Procalcitonin A Useful Tool Thomas File M D
- Slides: 39
Procalcitonin: A Useful Tool? Thomas File, M. D. , M. Sc. MACP, FIDSA, FCCP Chair, Infectious Disease Division Summa Health System, Akron, OH; Chair, Infectious Disease Section Northeast Ohio Medical University, Rootstown, Ohio
DISCLOSURES • Consultant for Actavis plc, Cempra, Merck & Co. Inc. , and Pfizer Inc • Serves on the scientific advisory boards for Motif. Bio, Nabriva Therapeutics and Tetraphase Pharmaceuticals
LEARNING OBJECTIVES • At the end of this lecture, the learner will be able to: – Interpret results of procalcitonin – Evaluate studies that have utilized procalcitonin to de-escalate or discontinue antibiotics – Use procalcitonin in the context of an antimicrobial stewardship program
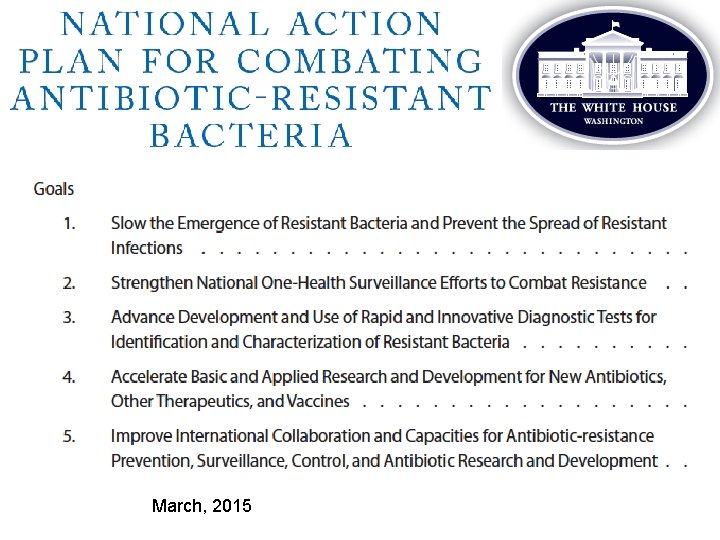
More Americans die each year from antibiotic-resistant bacteria than AIDS, and there are no new drugs coming By Tim Fernholz — November 7, 2013 “…unless we level the playing field on microbes…. it is no dramatization to say that much of modern medicine is at risk. ” T Frieden March 2, 2015 4
March, 2015
Solution: Antimicrobial Stewardship Clin Infect Dis. 2014; 59: S 93 -96
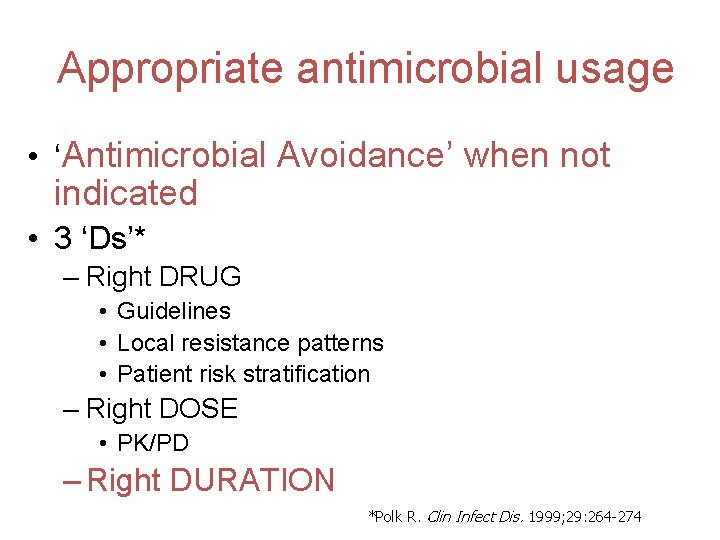
Appropriate antimicrobial usage • ‘Antimicrobial Avoidance’ when not indicated • 3 ‘Ds’* – Right DRUG • Guidelines • Local resistance patterns • Patient risk stratification – Right DOSE • PK/PD – Right DURATION *Polk R. Clin Infect Dis. 1999; 29: 264 -274
– “ Two nonsynchronous events have affected management of CAP • Spiraling empiricims – Broad spectrum antimicrobial therapy with deemphasis of microbiology » Just treat for everything » Consequence of increase resistance – “golden era” of clinical microbiology » Non culture-based (e. g. , Urinary Antigen, Molecular tests) » Rapid ID of pathogen » Offers more specific therapy (Chest 2009; 136: 1618)
