Promoting Excellence in Dementia Masterclass Supporting People with
- Slides: 50
Promoting Excellence in Dementia Masterclass Supporting People with Dementia in Hospital and Understanding Their Experience from Their Perspective NHS Tayside Older People Psychological Therapies Service Dr Helen Nicholson – Langley , Clinical Psychologist & Dr Fiona Macleod Consultant Clinical Psychologist/Lead Clinician 9 th October 2014
Part I: Assessment Dr Helen Nicholson – Langley Clinical Psychologist
Overview: Assessment • • Gathering useful information Assessment tools Understanding the person first, then Understanding the person with dementia
Assessment Formulation Intervention
Gathering Relevant Information should be relevant and useful. Whilst we do not always know in advance what information will prove relevant, we can predict what types of information will be useful at the formulation stage and so this can and should help guide the assessment.
Gathering Useful Information: Where Do We Begin? Information can be broken into 4 main categories (the bio-psycho-social model): • • Biological Psychological Social Environmental or contextual
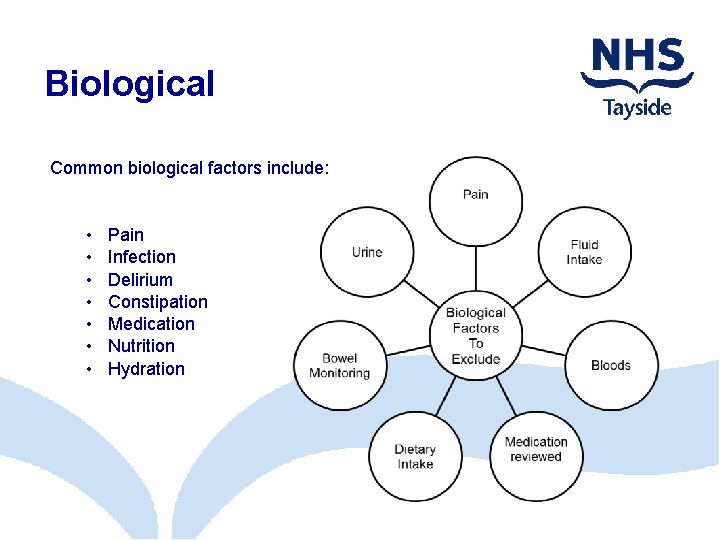
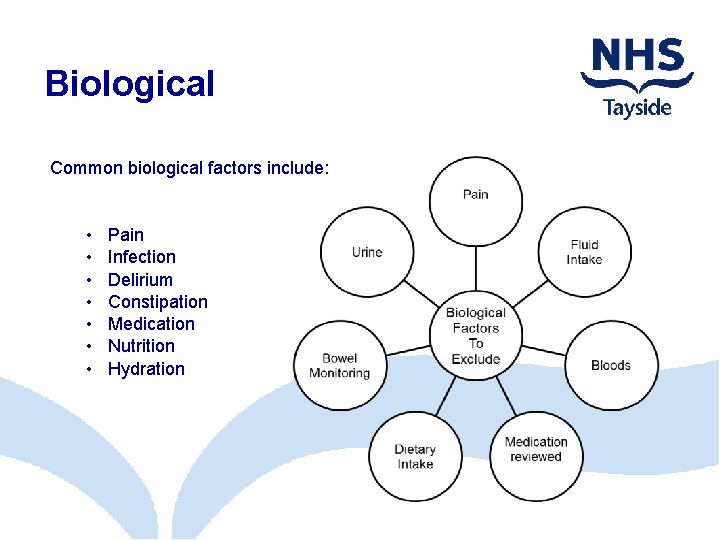
Biological Common biological factors include: • • Pain Infection Delirium Constipation Medication Nutrition Hydration
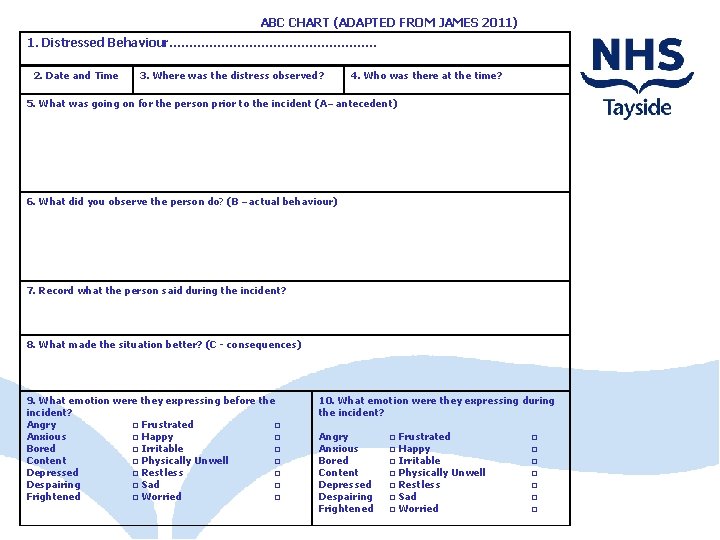
Useful Measures/Tools I • • • Nutrition/fluid/sleep charts Abbey Pain Scale AMT 10/4 AT Frequency charts Observations: What do you see? What do you hear? a narrative in time limited sections e. g. 10 minutes • ABC charts • Challenging Behaviour Scale Identify the sign/symptom/behaviour/concern, record the frequency and severity
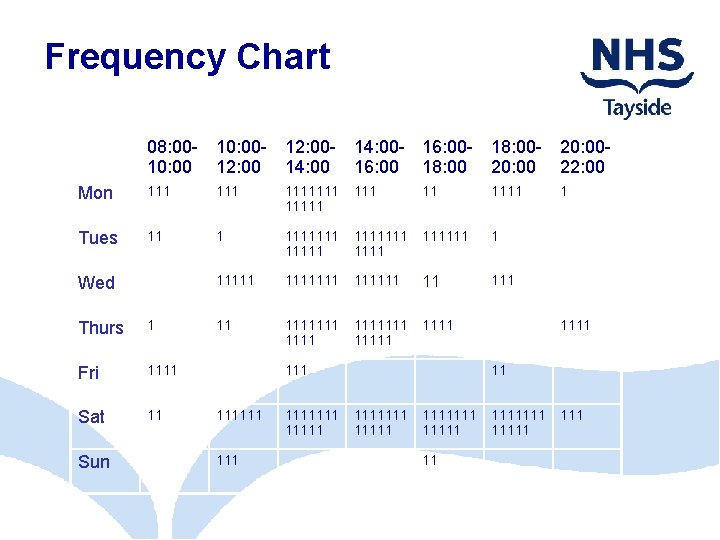
Frequency Charts • Sometimes a behaviour is so frequent it would be impossible to complete an ABC chart for each incidence • In these cases a frequency chart can be useful to identify when the behaviour is happening and whether the frequency is affected by the time of day
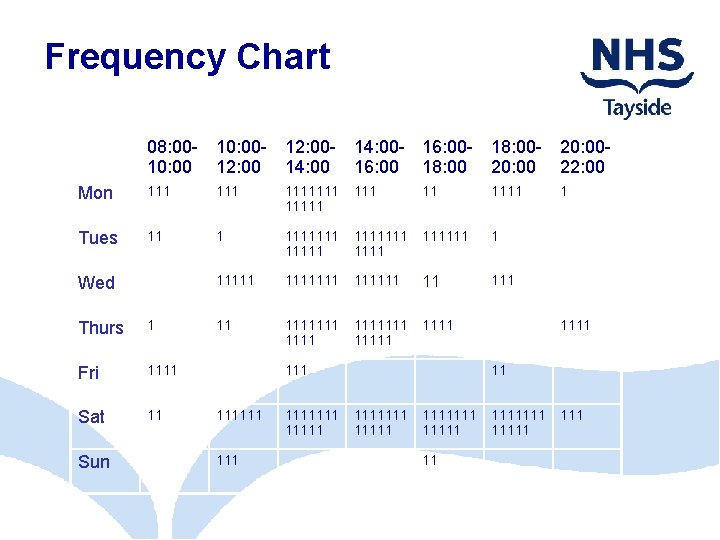
Frequency Chart 08: 00 - 10: 00 - 12: 00 - 14: 00 - 16: 00 - 18: 00 - 20: 0010: 00 12: 00 14: 00 16: 00 18: 00 20: 00 22: 00 Mon 111 1111111 1111 Tues 11 1 1111111 111111 1 1111111 11 1111111 1111 Wed Thurs 1 Fri 1111 Sat 11 Sun 111 1111111 1 1111 11 1111111 11 11111 111
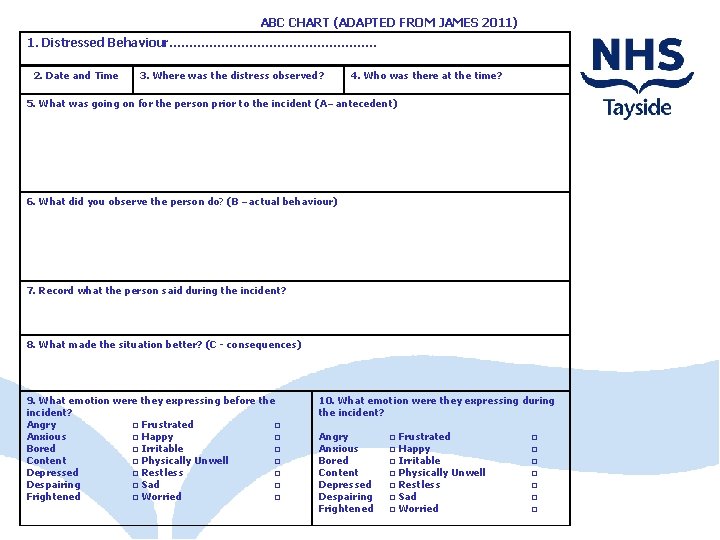
