Spine Oncology Required Reading for the Neuroradiologist Wende

![Location (L 4) = Mobile [2] Osseous character = Lytic [2] Alignment = Normal Location (L 4) = Mobile [2] Osseous character = Lytic [2] Alignment = Normal](https://slidetodoc.com/presentation_image_h/ac8edf6e11abd6a9a1a2b7be32911236/image-20.jpg)
![T 9 Lesion: Location (T 9) = Semi-rigid [1] Osseous character = lytic [2] T 9 Lesion: Location (T 9) = Semi-rigid [1] Osseous character = lytic [2]](https://slidetodoc.com/presentation_image_h/ac8edf6e11abd6a9a1a2b7be32911236/image-22.jpg)
- Slides: 31
Spine Oncology: Required Reading for the Neuroradiologist Wende N Gibbs, MD, Paul E Kim, MD, and Meng Law, MBBS, FRACR Department of Neuroradiology University of Southern California, Keck School of Medicine # 1968
Disclosures of Commercial Interest • None of the authors or their immediate family members have a financial relationship with a commercial organization that may have a direct or indirect interest in the content of this presentation
Objectives 1. Provide a comprehensive overview of the current multidisciplinary treatment options for osseous spinal metastatic disease 2. Describe the NOMS paradigm: an important new decision-making tool that is used by spine surgeons and oncologists to provide optimized, individualized treatment 3. Detail specific classification systems utilized in NOMS, with emphasis on information that neuroradiologists should provide the multidisciplinary treatment team 4. Discuss the emerging role that radiologists play in treatment of select patients with spine metastases
Introduction • 1. 6 million new cancer cases per year in the US 1 • Osseous spinal metastases occur in up to 40% of cancer patients 2 • Advances in spine oncology – new technologies and therapeutic options - have increased patient survival • Radiologists play a vital role in patient management, providing data used in decision-making and in some cases, minimally invasive treatments
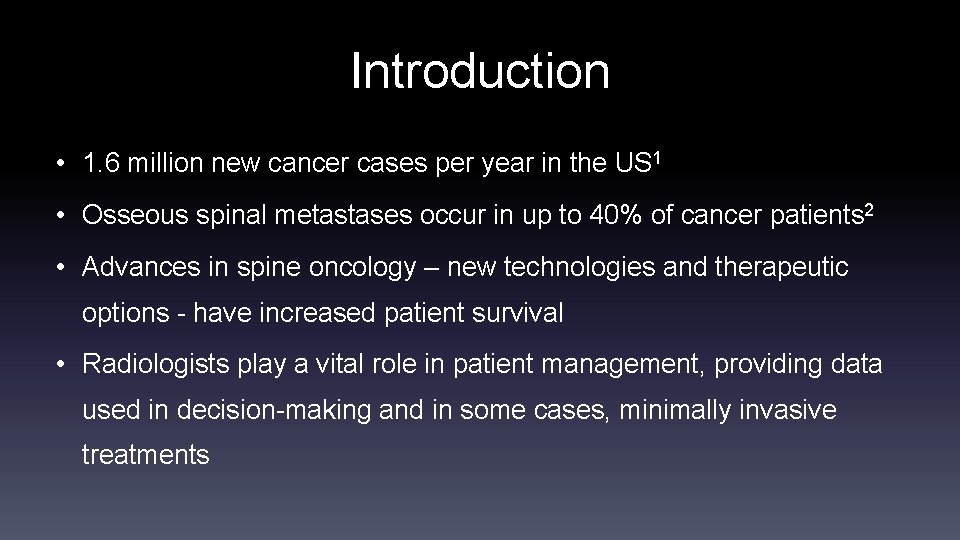
Spinal Metastases: Treatment • Spinal metastases have a significant impact on quality of life, as a result of disabling pain, fracture, or paralysis secondary to cord compression • Treatment goals include: – Effective pain palliation – Maintenance or recovery of neurological function and ambulation – Local durable pain control – Spinal stability – Improved quality of life 52 -year-old man with metastatic lung cancer producing spinal cord compression
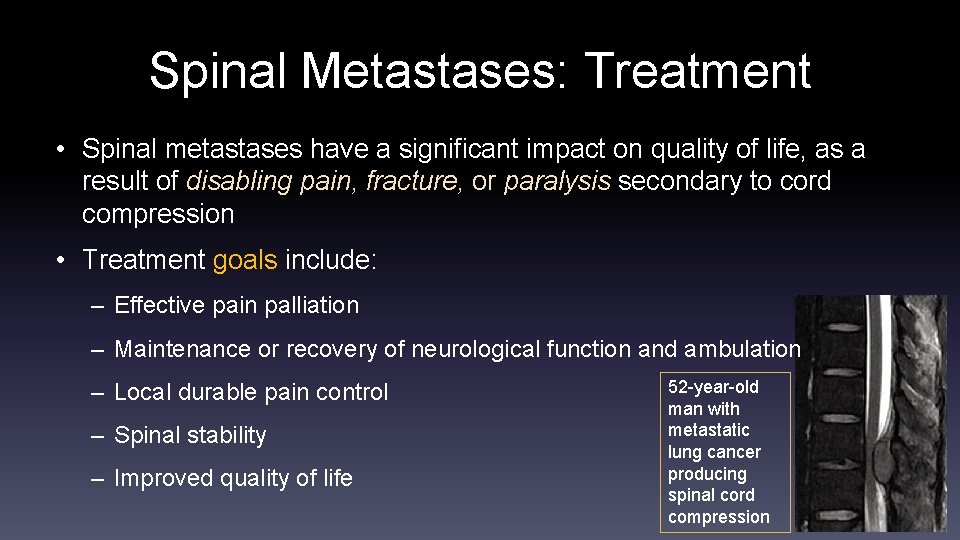
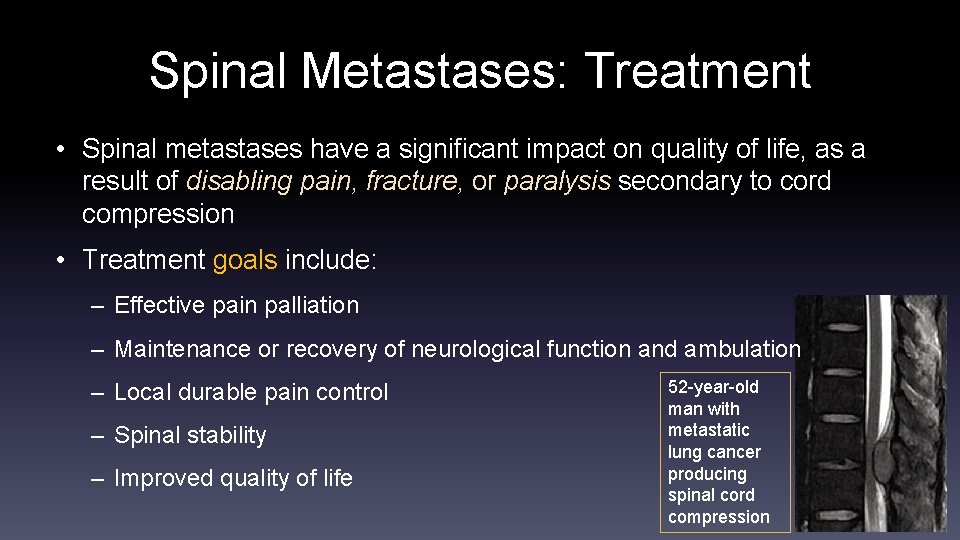
