Sex Hormones Female Reproduction Male Reproduction Assoc prof








































- Slides: 113
Sex Hormones Female Reproduction Male Reproduction Assoc. prof. Edyta Mądry MD Ph. D Poznań University of Medical Sciences


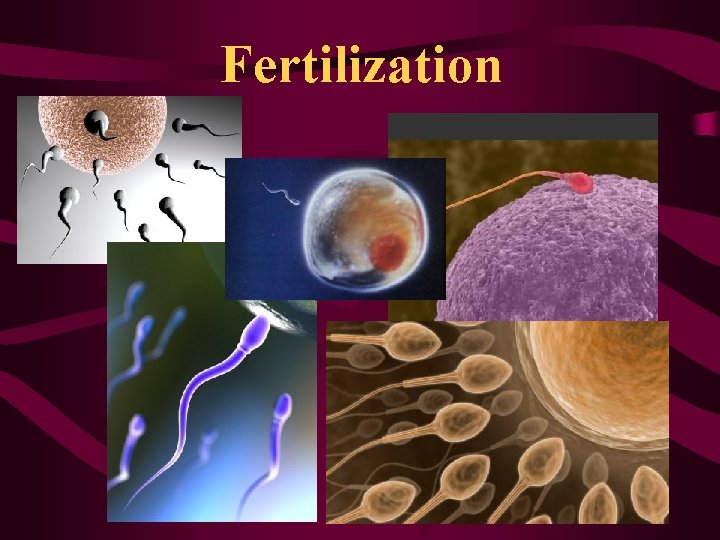
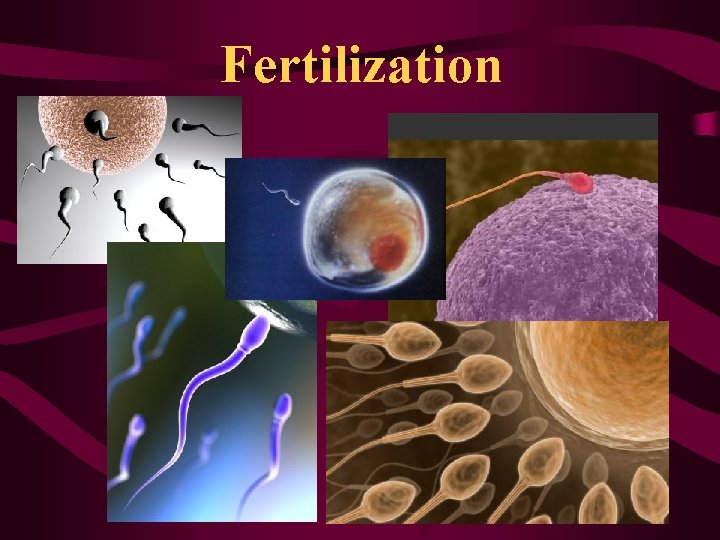
Fertilization

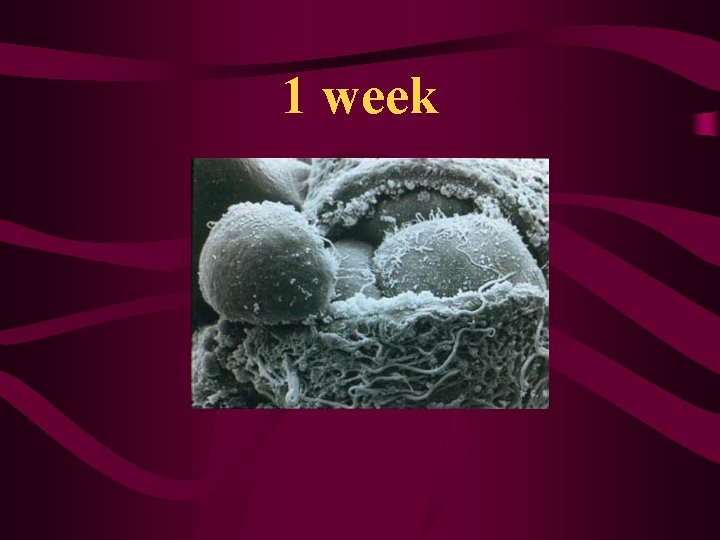
1 week
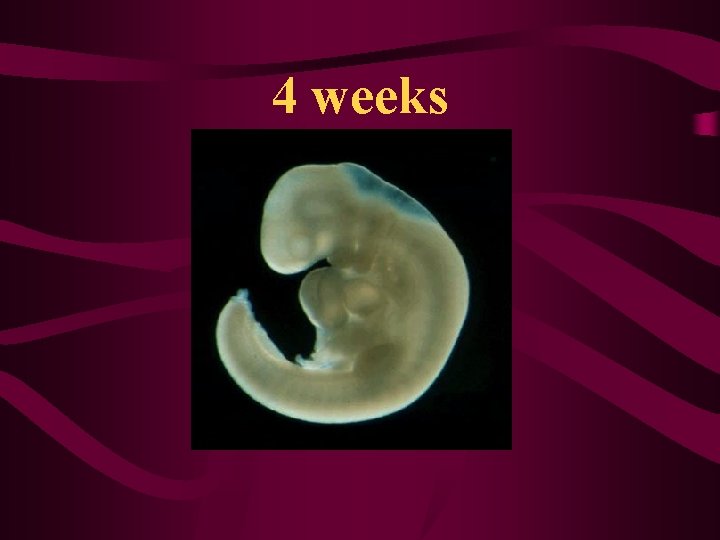
4 weeks

14 weeks
Newborn Girl or Boy ? ? ?
Girl or Boy?

Neonates

10 -11 years
teenagers
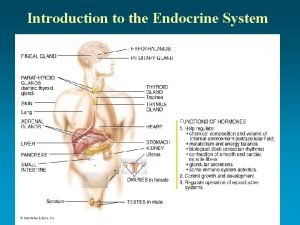
Hormone – hormaein means „to excite” or to „arouse”
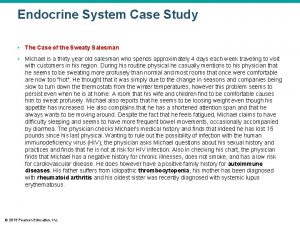
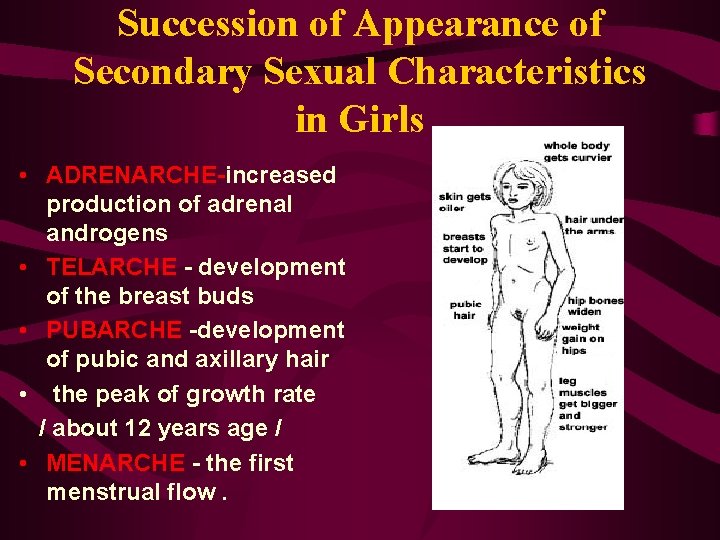
PUBERTY • The earliest hormonal change heralding the onset of puberty is increased secretion of androgens / (dehydroepiandrosterone, dehydroepiandrosterone sulfate) from the adrenal cortex. The level of these hormones increases progressively from the age of 6 to 8 years.

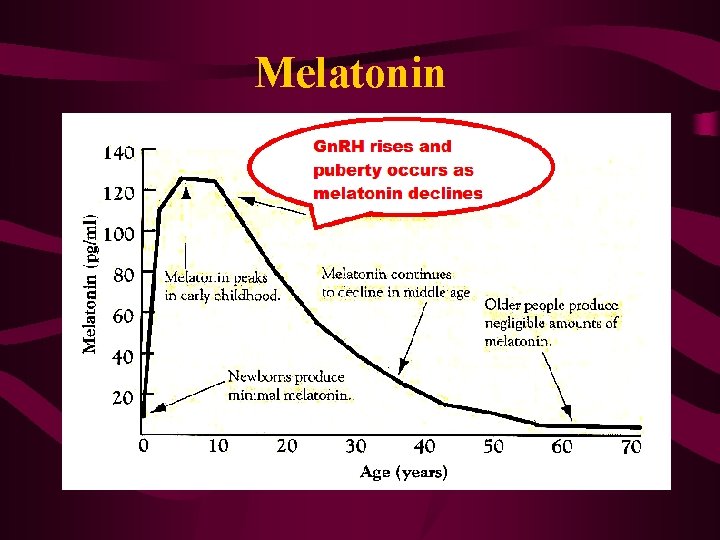
Melatonin
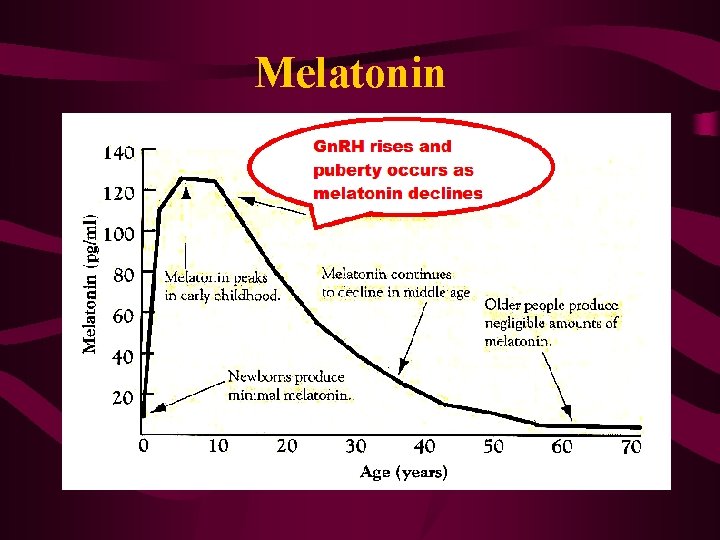
Melatonin
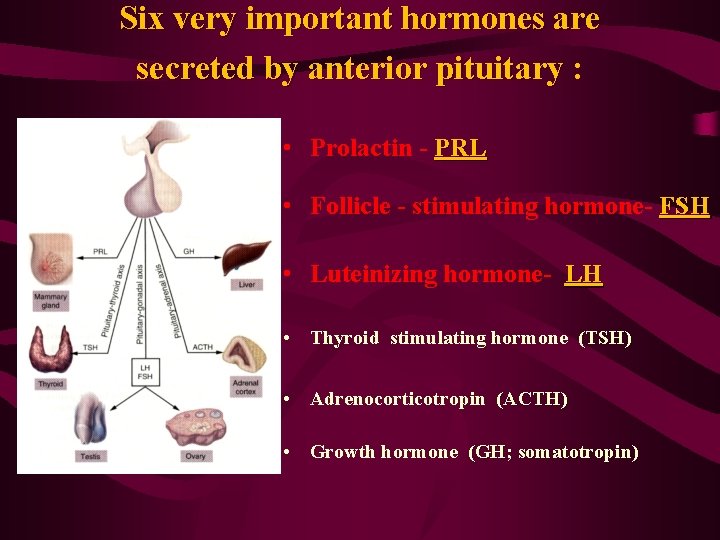
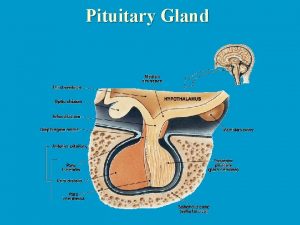
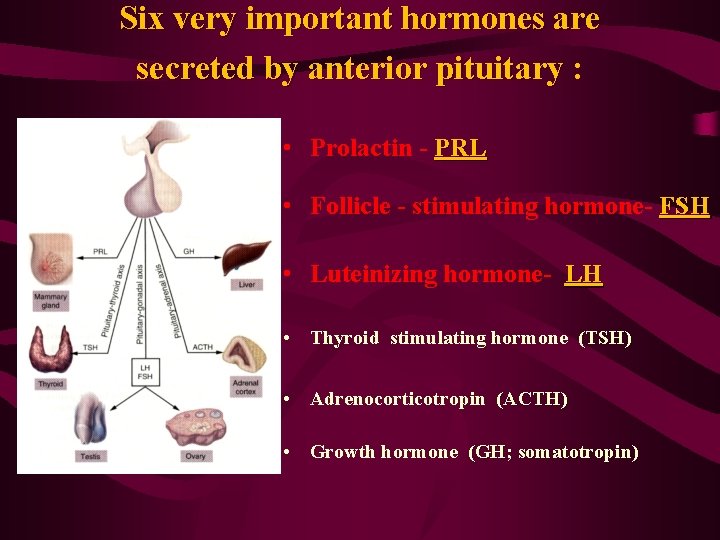
Six very important hormones are secreted by anterior pituitary : • Prolactin - PRL • Follicle - stimulating hormone- FSH • Luteinizing hormone- LH • Thyroid stimulating hormone (TSH) • Adrenocorticotropin (ACTH) • Growth hormone (GH; somatotropin)
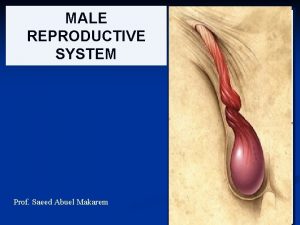
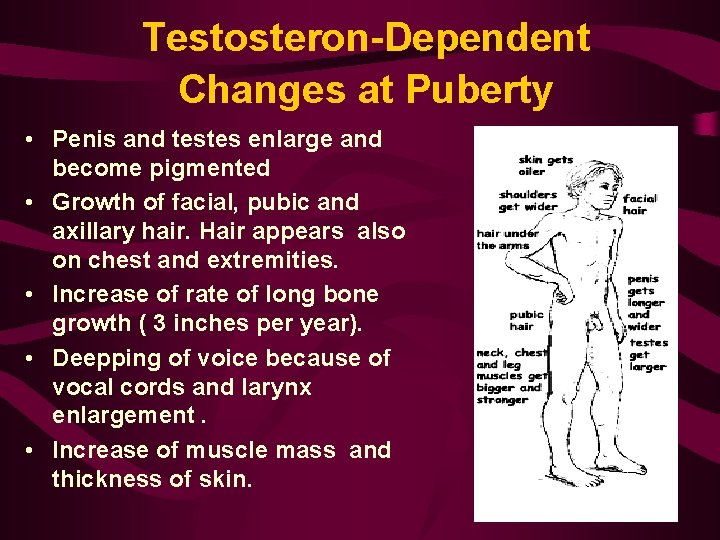
Male Reproductive Function

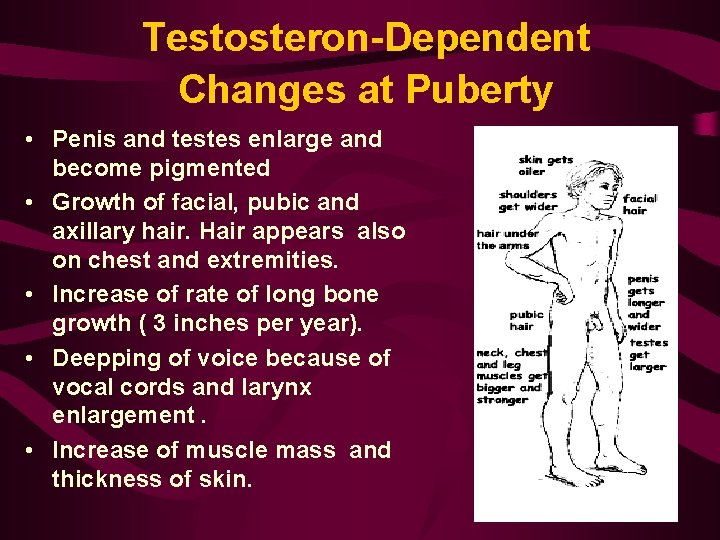
Testosteron-Dependent Changes at Puberty • Penis and testes enlarge and become pigmented • Growth of facial, pubic and axillary hair. Hair appears also on chest and extremities. • Increase of rate of long bone growth ( 3 inches per year). • Deepping of voice because of vocal cords and larynx enlargement. • Increase of muscle mass and thickness of skin.