ABC CHART (ADAPTED FROM JAMES 2011) 1. Distressed Behaviour………………………. 2. Date and Time 3. Where was the distress observed? 4. Who was there at the time? 5. What was going on for the person prior to the incident (A – antecedent) 6. What did you observe the person do? (B – actual behaviour) 7. Record what the person said during the incident? 8. What made the situation better? (C - consequences) 9. What emotion were they expressing before the incident? Angry □ Frustrated □ Anxious □ Happy □ Bored □ Irritable □ Content □ Physically Unwell □ Depressed □ Restless □ Despairing □ Sad □ Frightened □ Worried □ 10. What emotion were they expressing during the incident? Angry Anxious Bored Content Depressed Despairing Frightened □ Frustrated □ Happy □ Irritable □ Physically Unwell □ Restless □ Sad □ Worried □ □ □ □
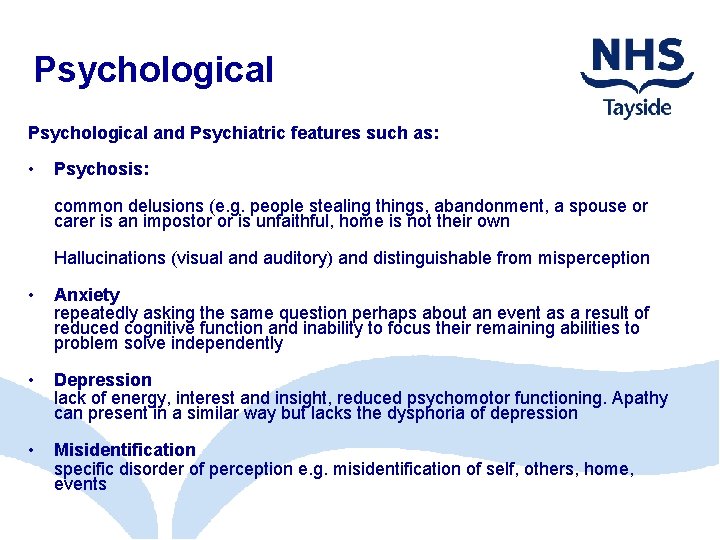
Psychological and Psychiatric features such as: • Psychosis: common delusions (e. g. people stealing things, abandonment, a spouse or carer is an impostor or is unfaithful, home is not their own Hallucinations (visual and auditory) and distinguishable from misperception • Anxiety repeatedly asking the same question perhaps about an event as a result of reduced cognitive function and inability to focus their remaining abilities to problem solve independently • Depression lack of energy, interest and insight, reduced psychomotor functioning. Apathy can present in a similar way but lacks the dysphoria of depression • Misidentification specific disorder of perception e. g. misidentification of self, others, home, events
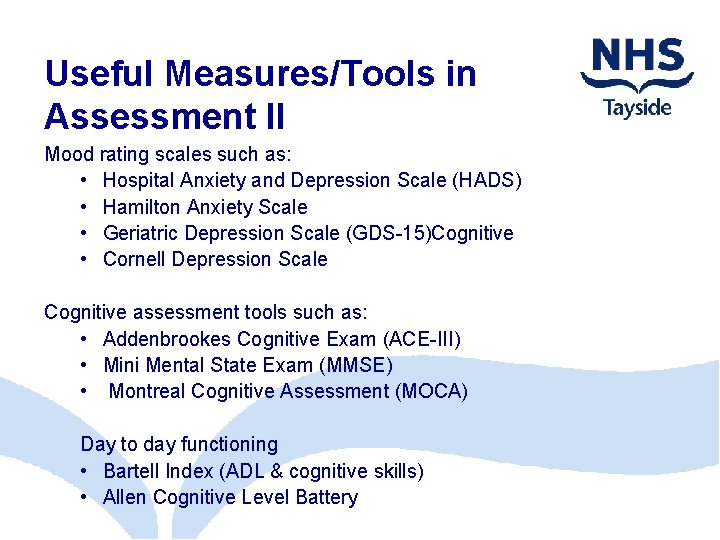
Useful Measures/Tools in Assessment II Mood rating scales such as: • Hospital Anxiety and Depression Scale (HADS) • Hamilton Anxiety Scale • Geriatric Depression Scale (GDS-15)Cognitive • Cornell Depression Scale Cognitive assessment tools such as: • Addenbrookes Cognitive Exam (ACE-III) • Mini Mental State Exam (MMSE) • Montreal Cognitive Assessment (MOCA) Day to day functioning • Bartell Index (ADL & cognitive skills) • Allen Cognitive Level Battery
Social • How does the person interact with others? • Do they shy away from or look for interaction? • What do interactions seem to centre around? • How do people adjust to loss of usual familiar faces and social routines? • What opportunities do they have in this new, unfamiliar environment?
