SHINE 3 Day Part D Counselor Training Day



- Slides: 51

SHINE 3 Day Part D Counselor Training
Day 1 Topics § § § § Overview of SHINE Original Medicare (Part A & B) Medicare Supplement Plans (Medigap) Medicare Advantage Plans (Part C) Other Sources of Supplementing Medicare Part D Extra Help Prescription Advantage
Day 2 & 3 Topics Day 2 § Review of Medicare Basics (Day 1) § Review Extra Help § Review Prescription Advantage § Medicare Plan Finder Demo Day 3 § Medicare. gov website (hands-on training)
Certified SHINE Counselors n Explain Medicare Part A, B, C and D benefits and gaps n Compare health insurance and prescription drug plan options, costs and benefits n Screen for public benefit programs and provide assistance with the application process n Help with claims and billing problems n Start appeals and explain grievance procedures
SHINE Part D Enrollment Counselors § Assist beneficiaries by comparing the cost and benefits of the programs available to them § Screen beneficiaries for Extra Help and Prescription Advantage § Provide enrollment assistance into these programs § Complete a client contact form after each appointment § The 3 day Part D Counselor Training is designed to help you handle BASIC matters

Medicare Parts A & B “Original Medicare” & Supplements (Part C & Medigaps)
Medicare n Enacted into law 1965, Title XVIII of the Social Security Act; Effective July 1 st , 1966 • Entitlement program n Federal health insurance program for: • Individuals over age 65 Ø Not necessarily full retirement age • Individuals under age 65 with a disability Ø Deemed “disabled” by Social Security for at least 24 months § Never intended to cover 100% of healthcare costs • NOT a comprehensive health insurance program
Medicare n Medicare only pays for services which are reasonable and medically necessary for the treatment and diagnosis of an accident or illness n Even when “medically necessary”, there are gaps in Medicare coverage and the beneficiary must pay a portion of the medical expenses
Medicare n 4 parts of Medicare • Part A: • Part B: • Part C: • Part D: n Hospital Insurance Medicare Advantage Plans Prescription Drug Coverage Part A & B called Original Medicare
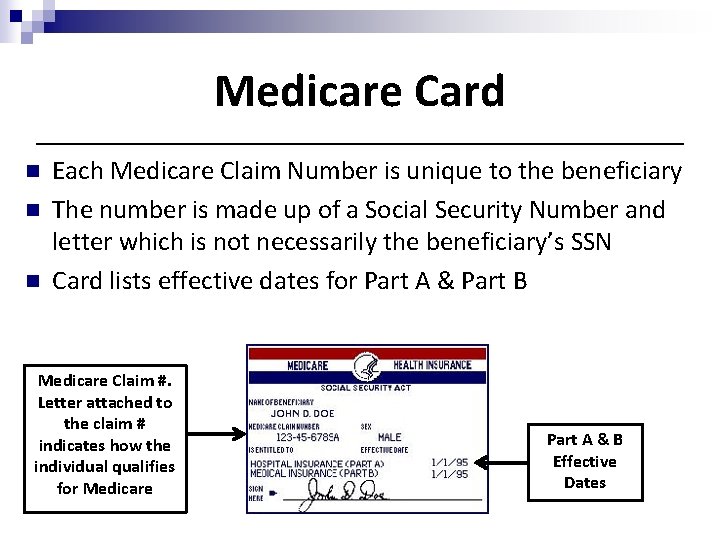
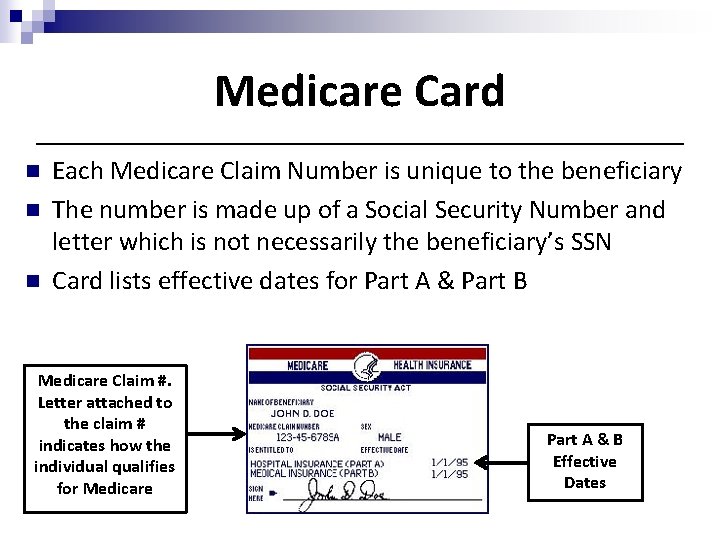
Medicare Card n n n Each Medicare Claim Number is unique to the beneficiary The number is made up of a Social Security Number and letter which is not necessarily the beneficiary’s SSN Card lists effective dates for Part A & Part B Medicare Claim #. Letter attached to the claim # indicates how the individual qualifies for Medicare Part A & B Effective Dates
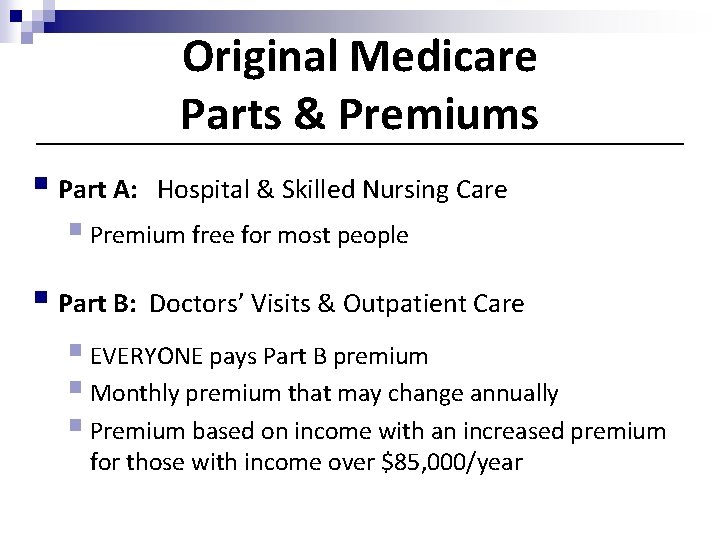
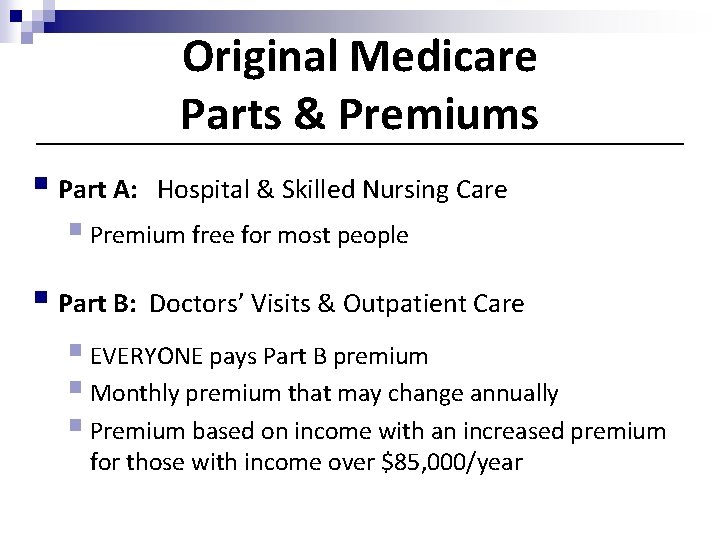