Function of Sertoli cells • maintenence of blood-testes barrier which prevents many substances from entering or leaving the seminiferous tubules. • removal of any damaged germ cells. • keep the sperm in the tubules from diffusing into the blood. • production of seminiferous tubular fluid • nourishment of developing germ cells • synthesize of ABP (androgen binding protein) • synthesize of Inhibin

Capacitation is associated with removal of adherent seminal plasma proteins, reorganization of plasma membrane lipids and proteins

Numbers to remember Man • lifetime of sperm after ejaculation- max. 72 h • duration of spermatogenesis (the production of mature sperm)- about 63 days • average volume of ejaculate- 3 -5 ml • average number of sperm cells in 1 ml of ejaculate- 40 -120 mln / 1 ml
Female reproductive function
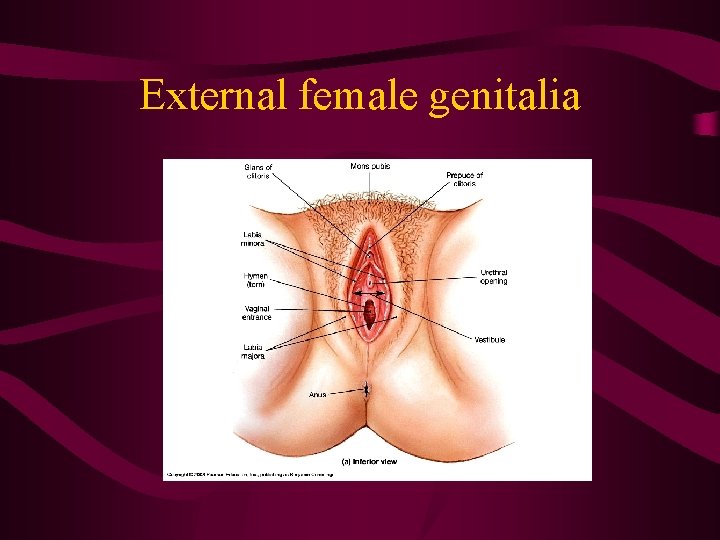
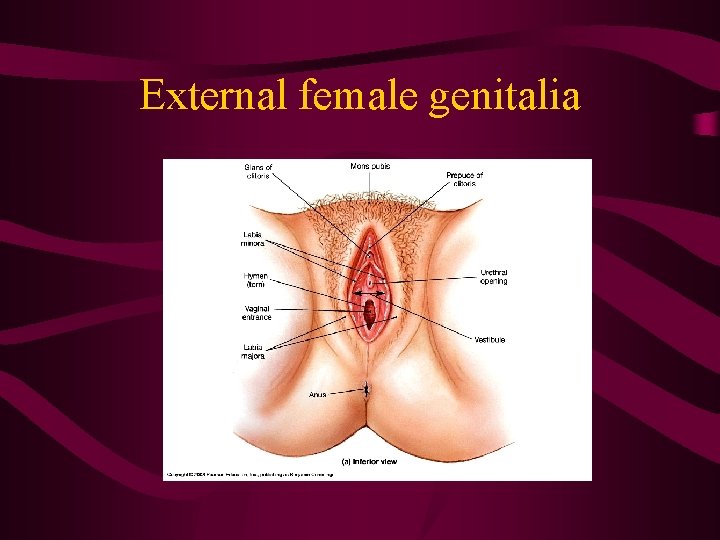
External female genitalia

Female reproductive tract
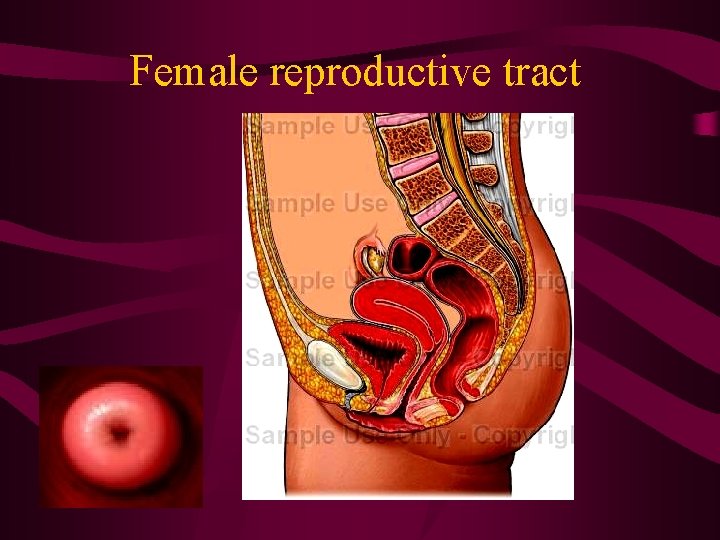
Female reproductive tract
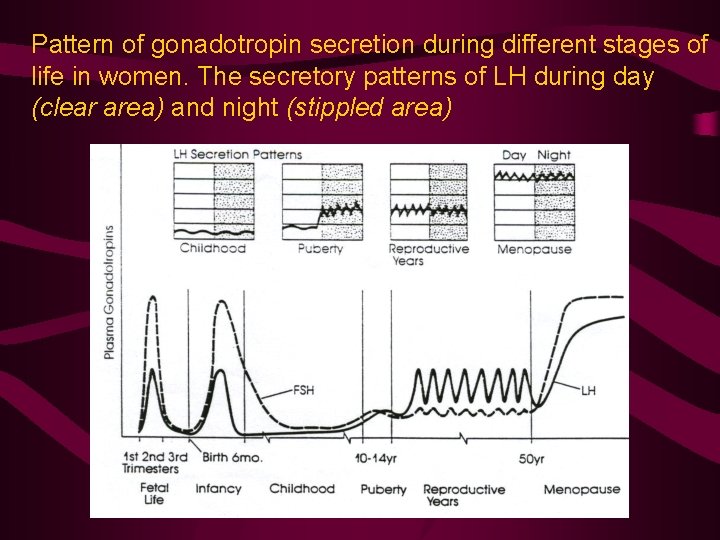
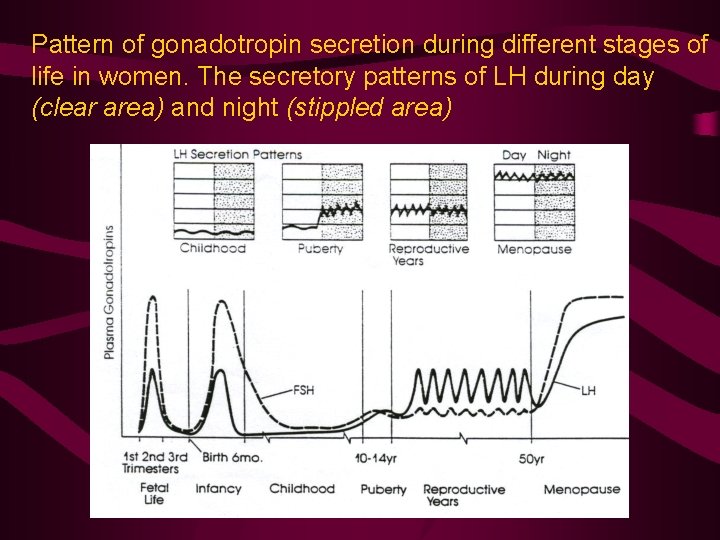
Pattern of gonadotropin secretion during different stages of life in women. The secretory patterns of LH during day (clear area) and night (stippled area)
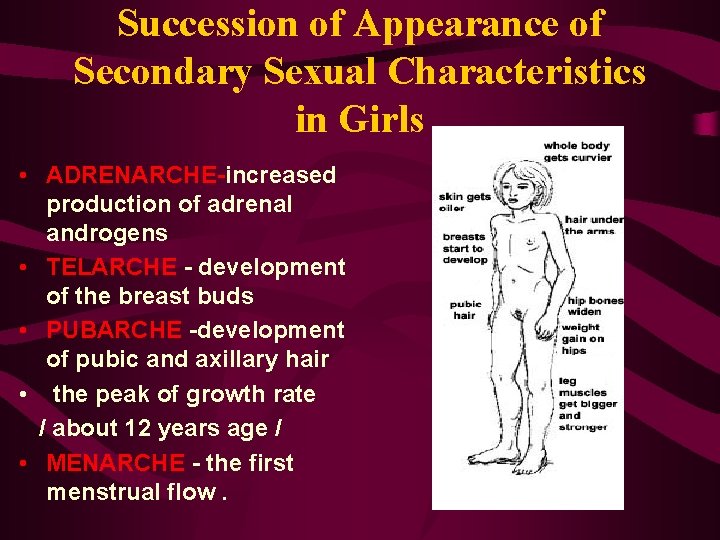
Succession of Appearance of Secondary Sexual Characteristics in Girls • ADRENARCHE-increased production of adrenal androgens • TELARCHE - development of the breast buds • PUBARCHE -development of pubic and axillary hair • the peak of growth rate / about 12 years age / • MENARCHE - the first menstrual flow.
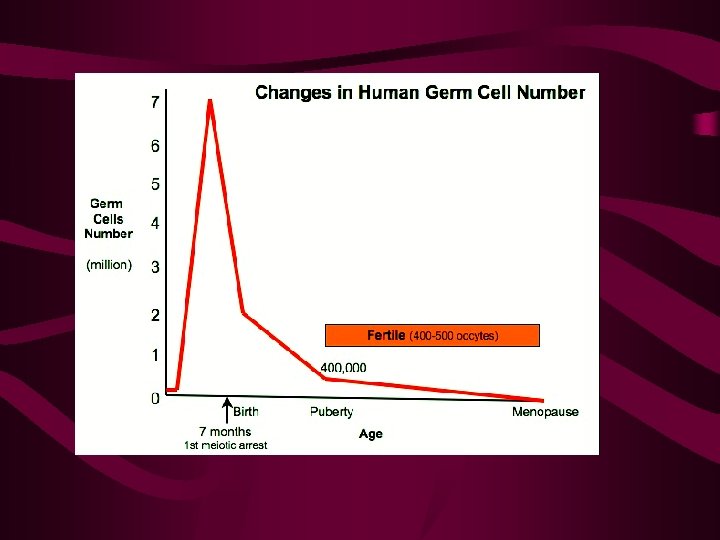



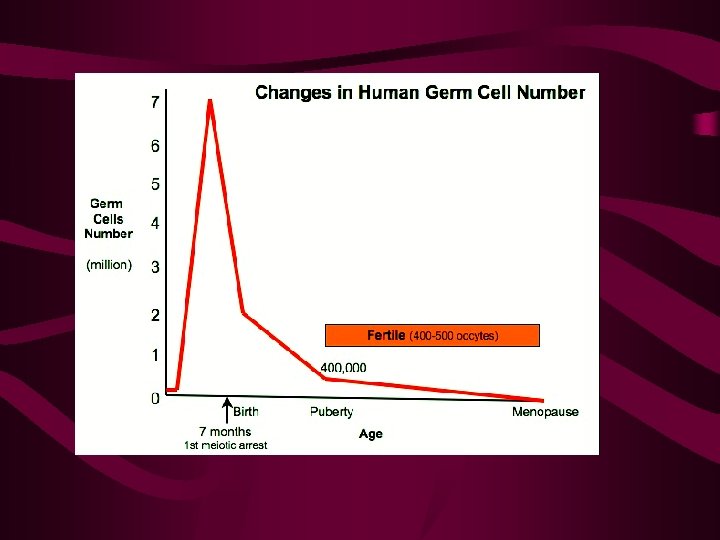
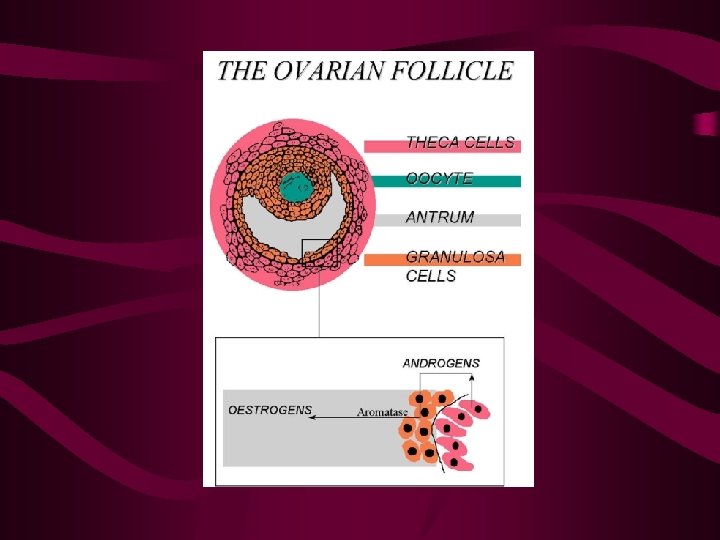
Phases of ovarian cycle • FOLLICULAR PHASE- development of follicles, selection of the dominant follicle=Graafian follicle, degeneration of the rest follicles • OVULATION • LUTEAL PHASE ( lasts 14 days !!!)
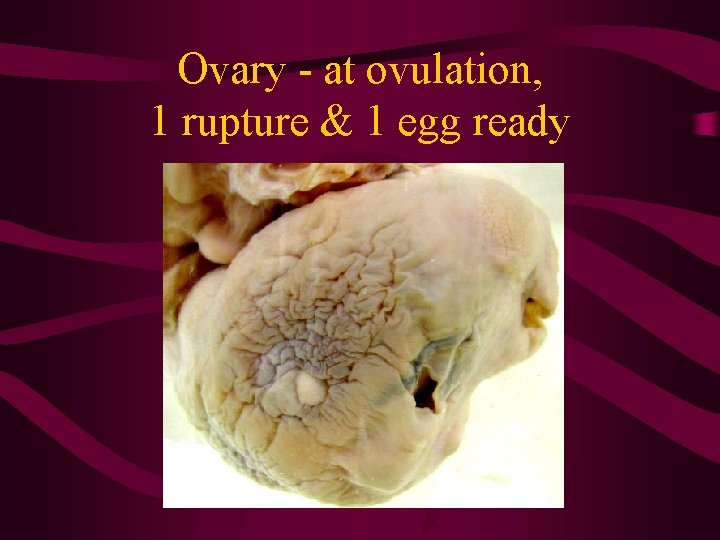
Ovary - at ovulation, 1 rupture & 1 egg ready
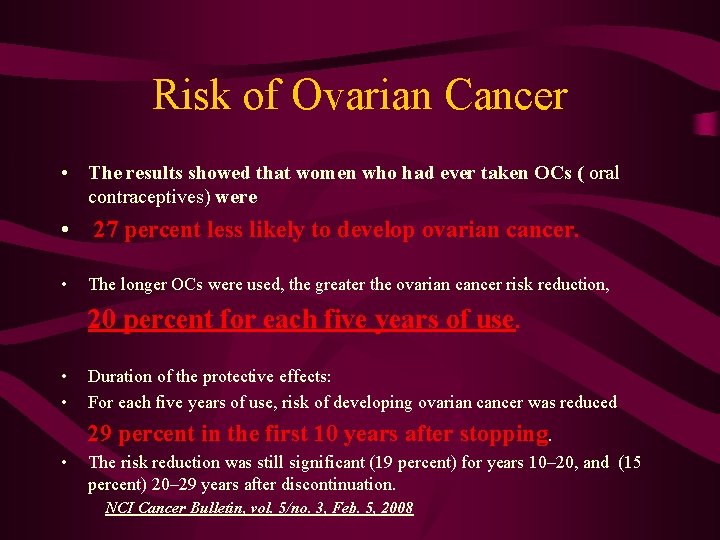
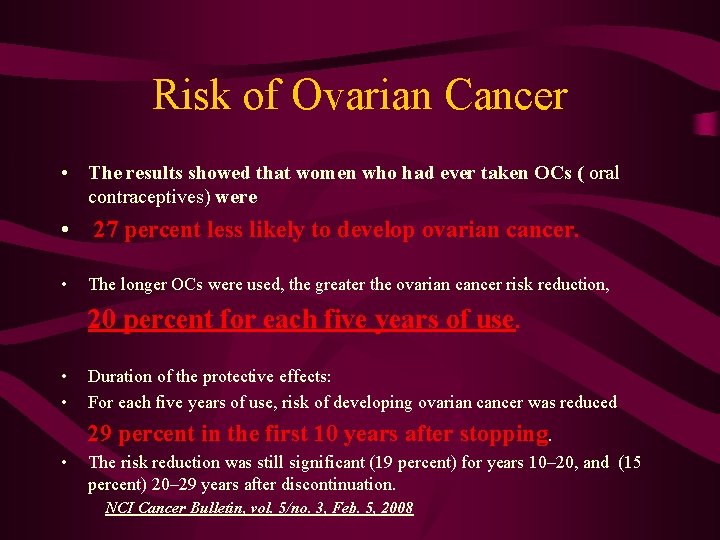
Risk of Ovarian Cancer • The results showed that women who had ever taken OCs ( oral contraceptives) were • 27 percent less likely to develop ovarian cancer. • The longer OCs were used, the greater the ovarian cancer risk reduction, 20 • • Duration of the protective effects: For each five years of use, risk of developing ovarian cancer was reduced 29 • percent for each five years of use. percent in the first 10 years after stopping. The risk reduction was still significant (19 percent) for years 10– 20, and (15 percent) 20– 29 years after discontinuation. NCI Cancer Bulletin, vol. 5/no. 3, Feb. 5, 2008