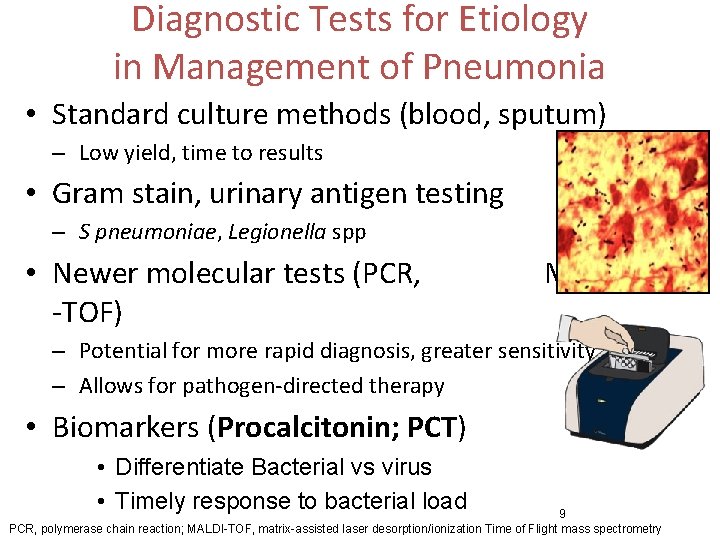
Diagnostic Tests for Etiology in Management of Pneumonia • Standard culture methods (blood, sputum) – Low yield, time to results • Gram stain, urinary antigen testing – S pneumoniae, Legionella spp • Newer molecular tests (PCR, -TOF) MALDI – Potential for more rapid diagnosis, greater sensitivity – Allows for pathogen-directed therapy • Biomarkers (Procalcitonin; PCT) • Differentiate Bacterial vs virus • Timely response to bacterial load 9 PCR, polymerase chain reaction; MALDI-TOF, matrix-assisted laser desorption/ionization Time of Flight mass spectrometry
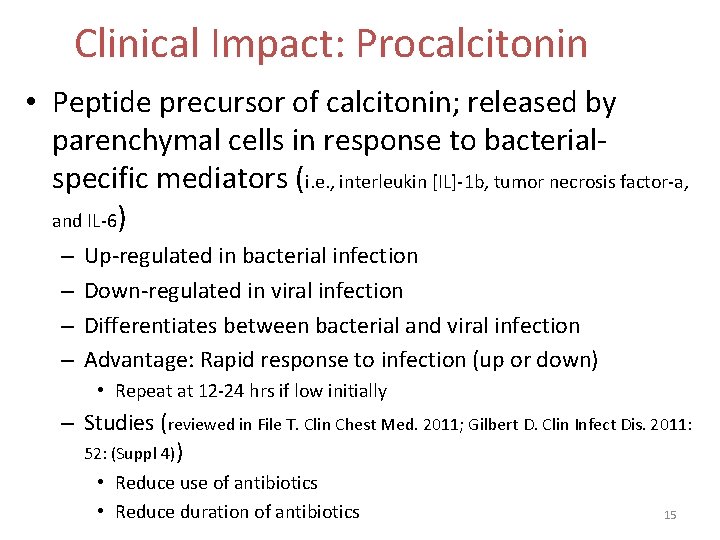
PROCALCITONIN (PCT) • Peptide precursor of calcitonin • ‘Hormokine’ – Expressed by neuroendocrine cells (e. g. thyroid) • Healthy individuals, non detected – Released like a cytokine by variety of parenchymal cells (e. g. liver, monoctes) in response to microbial toxins and proinflammatory mediators (IL-1, TNFα, IL-6) • Increased in bacterial infection – PCT inhibited by TNF-ϒ in response to variety viral infections • Attenuated in viral infection Niederman Clin Infect Dis. 2008; 47: S 127 -; Gilbert Clin Infect Dis 2011
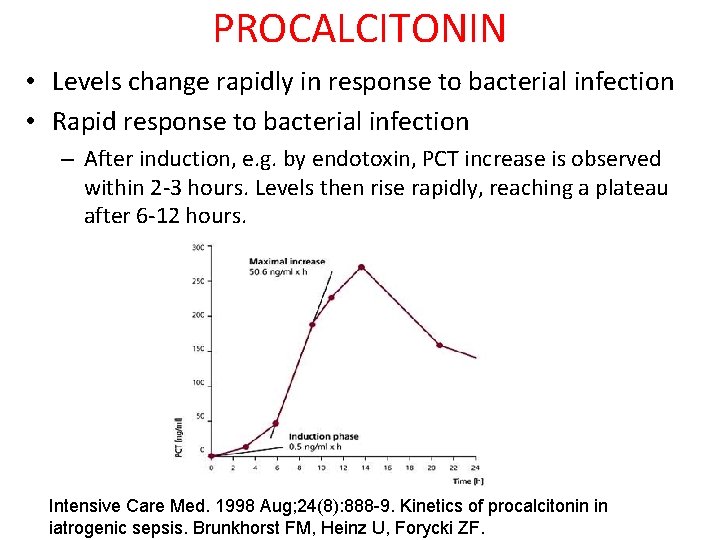
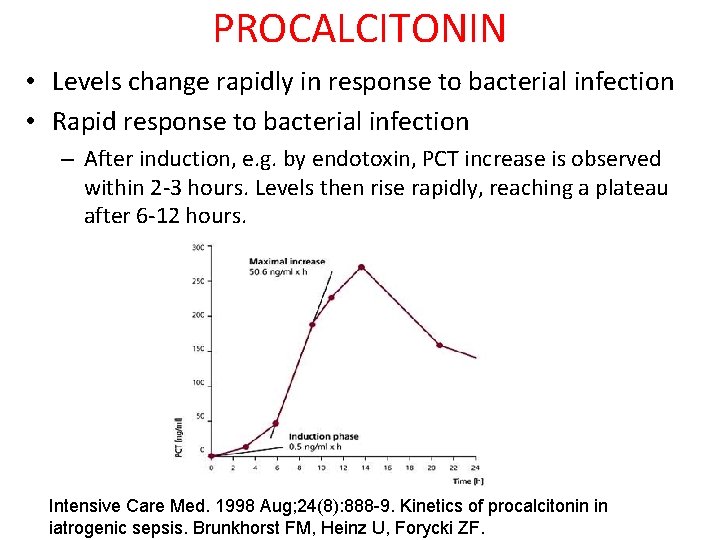
PROCALCITONIN • Levels change rapidly in response to bacterial infection • Rapid response to bacterial infection – After induction, e. g. by endotoxin, PCT increase is observed within 2 -3 hours. Levels then rise rapidly, reaching a plateau after 6 -12 hours. Intensive Care Med. 1998 Aug; 24(8): 888 -9. Kinetics of procalcitonin in iatrogenic sepsis. Brunkhorst FM, Heinz U, Forycki ZF.
