Set a goal Why SelfGovernance Identify action steps

- Slides: 56
§ Set a goal – Why Self-Governance? § Identify action steps § Prepare a timeline § Allocate resources – internal capacity and Tribal leadership § Identify possible problems § Develop strategies for monitoring progress § Assign tasks § Estimate costs § Execute the plan
§ Determine Eligibility § Plan to Maintain § Identify Resources § Internal & External § Set a Timeline § Research Programs, Services, Functions, and Activities (PSFAs) § Select PSFAs for Assumption § Negotiate Compact and Funding Agreement § Plan for Transition
§ Use of Internal Teams § Organized by subject matter/expertise § Finance § Human Resource § Health Policy § Others? § Planning § Negotiation § Implementation
§ Should supplement internal/tribal capacity § Tribally-driven process § Goals-driven process § Possible Areas for Consulting: § Finance/Audit Finding Resolution § Health Management & Policy § Self-Governance
§ Other Area Tribes, Self-Governance Tribes § Other Tribal Programs § Related and unrelated to Health § Examples? § Indian Health Service – OTSG, Program Offices, Business Office, etc. § Local and Regional Providers § Higher Education Institutions
§ Specific Program Assumption: § Collaboration with Tribal Programs § Phase-in strategies: § Very useful for Tribes new to SG; § “Roll over” Title I Contracts into FA and add Tribal Shares and related PSFAs; § Incrementally add ‘feasible’ PSFAs over time; and § Allows infrastructure growth along side Tribal assumption of health programs. § Total Service Unit Assumption: § Plan, plan § Anticipate execution § Identify possible problems
§ Programs, Services, Functions and Activities; § Programs (high level), Activities (detailed level); § Describe all “contractible” operations of the IHS, both administrative and programmatic, at each organizational level;
§ Detailed information is needed on all PSFAs considered for assumption by the Tribe; § For new SG Tribes, it is advised that information be obtained on all PSFAs; § Research will allow the Tribe to make informed decisions about PSFAs to assume, conduct internal management planning, as well as to provide awareness of remaining responsibilities of the IHS.
§ Agency Lead Negotiator (ALN); § Office of Tribal Self-Governance; § HQ, Area and Service Unit staff; § Self-Governance Education & Communication; § Other Self-Governance Tribes.
§ Request/Obtain financial and PSFA information from the ALN, including all PSFA manuals applicable to your Tribe; § Review in conjunction with the financial information provided; § Request meetings with HQ, Area or SU staff as needed to answer questions and provide in-depth information about IHS operations; § Utilize SG Tribal networks.
§ Community and Tribal Leader direction – this should guide overall PSFA analysis and priority-setting. This will ensure that the resulting course of action will contain strategies to make health services more responsive to the articulated needs and desires of the Tribal community and its Leaders. “The Congress hereby recognizes the obligation of the United States to respond to the strong expression of the Indian people for self-determination by assuring maximum Indian participation in the direction of educational as well as other Federal services to Indian communities as to render such services more responsive to the needs and desires of those communities. ” (25 U. S. C. § 450 a(a))
§ Determining feasibility of assuming specific PSFAs, or portions thereof: § Population to be served; § Financial considerations; § Opportunities and challenges; § Internal management preparedness; § Improvement of healthcare outcomes; § “Phase-in” strategies. § Consideration of opportunities and challenges: § Review and consider strategies to capitalize on opportunities that may be available to the Tribe to leverage its health care services, such as third party billing; partnerships with IHS and other organizations and providers; Inter-Tribal partnerships; Affordable Care Act opportunities; and innovative health care delivery system models. § Identify barriers and challenges and develop strategies to address such barriers.
§ Orderly transition to Tribal administration of health care programs: § Identify management systems and infrastructure needed; § Appropriations and budget; § Tribal legal infrastructure; § HR, Finance and other management systems; § Health service delivery infrastructure; § Identify transition strategies; § Exp: Purchased and referred care; personnel, vendor contracts, etc. § Identify health care program implementation strategies. § Partnerships, health priorities, health service delivery models, facilities, providers and staffing.