Original Medicare Parts & Premiums § Part A: Hospital & Skilled Nursing Care § Premium free for most people § Part B: Doctors’ Visits & Outpatient Care § EVERYONE pays Part B premium § Monthly premium that may change annually § Premium based on income with an increased premium for those with income over $85, 000/year
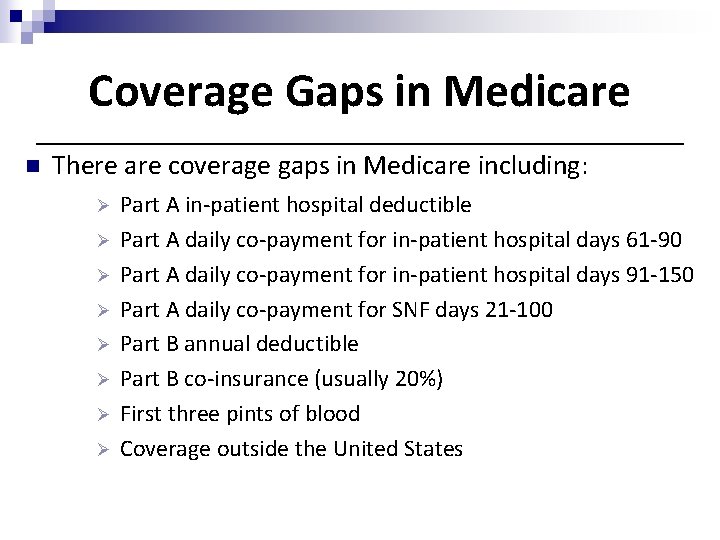
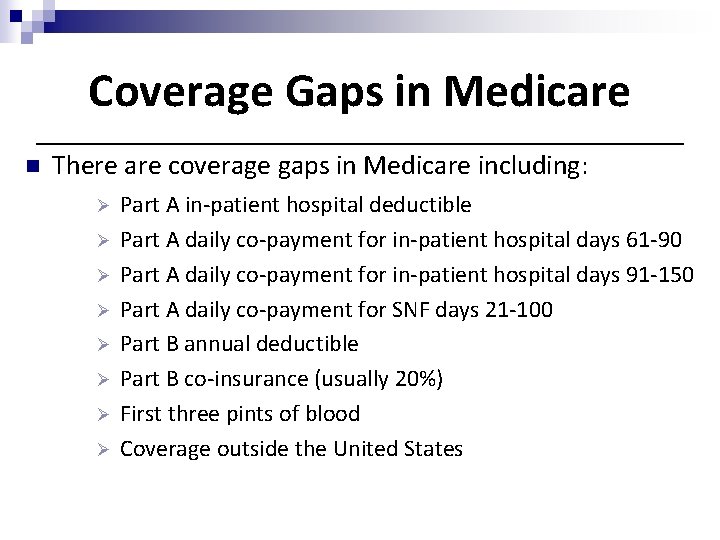
Coverage Gaps in Medicare n There are coverage gaps in Medicare including: Ø Ø Ø Ø Part A in-patient hospital deductible Part A daily co-payment for in-patient hospital days 61 -90 Part A daily co-payment for in-patient hospital days 91 -150 Part A daily co-payment for SNF days 21 -100 Part B annual deductible Part B co-insurance (usually 20%) First three pints of blood Coverage outside the United States
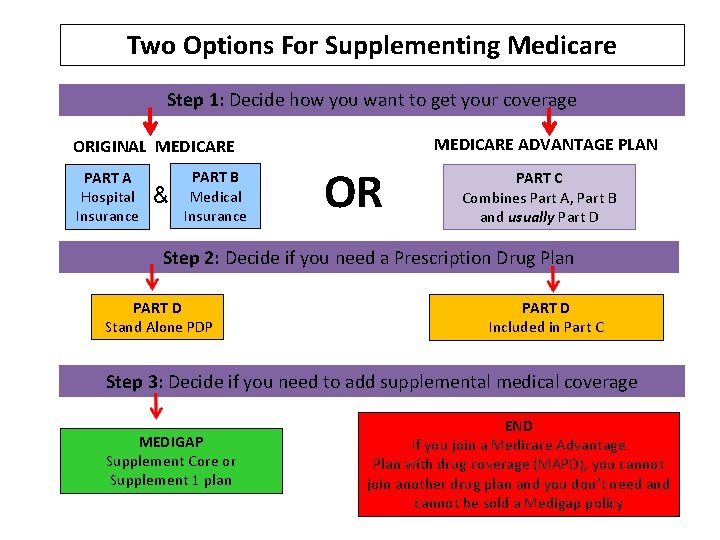
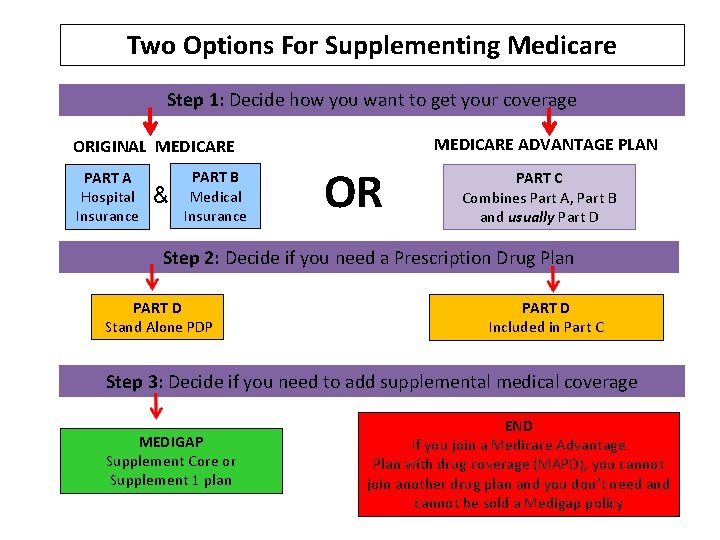
Two Options For Supplementing Medicare Step 1: Decide how you want to get your coverage MEDICARE ADVANTAGE PLAN ORIGINAL MEDICARE PART A Hospital Insurance & PART B Medical Insurance OR PART C Combines Part A, Part B and usually Part D Step 2: Decide if you need a Prescription Drug Plan PART D Stand Alone PDP PART D Included in Part C Step 3: Decide if you need to add supplemental medical coverage MEDIGAP Supplement Core or Supplement 1 plan END If you join a Medicare Advantage Plan with drug coverage (MAPD), you cannot join another drug plan and you don’t need and cannot be sold a Medigap policy
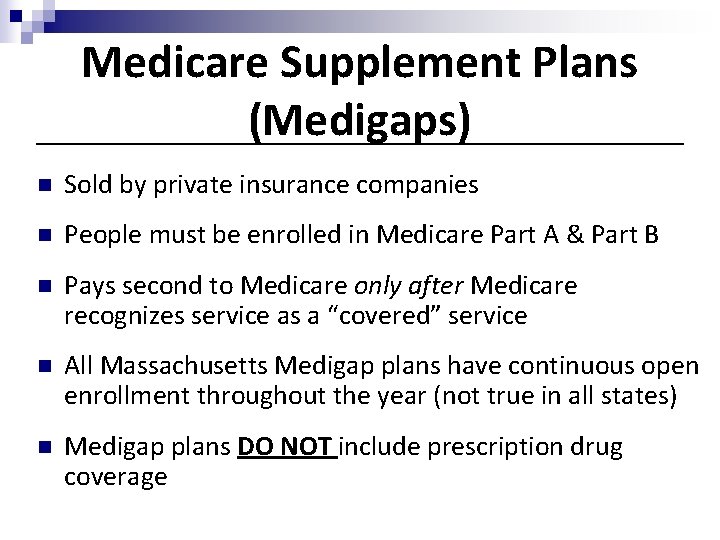
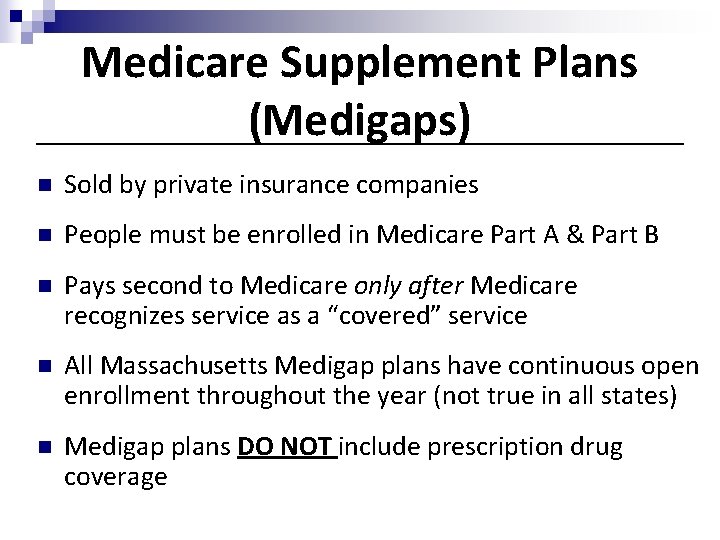
Medicare Supplement Plans (Medigaps) n Sold by private insurance companies n People must be enrolled in Medicare Part A & Part B n Pays second to Medicare only after Medicare recognizes service as a “covered” service n All Massachusetts Medigap plans have continuous open enrollment throughout the year (not true in all states) n Medigap plans DO NOT include prescription drug coverage
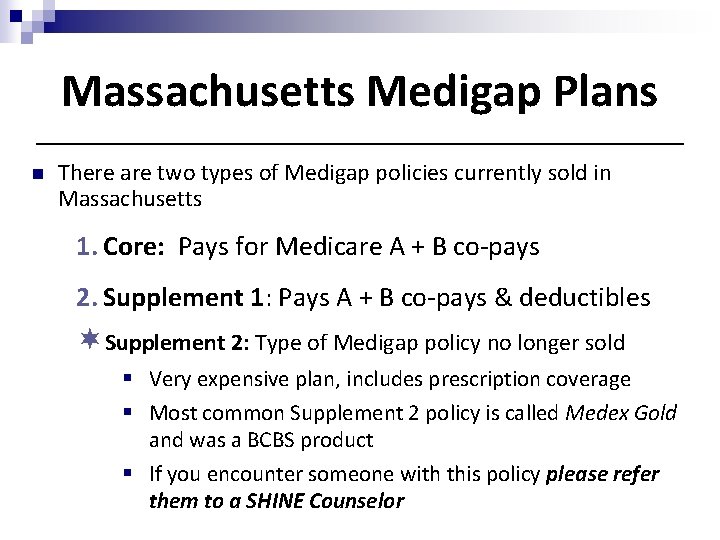
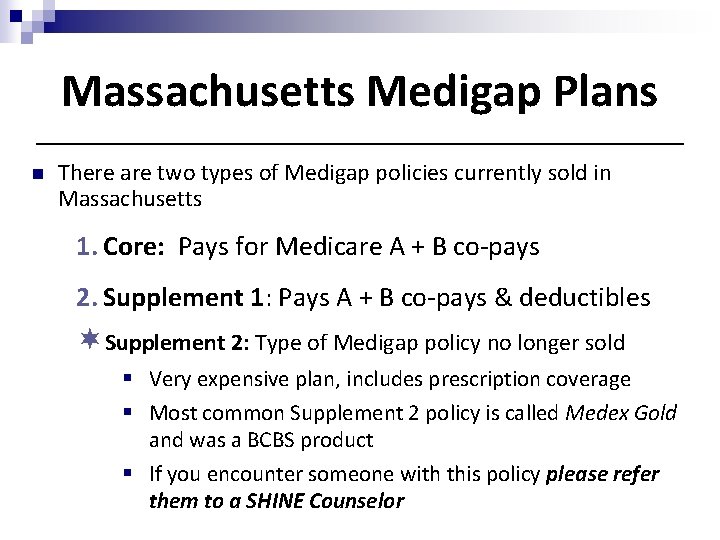
Massachusetts Medigap Plans n There are two types of Medigap policies currently sold in Massachusetts 1. Core: Pays for Medicare A + B co-pays 2. Supplement 1: Pays A + B co-pays & deductibles ¬Supplement 2: Type of Medigap policy no longer sold § Very expensive plan, includes prescription coverage § Most common Supplement 2 policy is called Medex Gold and was a BCBS product § If you encounter someone with this policy please refer them to a SHINE Counselor
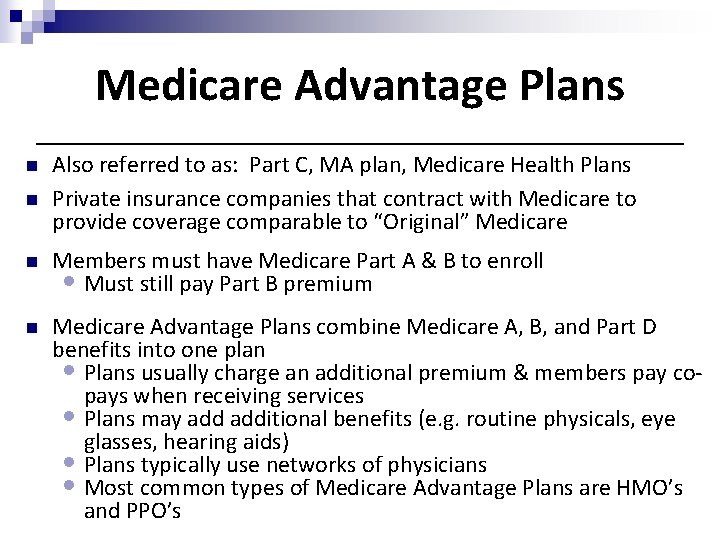
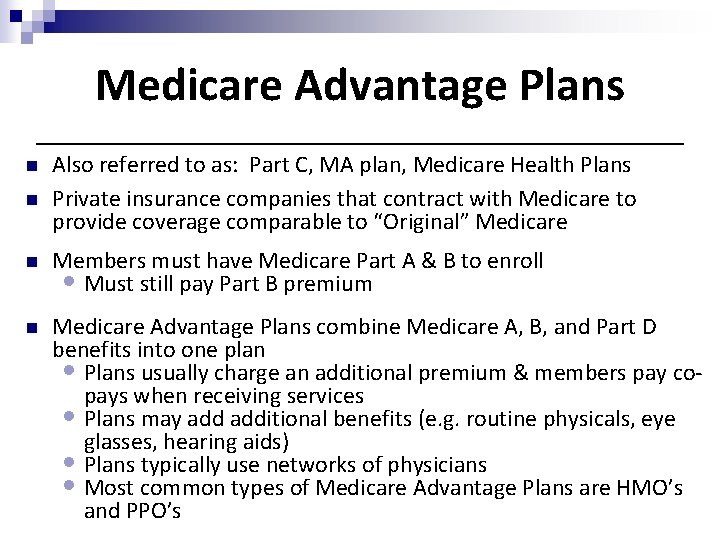