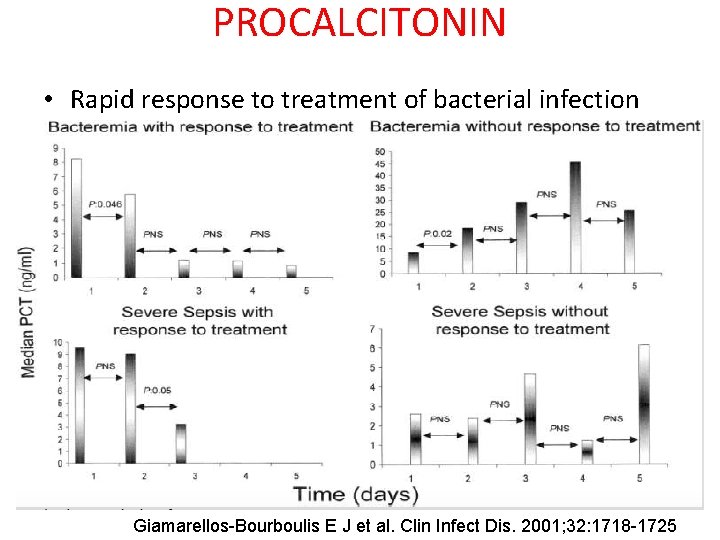
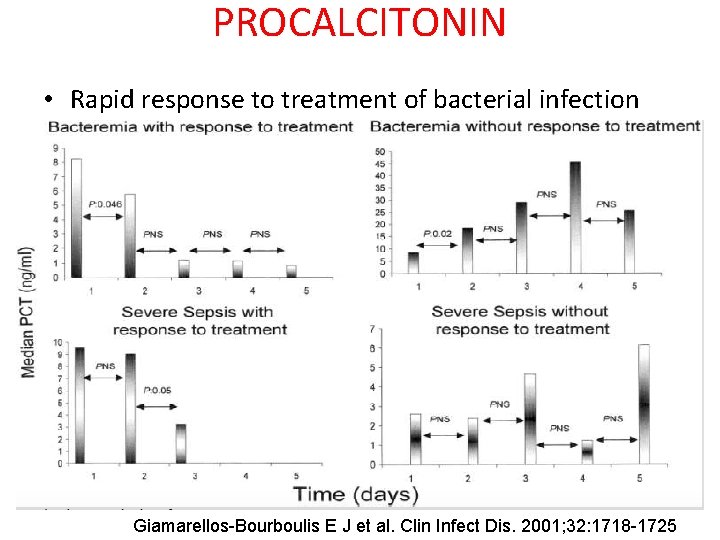
PROCALCITONIN • Rapid response to treatment of bacterial infection Giamarellos-Bourboulis E J et al. Clin Infect Dis. 2001; 32: 1718 -1725
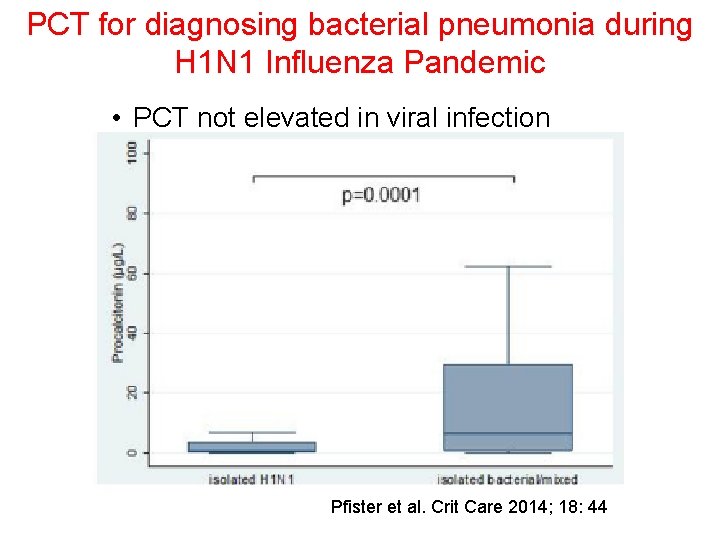
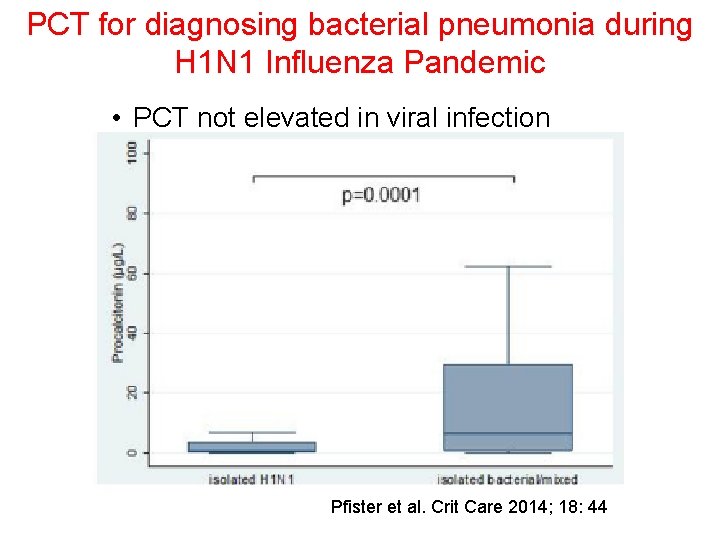
PCT for diagnosing bacterial pneumonia during H 1 N 1 Influenza Pandemic • PCT not elevated in viral infection Pfister et al. Crit Care 2014; 18: 44
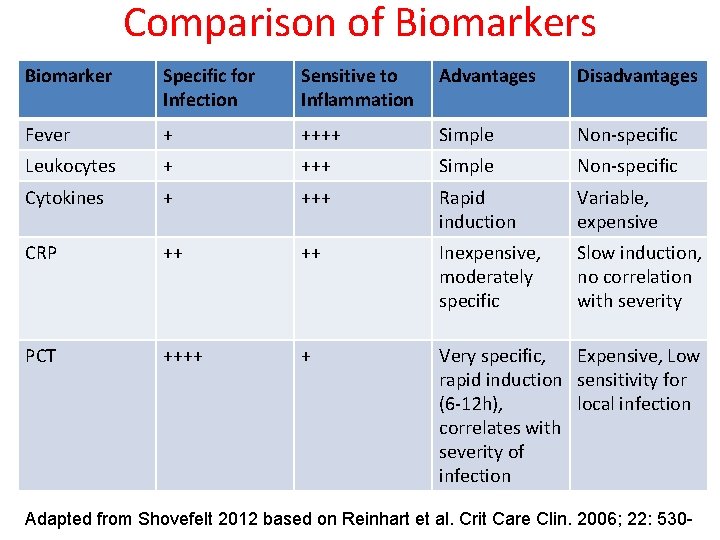
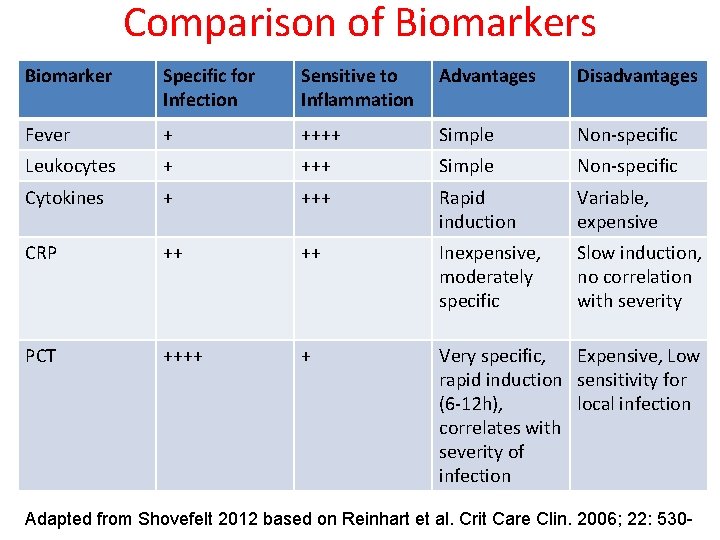
Comparison of Biomarkers Biomarker Specific for Infection Sensitive to Inflammation Advantages Disadvantages Fever + ++++ Simple Non-specific Leukocytes + +++ Simple Non-specific Cytokines + +++ Rapid induction Variable, expensive CRP ++ ++ Inexpensive, moderately specific Slow induction, no correlation with severity PCT ++++ + Very specific, Expensive, Low rapid induction sensitivity for (6 -12 h), local infection correlates with severity of infection Adapted from Shovefelt 2012 based on Reinhart et al. Crit Care Clin. 2006; 22: 530 -
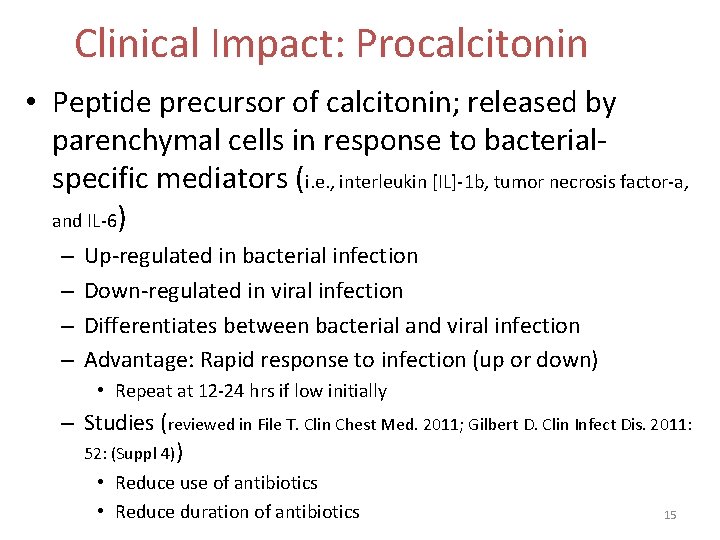
Clinical Impact: Procalcitonin • Peptide precursor of calcitonin; released by parenchymal cells in response to bacterialspecific mediators (i. e. , interleukin [IL]-1 b, tumor necrosis factor-a, and IL-6) – – Up-regulated in bacterial infection Down-regulated in viral infection