Sports Management ACUTE MANAGEMENT OF SPORTS INJURIES AND















- Slides: 50
Sports Management ACUTE MANAGEMENT OF SPORTS INJURIES, AND EVENT ADMINISTRATION
Objectives Prepare you to act so the athletes can receive appropriate care and treatment in the case of an emergency. The secondary purpose is for the overall event management.
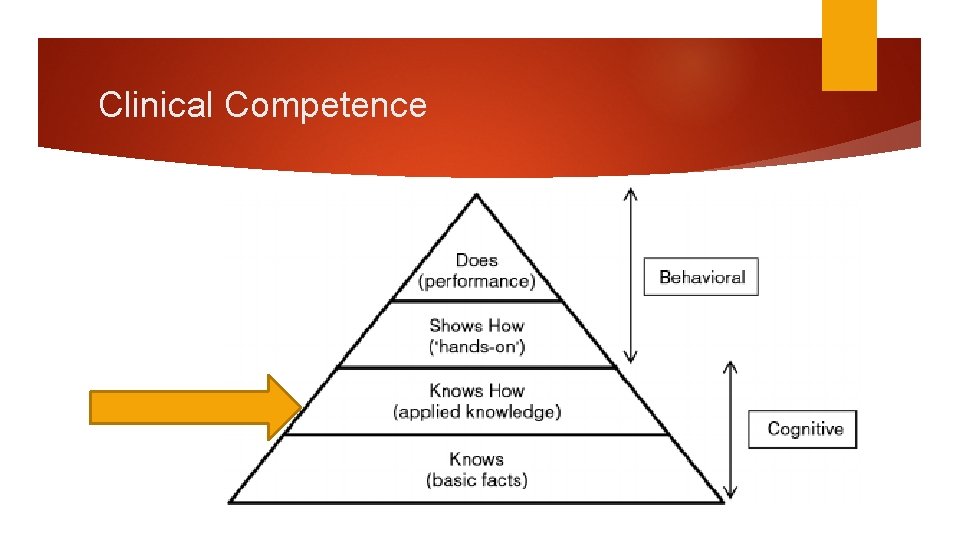
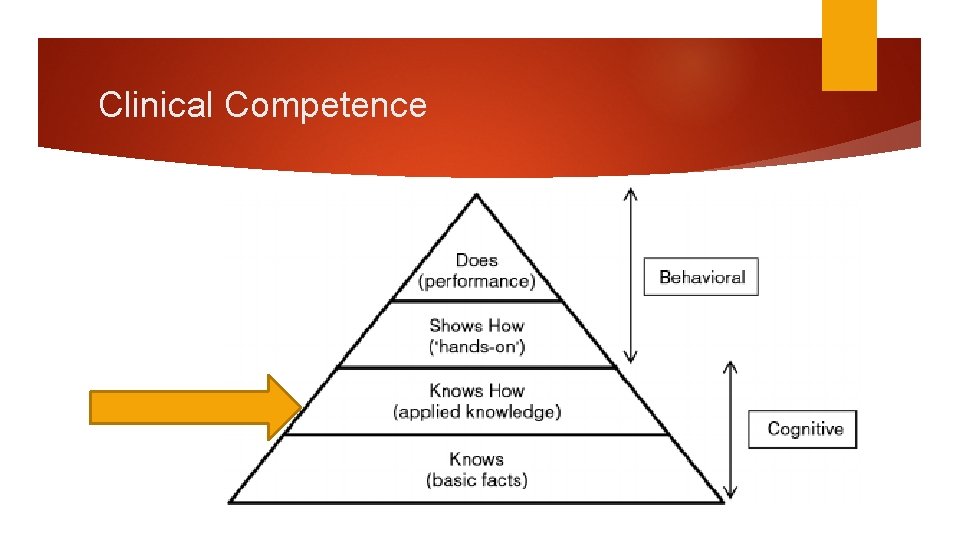
Clinical Competence
“ Before anything else, preparation is the key to success ALEXANDER GRAHAM BELL Understand the Risk ”

~ 8 MILLION ATHLETES IN SECONDARY SCHOOLS ~ 31 MILLION AGE 6 TO 14 PLAY ≥ 1 SPORT Athletes of All Shapes and Sizes ~ 39% OF LIFE-THREATENING INJURIES TO ER WERE SPORT RELATED ADVERSE EVENTS ARE UNDER REPORTED SUDDEN CARDIAC DEATH (SCD) – LEADING CAUSE OF DEATH – HIGH SCHOOL ATHLETES = 1 IN 50, 000 – 80, 000

Prepare Yourself Know your responsibilities Know the resources available Know where to go Know how to communicate Know the sport Know the potential for injury
“ In preparing for battle I have always found that plans are useless, but planning is indispensable DWIGHT D. EISENHOWER Event Management ”
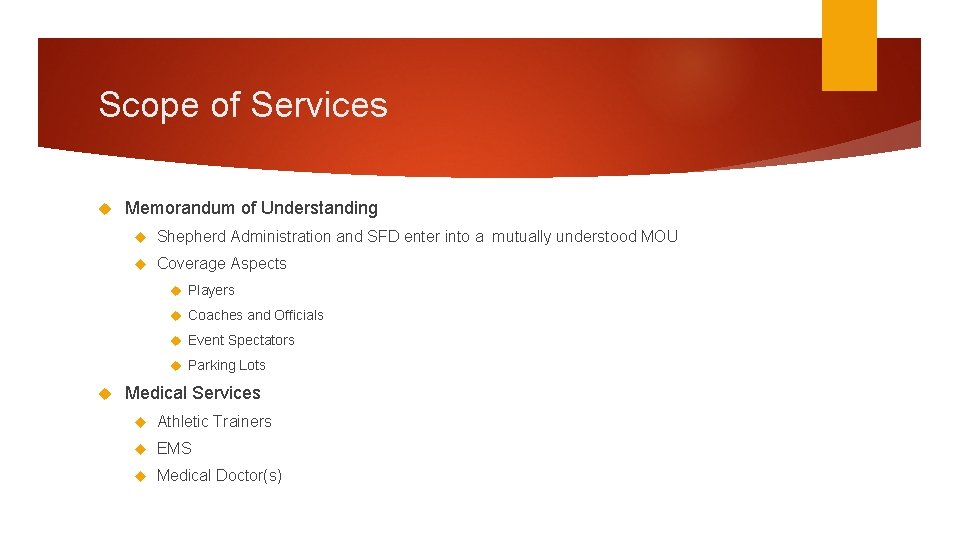