Spinal Metastases: Treatment • Treatment decisions are based upon the individual patient’s symptoms, tumor type, and comorbidities • Treatment options include: – Surgery* – Radiation* – Chemotherapy – Immunotherapy – Radionuclides – Hormonal therapy *Surgery and radiation are presently the most effective treatments for spinal metastases 55 -year-old man with metastatic renal cell carcinoma. L 4 pathologic fracture was treated with surgical resection and stabilization followed by radiation therapy.
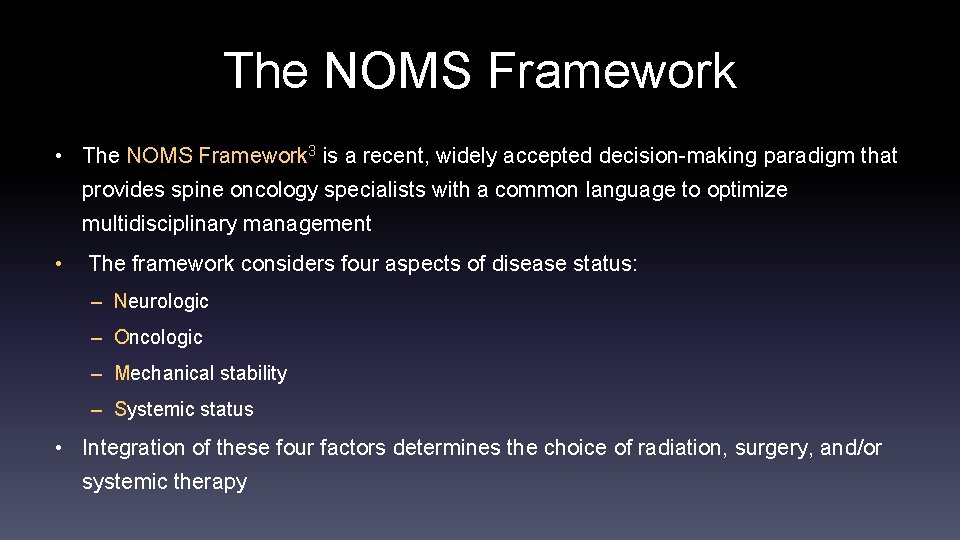
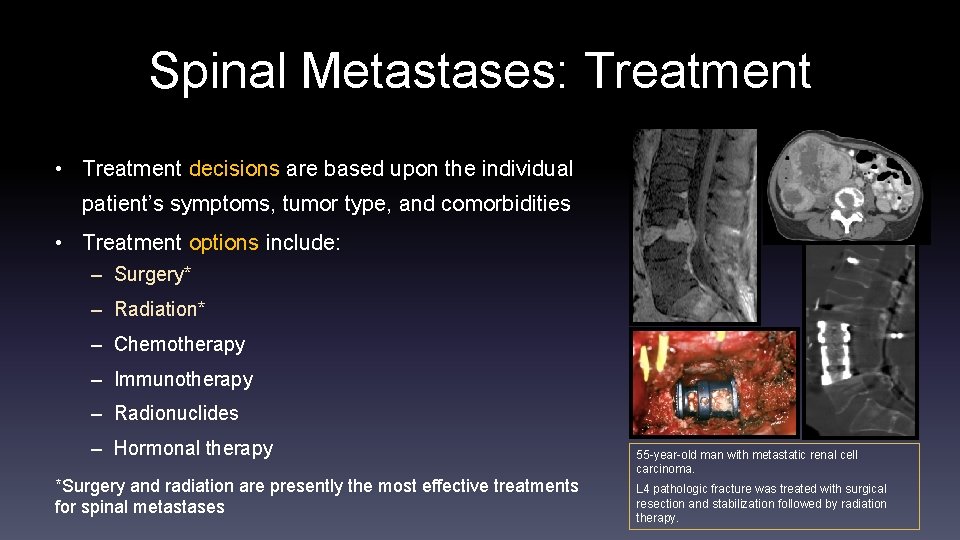
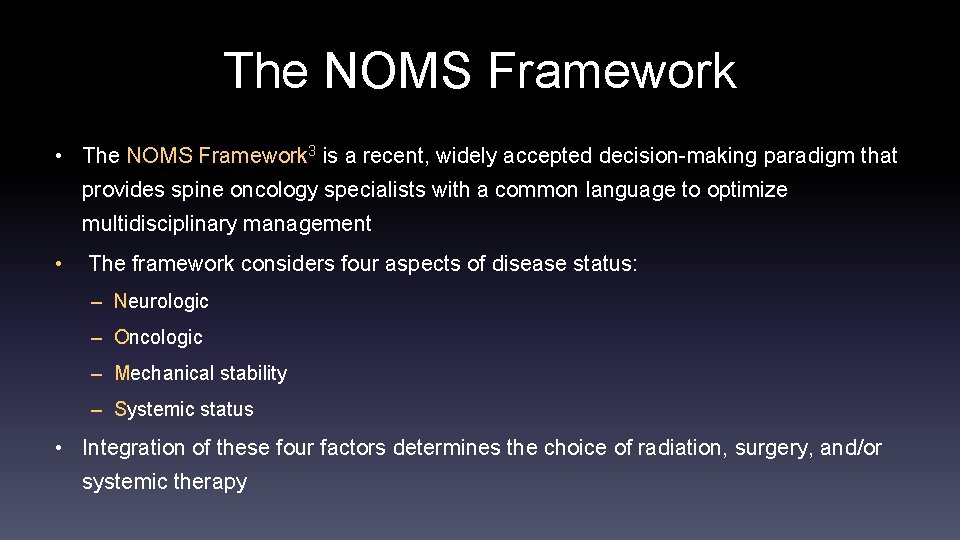
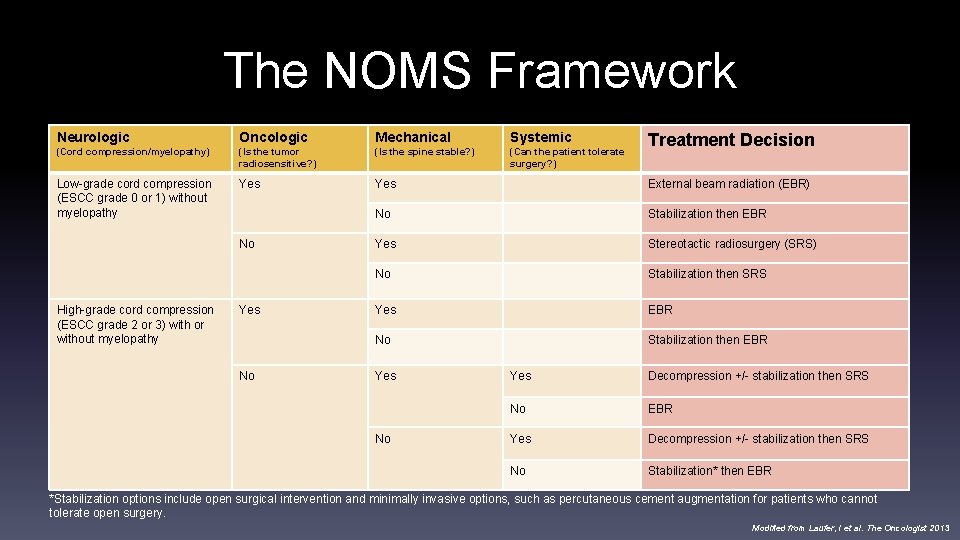
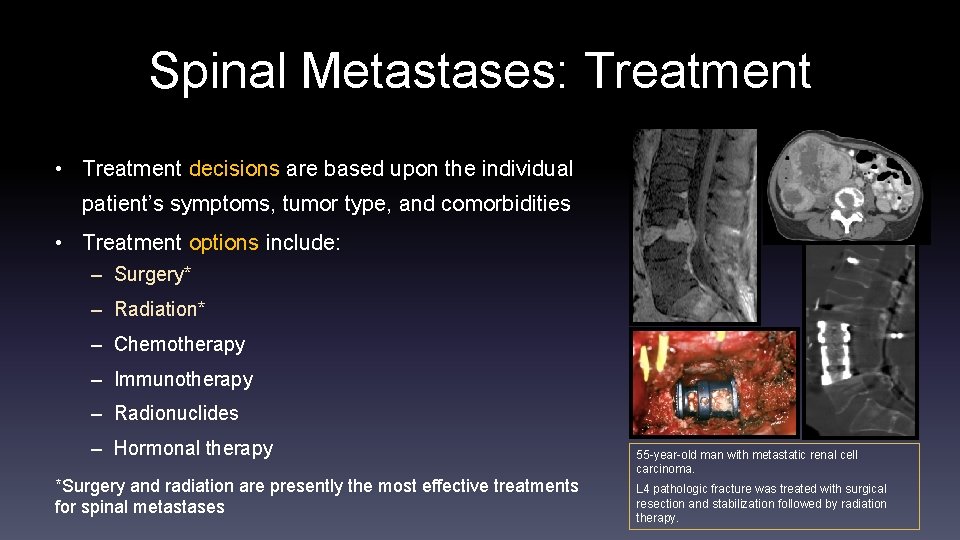
The NOMS Framework • The NOMS Framework 3 is a recent, widely accepted decision-making paradigm that provides spine oncology specialists with a common language to optimize multidisciplinary management • The framework considers four aspects of disease status: – Neurologic – Oncologic – Mechanical stability – Systemic status • Integration of these four factors determines the choice of radiation, surgery, and/or systemic therapy
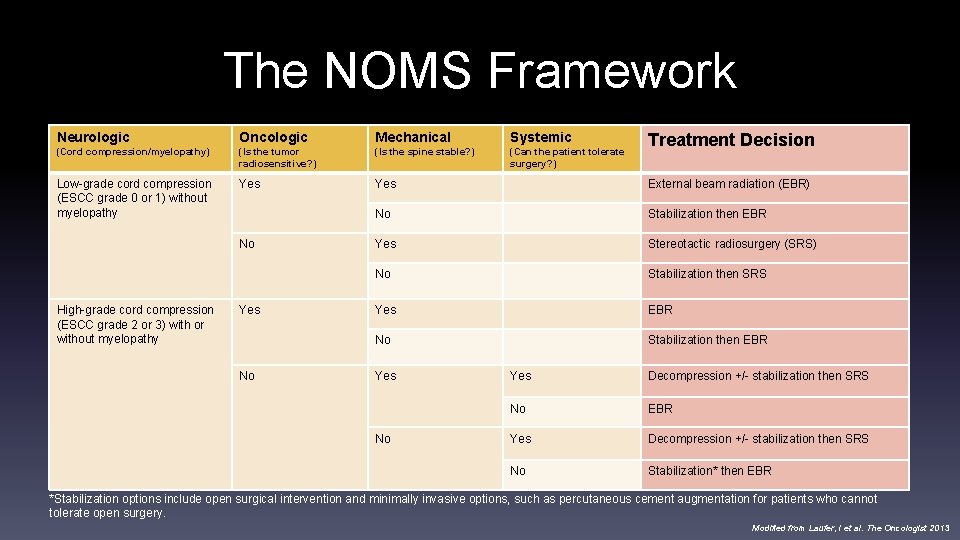
The NOMS Framework Neurologic Oncologic Mechanical Systemic (Cord compression/myelopathy) (Is the tumor radiosensitive? ) (Is the spine stable? ) (Can the patient tolerate surgery? ) Low-grade cord compression (ESCC grade 0 or 1) without myelopathy Yes External beam radiation (EBR) No Stabilization then EBR Yes Stereotactic radiosurgery (SRS) No Stabilization then SRS Yes EBR No Stabilization then EBR No High-grade cord compression (ESCC grade 2 or 3) with or without myelopathy Yes No Treatment Decision Yes Decompression +/- stabilization then SRS No EBR Yes Decompression +/- stabilization then SRS No Stabilization* then EBR *Stabilization options include open surgical intervention and minimally invasive options, such as percutaneous cement augmentation for patients who cannot tolerate open surgery. Modified from Laufer, I et al. The Oncologist 2013
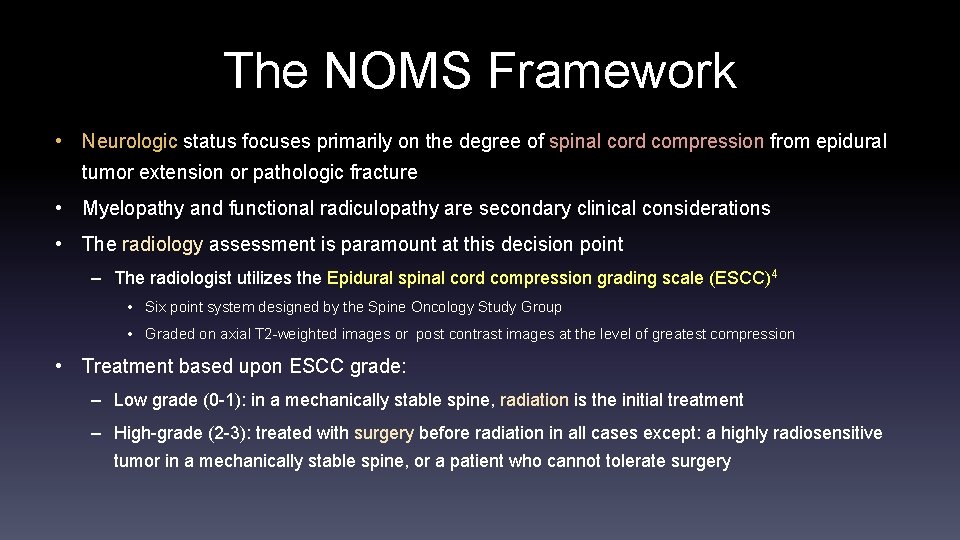
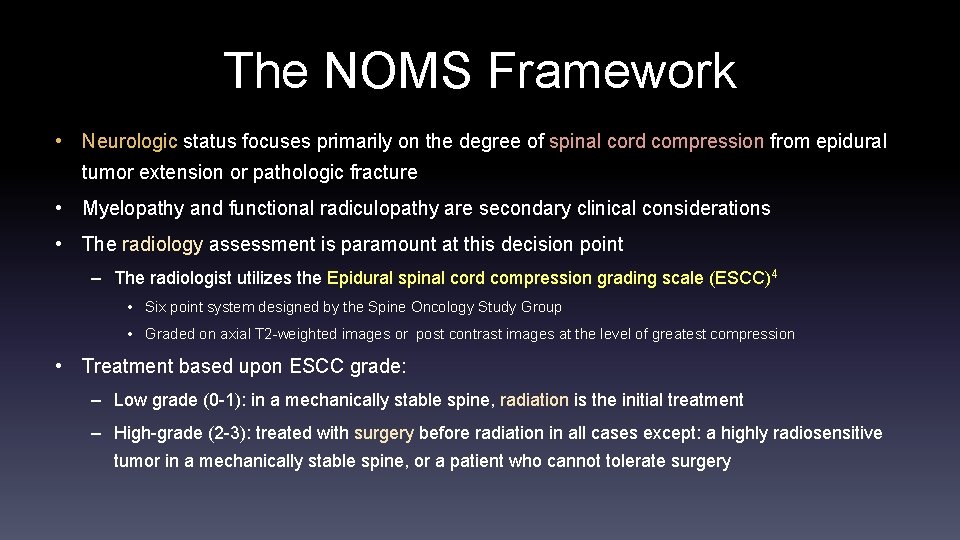
The NOMS Framework • Neurologic status focuses primarily on the degree of spinal cord compression from epidural tumor extension or pathologic fracture • Myelopathy and functional radiculopathy are secondary clinical considerations • The radiology assessment is paramount at this decision point – The radiologist utilizes the Epidural spinal cord compression grading scale (ESCC)4 • Six point system designed by the Spine Oncology Study Group • Graded on axial T 2 -weighted images or post contrast images at the level of greatest compression • Treatment based upon ESCC grade: – Low grade (0 -1): in a mechanically stable spine, radiation is the initial treatment – High-grade (2 -3): treated with surgery before radiation in all cases except: a highly radiosensitive tumor in a mechanically stable spine, or a patient who cannot tolerate surgery