Communication • • Has there been SALT input What aids does the person require Consider receptive and expressive language Remember only 7% of communication is verbal – how else are we/others communicating? • What are we/others communicating?
What else should we consider? I Sensory Visual – consider the impact of normal aging, co-morbid conditions, does the person have their regular glasses, do they use them? ) Auditory – age related hearing loss, noise levels, do they have access to hearing aids, can they hear too little/too much? Tactile – when other sense deteriorate, do we rely on e. g. Touch. What does a ward environment ‘feel like’, touch can help make sense of things, e. g. Recognition Olfactory/taste - what does the environment smell like? Pleasant/unpleasant smells? Our sense of smell can remind us of another time or place, a person
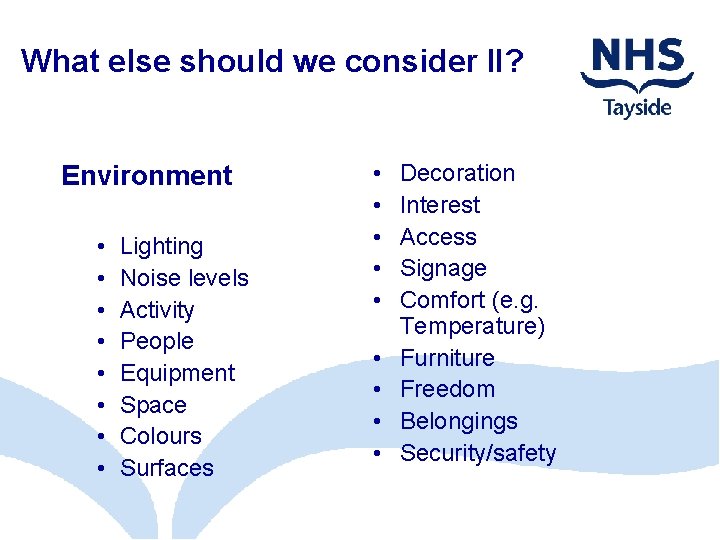
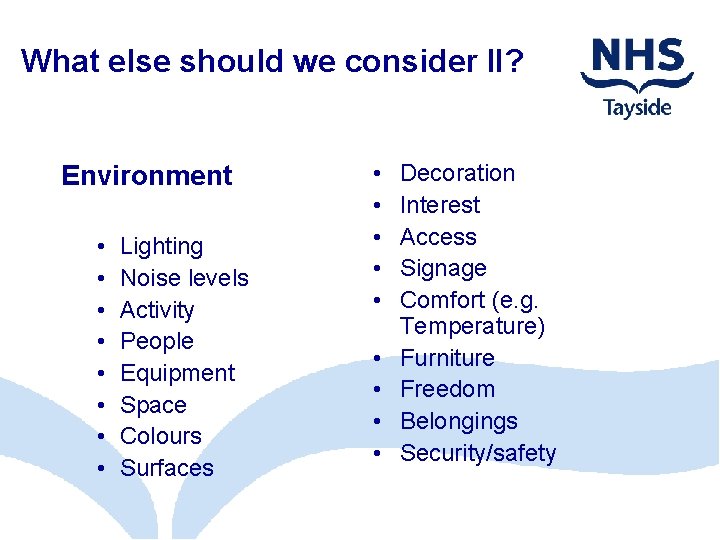
What else should we consider II? Environment • • Lighting Noise levels Activity People Equipment Space Colours Surfaces • • • Decoration Interest Access Signage Comfort (e. g. Temperature) Furniture Freedom Belongings Security/safety
What else should we consider III? Stimulation • How much stimulation is there? Too much, too little? • Is it internal/external? • Does the person have any control over this? • Can or are they self stimulating (e. g. vocalisation, ‘picking’, self harm)
Understanding the Person FIRST • We often consider all these previous points when there is a problem (i. e. Stress and distress) but before we can understand the problem, we need to understand the person • This is required for a useful and complete formulation • To understand a person we need to know about them and their life e. g. “Getting to know You”, current lifestyle, history, key people
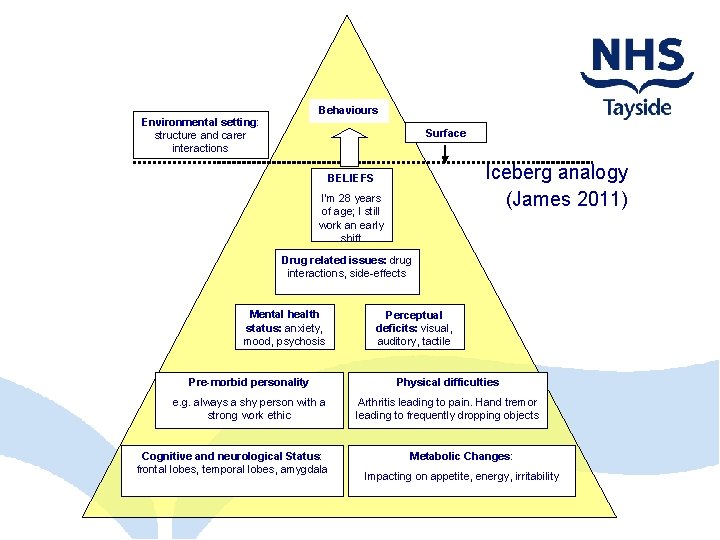
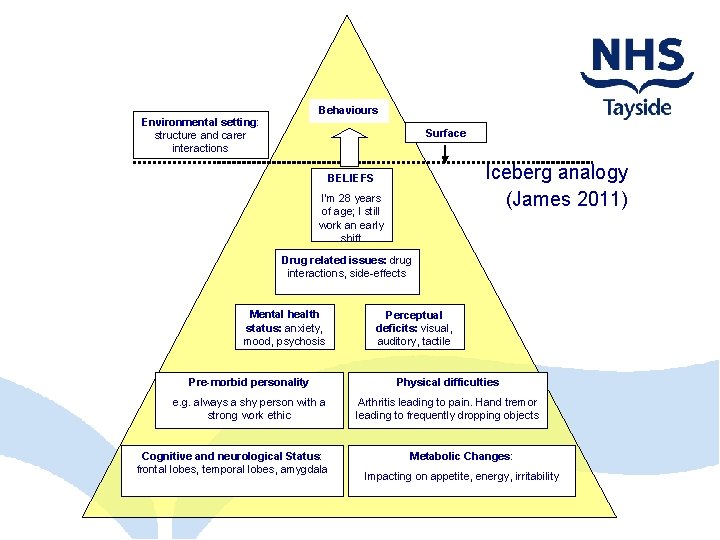
Behaviours Environmental setting: structure and carer interactions Surface Iceberg analogy (James 2011) BELIEFS I’m 28 years of age; I still work an early shift Drug related issues: drug interactions, side-effects Mental health status: anxiety, mood, psychosis Perceptual deficits: visual, auditory, tactile Pre-morbid personality Physical difficulties e. g. always a shy person with a strong work ethic Arthritis leading to pain. Hand tremor leading to frequently dropping objects Cognitive and neurological Status: frontal lobes, temporal lobes, amygdala Metabolic Changes: Impacting on appetite, energy, irritability