Scope of Services Memorandum of Understanding Shepherd Administration and SFD enter into a mutually understood MOU Coverage Aspects Players Coaches and Officials Event Spectators Parking Lots Medical Services Athletic Trainers EMS Medical Doctor(s)
Event Management Considerations Develop standard operating procedures Develop emergency action plans and treatment protocols Educating Athletes and Coaches Spectators and Parents Other Medical staff Staffing Needs 10% Treatment within 10 minutes (FEMA) 10% of 6, 000 is 600 – How many EMS crews?
Event Management Considerations Inform Applicable Personnel of details (time, location, access) Closest Emergency Facility Shelter in Place Where? What can they handle? Other Fire and EMS Where? What can they handle? How far away is mutual aid? Police Consultation Who’s in charge, when?
Event Management Considerations Chain of Command Unified Command Location Identify Key Personnel Who responds to Unified Command Post Organization Should Begin Early Failing to plan, is planning to fail.
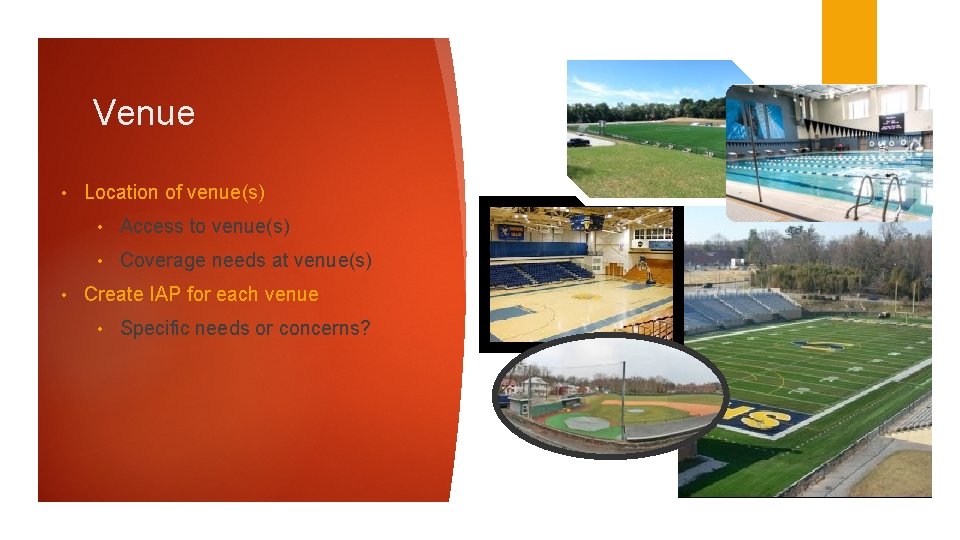
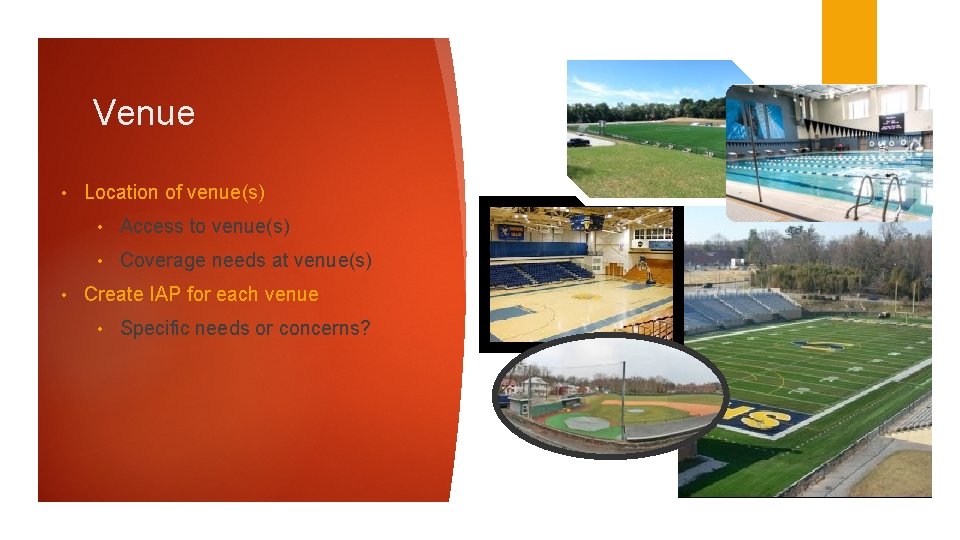
Venue • • Location of venue(s) • Access to venue(s) • Coverage needs at venue(s) Create IAP for each venue • Specific needs or concerns?
