Restrictive Management of Individuals Promoting Excellence in Dementia













- Slides: 36

Restrictive Management of Individuals Promoting Excellence in Dementia Masterclass 25 th March 2014 Stirling Management Centre George Kappler Deputy Chief Executive Mental Welfare Commission for Scotland

• When do we need to seek legal authority for a care and treatment plan? • What legal authority should be sought for which aspects of care plans? • Balancing autonomy, risk & protection • Human rights as a framework for decisions

Human rights as common foundation of values & law Values Law PANEL approach- International treaties – Participation – Accountability (including International Convention on Economic, Social & Cultural Rights- right to adequate standard of living & UN Convention on the Rights of Persons with Disabilities- right to Independent living) – Nondiscrimination European Rights – Empowerment (including right to life, prohibition on inhuman or degrading treatment, right to a private home & family life etc) – Legality Convention on Human Rights Act 1998, Scotland Act 1998 (incorporating ECHR into domestic law, s 6 duty on all those providing public function)
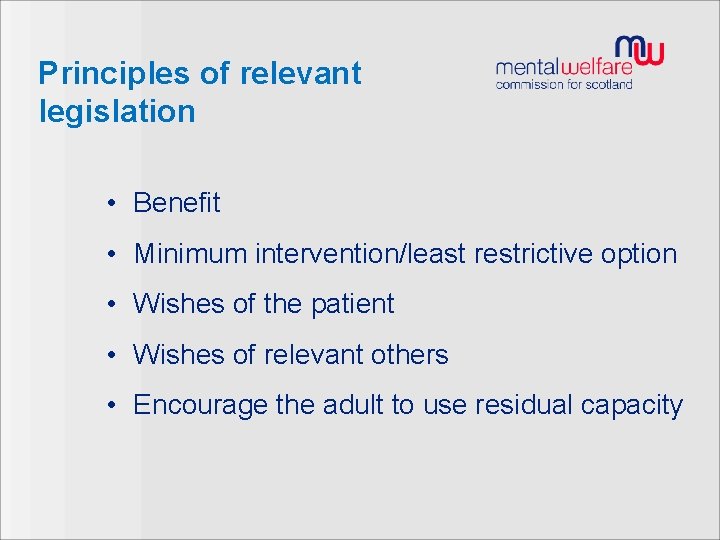
Principles of relevant legislation • Benefit • Minimum intervention/least restrictive option • Wishes of the patient • Wishes of relevant others • Encourage the adult to use residual capacity

Rights protected by HRA Article 2 - right to life Article 3 - prohibition of torture inhuman or degrading treatment or punishment Article 5 - right to liberty Article 6 - right to a fair & public hearing Article 8 - right to respect for private & family life, home & correspondence Article 9 - right to respect for freedom of thought, conscience & religion Article 10 - right to freedom of expression Article 11 - right to freedom of assembly & association Article 14 - Non-discrimination Article 1, Protocol 1 - right to property Article 2, Protocol 1 - right to education
Deprivation of Liberty (1) • We need to seek legal authority to implement a care/treatment plan when aspects of that care or treatment constitute a deprivation of liberty. (Article 5 ECHR) “Deprivation of liberty”, however, cannot be rigidly or, even, easily defined. • Depends on the individual circumstances of the case • Not restricted to institutional care • Determinations involve professional judgement based on good information and communication and, where possible, shared decision making • Determination involves objective as well as subjective elements