Medicare Advantage Plans n n Also referred to as: Part C, MA plan, Medicare Health Plans Private insurance companies that contract with Medicare to provide coverage comparable to “Original” Medicare n Members must have Medicare Part A & B to enroll • Must still pay Part B premium n Medicare Advantage Plans combine Medicare A, B, and Part D benefits into one plan • Plans usually charge an additional premium & members pay copays when receiving services • Plans may additional benefits (e. g. routine physicals, eye glasses, hearing aids) • Plans typically use networks of physicians • Most common types of Medicare Advantage Plans are HMO’s and PPO’s
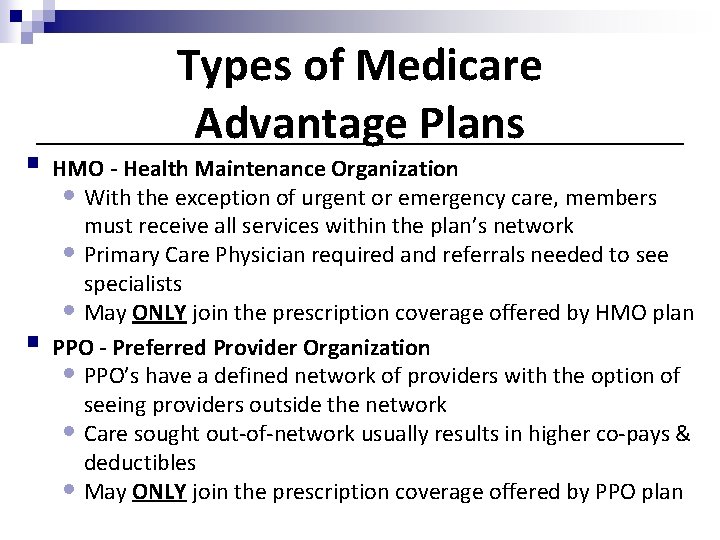
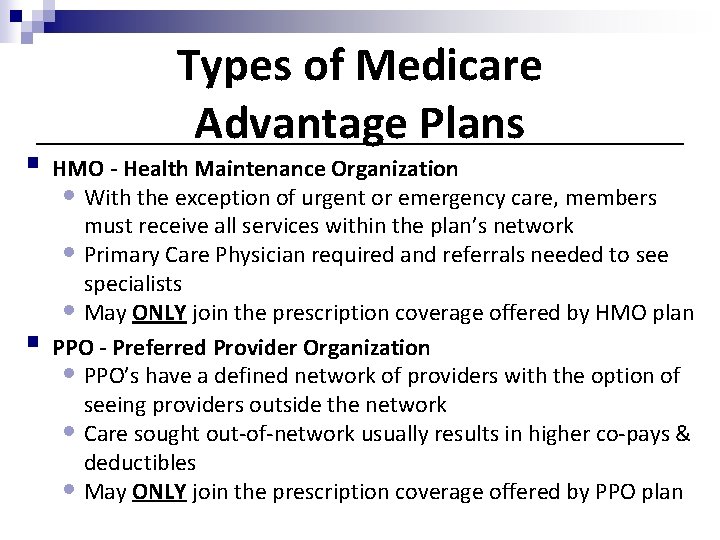
Types of Medicare Advantage Plans § HMO - Health Maintenance Organization • With the exception of urgent or emergency care, members § must receive all services within the plan’s network • Primary Care Physician required and referrals needed to see specialists • May ONLY join the prescription coverage offered by HMO plan PPO - Preferred Provider Organization • PPO’s have a defined network of providers with the option of seeing providers outside the network • Care sought out-of-network usually results in higher co-pays & deductibles • May ONLY join the prescription coverage offered by PPO plan
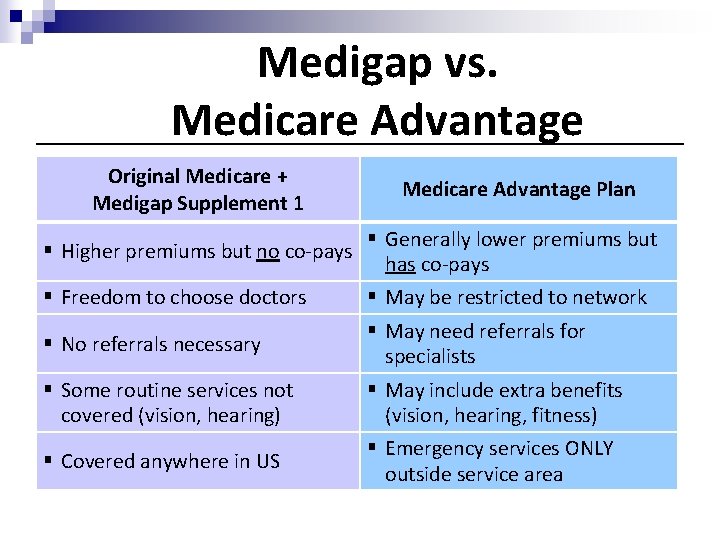
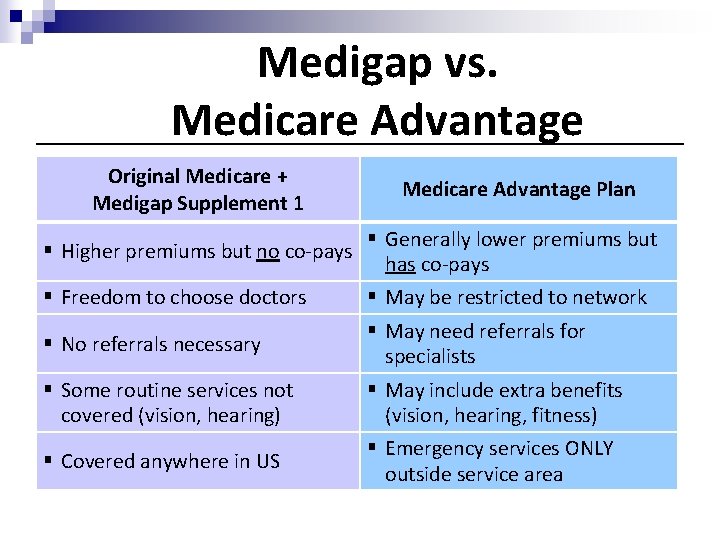
Medigap vs. Medicare Advantage Original Medicare + Medigap Supplement 1 § Higher premiums but no co-pays § Freedom to choose doctors § No referrals necessary § Some routine services not covered (vision, hearing) § Covered anywhere in US Medicare Advantage Plan § Generally lower premiums but has co-pays § May be restricted to network § May need referrals for specialists § May include extra benefits (vision, hearing, fitness) § Emergency services ONLY outside service area
Other ways to supplement Medicare n Retiree Health Plans (group plans) • Each retiree plan is different n Veterans Administration n Medicaid/Mass. Health (for very low- income)
Medicare and Mass. Health n A beneficiary who has Medicare and Mass. Health is referred to as “Dual Eligible” n For hospital and medical services, Medicare always primary and Mass. Health pays secondary as long as the provider accepts Mass. Health n Dual eligibles who want drug coverage must get it through a Medicare Part D plan • Mass. Health will help pay for some medications not covered by Part D (ex. OTC medications) n Dual eligibles qualify for reduced Part D premiums, deductibles, and drug co-pays
Medicare Part D
Part D Overview § Medicare offers prescription drug coverage to everyone with Medicare § Beneficiaries with Part A and/or Part B are eligible § 2 ways to get prescription coverage: 1. Medicare Prescription Drug Plans (PDPs); also known as stand alone plans 2. Medicare Advantage Plans with drug coverage (MA-PD’s) § Part D is voluntary, but eligible beneficiaries who do not enroll may be subject to a penalty § Provides outpatient prescription drugs
