Sexual health in primary care Dr Louise Knowles






- Slides: 84
Sexual health in primary care Dr Louise Knowles, GP. 12/12/16
Aims for today � STI trends � Sexual history taking/techniques � Management of common STI’s � Vaginal discharge
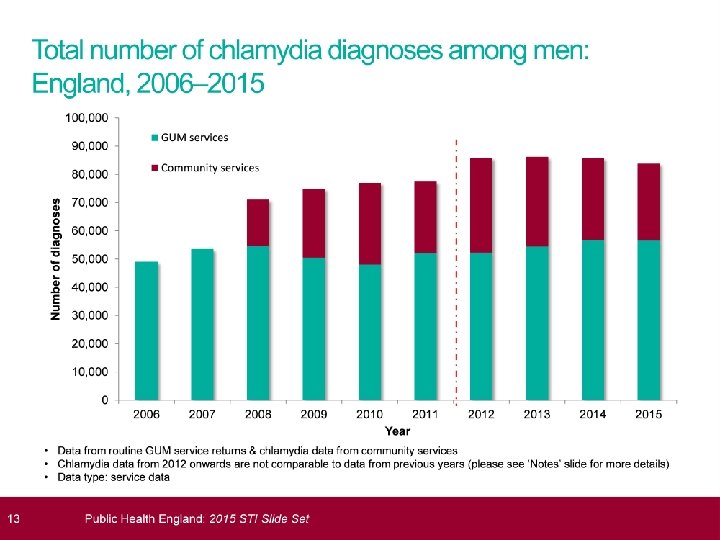
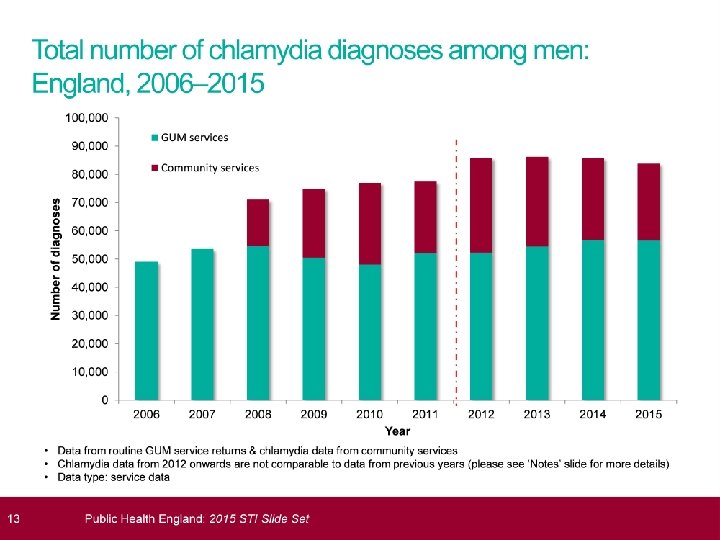
STI’s 2015; HPA data � 435, 000 diagnoses STI � Mainly heterosexuals<25 and MSM � Most common chlamydia; 200, 288 cases � Largest proportional increases in syphllis (20%increase) and gonorrhoea ( 11%increase) � Genital warts ( new) reduced by 7% � More than 1. 5 million chlamydia tests and 129, 100 cases. � Overall reduction in rate of chlamydia testing

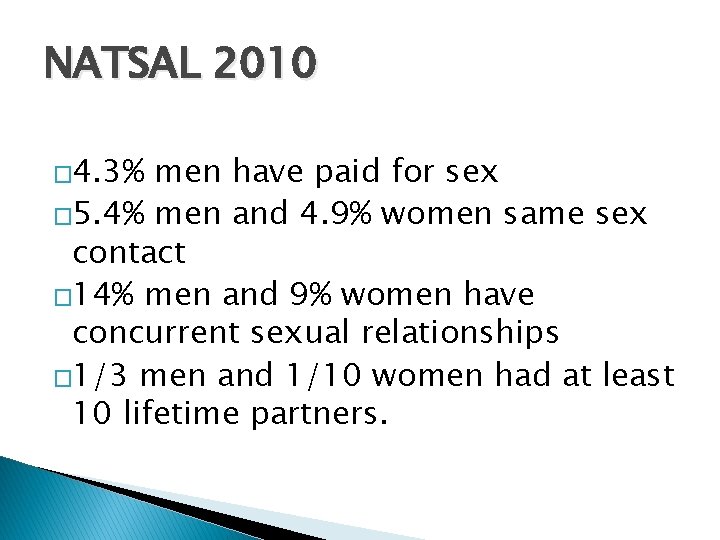
NATSAL 2010 � 4. 3% men have paid for sex � 5. 4% men and 4. 9% women same sex contact � 14% men and 9% women have concurrent sexual relationships � 1/3 men and 1/10 women had at least 10 lifetime partners.
What is sexual health care? �Risk assessment �STI; prevention, diagnosis, treatment �Contraception �Management of unplanned pregnancy.
Setting the scene �You are running 20 minutes behind �Just moved from 15 to 10 minute appointments �Your nurse is off sick �“while I’m here. . . ”
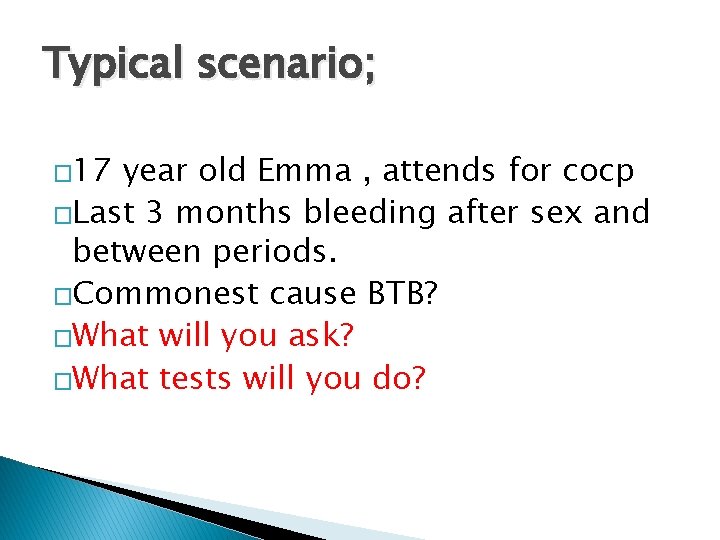
Typical scenario; � 17 year old Emma , attends for cocp �Last 3 months bleeding after sex and between periods. �Commonest cause BTB? �What will you ask? �What tests will you do?
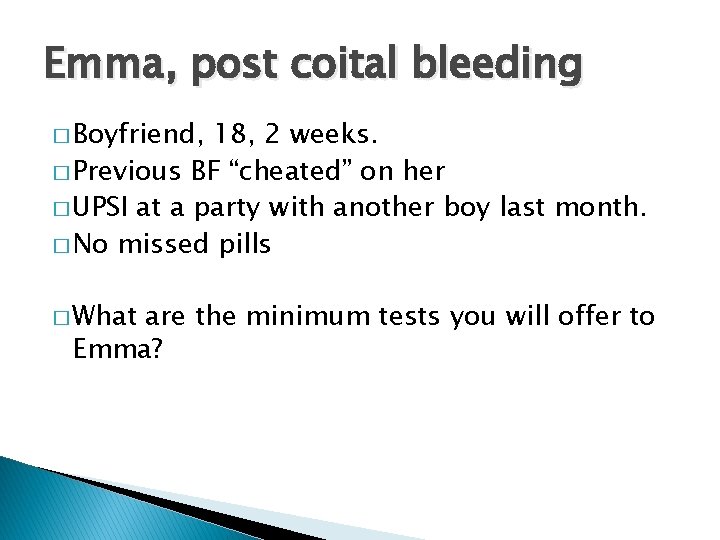
Emma, post coital bleeding � Boyfriend, 18, 2 weeks. � Previous BF “cheated” on her � UPSI at a party with another boy last month. � No missed pills � What are the minimum tests you will offer to Emma?
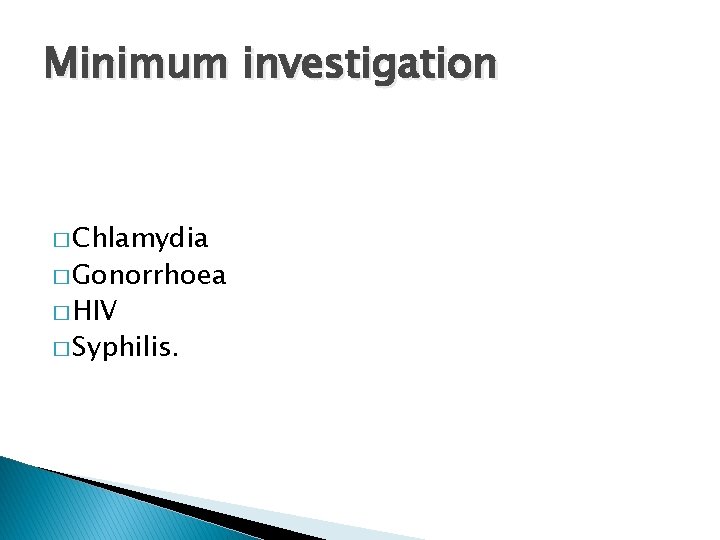
Minimum investigation � Chlamydia � Gonorrhoea � HIV � Syphilis.