§ Governance/Organizational Structure § Health Department or System § Internal Management Support: § Finance § Human Resources § IT § Procurement/Contracts § Facilities
§ Governance and Decision-Making Structure § Health Governance Models § Organizational Structure § Decision Making hierarchy § Budget § Programmatic design/partnerships § Policy § Considerations § Responsiveness to Community § Flexibility § Unique healthcare operations
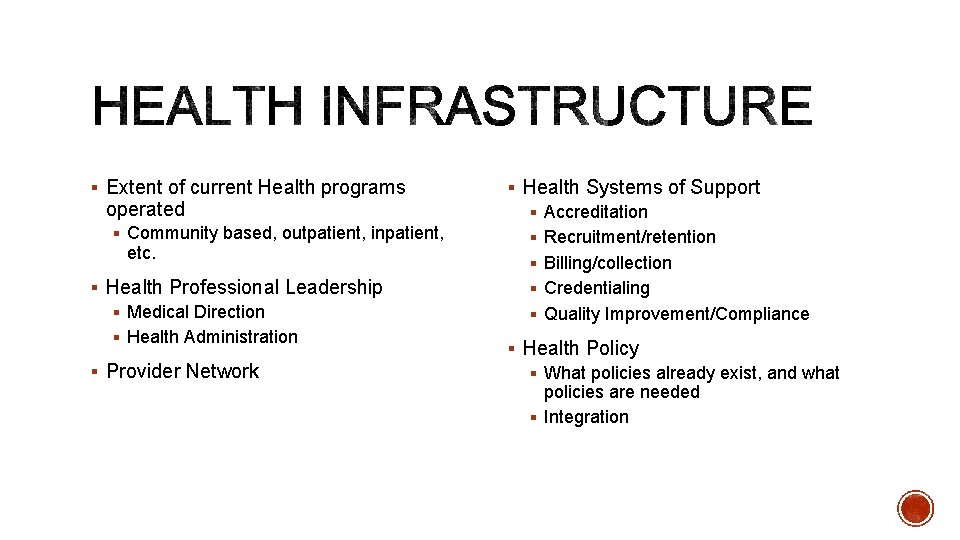
§ Extent of current Health programs operated § Community based, outpatient, inpatient, etc. § Health Professional Leadership § Medical Direction § Health Administration § Provider Network § Health Systems of Support § Accreditation § Recruitment/retention § Billing/collection § Credentialing § Quality Improvement/Compliance § Health Policy § What policies already exist, and what policies are needed § Integration
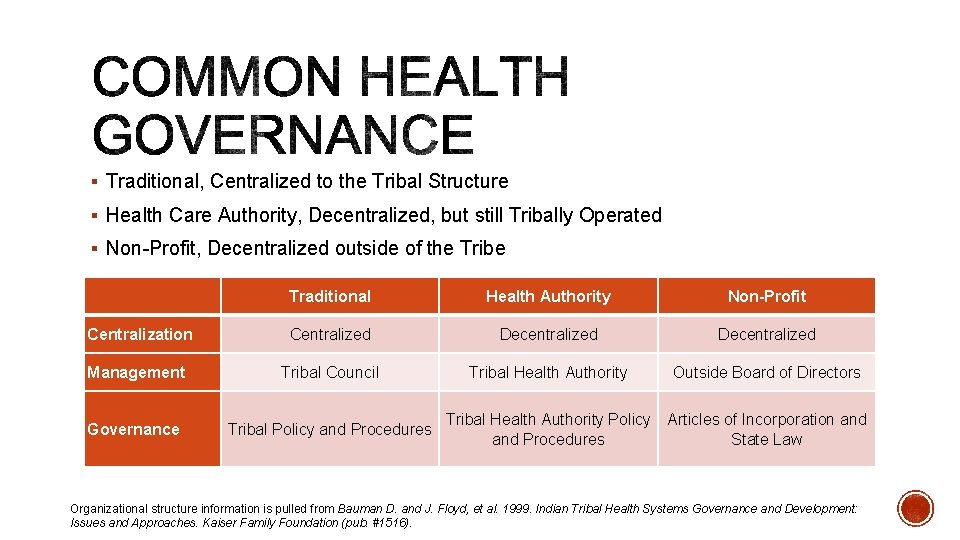
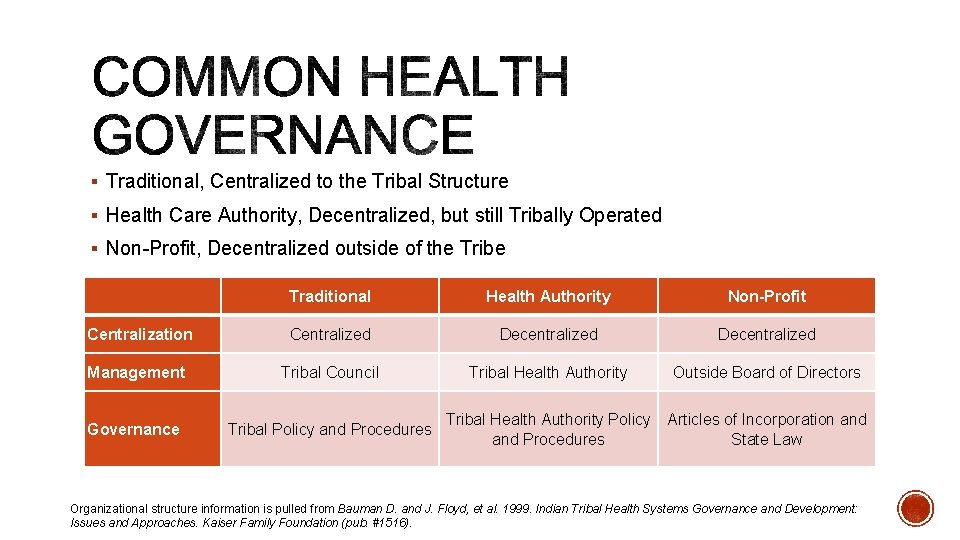
§ Traditional, Centralized to the Tribal Structure § Health Care Authority, Decentralized, but still Tribally Operated § Non-Profit, Decentralized outside of the Tribe Traditional Health Authority Non-Profit Centralization Centralized Decentralized Management Tribal Council Tribal Health Authority Outside Board of Directors Governance Tribal Policy and Procedures Tribal Health Authority Policy Articles of Incorporation and Procedures State Law Organizational structure information is pulled from Bauman D. and J. Floyd, et al. 1999. Indian Tribal Health Systems Governance and Development: Issues and Approaches. Kaiser Family Foundation (pub. #1516).