Formulary n The prescription benefit includes a list of “covered drugs” and this list is called the “formulary” n If the insurer is very selective about which drugs are to be covered, then it is sometimes referred to as a “closed formulary”. If the formulary is open to all drugs but places drugs into different cost sharing categories or “tiers”, it is referred to as an “open formulary” n Each plan must meet formulary standards. The formulary must include and cover certain drugs or certain classes of drugs. Medicare has established a category of excluded drugs
Examples of Part D Excluded Drugs n Drugs for anorexia, weight loss or weight gain n Drugs for the symptomatic relief of cough and colds n Prescription vitamins and mineral products, except prenatal vitamins and fluoride preparations n Non-prescription drugs (over the counter) n Drugs that could be covered under Medicare Part A and/or Medicare Part B
Appeals to Formulary n Beneficiaries can take the following steps when a drug they are taking is not covered under the formulary: • Ask their prescriber if she/he meets prior authorization or step therapy requirements or if there are generic, over-thecounter or less expensive brand name drugs • Request an coverage determination (including an “exception”) that the plan cover the drug • Try to find a SEP that they are eligible for in order to switch Part D plans to one that has a formulary that covers all of the beneficiaries drugs
Not all Part D Plans are made equal! n PDPs and MA-PDs may vary based on: • • Benefit Design Monthly Premium Deductible Co-payments Formulary Drug Prices Drug Restrictions Pharmacy Network
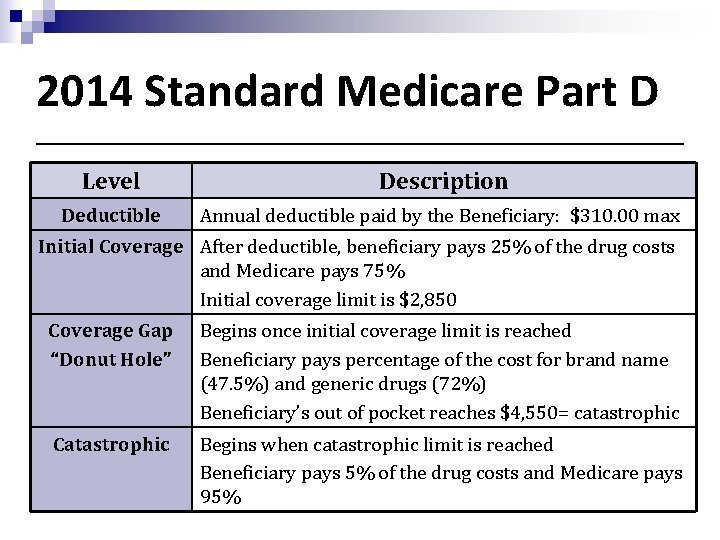
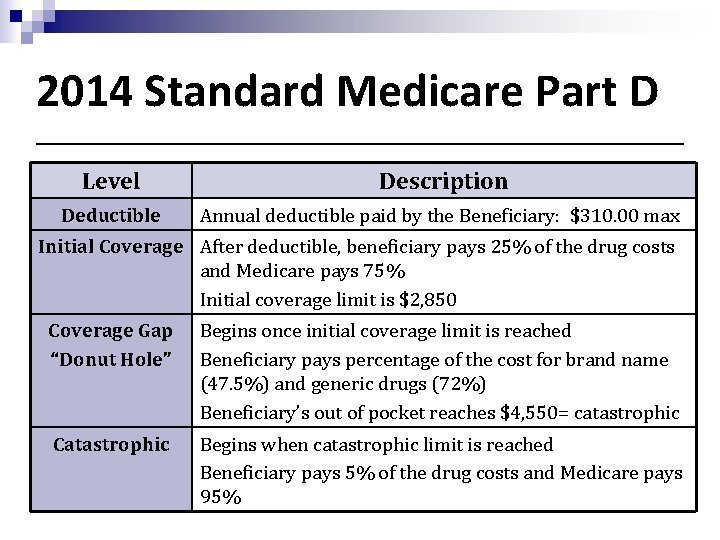
2014 Standard Medicare Part D Level Description Deductible Annual deductible paid by the Beneficiary: $310. 00 max Initial Coverage After deductible, beneficiary pays 25% of the drug costs and Medicare pays 75% Initial coverage limit is $2, 850 Coverage Gap “Donut Hole” Begins once initial coverage limit is reached Beneficiary pays percentage of the cost for brand name (47. 5%) and generic drugs (72%) Beneficiary’s out of pocket reaches $4, 550= catastrophic Catastrophic Begins when catastrophic limit is reached Beneficiary pays 5% of the drug costs and Medicare pays 95%
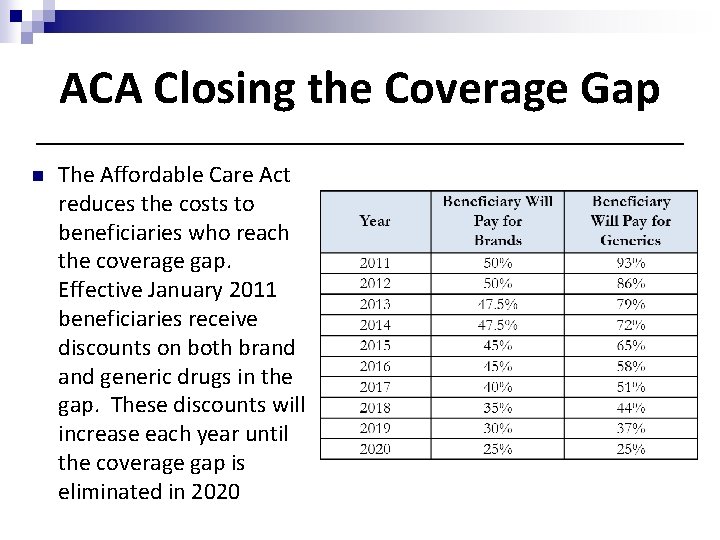
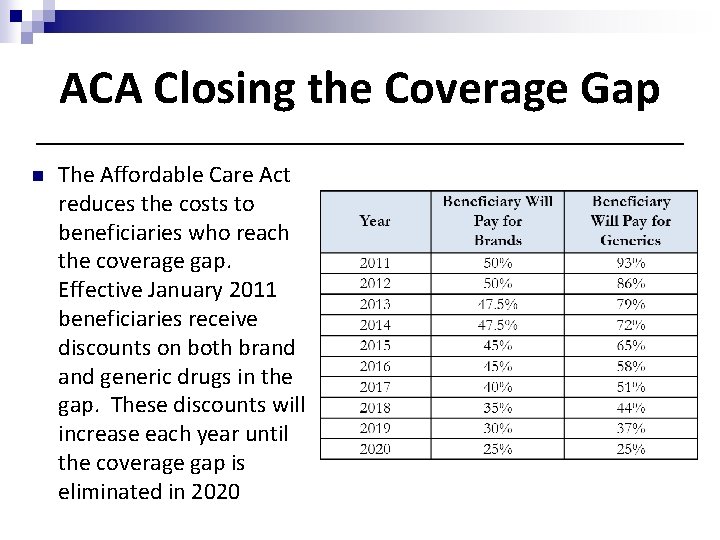
ACA Closing the Coverage Gap n The Affordable Care Act reduces the costs to beneficiaries who reach the coverage gap. Effective January 2011 beneficiaries receive discounts on both brand generic drugs in the gap. These discounts will increase each year until the coverage gap is eliminated in 2020
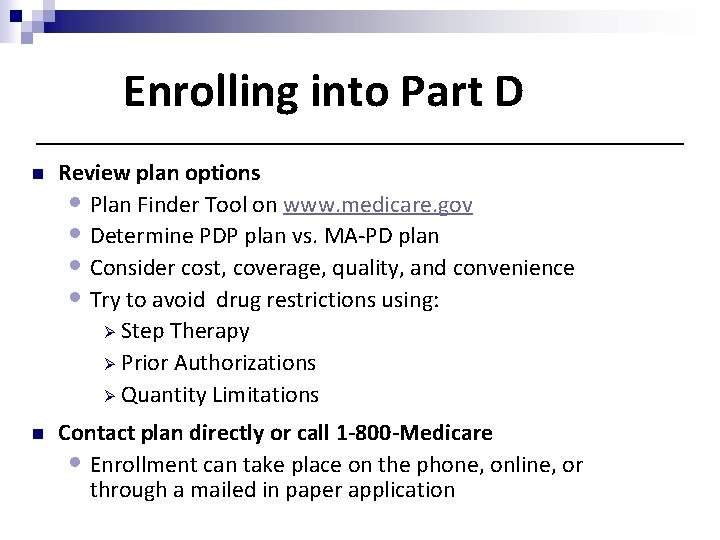
