The Knee and Related Structures Chapter 16 Pages




- Slides: 21
The Knee and Related Structures Chapter 16 Pages 384 -409
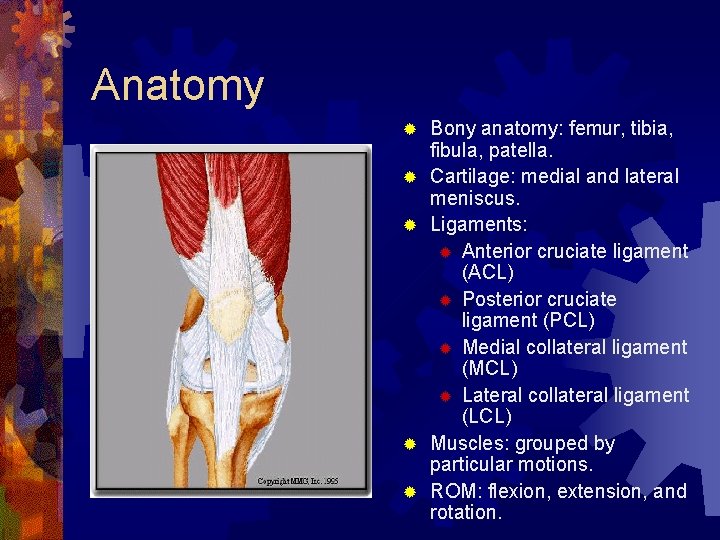
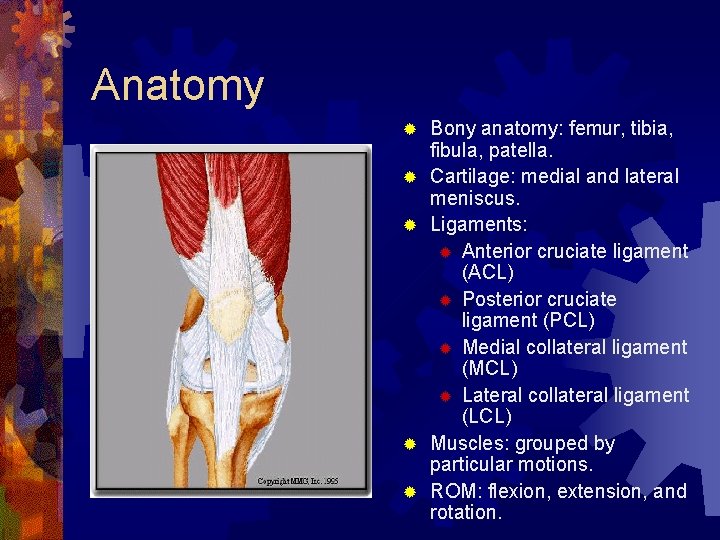
Anatomy ® ® ® Bony anatomy: femur, tibia, fibula, patella. Cartilage: medial and lateral meniscus. Ligaments: ® Anterior cruciate ligament (ACL) ® Posterior cruciate ligament (PCL) ® Medial collateral ligament (MCL) ® Lateral collateral ligament (LCL) Muscles: grouped by particular motions. ROM: flexion, extension, and rotation.

