Pulmonary Diseases Disorders Assessment Pulmonary Diseases Disorders n
- Slides: 38
Pulmonary Diseases & Disorders: Assessment
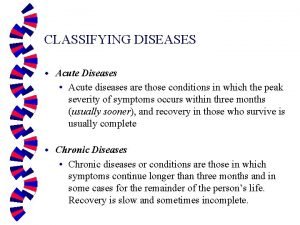
Pulmonary Diseases & Disorders n Epidemiology u 28% of all EMS Chief Complaints in the US u >200, 000 deaths annually due to respiratory emergencies
Pulmonary Diseases & Disorders n Many, many pulmonary diseases u Difficult to learn all pathophysiologies u All can be categorized as affecting: F Ventilation F Diffusion (Respiration) F Perfusion u Treatment can be focused on identifying and treating source of ventilatory/respiratory impairment
Sources of Pulmonary Impairment n n Pulmonary Diseases Disorders of the Pulmonary System Non-Pulmonary Disorders/Disease Impairing Ventilation or Respiration What examples can you list for each of these?
Sources of Pulmonary Impairment n Ventilation u Upper Airway Trauma F Epiglottitis F FBAO F Inflammation of tonsils F u Lower Airway Trauma F Obstructive lung disease F Mucous accumulation F Smooth muscle spasm F Airway edema F
Sources of Pulmonary Impairment n Ventilation u Chest Wall Impairment Trauma F Hemothorax F Pneumothorax F Empyema F Pleural inflammation F Neuromuscular diseases F u Neurologic Control Brainstem dysfunction F Phrenic or spinal nerve dysfunction F
Sources of Pulmonary Impairment n Diffusion Inadequate Fi. O 2 u Diseased alveoli u asbestosis F COPD F inhalation injury F u Capillary bed disease F atherosclerosis u Interstitial space disease High pressure pulmonary edema F High permeability pulmonary edema F
Sources of Pulmonary Impairment n Perfusion u Inadequate blood u Impaired blood flow F pulmonary embolus volume or hemoblogin u Capillary wall F hypovolemia pathology F anemia F trauma
Risk Factors for Pulmonary Disease n Intrinsic Risk Factors u Genetic predisposition F asthma F COPD F carcinoma u Cardiac or Circulatory pathologies F Source for pulmonary edema F Source for pulmonary emboli u Stress
Risk Factors for Pulmonary Disease n Extrinsic Factors u Smoking prevalence of COPD & carcinomas F severity of pulmonary disease F u Environmental Factors prevalence of COPD & asthma F severity of all obstructive disorders F
Function of the Pulmonary System n Gas Exchange System u ~10, 000 liters of air are filtered, warmed and humidified daily u Oxygen diffused into blood u Carbon dioxide excreted from the body
Function of the Pulmonary System n Physiology of Ventilation u Requires neurologic initiation (brainstem) u Nerve conduction pathways between brainstem and muscles of respiration u Intact & patent Upper and Lower airways u Intact & non-collapsed alveoli
Function of the Pulmonary System n Physiology of Respiration u Simple diffusion process at the pulmonarycapillary bed u Diffusion Requirements F Intact, non-thickened alveolar walls F Minimal interstitial space & without additional fluid F Intact, non-thickened capillary walls
Function of the Pulmonary System n Physiology of Perfusion u Process of circulating blood through the capillary bed u Perfusion Requirements F Adequate blood volume F Adequate hemoglobin F Intact, non-occluded pulmonary capillaries F Functioning Left Heart
Control of Ventilation n Control ventilation in response to physiologic needs u Driven 1° by p. H of CSF F influenced largely by Pa. CO 2 u 2° drive = Pa. CO 2 u 3° drive = Pa. O 2 detected by chemoreceptors F very small population with severe COPD
Nervous System Effect on Ventilation n Medulla u Stimulation n Phrenic Nerve u Innervation n of the diaphragm Spinal Nerves at Thoracic levels u Innervation n to initiate ventilation of intercostal muscles Hering-Breuer reflex u Prevents overinflation
General Assessment n Size-Up u Environment F Airborne Hazards F Number of patients F Needs • Specialized rescue equipment • Protective equipment u Is the environment creating or exacerbating the pulmonary condition?
