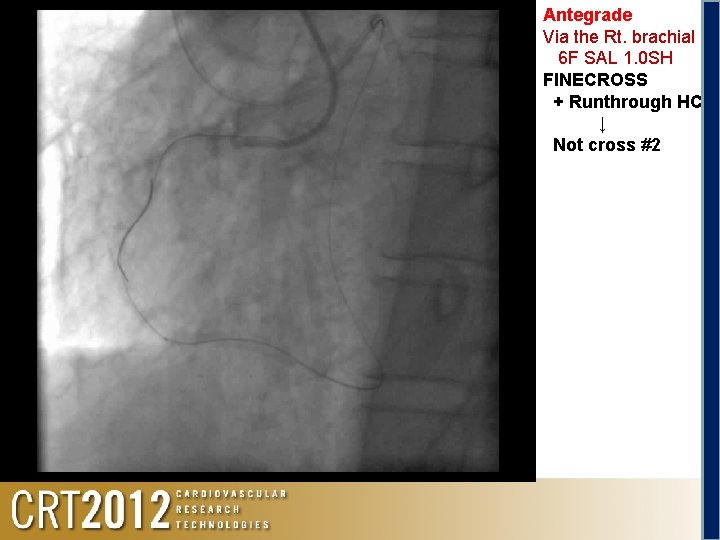
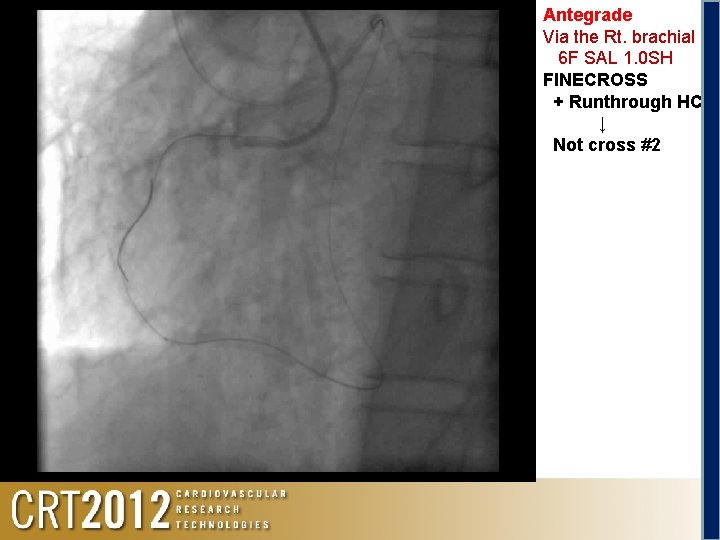
Antegrade Via the Rt. brachial 6 F SAL 1. 0 SH FINECROSS + Runthrough HC ↓ Not cross #2
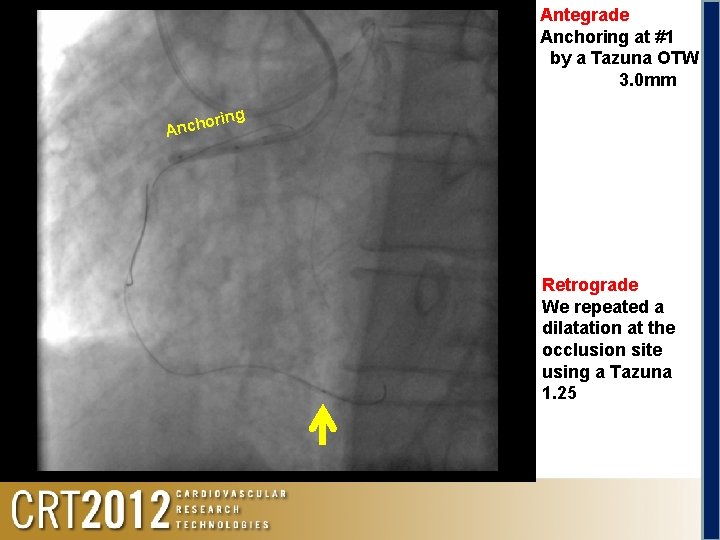
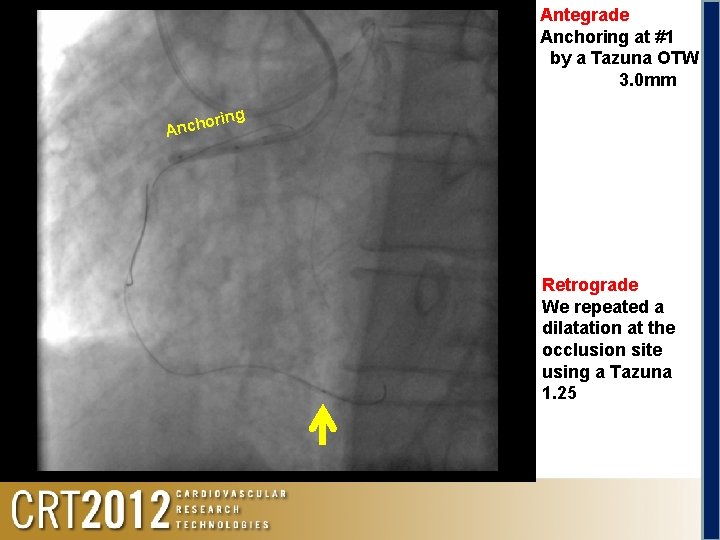
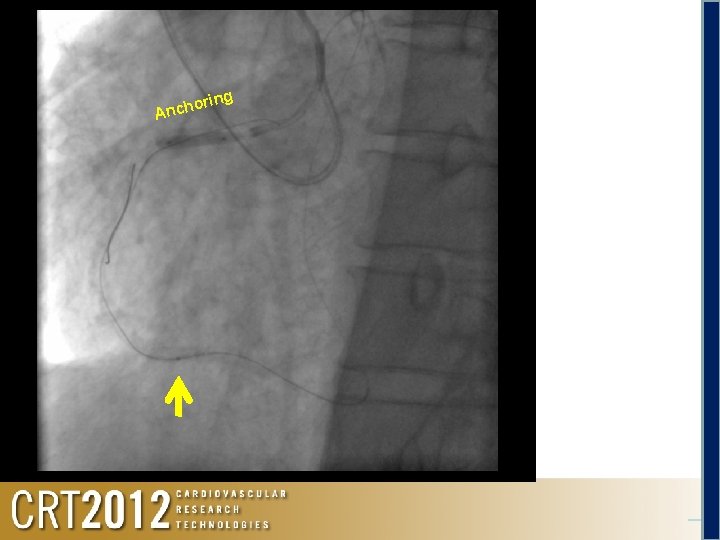
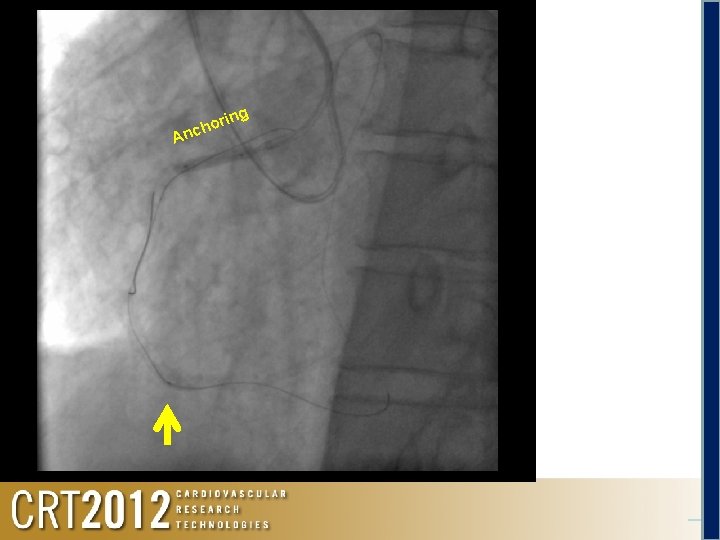
Antegrade Anchoring at #1 by a Tazuna OTW 3. 0 mm oring h c n A Retrograde We repeated a dilatation at the occlusion site using a Tazuna 1. 25
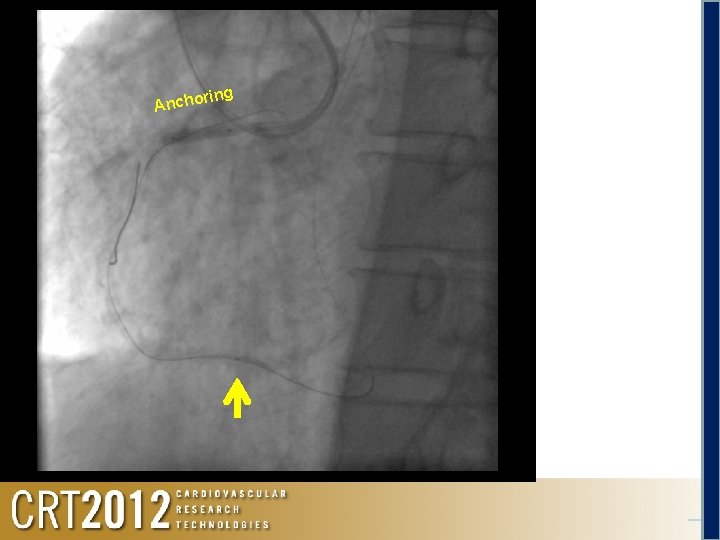
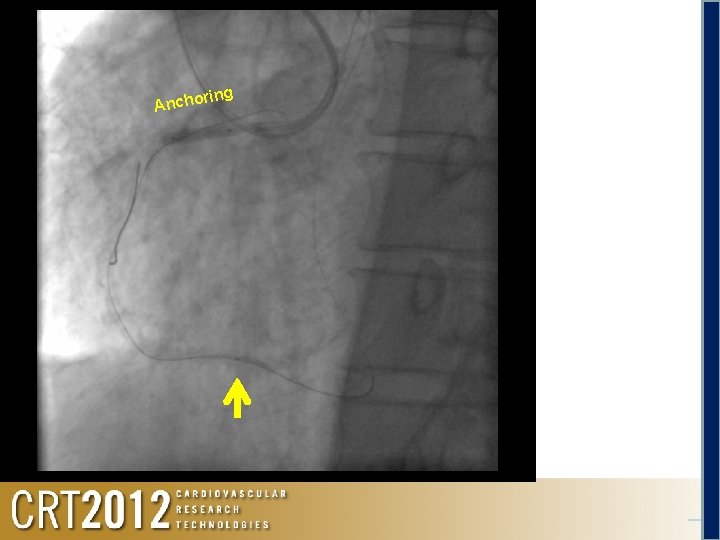
r Ancho ing