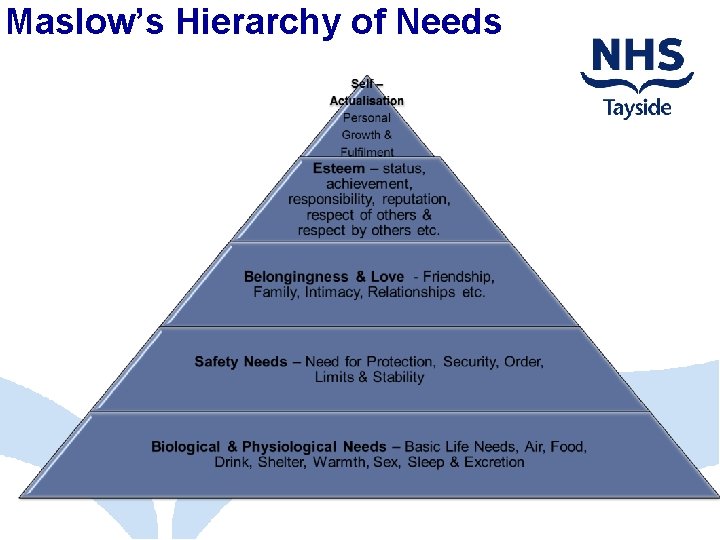
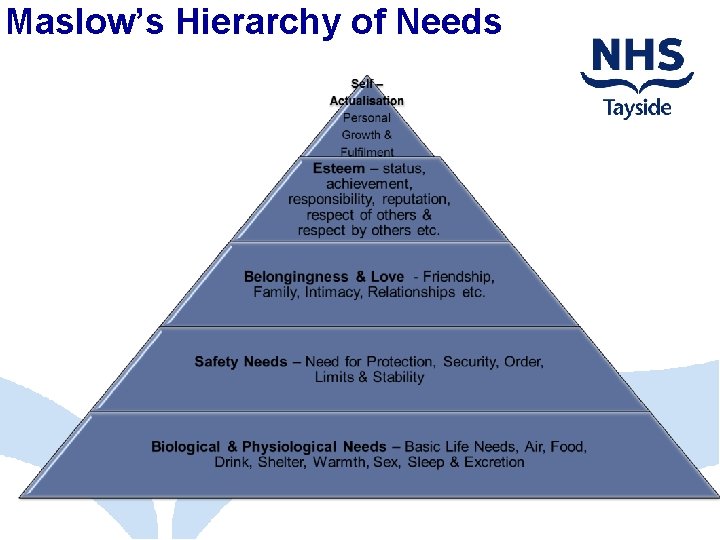
Maslow’s Hierarchy of Needs
Human Needs • Maslow proposed that: basic biological needs are at the bottom of the hierarchy and more complex psychological motivations or needs are at the top needs low in the hierarchy must be at least partially satisfied before needs higher in the hierarchy become important to us needs, and the stage at which they are within the hierarchy, determine actions
Understanding the Person with Dementia I personality is ‘the distinctive character or qualities of a person’. Oxford English Dictionary (2005) Nature v’s Nurture: In fact we know that it is a combination of genetics and what we learn through experience that makes us who we are. Each person is an individual. There may be similarities but no two people are the same.
Understanding the Person with Dementia II • • • Personal history including key life events Pre-morbid personality Likes/dislikes, hobbies and interests Routines –past and present Roles and relationships Needs
Needs of People with Dementia I • Kitwood proposes 5 categories of need: • Attachment: we need to feel attachments to others and objects especially during periods of change where we may feel insecure • Identity: to know who you are and how you feel about yourself • Occupation: being involved in an activity that is meaningful to you • Inclusion: belonging to and being part of a group, community or social environment • Comfort: feeling closeness to others and warmth comforted
Where do we find all this information?
Enter the Person’s World We often say we understand the person, behaviour, the stress & distress of the person with dementia but what we really do is have our ‘best guess’ – that’s what our formulation is. However, we are still effectively trying to bring the person out of their world and into ours – to engage them in activities, conversations, the social environment - albeit modified. Remember, it is easier for us to step into their world – and out again – than for them to step into ours. Sometimes, taking time out to spend with them, not asking anything of them, just being, can be the best that we can offer (intervention). It can also be a helpful part of assessment. Try to put yourself into their shoes. What do they see, think, feel, believe? Whilst it is impossible to ‘know’ this, we can imagine and use what we know about this person and how they are presenting to understand. Empathy, comfort, security, understanding.