Deprivation of Liberty (2) The objective elements concern a person’s confinement in a particular restricted space for a not negligible length of time and the following should be taken into account: 1. The type, duration, effects & manner of implementation of the measure in question 2. Is the person free to leave 3. Use of restraint does not necessarily amount to a deprivation of liberty. It depends on its degree & intensity 4. Use of intrusive surveillance such as CCTV in bedrooms or bathrooms (Possible Article 8 ECHR issue - respect for private and family life) 5. Use of seclusion or time out 6. Complete & effective control over person’s care & movements 7. Restraints may be lawfully imposed at times when use gives someone with a disability as much freedom as possible in light of this disability – some European Courts have ruled
Deprivation of Liberty (3) Many judgements re deprivation of liberty will centre on the subjective elements: 1. The person’s capacity to give valid consent to measures restricting liberty on a clear & unequivocal basis 2. While caution should be urged, a person’s consent to their confinement may be inferred from the fact that the person does not object 3. However, later attempts to leave if blocked are likely to constitute a deprivation of liberty 4. Consent to one measure or set of measures does not imply consent to further additional measures 5. A person who lacks capacity to consent to detention who allows himself to be taken into detention does not mean they have consented to their detention. The right to liberty is too important in a democratic society for the person to lose the benefit of ECHR protection
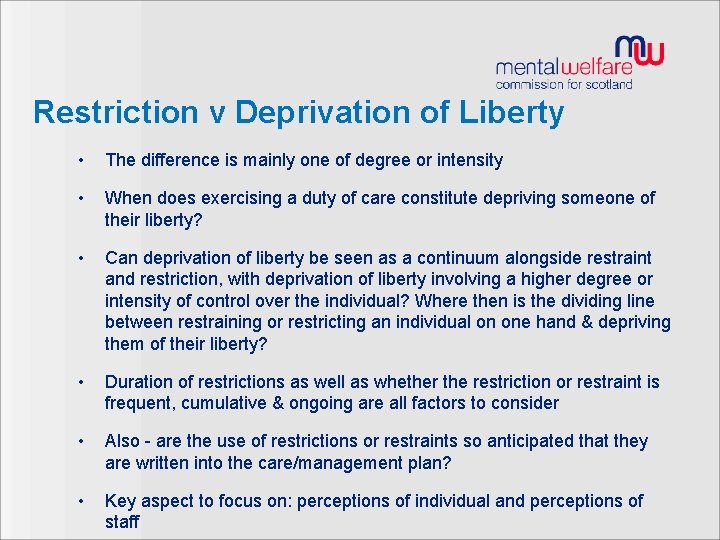
Restriction v Deprivation of Liberty • The difference is mainly one of degree or intensity • When does exercising a duty of care constitute depriving someone of their liberty? • Can deprivation of liberty be seen as a continuum alongside restraint and restriction, with deprivation of liberty involving a higher degree or intensity of control over the individual? Where then is the dividing line between restraining or restricting an individual on one hand & depriving them of their liberty? • Duration of restrictions as well as whether the restriction or restraint is frequent, cumulative & ongoing are all factors to consider • Also - are the use of restrictions or restraints so anticipated that they are written into the care/management plan? • Key aspect to focus on: perceptions of individual and perceptions of staff