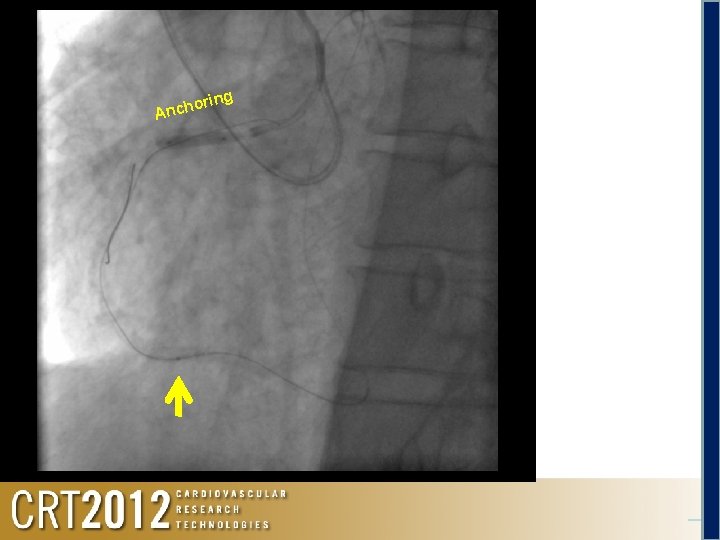
ring o h c An
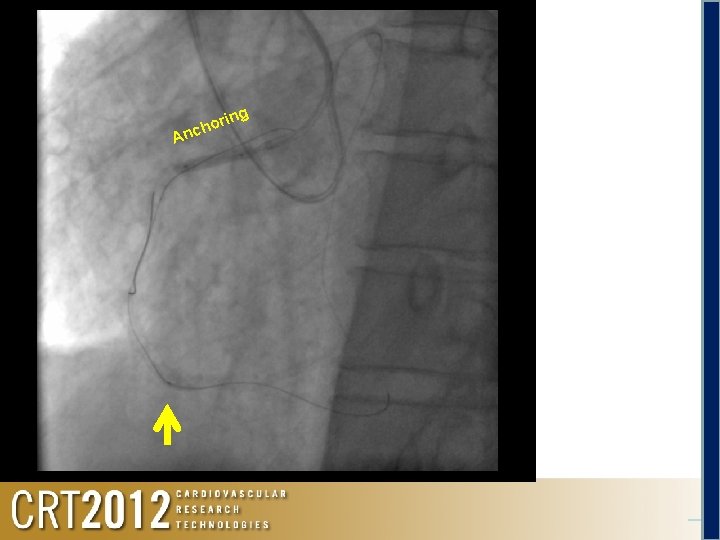
A or h c n ing
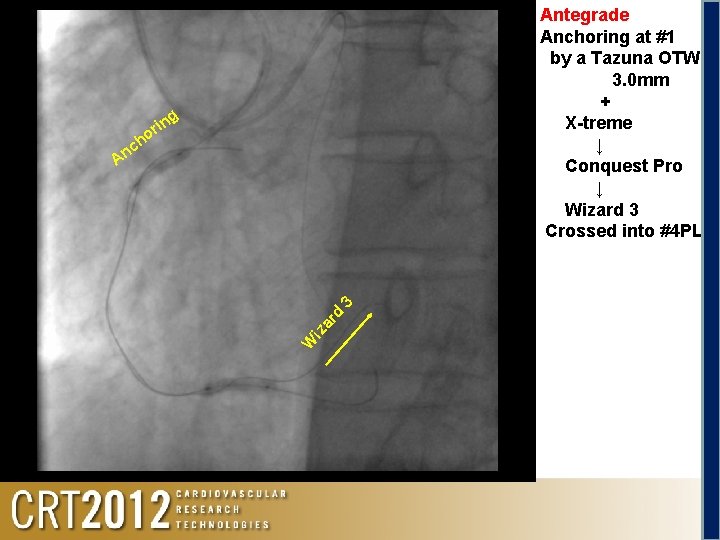
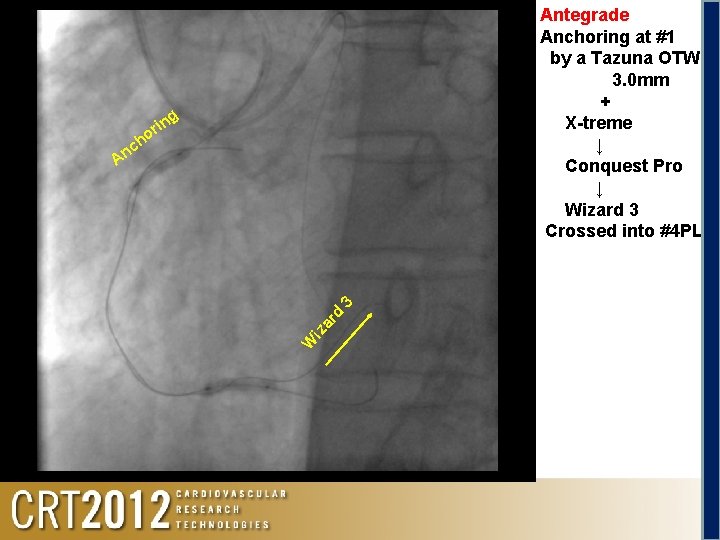
Antegrade Anchoring at #1 by a Tazuna OTW 3. 0 mm + X-treme ↓ Conquest Pro ↓ Wizard 3 Crossed into #4 PL g rin o ch W iz ar d 3 An
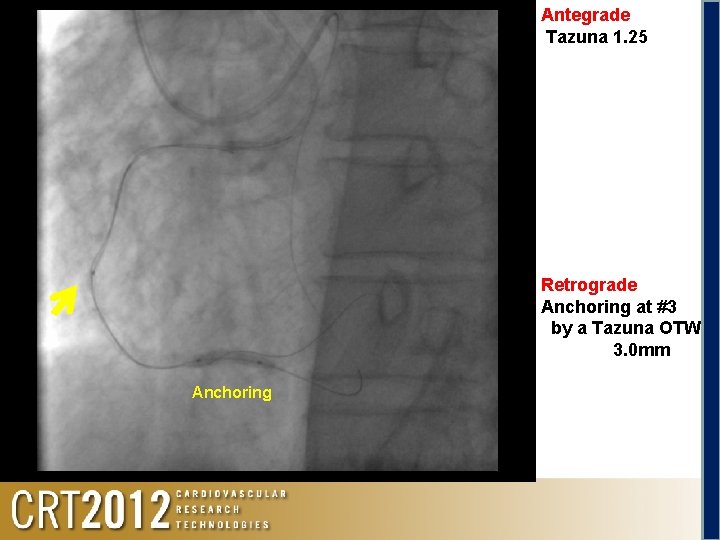
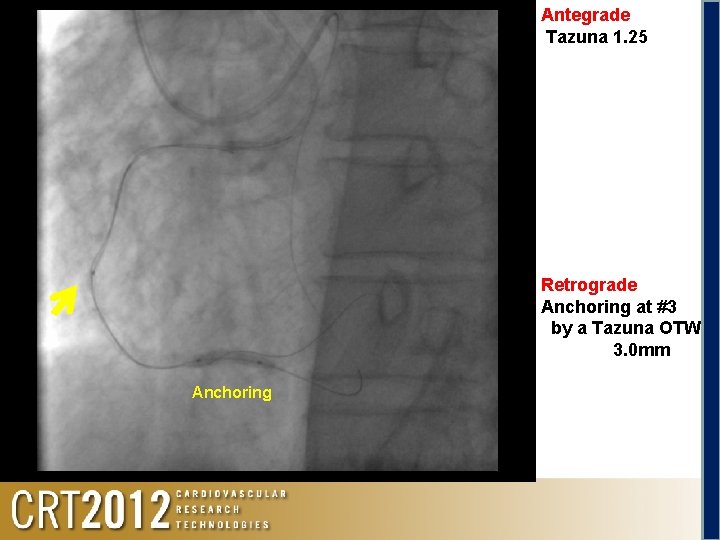
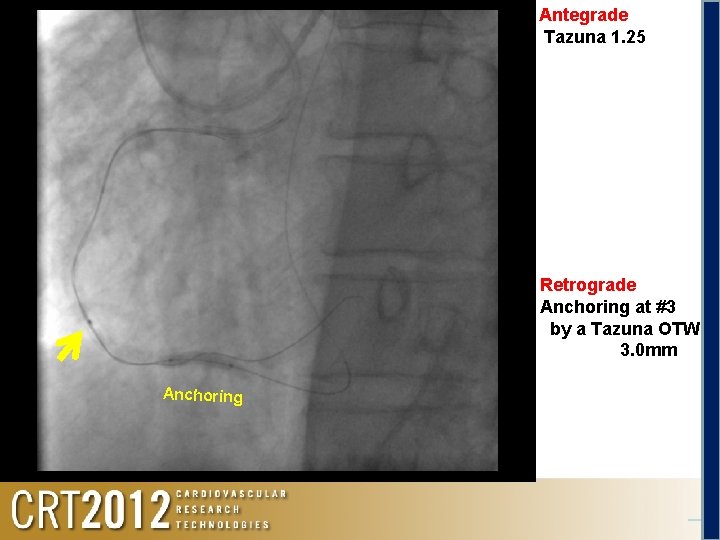
Antegrade Tazuna 1. 25 Retrograde Anchoring at #3 by a Tazuna OTW 3. 0 mm Anchoring