The Time Machine
Exercise 1: Case study
Part II Formulation Dr Fiona Macleod Consultant Clinical Psychologist/Lead Clinician
Overview • • • What is Formulation? What is Formulation NOT? Why is Formulation Important? What does a Formulation look like? Reformulation Case Study
What is Formulation? • ‘Best Guess’ based on information gathered at assessment. • Takes into account the whole picture. • Helps us understand why THIS person has developed THESE problems or behaviours at THIS particular time. • Brings together multiple pieces of information to help develop a shared understanding of the problem. • Builds on our instincts to make sense of things. • Flexible and open to change • Jigsaw Approach
What is Formulation NOT? • • • Not the same as a diagnosis No right or wrong answers. Not the same thing as a care plan. Not created in isolation. Not owned by one profession.
Why is Formulation Important? • Enables us to have an understanding of the patient and their experiences • Provides a coherent story for the patient’s presentation • Allows for an integrative approach bringing together assessment information from all disciplines. • Enhances common goals for the care by developing a mutual understanding through collaborative working. • Helps select, guide and inform patient care. • Helps to predict and overcome possible obstacles to care • Decreases stress for individual workers
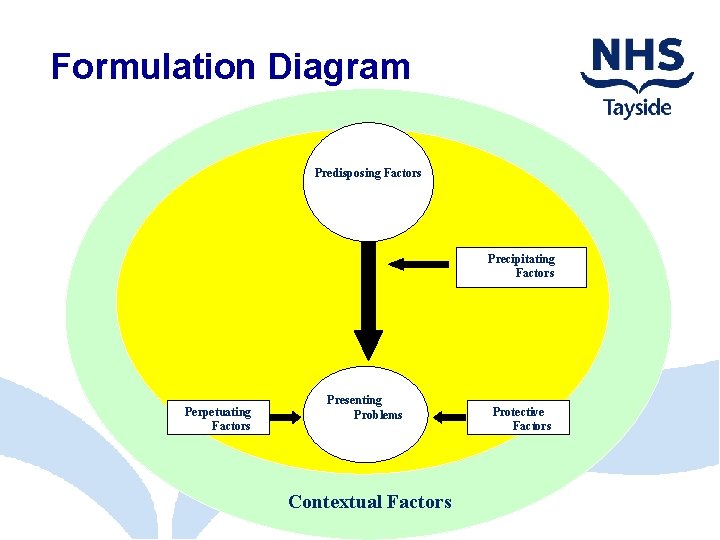
Models of Formulation • Formulation skills are used in different therapeutic approaches. • However there are components to any formulation approach. • These core components are - Predisposing Factors - Precipitating Factors - Perpetuating Factors - Protective Factors - Presenting Problems