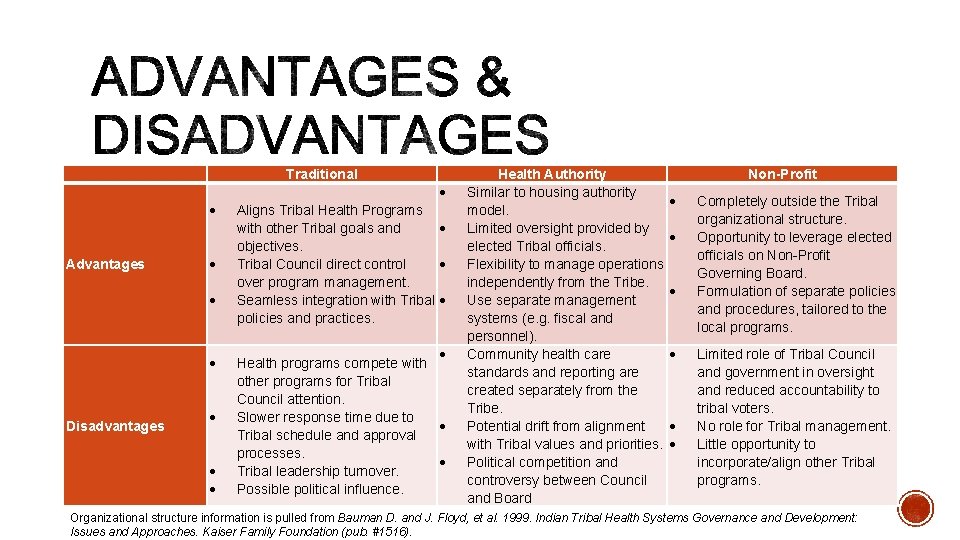
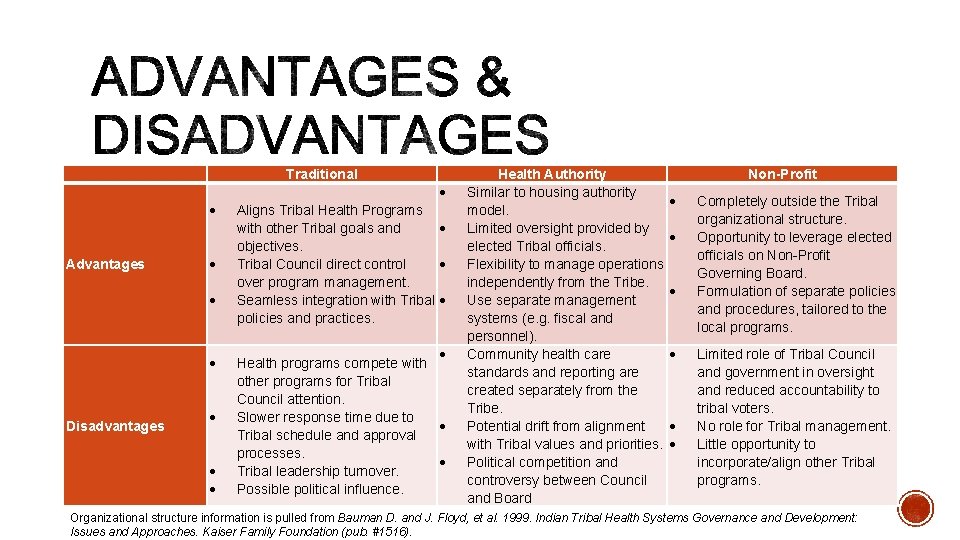
Traditional Advantages Disadvantages Aligns Tribal Health Programs with other Tribal goals and objectives. Tribal Council direct control over program management. Seamless integration with Tribal policies and practices. Health programs compete with other programs for Tribal Council attention. Slower response time due to Tribal schedule and approval processes. Tribal leadership turnover. Possible political influence. Health Authority Similar to housing authority model. Limited oversight provided by elected Tribal officials. Flexibility to manage operations independently from the Tribe. Use separate management systems (e. g. fiscal and personnel). Community health care standards and reporting are created separately from the Tribe. Potential drift from alignment with Tribal values and priorities. Political competition and controversy between Council and Board Non-Profit Completely outside the Tribal organizational structure. Opportunity to leverage elected officials on Non-Profit Governing Board. Formulation of separate policies and procedures, tailored to the local programs. Limited role of Tribal Council and government in oversight and reduced accountability to tribal voters. No role for Tribal management. Little opportunity to incorporate/align other Tribal programs. Organizational structure information is pulled from Bauman D. and J. Floyd, et al. 1999. Indian Tribal Health Systems Governance and Development: Issues and Approaches. Kaiser Family Foundation (pub. #1516).