Antegrade Tazuna 1. 25 Retrograde Anchoring at #3 by a Tazuna OTW 3. 0 mm Anchoring
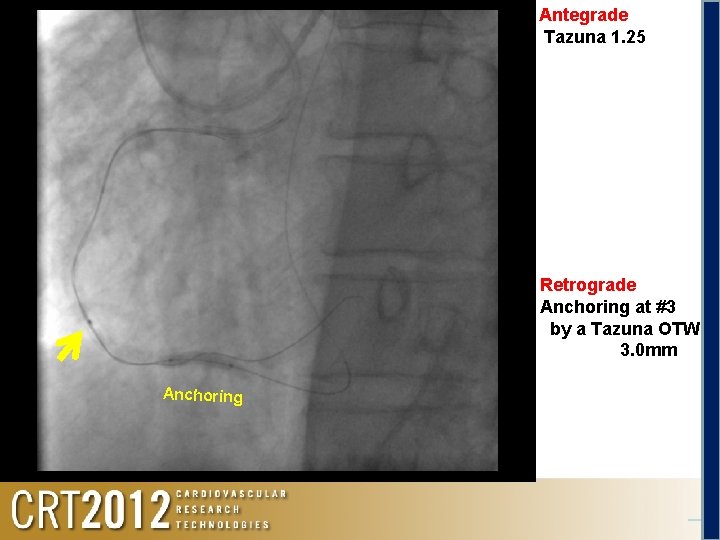
Antegrade Tazuna 1. 25 Retrograde Anchoring at #3 by a Tazuna OTW 3. 0 mm Anchoring
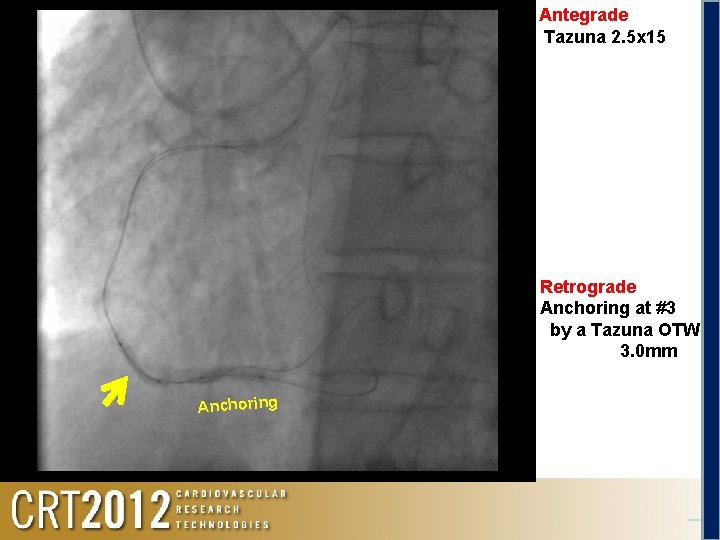
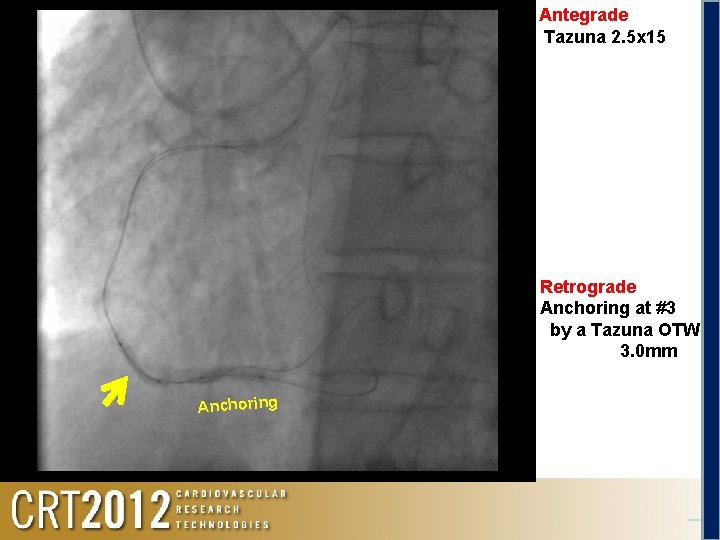
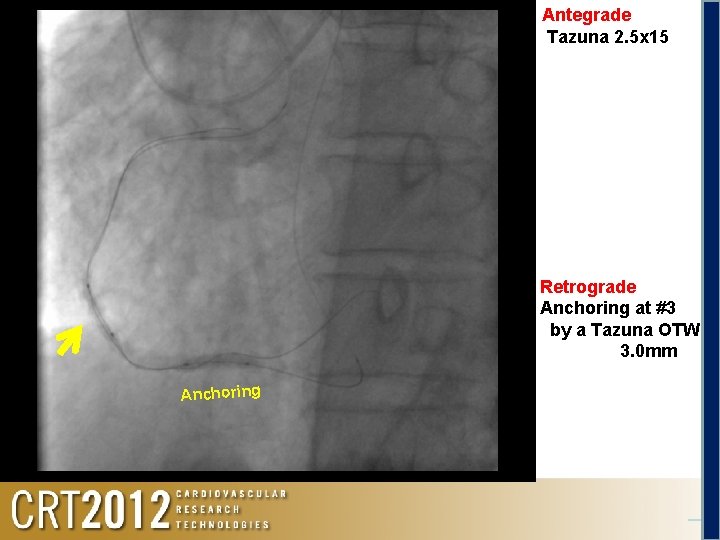
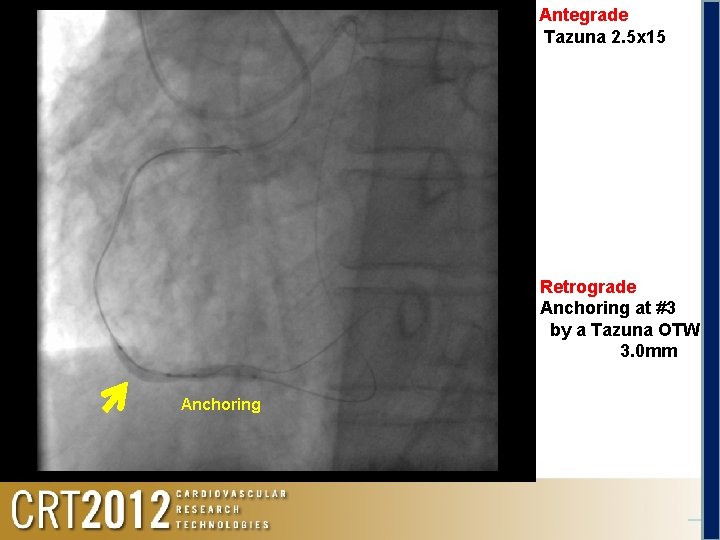
Antegrade Tazuna 2. 5 x 15 Retrograde Anchoring at #3 by a Tazuna OTW 3. 0 mm Anchoring
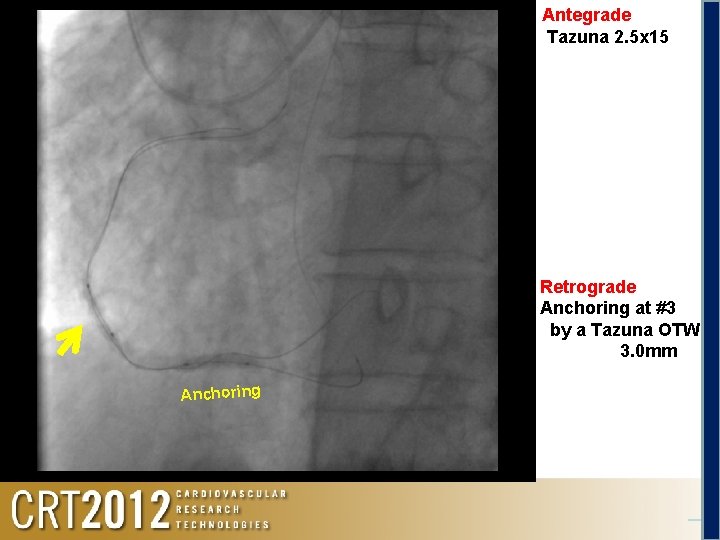
Antegrade Tazuna 2. 5 x 15 Retrograde Anchoring at #3 by a Tazuna OTW 3. 0 mm Anchoring
