SEX HORMONES 1 FEMALE SEX HORMONES Estrogens and








- Slides: 53

SEX HORMONES

1 -FEMALE SEX HORMONES
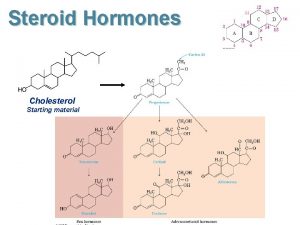
Estrogens and progestins are steroid hormones with numerous physiological actions. In women, these include developmental effects, control of ovulation, cyclical preparation of the reproductive tract for fertilization and implantation, and metabolic actions. The female sex hormones are also synthesized in smaller amounts in the adrenal cortex. Estrogens also have important actions in males, including effects on bone, spermatogenesis, and behavior.
ESTROGENS Natural estrogens are synthesized from cholesterol in human females, estradiol, estriol and estrone. Physiological and pharmacological actions: 1 -Normal maturation of female sex organs. 2 -The secondary sexual characters 3 -Important for normal menstrual cycle. 4 -Relatively high doses of estrogens suppress the secretion of FSH and FSHRH. These effects lead to inhibition of ovulation.
5 -Metabolic effects: a-They decrease the rate of bone resorption. b-Estrogens decreasing the concentration of LDL and cholesterol and increasing HDL. c-They increase the circulating proteins which are responsible for the transport of thyroxine, cortisol, iron and other substances. d-They also reduce sebaceous gland activity. 6 -Cause salt and water retention. 7 -They enhance coagulability of blood

Mechanism of action: Plasma estrogens are bound to SHBG, from which they dissociate to enter the cell and bind to their receptor. The estrogen receptors are found predominantly in the nucleus bound to heat shock proteins that stabilize them. Binding of the hormone to its receptor alters its conformation and releases it from the stabilizing proteins (predominantly Hsp 90). The receptor-hormone complex bind to estrogen response elements (EREs) to regulate gene transcription.
Clinical indications: l-As a component of oral contraceptives. 2 -Replacement therapy in patients with estrogendeficiency as in: a-Female hypogonadism, atrophic vaginitis, primary ovarian failure. b-Postmenopausal women.
NB: 1 -The administration of estrogen in postmenopausal women is associated with an increased risk of endometrial carcinoma. 2 -Dose of estrogen needed for postmenopausal hormone replacement therapy is less than that used in oral contraception. 3 - In patients in whom estrogen replacement therapy is contraindicated, such as those with estrogen-sensitive tumors, relief of vasomotor symptoms may be obtained by the use of clonidine.
Adverse reactions: l-Common side effects: Nausea, vomiting, anorexia and dizziness 2 -Moderate doses: may cause breast tenderness, endometrial hyperplasia and breakthrough bleeding. 3 -Over long periods: salt and water retention leading to edema. 4 -They may increase the risk of gall bladder disease and endometrial carcinoma. 5 -Estrogen use may also associated with thromboembolic disorders, carbohydrate intolerance, hyperpigmentation and headache.