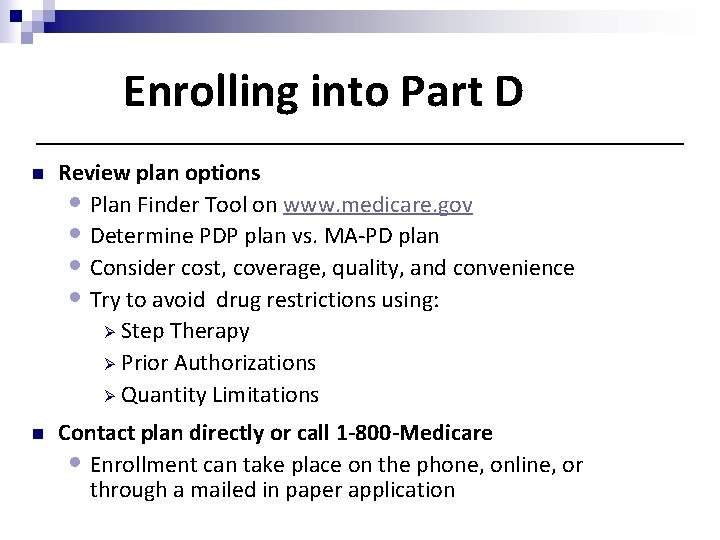
Enrolling into Part D n Review plan options • Plan Finder Tool on www. medicare. gov • Determine PDP plan vs. MA-PD plan • Consider cost, coverage, quality, and convenience • Try to avoid drug restrictions using: Ø Step Therapy Ø Prior Authorizations Ø Quantity Limitations n Contact plan directly or call 1 -800 -Medicare • Enrollment can take place on the phone, online, or through a mailed in paper application
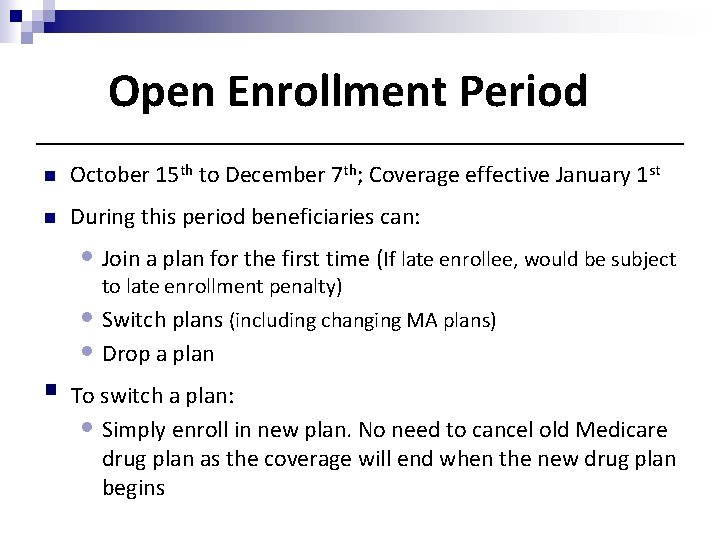
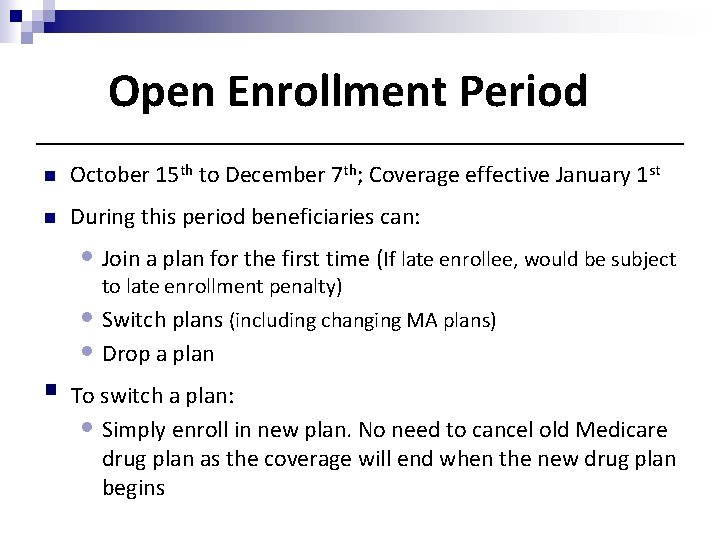
Open Enrollment Period n October 15 th to December 7 th; Coverage effective January 1 st n During this period beneficiaries can: • Join a plan for the first time (If late enrollee, would be subject to late enrollment penalty) • Switch plans (including changing MA plans) • Drop a plan § To switch a plan: • Simply enroll in new plan. No need to cancel old Medicare drug plan as the coverage will end when the new drug plan begins
Late Enrollment n If a Medicare beneficiary does not join a Medicare Prescription Drug Plan when first eligible and didn’t have other creditable prescription drug coverage that met Medicare’s minimum standards, they could incur a late enrollment penalty n All Medicare beneficiaries (including those who are still working) must have creditable coverage to avoid the late enrollment penalty
Creditable Coverage n Coverage that is at least as good as Medicare Part D n Protects a beneficiary from the Part D penalty n Employer or retiree coverage, union coverage, VA coverage: Need proof of coverage to avoid penalty n Beneficiaries still working: • Benefits administrator has information about whether the employer coverage is creditable • Beneficiaries should be encouraged to ask the benefits administrator about their creditable coverage status if they have not been notified
Late Enrollment Penalty n Penalty is 1% of the national base beneficiary premium for EACH MONTH the beneficiary: • Did not enroll in a Medicare PDP when they were first eligible AND: Had no prescription drug coverage OR Ø Had coverage that was not considered “creditable” OR Ø Had a lapse in creditable coverage of 2 full months (63 days) Ø
Late Enrollment Penalty Example John enrolled in Original Medicare when he turned 65 but did not pick up Part D because he was not taking medication at the time. He is now 70 and enrolls in a Part D plan during open enrollment because his doctor prescribed him 2 medications. Upon enrolling in his Part D plan he was notified of the Late Enrollment Penalty (LEP) he must pay for failing to sign up when he was first eligible. n 5 years without coverage = 60 months n 1% of 2013 benchmark $31. 17 =. 31 n 60 months x. 31 = $18. 60 Monthly LEP Ø John is responsible to pay the LEP every month in addition to his regular Part D premium Ø This penalty increases slightly each year with the increase in the benchmark premium