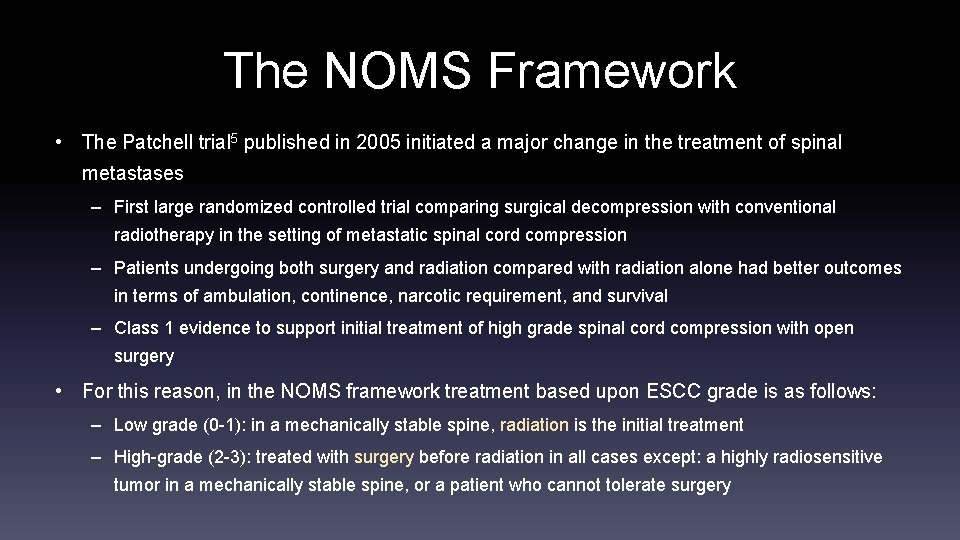
The NOMS Framework • The Patchell trial 5 published in 2005 initiated a major change in the treatment of spinal metastases – First large randomized controlled trial comparing surgical decompression with conventional radiotherapy in the setting of metastatic spinal cord compression – Patients undergoing both surgery and radiation compared with radiation alone had better outcomes in terms of ambulation, continence, narcotic requirement, and survival – Class 1 evidence to support initial treatment of high grade spinal cord compression with open surgery • For this reason, in the NOMS framework treatment based upon ESCC grade is as follows: – Low grade (0 -1): in a mechanically stable spine, radiation is the initial treatment – High-grade (2 -3): treated with surgery before radiation in all cases except: a highly radiosensitive tumor in a mechanically stable spine, or a patient who cannot tolerate surgery
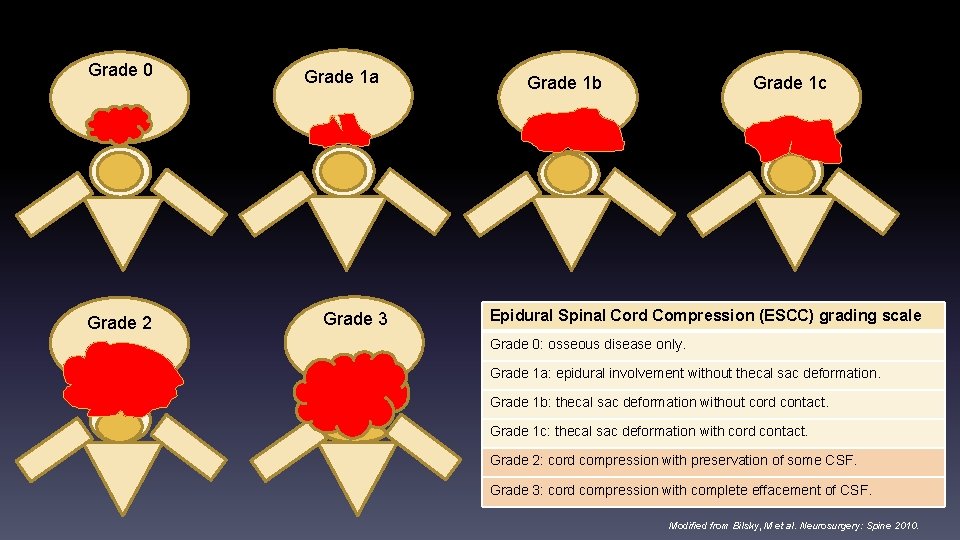
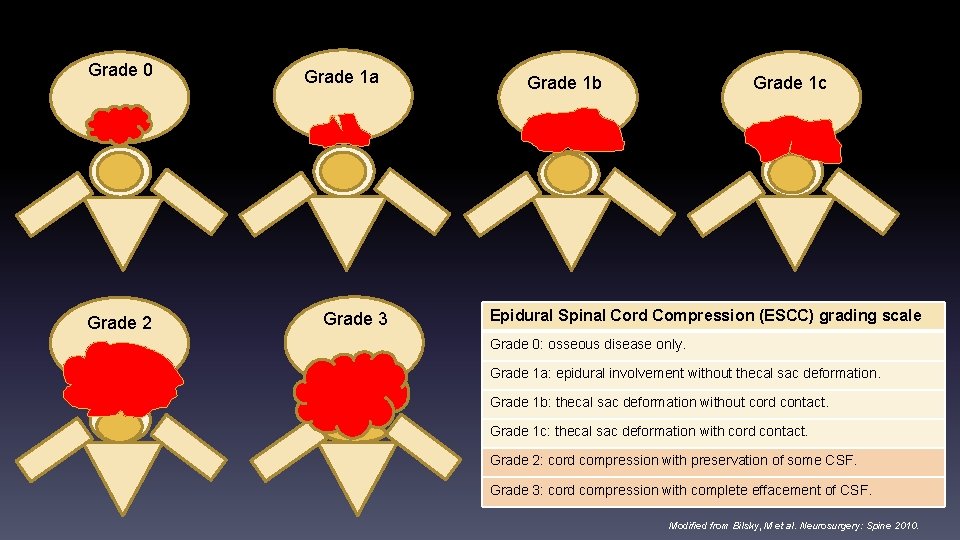
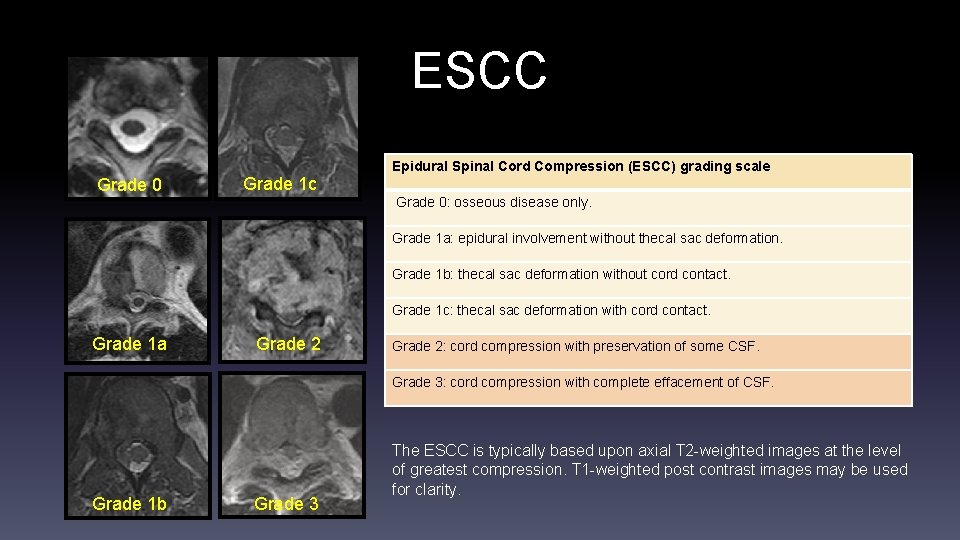
Grade 0 Grade 2 Grade 1 a Grade 3 Grade 1 c Grade 1 b Epidural Spinal Cord Compression (ESCC) grading scale Grade 0: osseous disease only. Grade 1 a: epidural involvement without thecal sac deformation. Grade 1 b: thecal sac deformation without cord contact. Grade 1 c: thecal sac deformation with cord contact. Grade 2: cord compression with preservation of some CSF. Grade 3: cord compression with complete effacement of CSF. Modified from Bilsky, M et al. Neurosurgery: Spine 2010.
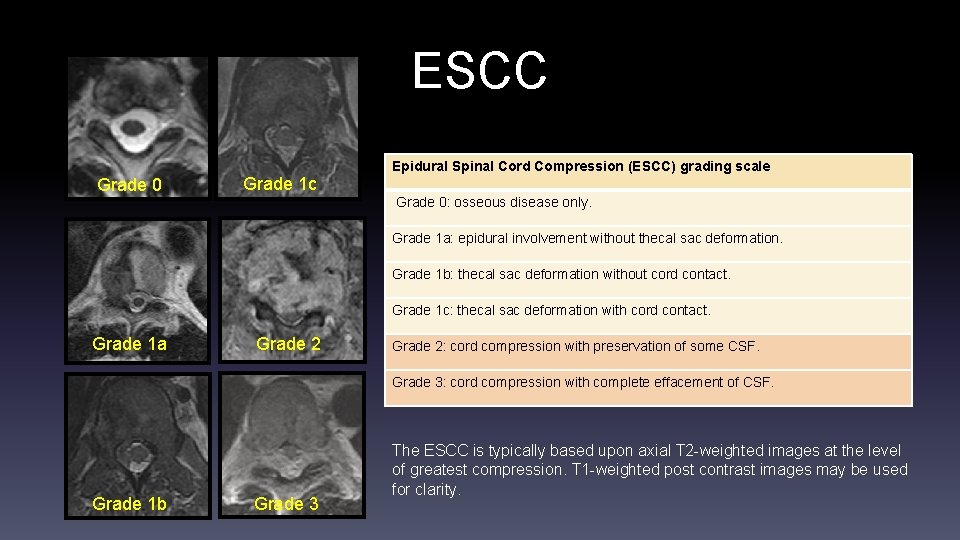
ESCC Grade 0 Grade 1 c Epidural Spinal Cord Compression (ESCC) grading scale Grade 0: osseous disease only. Grade 1 a: epidural involvement without thecal sac deformation. Grade 1 b: thecal sac deformation without cord contact. Grade 1 c: thecal sac deformation with cord contact. Grade 1 a Grade 2: cord compression with preservation of some CSF. Grade 3: cord compression with complete effacement of CSF. Grade 1 b Grade 3 The ESCC is typically based upon axial T 2 -weighted images at the level of greatest compression. T 1 -weighted post contrast images may be used for clarity.