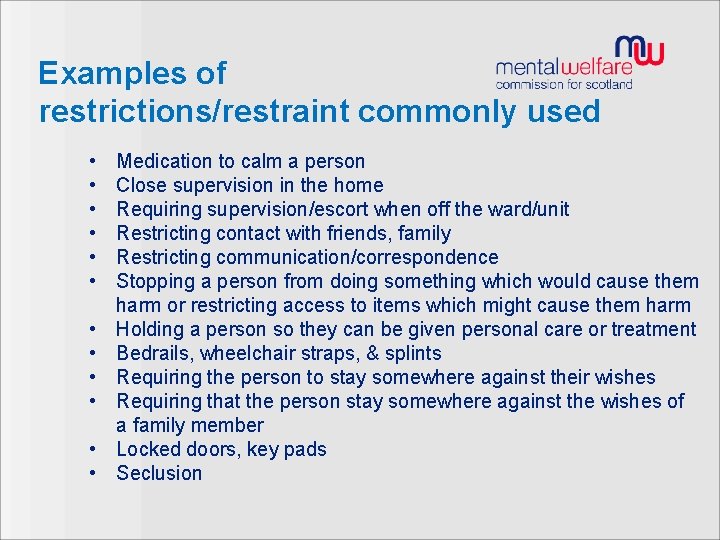
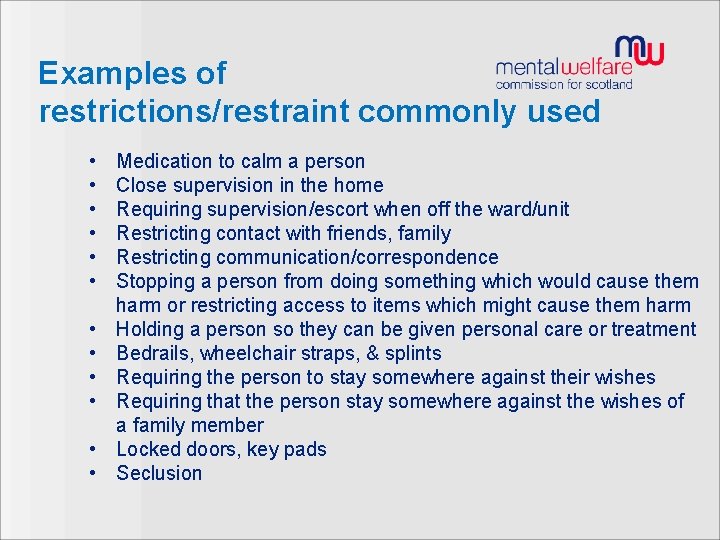
Examples of restrictions/restraint commonly used • • • Medication to calm a person Close supervision in the home Requiring supervision/escort when off the ward/unit Restricting contact with friends, family Restricting communication/correspondence Stopping a person from doing something which would cause them harm or restricting access to items which might cause them harm Holding a person so they can be given personal care or treatment Bedrails, wheelchair straps, & splints Requiring the person to stay somewhere against their wishes Requiring that the person stay somewhere against the wishes of a family member Locked doors, key pads Seclusion
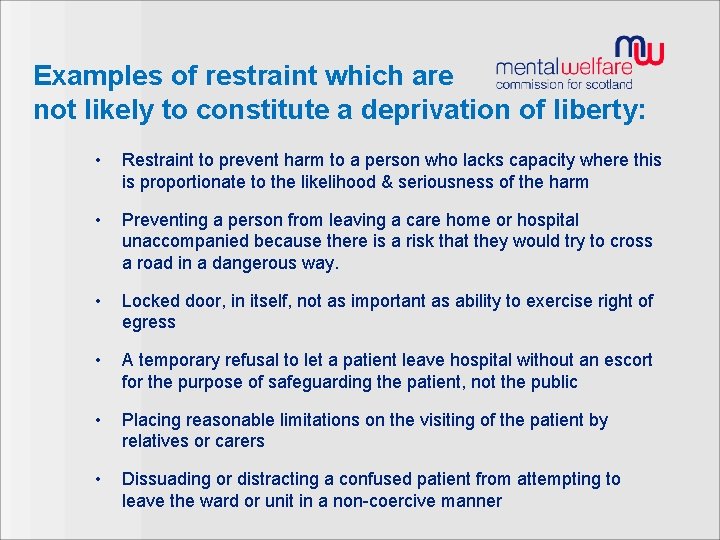
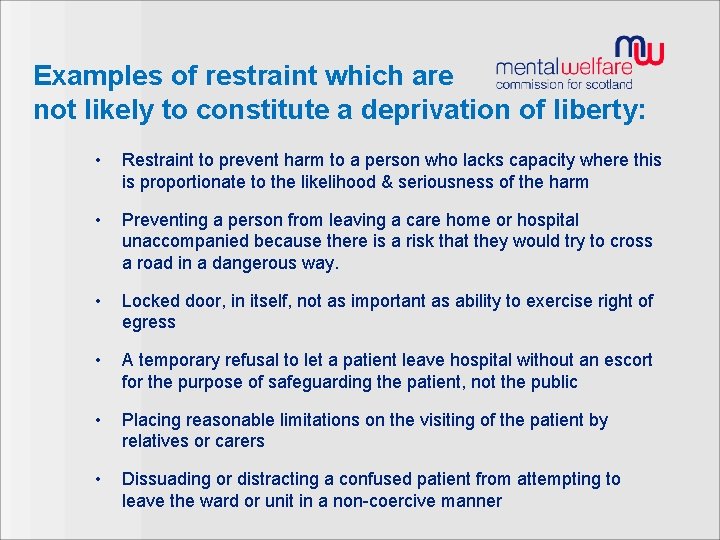
Examples of restraint which are not likely to constitute a deprivation of liberty: • Restraint to prevent harm to a person who lacks capacity where this is proportionate to the likelihood & seriousness of the harm • Preventing a person from leaving a care home or hospital unaccompanied because there is a risk that they would try to cross a road in a dangerous way. • Locked door, in itself, not as important as ability to exercise right of egress • A temporary refusal to let a patient leave hospital without an escort for the purpose of safeguarding the patient, not the public • Placing reasonable limitations on the visiting of the patient by relatives or carers • Dissuading or distracting a confused patient from attempting to leave the ward or unit in a non-coercive manner
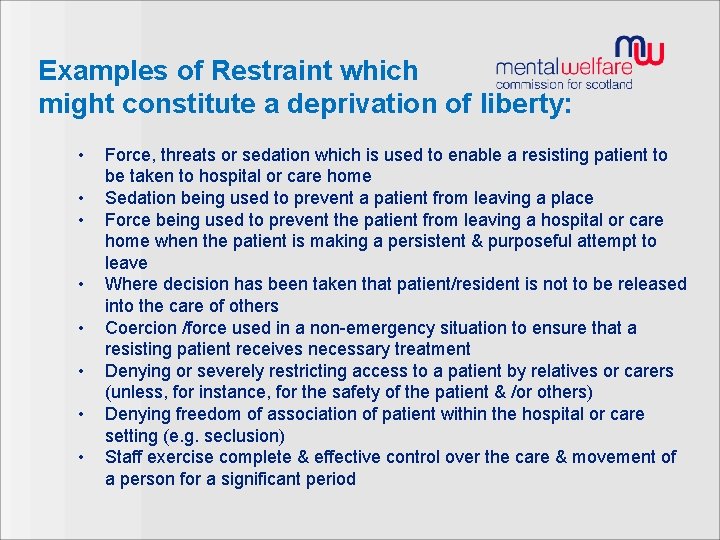
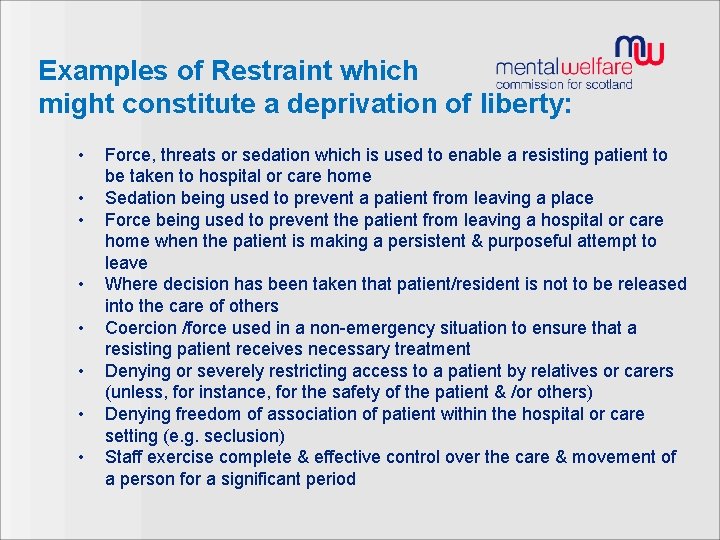
Examples of Restraint which might constitute a deprivation of liberty: • • Force, threats or sedation which is used to enable a resisting patient to be taken to hospital or care home Sedation being used to prevent a patient from leaving a place Force being used to prevent the patient from leaving a hospital or care home when the patient is making a persistent & purposeful attempt to leave Where decision has been taken that patient/resident is not to be released into the care of others Coercion /force used in a non-emergency situation to ensure that a resisting patient receives necessary treatment Denying or severely restricting access to a patient by relatives or carers (unless, for instance, for the safety of the patient & /or others) Denying freedom of association of patient within the hospital or care setting (e. g. seclusion) Staff exercise complete & effective control over the care & movement of a person for a significant period