Precautions and contraindications: Estrogens should not be used in patients with estrogen dependent tumours as breast or endometrial carcinoma. They should be avoided in patients with history of thromboembolic disorders or cholestatic jaundice and in patients with epilepsy, mental depression, migraine, bronchial asthma, hepatic dysfunction, diabetes and cardiovascular diseases.
Preparations: The natural estrogens are ineffective orally. Semisynthetic and synthetic estrogens include ethinyl estradiol, diethylstilbestrol and dienestrol. They are orally effective and are used also by injection.
PROGESTINS Progesterone is the major natural progestin in humans. It is rapidly metabolized in the liver and has a very low oral bioavailability and short half-life. lts short duration of action and its ineffectiveness by oral administration limit its therapeutic uses. A number of synthetic drugs with progestational activities which are effective orally and have more prolonged duration of action than progesterone are called progestins. They are basically used for replacement therapy and in hormonal contraceptives.
Physiological and pharmacological action: l-Progesterone causes maturation of the uterine endometrium, facilitates implantation of the fertilized ovum and maintains pregnancy. 2 -Progesterone induces the cervix to secrete thick and viscid secretions. 3 -Progesterone in relatively high dose inhibits LH hormone and consequently ovulation. 4 -lt diminishes the spontaneous rhythmic contractions of the uterus and causes uterine relaxation. 5 -lt induces the development of secretory tissues in the breast. 6 -It has a thermogenic effect through the hypotholamus and causes slight rise in the body temperature.
Mechanism of action Similar to that of other steroid hormones, Progestins enter the cell and bind to progesterone receptors that are distributed between the nucleus and the cytoplasm. The ligand-receptor complex binds to a progesterone response element (PRE) to activate gene transcription.
Clinical indications: l-The major clinical use of synthetic progestins is for oral contraception either alone or combined with an estrogen. 2 -Combined with estrogens in hormonal replacement therapy of postmenopausal women. 3 -Treatment of endometriosis to produce long lasting ovarian suppression. 4 -Treatment of amenorrhea and functional uterine bleeding.
5 -Progestins are highly efficacious in decreasing the occurrence of endometrial hyperplasia and carcinoma caused by unopposed estrogens. 6 -Progestins have been used as a palliative measure for metastatic endometrial carcinoma and as a second-line treatment for breast cancer. 7 -As diagnostic test for estrogen secretion and for responsiveness of the endometrium. Progestin is given for 57 days to amenorrheic women, withdrawal bleeding will occur if the endometrium has been stimulated by endogenous estrogens.
Adverse reactions: Progestins may produce nausea, weight gain, change in libido, hirsutism and acne. They also may increase the blood pressure and decrease the level of HDL. Contraindications: Progestins are contraindicated in undiagnosed vaginal bleeding, hepatic dysfunction, suspected pregnancy and thromboembolic disorders. They should be used cautiously in bronchial asthma, epilepsy, mental depression and migraine headache.
Preparations The following are examples of synthetic progestins: i) Norethindrone acetate. ii) Norgestrel iii) Norethynodrel. iv) Medroxyprogesterone acetate.
HORMONAL CONTRACEPTIVES (I) ORAL CONTRACEPTIVES: Synthetic estrogens and synthetic progestins are used because they resist destruction by the liver after oral administration. The most commonly used estrogens are ethinylestradiol and mestranol and the most commonly used progestins are norethindrone, norethynodrel and norgestrel. Two types of oral contraceptives for women have been developed, combined preparations and single entity preparations.

(1)Combined Preparations: They are the most widely and the most effective preparations used. The low failure rate of these preparations is attributed to their multiple mechanism of action: 1 -Inhibition of ovulation. 2 -Progestins also thicken the cervical secretions. 3 -Combined contraceptives can cause disturbance in the endometrium. 4 -Alteration in tubular transport of the ova.
Types of combined oral contraceptives: 1 -Monophasic 2 -Biphasic 3 -Triphasic The available combined contraceptives differ from one another in their contents of estrogen and progestin. The choice of the suitable preparation is dependent mainly on the pre-existing hormonal status of the woman.
(2)Progestin-Only Contraceptives: These preparations contain progestin alone in doses which are lower than those contained in the combined preparations. They are taken daily continuously. They are less effective, less popular than the combined types and indicated whenever estrogen is contraindicated. There is high incidence of abnormal bleeding.
Emergency (postcoital) Contraception: Emergency contraception can prevent implantation and pregnancy after unprotected sexual intercourse. Treatment should be started within 72 hours. Preparations as: l)Levonorgestrel 0. 75 mg : Two pills (one immediately and the other after 12 hours). It has a 1% failure rate. 2)Levonorgestrel 0. 25 mg with ethinylestradiol 0. 05 mg : Four pills (two immediately and two alter 12 hours). The failure rate is about 3%. There is higher incidence of nausea and vomiting and antiemetics should be provided.
Indications of oral contraceptives 1)Oral contraceptives are mainly used for prevention of pregnancy. 2)They may also be used in dysmenorrhea, amenorrhea, dysfunctional uterine bleeding and endometriosis. 3)They are used to suppress lactation and to postpone menstruation.
Beneficial Effects of Contraceptives Apart from contraception, oral contraceptives were found to reduce the incidence of ovarian cysts, ovarian and endometrial carcinomas and benign fibrocystic breast disease. There is lower incidence of ectopic pregnancy, pelvic inflammatory disease and rheumatoid arthritis. There is more regular menstruation with less blood loss and less iron- deficiency anemia.
Adverse effects: Less serious but more common side effects include: l-nausea, vomiting, dizziness, headache, weight gain and discomfort in breast are attributed to the estrogen content. 2 -depression of mood, easy fatigue and lack of initiative have been attributed to the progestins. 3 -irregular menstrual bleeding (breakthrough bleeding). This is less troublesome with preparations containing large doses of estrogens. 4 -skin rash, alopecia, brown skin pigmentation of face and hirsutism.
More serious but less common undesirable effects include: 1 - Cardiovascular system: a-Venous thromboembolism: This complication appears to be attributable to the estrogen in these preparations which produces: i-increased platelet aggregation. ii-decreased plasma levels of antithrombin III. iii-increased circulating levels of factors II, VII, IX, X.
b-Myocardial infarction and stroke: This risk is more in women over 35 years and smoking. c-Hypertension: The estrogens and progestins are responsible for this as they facilitate salt and water retention secondary to increase in plasma renin activity and subsequent formation of angiotensin. 2 -Gastrointestinal disorders: cholestatic jaundice and increased incidence of gall stones.
Contraindications: l-History of thrombembolism. 2 -Moderate-severe hypertension. 3 -Activc liver disease. 4 -lmpending major surgery. 5 -Women over 35 years and cigarette smokers. 6 -Estrogen dependent tumors. Patients with migraine; cerebral insufficiency, severe diabetes mellitus and cardiovascular diseases should be very cautious when taking the pills.
Drug interactions: Failure of oral contraception can be precipitated by : 1 -coadministration of drugs that induce hepatic microsomal enzymes as antiepileptics (phenobarbital, Phenytoin, primidone, carbamazepine), rifampicin, chlordiazepoxidc. 2 -administration of broad spectrum antibiotics. Estrogens are conjugated in the liver and pass with bile to intestine where the hydrolytic enzymes produced by gut bacteria cleave these conjugates and release the free estrogen which is then reabsorbed (enterohepatic circulation).