Differentiates between bacterial and viral infection Advantage: Rapid response to infection (up or down) • Repeat at 12 -24 hrs if low initially – Studies (reviewed in File T. Clin Chest Med. 2011; Gilbert D. Clin Infect Dis. 2011: 52: (Suppl 4)) • Reduce use of antibiotics • Reduce duration of antibiotics 15
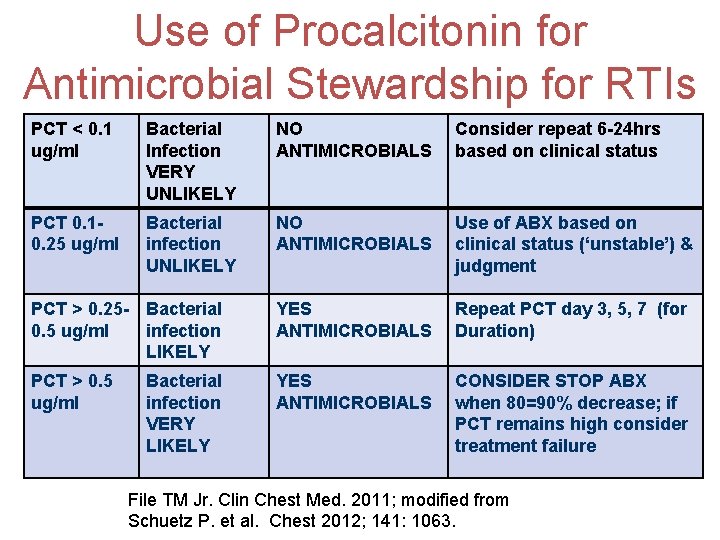
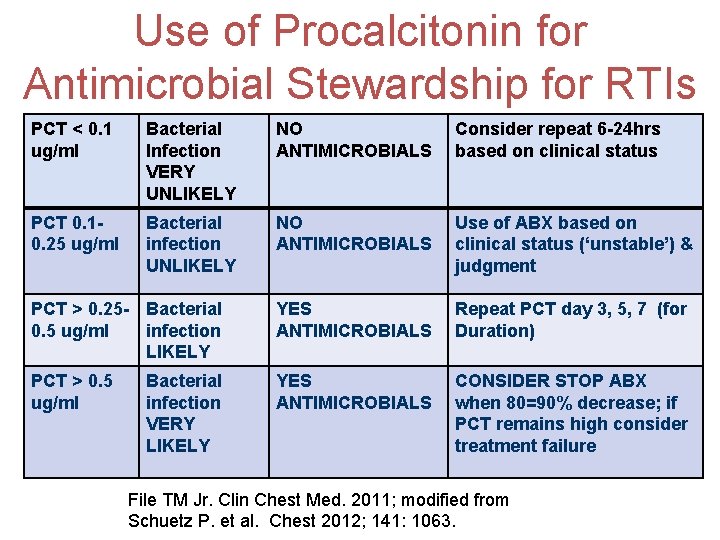
Use of Procalcitonin for Antimicrobial Stewardship for RTIs PCT < 0. 1 ug/ml Bacterial Infection VERY UNLIKELY NO ANTIMICROBIALS Consider repeat 6 -24 hrs based on clinical status PCT 0. 10. 25 ug/ml Bacterial infection UNLIKELY NO ANTIMICROBIALS Use of ABX based on clinical status (‘unstable’) & judgment PCT > 0. 25 - Bacterial 0. 5 ug/ml infection LIKELY YES ANTIMICROBIALS Repeat PCT day 3, 5, 7 (for Duration) PCT > 0. 5 ug/ml YES ANTIMICROBIALS CONSIDER STOP ABX when 80=90% decrease; if PCT remains high consider treatment failure Bacterial infection VERY LIKELY File TM Jr. Clin Chest Med. 2011; modified from Schuetz P. et al. Chest 2012; 141: 1063.
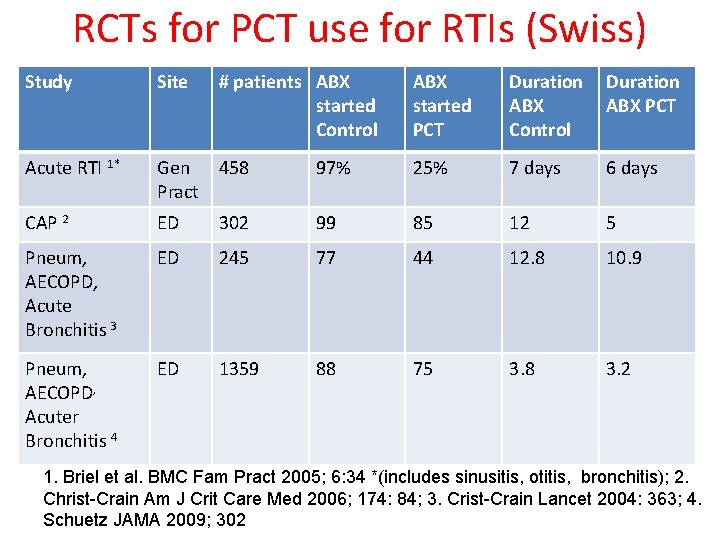
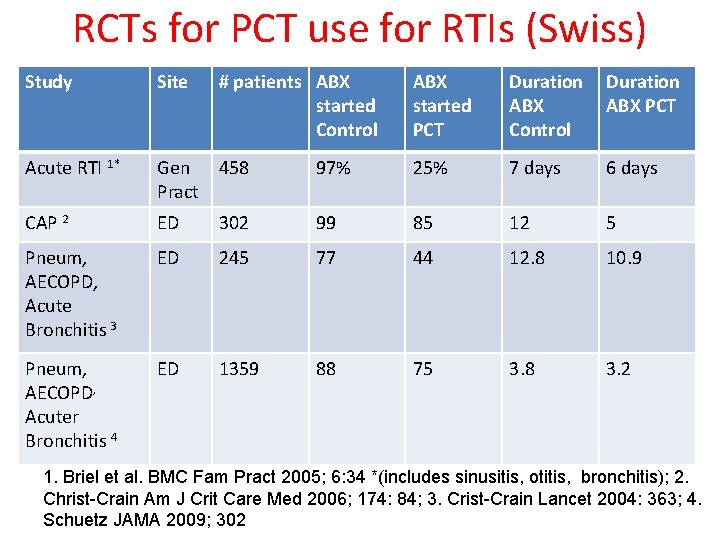
RCTs for PCT use for RTIs (Swiss) Study Site # patients ABX started Control ABX started PCT Duration ABX Control Duration ABX PCT Acute RTI 1* Gen 458 Pract 97% 25% 7 days 6 days CAP 2 ED 302 99 85 12 5 Pneum, AECOPD, Acute Bronchitis 3 ED 245 77 44 12. 