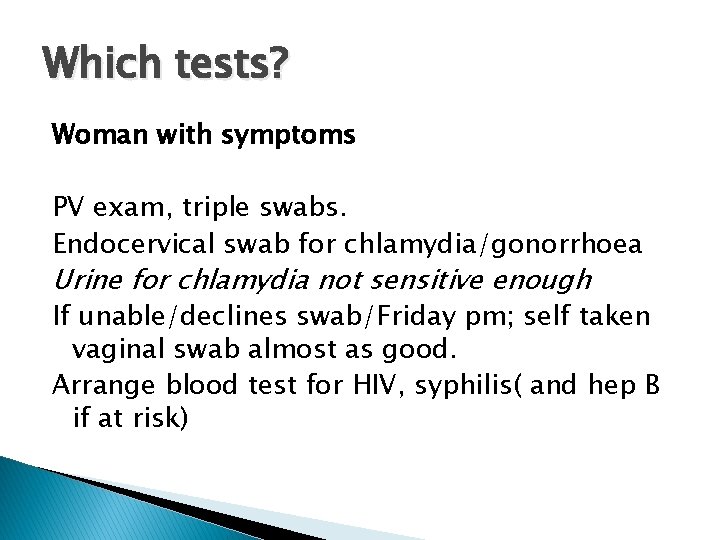
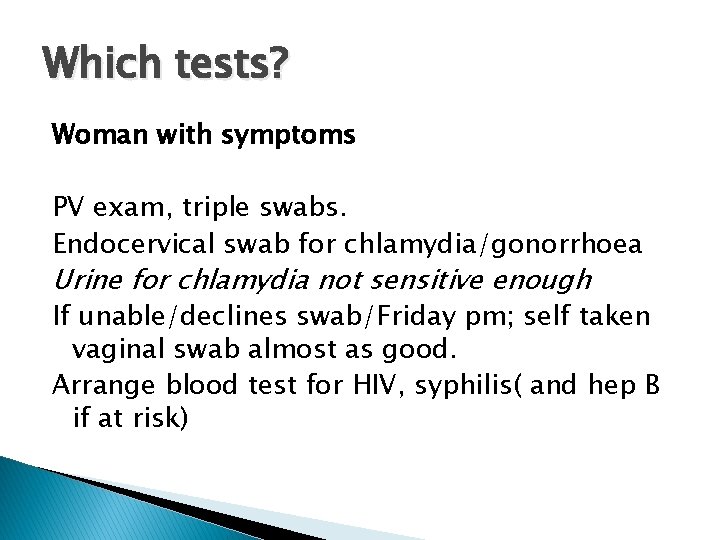
Which tests? Woman with symptoms PV exam, triple swabs. Endocervical swab for chlamydia/gonorrhoea Urine for chlamydia not sensitive enough If unable/declines swab/Friday pm; self taken vaginal swab almost as good. Arrange blood test for HIV, syphilis( and hep B if at risk)
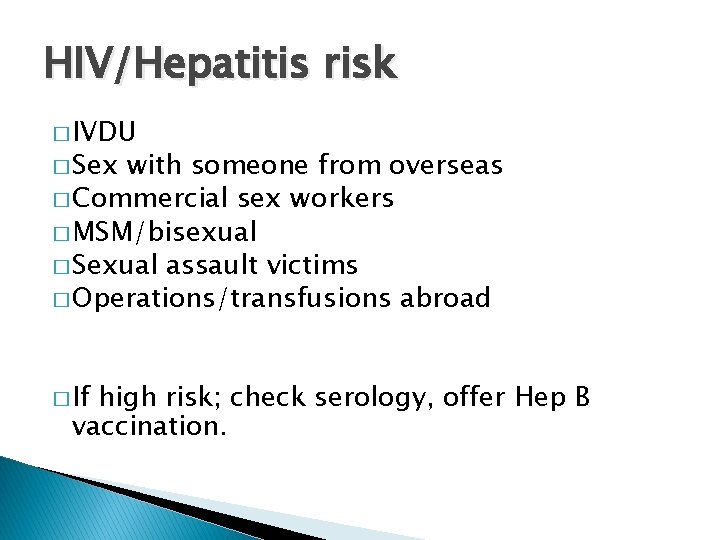
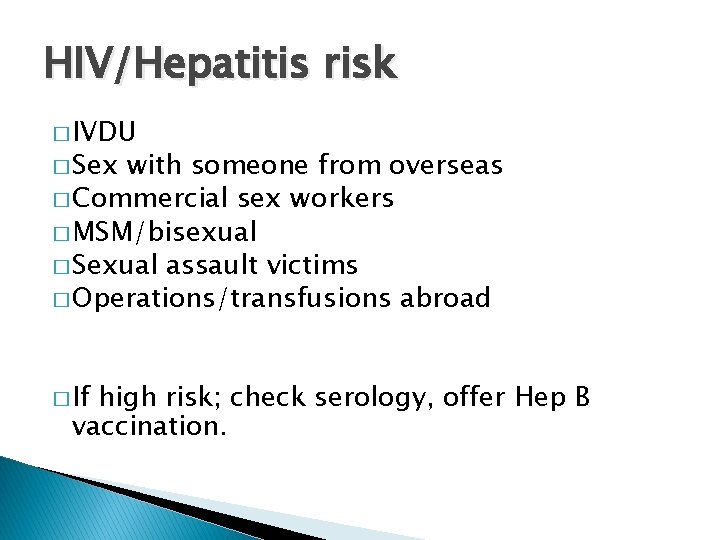
HIV/Hepatitis risk � IVDU � Sex with someone from overseas � Commercial sex workers � MSM/bisexual � Sexual assault victims � Operations/transfusions abroad � If high risk; check serology, offer Hep B vaccination.
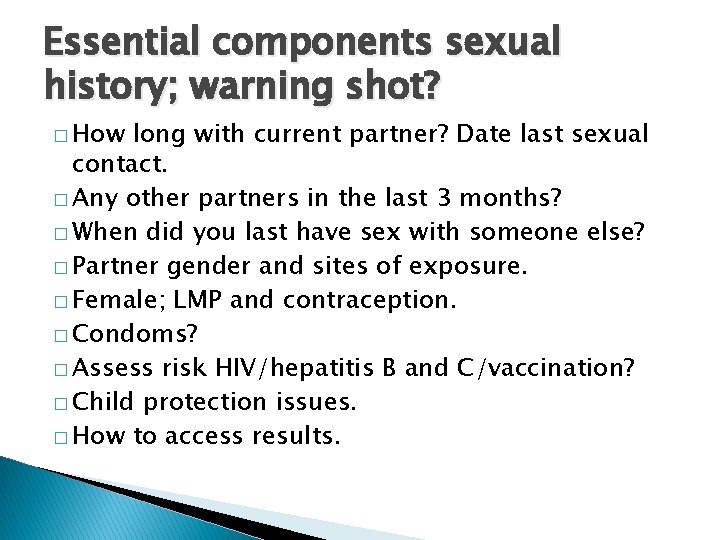
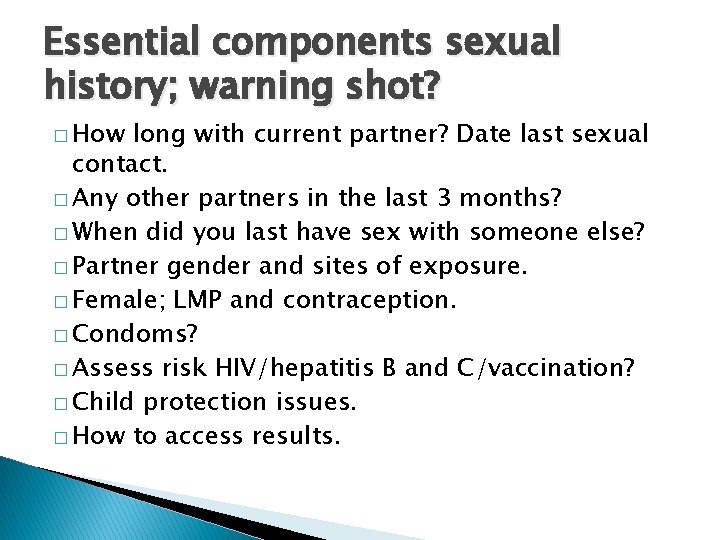
Essential components sexual history; warning shot? � How long with current partner? Date last sexual contact. � Any other partners in the last 3 months? � When did you last have sex with someone else? � Partner gender and sites of exposure. � Female; LMP and contraception. � Condoms? � Assess risk HIV/hepatitis B and C/vaccination? � Child protection issues. � How to access results.
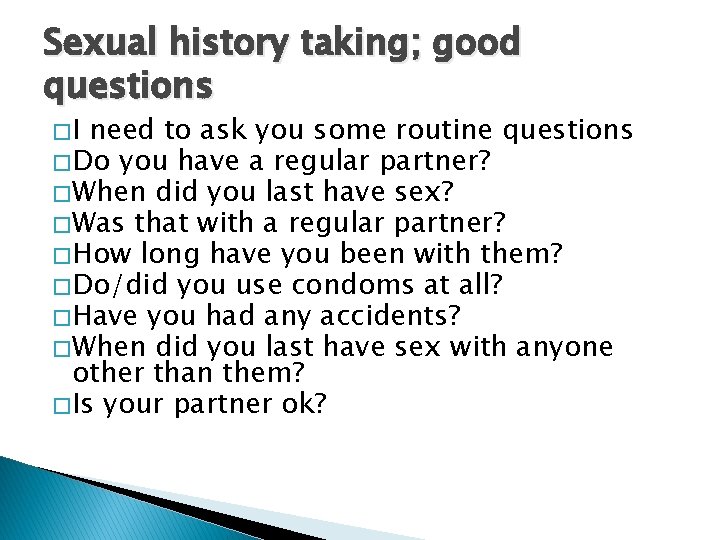
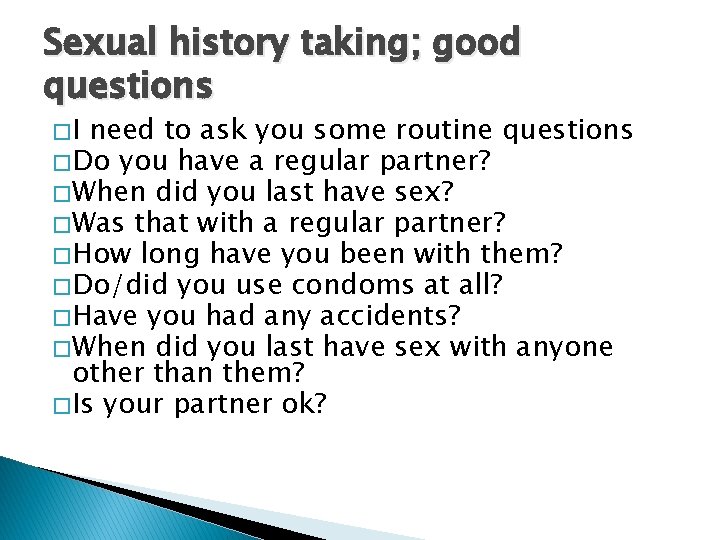
Sexual history taking; good questions �I need to ask you some routine questions � Do you have a regular partner? � When did you last have sex? � Was that with a regular partner? � How long have you been with them? � Do/did you use condoms at all? � Have you had any accidents? � When did you last have sex with anyone other than them? � Is your partner ok?