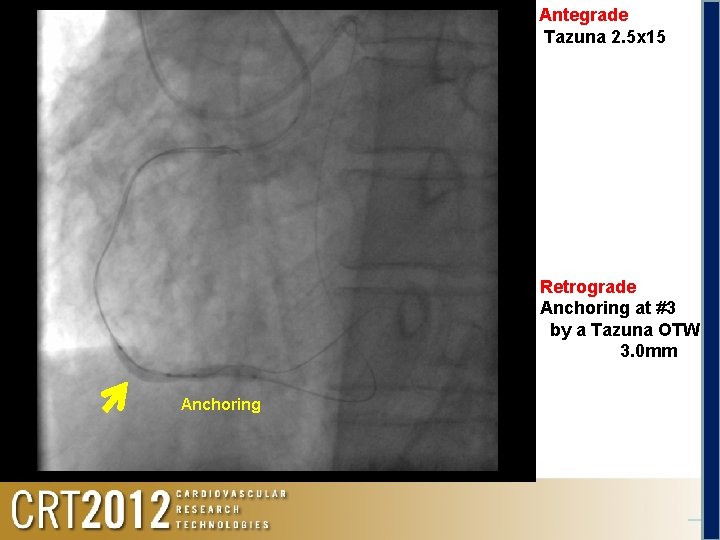
Antegrade Tazuna 2. 5 x 15 Retrograde Anchoring at #3 by a Tazuna OTW 3. 0 mm Anchoring

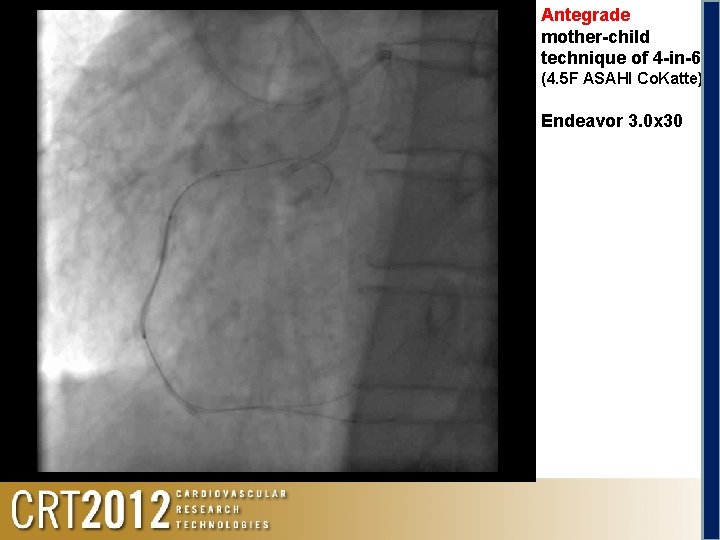
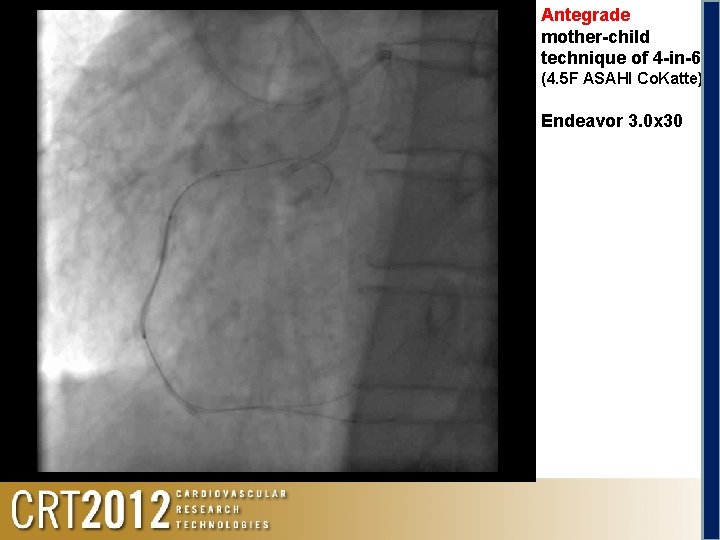
Antegrade mother-child technique of 4 -in-6 (4. 5 F ASAHI Co. Katte) Endeavor 3. 0 x 30








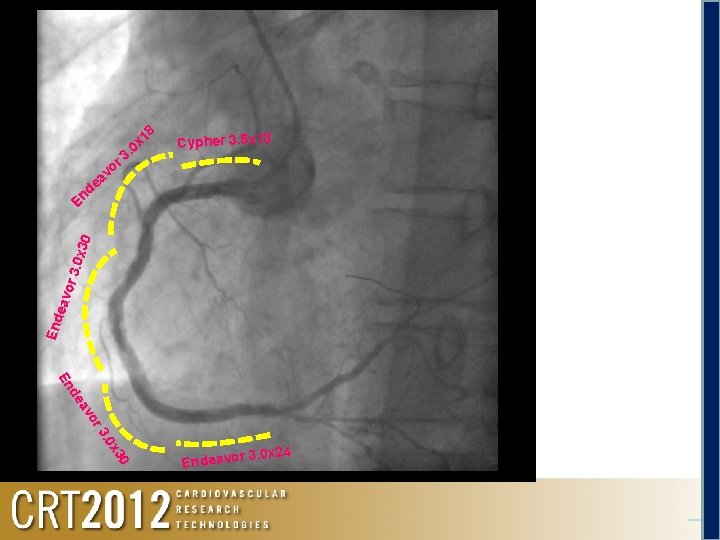
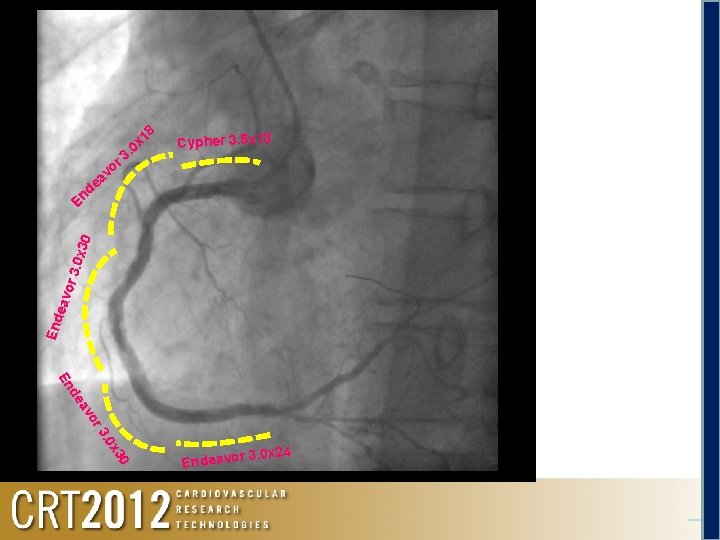
Cypher 3. 5 x 13 End eav or 3. 0 x 3 0 18 x 0 3. or v ea d En 0 x 3 3. 0 or av de En 3. 0 x 24 Endeavor

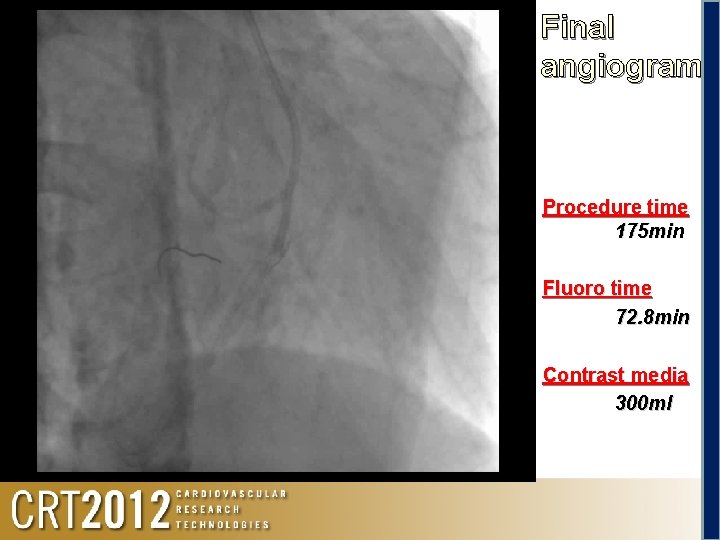
Final angiogram
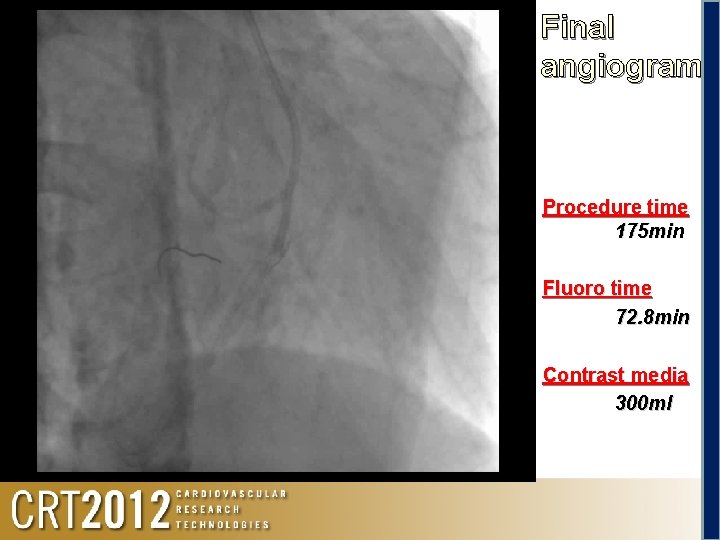
Final angiogram Procedure time 175 min Fluoro time 72. 8 min Contrast media 300 ml
ü Because of a severe calcified lesion, catheter procedure was difficult, but the CTO lesion was ultimately opened. ü This case was challenging in that no mechanical devices for hemodynamic support were available to use because of bifemoral occlusions and even only one complication could have become very serious and potentially fatal. ü We performed a PCI for the CTO with a bidirectional approach via the ipsilateral radial and brachial arteries due to necessity.