8 10. 9 Pneum, AECOPD, Acuter Bronchitis 4 ED 1359 88 75 3. 8 3. 2 1. Briel et al. BMC Fam Pract 2005; 6: 34 *(includes sinusitis, otitis, bronchitis); 2. Christ-Crain Am J Crit Care Med 2006; 174: 84; 3. Crist-Crain Lancet 2004: 363; 4. Schuetz JAMA 2009; 302
Procalcitonin guidance of antibiotic therapy in CAP • RCT; 302 patients; ABX based on PCT (<0. 1; strongly discouraged) vs ‘usual practice’ • Findings: – Reduced ABX prescriptions (85 vs 99%, < 0. 001) – Reduced ABX duration (5 vs 12 d, p < 0. 001) – Clinical success at 4 -6 weeks; CAP recurrence similar in both groups • Conclusions: PCT substantially reduces ABX use Christ-Crain. AM J Crit Care Med. 2006
PCT to Initiate or Discontinue Antibiotics for RTI • Systematic Review • Findings • 14 trials, 4221 particicpants • Robust data for reduced ABX use and duration (8 to 4 d) • Treatment failure: PCT 19% vs 22% • Conclusions • Use of procalcitonin to guide initiation and duration of antibiotic treatment in patients with ARI assoc with less ABX use and not associated with higher mortality rates or treatment failure. Scheutz P eta l. Cochrane Database of Systematic Reviews 2012, Issue 9. Art. No. : CD 007498
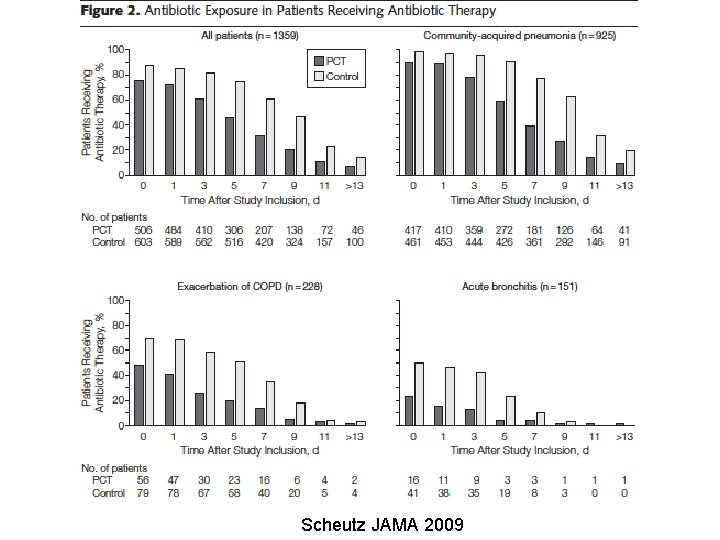