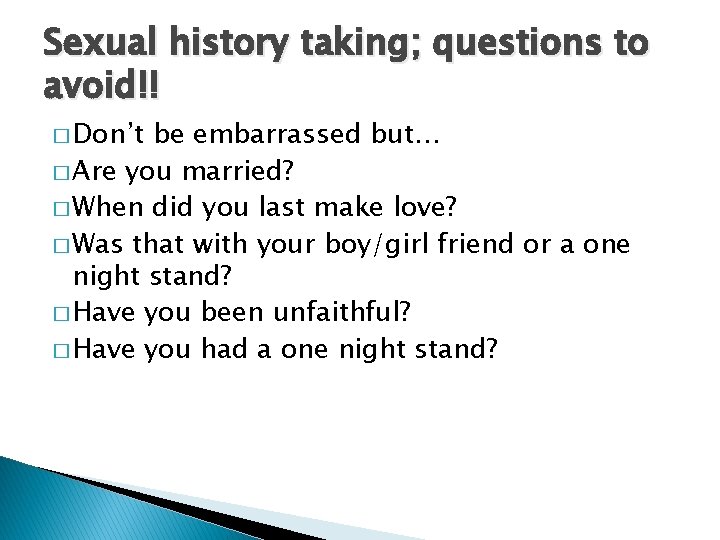
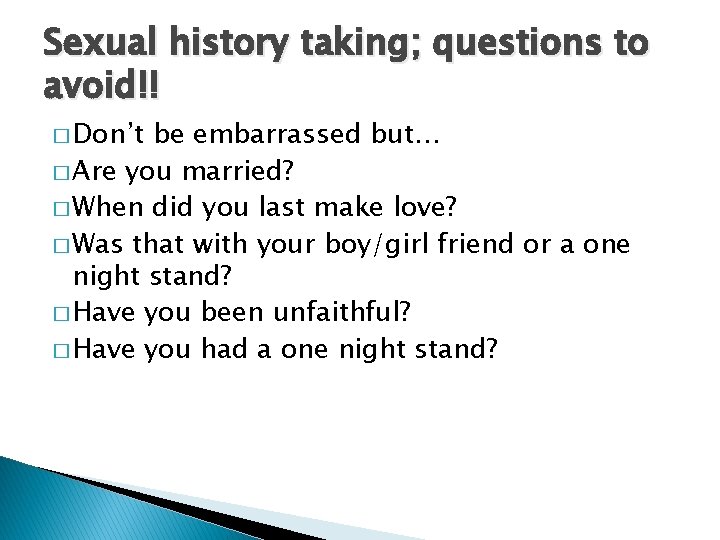
Sexual history taking; questions to avoid!! � Don’t be embarrassed but… � Are you married? � When did you last make love? � Was that with your boy/girl friend or a one night stand? � Have you been unfaithful? � Have you had a one night stand?
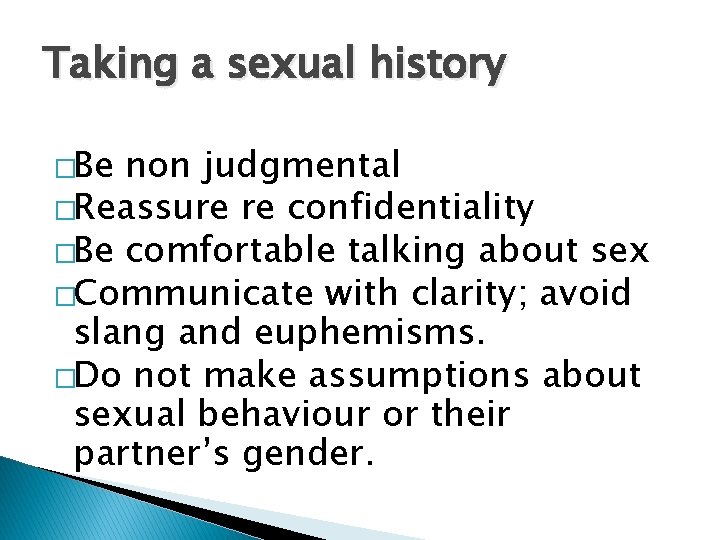
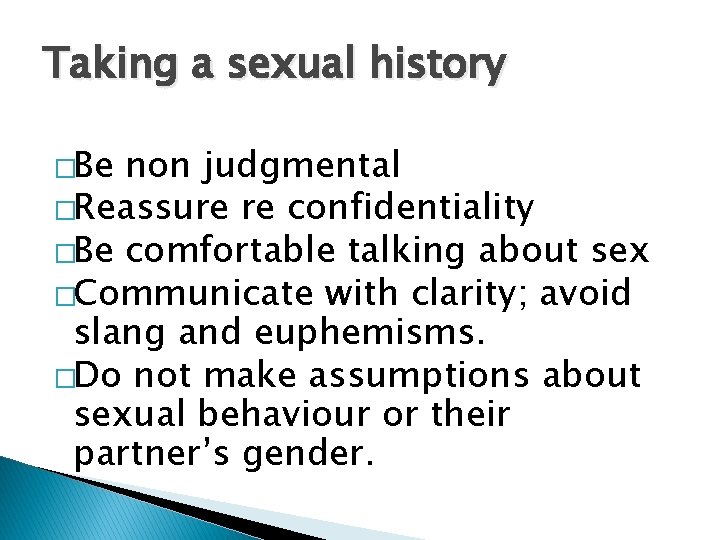
Taking a sexual history �Be non judgmental �Reassure re confidentiality �Be comfortable talking about sex �Communicate with clarity; avoid slang and euphemisms. �Do not make assumptions about sexual behaviour or their partner’s gender.
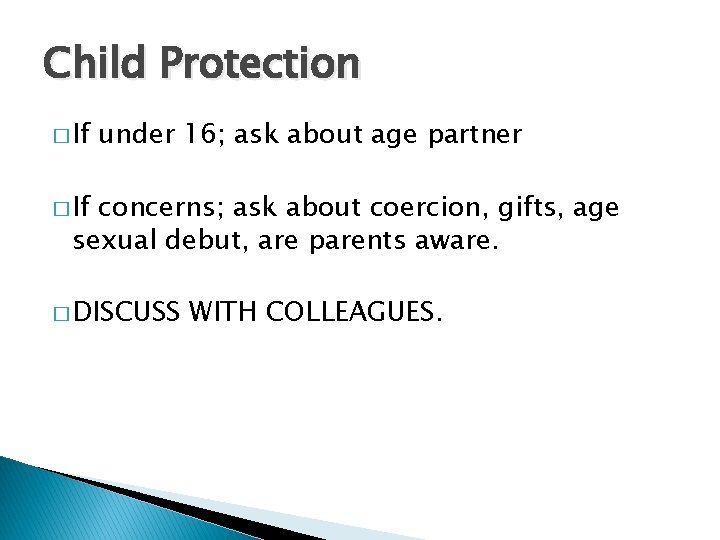
Child Protection � If under 16; ask about age partner � If concerns; ask about coercion, gifts, age sexual debut, are parents aware. � DISCUSS WITH COLLEAGUES.
Men with symptoms. �John 18 , presents Friday pm with a tender swollen testicle. �What are you going to ask?
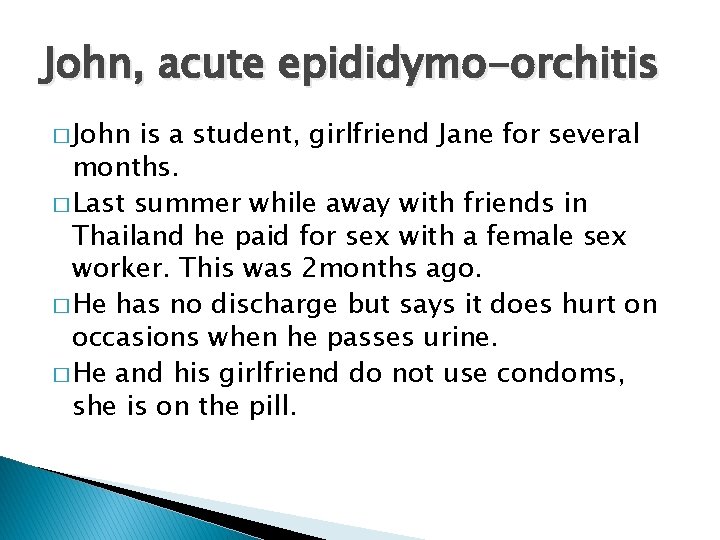
John, acute epididymo-orchitis � John is a student, girlfriend Jane for several months. � Last summer while away with friends in Thailand he paid for sex with a female sex worker. This was 2 months ago. � He has no discharge but says it does hurt on occasions when he passes urine. � He and his girlfriend do not use condoms, she is on the pill.