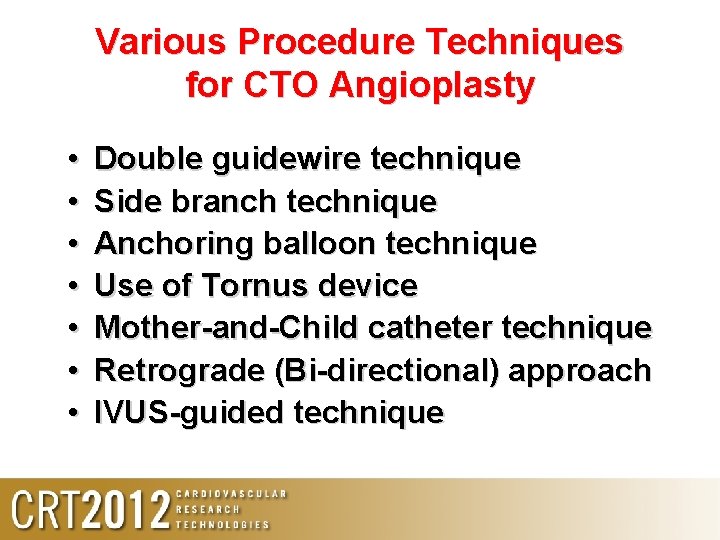
Various Procedure Techniques for CTO Angioplasty • • Double guidewire technique Side branch technique Anchoring balloon technique Use of Tornus device Mother-and-Child catheter technique Retrograde (Bi-directional) approach IVUS-guided technique
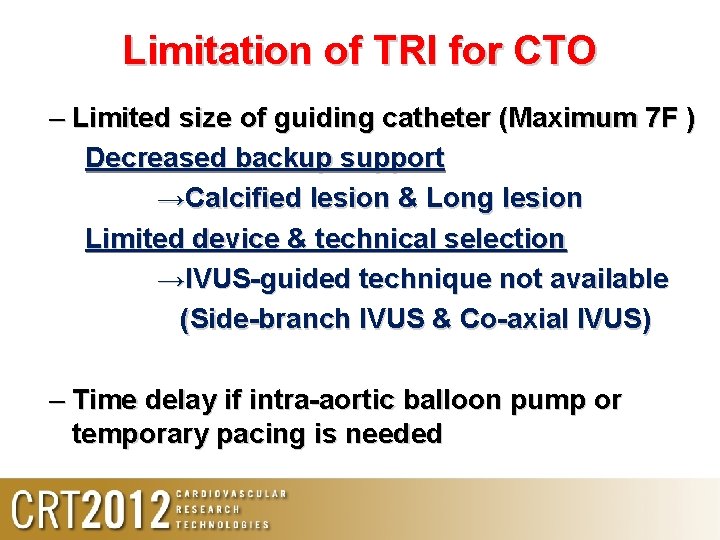
Limitation of TRI for CTO – Limited size of guiding catheter (Maximum 7 F ) Decreased backup support →Calcified lesion & Long lesion Limited device & technical selection →IVUS-guided technique not available (Side-branch IVUS & Co-axial IVUS) – Time delay if intra-aortic balloon pump or temporary pacing is needed
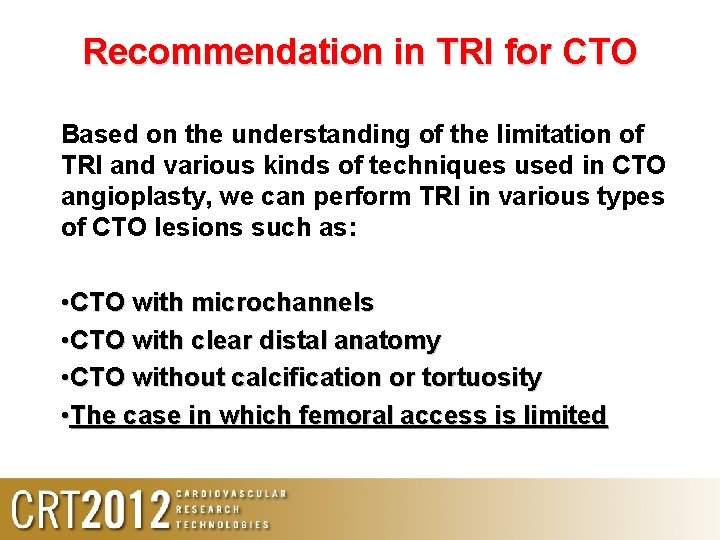
Recommendation in TRI for CTO Based on the understanding of the limitation of TRI and various kinds of techniques used in CTO angioplasty, we can perform TRI in various types of CTO lesions such as: • CTO with microchannels • CTO with clear distal anatomy • CTO without calcification or tortuosity • The case in which femoral access is limited
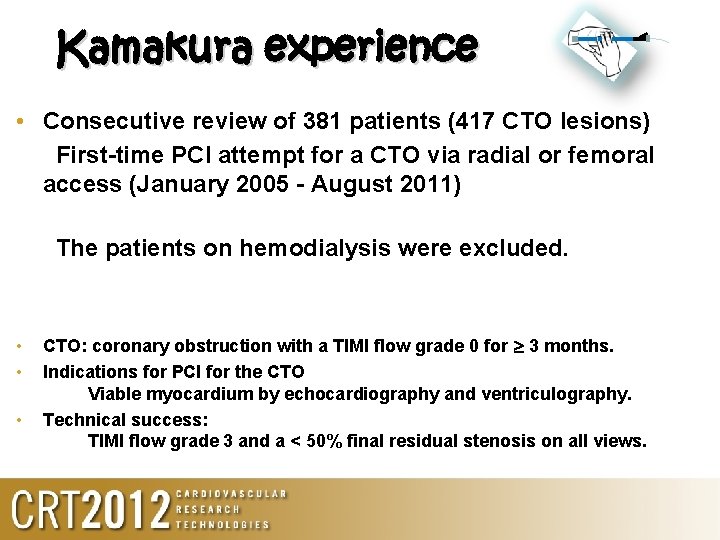
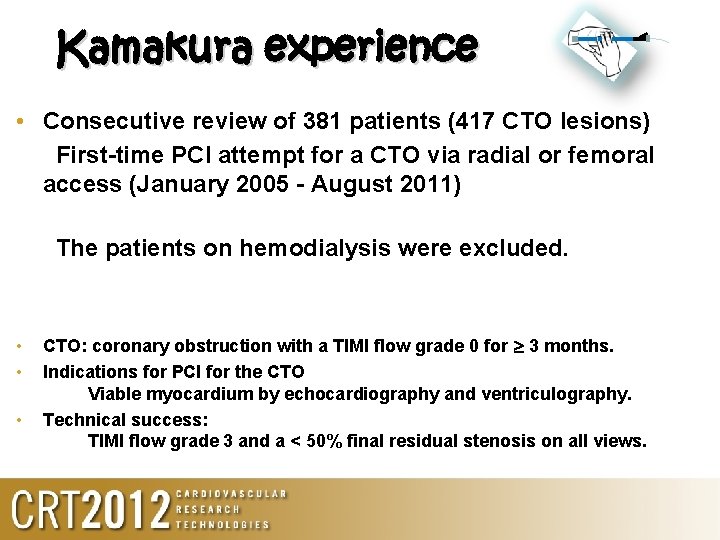
Kamakura experience • Consecutive review of 381 patients (417 CTO lesions) First-time PCI attempt for a CTO via radial or femoral access (January 2005 - August 2011) The patients on hemodialysis were excluded. • • • CTO: coronary obstruction with a TIMI flow grade 0 for 3 months. Indications for PCI for the CTO Viable myocardium by echocardiography and ventriculography. Technical success: TIMI flow grade 3 and a < 50% final residual stenosis on all views.