Predisposing Factors – Background History • Life Story • Personality • Past Mental Health History • Physical Health • Social Environment • Cognitive Level • Medication
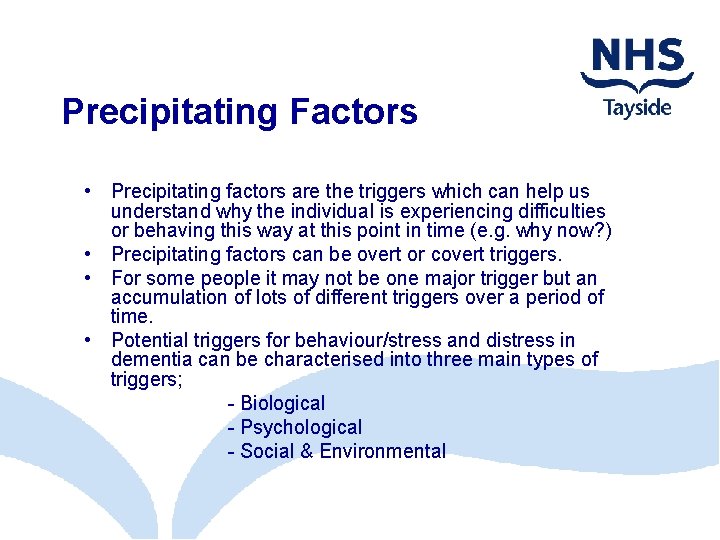
Precipitating Factors • Precipitating factors are the triggers which can help us understand why the individual is experiencing difficulties or behaving this way at this point in time (e. g. why now? ) • Precipitating factors can be overt or covert triggers. • For some people it may not be one major trigger but an accumulation of lots of different triggers over a period of time. • Potential triggers for behaviour/stress and distress in dementia can be characterised into three main types of triggers; - Biological - Psychological - Social & Environmental
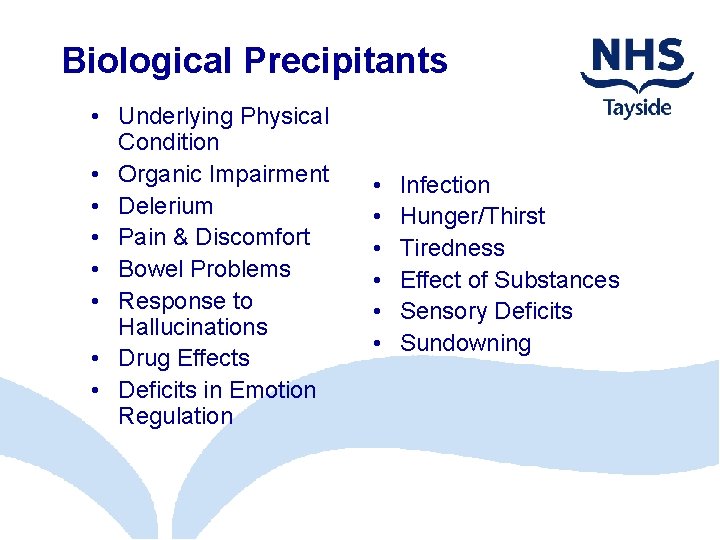
Biological Precipitants • Underlying Physical Condition • Organic Impairment • Delerium • Pain & Discomfort • Bowel Problems • Response to Hallucinations • Drug Effects • Deficits in Emotion Regulation • • • Infection Hunger/Thirst Tiredness Effect of Substances Sensory Deficits Sundowning
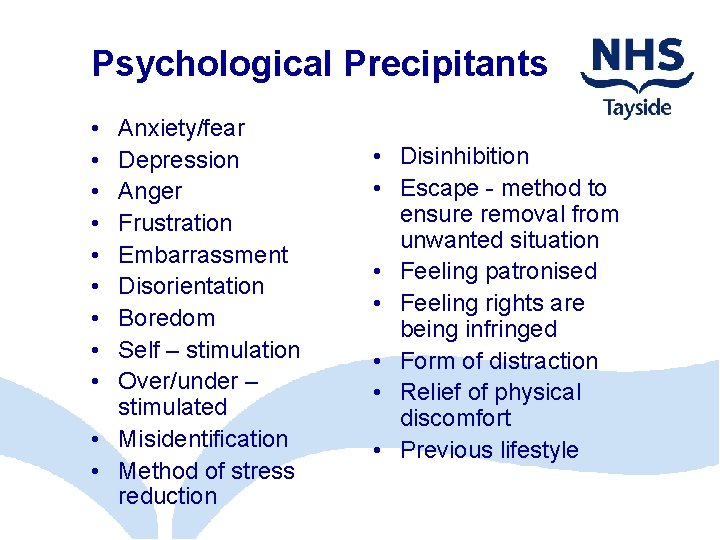
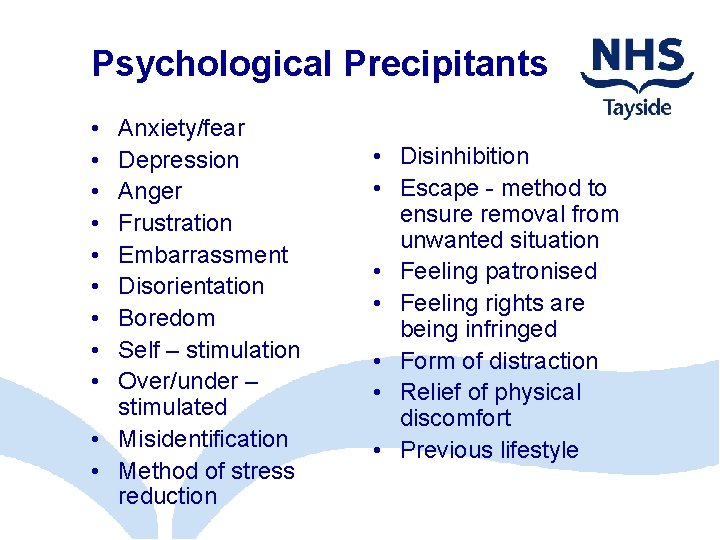
Psychological Precipitants • • • Anxiety/fear Depression Anger Frustration Embarrassment Disorientation Boredom Self – stimulation Over/under – stimulated • Misidentification • Method of stress reduction • Disinhibition • Escape - method to ensure removal from unwanted situation • Feeling patronised • Feeling rights are being infringed • Form of distraction • Relief of physical discomfort • Previous lifestyle
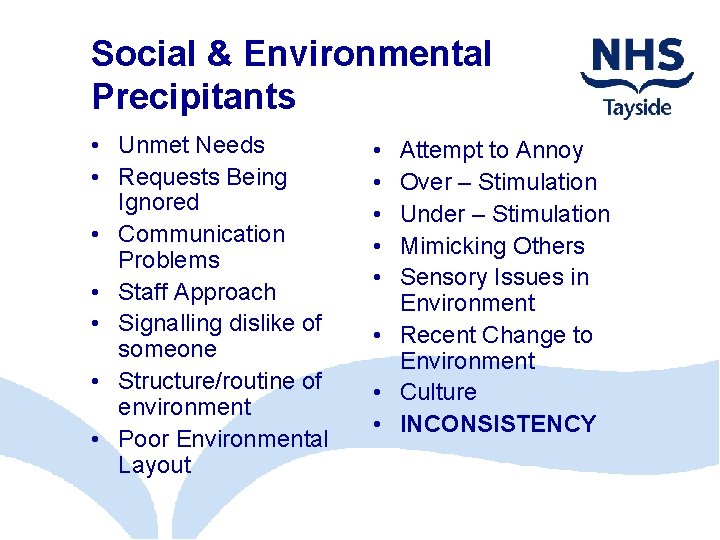
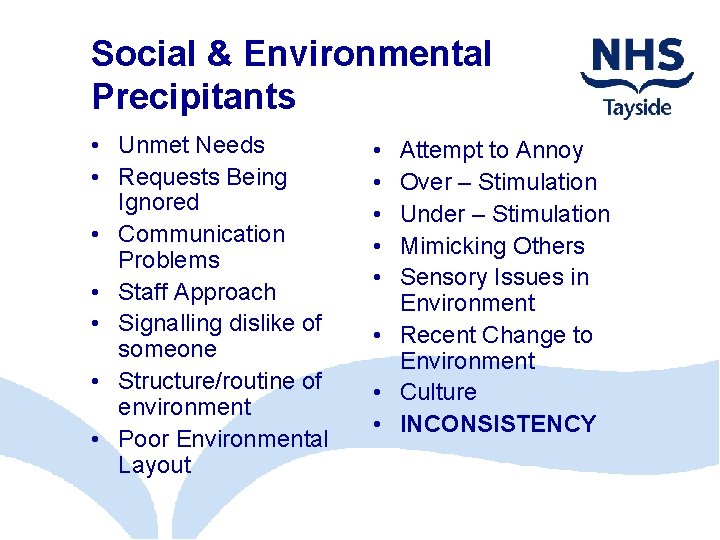