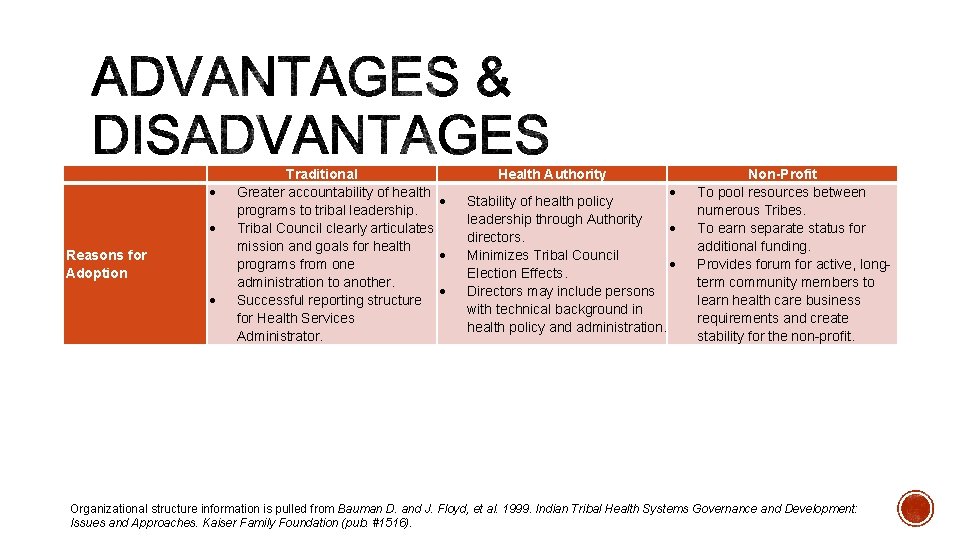
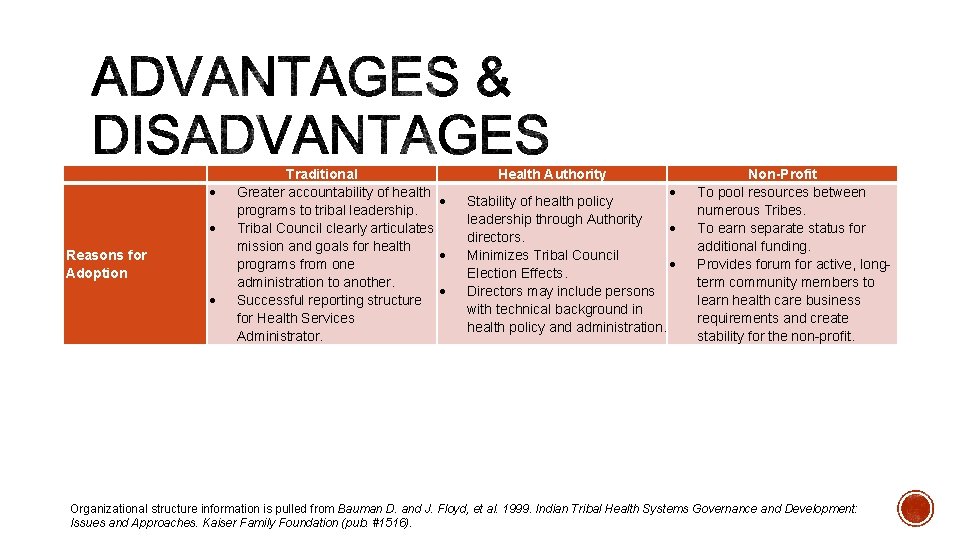
Reasons for Adoption Traditional Greater accountability of health programs to tribal leadership. Tribal Council clearly articulates mission and goals for health programs from one administration to another. Successful reporting structure for Health Services Administrator. Health Authority Stability of health policy leadership through Authority directors. Minimizes Tribal Council Election Effects. Directors may include persons with technical background in health policy and administration. Non-Profit To pool resources between numerous Tribes. To earn separate status for additional funding. Provides forum for active, longterm community members to learn health care business requirements and create stability for the non-profit. Organizational structure information is pulled from Bauman D. and J. Floyd, et al. 1999. Indian Tribal Health Systems Governance and Development: Issues and Approaches. Kaiser Family Foundation (pub. #1516).