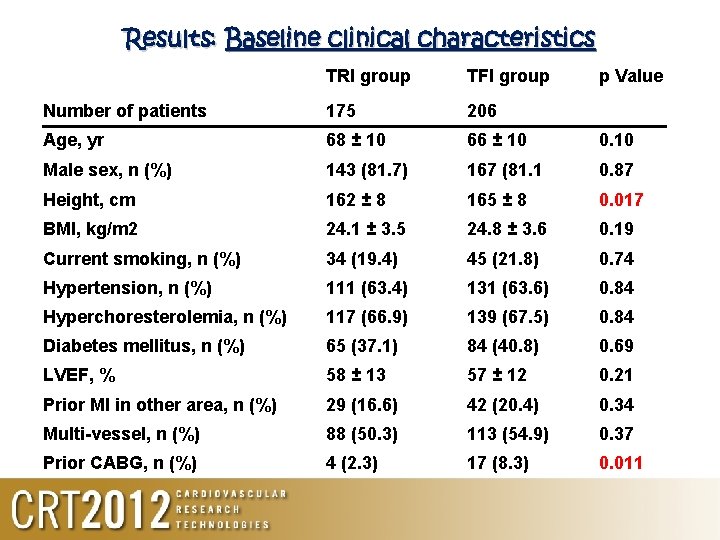
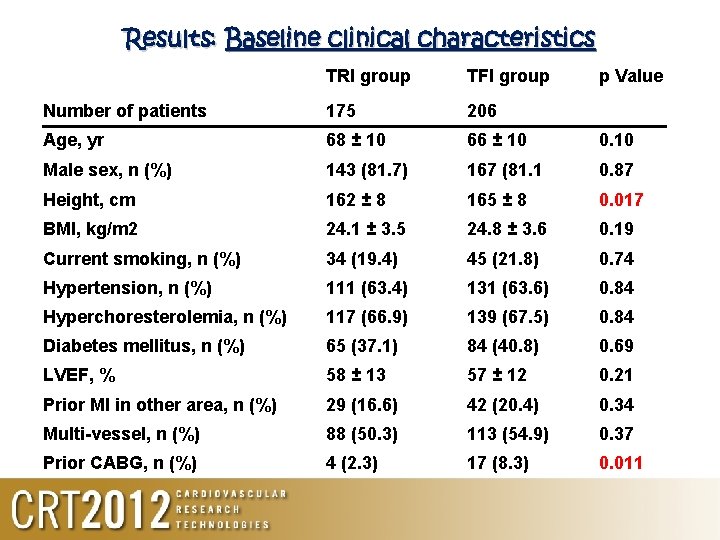
Results: Baseline clinical characteristics TRI group TFI group p Value Number of patients 175 206 Age, yr 68 ± 10 66 ± 10 0. 10 Male sex, n (%) 143 (81. 7) 167 (81. 1 0. 87 Height, cm 162 ± 8 165 ± 8 0. 017 BMI, kg/m 2 24. 1 ± 3. 5 24. 8 ± 3. 6 0. 19 Current smoking, n (%) 34 (19. 4) 45 (21. 8) 0. 74 Hypertension, n (%) 111 (63. 4) 131 (63. 6) 0. 84 Hyperchoresterolemia, n (%) 117 (66. 9) 139 (67. 5) 0. 84 Diabetes mellitus, n (%) 65 (37. 1) 84 (40. 8) 0. 69 LVEF, % 58 ± 13 57 ± 12 0. 21 Prior MI in other area, n (%) 29 (16. 6) 42 (20. 4) 0. 34 Multi-vessel, n (%) 88 (50. 3) 113 (54. 9) 0. 37 Prior CABG, n (%) 4 (2. 3) 17 (8. 3) 0. 011
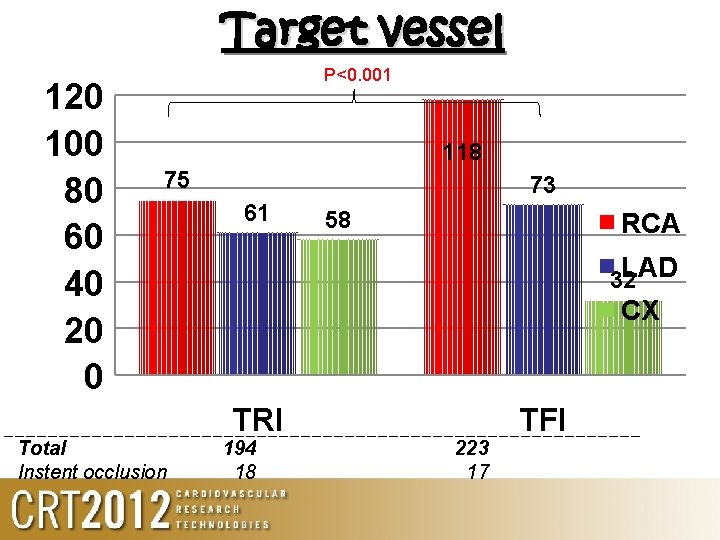
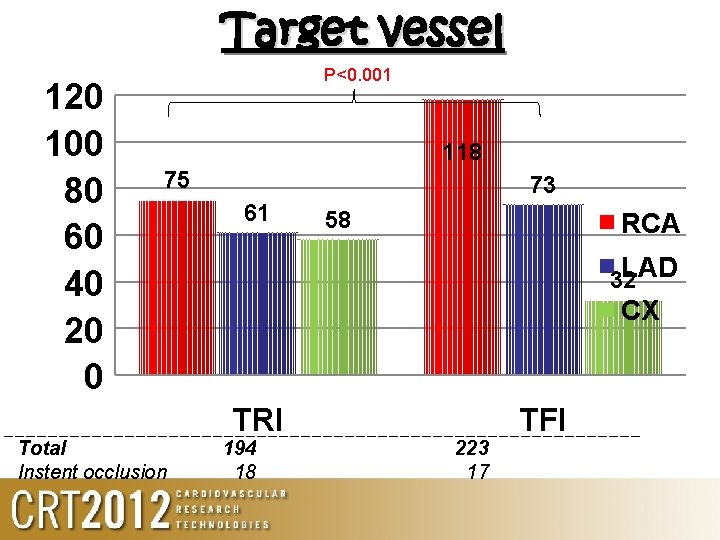
Target vessel 120 100 80 60 40 20 0 P<0. 001 118 75 Total Instent occlusion 73 61 58 RCA LAD 32 CX TRI 194 18 223 17 TFI
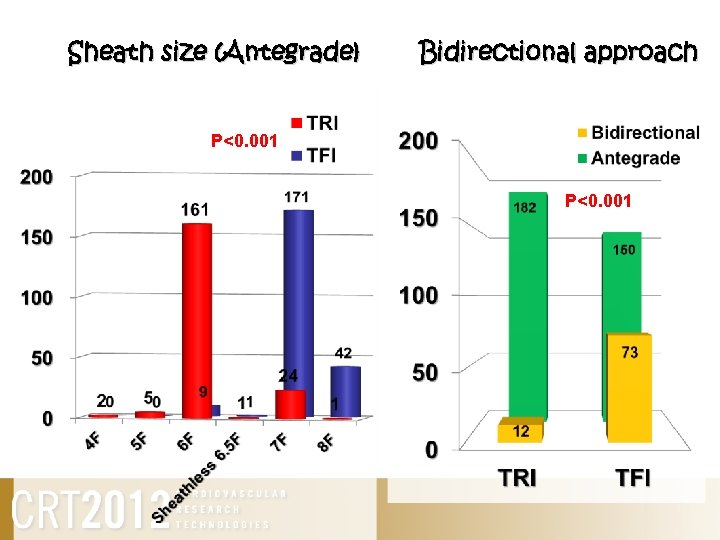
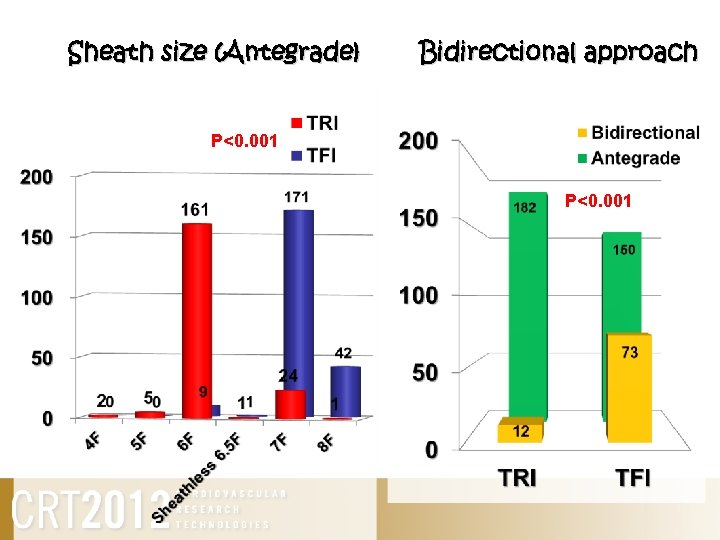
Sheath size (Antegrade) Bidirectional approach P<0. 001
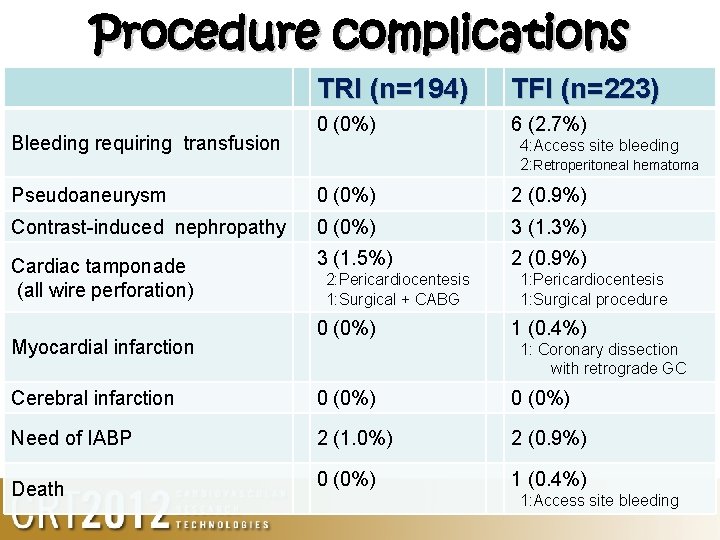
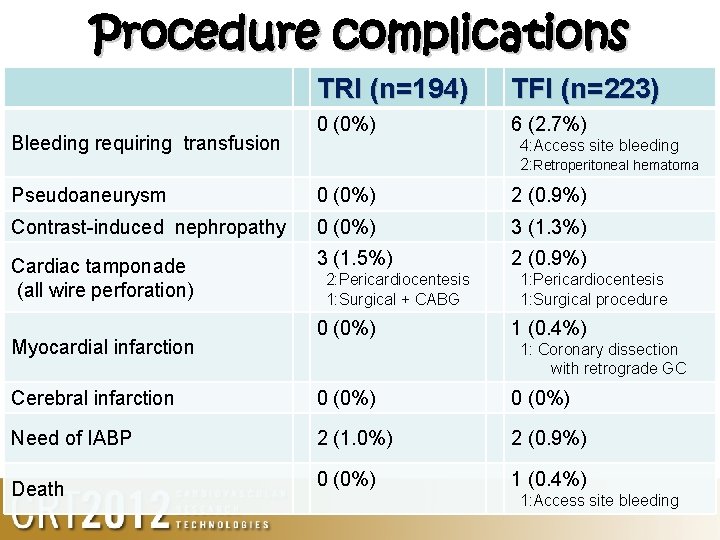
Procedure complications Bleeding requiring transfusion TRI (n=194) TFI (n=223) 0 (0%) 6 (2. 7%) 4: Access site bleeding 2: Retroperitoneal hematoma Pseudoaneurysm 0 (0%) 2 (0. 9%) Contrast-induced nephropathy 0 (0%) 3 (1. 3%) Cardiac tamponade (all wire perforation) 3 (1. 5%) 2 (0. 9%) Myocardial infarction 2: Pericardiocentesis 1: Surgical + CABG 0 (0%) 1: Pericardiocentesis 1: Surgical procedure 1 (0. 4%) 1: Coronary dissection with retrograde GC Cerebral infarction 0 (0%) Need of IABP 2 (1. 0%) 2 (0. 9%) Death 0 (0%) 1 (0. 4%) 1: Access site bleeding
With an appropriate patient/lesion selection, TRI for CTO lesions may result in more favorable short-term outcomes with acceptably high procedural success and lower complication rates. At least 35% of the total CTO lesions can be successfully recanalized by TRI. Therefore, given the correct circumstances, TRI should be considered as an appropriate first-line intervention for CTO lesions.