Phases of endometrial= (uterine ) cycle • Menstruation= menstrual bleeding- desquamation of uterine epithelium • Proliferative phase- increase endometrium in thickness • Secretory phase- accumulation of nutrients, mainly glycoproteins
Numbers to remember WOMAN • lifetime of the ovum after ovulation- max. 24 h (possibility for fertilization) • average duration of reproductive cycle- 28 days • ranges of reproductive cycle duration- 21 -35 days • menstrual bleeding- duration - 3 -7 days / , loss of blood and serous fluid < than 100 ml) • Lasting of luteal phase- 14 days


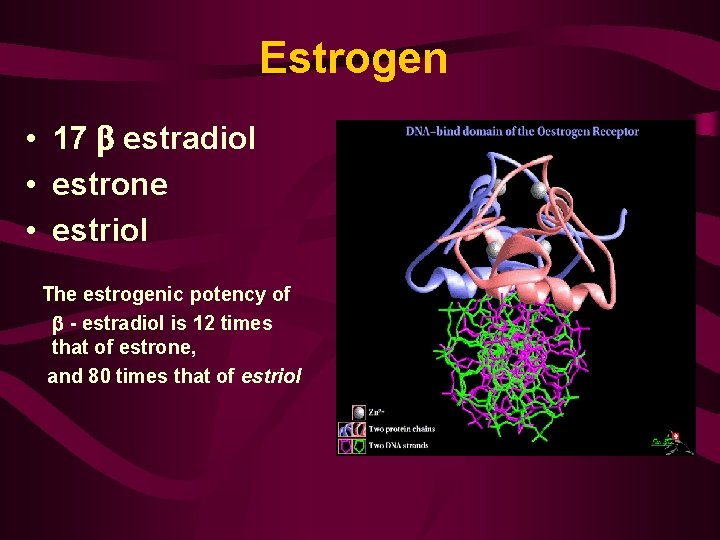
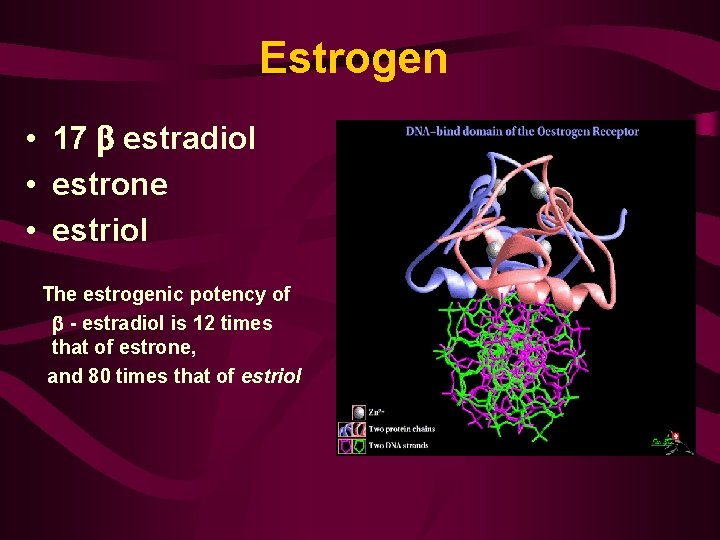
Estrogen • 17 estradiol • estrone • estriol The estrogenic potency of - estradiol is 12 times that of estrone, and 80 times that of estriol

Estrogen • changes the vaginal epithelium from a cuboidal into a stratified type • causes the proliferation of the endometrial stroma and endometrial glands and increases the number of cilia in the fallopian tubes. • cause increased osteoblastic activity and they are responsible for the peak of growth rate during puberty. • initiate growth of the breast and they are responsible for the characteristic appearance of the mature female breast.
Estrogen • cause uniting of the epiphyses of the long bones and this in turn ceases the growth about the time of menarche. • cause deposition of fat in the subcutaneous tissue, breasts, buttocks and thighs - that give the characteristic female shape. • affect hair development in the pubic and axillary regions. • acts on the skin and makes it soft and more vascular which increases the warmth of female skin.

Menopause • At the age of 40 to 50 years the sexual cycles usually become irregular , and ovulation fails to occur during many of the cycles. • The menopause is defined as the final episode of menstrual bleeding in women. • However, the term is used commonly to refer to the period of several years before and after the menopause.
Symptoms of Menopause q depression !!! q hot flushes / due to vascular instability / q psychic sensations of dyspnea q irritability q fatigue q anxiety q atrophy of the urogenital epithelium and skin q decreased size of the breasts q osteoporosis
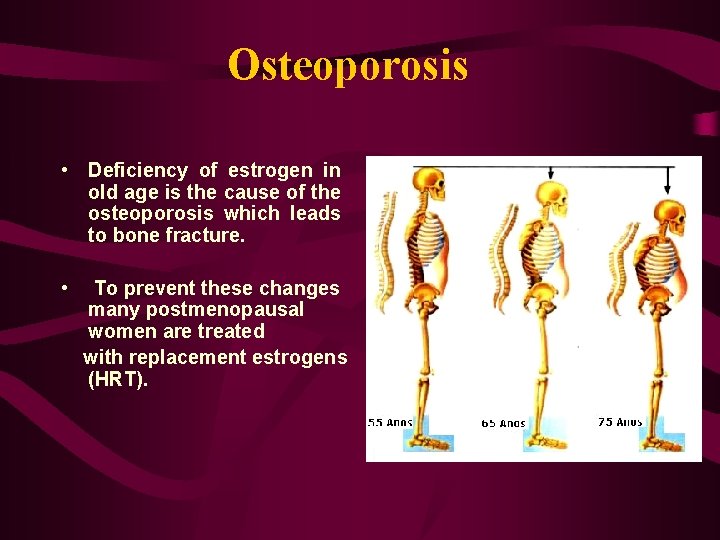
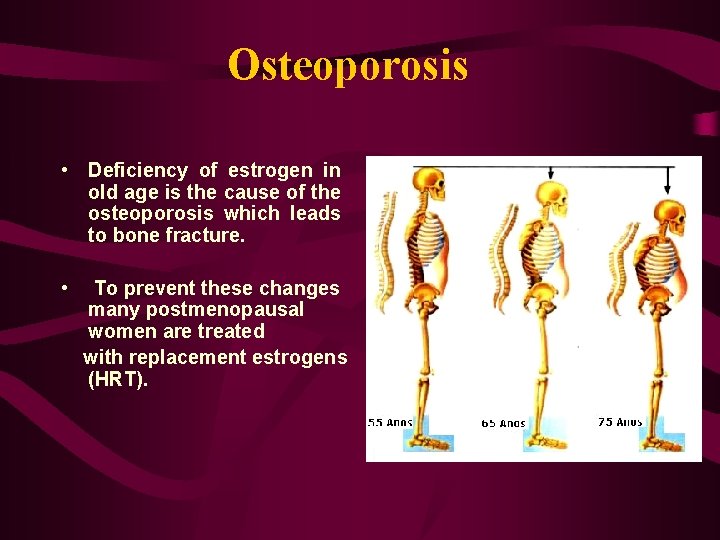
Osteoporosis • Deficiency of estrogen in old age is the cause of the osteoporosis which leads to bone fracture. • To prevent these changes many postmenopausal women are treated with replacement estrogens (HRT).
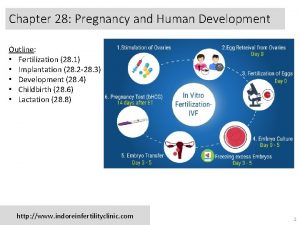
Pregnancy

PREGNANCY Edyta Mądry MD, Ph. D Department of Physiology Medical University Poznań 54
Pregnancy Definition The period from conception to birth. 55
Conception • Conception means a woman's egg has been fertilized by a man's sperm. 56
Conception • A secondary oocyte can be fertilized for about 24 hours after ovulation • Sperm remain viable for up to 72 hours within the female reproductive tract 57

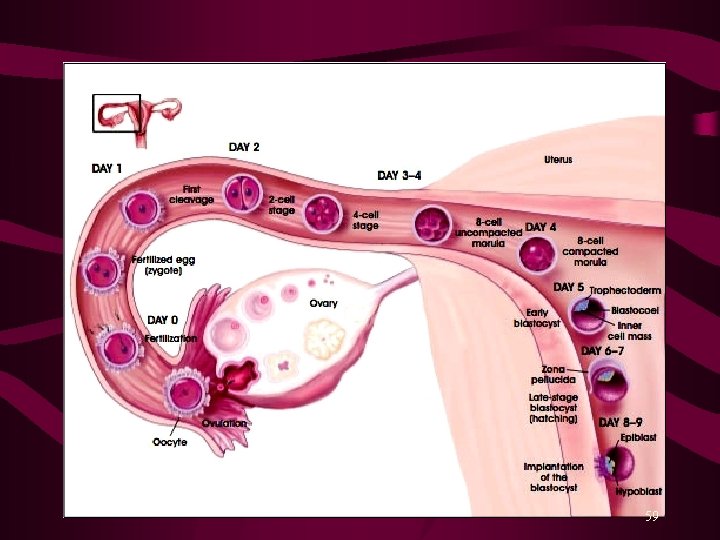
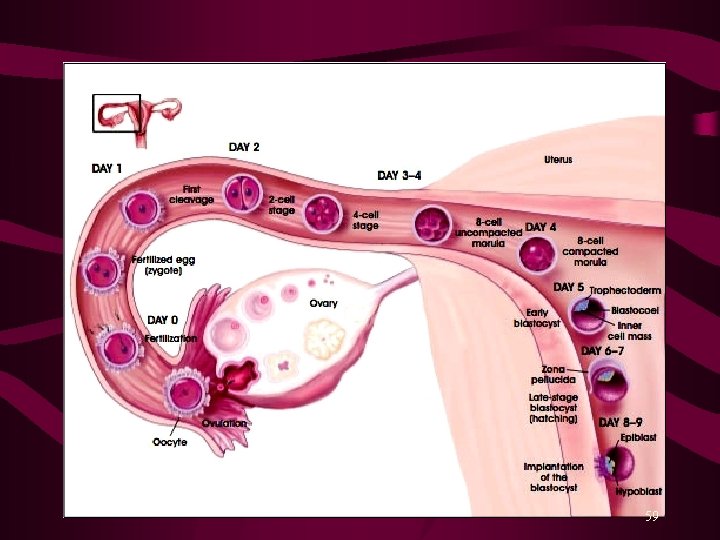
Fertilization • Fertilization usually takes place in the outer one-third of the uterine tube (ampulla of oviduct), but can ocasionaly take place in the abdominal cavity cervics of uterus (ectopic pregnancy) • Sperm swim up the female reproductive tract, aided by muscular contractions of the uterus stimulated by prostaglandins in the semen. 58
59

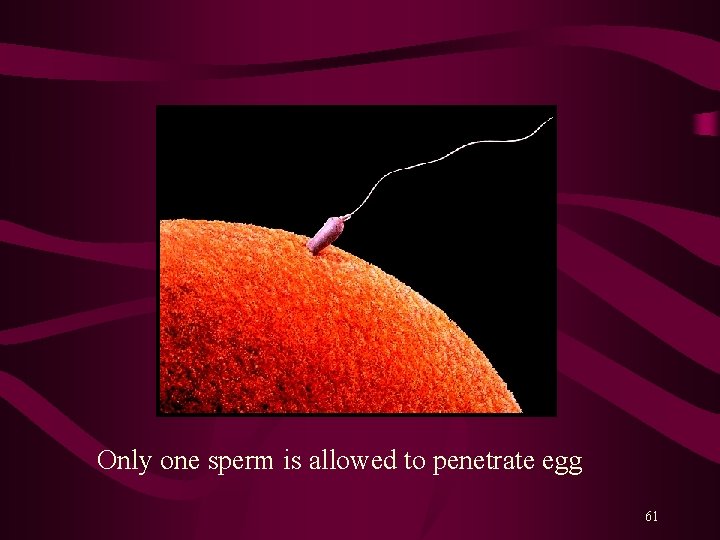
How does it start? • Sperm reach ovum and cluster around it 60
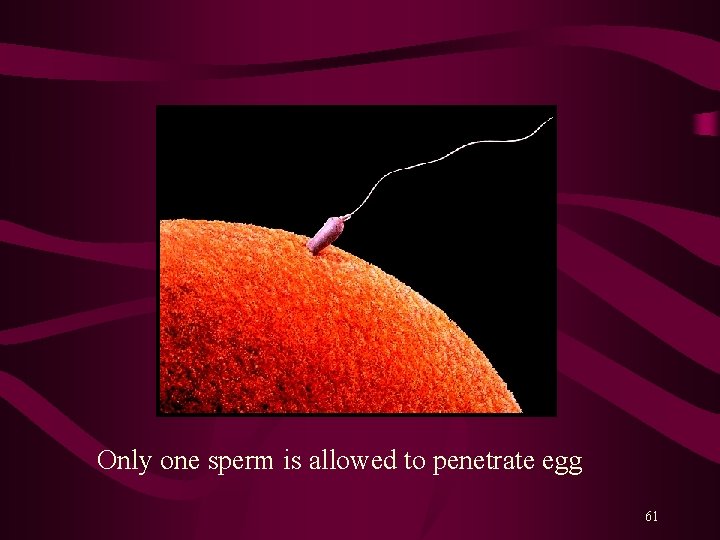
Only one sperm is allowed to penetrate egg 61
Gestation in singleton pregnancies lasts an average of 40 weeks (280 days) from the first day of the last normalmenstrual period (LNMP). • Assumption: Fertilized 14 days after the first day of LNMP Gives birth 38 weeks after fertilization (+ or - 2 weeks) 10 lunar months = 9 calendar months = 280 days (+ or – 2 weeks) 62
How to calculate the time of birth Naegele's rule 1. Determine first day of LNMP 2. Add one year 3. Subtract three months 4. Add seven days For example: first day of LNMP April 21 st, 2015 Resulting data of estimated data of birth : January 28 , 2016 (+ or – 2 weeks ) 63
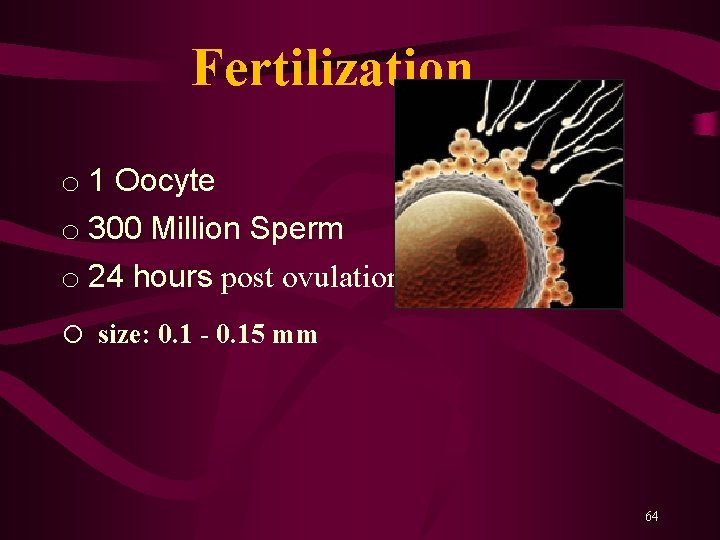
Fertilization o 1 Oocyte o 300 Million Sperm o 24 hours post ovulation o size: 0. 1 - 0. 15 mm 64
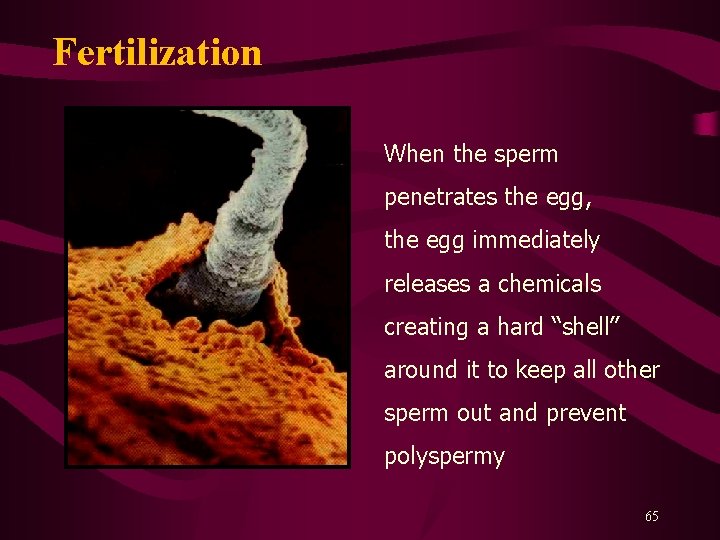
Fertilization When the sperm penetrates the egg, the egg immediately releases a chemicals creating a hard “shell” around it to keep all other sperm out and prevent polyspermy 65
Fertilization • FERTILIZED EGG = ZYGOTE • The fertilization process takes about 24 hours. – It takes about ten hours to navigate the female productive track, moving up the vaginal canal, through the cervix, and into the fallopian tube where fertilization begins. 66