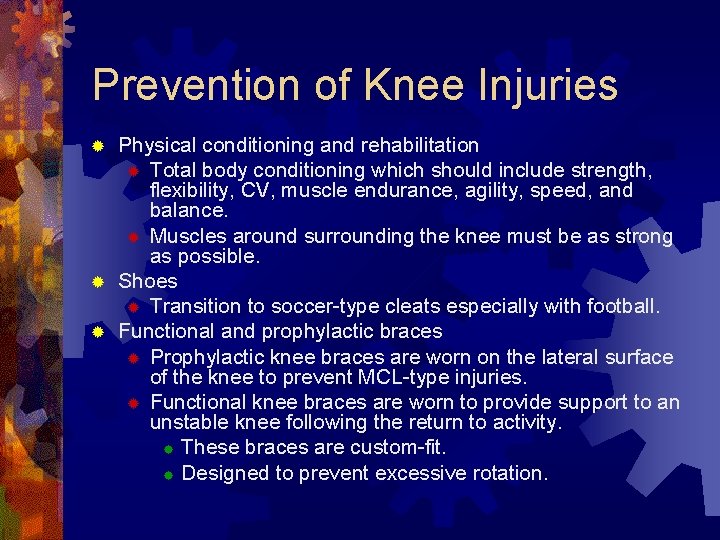
Prevention of Knee Injuries Physical conditioning and rehabilitation ® Total body conditioning which should include strength, flexibility, CV, muscle endurance, agility, speed, and balance. ® Muscles around surrounding the knee must be as strong as possible. ® Shoes ® Transition to soccer-type cleats especially with football. ® Functional and prophylactic braces ® Prophylactic knee braces are worn on the lateral surface of the knee to prevent MCL-type injuries. ® Functional knee braces are worn to provide support to an unstable knee following the return to activity. ® These braces are custom-fit. ® Designed to prevent excessive rotation. ®
Assessment Principles: History ® Current injury: ® ® ® ® What were you doing when the knee was hurt? What position was your body in? Did the knee collapse? Did you hear a noise or feel any sensation at time of injury? Could you move knee after injury? Did swelling occur? Where is pain? Have you hurt knee before? ® Recurrent/chronic injury: ® What is your major compliant? When did you first notice the condition? Is there recurrent swelling? Does the knee ever lock or catch? Is there constant or intermittent pain? Do you feel any grating/grinding sensations? Does your knee feel like it’s going to give away? What does it feel like when you go up/down stairs? What previous treatment have you received? ® ® ® ®
Assessment Principles: Observation ® Do knees appear to be symmetrical? ® Is one knee obviously swollen? ® Is muscle atrophy apparent? ® Does athlete walk with limp? ® Can the athlete fully bear weight? ® Can athlete perform half-squat to extension? ® Can athlete go up and down stairs with ease?
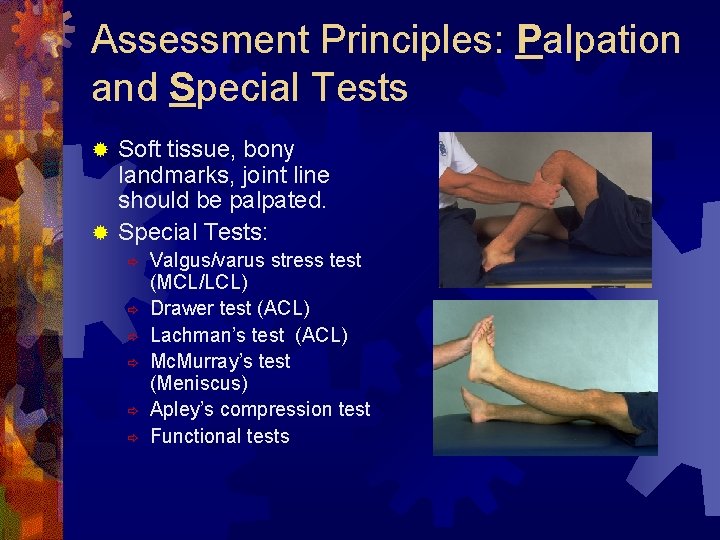
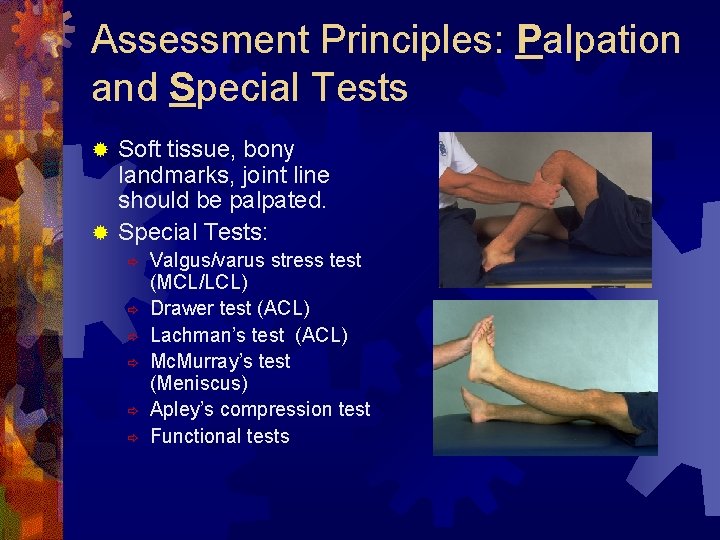
Assessment Principles: Palpation and Special Tests Soft tissue, bony landmarks, joint line should be palpated. ® Special Tests: ® ð ð ð Valgus/varus stress test (MCL/LCL) Drawer test (ACL) Lachman’s test (ACL) Mc. Murray’s test (Meniscus) Apley’s compression test Functional tests

Knee Injuries ® ® ® MCL/LCL sprain ACL sprain PCL sprain Meniscus injuries Joint contusions Bursitis Runner’s knee Fractured patella Patella dislocation/subluxation Chondromalacia patella Patellar tendinitis Osgood-schlatter’s disease
MCL Sprain ® MOI: ® Valgus force from lateral side or external rotation of the tibia. ® S&S: ® Joint stability should be tested immediately. ® G 1, 2, 3 ® Treatment: ® RICE for 24 hours, crutches, knee immobilizer for 2 -5 days, ROM, isometrics, bike, and more functional activities. ® http: //www. youtube. com/watch? v=Le 8 r. Mn. L 56 w 8
LCL Sprain ® MOI: ® Laterally directed varus force from the medial side or from internal rotation of the tibia. ® S&S: ® Pain and tenderness over LCL, swelling and effusion, laxity with varus stress test at 30 degrees. ® Treatment: ® Same as MCL.