 Ordinal utility and cardinal utility
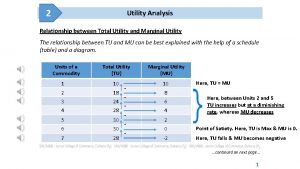
Ordinal utility and cardinal utility Relation between marginal utility and total utility
Relation between marginal utility and total utility Anti radial vs radial ultrasound
Anti radial vs radial ultrasound Law of equi marginal utility
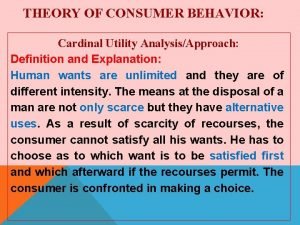
Law of equi marginal utility Cardinal utility
Cardinal utility Miraclebros guidewire
Miraclebros guidewire Cto survey
Cto survey Cto
Cto Posack obligation
Posack obligation Somi brace indications
Somi brace indications Tata motors cto
Tata motors cto Manuales cto
Manuales cto Hybrid algorithm cto
Hybrid algorithm cto Gponhub
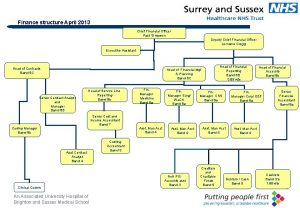
Gponhub Ceo direct reports
Ceo direct reports Cto
Cto Cto forum magazine
Cto forum magazine Cto ceo cmo
Cto ceo cmo Star cto technique
Star cto technique Apa itu cto
Apa itu cto Cto workday
Cto workday Vertical
Vertical Barclays digital transformation
Barclays digital transformation Cto organizational chart
Cto organizational chart Uscybercom cto 10-084
Uscybercom cto 10-084 Dts stuck at cto booked
Dts stuck at cto booked Cto persona
Cto persona Sfa cto
Sfa cto Gaia second wire
Gaia second wire Thomson reuters labs
Thomson reuters labs Cto sims
Cto sims Pci-32765
Pci-32765 Pci sabirnica
Pci sabirnica Sox pci compliance wikipedia
Sox pci compliance wikipedia Pci magistrala
Pci magistrala Agp pci
Agp pci Niveaux pci dss
Niveaux pci dss Datakiosk
Datakiosk Pci uex
Pci uex Pci en salud
Pci en salud Pci en salud
Pci en salud Pci-8330
Pci-8330 Pci tutorial
Pci tutorial Controller acquisizione dati e elaborazione segnali pci
Controller acquisizione dati e elaborazione segnali pci Redual
Redual Geometria dos pares de eletrons
Geometria dos pares de eletrons Barramento pci
Barramento pci Pci osi
Pci osi Pci reading
Pci reading Pci class codes
Pci class codes Headed concrete anchors
Headed concrete anchors Pci en salud
Pci en salud Tipos de barramentos
Tipos de barramentos Microsoft from back doors gov active
Microsoft from back doors gov active Pci
Pci Palin pci manual
Palin pci manual