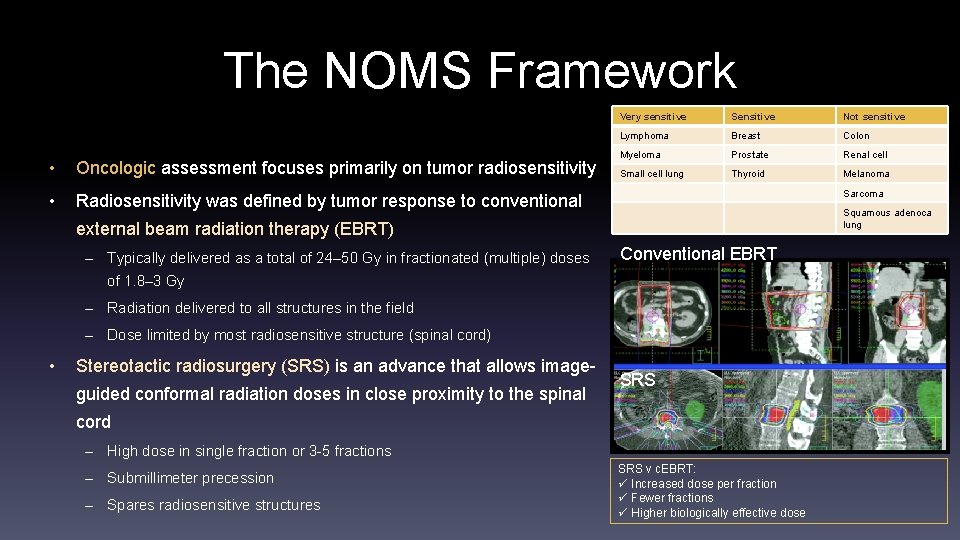
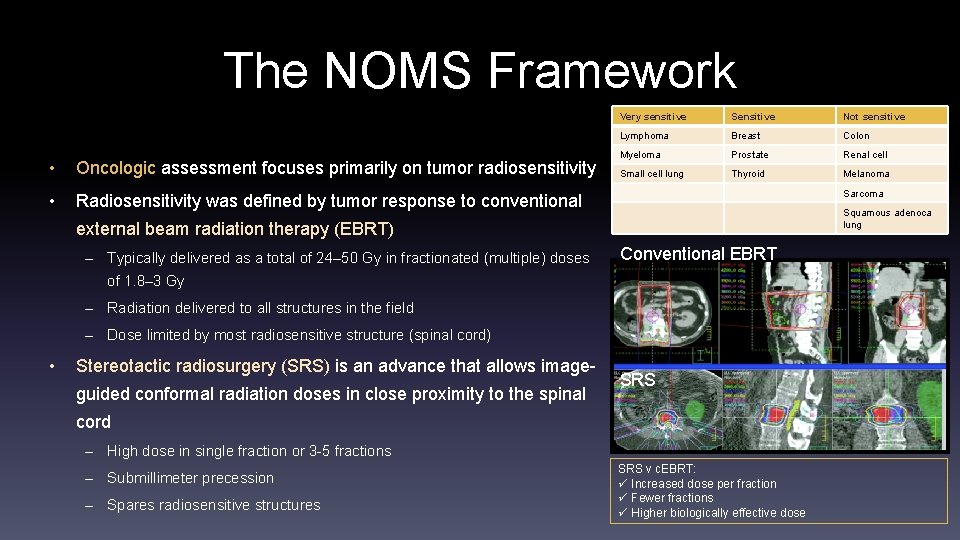
The NOMS Framework • Oncologic assessment focuses primarily on tumor radiosensitivity • Radiosensitivity was defined by tumor response to conventional Very sensitive Sensitive Not sensitive Lymphoma Breast Colon Myeloma Prostate Renal cell Small cell lung Thyroid Melanoma Sarcoma Squamous adenoca lung external beam radiation therapy (EBRT) – Typically delivered as a total of 24– 50 Gy in fractionated (multiple) doses Conventional EBRT of 1. 8– 3 Gy – Radiation delivered to all structures in the field – Dose limited by most radiosensitive structure (spinal cord) • Stereotactic radiosurgery (SRS) is an advance that allows imageguided conformal radiation doses in close proximity to the spinal SRS cord – High dose in single fraction or 3 -5 fractions – Submillimeter precession – Spares radiosensitive structures SRS v c. EBRT: ü Increased dose per fraction ü Fewer fractions ü Higher biologically effective dose
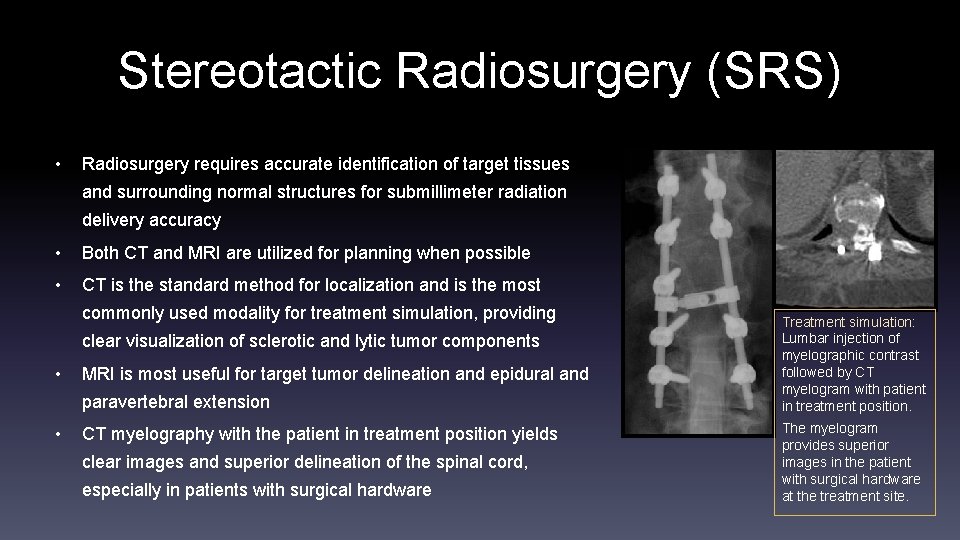
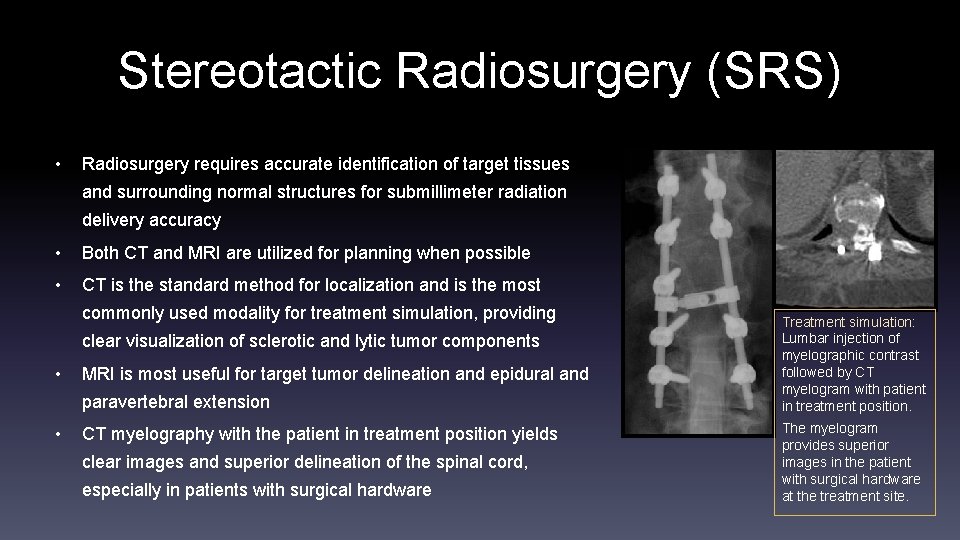
Stereotactic Radiosurgery (SRS) • Radiosurgery requires accurate identification of target tissues and surrounding normal structures for submillimeter radiation delivery accuracy • Both CT and MRI are utilized for planning when possible • CT is the standard method for localization and is the most commonly used modality for treatment simulation, providing clear visualization of sclerotic and lytic tumor components • MRI is most useful for target tumor delineation and epidural and paravertebral extension • CT myelography with the patient in treatment position yields clear images and superior delineation of the spinal cord, especially in patients with surgical hardware Treatment simulation: Lumbar injection of myelographic contrast followed by CT myelogram with patient in treatment position. The myelogram provides superior images in the patient with surgical hardware at the treatment site.
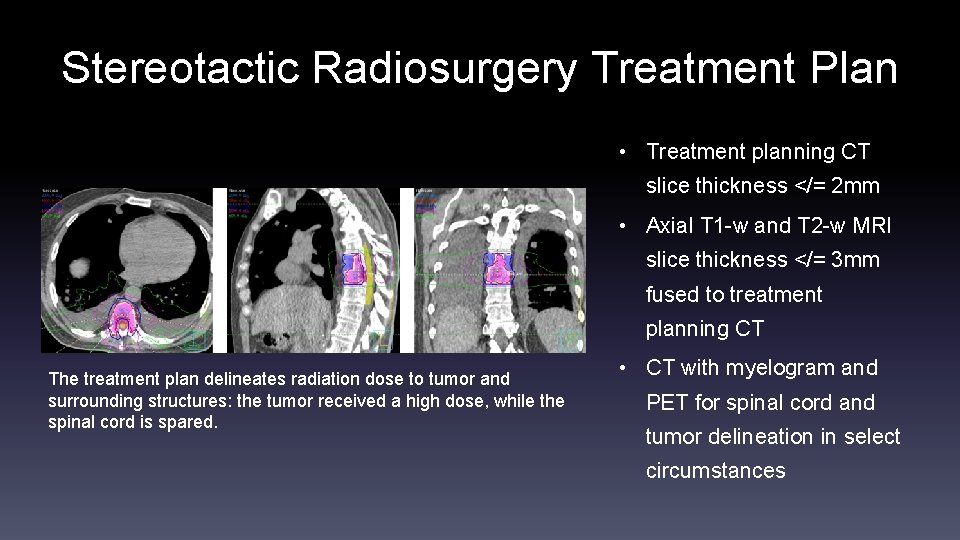
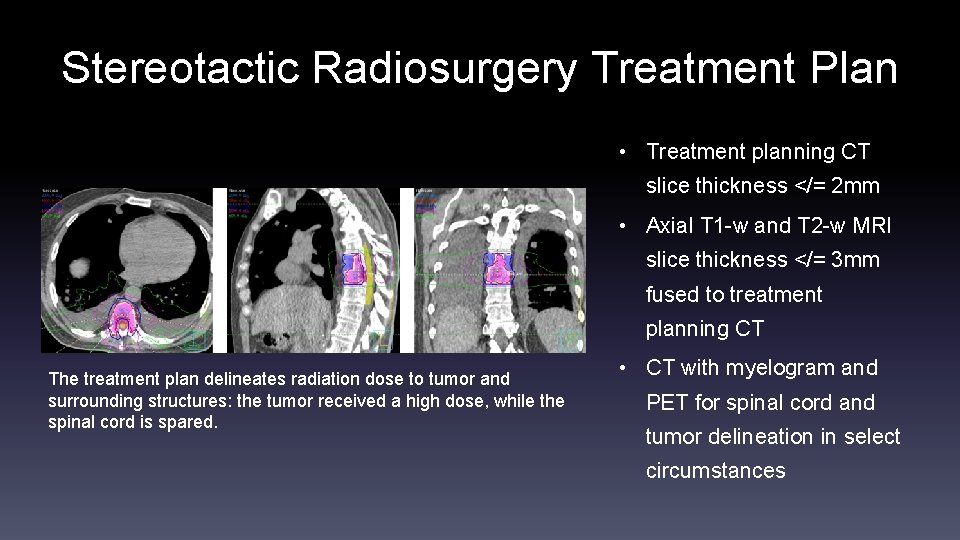
Stereotactic Radiosurgery Treatment Plan • Treatment planning CT slice thickness </= 2 mm • Axial T 1 -w and T 2 -w MRI slice thickness </= 3 mm fused to treatment planning CT The treatment plan delineates radiation dose to tumor and surrounding structures: the tumor received a high dose, while the spinal cord is spared. • CT with myelogram and PET for spinal cord and tumor delineation in select circumstances
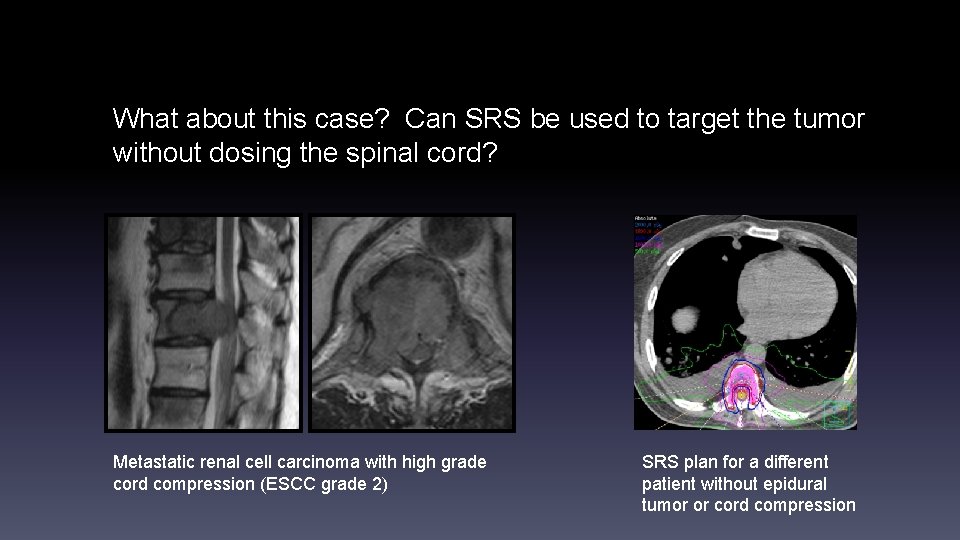
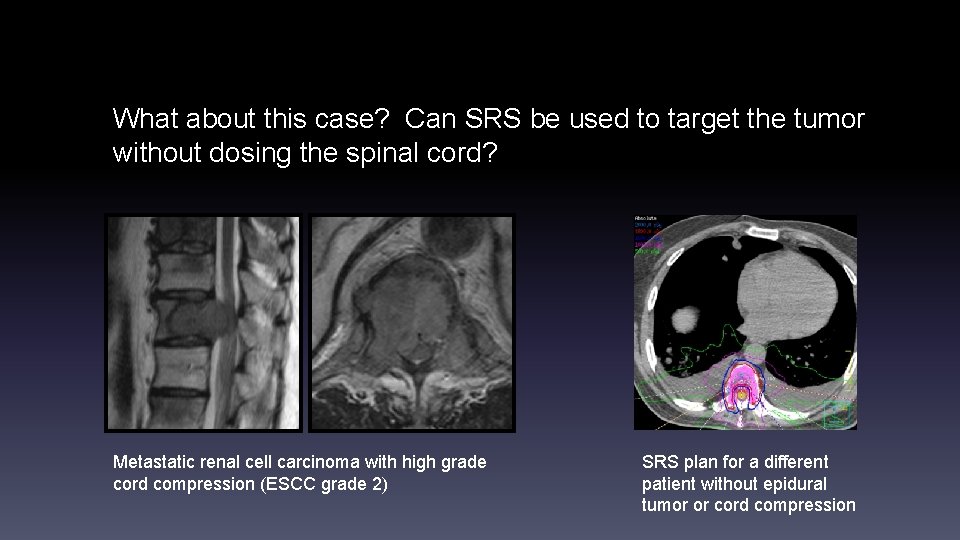