Cleavage • First Cell Division, • Mitotic division • size 0. 1 - 0. 2 mm • 1. 5 - 3 days post-ovulation 67

2 cell zygote The zygote begins to develop 4 cell zygote 68
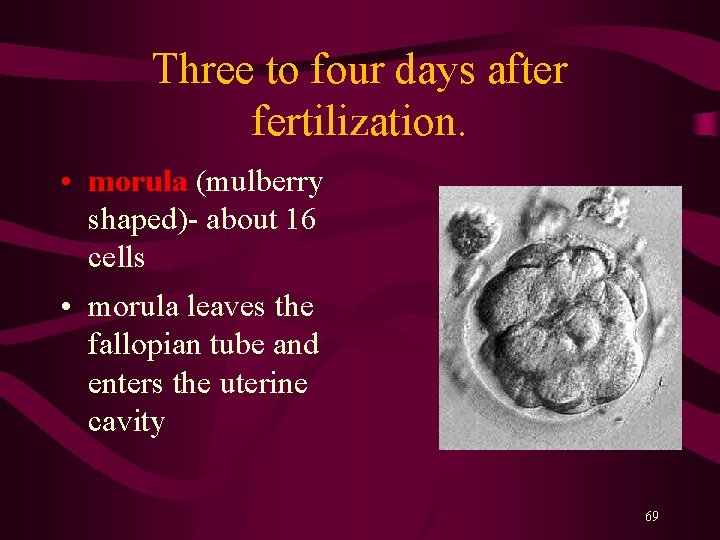
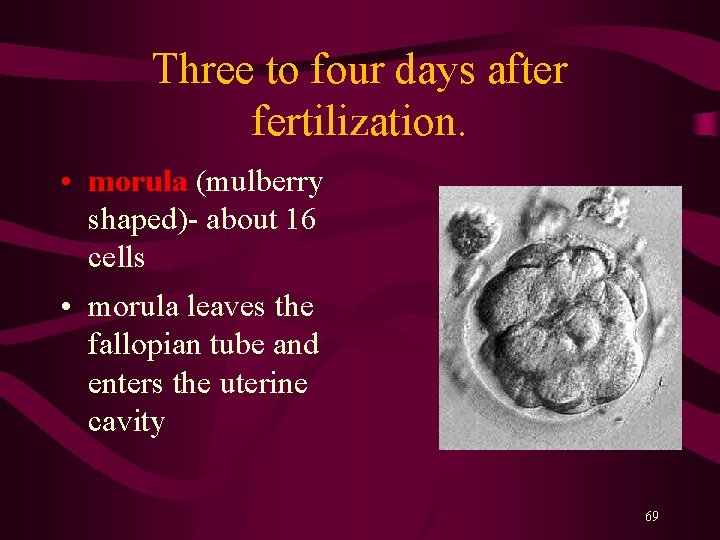
Three to four days after fertilization. • morula (mulberry shaped)- about 16 cells • morula leaves the fallopian tube and enters the uterine cavity 69

8 cell zygote 16 cell morula 70

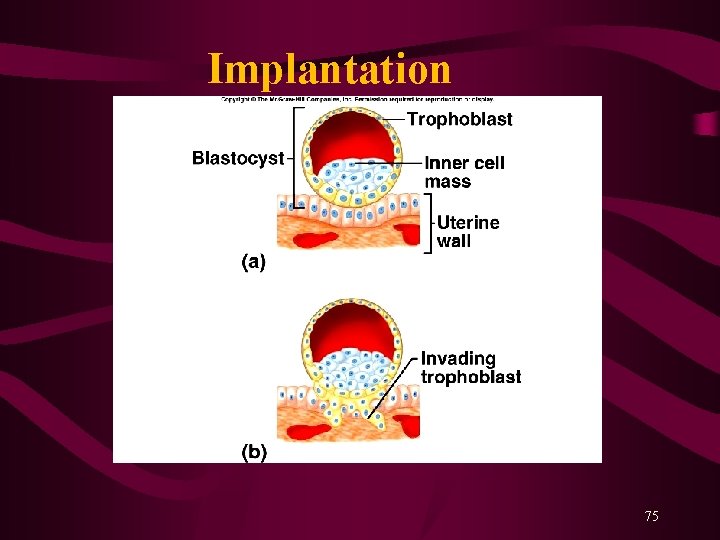
Early Blastocyst • When zygote divides to 32 cells it • • • becomes known as a blastocyst size 0. 1 - 0. 2 mm 4 days post-ovulation blastocyst formation • Two cell types are forming: – embryoblast (inner cell mass on the inside of the blastocele) – trophoblast (the cells on the outside of the blastocele). 71

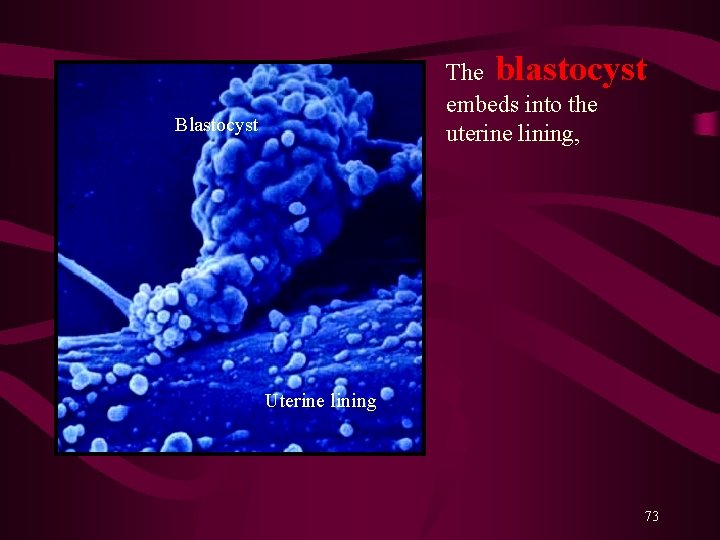
Implantation Begins • Human Chorionic Gonadotropin (h. CG) level rise • 0. 1 - 0. 2 mm • 5 - 6 days post-ovulation • The trophoblast cells secretes an enzyme which erodes the epithelial uterine lining and creates an implantation site for the blastocyst (see slide number 22) 72
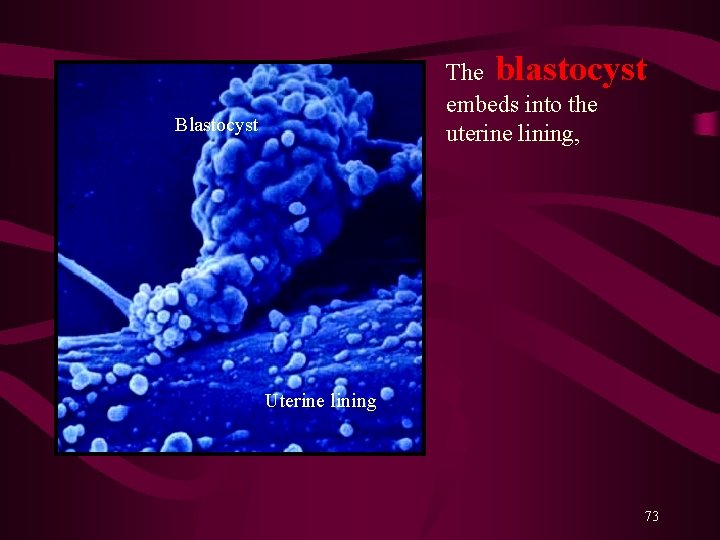
The blastocyst embeds into the uterine lining, Blastocyst Uterine lining 73

Implantation • ovary continues producing progesterone • trophoblast cells continue releasing human chorionic gonadotropin (h. CG) • Endometrial glands in the uterus enlarge in response to the blastocyst and the implantation site becomes swollen with new capillaries ( see slaids 26 and 27). 74
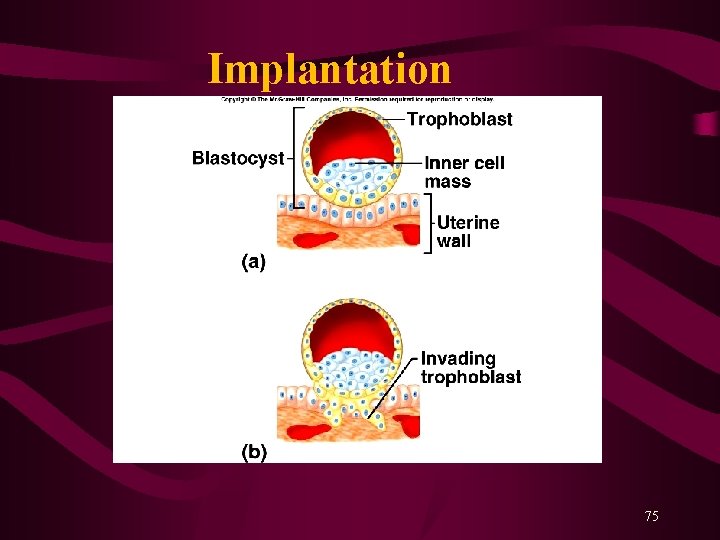
Implantation 75
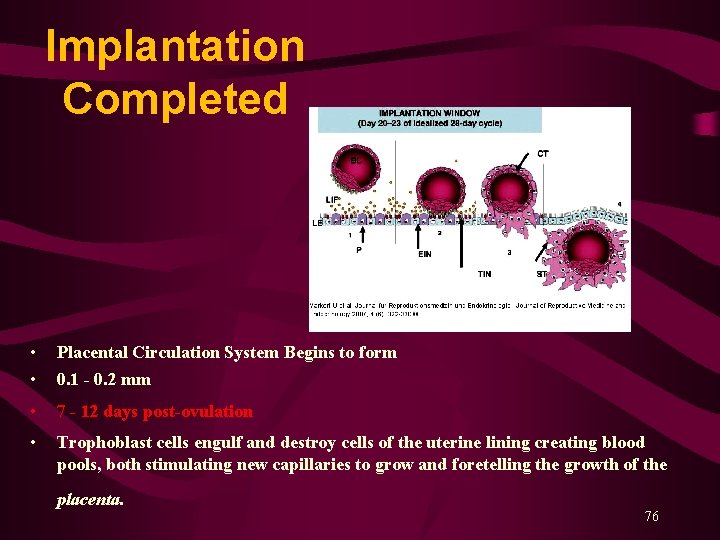
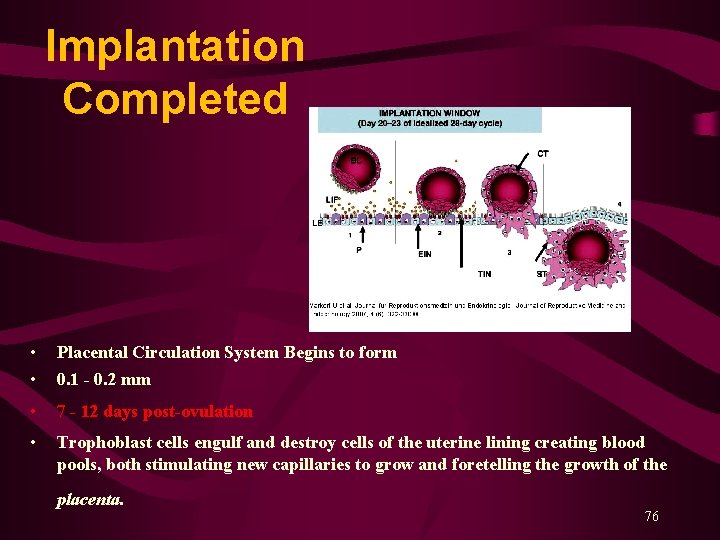
Implantation Completed • • Placental Circulation System Begins to form 0. 1 - 0. 2 mm • 7 - 12 days post-ovulation • Trophoblast cells engulf and destroy cells of the uterine lining creating blood pools, both stimulating new capillaries to grow and foretelling the growth of the placenta. 76
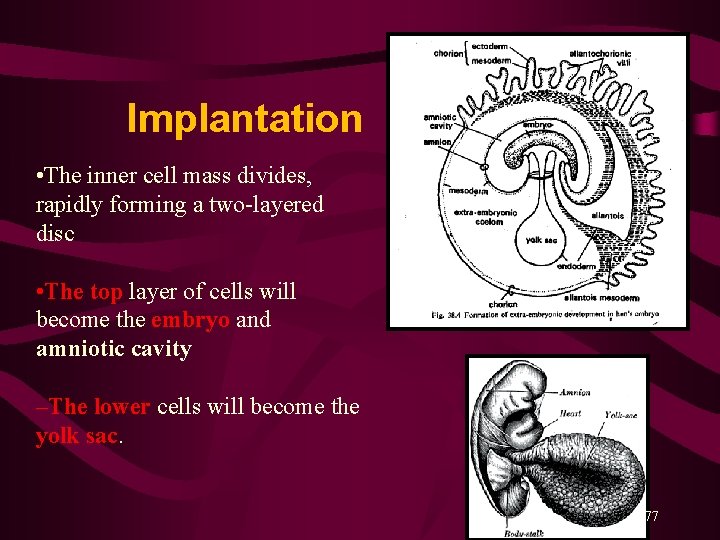
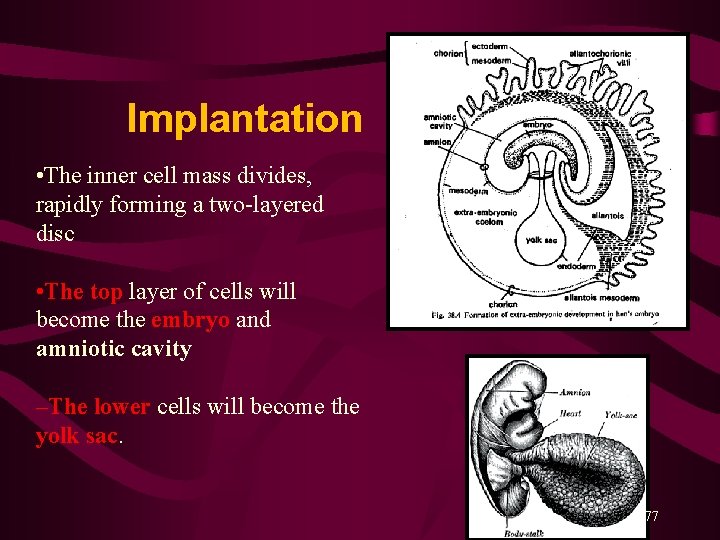
Implantation Completed • The inner cell mass divides, rapidly forming a two-layered disc • The top layer of cells will become the embryo and amniotic cavity –The lower cells will become the yolk sac. 77
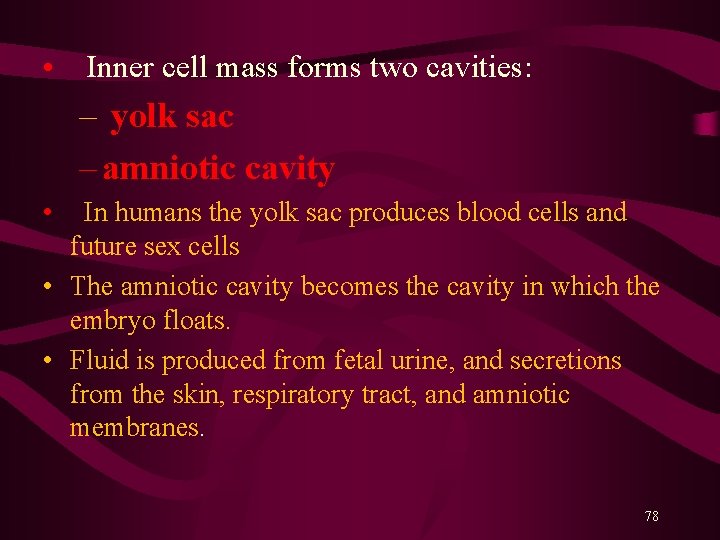
• Inner cell mass forms two cavities: – yolk sac – amniotic cavity • In humans the yolk sac produces blood cells and future sex cells • The amniotic cavity becomes the cavity in which the embryo floats. • Fluid is produced from fetal urine, and secretions from the skin, respiratory tract, and amniotic membranes. 78
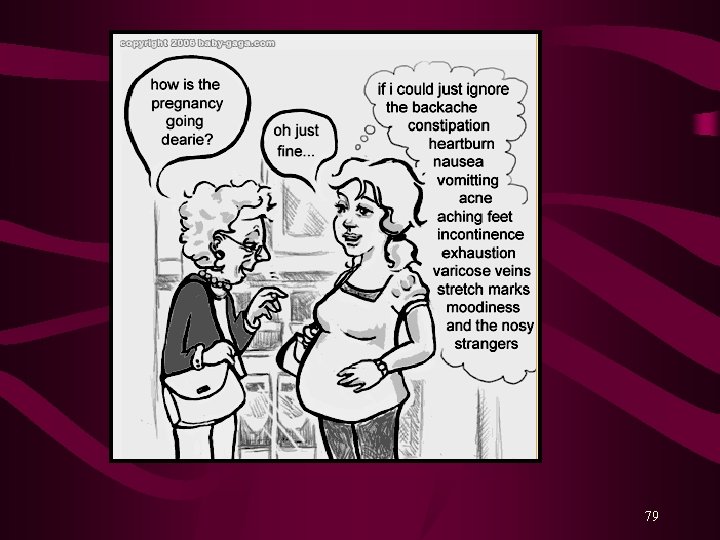
79