Supplement 2 (aka Medex Gold) n Considered creditable coverage n No penalty if beneficiary eventually joins a Part D plan n Beneficiary can join during a Part D plan during the Open Enrollment Period or if they qualify for a Special Enrollment Period • Dis-enrolling from the plan is not in of itself a SEP
Extra Help / Limited Income Subsidy & Prescription Advantage
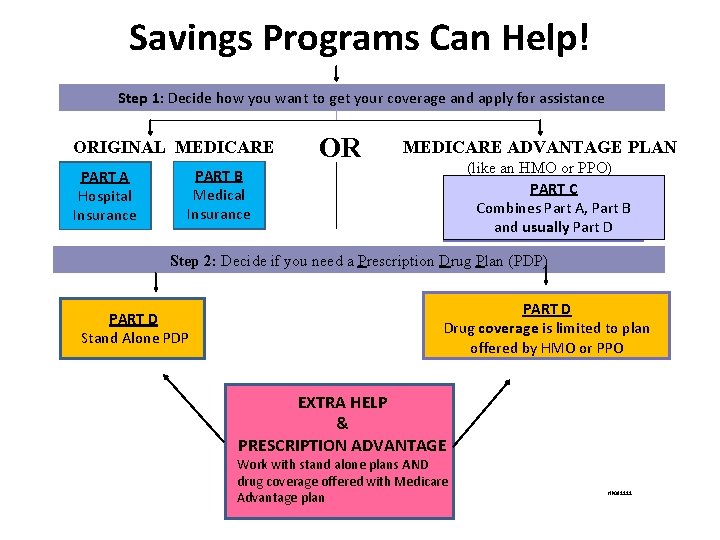
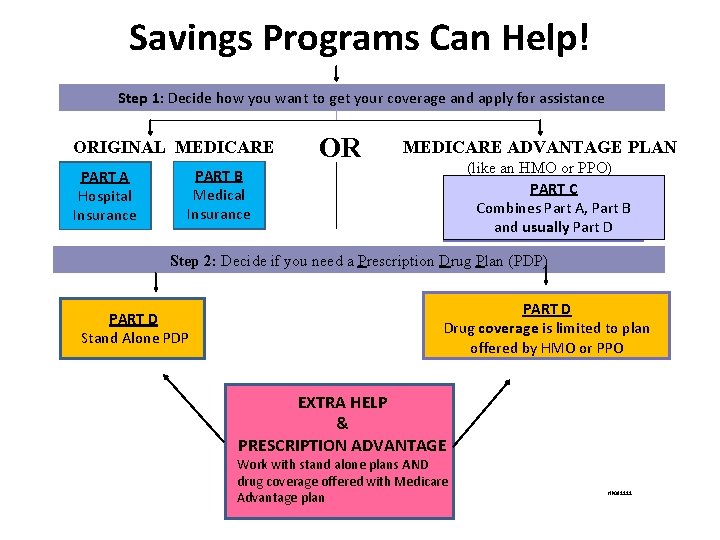
Savings Programs Can Help! Step 1: Decide how you want to get your coverage and apply for assistance ORIGINAL MEDICARE PART A Hospital Insurance OR MEDICARE ADVANTAGE PLAN (like an HMO or PPO) PART C Combines. CPart A, Part B and usually Part D PART B Medical Insurance Step 2: Decide if you need a Prescription Drug Plan (PDP) PART D Stand Alone PDP PART D Drug coverage is limited to plan offered by HMO or PPO EXTRA HELP & PRESCRIPTION ADVANTAGE Work with stand alone plans AND drug coverage offered with Medicare Advantage plan HP 081111
Extra Help/Low Income Subsidy (LIS) n Extra Help is a federal assistance program to help low-income and lowasset Medicare beneficiaries with costs related to Medicare Part D n Extra Help subsidizes: • Premiums • Deductibles • Co-payments • Coverage Gap “Donut Hole” • Late Enrollment Penalty n Does NOT subsidize non-formulary or excluded medications n Apply through Social Security Administration

2 Levels of Extra Help n Full Extra Help • 135% of the Federal Poverty Level (FPL) and asset limits • Full premium assistance with no deductible • Low, capped co-payments. Could be $0 for some generics at any level § Partial Extra Help • • • 150% of the FPL and asset limits Reduced premiums (sliding scale – between 25% -75% assistance dependent upon income) Reduced deductible and 15% copayments
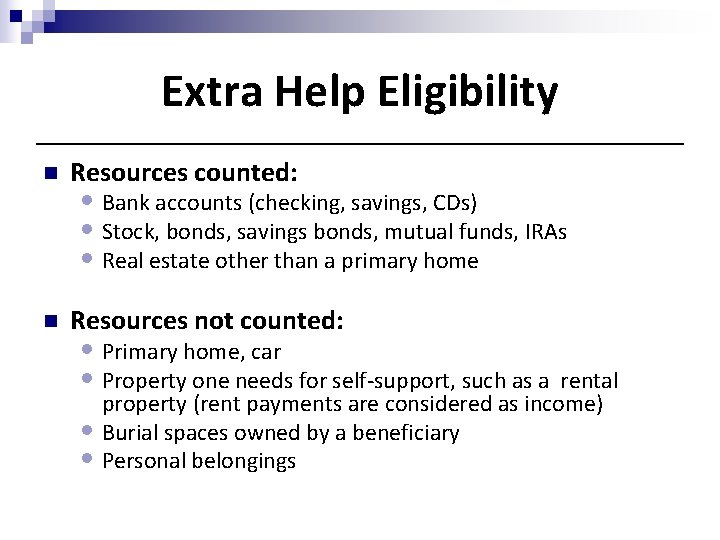
Extra Help Eligibility n Resources counted: n Resources not counted: • Bank accounts (checking, savings, CDs) • Stock, bonds, savings bonds, mutual funds, IRAs • Real estate other than a primary home • Primary home, car • Property one needs for self-support, such as a rental property (rent payments are considered as income) • Burial spaces owned by a beneficiary • Personal belongings
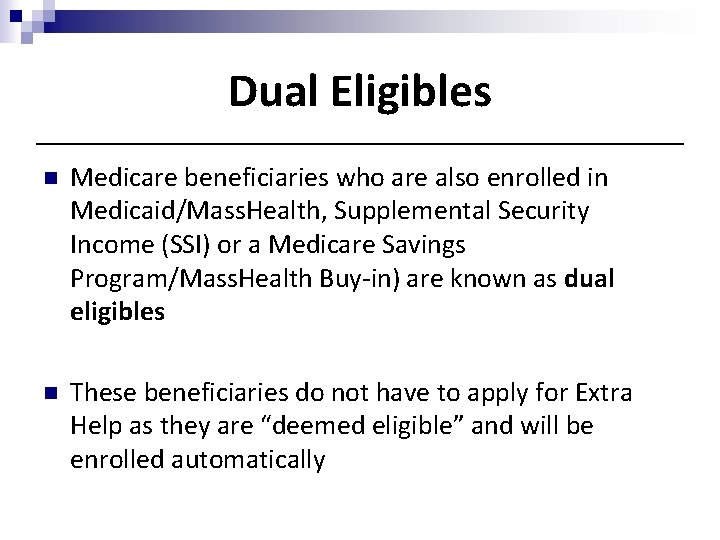
Dual Eligibles n Medicare beneficiaries who are also enrolled in Medicaid/Mass. Health, Supplemental Security Income (SSI) or a Medicare Savings Program/Mass. Health Buy-in) are known as dual eligibles n These beneficiaries do not have to apply for Extra Help as they are “deemed eligible” and will be enrolled automatically
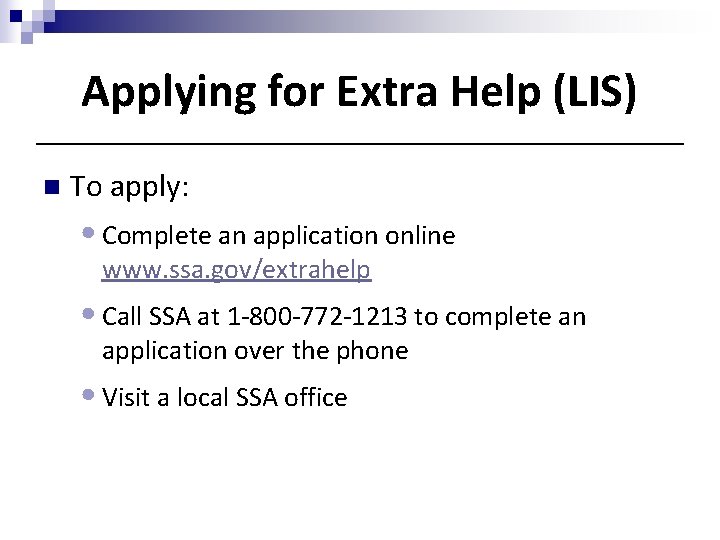