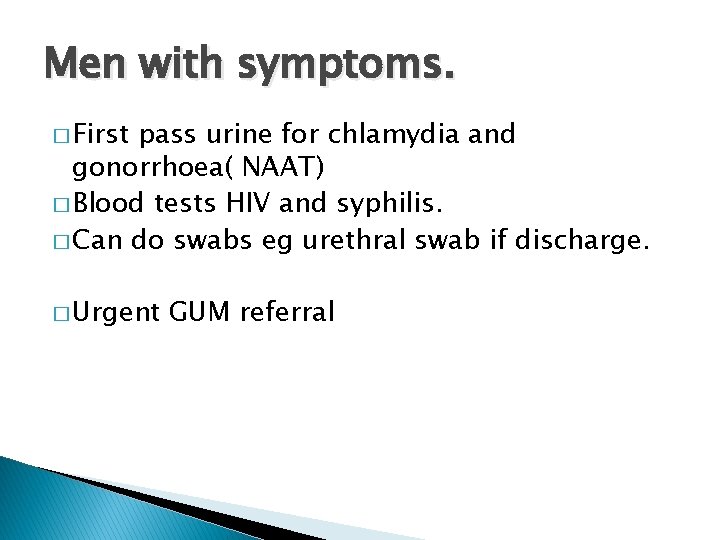
Men with symptoms. � First pass urine for chlamydia and gonorrhoea( NAAT) � Blood tests HIV and syphilis. � Can do swabs eg urethral swab if discharge. � Urgent GUM referral
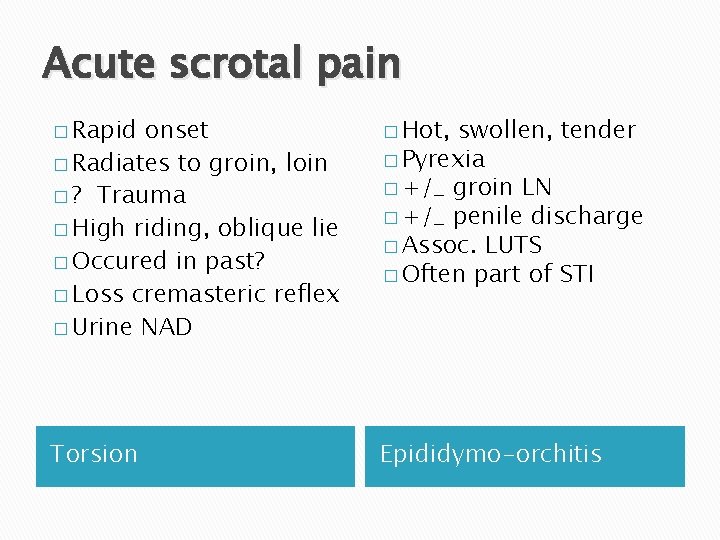
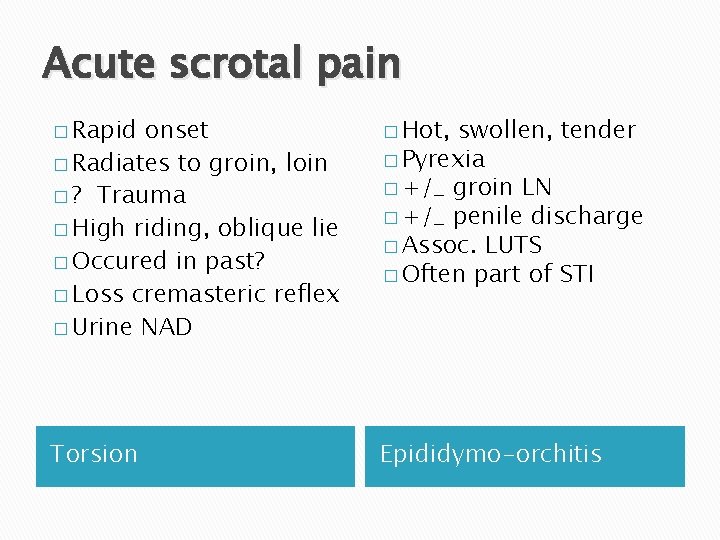
Acute scrotal pain � Rapid onset � Radiates to groin, loin � ? Trauma � High riding, oblique lie � Occured in past? � Loss cremasteric reflex � Urine NAD � Hot, swollen, tender � Pyrexia � +/_ groin LN � +/_ penile discharge � Assoc. LUTS � Often part of STI Torsion Epididymo-orchitis
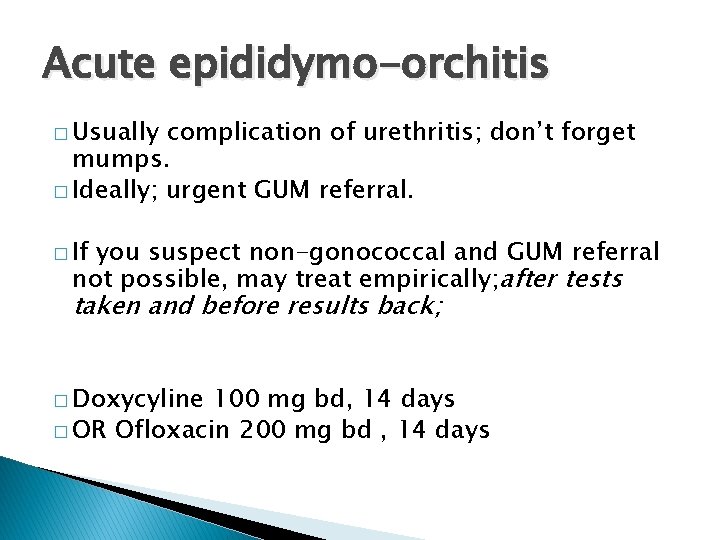
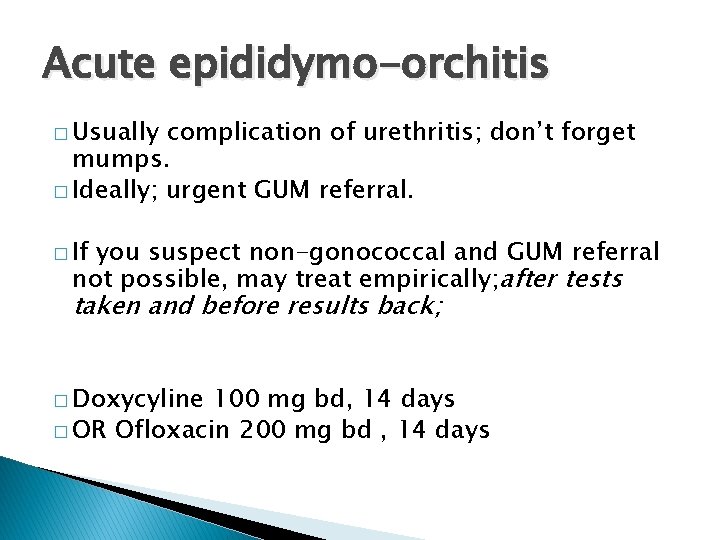
Acute epididymo-orchitis � Usually complication of urethritis; don’t forget mumps. � Ideally; urgent GUM referral. � If you suspect non-gonococcal and GUM referral not possible, may treat empirically; after tests taken and before results back; � Doxycyline 100 mg bd, 14 days � OR Ofloxacin 200 mg bd , 14 days
Why refer GUM? � Partner notification � More rapid diagnosis � Culture and senstivity needed for gonorrhoea � Counsellors and support service. � Gonorrhoea; complex; treatment includes injection � Gold standard tests. � Uncertainty about diagnosis � Free treatment


Common STI’s � Many opportunities � High index suspicion in under 25’s � Basic knowledge of how may present. � Reservoir of asymptomatic infection! � Have procedures in place for initial investigation. � Be aware of onward path referral/partner notification.
Don’t forget… � Agree how you are going to communicate results. � Ensure up to date mobile number.
Common STI’s � Chlamydia � Genital warts � Genital herpes � Trichomoniasis � Gonorrhoea � (HIV)
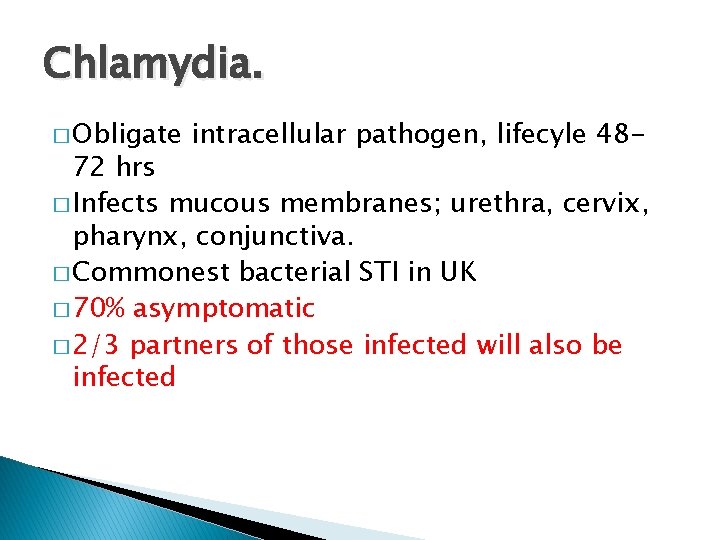
Chlamydia. � Obligate intracellular pathogen, lifecyle 48 - 72 hrs � Infects mucous membranes; urethra, cervix, pharynx, conjunctiva. � Commonest bacterial STI in UK � 70% asymptomatic � 2/3 partners of those infected will also be infected

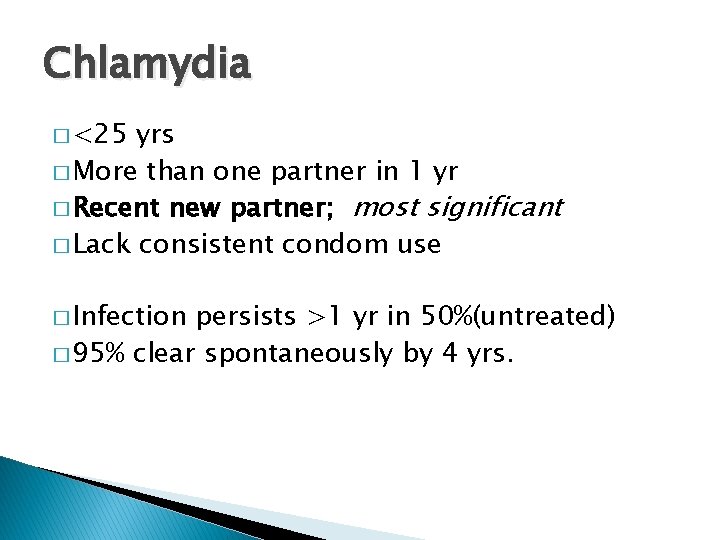
Chlamydia � <25 yrs � More than one partner in 1 yr � Recent new partner; most significant � Lack consistent condom use � Infection persists >1 yr in 50%(untreated) � 95% clear spontaneously by 4 yrs.