ACL Sprain ® MOI: ® External rotation of the foot and internal rotation of the knee. Hyperextension. ® S&S: ® Audible pop, rapid swelling, intense pain, positive Lachman’s. ® Treatment: ® Immediate RICE, crutches, surgery, 3 -5 weeks in brace, 4 -6 months in rehab, functional knee brace. ® ® http: //www. youtube. com/watch? v=Lu. Cl. We. D 9 ou. I&feature=related http: //www. youtube. com/watch? v=Wc. G 0 Ryl. J 8 y. E&feature=related http: //www. youtube. com/watch? v=ct. AP-1 e. OJxk&feature=related http: //www. youtube. com/watch? v=j. MLFz-i. Ig 4 c
PCL Sprain ® MOI: ® Knee is hyperflexed from falling with full weight on the anterior aspect of the bent knee with the foot in plantarflexion. ® S&S: ® A pop in the back of the knee, tenderness and swelling in the popliteal fossa, laxity with Posterior Drawer. ® Treatment: ® RICE, non-operative for G 1 and 2, quad strength. G 3 is controversial.
Meniscus Injuries ® MOI: ® ® ® S&S: ® ® ® Weight bearing combined with rotational force while extending or flexing the knee. Medial meniscus has higher incidence of injury than the lateral meniscus. Effusion over 48 -72 hours, joint-line pain, loss of ROM, locking and giving away, pain with squatting. Chronic lesions have recurrent swelling and muscle atrophy around the knee. Treatment: ® RICE, arthoscopic surgery.
Joint Contusion ® MOI: ® Direct trauma. Especially the vastus medialis. ® S&S: ® May appear to be a knee sprain. ® Severe pain, loss of ROM, and signs of acute inflammation. ® Treatment: ® Compression and ice, and rest for at least 24 hours. ® If swelling and pain are intense, refer to physician. ® Protective padding.