Venue Considerations Contained, offer privacy, and protection from the environment Medical tent Tables/chairs Cots Power Heating/cooling Adequate Medical supplies
Venue Considerations Communication: Radio Channel Who’s Listening? Cell phones Wi. Fi Develop a communications plan to direct emergency care Connecting family members to ill or injured participants Family waiting area?
Incident Action Plan Written, Reviewed, Practiced!! Action Plan Should Include Directions to each venue Contact person at venue Detailed map of aid station/first aid locations Note any barriers to response Road closures, locked gates Notification and timing of closures Hospital travel routes Secondary EMS/Fire Support
Incident Action Plan: Plan B?
“ Injuries is a part of a sportsmans life; you have to live with it. RANDY JOHNSON Sports Injuries ”

Where is the injury?

First Response Your priority is to ensure the is athlete safe and stable. Do not immediately move the athlete Determine if the athlete in conscious Assume the worst – every injured player should be approached as having a serious injury until proven otherwise AVPU Check their ABC’s (Airway, Breathing, Circulation)
First Response Take control of the situation – remember spectators! Assess what care the injury may require Be efficient and effective Send somebody for equipment, if necessary If required, start CPR immediately
Professional Response

Levels of Injury Priority Second Priority Third Priority Injuries that pose an immediate threat to life: Urgent injuries that are potential threats to life or limb: Mild limb injuries: Airway obstruction Head injury Small bone fx Cardiac arrest Spinal injury Cuts and Bruises Uncontrolled bleeding Serious limb injuries First Priority Blood vessel / nerve injury Sprain / Strain
Take Control, and Calm the Situation As the Sports Responder, it is your responsibility to calm down the injured athlete Ways to help calm an athlete down: Let the athlete know they are going to be alright and you are going to take care of them Talk slowly, calmly, and at eye level Touch is an effective method to calm an anxious athlete Encourage them to take slow deep breaths Remove unnecessary personnel (i. e. teammates, opponents, or onlookers) Remove them from the field of play, safely and quickly
“ Kindness goes a long way. And a sense of humor. It’s like medicine – very healing. MAX IRONS Treatment of Common Sports Injuries ”