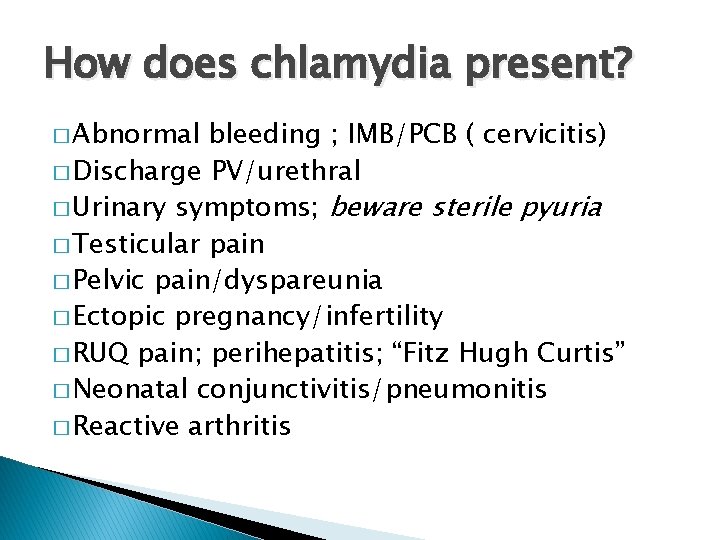
How does chlamydia present? � Abnormal bleeding ; IMB/PCB ( cervicitis) � Discharge PV/urethral � Urinary symptoms; beware sterile pyuria � Testicular pain � Pelvic pain/dyspareunia � Ectopic pregnancy/infertility � RUQ pain; perihepatitis; “Fitz Hugh Curtis” � Neonatal conjunctivitis/pneumonitis � Reactive arthritis
Chlamydia testing � Opportunistic screening…. NCSP � TOP � Change partner; suggest 2 week time window
Which test? ~women � Symptomatic; endocervical swab 360 degrees in cervical os. (NAAT) � Or if not possible; self taken vulvovaginal swab has good sensitivity � Self taken swab; 2 inches inside vagina, rotate for 30 secs. . . BASHH guidelines. � NAAT samples can be tested several days later
Which test; men � First pass urine( hold for one hour) � Urethral swab? � Look back period; 4 w for acute urethritis, 6 m for other presentations.
Chlamydia positive � Need full STI screen � Will need GUM referral for partner notification � Document reasons for this. Treatment; Azithromycin 1 G stat or Doxycyline 100 mg bd 7/7 IUD in situ; no need to remove
Chlamydia in pregnancy � BNF suggest avoiding azithromycin but no evidence harm; off licence � Can use erythromycin 500 mg bd 10 -14 d. or ofloxacin 200 mg bd 7 d. � SIGN recommends use of azithro for pragmatic reasons; compliance. � Test of cure recommended
NO SEX FOR 7 DAYS AFTER STAT DOSE.
Genital herpes � Most infection acquired without symptoms � 80% UNAWARE they are infected � HSV 1 and 2 oral and genital � Infection is LIFELONG � Primary attack may be many months after exposure. � Increasing numbers first episodes; change sexual behaviour and use highly sensitive diagnostic tests.
Genital herpes �Primary infection; malaise, flu like symptoms, tingling sacral dermatomes �Tender inguinal LN �Dysuria and blister; 3 weeks �The “dripping tap”
Genital herpes � Inv; � HSV � Rx. � � viral swab ( NAAT); 71% detection culture will miss 30% Saline bathing Oral antiviral Lidocaine ointment 5% � Follow up; full STI screen 2 -3 w later.
Episodic treatment HSV � No advantage between different antivirals. � Consider short course treatment ( more cost effective/better compliance) BASHH � Rx Aciclovir 800 mg tds 2/7 � ( Aciclovir 200 mg 5 times daily 5/7) � Patient intiated treatment
Recurrent genital herpes �Prodromal symptoms �Less severe �Start with prodrome �Average recurrence higher with HSV 2 �Can consider suppressive therapy. �eg aciclovir 400 mg bd.
Points you should cover; HSV � Abstain during prodrome/lesions � Asymptomatic viral shedding � Male condoms reduce risk transmission � Disclosure advised. � Document these discussions.
Genital herpes � Partner notification? � BASHH statement of criminal prosecution 2011. ( Golding) � UK: COURT OF APPEAL UPHOLDS MAN’S CONVICTION FOR RECKLESSLY PASSING ON GENITAL HERPES DURING SEX WITH EXGIRLFRIEND
Pregnancy and HSV � Primary infection higher risk � Refer GUM � Rare but catastrophic neonatal infection � Aciclovir may be given from 36 weeks � Aim for vaginal delivery if no vulval lesions at labour.
Psychological distress+++ � When did I catch this? � Will my partner get warts? � Does it mean I will get cervical cancer? � Should I have more frequent smears? � How can I get rid of it? � Will it come back? � Can I be cured?
Genital warts; the facts � HPV 6 and 11 � CIN 16 and 18 � Head and neck cancers 16 � 30 -50% sexually active adults have postive serology for genital HPV � Sexual transmission; digital or oro-genital � Most commonly in areas of abrasion but CAN OCCUR ANYWHERE.
Warts are just cosmetic. � There is often a long latent period before wart appears � Most infection is sub-clinical � <10% of those infected get lesions � HPV DNA no longer detectable in 95% by 2 yrs post infection. � Worse in smoker, pregnancy, immunosuppressed. � Don’t assume perianal warts due to anal intercourse.
Genital warts; treatment �None �Destruction ( cryo) �Anti-mitotic ( Podophyllotoxin) �Immune modfication ( Imiquimod) �Surgery
Warts; refer GUM? � Podophyllotoxin, cream or solution � Apply bd for 3 days, 4 day break, up to 4 courses � Imiquimod; apply nightly 3 nights per week for up to 16 weeks. � No partner notification , screen other STD’s
Gonorrhoea; who? � Urban areas � Young adults � MSM � Black/ethinic minority populations � Partners of the above!


Gonorrhoea. � Infects mucous membranes, oropharynx, rectum, urethra, conjunctivae. � Enhances transmission HIV � Test no less than 3 days after contact; convention is to test 14 d after for GC and chlamydia � Which test?
Testing for gonorrhoea � Endocervical/self taken swab for culture; minimal delay to lab � NAAT’s more sensitive, less invasive. ( can be done on first pass urine men, self taken HVS women) � If NAAT positive always need swabs for culture for sensitivities. � GUM referral!
Gonorrhoea resistance. � Outbreak high level azithromycin resistant cases originated in Leeds, heterosexuals. � 17 cases so far this yr, spreading into MSM population � First case in 2016 of dual resistance to azithromycin/ceftriax one
Treatment of gonorrhoea � REFER GUM � Testing required to test sensitivity. � Treatment is with IM ceftriaxone and oral azithromycin, both as stat dose. � Not a role for primary care!
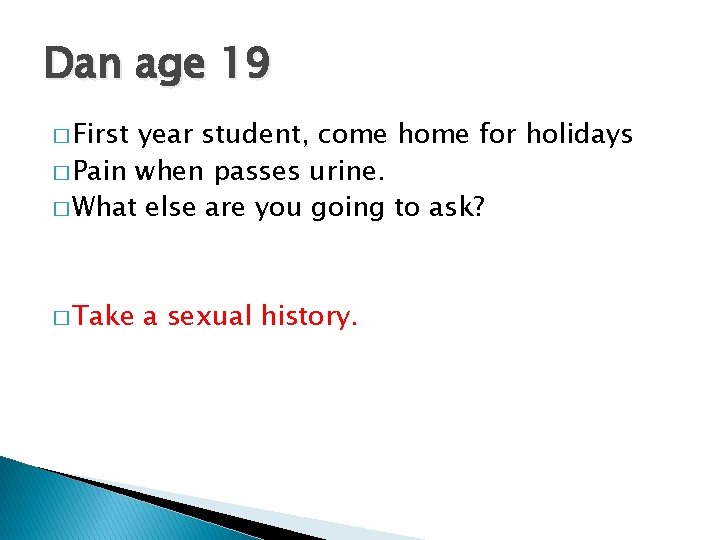
Dan age 19 � First year student, come home for holidays � Pain when passes urine. � What else are you going to ask? � Take a sexual history.