Effect of PCT-based Guidelines vs Standard Guidelines on Antibiotic Use in LRTIs (Pro. HOSP Trial) • Multicenter, RCT, 6 Swiss Eds – randomized to use of antibiotics based on a PCT algorithm with predefined cutoff ranges for initiating or stopping antibiotics (PCT group) or according to standard guidelines (control group). • Findings: – Reduction ABX PCT 5. 7 vs Control 8. 7 days (-38%; 40, -28) – Adverse outcome PCT 15. 5% vs 18. 9% (-7, 0. 4) • ABX Assoc PCT 19. 8% vs 28. 1% ( -12. 7, -3. 7) Schuetz P et al. JAMA 2009; 302: 1059 -
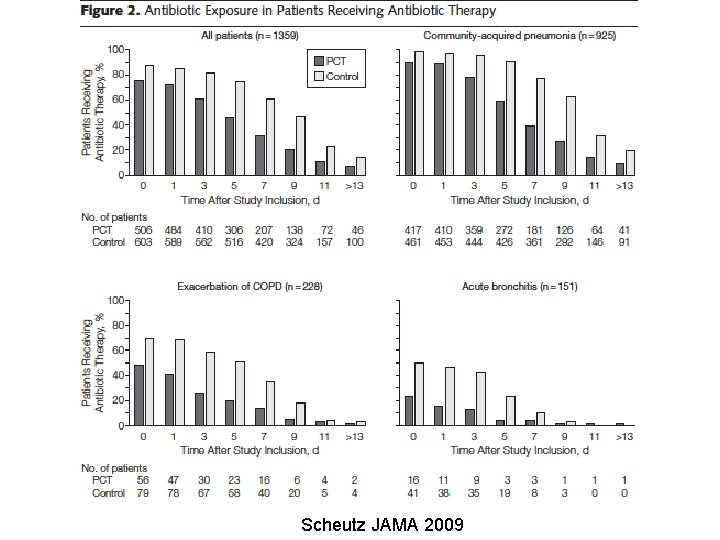
Scheutz JAMA 2009
PCT and VAP • Cochrane Systematic Review • 3 trials investigating use of PCT. • Based on recommendation for ABX duration based on PCT level – associated with significantly reduced duration of ABX therapy (mean difference -3. 20 days; 95% CI -4. 45 to 1. 95) and 28 -day antibiotic-free days (MD 2. 80 days; 95% CI 1. 39 to 4. 21). – There were no significant differences in other outcomes, though a trend towards greater recurrence was observed in one study. Pugh R, et al. Cochrane Database of Systematic Reviews 2011, Issue 10. Art. No. : CD 007577
Use of procalcitonin to shorten antibiotic treatment duration in septic patients • RCT: DC ABX when PCT decreased 90% vs clinical jusdgement • Results: – In pts in whom decision could be made based on PCT, PCT guidance led to 4 -day reduction of ABX therapy (n=69, p = 0. 003) and less ABX use (p = 0. 0002); 2 - day shorter ICU LOS – Similar mortality & recurrence • Conclusion: PCT protocol allow reducing ABX duration and exposure in sepsis – Nobre et al. Am J Respir Crit Care Med 2008; 177: 498 -