Social & Environmental Precipitants • Unmet Needs • Requests Being Ignored • Communication Problems • Staff Approach • Signalling dislike of someone • Structure/routine of environment • Poor Environmental Layout • • • Attempt to Annoy Over – Stimulation Under – Stimulation Mimicking Others Sensory Issues in Environment • Recent Change to Environment • Culture • INCONSISTENCY
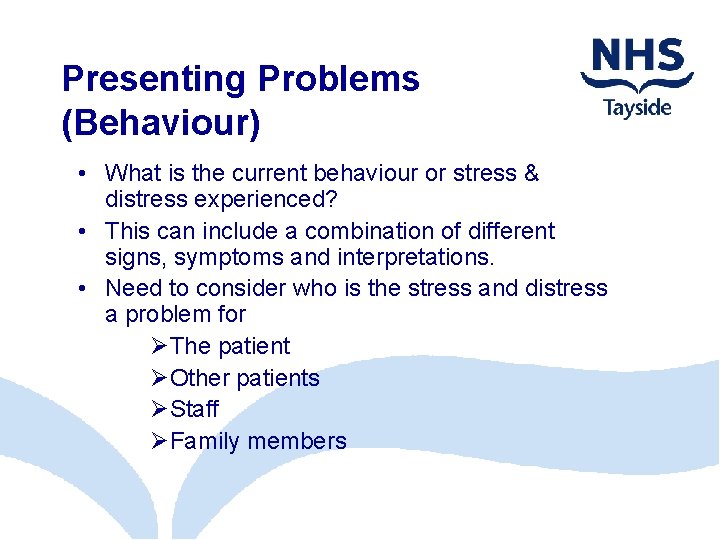
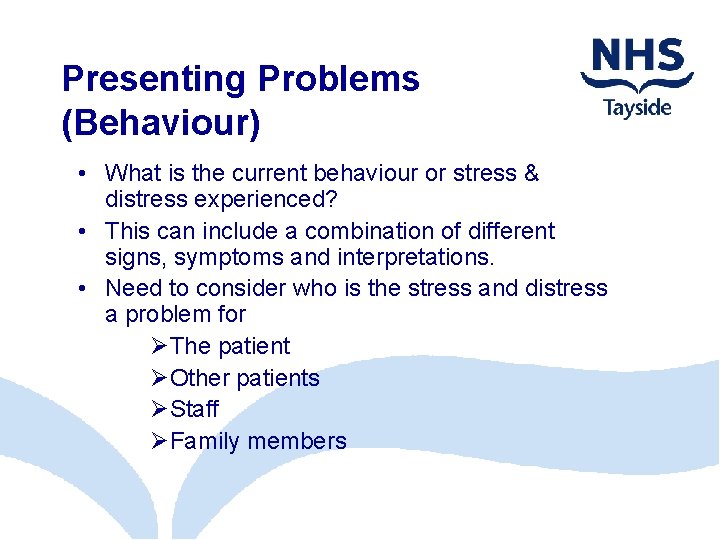
Presenting Problems (Behaviour) • What is the current behaviour or stress & distress experienced? • This can include a combination of different signs, symptoms and interpretations. • Need to consider who is the stress and distress a problem for ØThe patient ØOther patients ØStaff ØFamily members
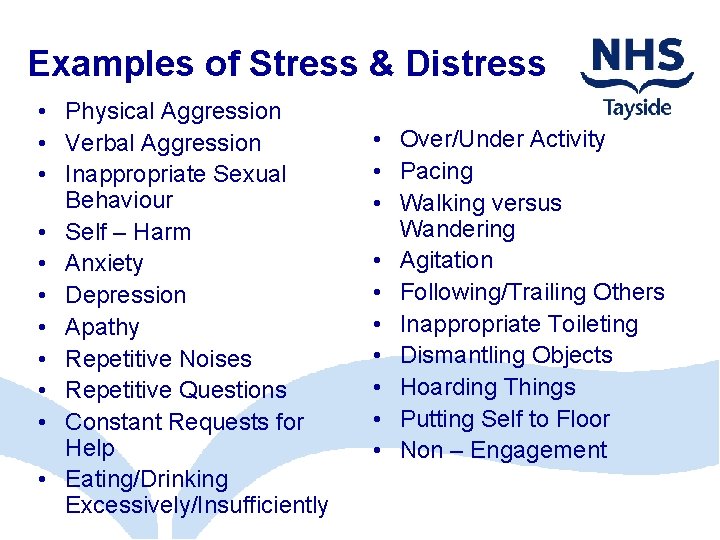
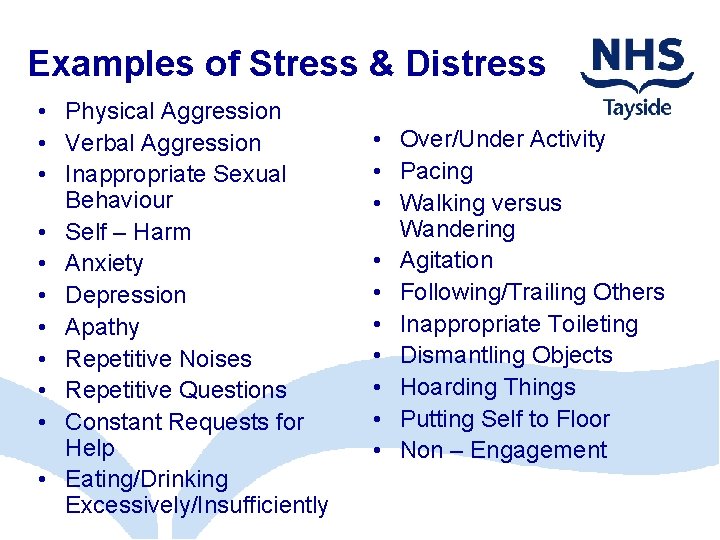
Examples of Stress & Distress • Physical Aggression • Verbal Aggression • Inappropriate Sexual Behaviour • Self – Harm • Anxiety • Depression • Apathy • Repetitive Noises • Repetitive Questions • Constant Requests for Help • Eating/Drinking Excessively/Insufficiently • Over/Under Activity • Pacing • Walking versus Wandering • Agitation • Following/Trailing Others • Inappropriate Toileting • Dismantling Objects • Hoarding Things • Putting Self to Floor • Non – Engagement
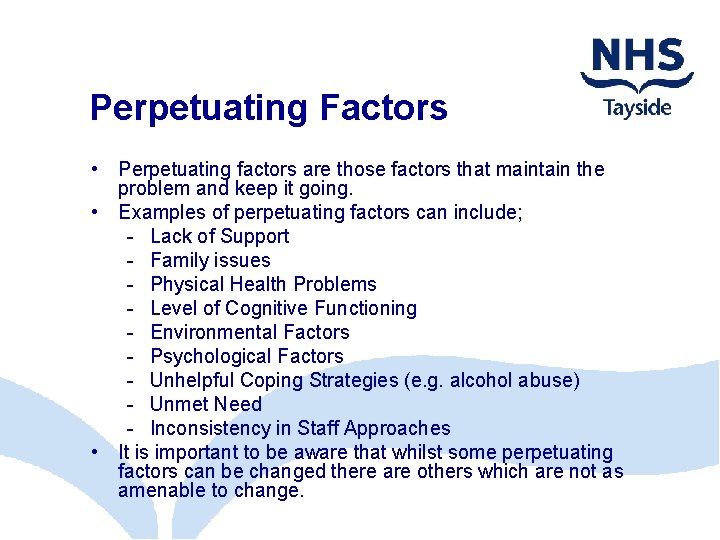
Perpetuating Factors • Perpetuating factors are those factors that maintain the problem and keep it going. • Examples of perpetuating factors can include; - Lack of Support - Family issues - Physical Health Problems - Level of Cognitive Functioning - Environmental Factors - Psychological Factors - Unhelpful Coping Strategies (e. g. alcohol abuse) - Unmet Need - Inconsistency in Staff Approaches • It is important to be aware that whilst some perpetuating factors can be changed there are others which are not as amenable to change.