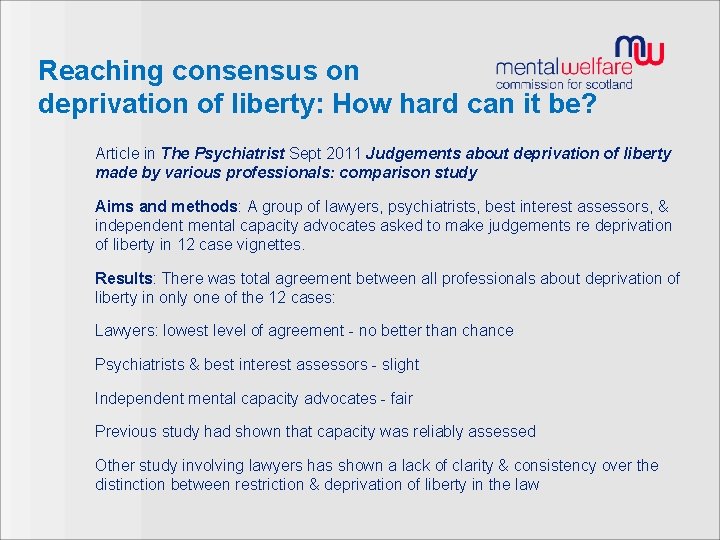
Reaching consensus on deprivation of liberty: How hard can it be? Article in The Psychiatrist Sept 2011 Judgements about deprivation of liberty made by various professionals: comparison study Aims and methods: A group of lawyers, psychiatrists, best interest assessors, & independent mental capacity advocates asked to make judgements re deprivation of liberty in 12 case vignettes. Results: There was total agreement between all professionals about deprivation of liberty in only one of the 12 cases: Lawyers: lowest level of agreement - no better than chance Psychiatrists & best interest assessors - slight Independent mental capacity advocates - fair Previous study had shown that capacity was reliably assessed Other study involving lawyers has shown a lack of clarity & consistency over the distinction between restriction & deprivation of liberty in the law
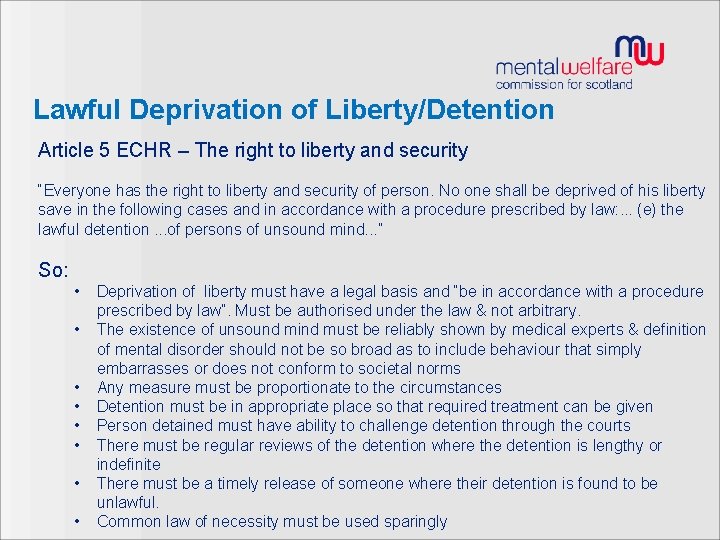
Lawful Deprivation of Liberty/Detention Article 5 ECHR – The right to liberty and security “Everyone has the right to liberty and security of person. No one shall be deprived of his liberty save in the following cases and in accordance with a procedure prescribed by law: . . . (e) the lawful detention. . . of persons of unsound mind. . . ” So: • • Deprivation of liberty must have a legal basis and “be in accordance with a procedure prescribed by law”. Must be authorised under the law & not arbitrary. The existence of unsound mind must be reliably shown by medical experts & definition of mental disorder should not be so broad as to include behaviour that simply embarrasses or does not conform to societal norms Any measure must be proportionate to the circumstances Detention must be in appropriate place so that required treatment can be given Person detained must have ability to challenge detention through the courts There must be regular reviews of the detention where the detention is lengthy or indefinite There must be a timely release of someone where their detention is found to be unlawful. Common law of necessity must be used sparingly