(II) INJECTABLE CONTRACEPTIVES MEDROXYPROGESTERONE ACETATE (depo Provera) is a long acting preparation. It is injected IM. in a dose of 150 mg every 3 months. It should only be used if the possibility of permanent infertility is acceptable by the woman. Side effects Headache, dizziness, depression and cycle disturbances (spotting, short and long lasting amenorrhea). Contraindications The same as those of oral contraceptives.
(III) IMPLANTABLE PROCESTIN: This method utilizes the subcutaneous implantation of six capsules each containing 36 mg levonorgestrel (Norplant). These capsules are extremely effective and last for 5 -6 years. The low level of hormone (30 µg are released daily) has little effect on lipid, protein and carbohydrate metabolism or serum chemistry. Disadvantages: The need for surgical insertion and removal of capsules and some irregular bleeding.
INHIBITORS AND ANTAGONISTS OF FEMALE SEX HORMONES
ESTROGEN INHIBITORS AND ANTAGONISTS 1)Antiestrogens: A-CLOMIPHENE CITRATE Clomiphene citrate is an antiestrogen. It competes with, and prevents the binding of estrogen with its receptors in the hypothalamus; thus it blocks the feed back inhibitory influence of estrogen on the hypothalamic Gn. RH. The drug will be ineffective in patients with ovarian or pituitary failure.
Indications: a-Clomiphene is used in the treatment of disorders of ovulation in patients with anovulatory cycles and wishing to become pregnant. If no response is observed after 6 courses, it should not be repeated. b-Diagnosis of ovarian function. c-ln combination with gonadotropins, clomiphene is used in ln-vitro fertilization.
Adverse reactions: The important drawback from ovarian hyperstimulation is the formation of multiple ovarian cysts and a high incidence of multiple births. Moreover. Clomiphene may cause hot flashes, headache, constipation, reversible hair loss, heavy menses and weight gain. Precautions: Clomiphene is not recommended in cases of abnormal vaginal bleeding, fibroid tumors of uterus, mental depression, thrombophlebitis and impairment of hepatic function.
B-FULVESTRANT: Is a selective estrogen receptor downregulator (SERD). It binds to the estrogen receptor, increasing markedly its proteolytic degradation and decreasing its number in cells, which may explain its efficacy in tamoxifenresistant advanced postmenopausal breast cancer.
2) SELECTIVE ESTROGEN RECEPTOR MODULATORS: Tamoxifen, Raloxifene and Toremifene are selective estrogen receptor modulators. Their pharmacological goal is to produce beneficial estrogenic actions in certain tissues (e. g. , bone, brain, and liver) but antagonist activity in others (e. g. , breast and endometrium). It is used mainly in the treatment of metastatic breast cancer in postmenopausal women with estrogen receptor-positive tumors. Nausea, vomiting, weight gain and hot flashes are the most frequent adverse reactions.