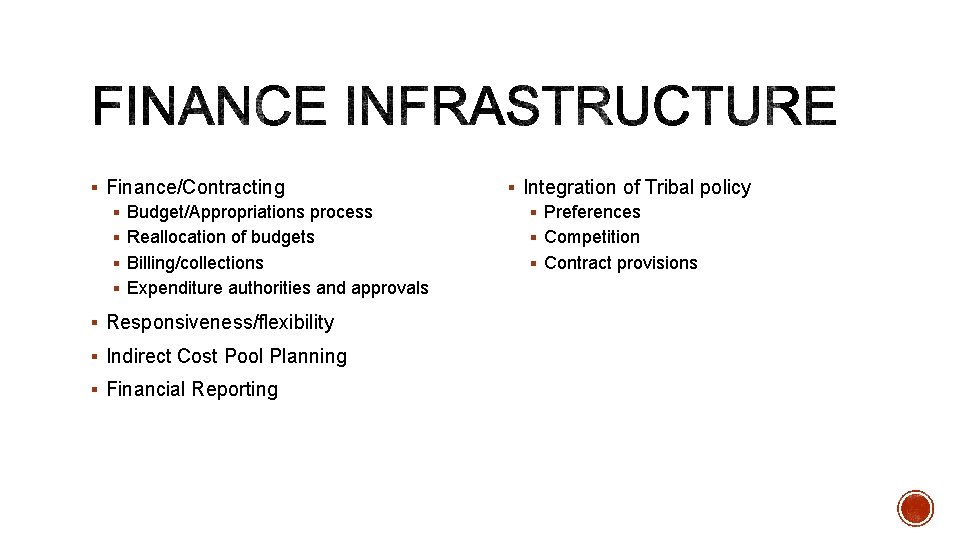
§ Finance/Contracting § Budget/Appropriations process § Reallocation of budgets § Billing/collections § Expenditure authorities and approvals § Responsiveness/flexibility § Indirect Cost Pool Planning § Financial Reporting § Integration of Tribal policy § Preferences § Competition § Contract provisions
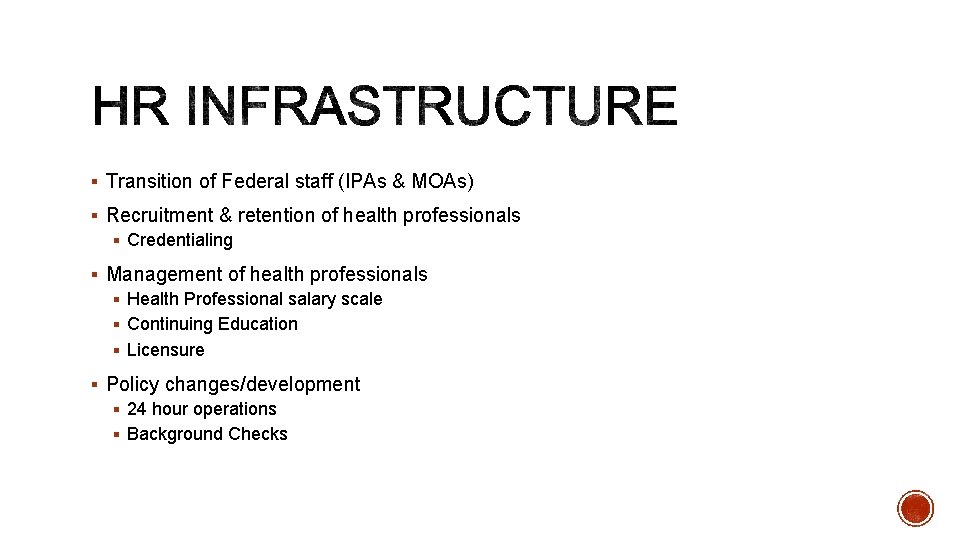
§ Transition of Federal staff (IPAs & MOAs) § Recruitment & retention of health professionals § Credentialing § Management of health professionals § Health Professional salary scale § Continuing Education § Licensure § Policy changes/development § 24 hour operations § Background Checks
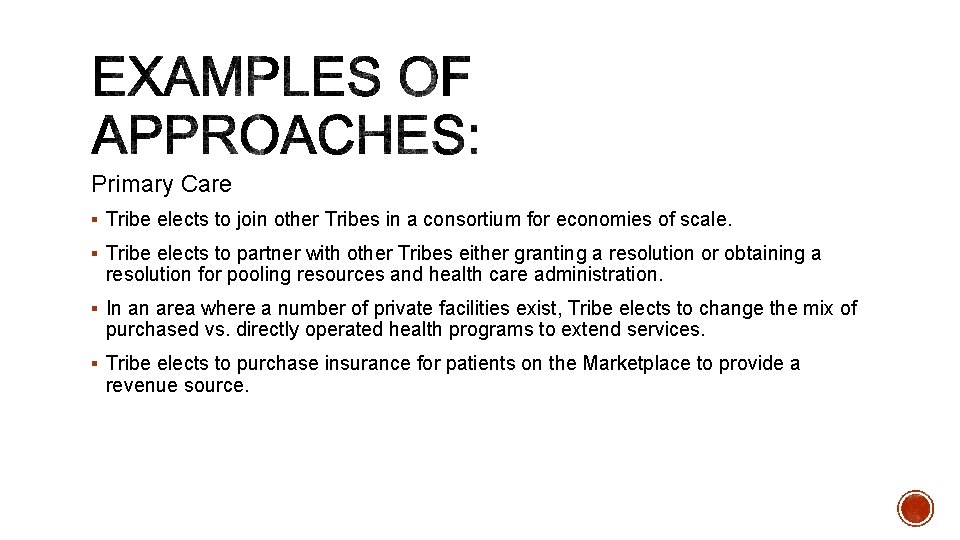
Primary Care § Tribe elects to join other Tribes in a consortium for economies of scale. § Tribe elects to partner with other Tribes either granting a resolution or obtaining a resolution for pooling resources and health care administration. § In an area where a number of private facilities exist, Tribe elects to change the mix of purchased vs. directly operated health programs to extend services. § Tribe elects to purchase insurance for patients on the Marketplace to provide a revenue source.