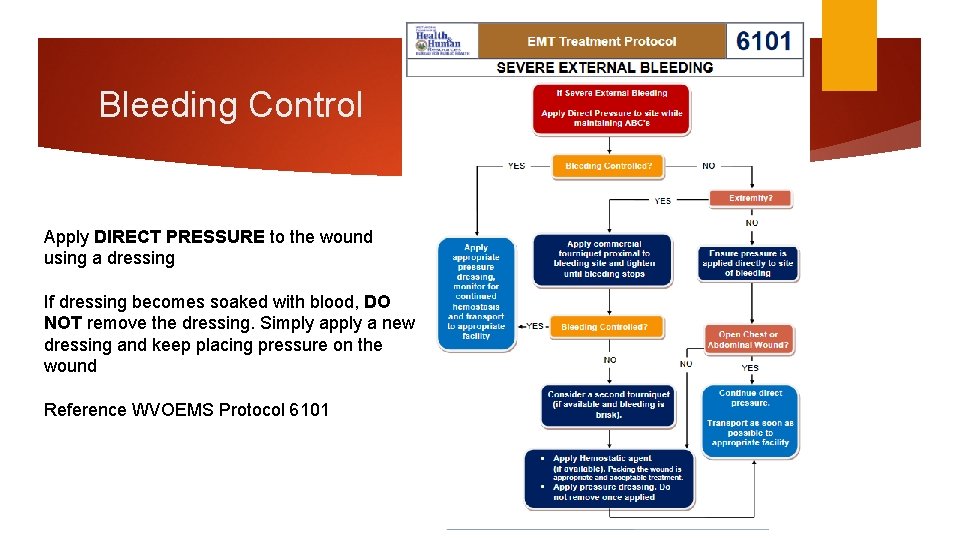
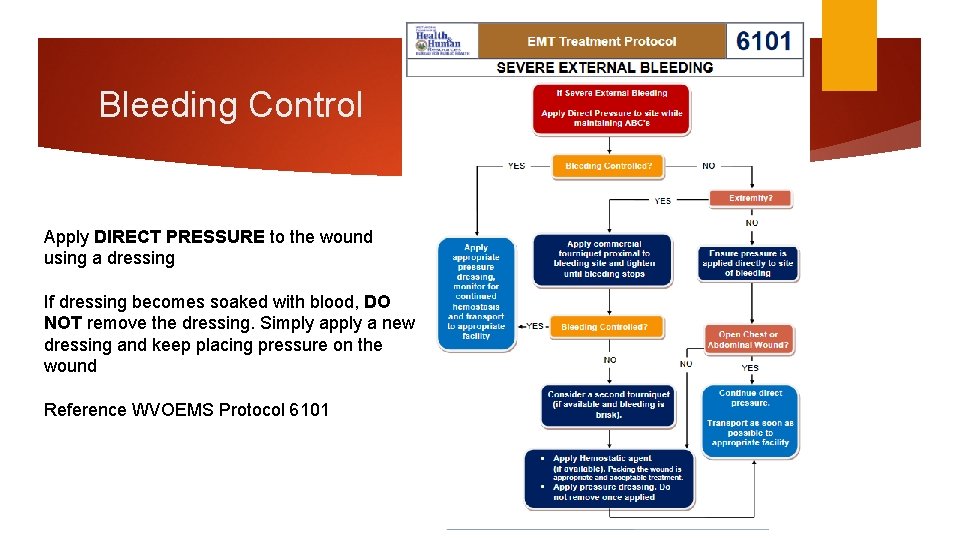
Bleeding Control Apply DIRECT PRESSURE to the wound using a dressing If dressing becomes soaked with blood, DO NOT remove the dressing. Simply apply a new dressing and keep placing pressure on the wound Reference WVOEMS Protocol 6101
Shock is always a possibility, but becomes a major concern with severe injuries Shock is an acute medical condition due to insufficient blood through the circulatory system Signs: Moist, pale, cool and clammy skin Weak and rapid pulse Fast and shallow breathing (hyperventilating)
Managing Shock Maintain body temperature (blankets) Elevate feet 8 -12 inches in most situations “If the face is red, raise the head; If the face is pale, raise the tail” Monitor Vitals (pulse and breathing) Shock can set in with the realization of a serious injury. This is why it is important to keep the athlete calm.

Concussion A brief period of unconsciousness followed by complete recovery Brain is “shaken” in skull All head injuries are potentially serious Injuries may be associated with damage to the brain tissue or blood vessels inside the skull Player should be regularly assessed for signs of deterioration worsening headache, drowsiness, blurred vision West Virginia 2013 legislation on sports concussion return to play requires mandatory removal from contest in all cases of suspected head injury identified by sideline physician, athletic trainer or coach. Return to play guidelines require a 5 day progression after symptom resolution and neuropsychological testing with physician involvement.
Cervical Spine Injury Results from extreme bending of neck with or without compression Every downed player should be treated as having a cervical spine injury until proven otherwise Head and neck stabilization techniques should be employed if a player is unconscious or suspected of having a neck injury (e. g midline neck pain) WVOEMS Protocol 6102
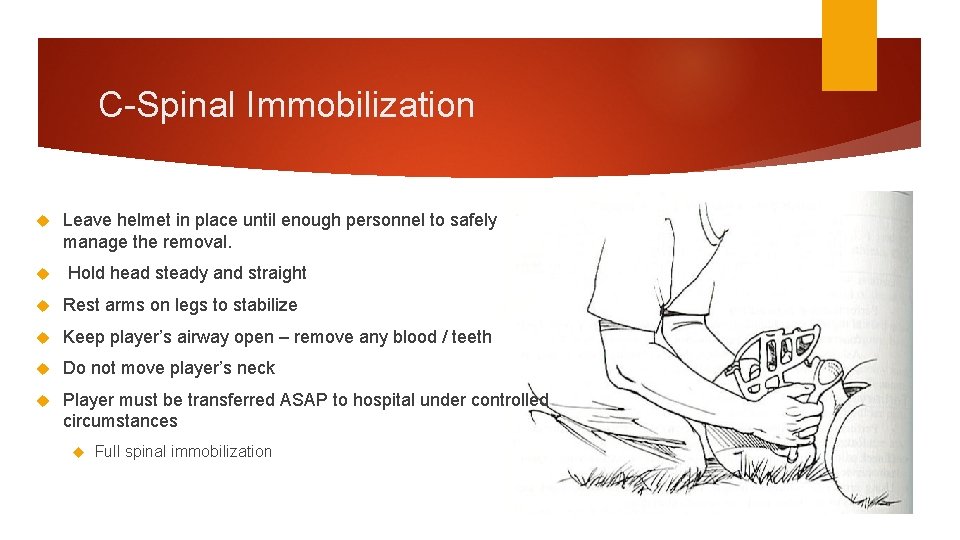
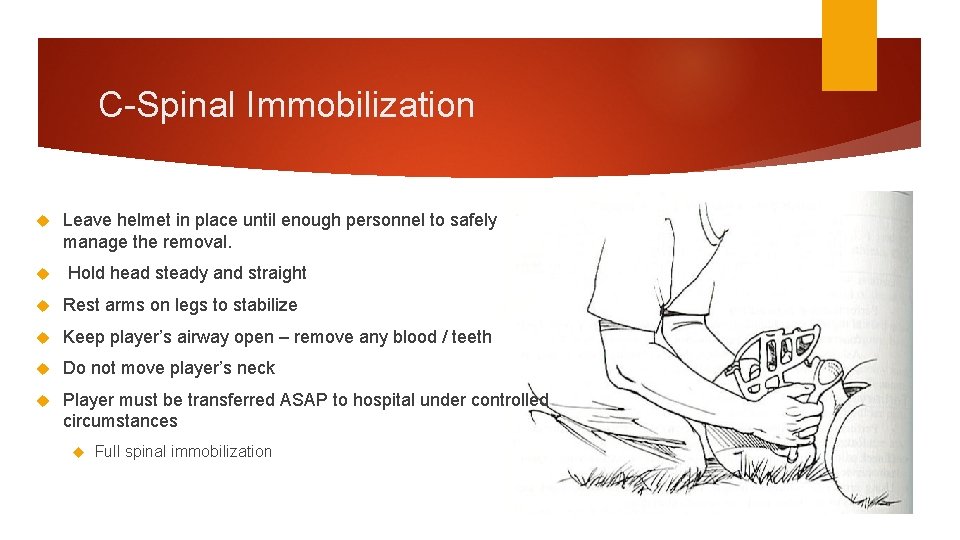
C-Spinal Immobilization Leave helmet in place until enough personnel to safely manage the removal. Hold head steady and straight Rest arms on legs to stabilize Keep player’s airway open – remove any blood / teeth Do not move player’s neck Player must be transferred ASAP to hospital under controlled circumstances Full spinal immobilization


WVOEMS Protocol 6106 TREAT ALL PAINFUL, SWOLLEN, OR DEFORMED AREAS AS FRACTURES.