Key rights explained – Article 8 - Right to respect for private & family life, home & correspondence • Potential widening scope relating to dignity & autonomy & positive & negative obligations applying to: – Autonomy & self-determination: to conduct your own life as you choose, including in ways seen to be harmful – Participation in decision making (e. g. decisions about treatment or care, consent to medical treatment, support for decision making etc) – Privacy (e. g. personal privacy at home or in care home, use of personal information etc) – Family life (e. g. separation from spouse in residential care, social isolation) – Physical & psychological integrity (e. g. poor quality care or inadequate service provision not amounting to inhuman treatment) – Legal tests of legality (in accordance with law), legitimate aim (justification) & proportionality (minimum necessary interference)

Interference with qualified rights Qualified rights include: § The right to respect for private & family life, home & correspondence § The right to freedom of thought, conscience & religion § The right to freedom of expression § The right to freedom of assembly & association § The right to protection of property Any restriction must be: § In accordance with the law: have a basis in domestic law, safeguards against arbitrary interference, foreseeable § In pursuit of a legitimate aim: including “the economic well-being of the country”; “the protection of health” § Necessary § Proportionate § Not discriminatory

Interference with qualified rights Proportionality § “Don’t use a sledgehammer to crack a nut. ” § What is the problem being addressed by the restriction upon someone’s rights? § Will the restriction lead to a reduction in the problem? § Does a less restrictive alternative exist & has it been tried? § Does that restriction involve a blanket policy or does it allow for different individual cases to be treated differently? § Has sufficient regard been paid to the rights & interests of those affected? § Do safeguards exist against error or abuse? § Does the restriction destroy the basic ideas behind the human rights at issue?
Framework for decisions • Is it an emergency? • What rights are affected? • Is it a right that can be restricted? • Is it in pursuit of a legitimate aim? • Is it lawful? • Is it necessary? • Is it a proportionate response?
Consider • What are the potentially restrictive practices? • Under what authority are staff carrying out their duties? • ECHR considerations? • What legal interventions should be considered? • Alternatives to current situation? • What difference does age and capacity make?