What about this case? Can SRS be used to target the tumor without dosing the spinal cord? Metastatic renal cell carcinoma with high grade cord compression (ESCC grade 2) SRS plan for a different patient without epidural tumor or cord compression
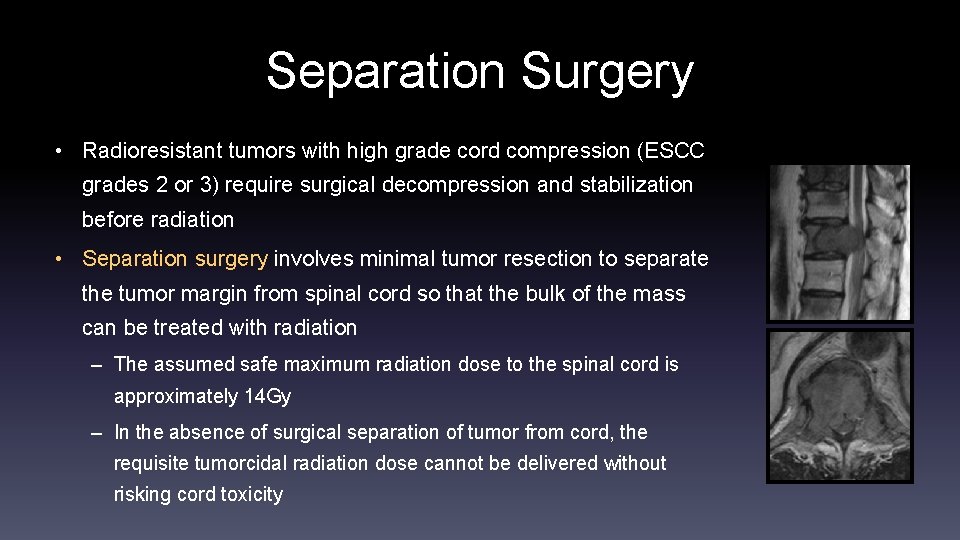
Separation Surgery • Radioresistant tumors with high grade cord compression (ESCC grades 2 or 3) require surgical decompression and stabilization before radiation • Separation surgery involves minimal tumor resection to separate the tumor margin from spinal cord so that the bulk of the mass can be treated with radiation – The assumed safe maximum radiation dose to the spinal cord is approximately 14 Gy – In the absence of surgical separation of tumor from cord, the requisite tumorcidal radiation dose cannot be delivered without risking cord toxicity
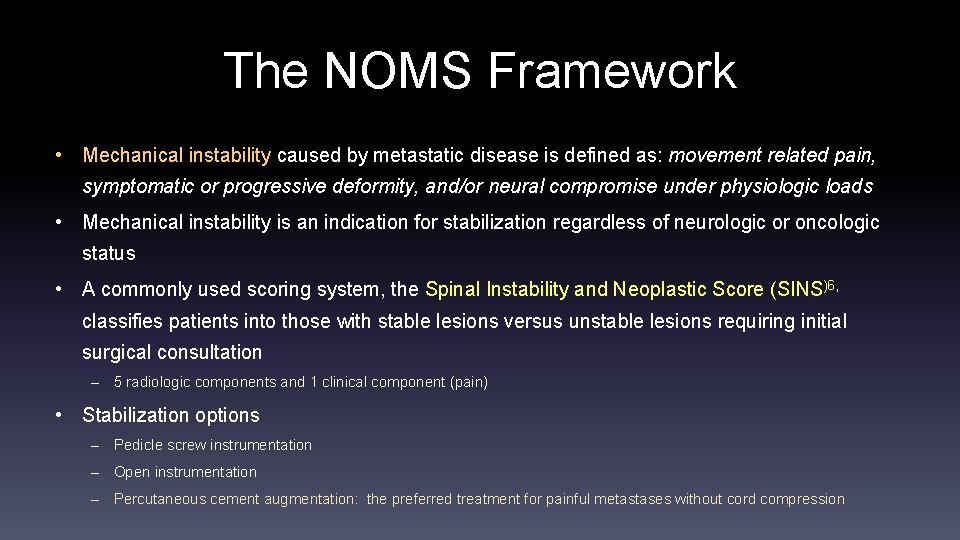
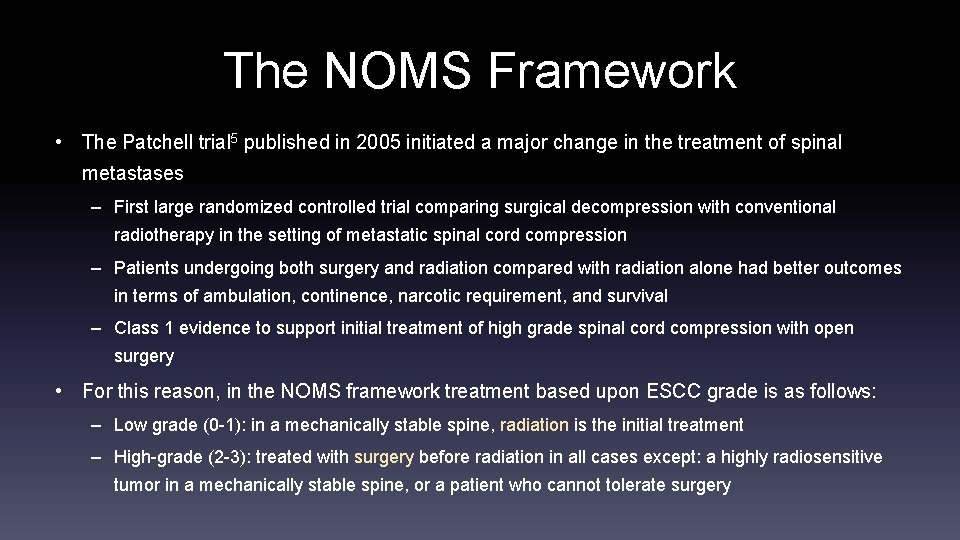
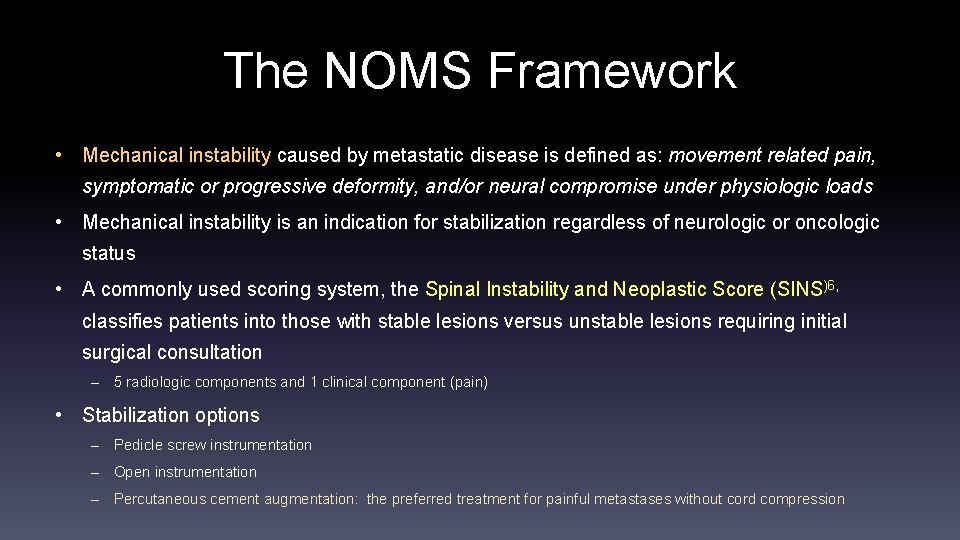
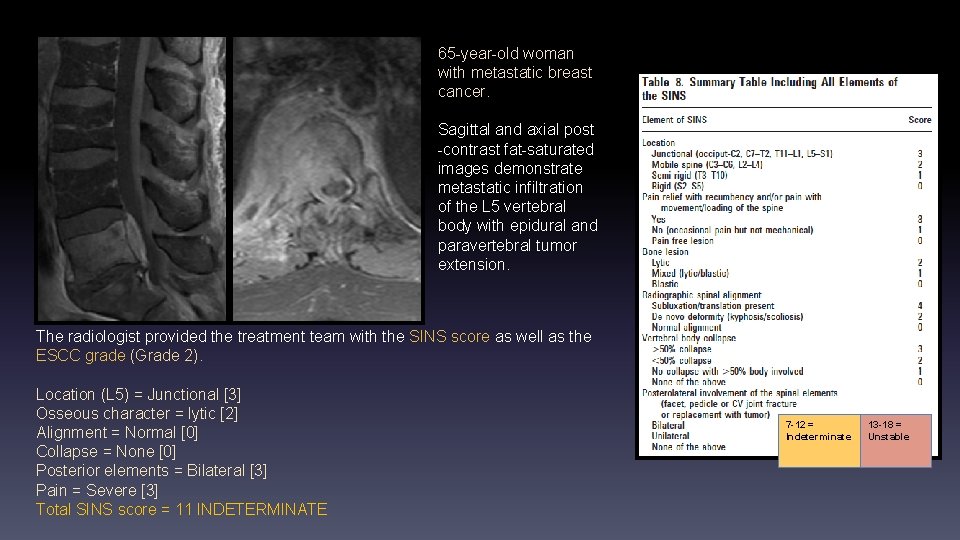
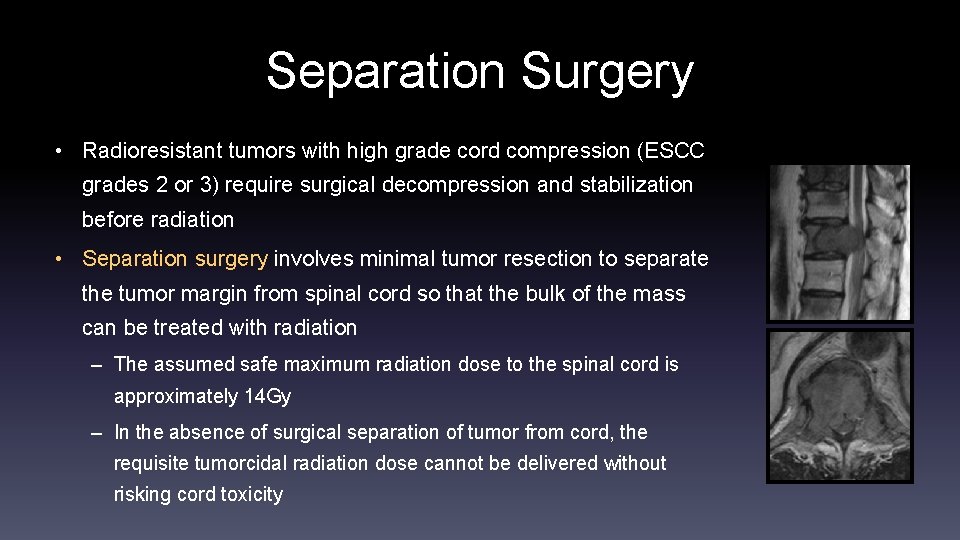
The NOMS Framework • Mechanical instability caused by metastatic disease is defined as: movement related pain, symptomatic or progressive deformity, and/or neural compromise under physiologic loads • Mechanical instability is an indication for stabilization regardless of neurologic or oncologic status • A commonly used scoring system, the Spinal Instability and Neoplastic Score (SINS)6, classifies patients into those with stable lesions versus unstable lesions requiring initial surgical consultation – 5 radiologic components and 1 clinical component (pain) • Stabilization options – Pedicle screw instrumentation – Open instrumentation – Percutaneous cement augmentation: the preferred treatment for painful metastases without cord compression

Location Osseous characteristics Radiographic alignment Vertebral body collapse Involvement of posterior elements Pain Junctional spine (occiput-C 2, C 7 -T 2, T 11 -L 1, L 5 -S 1) Subluxation >50% collapse Bilateral Yes Score = 3 Score = 4 Score = 3 No collapse >50% body involved Unilateral Occasional, not mechanical Score = 1 Mobile spine (C 3 -6, L 2 -4) Lytic Deformity (kyphosis, scoliosis) < 50% collapse Score = 2 Semi-rigid spine (T 3 -10) Mixed (lytic and blastic) Score = 1 Rigid spine (S 2 -5) Blastic Normal None No Score = 0 Score = 0 Total score 0 -6 = Stable 7 -12 = Indeterminate 13 -18 = Unstable Spinal Instability Neoplastic Scale. The scores for the five radiographic components and one clinical component are added together to yield a total SINS score ranging from 0 to 18. Modified from Fisher CG, Spine 2010.