Economic evaluation of procalcitoninguided antibiotic therapy in acute respiratory infections (US) • Cost-impact model based on meta-analysis data of RCTs for RTIs (out and In patients) • Results: – Net savings of $6 million to US integrated delivery network per one million member cohort (2014), most from outpatient – For whole US insured, results in $1. 6 billion savings annually Scheutz et al. Clin Chem Lab Med. 2015; pre print
PCT: limitations • Expense • Turn Around Time – Dependent on lab processes • May require Serial determinations • Causes other than bacterial infection • Optimal cutoff
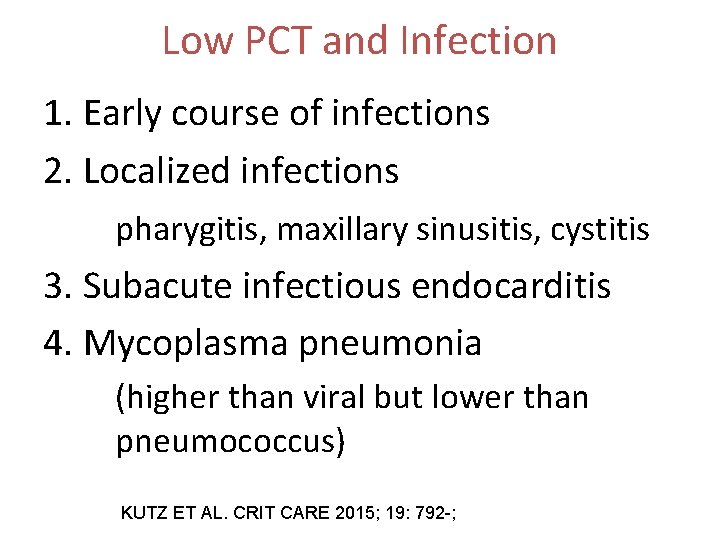
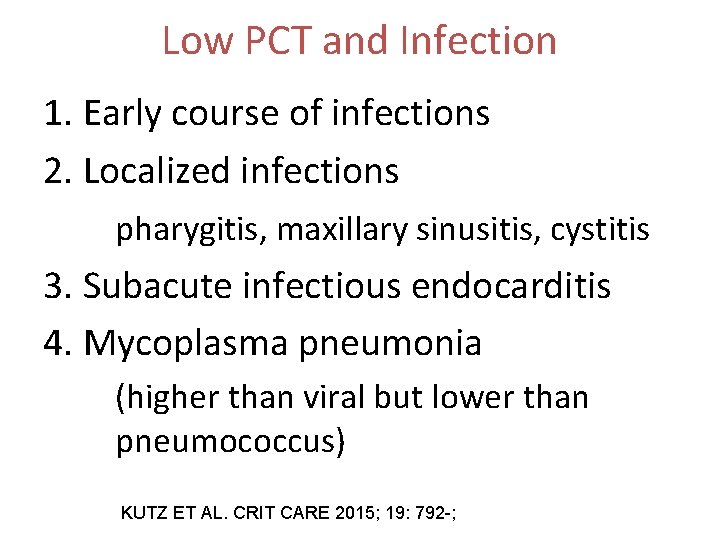
Low PCT and Infection 1. Early course of infections 2. Localized infections pharygitis, maxillary sinusitis, cystitis 3. Subacute infectious endocarditis 4. Mycoplasma pneumonia (higher than viral but lower than pneumococcus) KUTZ ET AL. CRIT CARE 2015; 19: 792 -;
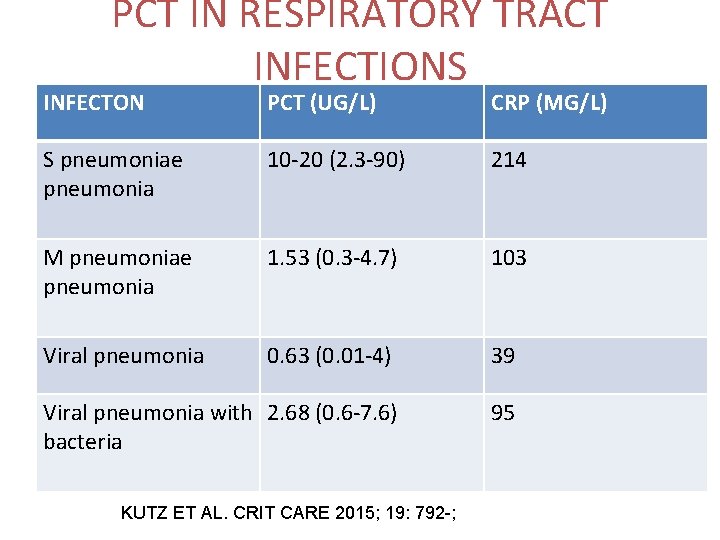
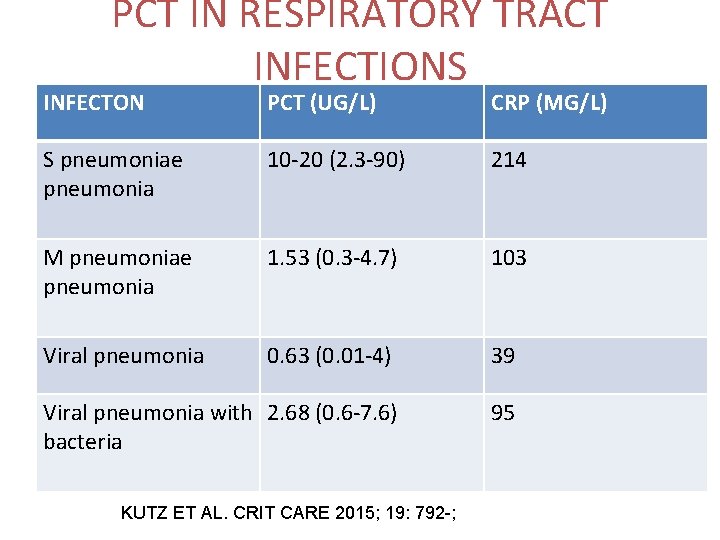
PCT IN RESPIRATORY TRACT INFECTIONS INFECTON PCT (UG/L) CRP (MG/L) S pneumoniae pneumonia 10 -20 (2. 3 -90) 214 M pneumoniae pneumonia 1. 53 (0. 3 -4. 7) 103 Viral pneumonia 0. 63 (0. 01 -4) 39 Viral pneumonia with 2. 68 (0. 6 -7. 6) bacteria 95 KUTZ ET AL. CRIT CARE 2015; 19: 792 -;