Proportionate response • Questions above on proportionality • Also consider: – Benefit v Risk – Consequences of acting or not acting – Level & seriousness of risk – Least restrictive option – Other actions considered – Views of individual & others considered
Restrictive Management of People with Mental Disorder: Relevant Provisions in Legislation • Adults with Incapacity (Scotland) Act 2000 • Mental Health (Care & Treatment) (Scotland) Act 2003 • Adult Support & Protection (Scotland) Act 2007
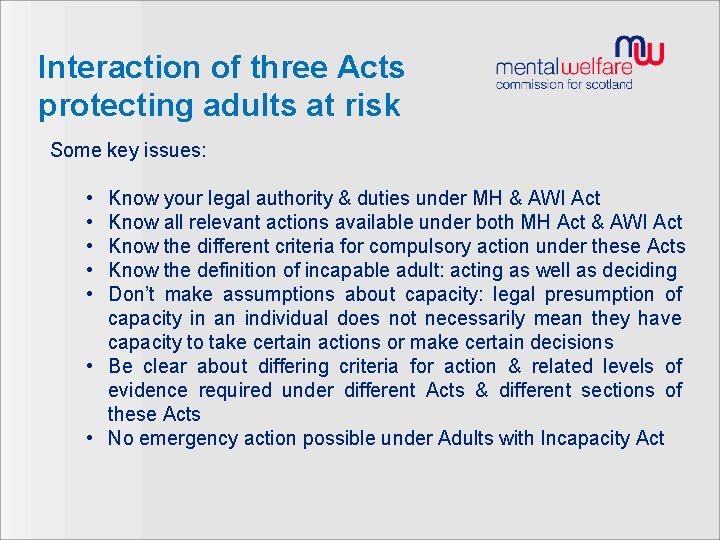
Interaction of three Acts protecting adults at risk Some key issues: • • • Know your legal authority & duties under MH & AWI Act Know all relevant actions available under both MH Act & AWI Act Know the different criteria for compulsory action under these Acts Know the definition of incapable adult: acting as well as deciding Don’t make assumptions about capacity: legal presumption of capacity in an individual does not necessarily mean they have capacity to take certain actions or make certain decisions • Be clear about differing criteria for action & related levels of evidence required under different Acts & different sections of these Acts • No emergency action possible under Adults with Incapacity Act
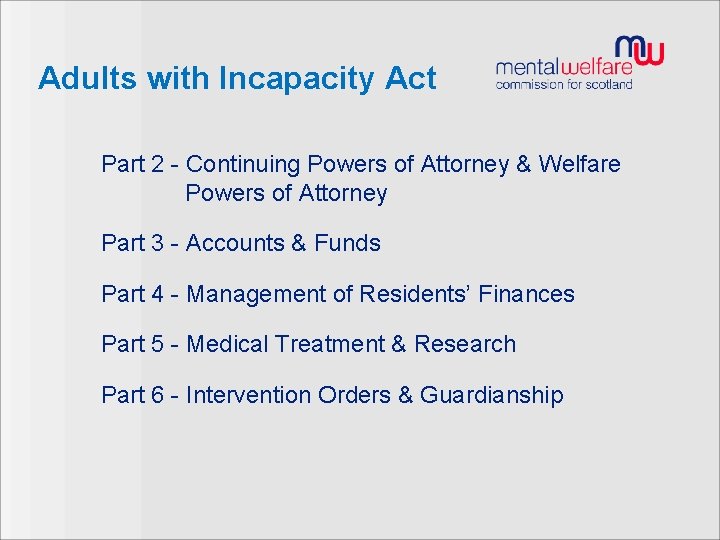
Adults with Incapacity Act Part 2 - Continuing Powers of Attorney & Welfare Powers of Attorney Part 3 - Accounts & Funds Part 4 - Management of Residents’ Finances Part 5 - Medical Treatment & Research Part 6 - Intervention Orders & Guardianship
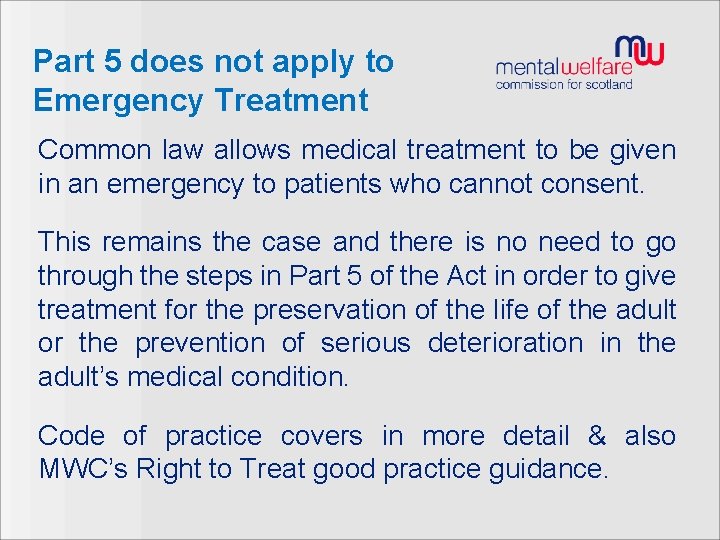
Part 5 does not apply to Emergency Treatment Common law allows medical treatment to be given in an emergency to patients who cannot consent. This remains the case and there is no need to go through the steps in Part 5 of the Act in order to give treatment for the preservation of the life of the adult or the prevention of serious deterioration in the adult’s medical condition. Code of practice covers in more detail & also MWC’s Right to Treat good practice guidance.