![Location L 4 Mobile 2 Osseous character Lytic 2 Alignment Normal Location (L 4) = Mobile [2] Osseous character = Lytic [2] Alignment = Normal](https://slidetodoc.com/presentation_image_h/ac8edf6e11abd6a9a1a2b7be32911236/image-20.jpg)
Location (L 4) = Mobile [2] Osseous character = Lytic [2] Alignment = Normal [0] Collapse = >50% [3] Posterior elements = bilateral [3] Pain = Yes, mechanical [3] Total SINS score = 13 UNSTABLE 7 -12 = Indeterminate 13 -18 = Unstable This patient with metastatic renal cell carcinoma had presurgical tumor embolization, surgical stabilization with corpectomy and graft placement followed by SRS.
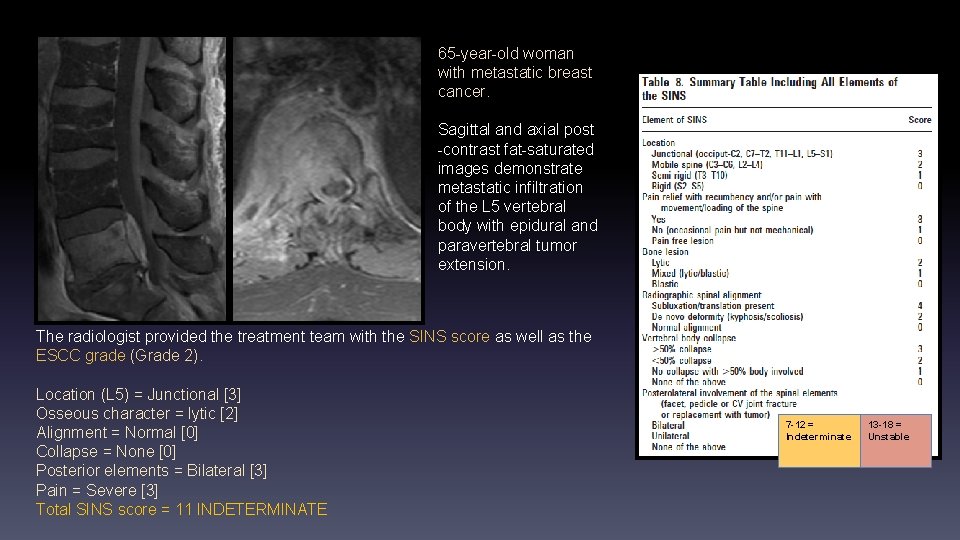
65 -year-old woman with metastatic breast cancer. Sagittal and axial post -contrast fat-saturated images demonstrate metastatic infiltration of the L 5 vertebral body with epidural and paravertebral tumor extension. The radiologist provided the treatment team with the SINS score as well as the ESCC grade (Grade 2). Location (L 5) = Junctional [3] Osseous character = lytic [2] Alignment = Normal [0] Collapse = None [0] Posterior elements = Bilateral [3] Pain = Severe [3] Total SINS score = 11 INDETERMINATE 7 -12 = Indeterminate 13 -18 = Unstable
![T 9 Lesion Location T 9 Semirigid 1 Osseous character lytic 2 T 9 Lesion: Location (T 9) = Semi-rigid [1] Osseous character = lytic [2]](https://slidetodoc.com/presentation_image_h/ac8edf6e11abd6a9a1a2b7be32911236/image-22.jpg)
T 9 Lesion: Location (T 9) = Semi-rigid [1] Osseous character = lytic [2] Alignment = Normal [0] Collapse = None [0] Posterior elements = Unilateral [1] Pain = Occasional [1] Total SINS score = 5 Stable Multiple metastases: grade each separately T 12 Lesion: Location (T 12) = Junctional [3] Osseous character = lytic [2] Alignment = Normal [0] Collapse = None [0] Posterior elements = Bilateral [3] Pain = Severe [3] Total SINS score = 11 Indeterminate 7 -12 = Indeterminate 13 -18 = Unstable High grade cord compression (ECSS Grade 2) = surgery before radiation
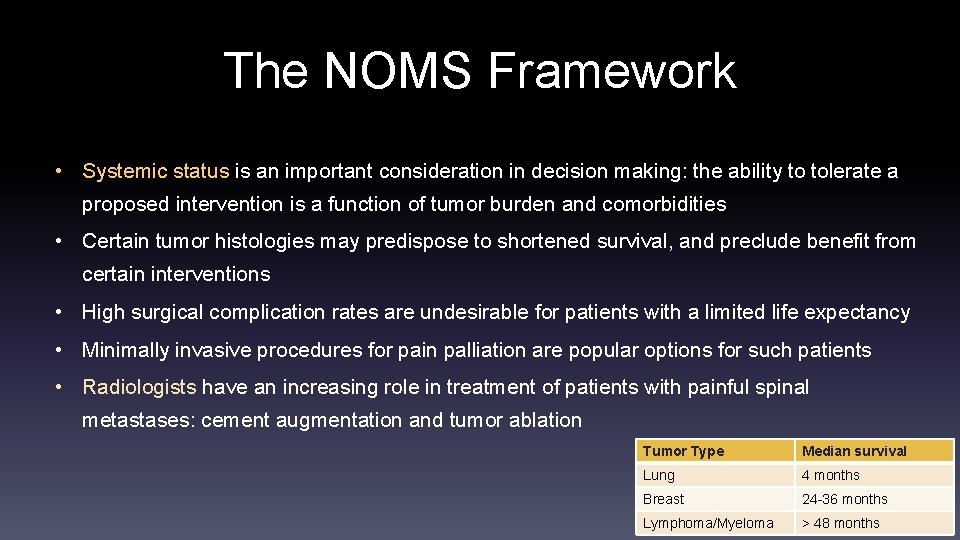
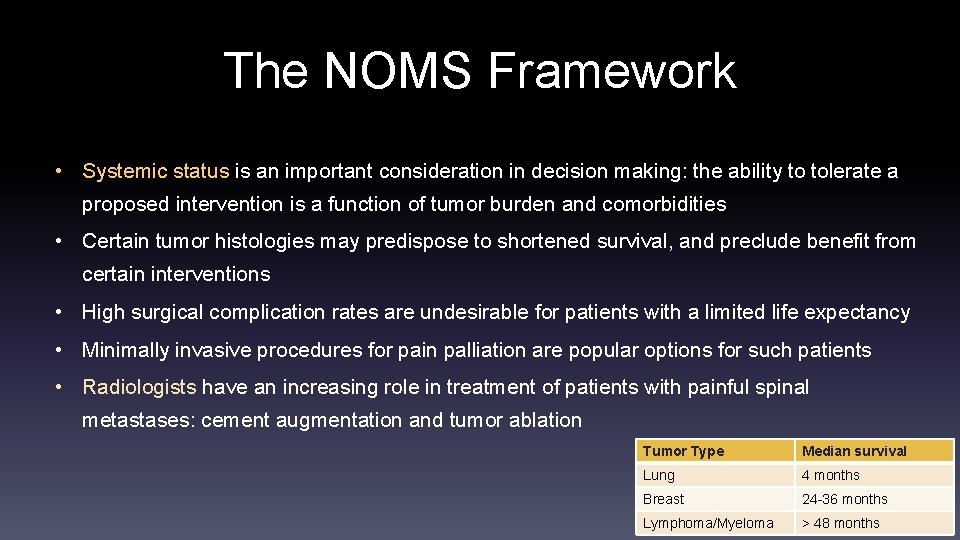
The NOMS Framework • Systemic status is an important consideration in decision making: the ability to tolerate a proposed intervention is a function of tumor burden and comorbidities • Certain tumor histologies may predispose to shortened survival, and preclude benefit from certain interventions • High surgical complication rates are undesirable for patients with a limited life expectancy • Minimally invasive procedures for pain palliation are popular options for such patients • Radiologists have an increasing role in treatment of patients with painful spinal metastases: cement augmentation and tumor ablation Tumor Type Median survival Lung 4 months Breast 24 -36 months Lymphoma/Myeloma > 48 months
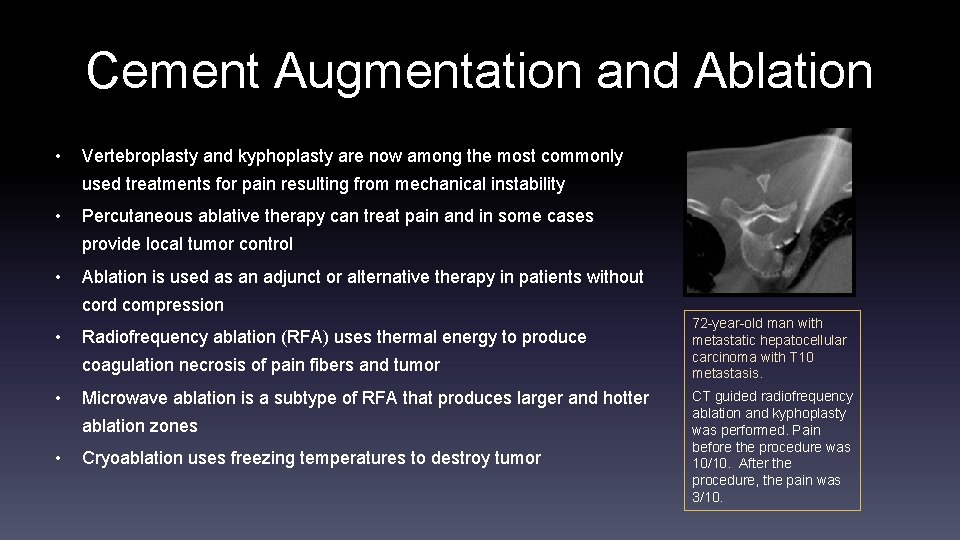
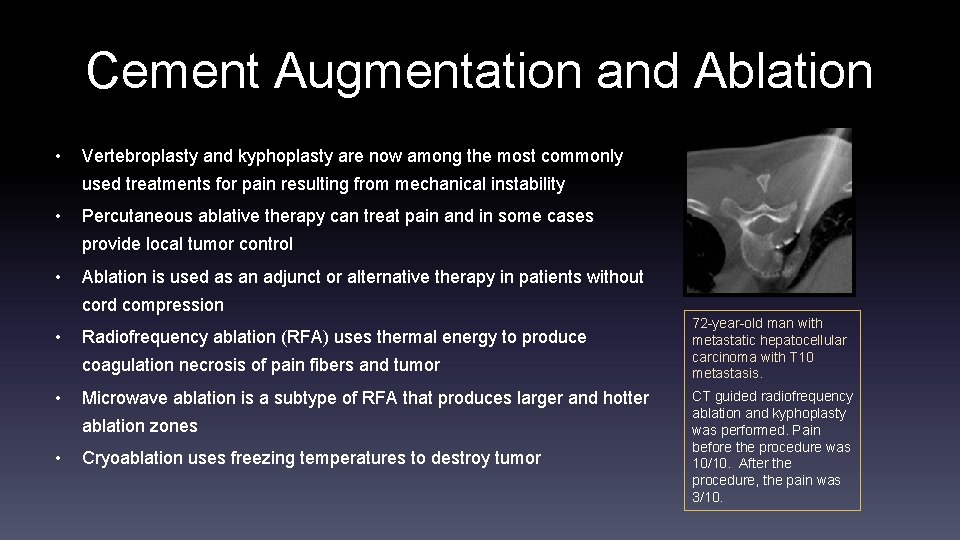
Cement Augmentation and Ablation • Vertebroplasty and kyphoplasty are now among the most commonly used treatments for pain resulting from mechanical instability • Percutaneous ablative therapy can treat pain and in some cases provide local tumor control • Ablation is used as an adjunct or alternative therapy in patients without cord compression • Radiofrequency ablation (RFA) uses thermal energy to produce coagulation necrosis of pain fibers and tumor • Microwave ablation is a subtype of RFA that produces larger and hotter ablation zones • Cryoablation uses freezing temperatures to destroy tumor 72 -year-old man with metastatic hepatocellular carcinoma with T 10 metastasis. CT guided radiofrequency ablation and kyphoplasty was performed. Pain before the procedure was 10/10. After the procedure, the pain was 3/10.