Applying for Extra Help (LIS) n To apply: • Complete an application online www. ssa. gov/extrahelp • Call SSA at 1 -800 -772 -1213 to complete an application over the phone • Visit a local SSA office
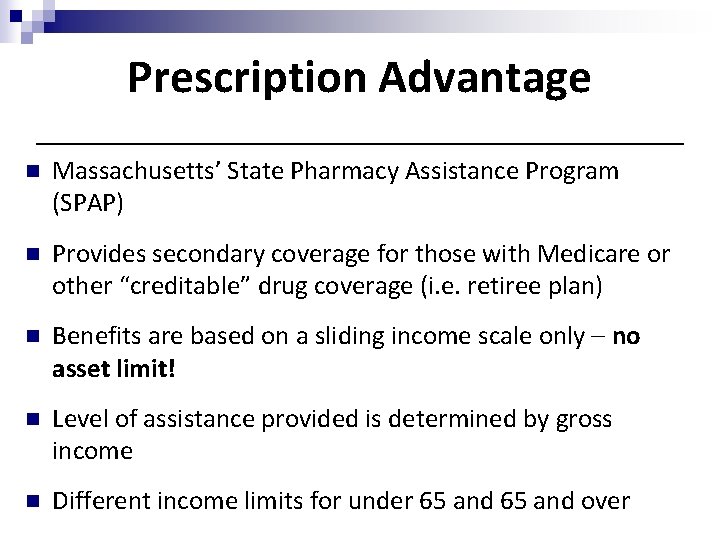
Prescription Advantage n Massachusetts’ State Pharmacy Assistance Program (SPAP) n Provides secondary coverage for those with Medicare or other “creditable” drug coverage (i. e. retiree plan) n Benefits are based on a sliding income scale only – no asset limit! n Level of assistance provided is determined by gross income n Different income limits for under 65 and over
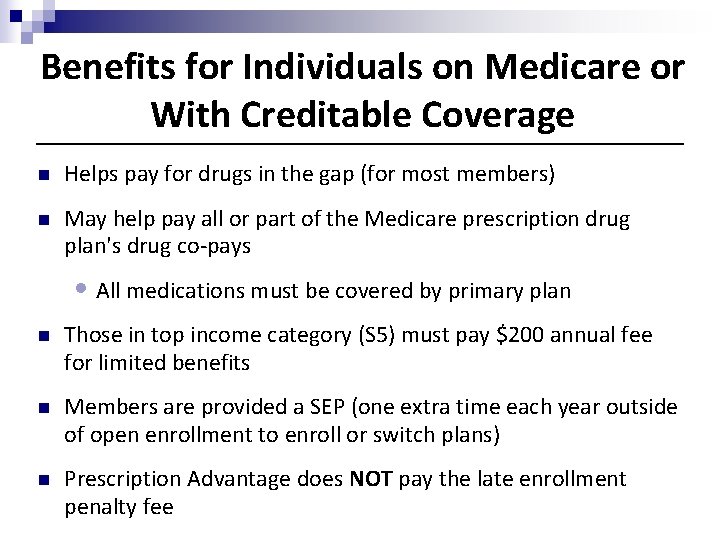
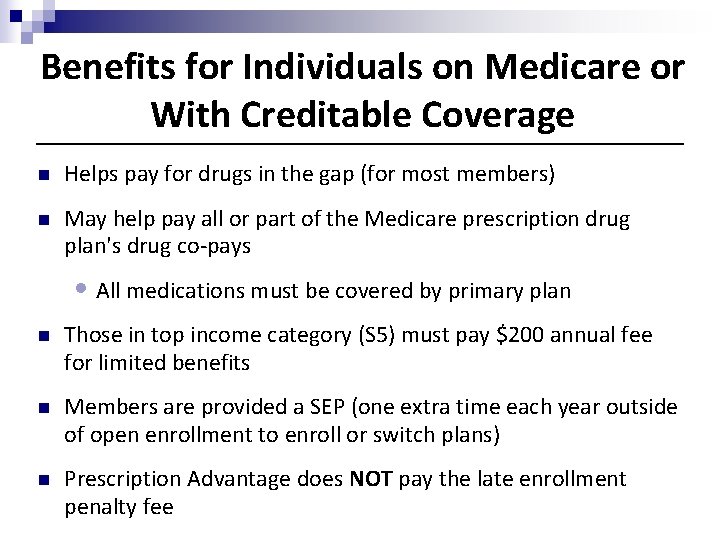
Benefits for Individuals on Medicare or With Creditable Coverage n Helps pay for drugs in the gap (for most members) n May help pay all or part of the Medicare prescription drug plan's drug co-pays • All medications must be covered by primary plan n Those in top income category (S 5) must pay $200 annual fee for limited benefits n Members are provided a SEP (one extra time each year outside of open enrollment to enroll or switch plans) n Prescription Advantage does NOT pay the late enrollment penalty fee
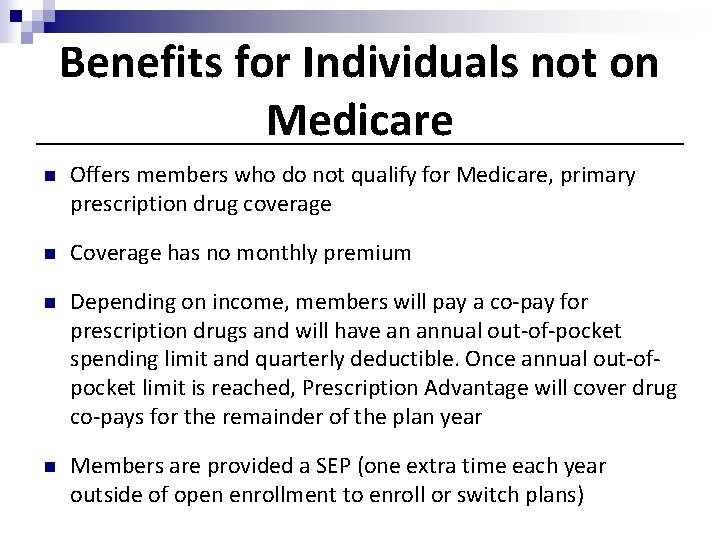
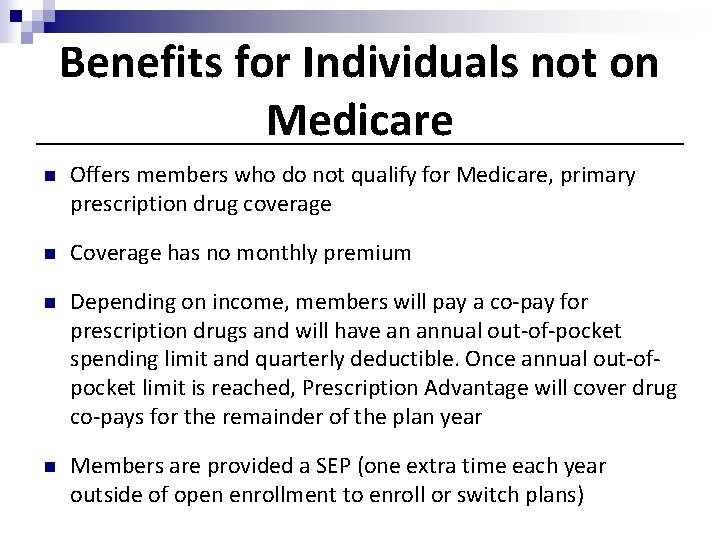
Benefits for Individuals not on Medicare n Offers members who do not qualify for Medicare, primary prescription drug coverage n Coverage has no monthly premium n Depending on income, members will pay a co-pay for prescription drugs and will have an annual out-of-pocket spending limit and quarterly deductible. Once annual out-ofpocket limit is reached, Prescription Advantage will cover drug co-pays for the remainder of the plan year n Members are provided a SEP (one extra time each year outside of open enrollment to enroll or switch plans)
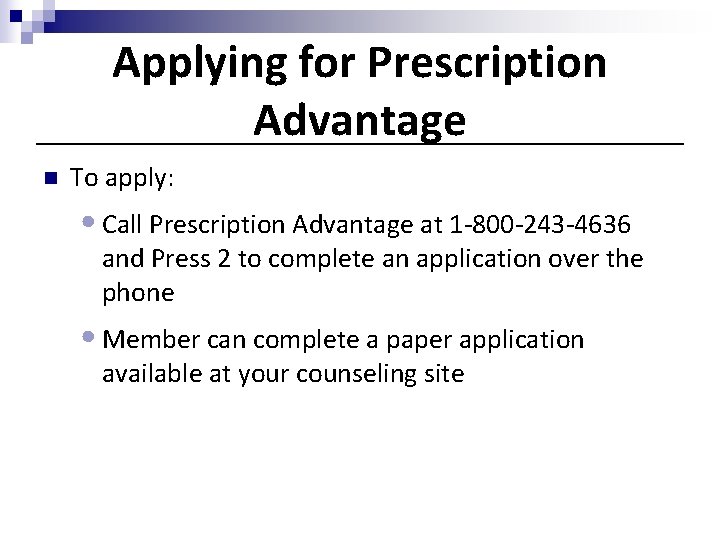
Applying for Prescription Advantage n To apply: • Call Prescription Advantage at 1 -800 -243 -4636 and Press 2 to complete an application over the phone • Member can complete a paper application available at your counseling site
Review § What is Medicare Part D and how is it offered? § Who is eligible? § What is creditable coverage? § How is the late enrollment penalty calculated? § When is the Open Enrollment Period? § When does the coverage gap or “donut hole” begin? § What programs are available to reduce drug costs?