3) Estrogen synthesis inhibitors: LETROZOLE, ANASTROZOLE, VOROZOLE and Exemestane These drugs are. They block specifically the local production of estrogen by inhibiting the enzyme aromatase which is responsible for the synthesis of estrogens from its precursors. They have been used for the second line treatment of breast cancer in patients for whom tamoxifen therapy is unsuccessful.
(II)ANTIPROGESTINS MIFEPRISTONE Mifepristone is an orally active competitive antagonist of progesterone and glucocorticoid receptors. It also has luteolytic properties. Clinical indications l-The major use of mifepristone is as abortifacient to terminate early pregnancy, usually in combination with prostaglandins. 2 -Other potential uses include the induction of labor after intrauterine fetal death, treatment of endometriosis, Cushing syndrome, breast cancer and other neoplasms that contain progesterone or glucocorticoid receptors.
III)GONADOTROPIN INHIBITORS DANAZOL Danazol is a synthetic androgen that inhibits the release of gonadotropins (FSH and LH) by the anterior pituitary, thus inhibiting the synthesis of sex hormones. In women this action arrests ovarian function, induces amenorrhea and causes atrophy of the normal and ectopic endometrial tissues. In addition, danazol increases the activity of the clotting factors VIII and IX.
Indications l-Treatment of endometriosis. 2 -Treatment of fibrocystic disease of the breast. It reduces the nodularity and relief pain and tenderness. 3 -It has been used in hematological disorders such as hemophilia and idiopathic thrombocytopenic purpura.
Adverse reactions Weight gain, edema, decreased breast size, deepening of voice, headache, hot flashes, changes in libido, increased hair growth and muscle cramps. Contraindications Danazol is contraindicated during pregnancy and breast feeding. It shoud be used cautiously in patients with hepatic dysfunction since it produces mild to moderate hepatocellular damage in some patients.
OVULATION INDUCING AGENTS Drugs that are used to stimulate ovulation include: l-Clomiphene citrate. 2 -Bromocriptine, used only in cases of hyperprolactinemia. 3 -Gonadotropins: human menopausal ganadotropins (HMG) and human chorionic ganadotropins (HCG) are useful in patients with hypopituitrism. 4 -Gonadotropin releasing hormone (Gn. RH) is useful in patients with hypothalamic amenorrhea.
B) MALE SEX HORMONES (TESTOSTERONE) Testosterone and other related androgens are synthesized in the testis and secreted also in very small quantities by adrenal cortex and ovaries. The production of testosterone by the interstitial cells of the testis is controlled by the anterior pituitary ICSH which in turn is controlled by the ICRH produced by the hypothalamus. Testosterone is converted in the body to dihydrotestosterone, the active hormone in tissues.