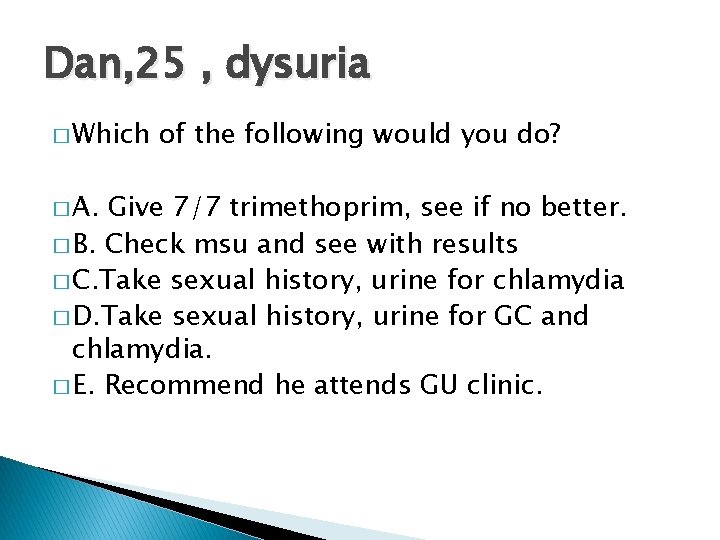
Dan, 25 , dysuria � Which � A. of the following would you do? Give 7/7 trimethoprim, see if no better. � B. Check msu and see with results � C. Take sexual history, urine for chlamydia � D. Take sexual history, urine for GC and chlamydia. � E. Recommend he attends GU clinic.
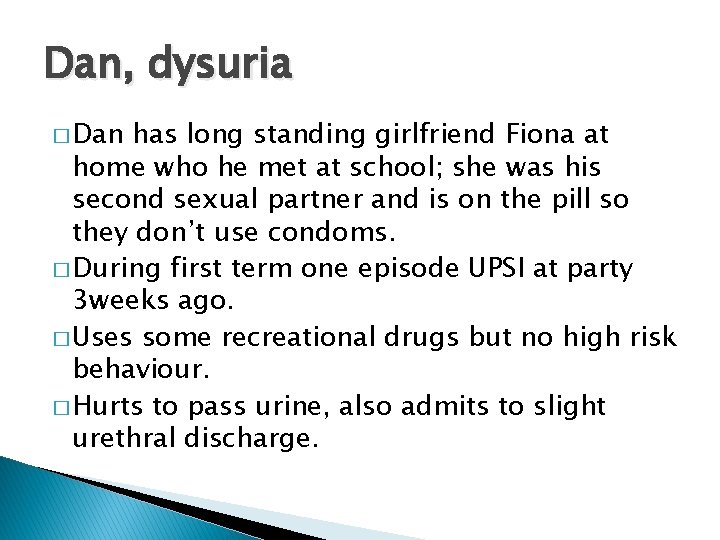
Dan, dysuria � Dan has long standing girlfriend Fiona at home who he met at school; she was his second sexual partner and is on the pill so they don’t use condoms. � During first term one episode UPSI at party 3 weeks ago. � Uses some recreational drugs but no high risk behaviour. � Hurts to pass urine, also admits to slight urethral discharge.
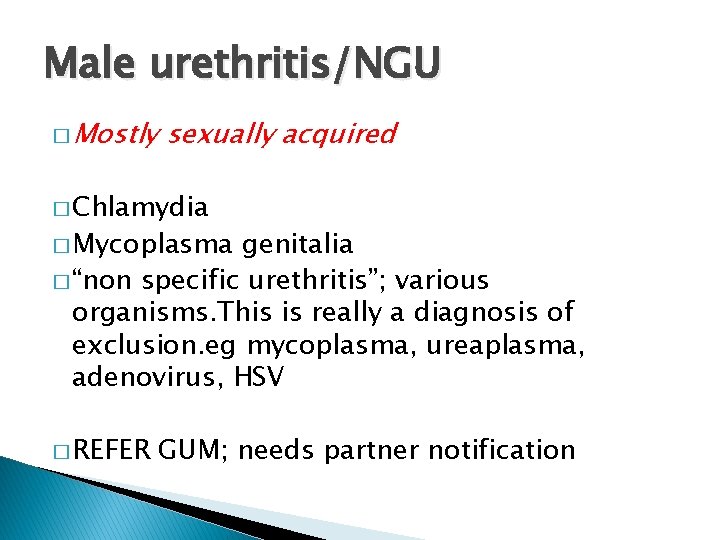
Male urethritis/NGU � Mostly sexually acquired � Chlamydia � Mycoplasma genitalia � “non specific urethritis”; various organisms. This is really a diagnosis of exclusion. eg mycoplasma, ureaplasma, adenovirus, HSV � REFER GUM; needs partner notification
Suspected chlamydia/GC/NSU � “syndromic” treatment; ie without tests, not recommended � “empirical “ treatment( ie treatment at time of consultation, before test results); may be appropriate, eg Friday pm, where investigation is declined or not possible. Don’t forget treatment for partners!
Vaginal discharge �Physiological �Commensals; candida, staph aureus, group B strep; can “overgrow” �Consider non infective causes �Eg. Foreign body, cervical ectopy, endometrial polyps, malignancy.
Infective causes Sexually transmitted Chlamydia Gonorrhoea Trichomonas HSV Non sexually transmitted Bacterial vaginosis Candida
Vaginal discharge; history. � Type of discharge. � Any itch or malodour? � What treatment tried otc? � Any symptoms to suggests PID? � Take a sensitive sexual history. � Symptoms or recent treatment for partner. � PMH � Cyclical symptoms?
Trichomonas � Infects vagina, urethra, under foreskin � Invariably sexually transmitted � Both sexes; 50% asymptomatic � Symptoms; discharge, dysuria, itch++ � Comps; preterm delivery, low birth weight � Enhances HIV transmission
Trichomonas � If you suspect it; refer GUM � If you find it; treat and refer for PN � Treatment; metronidazole 2 G stat/400 mg bd 5 -7 days. � Partners should be screened for all STI’s and treated for TV regardless of results.
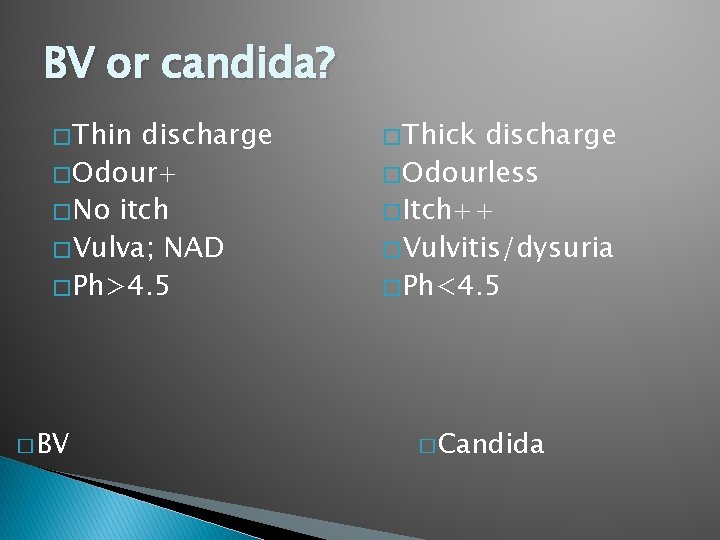
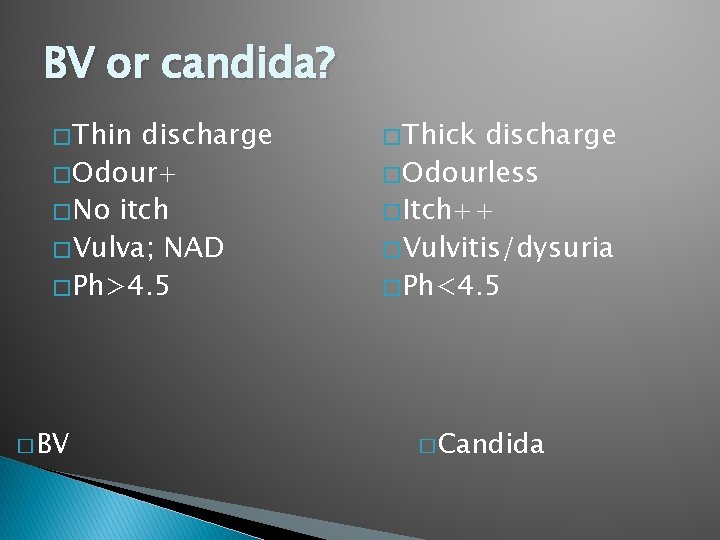
BV or candida? � Thin discharge � Odour+ � No itch � Vulva; NAD � Ph>4. 5 � BV � Thick discharge � Odourless � Itch++ � Vulvitis/dysuria � Ph<4. 5 � Candida
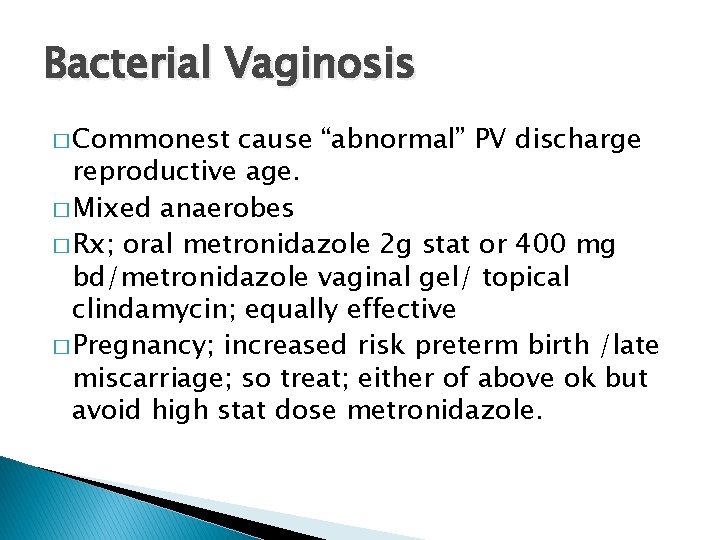
Bacterial Vaginosis � Commonest cause “abnormal” PV discharge reproductive age. � Mixed anaerobes � Rx; oral metronidazole 2 g stat or 400 mg bd/metronidazole vaginal gel/ topical clindamycin; equally effective � Pregnancy; increased risk preterm birth /late miscarriage; so treat; either of above ok but avoid high stat dose metronidazole.