§ Title I Functions to Title V Funding Agreement § Greater flexibility. § Time to build Tribal infrastructure. § Retention of Title V Eligibility. § Possible Third Party Revenue Generation. § Note: Pre-award and start up CSC may not be available for a simple roll over of services between Contract and Compact. § Associated functions with current Title I Programs § Example: Mobile Health Unit to provide preventative services (CHR and PHN Services)
§ Office of Information Technology: § Frequent decisions by Tribes to assume portions of PSFAs, based upon cost and Tribal IT system and infrastructure. § For ease of decision making, IHS is preparing OIT “packages” of related IT services. § Total Assumption: § Top to bottom assumption. § Requires adequate planning, time and negotiation of transition challenges. § Licensure and provider numbers for billing.
§ Business Office Management (AO): Plans, implements, directs, manages, and coordinates all third party billing and collection activities. Ensures all IHS Service Units maximize reimbursements from all alternative resources. Manages the Medicare and Medicaid resources in accordance with program regulations. Serves as liaison between Federal, State, and local programs in assuring compliance of all laws, regulations, and policies. Provides technical assistance, advice, and training regarding the entire third party revenue generation process. § Evaluate Current Service: Where are these services provided? Area Office or Service Unit? How many staff are currently conducting these functions? Is there a contractor? § Evaluate Efficiency: How much is the Service Unit billing? What is the turn around? § Evaluate Network: How many users are covered? What services are provided and billed for? § Evaluate Opportunities: Can you increase billing? Examples – Increase covered users, increase billable services, etc.
§ MATERNAL CHILD HEALTH (AO) § Technical Assistance/Guidance, Policy Development, Program Development and Evaluation, Budgeting, Training § Evaluate Current Service: What services is the Tribe currently receiving? What are the benefits? § Evaluate Efficiency: Is the Tribal Share amount enough to maintain and grow current services provided? If not, can the Tribe or health system create additional revenue to grow and enhance the program? § Evaluate Opportunities: Would a Tribal network be more conducive? Can some of the services be left at the AO and some be assumed?
§ 25 U. S. C. § 458 aaa-4(b)(1): § “Each funding agreement…shall, as determined by the Indian tribe, authorize the Indian tribe to plan, conduct, consolidate, administer…all programs services, functions and activities (or portions thereof)…without regard to the agency or office of the Indian Health Service within which the program, service, function, or activity (or portion thereof) is performed. ”
§ Compact & Funding Agreement § Programs, Services, Functions and Activities (PSFAs) § Programs (high level) Activities (detailed level); and § Describe all “contractible” operations of the IHS, both administrative and programmatic, at each organizational level § FTCA coverage § Tribal Shares Associated with PSFAs § Intergovernmental Personnel Agreements and Memorandum of Agreements § Transition Issues

Negotiation s Evaluation Compact Service Delivery Funding Agreement Processing & Payment
§ Elected Tribal Leaders; § Tribal Leader or Designee with decision making authority (Lead Negotiator); § Financial representation; § Legal representation; § SG expert/SG coordinator; § Health programmatic staff; § Others based upon Tribal priorities.
§ Agency Lead Negotiator (ALN) – represents the Director of IHS; § OTSG – office of record, provides technical assistance throughout (Program Analyst and Financial Analyst); § HQ Staff – for financial and/or PSFA support; § Area Staff – for financial and/or PSFA support; § Office of General Counsel, HHS – for legal advice to the IHS.
§ Enables a Tribe to set its own priorities to assume PSFAs; § Observes the Nation-to-Nation relationship between the Unites States and each Tribe; § Involves the active participation of both Tribal and Federal representatives; § Goal: To achieve full agreement on a SG Compact and Funding Agreement that facilitates the Tribe’s vision for health care.