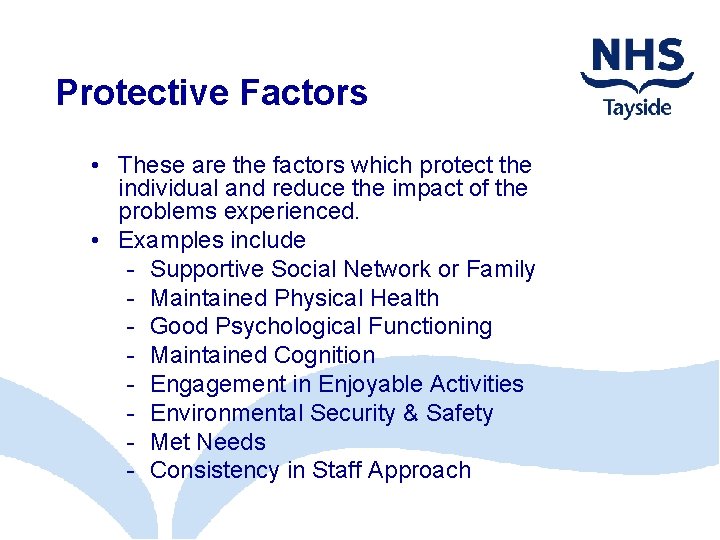
Protective Factors • These are the factors which protect the individual and reduce the impact of the problems experienced. • Examples include - Supportive Social Network or Family - Maintained Physical Health - Good Psychological Functioning - Maintained Cognition - Engagement in Enjoyable Activities - Environmental Security & Safety - Met Needs - Consistency in Staff Approach
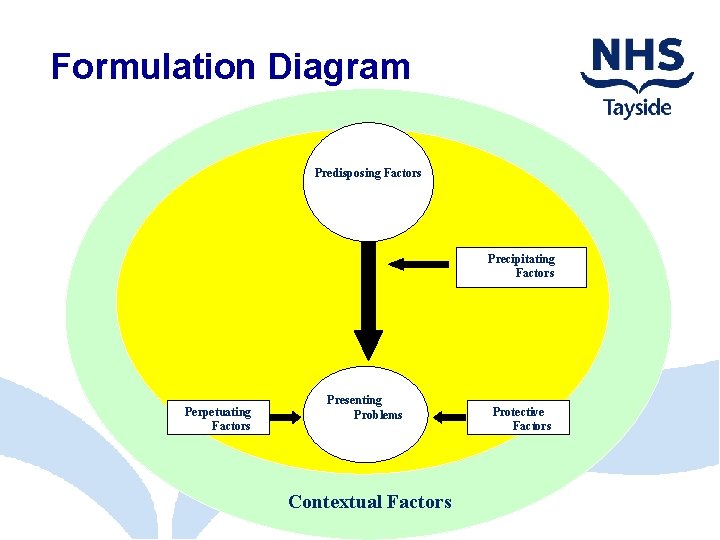
Formulation Diagram Predisposing Factors Precipitating Factors Perpetuating Factors Presenting Problems Contextual Factors Protective Factors
Exercise 2: Formulation of the Case Studies
Reformulation • The initial formulation is not a static thing. • It is flexible and evolving and MAY need to be adapted in light of new information. • The initial formulation may also need to be changed in light of changing circumstances and context (e. g. change in housing or physical health etc. ) • Reformulation does not involve going back to scratch. It is building on what you already know. • It is important to be aware that a change in an individual’s presentation does not necessarily require a reformulation. Rather it may be a reflection of support for the initial formulation.
Overview • Formulation helps us understand why THIS person has developed THESE problems at THIS particular time. • Formulation brings together multiple pieces of information to help develop a shared understanding of the problem. • The model including Predisposing Factors, Precipitating Factors, Presenting Problems, Protective Factors and Perpetuating Factors is useful in helping us to formulate cases. • Formulation is a helpful tool that guides assessment, care and treatment.
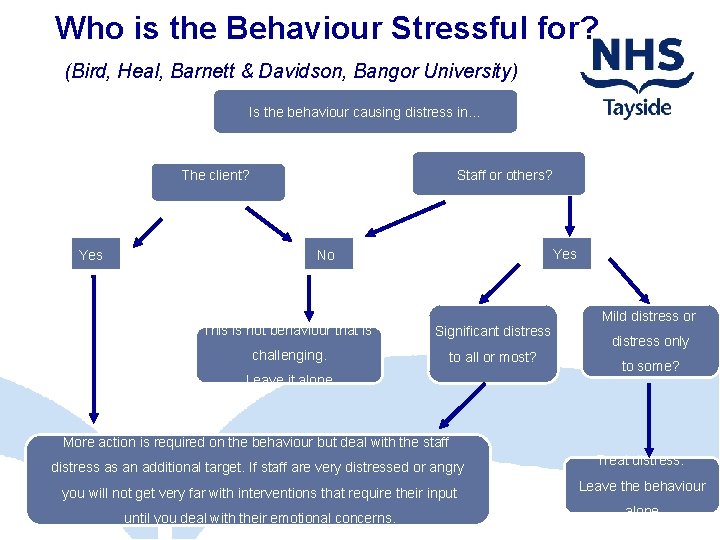
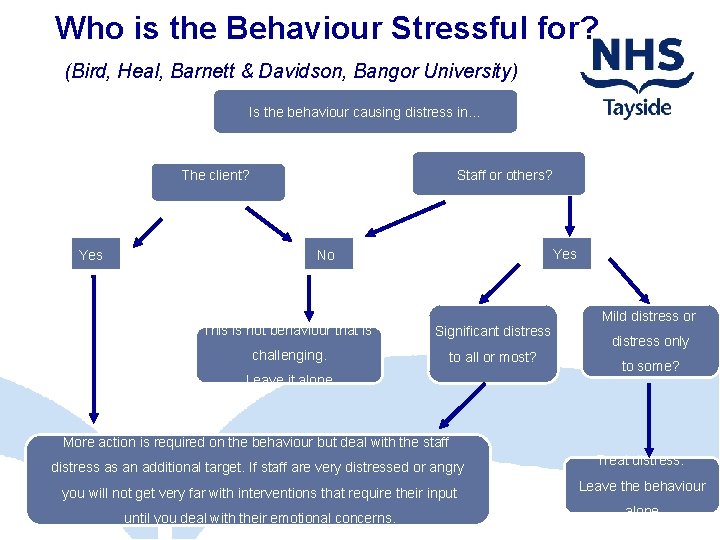
Who is the Behaviour Stressful for? (Bird, Heal, Barnett & Davidson, Bangor University) Is the behaviour causing distress in… The client? Yes Staff or others? Yes No This is not behaviour that is Significant distress challenging. to all or most? Leave it alone Mild distress or distress only to some? More action is required on the behaviour but deal with the staff distress as an additional target. If staff are very distressed or angry Treat distress. you will not get very far with interventions that require their input Leave the behaviour until you deal with their emotional concerns. alone.
Dr Helen Nicholson – Langley helen. nicholson-langley@nhs. net Dr Fiona Macleod fmacleod@nhs. net