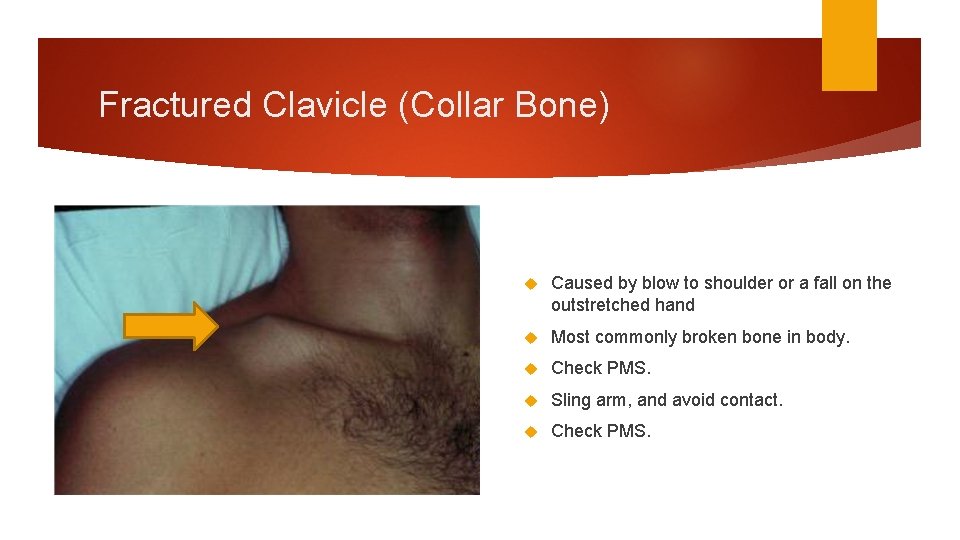
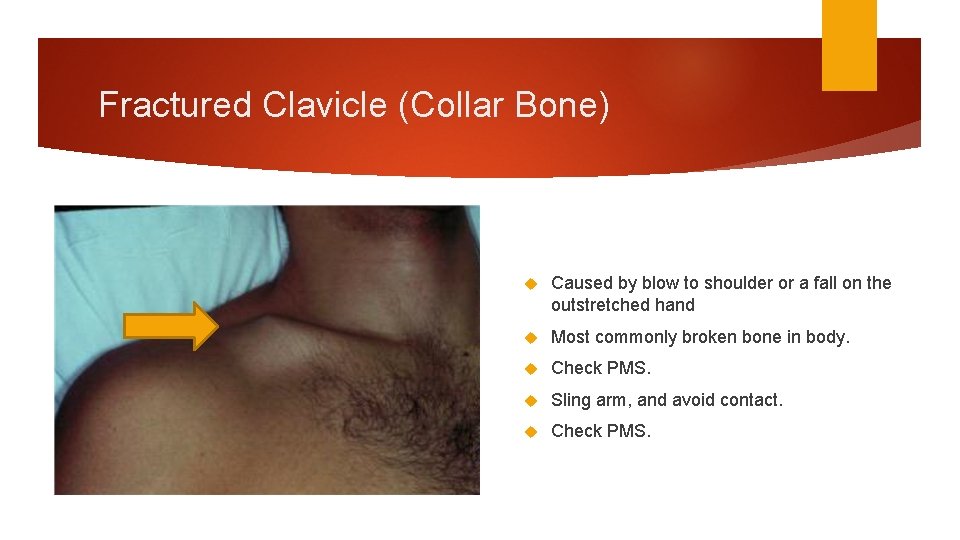
Fractured Clavicle (Collar Bone) Caused by blow to shoulder or a fall on the outstretched hand Most commonly broken bone in body. Check PMS. Sling arm, and avoid contact. Check PMS.