Symptoms of early pregnancy Food cravings or aversions Smell sensitivity Heartburn Missed Period Morning Sickness Constipation Mood Swings/ Irritability Higher body temperature Low Back Pain Tender breast Bloating / Weight Gain Fatigue 80
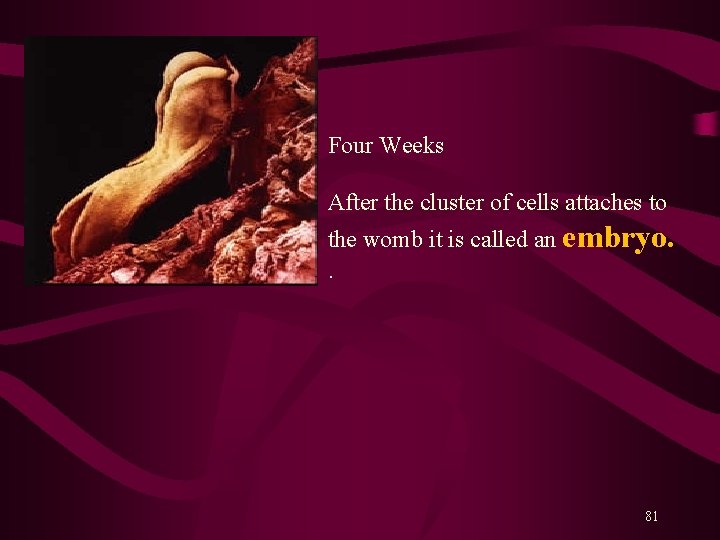
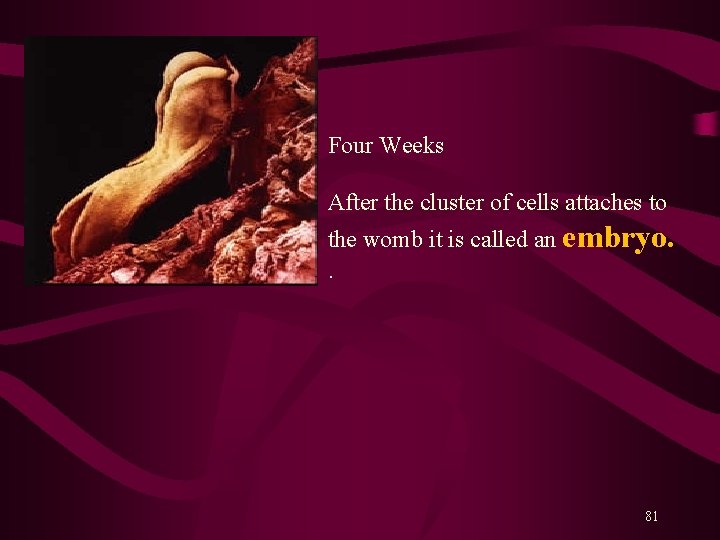
Four Weeks After the cluster of cells attaches to the womb it is called an embryo. . 81

Day 24 Day 22 82

Day 26 Day 28 83
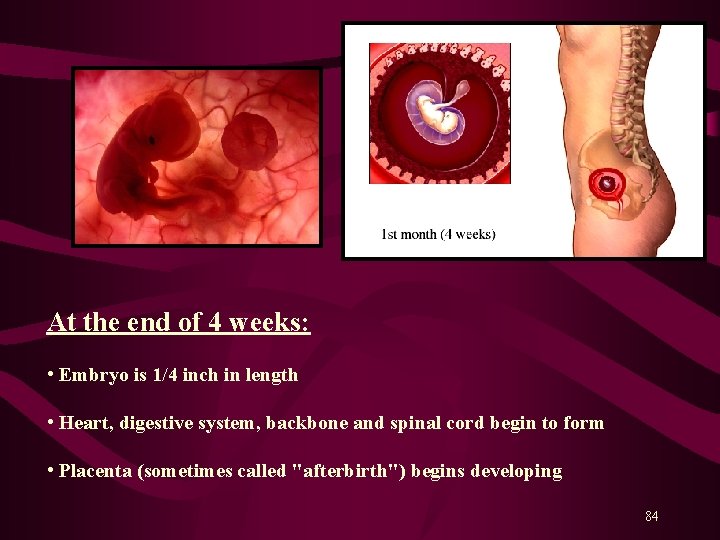
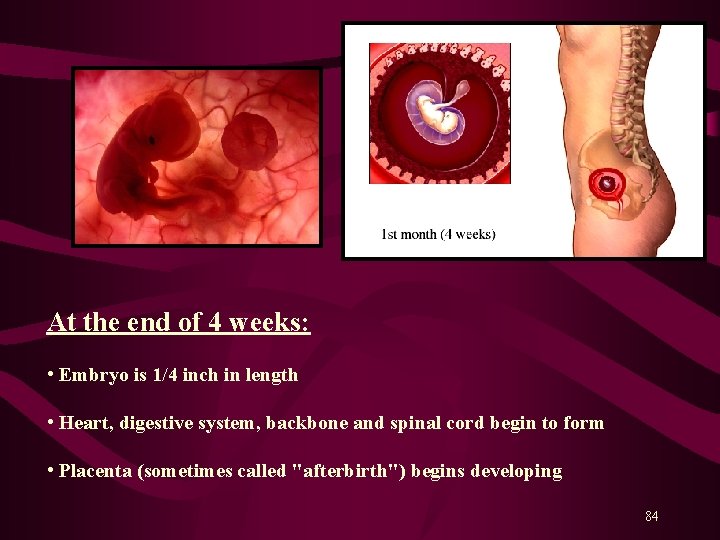
At the end of 4 weeks: • Embryo is 1/4 inch in length • Heart, digestive system, backbone and spinal cord begin to form • Placenta (sometimes called "afterbirth") begins developing 84
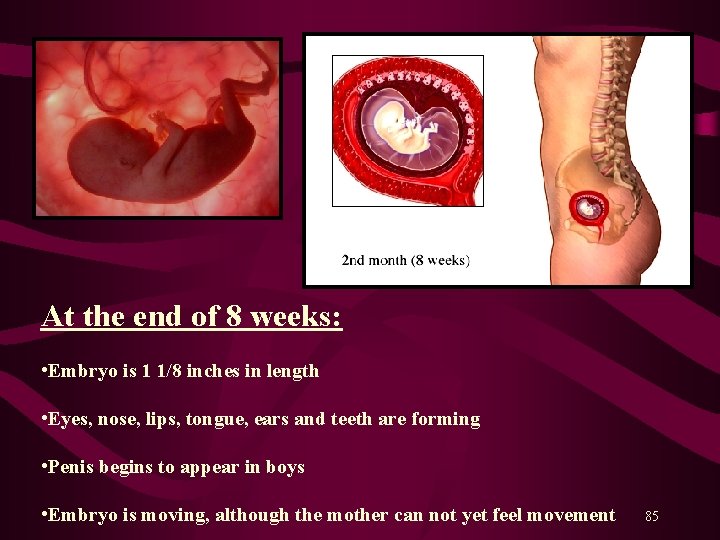
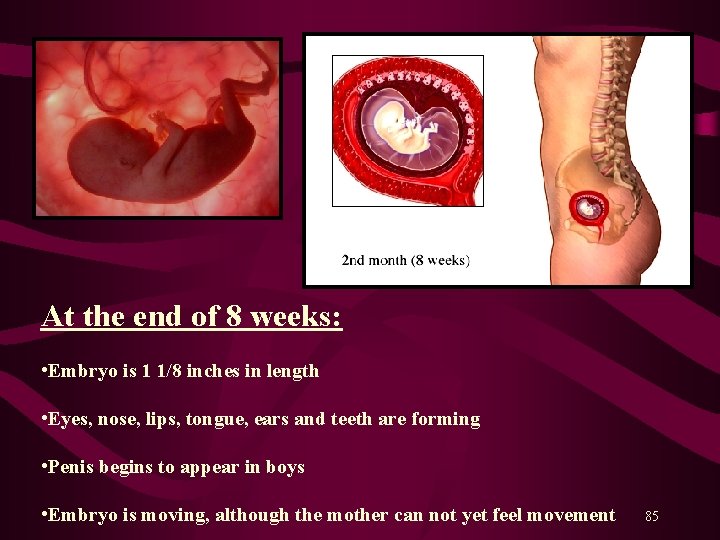
At the end of 8 weeks: • Embryo is 1 1/8 inches in length • Eyes, nose, lips, tongue, ears and teeth are forming • Penis begins to appear in boys • Embryo is moving, although the mother can not yet feel movement 85
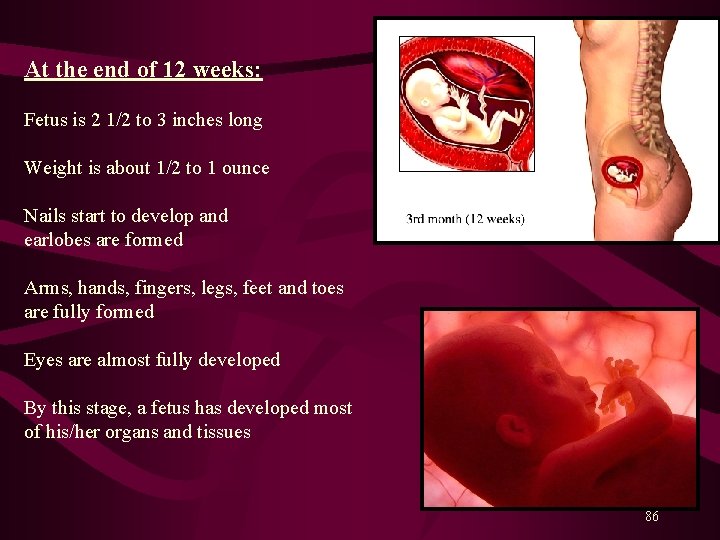
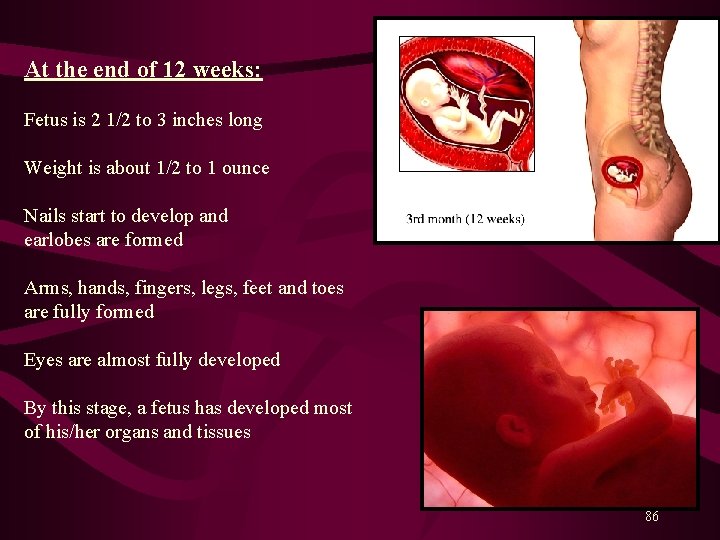
At the end of 12 weeks: Fetus is 2 1/2 to 3 inches long Weight is about 1/2 to 1 ounce Nails start to develop and earlobes are formed Arms, hands, fingers, legs, feet and toes are fully formed Eyes are almost fully developed By this stage, a fetus has developed most of his/her organs and tissues 86
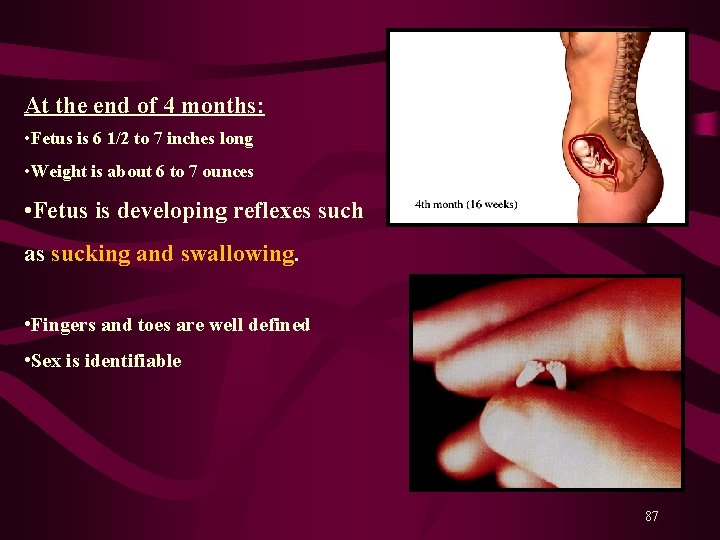
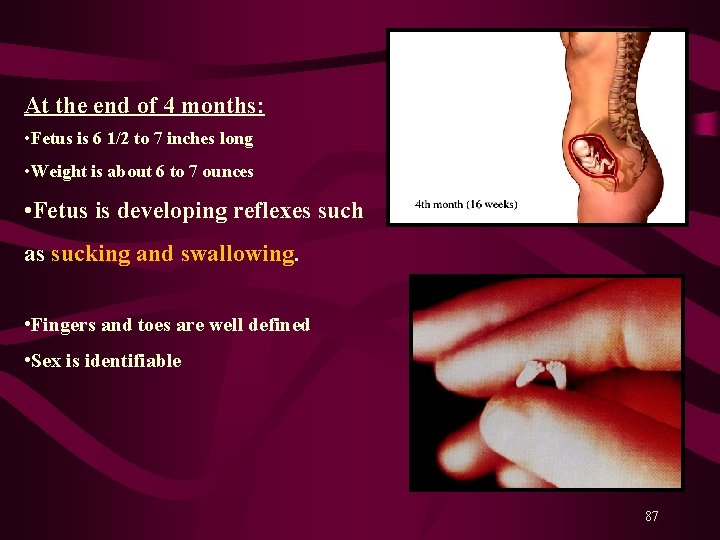
At the end of 4 months: • Fetus is 6 1/2 to 7 inches long • Weight is about 6 to 7 ounces • Fetus is developing reflexes such as sucking and swallowing. • Fingers and toes are well defined • Sex is identifiable 87