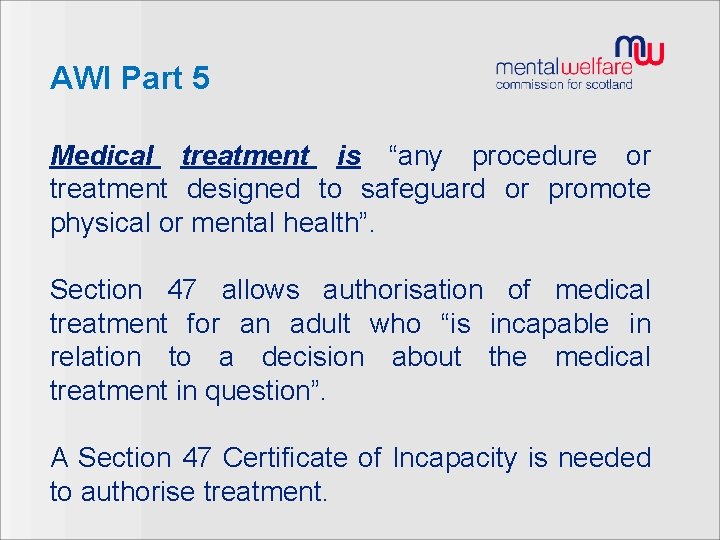
AWI Part 5 Medical treatment is “any procedure or treatment designed to safeguard or promote physical or mental health”. Section 47 allows authorisation of medical treatment for an adult who “is incapable in relation to a decision about the medical treatment in question”. A Section 47 Certificate of Incapacity is needed to authorise treatment.
AWI Part 5 Section 47 certificate needed, but cannot alone authorise treatments subject to further safeguards under S 48/Regulations. Need MWC-appointed Doctor arranged to approve: • Drug treatment for the purpose of reducing sex drive, other than surgical implantation of hormones. • ECT for mental disorder. • Abortion. • Any medical treatment which is considered likely by the medical practitioner primarily responsible to lead to sterilisation as an unavoidable result.
AWI Part 5 Section 47 and Mental Disorder § Section 47 cannot authorise treatment for mental disorder for an adult to whom Part 16 of the Mental Health Act applies (i. e. treatment of mental disorder authorised under Mental Health Act). § MWC advises advise using the Mental Health Act if it is necessary to give treatment for mental disorder & the person resists or objects to that treatment.
AWI Part 5 Who can assess the adult’s capacity and complete a Section 47 certificate? 1. The medical practitioner primarily responsible for the medical treatment of the adult 2. Since amendment of 2005, a dental practitioner; ophthalmic optician; registered nurse if…………………. they have done the training, & are primarily responsible for medical treatment of the kind in question Usually completion of S 47 certificate falls to doctor (can be paid for dental certificates).