Fractures of Extremities/Hands/Fingers Remove Jewelry Splint Support Cold Injury Site Packs Transport
Ankle Fractures Type of ankle fracture depends on the foot position at time of injury and the direction of force exerted Injury can result from Falling to one side (“going over on ankle”) Twisting injuries Player will complain of Tenderness, swelling and bruising over ankle Deformity of affected ankle
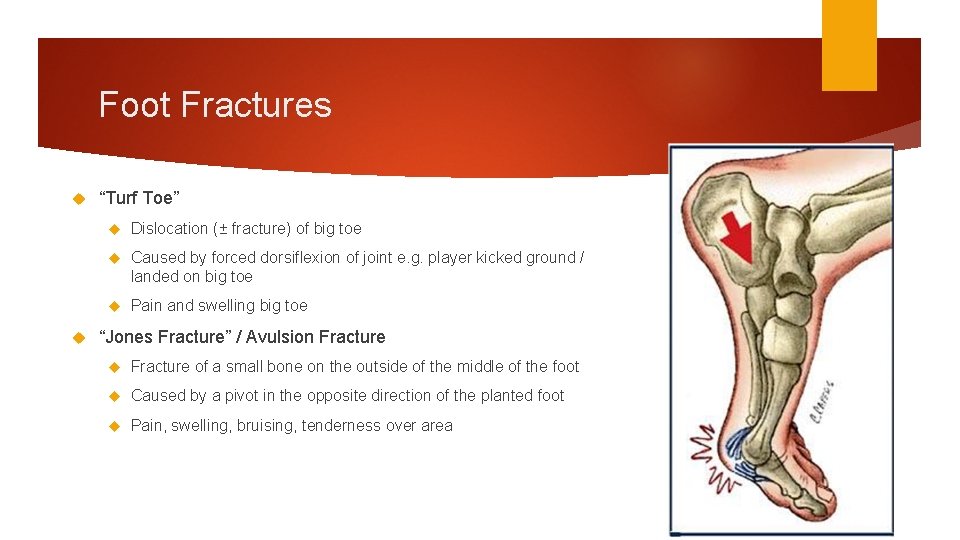
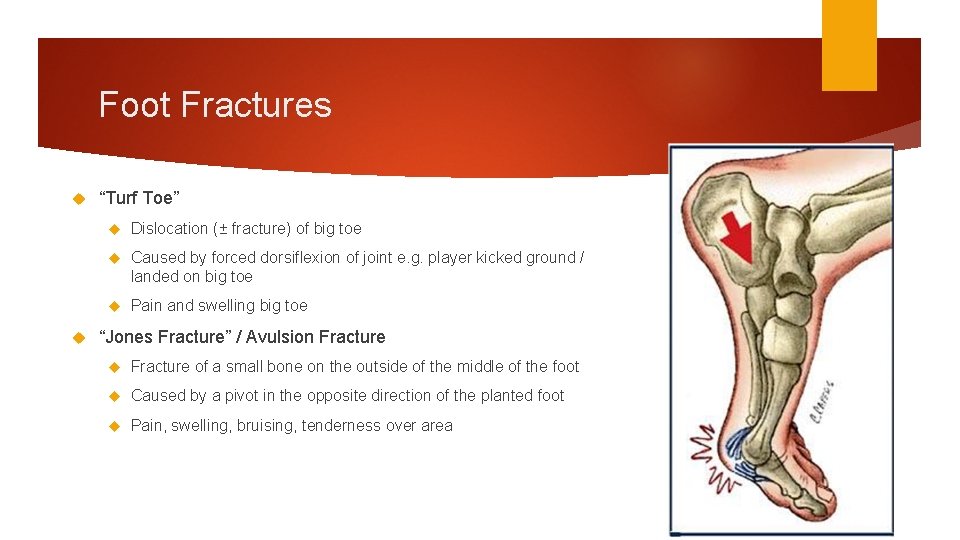
Foot Fractures “Turf Toe” Dislocation (± fracture) of big toe Caused by forced dorsiflexion of joint e. g. player kicked ground / landed on big toe Pain and swelling big toe “Jones Fracture” / Avulsion Fracture of a small bone on the outside of the middle of the foot Caused by a pivot in the opposite direction of the planted foot Pain, swelling, bruising, tenderness over area
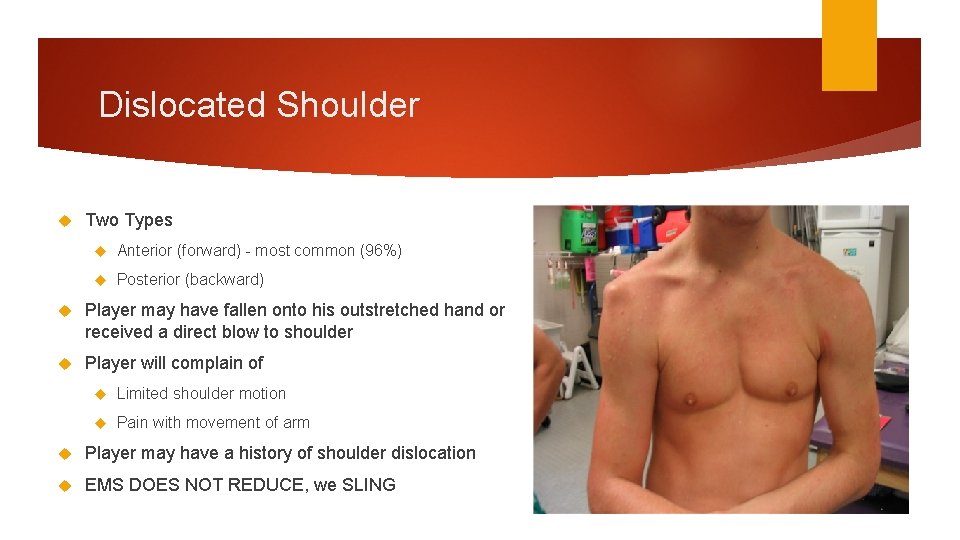