At the end of 5 months: • Fetus is 8 to 10 inches long • Weight is about 1 pound • Hair begins to grow on his/her head • Soft woolly hair called lanugo covers fetus body Mother begins to feel fetal movement 88
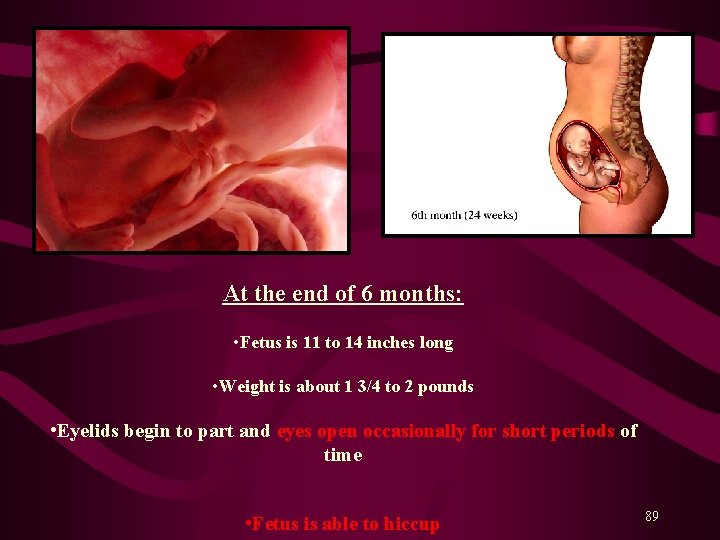
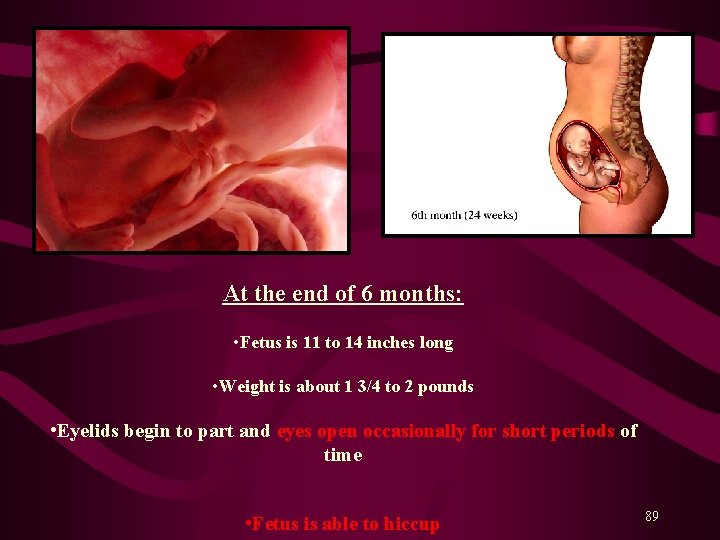
At the end of 6 months: • Fetus is 11 to 14 inches long • Weight is about 1 3/4 to 2 pounds • Eyelids begin to part and eyes open occasionally for short periods of time • Fetus is able to hiccup 89
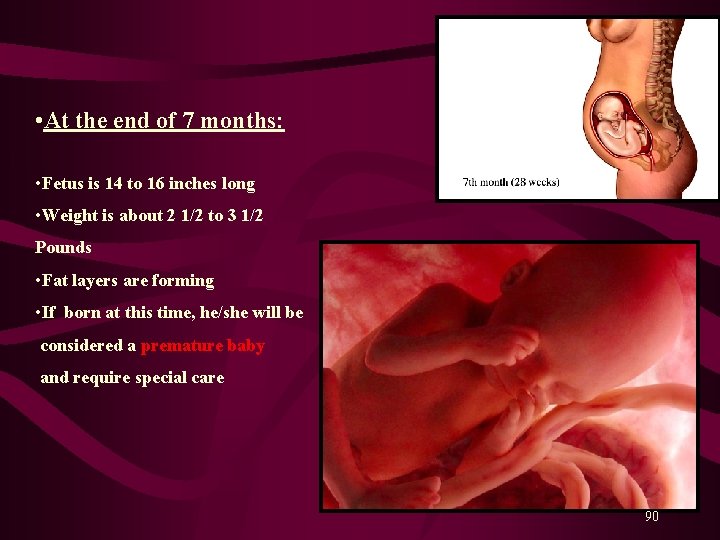
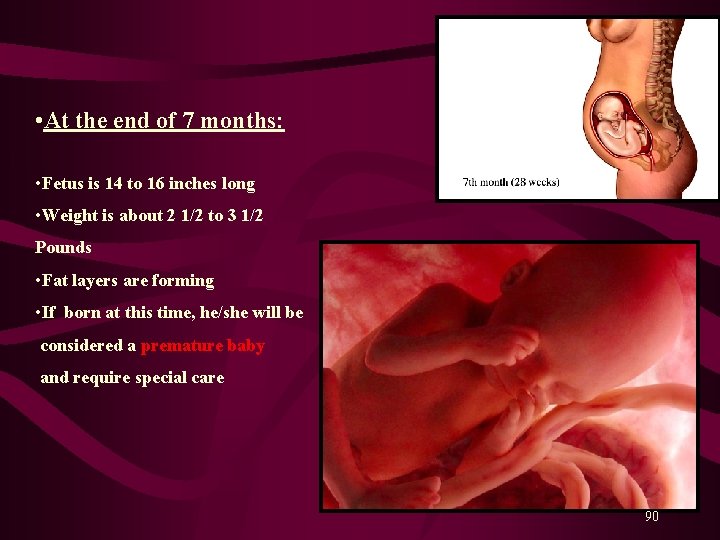
• At the end of 7 months: • Fetus is 14 to 16 inches long • Weight is about 2 1/2 to 3 1/2 Pounds • Fat layers are forming • If born at this time, he/she will be considered a premature baby and require special care 90
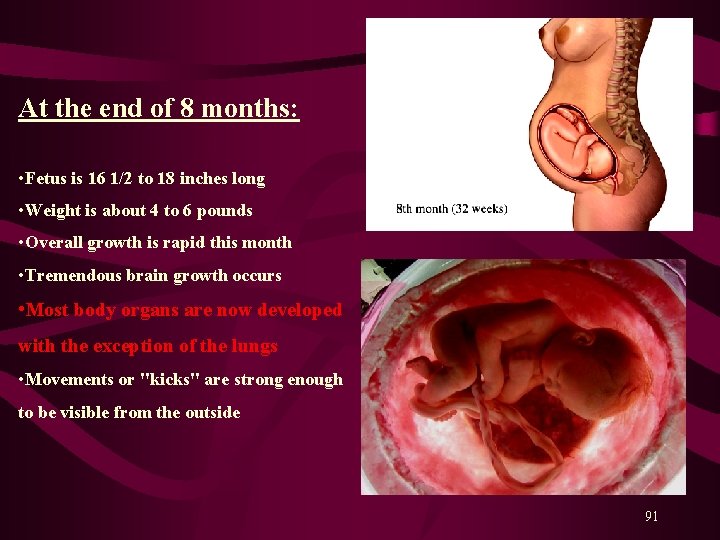
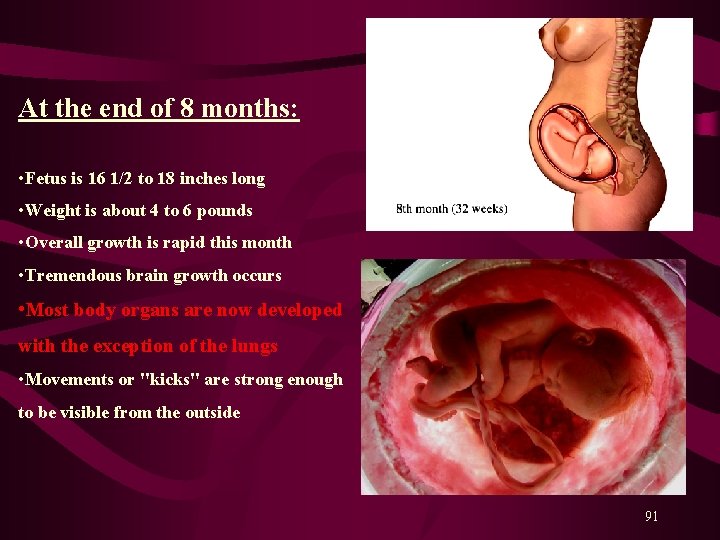
At the end of 8 months: • Fetus is 16 1/2 to 18 inches long • Weight is about 4 to 6 pounds • Overall growth is rapid this month • Tremendous brain growth occurs • Most body organs are now developed with the exception of the lungs • Movements or "kicks" are strong enough to be visible from the outside 91
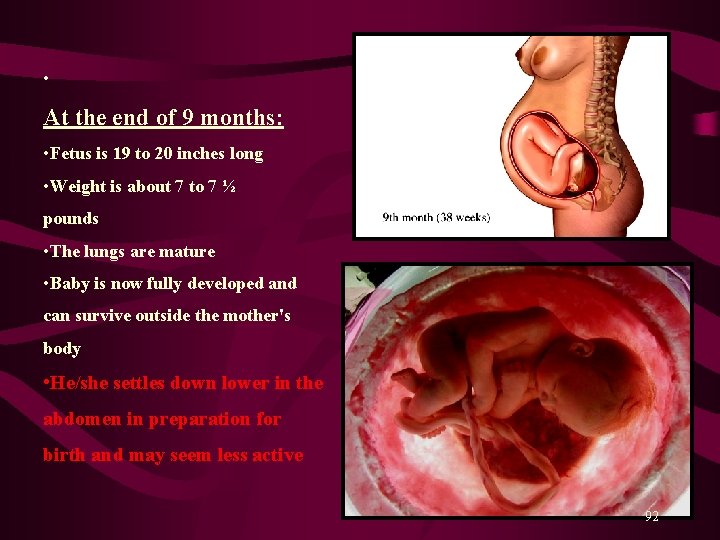
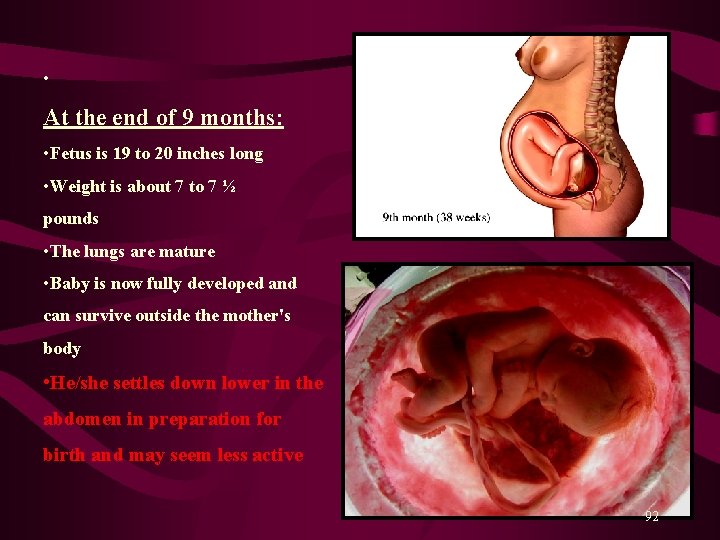
• At the end of 9 months: • Fetus is 19 to 20 inches long • Weight is about 7 to 7 ½ pounds • The lungs are mature • Baby is now fully developed and can survive outside the mother's body • He/she settles down lower in the abdomen in preparation for birth and may seem less active 92
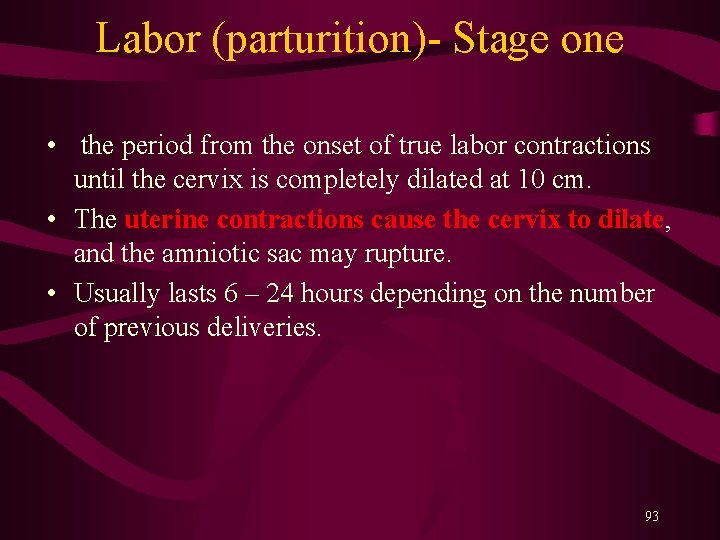
Labor (parturition)- Stage one • the period from the onset of true labor contractions until the cervix is completely dilated at 10 cm. • The uterine contractions cause the cervix to dilate, and the amniotic sac may rupture. • Usually lasts 6 – 24 hours depending on the number of previous deliveries. 93
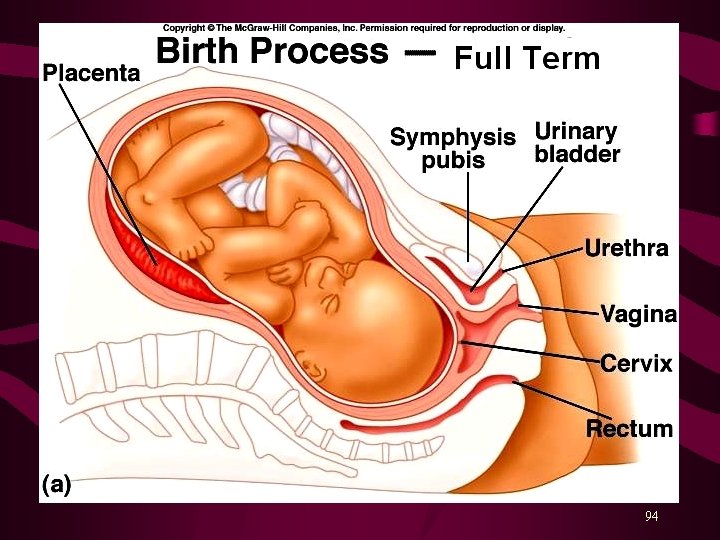
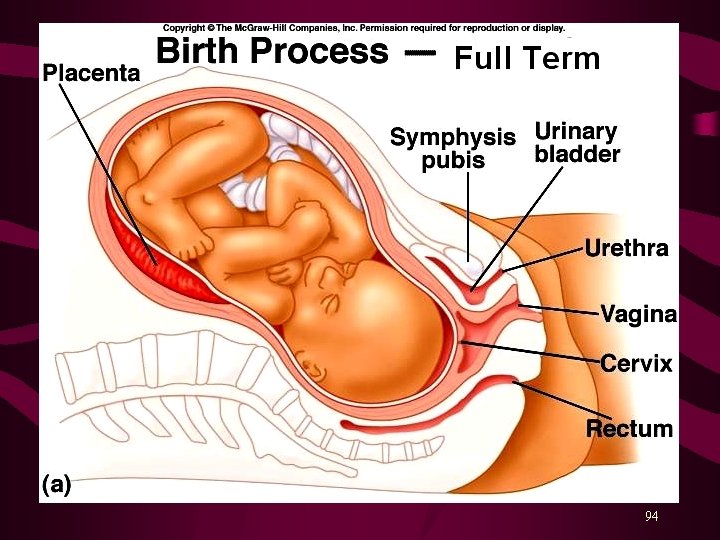
94