Case Study 1: Phil Harmonic comes to see you in October because he needs help reviewing his drug plan for 2014. He tells you he enrolled in a Medicare Part D Plan when he turned 65. He currently takes generic medications and is in a low premium plan; however, his doctor recently informed him that he will be starting a brand name medication in January. Phil is worried that he may enter the donut hole in with this new medication but he’s not sure. He tells you he is single and has a gross monthly income of $1, 300. He also has $5, 000 in a checking account and owns a life insurance policy. n n What information will you need to assist Phil with a drug plan search? When is Phil able to change his drug plan? What would you tell Phil about the donut hole? What subsidy programs may Phil qualify for and how would he apply?
Case Study 2: Bart Ender Bart comes to see you during Medicare Open Enrollment. He is 70 years old, has Original Medicare, a Part D plan and tells you he just got a letter from Social Security informing him he’s been approved for Extra Help. Bart explains that he has been paying very high copays for several of his brand name medications this year and a friend of his helped him apply for Extra Help on the Social Security website. He mentions to you that he enrolled into Medicare Part D late and has also been paying a penalty. He wants to know how this Extra Help program will lower his costs. n n n How could you figure out what level of Extra Help Bart has? How would Extra Help reduce his drug costs? Would Extra Help pay his Late Enrollment Penalty? Now that Bart has Extra Help, how often can he change his Part D plan? How else would you assist Bart?
Case Study 3: Pat E. Cake meets with you on November 20 th. She says she belongs to a Medicare Advantage Plan (HMO). She tells you the prescription drug plan built into her Medicare Advantage plan costs more than she wants to pay, so she has decided to enroll in a Part D plan the offered to her by the agent she met at CVS. n n n What will happen if Pat enrolls in this Part D plan? If Pat wants to explore other Medicare coverage options how would you help her? If Pat makes a change to her coverage now, when will the change take effect?
Case Study 4: Lucy and Ricky come into the SHINE office on December 1 st. They want to know if there is still time to review their drug plan options for next year. They both have Medicare, a Medigap Supplement 1 Plan and a Part D plan. Ricky explains that Lucy was supposed to make an appointment to see the SHINE counselor weeks ago but forgot. In fact, she has been forgetting so much that the doctor has put her on a new brand name medication which is starting to help. Ricky explains that the only issue now is that the medication is very expensive. The couple’s monthly income is $3, 700/month and they have $50, 000 in assets. Lucy also wants to know why her new over the counter supplement “Vitameatavegamin” is not covered by Medicare Part D. n n Why should Lucy and Ricky review their drug plan for the next year? Do they still have time to make a change? Would they qualify for any assistance programs? Should Lucy’s OTC medication be covered?