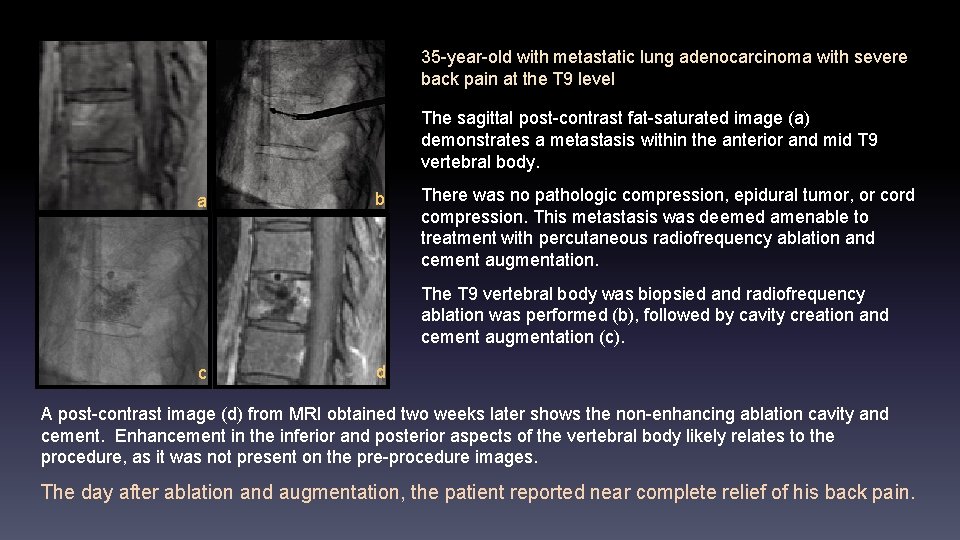
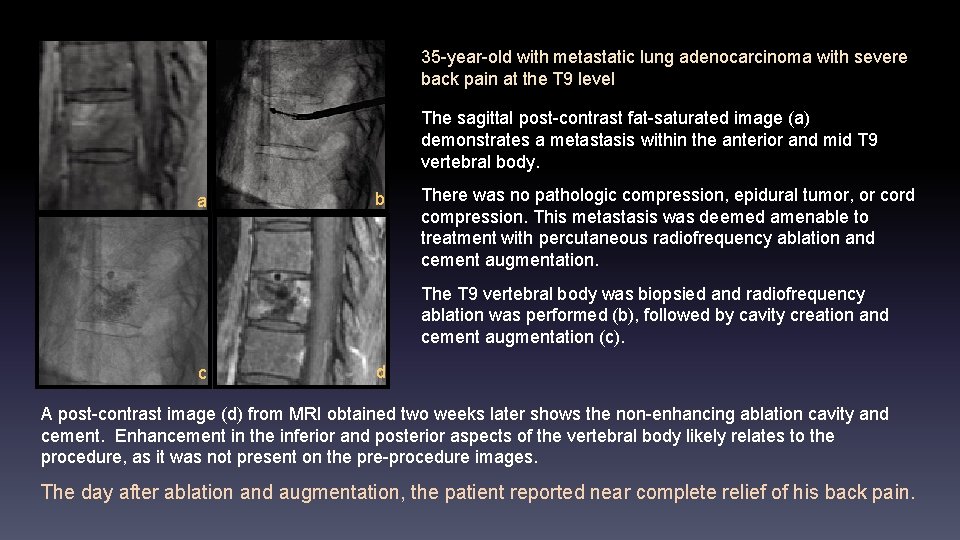
35 -year-old with metastatic lung adenocarcinoma with severe back pain at the T 9 level The sagittal post-contrast fat-saturated image (a) demonstrates a metastasis within the anterior and mid T 9 vertebral body. a b There was no pathologic compression, epidural tumor, or cord compression. This metastasis was deemed amenable to treatment with percutaneous radiofrequency ablation and cement augmentation. The T 9 vertebral body was biopsied and radiofrequency ablation was performed (b), followed by cavity creation and cement augmentation (c). c d A post-contrast image (d) from MRI obtained two weeks later shows the non-enhancing ablation cavity and cement. Enhancement in the inferior and posterior aspects of the vertebral body likely relates to the procedure, as it was not present on the pre-procedure images. The day after ablation and augmentation, the patient reported near complete relief of his back pain.
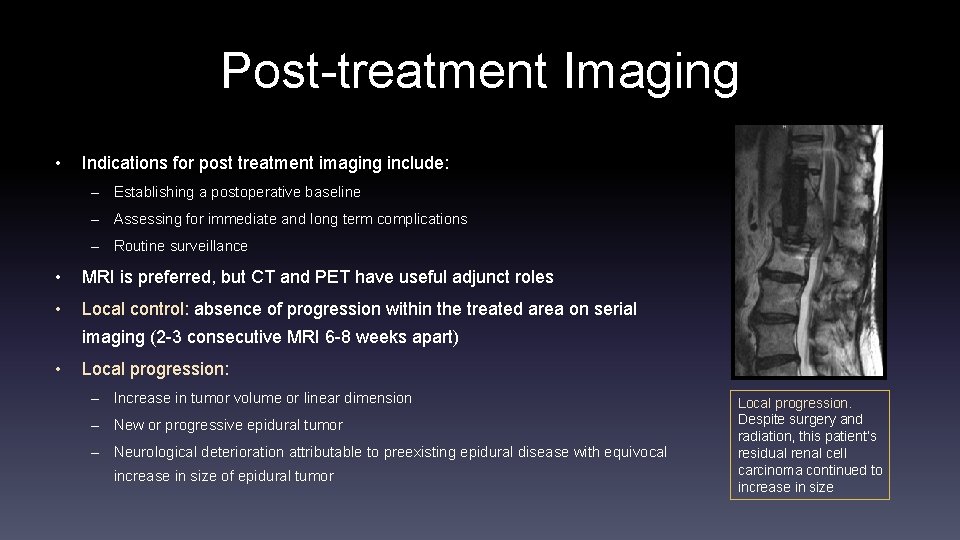
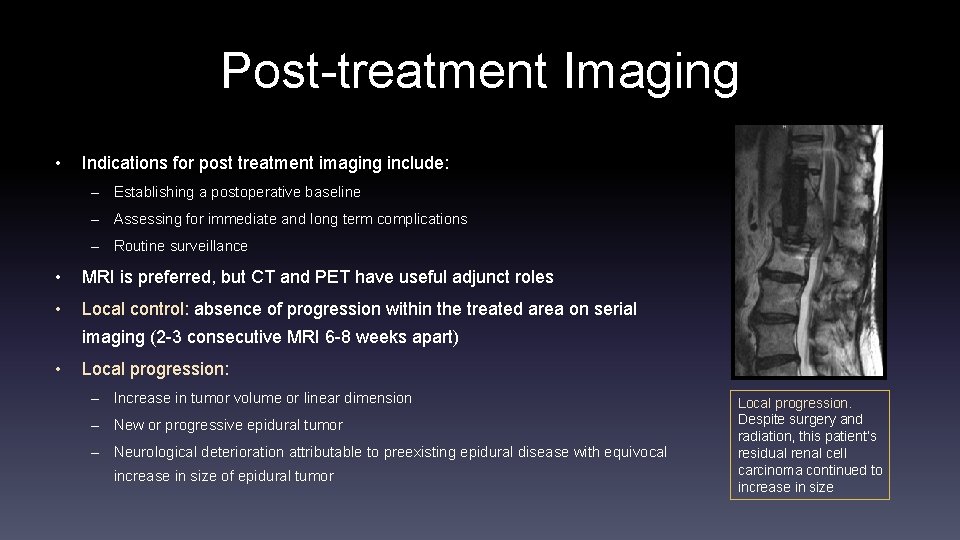
Post-treatment Imaging • Indications for post treatment imaging include: – Establishing a postoperative baseline – Assessing for immediate and long term complications – Routine surveillance • MRI is preferred, but CT and PET have useful adjunct roles • Local control: absence of progression within the treated area on serial imaging (2 -3 consecutive MRI 6 -8 weeks apart) • Local progression: – Increase in tumor volume or linear dimension – New or progressive epidural tumor – Neurological deterioration attributable to preexisting epidural disease with equivocal increase in size of epidural tumor Local progression. Despite surgery and radiation, this patient’s residual renal cell carcinoma continued to increase in size
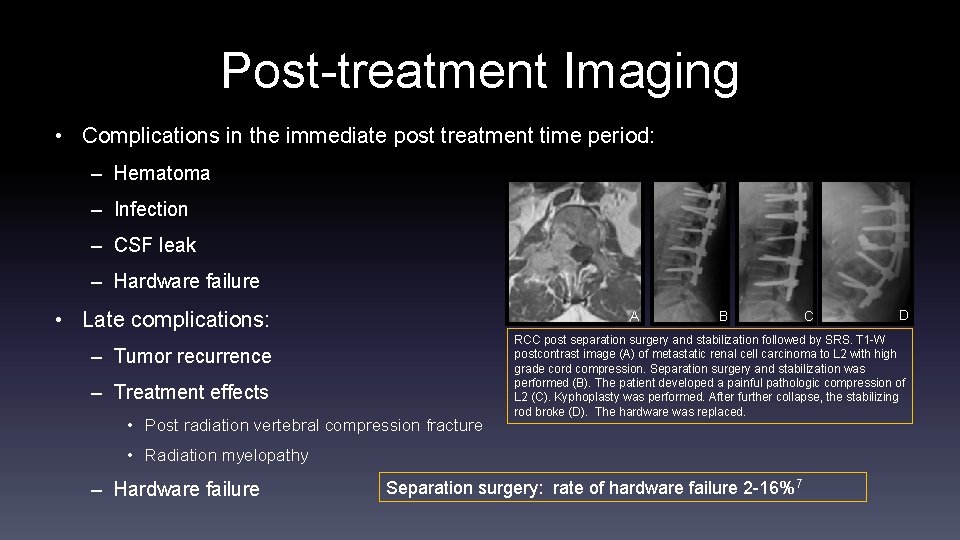
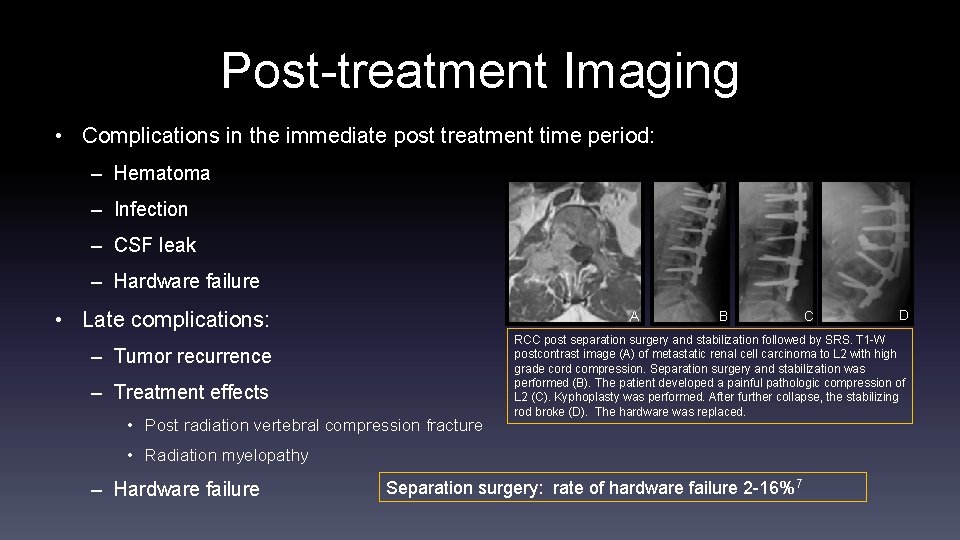
Post-treatment Imaging • Complications in the immediate post treatment time period: – Hematoma – Infection – CSF leak – Hardware failure • Late complications: A – Tumor recurrence – Treatment effects • Post radiation vertebral compression fracture B D RCC post separation surgery and stabilization followed by SRS. T 1 -W postcontrast image (A) of metastatic renal cell carcinoma to L 2 with high grade cord compression. Separation surgery and stabilization was performed (B). The patient developed a painful pathologic compression of L 2 (C). Kyphoplasty was performed. After further collapse, the stabilizing rod broke (D). The hardware was replaced. • Radiation myelopathy – Hardware failure C Separation surgery: rate of hardware failure 2 -16%7
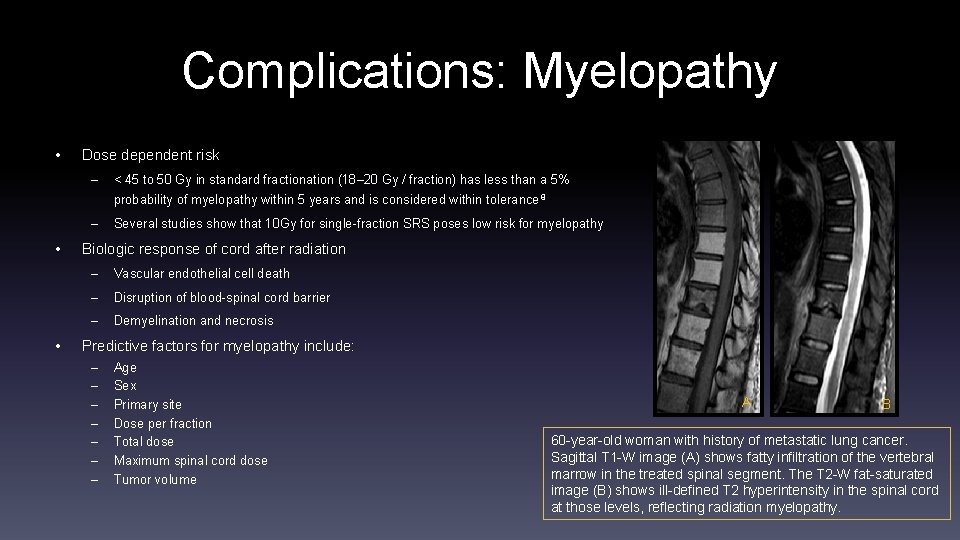
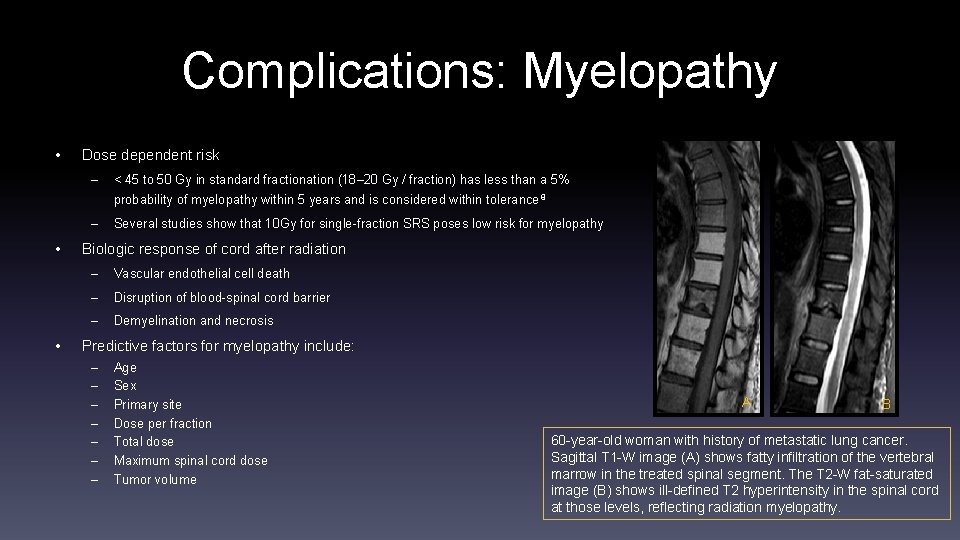
Complications: Myelopathy • Dose dependent risk – < 45 to 50 Gy in standard fractionation (18– 20 Gy / fraction) has less than a 5% probability of myelopathy within 5 years and is considered within tolerance 8 – • • Several studies show that 10 Gy for single-fraction SRS poses low risk for myelopathy Biologic response of cord after radiation – Vascular endothelial cell death – Disruption of blood-spinal cord barrier – Demyelination and necrosis Predictive factors for myelopathy include: – – – – Age Sex Primary site Dose per fraction Total dose Maximum spinal cord dose Tumor volume A B 60 -year-old woman with history of metastatic lung cancer. Sagittal T 1 -W image (A) shows fatty infiltration of the vertebral marrow in the treated spinal segment. The T 2 -W fat-saturated image (B) shows ill-defined T 2 hyperintensity in the spinal cord at those levels, reflecting radiation myelopathy.
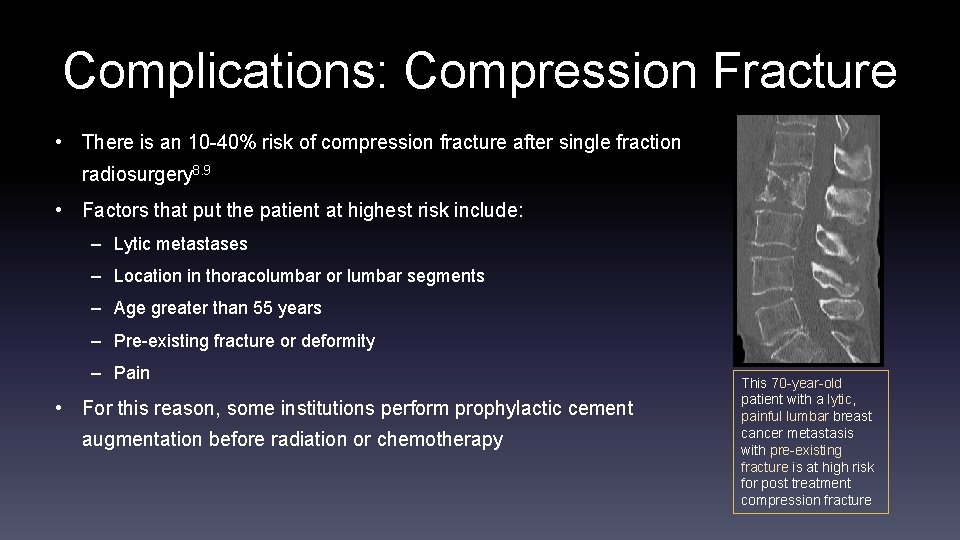
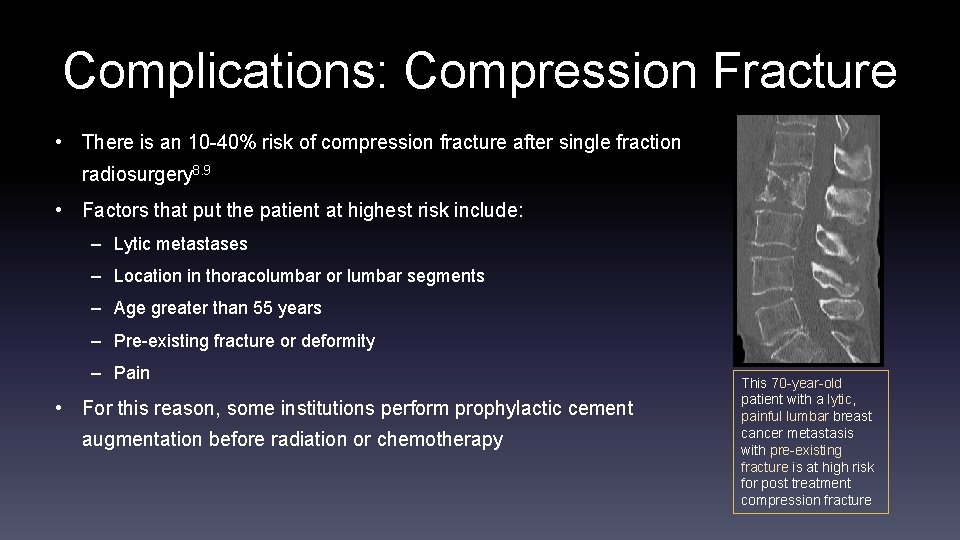
Complications: Compression Fracture • There is an 10 -40% risk of compression fracture after single fraction radiosurgery 8. 9 • Factors that put the patient at highest risk include: – Lytic metastases – Location in thoracolumbar or lumbar segments – Age greater than 55 years – Pre-existing fracture or deformity – Pain • For this reason, some institutions perform prophylactic cement augmentation before radiation or chemotherapy This 70 -year-old patient with a lytic, painful lumbar breast cancer metastasis with pre-existing fracture is at high risk for post treatment compression fracture