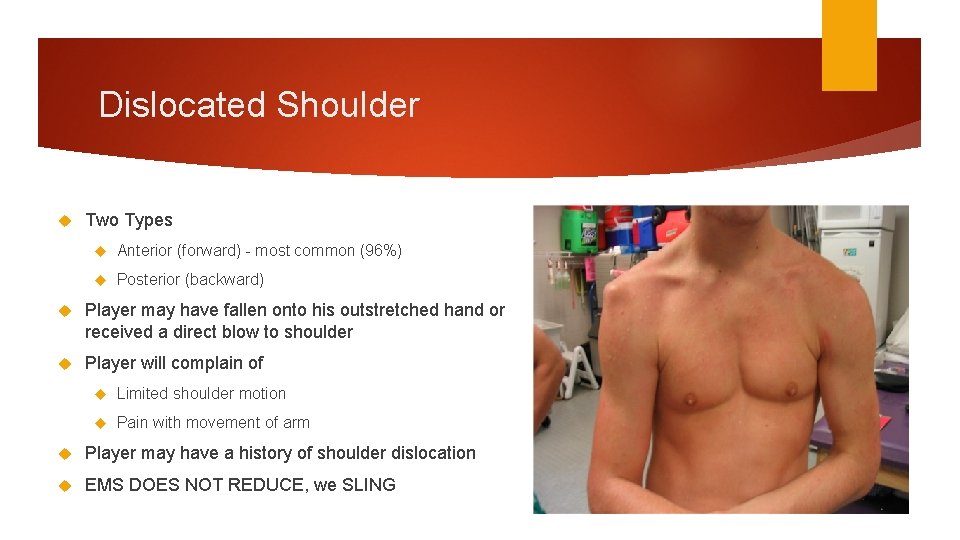
Dislocated Shoulder Two Types Anterior (forward) - most common (96%) Posterior (backward) Player may have fallen onto his outstretched hand or received a direct blow to shoulder Player will complain of Limited shoulder motion Pain with movement of arm Player may have a history of shoulder dislocation EMS DOES NOT REDUCE, we SLING
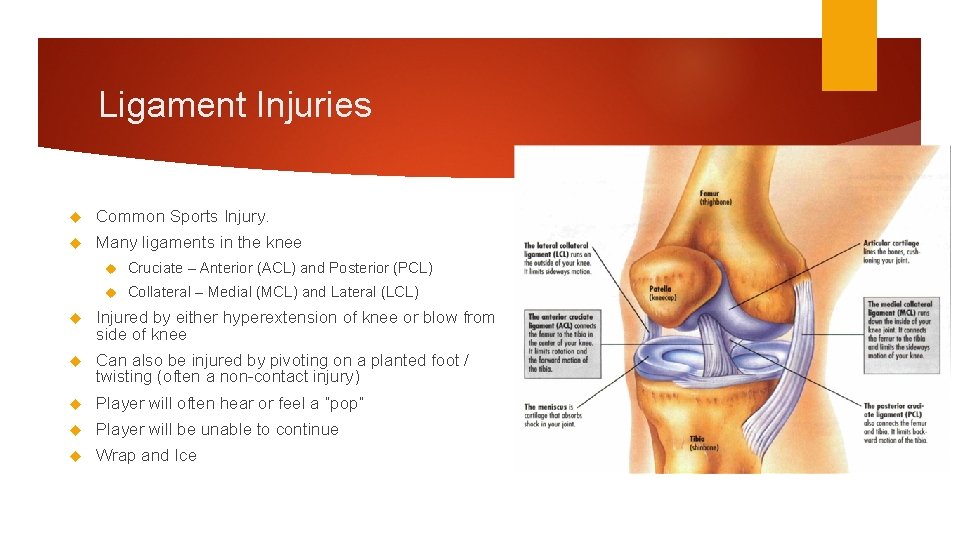
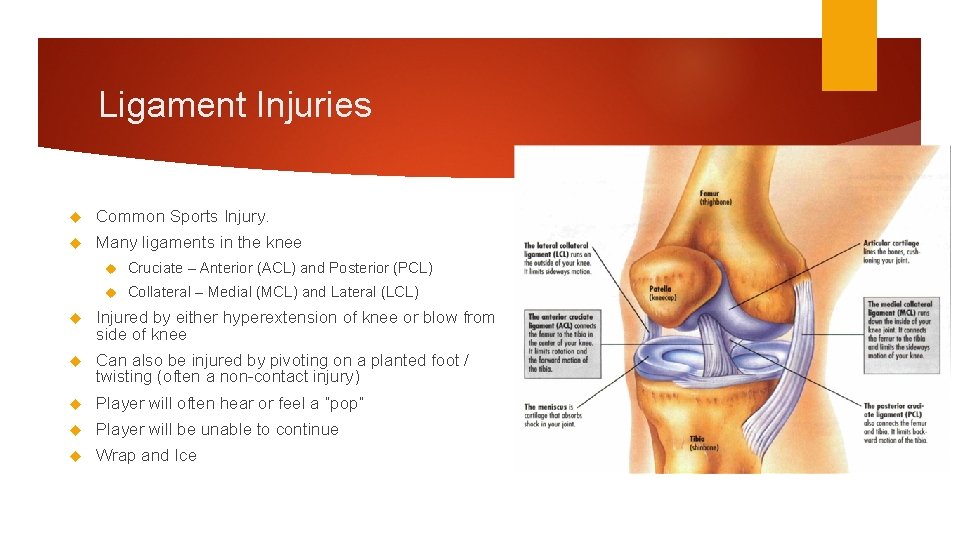
Ligament Injuries Common Sports Injury. Many ligaments in the knee Cruciate – Anterior (ACL) and Posterior (PCL) Collateral – Medial (MCL) and Lateral (LCL) Injured by either hyperextension of knee or blow from side of knee Can also be injured by pivoting on a planted foot / twisting (often a non-contact injury) Player will often hear or feel a “pop” Player will be unable to continue Wrap and Ice


NOT all Sports Injuries are Orthopedics.