Physiological and pharmacological actions: l)Testosterone is responsible for the development and maintenance of secondary sex organs and the secondary sex characters. 2)Androgenic hormones have an anabolic action. 3)Androgens cause water and salt retention. 4)Androgens increase growth and secretion sebaceous glands clinically mainfested as acne. of
Preparations: Testosterone is less effective orally as it is greatly inactivated by the liver. Synthetic preparations have a longer duration of action and are active orally such as methyltestosterone. Synthetic anabolic steroids related to testosterone are also available; they possess a high anabolic and low androgenic activity ratios such as nandrolone and oxymetholone.
Clinical indications: l-Replacement therapy in hypogonadism in males such as cryptorchidism, delayed puberty and impotence. 2 -Anabolic steroids which increase protein synthesis and enhance muscle development with little androgenic activity are used in debilitating and wasting conditions, osteoporosis and illegally by some athletes to increase muscle bulk and performance.
Adverse reactions l-They may cause cholestatic jaundice and prolonged use may produce hepatocellular carcinoma. 2 -Salt and water retention leads to edema. 3 -They may cause infertility in men, disturbance of growth in children and musculinization of females. Contraindications They are contraindicated in breast cancer in male, and cancer prostate. Androgens should be used with caution in cases of cardiac failure, liver dysfunction, diabetes and hypercalcemia.
ANTIANDROGENS (A)ANDROGEN RECEPTOR ANTAGONISTS l-Flutamide and Bicalutamide: flutamide is a competitive antagonist of dihydrotestosterone for the androgen receptors. It has been used in the treatment of metastatic prostatic carcinoma usually in conjunction with Gn. RH analog such as leuprolide. It frequently causes mild gynecomastia and mild reversible hepatic toxicity. Bicalutamide is similar to flutamide but has the advantage of being less hepatotoxic and is taken once daily instead of three times a day.
2 -Cyproterone acetate: cyproterone is a derivative of progesterone but has weak progestational activity. It is a partial agonist at androgen receptors; it competes with dihydrotestosterone for binding to these receptors in target tissues. It also depresses the synthesis of gonadotropins through an action on the hypothalamus. Cyproterone is used mainly to decrease excessive sexual desire in men and to treat hirsutism in females.
(B) 5 α-REDUCTASE INHIBITORS Finasteride It is a specific inhibitor of steroid 5α-reductase. Dihydrotestosterone is responsible for androgen actions in prostate and hair follicles. Finasteride is mainly used in patients with benign prostatic hyperplasia, where it reduces prostatic size and improves urinary flow, but selective α 1 adrenergic blockers (e. g. terazocin) have been found more effective. The drug is also used for the treatment of androgenetic alopecia. Impotence is an infrequent side effect.
 Secretes estrogens and progesterone
Secretes estrogens and progesterone Sex sex sex
Sex sex sex Sex sex sex
Sex sex sex Sex sex sex
Sex sex sex Sex sex sex
Sex sex sex Sex sex sex
Sex sex sex Male and female hormones
Male and female hormones Male and female hormones
Male and female hormones Octopomine
Octopomine Sex male and female
Sex male and female X-linked punnett square
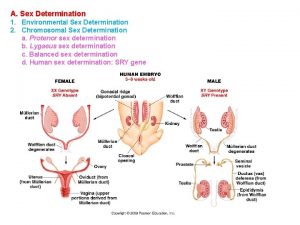
X-linked punnett square Sex determination and sex linkage
Sex determination and sex linkage Sex determination and sex linkage
Sex determination and sex linkage Primary sex organs of the female *
Primary sex organs of the female * System reproductive female
System reproductive female Female urogenital triangle
Female urogenital triangle Fornix of vagina
Fornix of vagina Once a sex offender always a sex offender
Once a sex offender always a sex offender Bioflix activity homeostasis hormones and homeostasis
Bioflix activity homeostasis hormones and homeostasis Calcitonin and pth are antagonistic hormones
Calcitonin and pth are antagonistic hormones Bioflix activity homeostasis high blood glucose
Bioflix activity homeostasis high blood glucose Plant hormones and responses
Plant hormones and responses Plant hormones and responses
Plant hormones and responses Synthesis and secretion of thyroid hormones
Synthesis and secretion of thyroid hormones Parathyroid gland chief cell
Parathyroid gland chief cell Nipple discharge color
Nipple discharge color Hormones
Hormones Steroid hormone lipid
Steroid hormone lipid Rolz group
Rolz group What is the chemical classification of this hormone
What is the chemical classification of this hormone Cytokinin function
Cytokinin function Prolactin hormones
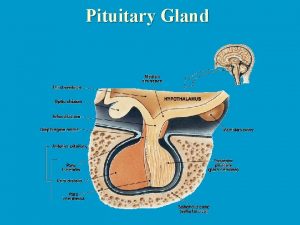
Prolactin hormones Hipofisis gland
Hipofisis gland Synthesis of amine hormones
Synthesis of amine hormones Prolactin target
Prolactin target Hypothalamus hormones
Hypothalamus hormones Lipid soluble hormones
Lipid soluble hormones Lipid soluble hormones examples
Lipid soluble hormones examples Gonadal hormones
Gonadal hormones Vasopresine
Vasopresine Tropic vs nontropic hormones
Tropic vs nontropic hormones Amino acid-based hormones
Amino acid-based hormones Hypothalmus
Hypothalmus Mechanism of action of hormones
Mechanism of action of hormones Tropic hormones
Tropic hormones Tropic hormones hypothalamus
Tropic hormones hypothalamus Four classes of hormones
Four classes of hormones Tropic vs nontropic hormones
Tropic vs nontropic hormones Hormones during pregnancy
Hormones during pregnancy What are the lipid soluble hormones
What are the lipid soluble hormones Autocrine hormones
Autocrine hormones Hypophysis
Hypophysis Hypothalamic hormones
Hypothalamic hormones Hunger motivation ap psychology
Hunger motivation ap psychology