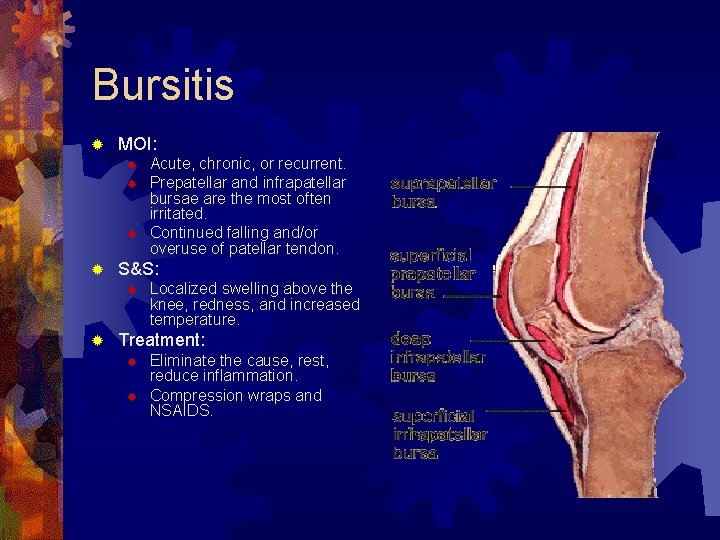
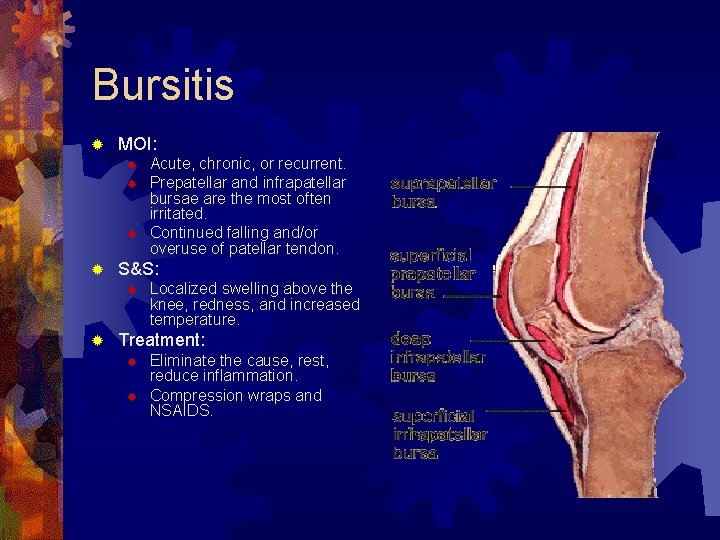
Bursitis ® MOI: ® ® S&S: ® ® Acute, chronic, or recurrent. Prepatellar and infrapatellar bursae are the most often irritated. Continued falling and/or overuse of patellar tendon. Localized swelling above the knee, redness, and increased temperature. Treatment: ® ® Eliminate the cause, rest, reduce inflammation. Compression wraps and NSAIDS.
Iliotibial Band Friction Syndrome ® MOI: ® ® ® S&S: ® ® ® ITBS is an overuse condition commonly occurring in runners or cyclists than can be attributed to malalignment and structural asymmetries of the foot and lower leg. Irritation is over the lateral femoral condyle. Tenderness, mild swelling, increased warmth and redness over the lateral femoral condyle. Pain increases with running or cycling activities. Treatment: ® Stretching, correction of foot/leg alignment problems, ice, decrease irritating activities, NSAIDS, transverse friction massage.
Patellar Fracture & Subluxation/Dislocation ® Patellar Fracture ® ® ® Patellar Subluxation/Dislocation MOI: ® ® ® Plants foot, decelerates, and cuts in the opposite direction from the weight bearing foot, thigh rotates internally and the lower leg rotates externally causing a medially directed valgus force at the knee. Displacement typically takes place laterally. S&S: ® ® Caused by direct or indirect trauma. Complete loss of knee function, pain, swelling, and the patella rests in an abnormal position. Treatment: ® ® Immobilization, ice, refer to physician, immobilized for 4 weeks, muscle rehab, knee sleeve. http: //www. youtube. com/watch? v=XO 6 vty. O 92 tk&feature=related

Jumper’s Knee ® MOI: ® ® S&S: ® ® Jumping, kicking, or running that places tension on the knee extensor muscle complex. May be a single acute injury or a repetitive injury. Patellar or quadriceps tendon. Vague pain and tenderness around the inferior portion of the patella or posterior aspect that worsens with jumping and/or running. Treatment: ® Rest, ice, NSAIDS, brace or strap, transverse friction massage.
Osgood-Schlatter Disease ® MOI: ® ® ® S&S: ® ® Occurs in the rapidly growing immature adolescent’s knee. Repeated pull of the patellar tendon at the tibial tubercle. Bony callus forms. Swelling, hemorrhage, gradual degeneration at the tibial tubercle, severe pain with kneeling, jumping, and running. Treatment: ® Stressful activities are decreased from 6 months to 1 year, padding, ice, isometric strengthening of quadriceps and hamstring muscles.

Osgood-Schlatter Disease
Visual Aids Courtesy of the Following Websites: ® http: //images. medicinenet. com/images/il lustrations/knee_joint. jpg ® http: //www. gla. ac. uk/ibls/fab/tutorial/ana tomy/knee 6. html ® http: //www. alimed. com/resources/comm on/images/products/full/6513_d. jpg ® http: //www. zadeh. co. uk/paediatricorthop aedics/osgood-schlatter_1. jpg