General Assessment n Initial Goal u Identify potentially life-threatening pulmonary conditions n Perform minimal PE & Hx u Initiate n immediate & appropriate therapies Then, continue PE & Hx u Try to determine if origin is ventilation, diffusion, perfusion or combination
General Assessment n Signs of potentially life-threatening pulmonary condition u altered mental status u absent signs of ventilation u Audible stridor or wheezing u Able to speak in short phrases only u Sustained Tachycardia u Pallor / Diaphoresis u Accessory muscle use / Retractions
Assessment: H&P n Present History (focused hx) u Chief Complaint F Dyspnea • “Subjective sensation that breathing is excessive, difficult or uncomfortable F CP F Cough, Hemoptysis u Associated F Fever, Symptoms Chills F sputum production F Fatigue
Assessment: H&P n Present History (focused hx) u Sputum Findings amount of sputum infection F Thick green or brown pneumonia or infection F Yellow or gray allergic or inflammatory response F Hemoptysis tuberculosis or carcinoma F Pink, frothy severe pulmonary edema F
Assessment: H&P n HX of Present Illness u How long has dyspnea been present? u Gradual or sudden onset? u What aggravates or alleviates? F Hx of orthopnea? u Coughing? u Productive cough? u What does sputum look/smell like? u Pain? u What does the pain feel like?
Assessment: H&P n Listen - To Pt. Breathe or Talk u Noisy Breathing is Obstructed Breathing u Not All Obstructed Breathing is Noisy u Snoring - Tongue Blocking Airway u Stridor - “Tight” Upper Airway from Partial Obstruction n Observe Breathing u Tachypnea u Bradypnea
Assessment: H&P n Observe u Body Positioning F Tripod F Legs in dependent position u Mental Status u Ventilatory Effort F Accessory muscle use / retractions F Abdominal muscle use F Chest wall expansion F Nasal flaring, pursed lips
Assessment: H&P n Physical Exam of the Chest u Increased A-P Diameter u Lung Sounds F Abnormal: stridor, wheezing, rhonchi, rales, pleural rub u Chest expansion u Symmetrical Findings u Evidence of Trauma
Assessment: H&P n Physical Exam u Cyanosis? F Late, unreliable sign of Hypoxia u Oxygenate Immediately! Especially If: Decreased LOC F Possible Shock F Possible Severe Hemorrhage F Chest Pain F Chest Trauma F Respiratory distress or dyspnea F HX of any Kind of Hypoxia F
Assessment: H&P n Physical Exam u Vital Signs F Skin Color, Temp & Moisture F Respiratory Rate • No an accurate lone indicator of respiratory status unless very slow F Respiratory Rhythm/Pattern F Pulse • Bradycardia vs Tachycardia F Blood Pressure
Assessment: H&P n Physical Exam - Circulatory assessment u Is the heart beating? u Is there major external hemorrhage? u Is the Pt. Perfusing vital organs? u Effects of hypoxia: F Early in adults - Tachycardia F Late in adults - Bradycardia F Children - Bradycardia
Assessment: H&P n n Don’t let respiratory failure distract you from assessing for circulatory failure. Vascular Access
Assessment: H&P n Physical Exam u Extremities F Peripheral Cyanosis F Clubbing F Carpopedal spasm F Peripheral edema
Assessment: H&P n Diagnostic Testing u Pulse oximetry Saturation F Inaccuracies & Disadvantages F u Peak Flow Meter Baseline measurement for obstructive lung disease F Often available from patient F u Capnometry real-time assessment of endotracheal tube placement F quantitative vs qualitative F
Assessment: H&P n Past History u Similar Episodes in Past F Patient’s description of acuity F “What happened last time you had an episode this bad? ” n Chronic Symptoms u Acute, Seasonal SOB episodes u Seasonal Allergies u Chronic cough u Recurrent flu, pulmonary infection or SOB
Assessment: H&P n Past History u Known diagnosis F Does the present H&P correlate with this past history? • CHF • Hypertension • Renal Failure u Previous intubation or hospitalization u Aggravating Factors (e. g. smoking)
Assessment: H&P n Past History u Medications F Class, Route, Frequency of Use F Pulmonary • • Sympathomimetics Corticosteroids MAST Cell Stabilizer Methylxanthines F Cardiovascular • Diuretics • Antihypertensives • Cardiac glycosides
Assessment: H&P n Disability u Restlessness, anxiety, combativeness = HYPOXIA Until Proven Otherwise u Drowsiness, lethargy = HYPERCARBIA When the patient stops fighting, he is not necessarily getting Better!!