§ Compact – an umbrella agreement that contains provisions that continue year-to-year, effective until terminated; § Funding Agreement – contains, at a minimum: § PSFA description; § The general budget category assigned (within the IHS budget); § Funds to be provided; § Time and method for transfer of funds § Responsibilities of the Secretary (IHS); § Any other provisions upon which the Tribe and the IHS agree. § 25 U. S. C. § 458 aaa— 4(d)
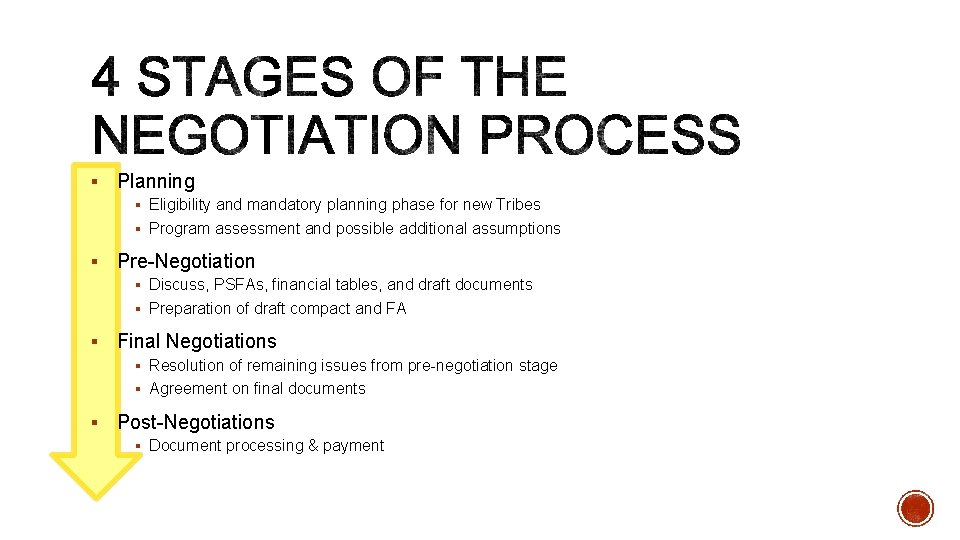
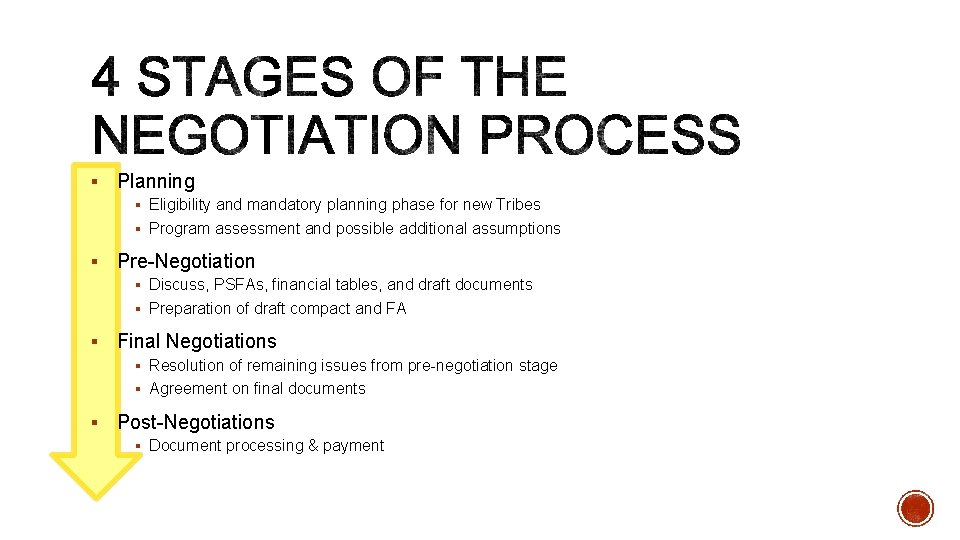
§ Planning § Eligibility and mandatory planning phase for new Tribes § Program assessment and possible additional assumptions § Pre-Negotiation § Discuss, PSFAs, financial tables, and draft documents § Preparation of draft compact and FA § Final Negotiations § Resolution of remaining issues from pre-negotiation stage § Agreement on final documents § Post-Negotiations § Document processing & payment
§ Usually, this stage is the longest and most work. § Title V of the ISDEAA requires completion of a planning phase to the satisfaction of the Tribe. § Must Include: § legal research § budgetary research § internal Tribal government planning and organization preparation relating to the administration of health care programs.
§ Information requests § Financial tables, billing and workload information; § Any PSFA updates; § Proposals for language from IHS (such as CSC or other issues); § Transitional information such as for contracts, equipment/facilities and personnel. § Negotiation Meetings
§ At Tribal request; § Individual Tribe, group of Tribes, or entire Area Office; § Review financial tables and gather more information about PSFAs. § Drafting or editing the compact & FA § Active discussion by negotiation teams: § Issues identified during planning § Draft compact, FA, and funding tables § “Pre-negotiations”: a meeting, in-person or by phone, with both negotiation teams meet to discuss any questions or concerns regarding the documents and tables prior to final negotiations.
§ Full Tribal and Federal negotiation teams (face-to-face, conference call, etc); § Teams work together to reach agreement on the final documents. § Tribe should set the agenda and identify meeting goals; § Exchange of draft documents ahead of time is helpful. § Once agreement on the final documents has been reached, two final copies are signed by the Tribe and provided to the ALN.
§ A collaborative process, with mutual respect; § Respects the Nation-to-Nation relationship; § Oriented towards Tribal goals for Self-Governance; § Secretary must exercise good faith “…to maximize implementation of the Self- Governance policy. ” (25 U. S. C. § 458 aaa— 6(e)) § Positively work towards mutual agreement wherever possible.