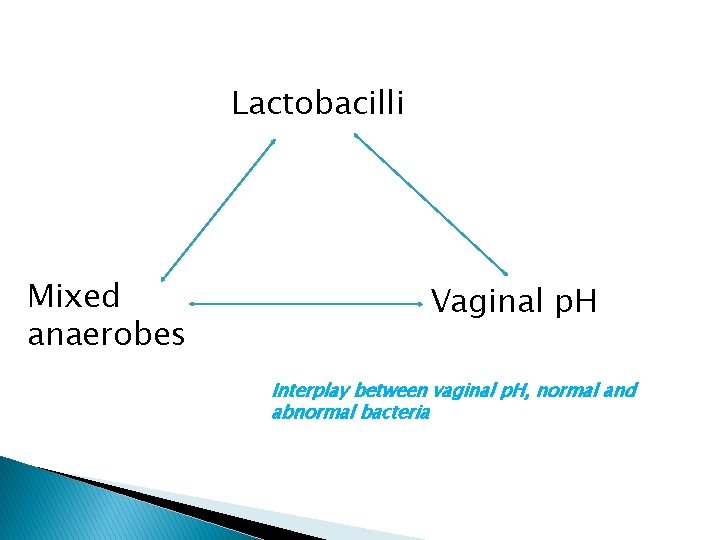
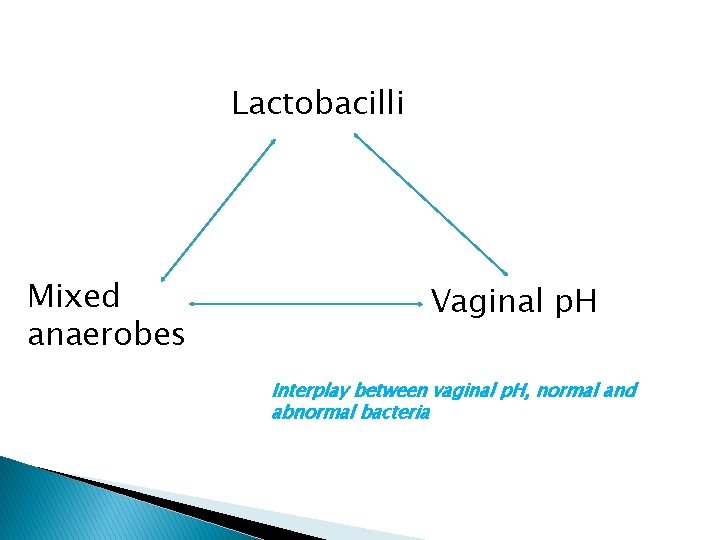
Lactobacilli Mixed anaerobes Vaginal p. H Interplay between vaginal p. H, normal and abnormal bacteria
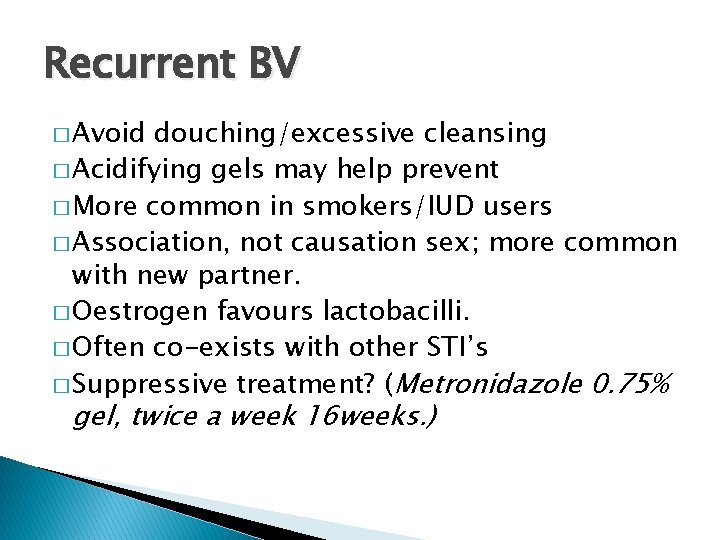
Recurrent BV � Avoid douching/excessive cleansing � Acidifying gels may help prevent � More common in smokers/IUD users � Association, not causation sex; more common with new partner. � Oestrogen favours lactobacilli. � Often co-exists with other STI’s � Suppressive treatment? (Metronidazole 0. 75% gel, twice a week 16 weeks. )
Recurrent candida; myths � Do not arise from re-infection by partner � No evidence for pro-biotics, natural yoghurt or special yeast free diets! � Believe negative swabs! � Asking for culture may yield non albicans.
Pathogenesis recurrent VVC � Some women have aggravated inflammatory response; genetic predisposition; atopic? � Minimal plaques but lots of inflammation v obvious candida plaques but minimal symptoms. � Topical skin care essential
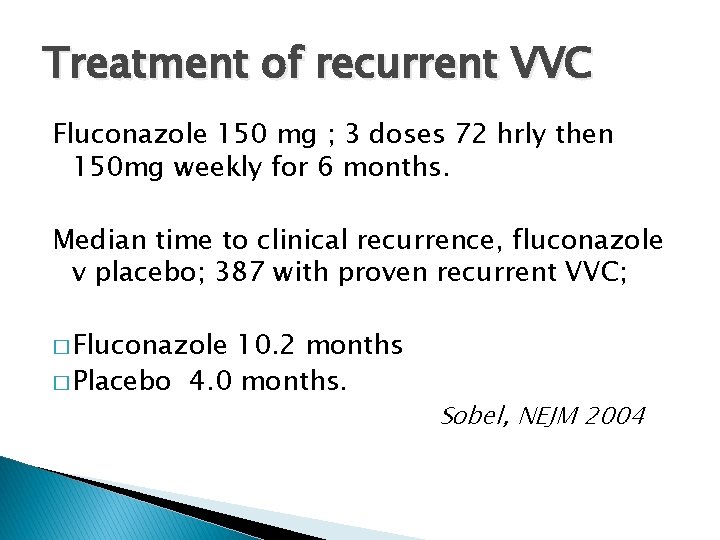
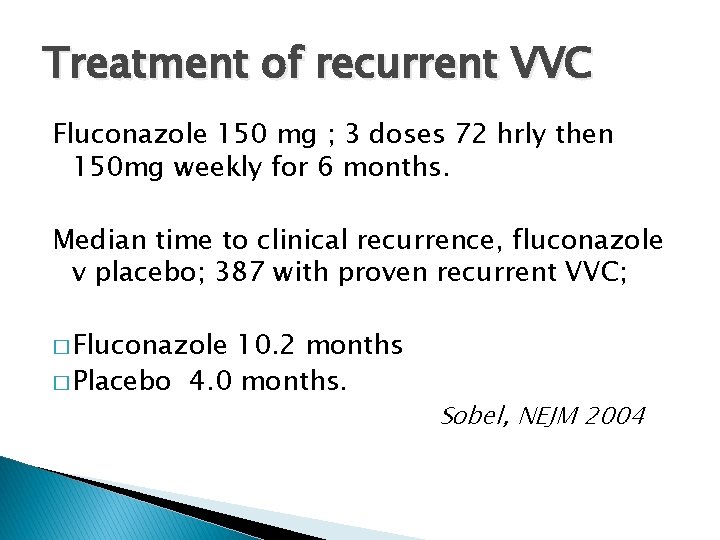
Treatment of recurrent VVC Fluconazole 150 mg ; 3 doses 72 hrly then 150 mg weekly for 6 months. Median time to clinical recurrence, fluconazole v placebo; 387 with proven recurrent VVC; � Fluconazole 10. 2 months � Placebo 4. 0 months. Sobel, NEJM 2004
HIV; always think about it! � HIV is treatable � Late diagnosis leads to high HIV related morbidity and mortality in UK � Test if indicator diseases. � In depth “counselling” not necessary � Insurance? � 3/12 “window”
HIV ; indicator diseases � Bacterial pneumonia � Severe seborrhoiec dermatitis � Peripheral neuropathy � Oral candidiasis � Chronic diarrhoea unknown cause � Weight loss unknown cause � Lymphadenopathy unknown cause � Neutropenia, lymphopenia
HIV PEPSE 2015 � Post exposure prophylaxis after sexual exposure � To start within 72 hrs, preferably within 24 � One month antiretroviral therapy � Patients may ask for it or you may feel it is worth giving after sexual history. � REFER GUM
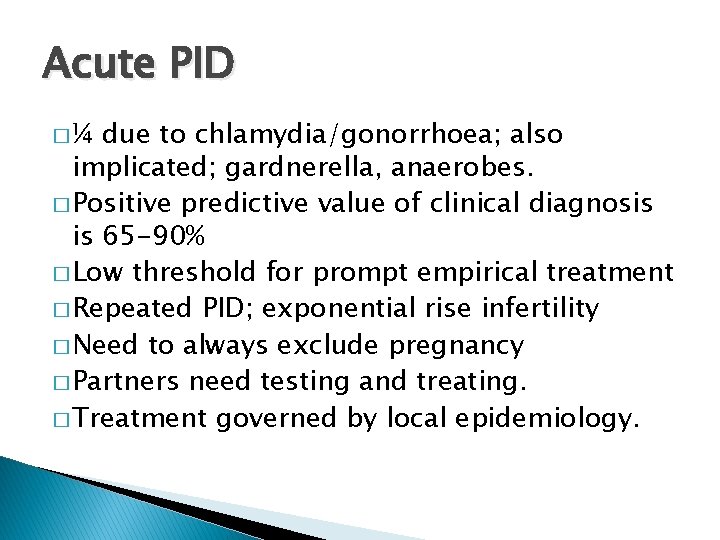
Acute PID �¼ due to chlamydia/gonorrhoea; also implicated; gardnerella, anaerobes. � Positive predictive value of clinical diagnosis is 65 -90% � Low threshold for prompt empirical treatment � Repeated PID; exponential rise infertility � Need to always exclude pregnancy � Partners need testing and treating. � Treatment governed by local epidemiology.