95
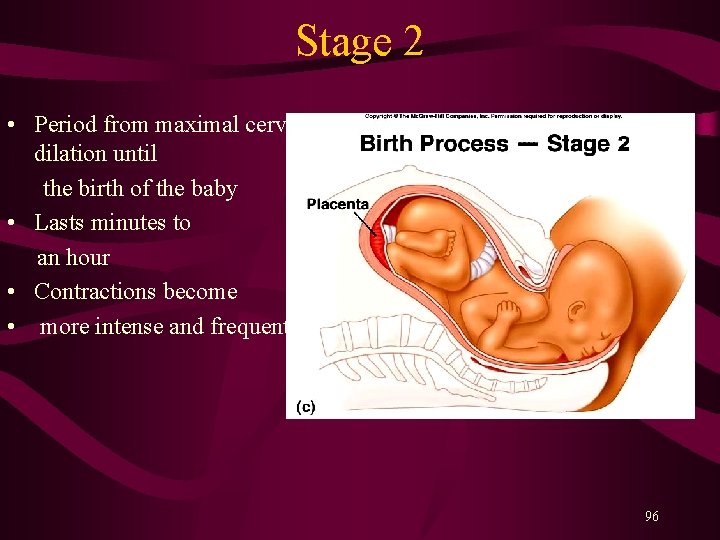
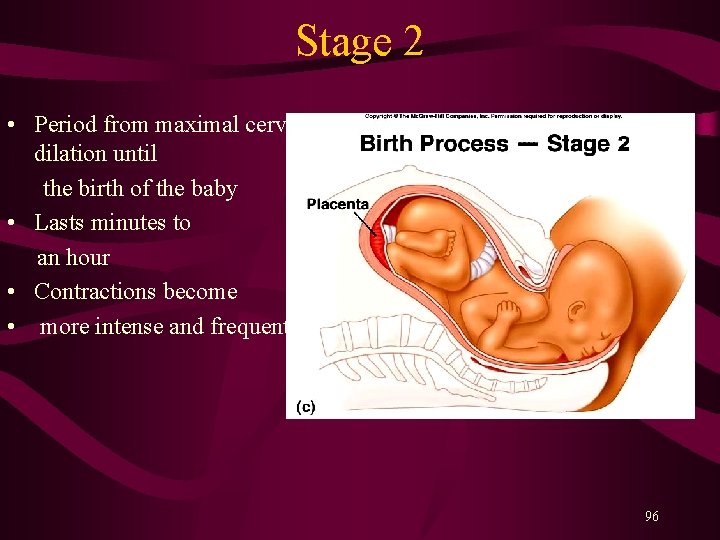
Stage 2 • Period from maximal cervical dilation until the birth of the baby • Lasts minutes to an hour • Contractions become • more intense and frequent. 96
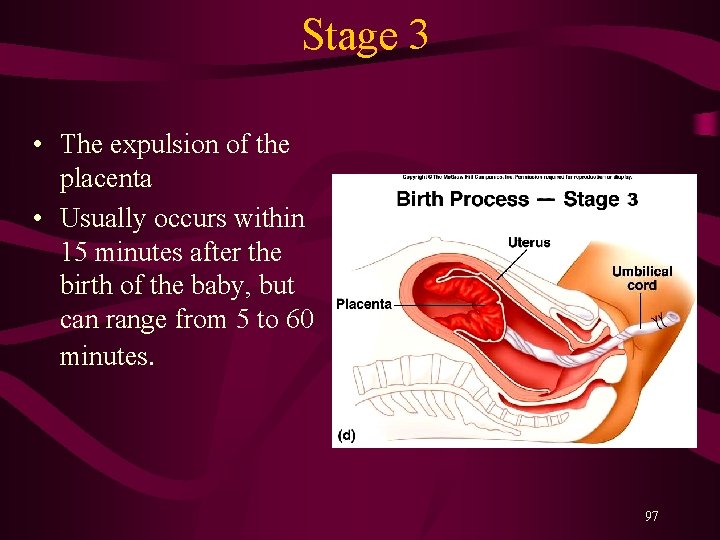
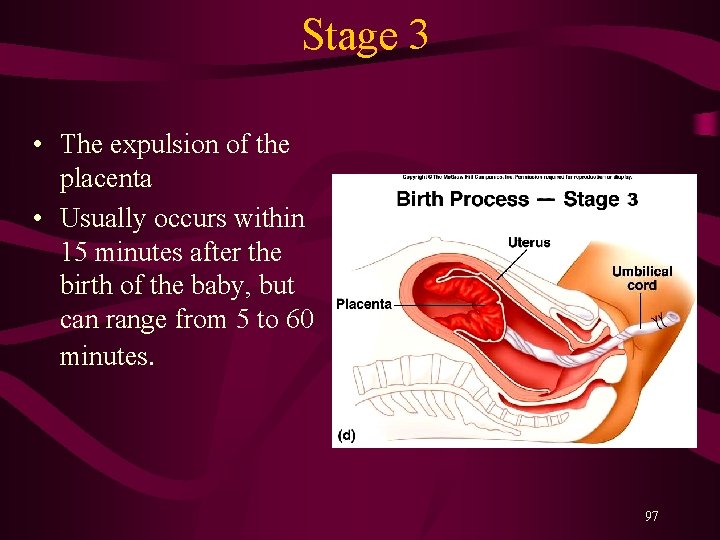
Stage 3 • The expulsion of the placenta • Usually occurs within 15 minutes after the birth of the baby, but can range from 5 to 60 minutes. 97

98
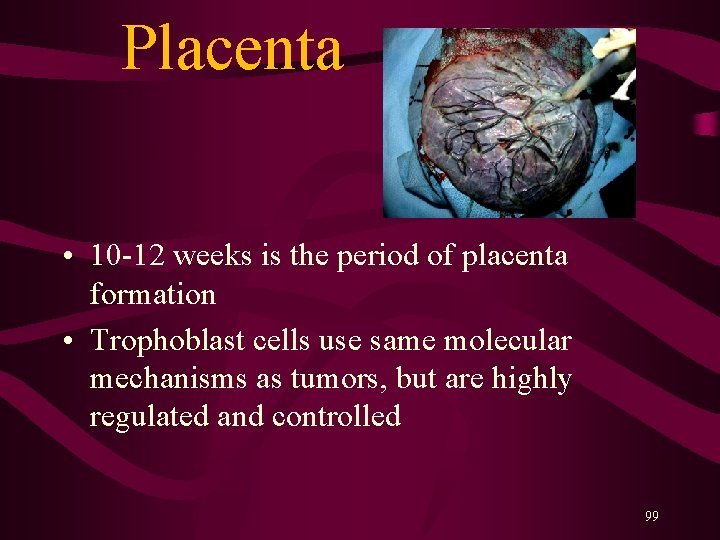
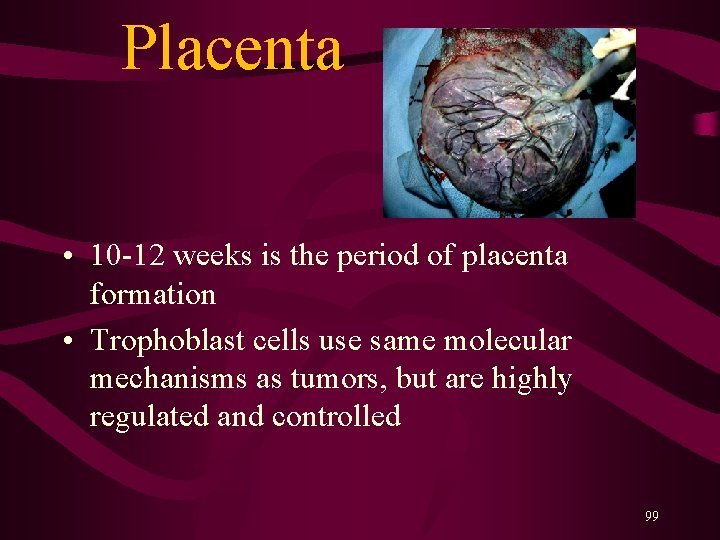
Placenta • 10 -12 weeks is the period of placenta formation • Trophoblast cells use same molecular mechanisms as tumors, but are highly regulated and controlled 99
Placenta • FETAL SIDE • MATERNAL SIDE • They provide… – protection – nutrition – respiration – excretion – hormone production 100

Functions of Placenta • Exchange of gases between fetus and mother • Delivery of nutrients from mother to fetus • Delivery of antibodies from mother to fetus • Removal of fetus waste • Secretion of hormons including human chorionic gonadotropin ( h. CG), progesterone, estrogen, and human chorinic somatotropin (h. CS) 101
Placental barrier • Maternal and fetal blood do not mix- “placental barrier” 102
Metabolic Functions of the Placenta • Glycogen synthesis and storage • Cholesterol synthesis: placental cholesterol is precursor for placental progesterone and estrogens • Protein production 103
Endocrine Functions • Placenta Produces Peptide hormones – Human Chorionic gonodotrophin (h. CG) - secreted early and helps to maintain synthesis of progesterone – Human placental lactogen (h. PL): increase supply of glucose to future by decreasing maternal stores of fatty acids by altering maternal secretion of insulin – Insulin-like growth factors (IGF): IGF signaling system is a major regulator of growth in fetus and infant 104
Endocrine Functions • Steroid hormones – Progesterone: produced by placenta, needed to maintain non-contractile uterus – Estrogen: produced by placenta drives many processes in pregnancy 105

How important are hormones ? An XY individual with androgen insensitivity syndrome. Despite the XY karyotype and the presence of testes, such individuals develop female secondary sex characteristics. Internally, however, these women lack the Müllerian duct derivatives and have undescended testes. (Photograph courtesy of C. B. Hammond. ) 106
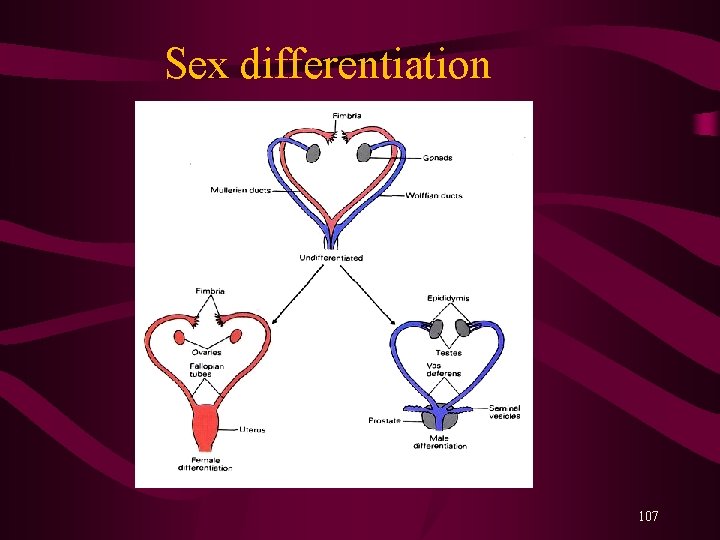
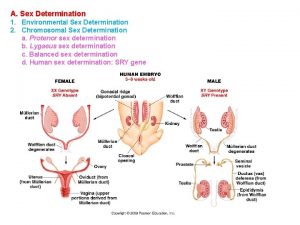
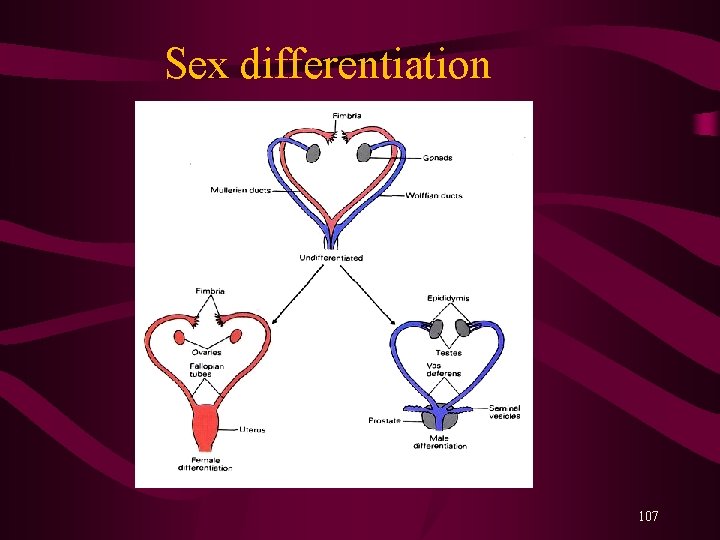
Sex differentiation 107
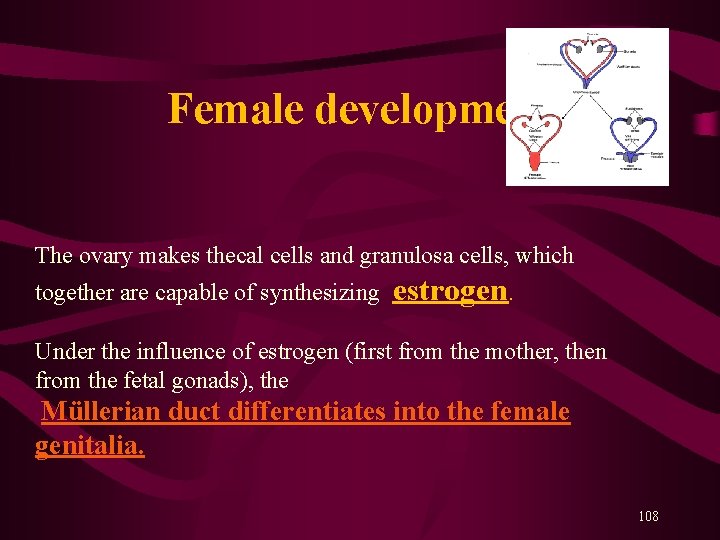
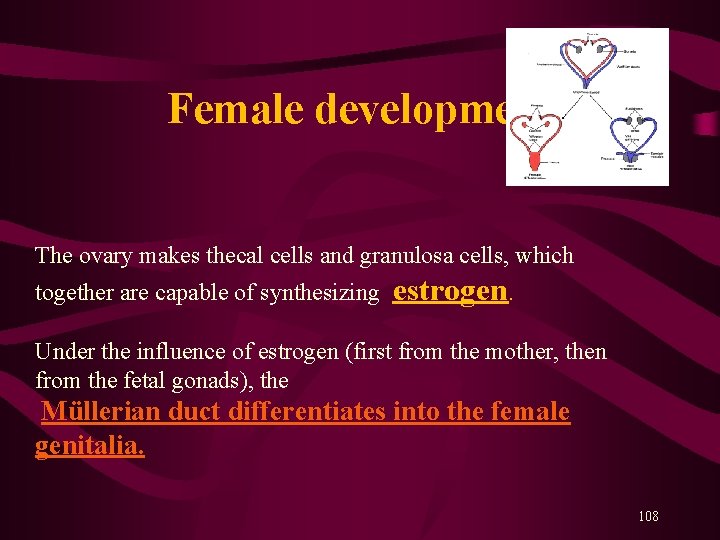
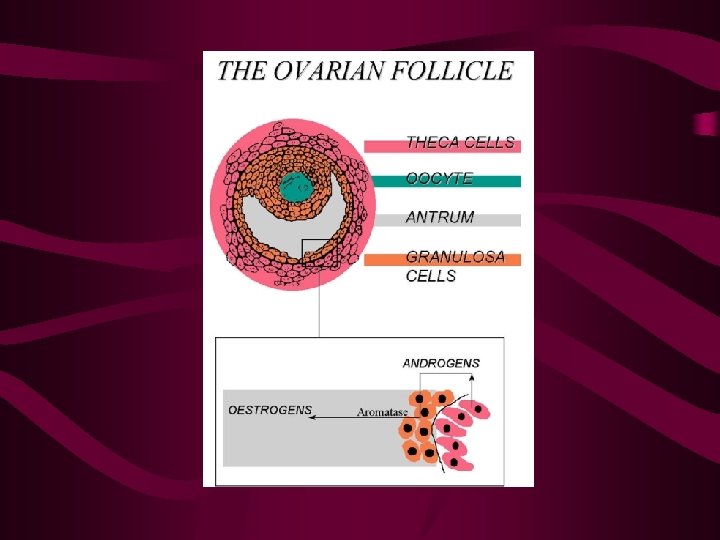
Female development The ovary makes thecal cells and granulosa cells, which together are capable of synthesizing estrogen. Under the influence of estrogen (first from the mother, then from the fetal gonads), the Müllerian duct differentiates into the female genitalia. 108