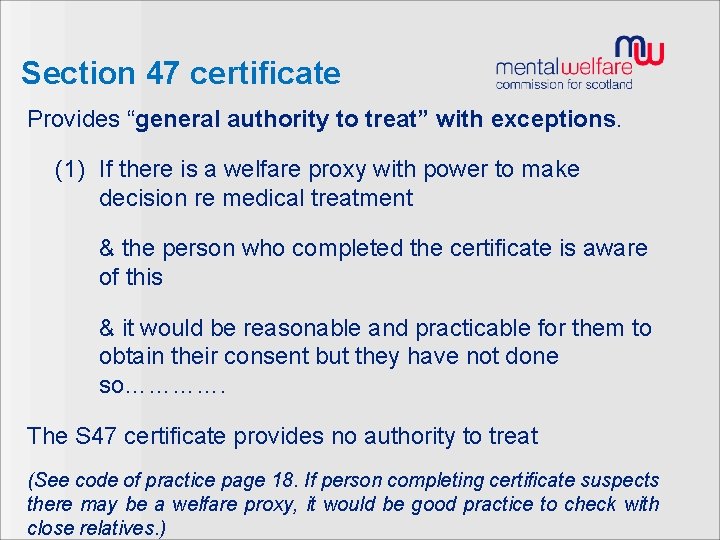
Section 47 certificate Provides “general authority to treat” with exceptions. (1) If there is a welfare proxy with power to make decision re medical treatment & the person who completed the certificate is aware of this & it would be reasonable and practicable for them to obtain their consent but they have not done so…………. The S 47 certificate provides no authority to treat (See code of practice page 18. If person completing certificate suspects there may be a welfare proxy, it would be good practice to check with close relatives. )
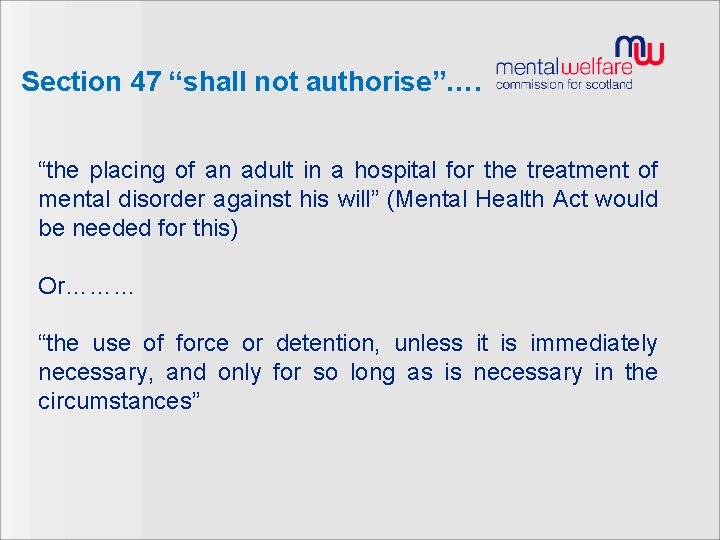
Section 47 “shall not authorise”…. “the placing of an adult in a hospital for the treatment of mental disorder against his will” (Mental Health Act would be needed for this) Or……… “the use of force or detention, unless it is immediately necessary, and only for so long as is necessary in the circumstances”



Guardianship & Care Homes


www. mwcscot. org. uk
 Promoting excellence in dementia care
Promoting excellence in dementia care Nonrestrictive clause definition
Nonrestrictive clause definition Risk management for enterprises and individuals
Risk management for enterprises and individuals Quality management for organizational excellence
Quality management for organizational excellence Project management center of excellence
Project management center of excellence Project management center of excellence
Project management center of excellence Project management center of excellence
Project management center of excellence Quality management for organizational excellence
Quality management for organizational excellence Promoting moral improvement
Promoting moral improvement Promote service arrange decide
Promote service arrange decide Promoting alternative thinking strategies
Promoting alternative thinking strategies Lesson 4 promoting health and wellness
Lesson 4 promoting health and wellness Do. 27 s. 2015 promoting family earthquake preparedness
Do. 27 s. 2015 promoting family earthquake preparedness Chapter 1 lesson 4 promoting health and wellness
Chapter 1 lesson 4 promoting health and wellness Promoting racial literacy in schools
Promoting racial literacy in schools Lesson 4 promoting health and wellness
Lesson 4 promoting health and wellness Methods of promoting intrapreneurship leaving cert
Methods of promoting intrapreneurship leaving cert Keeping an infant safe and well section 7-3
Keeping an infant safe and well section 7-3 Example of deontology
Example of deontology Chapter 7 promoting health and wellness
Chapter 7 promoting health and wellness Chapter 30 promoting bowel elimination
Chapter 30 promoting bowel elimination Chapter 13 distributing and promoting products
Chapter 13 distributing and promoting products Promoting services and educating customers
Promoting services and educating customers Health promoting schools model
Health promoting schools model Rehearsal strategies
Rehearsal strategies Promoting a positive health and safety culture
Promoting a positive health and safety culture Unit 11 safeguarding adults and promoting independence
Unit 11 safeguarding adults and promoting independence Promoting national integration
Promoting national integration Explain the role of sido in promoting entrepreneurship.
Explain the role of sido in promoting entrepreneurship. Health promoting school
Health promoting school Japan's principal asset in promoting development is
Japan's principal asset in promoting development is Health and wellness vocabulary
Health and wellness vocabulary Unjustified restrictive gatekeeping
Unjustified restrictive gatekeeping Obstructive vs restrictive
Obstructive vs restrictive Politique monetaire restrictive
Politique monetaire restrictive Lung
Lung Iep justification statement examples
Iep justification statement examples