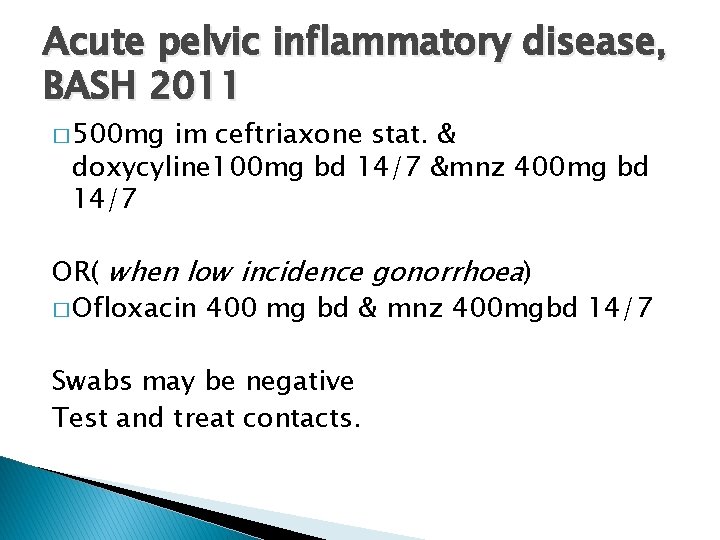
Acute pelvic inflammatory disease, BASH 2011 � 500 mg im ceftriaxone stat. & doxycyline 100 mg bd 14/7 &mnz 400 mg bd 14/7 OR( when low incidence gonorrhoea) � Ofloxacin 400 mg bd & mnz 400 mgbd 14/7 Swabs may be negative Test and treat contacts.
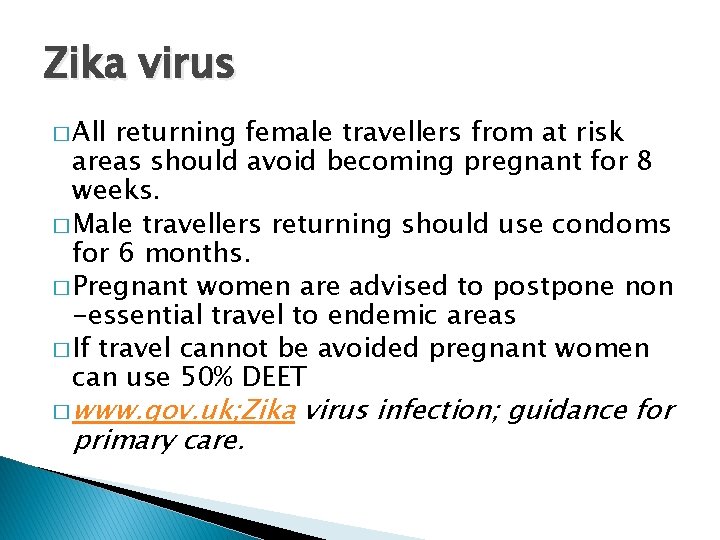
Zika virus � All returning female travellers from at risk areas should avoid becoming pregnant for 8 weeks. � Male travellers returning should use condoms for 6 months. � Pregnant women are advised to postpone non -essential travel to endemic areas � If travel cannot be avoided pregnant women can use 50% DEET � www. gov. uk; Zika primary care. virus infection; guidance for
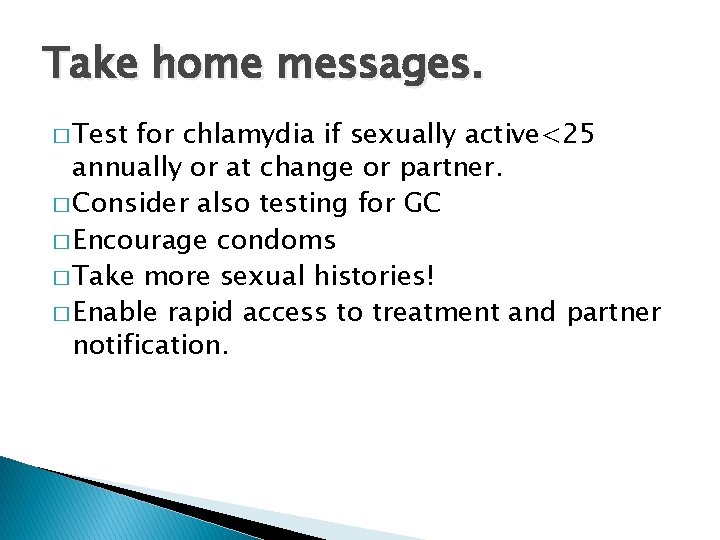
Take home messages. � Test for chlamydia if sexually active<25 annually or at change or partner. � Consider also testing for GC � Encourage condoms � Take more sexual histories! � Enable rapid access to treatment and partner notification.
References � www. bashh. org( � www. fsrh. org joint guidelines RCGP 2013) � www. chestersexualhealth. co. uk � 2013 national guidelines sexual history taking; BASHH. � Management of vaginal discharge in non GU settings, FSRH 2012
 Louise knowles
Louise knowles Primary secondary and tertiary care
Primary secondary and tertiary care Lewinda knowles
Lewinda knowles Malcolm knowles theory
Malcolm knowles theory Empat asumsi yang membedakan andragogi dan pedagogi
Empat asumsi yang membedakan andragogi dan pedagogi Geoff knowles
Geoff knowles Malcolm knowles
Malcolm knowles Sheepsheaf
Sheepsheaf Michael knowles vpn
Michael knowles vpn Uccs health circle primary care clinic
Uccs health circle primary care clinic Australian primary health care research institute
Australian primary health care research institute Pengertian primary care
Pengertian primary care Principles of primary health care
Principles of primary health care Advantages of selective primary health care
Advantages of selective primary health care Defination of primary health care
Defination of primary health care Provision of essential drugs
Provision of essential drugs Basic requirements for sound phc
Basic requirements for sound phc Structural adjustment programs
Structural adjustment programs Qliance
Qliance Principles of phc
Principles of phc Nutrition in primary health care
Nutrition in primary health care Elements of primary health care
Elements of primary health care Comprehensive primary health care approach
Comprehensive primary health care approach Importance of community health nursing
Importance of community health nursing Enhanced primary care mental health
Enhanced primary care mental health Albany area primary health care rural clinic
Albany area primary health care rural clinic Definition of primary health care services
Definition of primary health care services Barbara starfield primary care principles
Barbara starfield primary care principles Definition of community health nursing
Definition of community health nursing Incidental medical services
Incidental medical services Vertical health programmes
Vertical health programmes Function
Function Objectives of primary health care
Objectives of primary health care Integrated primary health care model
Integrated primary health care model Integrating public health and primary care
Integrating public health and primary care Hrsa bureau of primary health care
Hrsa bureau of primary health care Epiphany health direct primary care
Epiphany health direct primary care Health and social care values unit 2
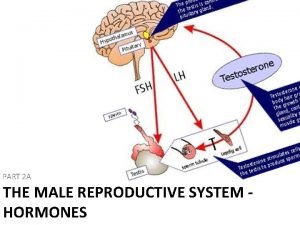
Health and social care values unit 2 Male reproductive system table
Male reproductive system table What are primary sexual characteristics
What are primary sexual characteristics Xx and xy chromosomes
Xx and xy chromosomes Primary sexual characteristics
Primary sexual characteristics Health and social component 3
Health and social component 3 Ceri evans
Ceri evans Buryfields clinic
Buryfields clinic What is sexual health
What is sexual health Sexual health
Sexual health Amsa sexual health leadership course
Amsa sexual health leadership course Sexual health and relationships education scotland
Sexual health and relationships education scotland Society of sexual health advisers
Society of sexual health advisers The primary pigments are _____ the primary colors.
The primary pigments are _____ the primary colors. Trafford primary care trust
Trafford primary care trust Starfield primary care
Starfield primary care Team nursing
Team nursing Dc primary care association
Dc primary care association Uhccp com tnenroll
Uhccp com tnenroll Mount auburn primary care
Mount auburn primary care Differenza tra primary nursing e case manager
Differenza tra primary nursing e case manager Icd 10 buka jahitan
Icd 10 buka jahitan Extended primary care team
Extended primary care team Multicultural primary care
Multicultural primary care Wellone primary care
Wellone primary care Primary care information project
Primary care information project Dr sanjiv ahluwalia
Dr sanjiv ahluwalia Primary care network map
Primary care network map Sutton & merton primary care trust
Sutton & merton primary care trust Primary care medicine goroll test bank
Primary care medicine goroll test bank Missouri primary care association
Missouri primary care association Kentucky primary care association
Kentucky primary care association Swedish primary care shoreline
Swedish primary care shoreline Feinberg match list
Feinberg match list Carecash
Carecash Severn school of primary care
Severn school of primary care Alexandra primary school student care
Alexandra primary school student care West lancashire primary care trust
West lancashire primary care trust Wellington primary school student care
Wellington primary school student care Team nursing care delivery model
Team nursing care delivery model Patient centered primary care collaborative
Patient centered primary care collaborative Patient centered care collaborative
Patient centered care collaborative Meritus definition
Meritus definition Mdpcp portal
Mdpcp portal Emily kark
Emily kark Alexandra primary school student care
Alexandra primary school student care South birmingham primary care trust
South birmingham primary care trust Maria principe
Maria principe