Conclusion • Advances in spine oncology have improved treatment and survival for patients with osseous spinal metastatic disease • To add value to the multidisciplinary treatment team, we should be familiar with and report data relevant to the NOMS framework, Epidural spinal cord compression grading scale (ESCC), and Spinal instability neoplastic score (SINS), as these are widely utilized by spinal surgeons and oncologists for patient management and decision-making • Radiologists have new opportunities to provide direct, minimally-invasive treatment for these patients, requiring maintenance of interventional skills and knowledge of the most current tools and techniques
References 1. American Cancer Society, Cancer Facts and Figures 2016, Available at: http: //www. cancer. org/research/cancerfactsstatistics/cancerfactsfigures 2016. Accessed January 1, 2016. 2. Thibault I, Chang EL, Sheehan J, et al. Response assessment after stereotactic body radiotherapy for spinal metastasis: a report from the SPIne response assessment in Neuro-Oncology (SPINO) group. Lancet Oncol. 2015; 16(16): e 595 -603. 3. Laufer I, Rubin DG, Lis E, et al. The NOMS framework: approach to the treatment of spinal metastatic tumors. Oncologist. 2013; 18(6): 744 -51. 4. Bilsky MH, Laufer I, Fourney DR, et al. Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine. 2010; 13(3): 324 -8. 5. Patchell RA, Tibbs PA, Regine WF, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005; 366(9486): 643 -8. 6. Fisher CG, Versteeg AL, Schouten R, et al. Reliability of the spinal instability neoplastic scale among radiologists: an assessment of instability secondary to spinal metastases. AJR Am J Roentgenol. 2014; 203(4): 869 -74. 7. Amankulor NM, Xu R, Iorgulescu JB, et al. The incidence and patterns of hardware failure after separation surgery in patients with spinal metastatic tumors. Spine J. 2014; 14(9): 1850 -9. 8. Sharan AD, Szulc A, Krystal J, Yassari R, Laufer I, Bilsky MH. The integration of radiosurgery for the treatment of patients with metastatic spine diseases. J Am Acad Orthop Surg. 2014; 22(7): 447 -54. 9. Jawad MS, Fahim DK, Gerszten PC, et al. Vertebral compression fractures after stereotactic body radiation therapy: a large, multi-institutional, multinational evaluation. J Neurosurg Spine. 2016; : 1 -9.
 Daniel birchall neuroradiologist
Daniel birchall neuroradiologist Wende lachendorf
Wende lachendorf Markierung einer wende ernst jandl
Markierung einer wende ernst jandl Kopernikanische wende pädagogik
Kopernikanische wende pädagogik Hamilton wende
Hamilton wende Aware huiselijk geweld
Aware huiselijk geweld While reading activities
While reading activities Anatomi organ reproduksi
Anatomi organ reproduksi Egg för emanuel
Egg för emanuel Tack för att ni har lyssnat
Tack för att ni har lyssnat Varians formel
Varians formel Tidbok för yrkesförare
Tidbok för yrkesförare Rutin för avvikelsehantering
Rutin för avvikelsehantering Mitos steg
Mitos steg Presentera för publik crossboss
Presentera för publik crossboss Formuö
Formuö Myndigheten för delaktighet
Myndigheten för delaktighet Att skriva debattartikel
Att skriva debattartikel Kung som dog 1611
Kung som dog 1611 Tack för att ni lyssnade
Tack för att ni lyssnade Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Referatmarkering
Referatmarkering Varför kallas perioden 1918-1939 för mellankrigstiden
Varför kallas perioden 1918-1939 för mellankrigstiden Lågenergihus nyproduktion
Lågenergihus nyproduktion Punkthöjd karttecken
Punkthöjd karttecken Rådet för byggkompetens
Rådet för byggkompetens Lufttryck formel
Lufttryck formel Elektronik för barn
Elektronik för barn Vad är densitet
Vad är densitet Tack för att ni har lyssnat
Tack för att ni har lyssnat Borra hål för knoppar
Borra hål för knoppar Smärtskolan kunskap för livet
Smärtskolan kunskap för livet