Environmental Heat Exposure Remove patient from hot environment and place in cool environment. Loosen or remove clothing. Norm Consciousness, encourage oral fluid intake Cool by fanning Cold Exposure Move to warm environment Remove wet/cold clothing, use blankets Actively warm with heating packs

Other Medical Seizures Protect Airway Request ALS, don’t delay transport Altered Mental Status Possible causes of unconsciousness or altered mental status (AEIOU-TIPS) Glucose Level?


Other Medical Nausea/Vomiting Position of Comfort 12 lead Zofran Hypoglycemia Oral Glucose

Hands On Group 1 Retrieve the dummy with the shoulder pads. Learn the components of pads. Roll onto the backboard Pad the Voids Safely move your patient Group 2 Retrieve the dummy with the football helmet Learn to assess neck for JVD, Trach. Dev. , and any signs. Learn to remove helmet safely and efficiently. Learn the components of the helmet. When all in group have achieved the objectives, switch groups.
 Chapter 11 assessment and evaluation of sports injuries
Chapter 11 assessment and evaluation of sports injuries How are sports injuries classified and managed
How are sports injuries classified and managed Westfield sports injuries
Westfield sports injuries Chapter 13 worksheet recognizing different sports injuries
Chapter 13 worksheet recognizing different sports injuries Sports injuries angus, on
Sports injuries angus, on Both indoor and outdoor sports
Both indoor and outdoor sports Unit 15:9 providing first aid for bone and joint injuries
Unit 15:9 providing first aid for bone and joint injuries A short backboard or vest-style immobilization
A short backboard or vest-style immobilization Chapter 21 caring for head and spine injuries
Chapter 21 caring for head and spine injuries Chapter 15 injuries to muscles and bones
Chapter 15 injuries to muscles and bones Chapter 14:1 using body mechanics
Chapter 14:1 using body mechanics Chapter 14 bleeding shock and soft tissue injuries
Chapter 14 bleeding shock and soft tissue injuries Chapter 13:2 preventing accidents and injuries
Chapter 13:2 preventing accidents and injuries Chapter 12 lesson 2 improving your fitness
Chapter 12 lesson 2 improving your fitness Common track injuries
Common track injuries Acute pancreatitis nursing management
Acute pancreatitis nursing management Neil beidleman
Neil beidleman Hunger games chapter questions
Hunger games chapter questions Strickler spine and sport
Strickler spine and sport Stobhill miu
Stobhill miu Two man carry human crutch
Two man carry human crutch Chapter 17:8 providing first aid for cold exposure
Chapter 17:8 providing first aid for cold exposure Chapter 11 injuries to the shoulder region
Chapter 11 injuries to the shoulder region Kristen wilson injuries
Kristen wilson injuries Pallet jack injuries
Pallet jack injuries The cause-specific mortality rate from roller-skating was:
The cause-specific mortality rate from roller-skating was: Jsp 539
Jsp 539 Climatic injuries
Climatic injuries Chapter 4 preventing injuries through fitness
Chapter 4 preventing injuries through fitness Chapter 4 basics of tissue injuries
Chapter 4 basics of tissue injuries Bo taoshi injuries
Bo taoshi injuries Miniscus injuries
Miniscus injuries Preventing hand injuries
Preventing hand injuries Intentional injury
Intentional injury Moulage recipes
Moulage recipes Define intentional fallacy
Define intentional fallacy Injury prevention safety and first aid
Injury prevention safety and first aid Pa wc bureau
Pa wc bureau Injuries first aid
Injuries first aid Characters of firearm injuries
Characters of firearm injuries Which osha document summarizes occupational injuries
Which osha document summarizes occupational injuries Biomechanics throwing football
Biomechanics throwing football What does atticus ask mayella
What does atticus ask mayella What does haymitch send katniss in chapter 14
What does haymitch send katniss in chapter 14 Chop saw injuries
Chop saw injuries Deadly dozen chest injuries
Deadly dozen chest injuries Carl clinton construction
Carl clinton construction 5 cardinal signs of inflammation
5 cardinal signs of inflammation Classify the following triangle as acute obtuse or right
Classify the following triangle as acute obtuse or right Vascular and cellular events of acute inflammation
Vascular and cellular events of acute inflammation 18 common chronic and acute conditions
18 common chronic and acute conditions