Other Adventitious Sounds n Cough u Forced exhalation against partially closed glottis u Reflex response to mucosa irritation u Determine circumstances At work F Postural changes F Lying down F u Productive vs non-productive
Other Adventitious Sounds n Sneeze u Forced exhalation via nasal route u Clears nasal passages u Reflex response to mucosa irritation n Sigh u Slow, deep inspiration - Prolonged, audible exhalation u Reexpands areas of atelectasis
Other Adventitious Sounds n Hiccough u Hiccups, singultus u Spasm of diaphragm followed by glottic closure u No useful purpose u Benign, transient
 Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Seborrheic keratoses
Seborrheic keratoses Chapter 10 lymphatic system diseases and disorders
Chapter 10 lymphatic system diseases and disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 10 nail disorders and diseases
Chapter 10 nail disorders and diseases Define a primary skin lesion and list three types
Define a primary skin lesion and list three types Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Milady nail diseases and disorders
Milady nail diseases and disorders Portfolio assessment matches assessment to teaching
Portfolio assessment matches assessment to teaching Stages in implementing portfolio assessment
Stages in implementing portfolio assessment Define dynamic assessment
Define dynamic assessment Nursing management of pulmonary tuberculosis
Nursing management of pulmonary tuberculosis Pac pulmonary artery catheter
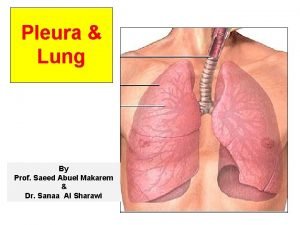
Pac pulmonary artery catheter Bronchial segments
Bronchial segments Svr calculation
Svr calculation Muscles of inspiration and expiration
Muscles of inspiration and expiration Pulmonary hypertension
Pulmonary hypertension Hypoventilation
Hypoventilation Rib anatomy anterior
Rib anatomy anterior Mean pulmonary arterial pressure
Mean pulmonary arterial pressure Thoracic aortic aneurysm
Thoracic aortic aneurysm Pulmonary embolism
Pulmonary embolism Function of coronary artery
Function of coronary artery 5 cyanotic congenital heart disease
5 cyanotic congenital heart disease Pac pulmonary artery catheter
Pac pulmonary artery catheter Pulmonary fibrosis
Pulmonary fibrosis Management of hemorrhage
Management of hemorrhage Bronchopneumonia
Bronchopneumonia Bronchopulmonary segments
Bronchopulmonary segments Chest pediatric pulmonary board review
Chest pediatric pulmonary board review Pulmonary hypoplasia with anasarca
Pulmonary hypoplasia with anasarca Cardiogenic vs noncardiogenic pulmonary edema
Cardiogenic vs noncardiogenic pulmonary edema Pah vs pulmonary hypertension
Pah vs pulmonary hypertension Saturacion 94
Saturacion 94 Pulmonary artery and aorta
Pulmonary artery and aorta Right atrium
Right atrium