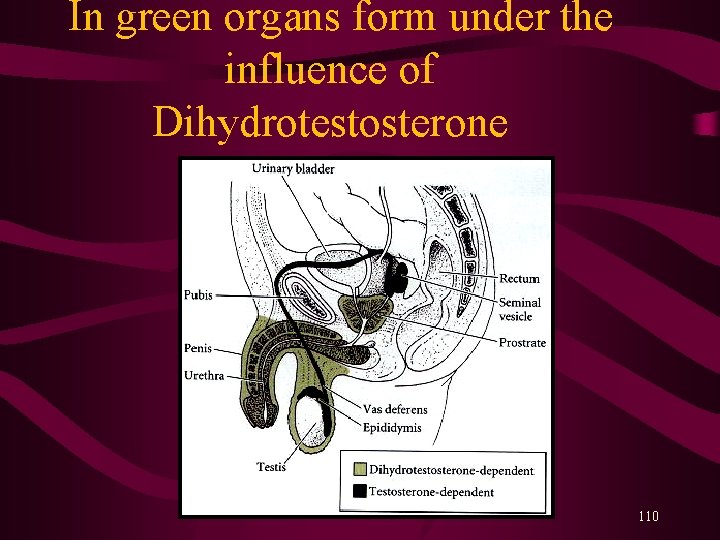
3 hormones necessary for male development 1. Müllerian Inhibiting Substance (MIS) = anti-Müllerian duct factor (AMH), causes the Müllerian duct to regress. 2. Testosterone, causes the differentiation of the Wolffian duct into the male internal genitalia. In the urogenital region, testosterone is converted into 3. Dihydrotestosterone (DHT), that causes the morphogenesis of the external genitali (penis) and prostate gland. 109
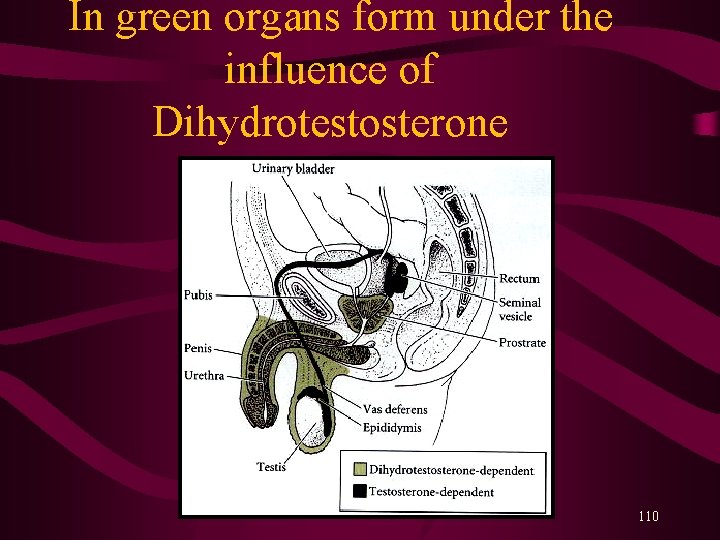
In green organs form under the influence of Dihydrotestosterone 110
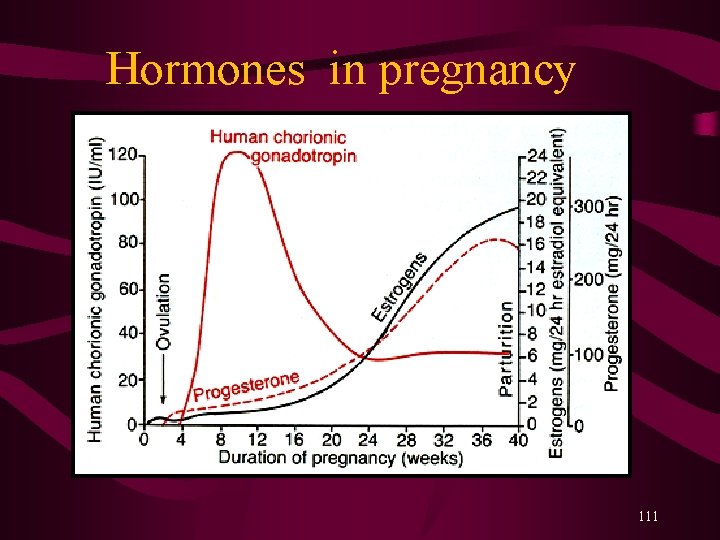
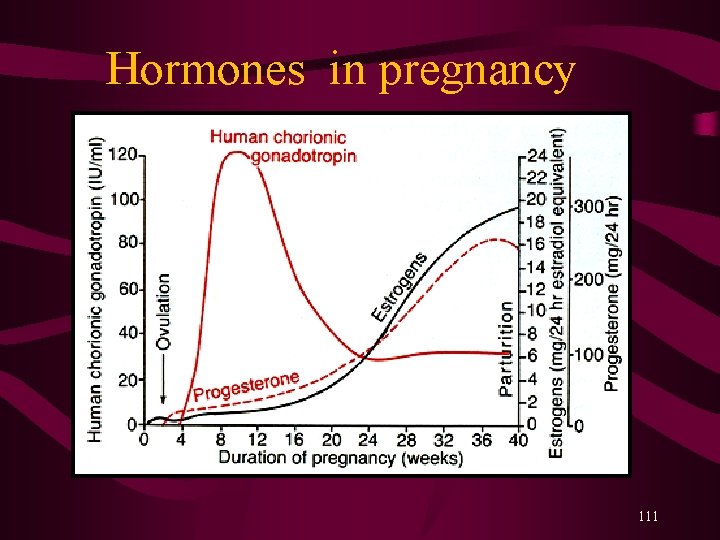
Hormones in pregnancy 111

Function of Human Chorionic Gonadotropin • Prevent degeneration of the corpus luteum • Stimulates the corpus luteum to secrete estrogen and progesteron • Stimulates steroid synthesis in the developing fetal adrenals • Stimulates fetal gonads, especially testosteron production by the fetal testes. • Suppresses maternal lymphocytes and reduces the possibility of immunoreactions against the fetus. 112
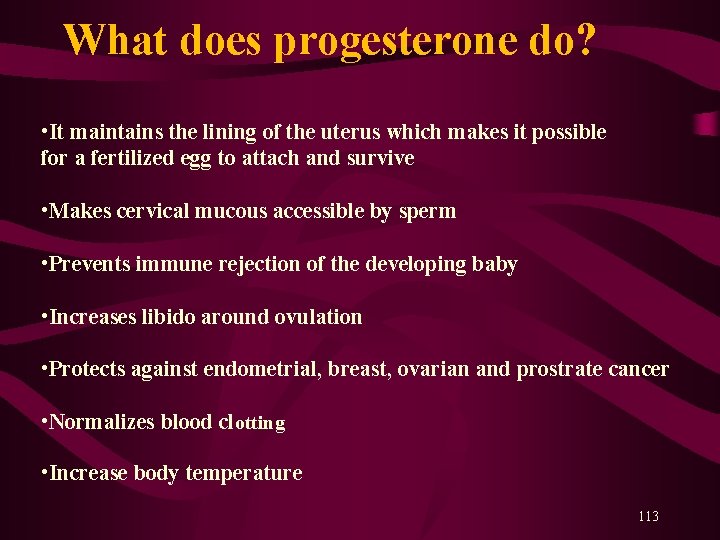
What does progesterone do? • It maintains the lining of the uterus which makes it possible for a fertilized egg to attach and survive • Makes cervical mucous accessible by sperm • Prevents immune rejection of the developing baby • Increases libido around ovulation • Protects against endometrial, breast, ovarian and prostrate cancer • Normalizes blood clotting • Increase body temperature 113
 Male and female hormones
Male and female hormones Male and female hormones
Male and female hormones Xxtesticles
Xxtesticles Sex sex sex
Sex sex sex Kurt bumby
Kurt bumby Sex sex sex
Sex sex sex Greenhouse sex
Greenhouse sex Androgen insensitivity
Androgen insensitivity Common lisp assoc
Common lisp assoc American angus association login
American angus association login Hormones after sex
Hormones after sex Uncircumcised gentiles photos
Uncircumcised gentiles photos Base of prostate gland
Base of prostate gland Combining form for semen
Combining form for semen Sex determination and sex linkage
Sex determination and sex linkage Once a sex offender always a sex offender
Once a sex offender always a sex offender Sex linkage
Sex linkage Sex linked punnett squares
Sex linked punnett squares Ladybug landing on you
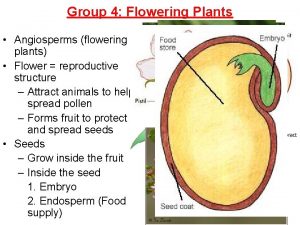
Ladybug landing on you Female parts of plants
Female parts of plants What is reproductive system
What is reproductive system Male vs female skull
Male vs female skull Red eyed female and white eyed male
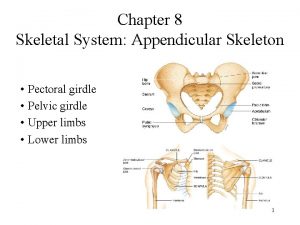
Red eyed female and white eyed male Appendicular skeleton pectoral girdle
Appendicular skeleton pectoral girdle Difference between male and female sharks
Difference between male and female sharks How do you know if a karyotype is male or female
How do you know if a karyotype is male or female Difference between male and female drosophila
Difference between male and female drosophila Male and female tortoise
Male and female tortoise External nares of frog
External nares of frog Male gaze vs female gaze
Male gaze vs female gaze Flowers are modified
Flowers are modified Lesson 14.2 male and female urinary structures
Lesson 14.2 male and female urinary structures Crossplay male to female
Crossplay male to female Female parts of plants
Female parts of plants Mitosis vs meiosis
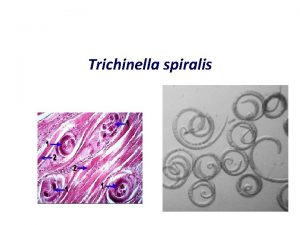
Mitosis vs meiosis Trichinella common name
Trichinella common name Zucchini male and female flowers
Zucchini male and female flowers Male and female parts of a plant
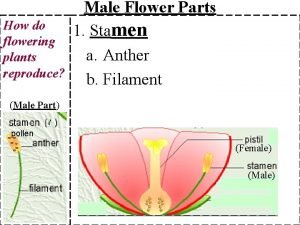
Male and female parts of a plant Sciatic notch male vs female
Sciatic notch male vs female Male vs female learning styles
Male vs female learning styles Major endocrine glands male and female
Major endocrine glands male and female Male and female gamete
Male and female gamete Similarities between male and female reproductive system
Similarities between male and female reproductive system Similarities between male and female reproductive system
Similarities between male and female reproductive system Shy lovers try positions that they can't handle
Shy lovers try positions that they can't handle Bispinous diameter
Bispinous diameter Punnett square for color blindness
Punnett square for color blindness Virtual skeleton identification lab
Virtual skeleton identification lab Aphi sada u rat yaya
Aphi sada u rat yaya Why is momentum p
Why is momentum p Blue jay male vs female
Blue jay male vs female Reproductive parts of a flower
Reproductive parts of a flower How many molars do adults have
How many molars do adults have Is it male or female
Is it male or female Chapter 16 matching questions 20-24
Chapter 16 matching questions 20-24 Pictures of a person born with both male and female parts
Pictures of a person born with both male and female parts Fetal pig gender
Fetal pig gender Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Bone bonanza lab answer key
Bone bonanza lab answer key Body farm pictures
Body farm pictures Frog testis labeled
Frog testis labeled Male vs female praying mantis
Male vs female praying mantis Anatomy of fish reproductive system
Anatomy of fish reproductive system Ascaris lumbricoides female cross section
Ascaris lumbricoides female cross section What is gonads
What is gonads Function of fsh
Function of fsh Theca interna
Theca interna Male reproductive system
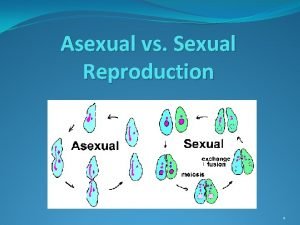
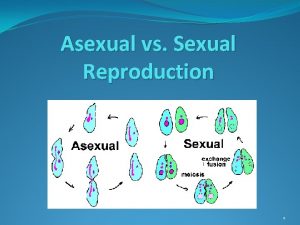
Male reproductive system Sexual reproduction vs asexual reproduction venn diagram
Sexual reproduction vs asexual reproduction venn diagram Sexual reproduction and asexual reproduction
Sexual reproduction and asexual reproduction Asexual reproduction vs sexual reproduction venn diagram
Asexual reproduction vs sexual reproduction venn diagram Classes of hormones
Classes of hormones Hormones secreted by adenohypophysis
Hormones secreted by adenohypophysis Lipid soluble hormones examples
Lipid soluble hormones examples Bioflix activity homeostasis high blood glucose
Bioflix activity homeostasis high blood glucose Are steroids proteins
Are steroids proteins Synthesis of thyroxine hormone
Synthesis of thyroxine hormone Secretory gland
Secretory gland Biochemistry of hormones
Biochemistry of hormones Vasoactive peptides
Vasoactive peptides Hormones during pregnancy
Hormones during pregnancy Phyllodes tumor mammogram
Phyllodes tumor mammogram Madhukar mittal
Madhukar mittal Tropic vs nontropic hormones
Tropic vs nontropic hormones Prolactin target
Prolactin target Thyroid dwarfism
Thyroid dwarfism Posterior pituitary hormones
Posterior pituitary hormones Git hormones
Git hormones Hypothalamic hormones
Hypothalamic hormones Endocrine system abbreviations
Endocrine system abbreviations A hormone
A hormone Hormones testes
Hormones testes Tropic hormones
Tropic hormones Hypothalamus hormones
Hypothalamus hormones Gonadal hormones
Gonadal hormones Hormones released by
Hormones released by Hypotalanus
Hypotalanus Prolactin hormones
Prolactin hormones Presanted
Presanted Steroid hormones are water soluble. true false
Steroid hormones are water soluble. true false Qsxx
Qsxx Ovary hormones
Ovary hormones Plant hormones
Plant hormones Chapter 18: the endocrine system answer key
Chapter 18: the endocrine system answer key What secretes hormones
What secretes hormones Amino acid-based hormones
Amino acid-based hormones Pituitary gland hormones
Pituitary gland hormones Releasing inhibiting hormones
Releasing inhibiting hormones What are the tropic hormones
What are the tropic hormones Neurotransimitters
Neurotransimitters Intracellular hormone binding
Intracellular hormone binding Incentive theory ap psychology
Incentive theory ap psychology Chapter 45 hormones and the endocrine system
Chapter 45 hormones and the endocrine system Glucose range
Glucose range