§ Get to know your Agency Lead Negotiator; § Set the agenda – identify your negotiation issues; § Ask a lot of questions – there are no ‘stupid’ questions! § Submit and track information requests to IHS; § Talk to experienced Tribes; § Keep a running list of outstanding negotiation issues; § Keep the document and proposal exchange moving, apart from formal meetings – update frequently;
§ Control the documents; § Prepare follow up action lists, with agreed upon timelines; § Be creative in problem-solving; § Delegate selected items to ‘sub’ negotiation teams to report back to larger group (examples: IT, legal issues) § Don’t forget to negotiate program coordination/implementation issues; § Don’t take ‘no’ for an answer. Look at all alternatives for achieving Tribal goals.
§ The Tribe/TO signs the final documents and returns them to the ALN. § The ALN then: § Reviews the documents § Packages them with the supporting documents, § Submits package to HQ for processing and signature by the IHS Director or a designee § Once the compact and FA have been signed by both parties, they become legally binding and enforceable.
25 U. S. C. § 458 aaa— 6(b) § For disagreements, in whole or in part; § Tribe formally submits to the ALN; § IHS determination within 45 days; § Failure to reject within 45 days is deemed agreement by IHS.
25 U. S. C. § 458 aaa— 6(c) § Amount of funds exceeds the applicable funding level the Tribe is entitled to; § PSFA is an inherent federal function; § Tribe cannot carry out PSFA without “significant danger or risk to the public health”; and § Tribe is not eligible to participate in self-governance. § IHS must provide: technical assistance, a hearing on the record, or an option for entering the several portions of the agreement(s) upon Tribal request.
§ IHS ALN must make a recommendation regarding the agreement(s) with the Tribe; § Office of General Counsel disagreement does not necessarily mean IHS disagreement; § Resulting agreements are maintained, tracked and coordinated by the Office of Tribal Self-Governance; § Successor agreement provision – the Funding Agreement remains in full force and effect until a subsequent agreement is executed. (25 U. S. C. § 458 aaa— 4(e))
§ Reach out – have any other Tribes experienced the same issue? Use SGCE and TSGAC networks. (Getting out of your IHS Area is key. ) § Request additional IHS information or involvement as necessary; § Request technical assistance from OTSG; § Use Tribally-acceptable alternatives and identify high priority issues.
§ Do they match your Self-Governance Goals? Community Health Needs? Tribal Leader direction? § Do you have the infrastructure to implement the PSFA? Is the funding adequate? § What would be the challenges? § Are there upfront costs? § Is there a plan for the transition?
§ How much detail must the PSFA description entail? § Ranges from very detailed, to broad program titles. § Considerations: Federal Tort Claims coverage, redesign authority, audit. § Inclusion of PSFA description of retained or inherent federal functions in FA. § Inclusion of PSFAs that are authorized under the Indian Health Care Improvement Act, but that IHS may not be conducting in your Area: § Example: Enhanced dental care, preventative health and wellness; § Example: Long-term Services and Supports; § Example: Home and community based services.
§ Business Office Management (AO): Plans, implements, directs, manages, and coordinates all third party billing and collection activities. Ensures all IHS Service Units maximize reimbursements from all alternative resources. Manages the Medicare and Medicaid resources in accordance with program regulations. Serves as liaison between Federal, State, and local programs in assuring compliance of all laws, regulations, and policies. Provides technical assistance, advice, and training regarding the entire third party revenue generation process. § Evaluate Current Service: Where are these services provided? Area Office or Service Unit? How many staff are currently conducting these functions? Is there a contractor? § Evaluate Efficiency: How much is the Service Unit billing? What is the turn around? § Evaluate Network: How many users are covered? What services are provided and billed for? § Evaluate Opportunities: Can you increase billing? Examples – Increase covered users, increase billable services, etc.
§ MATERNAL CHILD HEALTH (AO) § Technical Assistance/Guidance, Policy Development, Program Development and Evaluation, Budgeting, Training § Evaluate Current Service: What services is the Tribe currently receiving? What are the benefits? § Evaluate Efficiency: Is the Tribal Share amount enough to maintain and grow current services provided? If not, can the Tribe or health system create additional revenue to grow and enhance the program? § Evaluate Opportunities: Would a Tribal network be more conducive? Can some of the services be left at the AO and some be assumed?
§ Tribal share of PRC identified at less than $100 k for user population identified at 1, 200 patients. One catastrophic PRC case could cause a cash flow crisis. Tribe elected not to assume PRC at that time. § Tribe elected to assume PRC without also assuming the associated Primary Care. Problems with continuity of care and cost control. § Tribe elects to shift traditionally-purchased services to direct services, rather than PRC, for cost savings and timely services.
§ Tribe elects to remain with IHS SU due to its small size for purposes of competing for SFC projects. Tribal members get served on a more frequent basis. § Tribe elects to compact SFC, but partners with Tribal communities, municipal and rural water systems to extend funding further and serve more Tribal members.