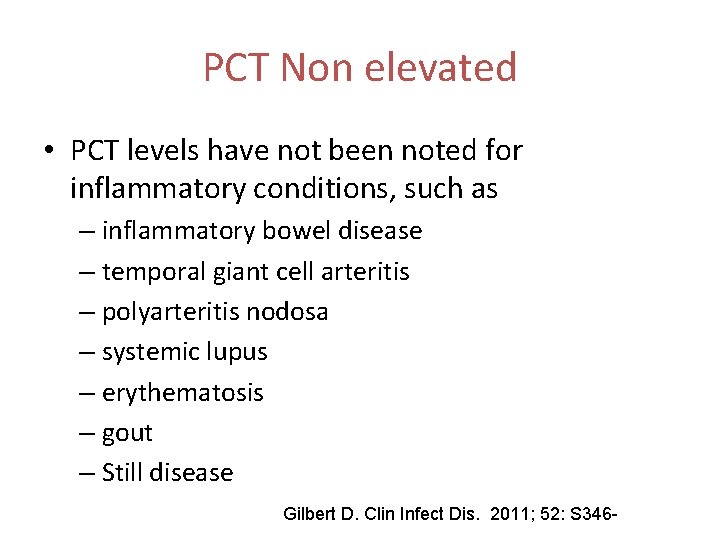
PCT Non elevated • PCT levels have not been noted for inflammatory conditions, such as – inflammatory bowel disease – temporal giant cell arteritis – polyarteritis nodosa – systemic lupus – erythematosis – gout – Still disease Gilbert D. Clin Infect Dis. 2011; 52: S 346 -
PCT Sepsis • Helpful to decrease duration • Present data suggests initial result unable to reliably use to withhold ABX Luyt CE, et al. Usefulness of procalcitonin for the diagnosis of ventilator-associated pneumonia. Intensive Care Med 2008; 34(8): 1434 -1440. Dallas J, et al. Diagnostic utility of plasma procalcitonin for nosocomial pneumonia in the intensive care unit setting. Respir Care 2011; 56(4): 412 -419. Ramirez P, et al. Sequential measurements of procalcitonin levels in diagnosing ventilator-associated pneumonia. Eur Respir J 2008; 31(2): 356 -362. Duflo F, et al. Alveolar and serum procalcitonin: diagnostic and prognostic value in ventilator-associated pneumonia. Anesthesiology 2002; 96(1): 74 -79. Liao X, Kang Y. Prognostic value of procalcitonin levels in predicting death for patients with ventilator-associated pneumonia. Intensive Care Med 2010; 36: S 102. Zhou et al. Diagnostic value of procalcitonin in ventilator associated pneumonia. [Chinese]. Chinese Critical Care Medicine 2006; 18(6): 370 -372.
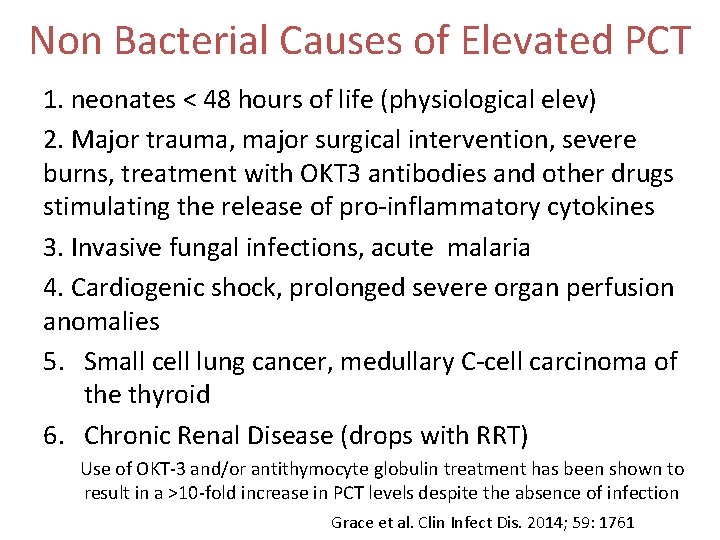
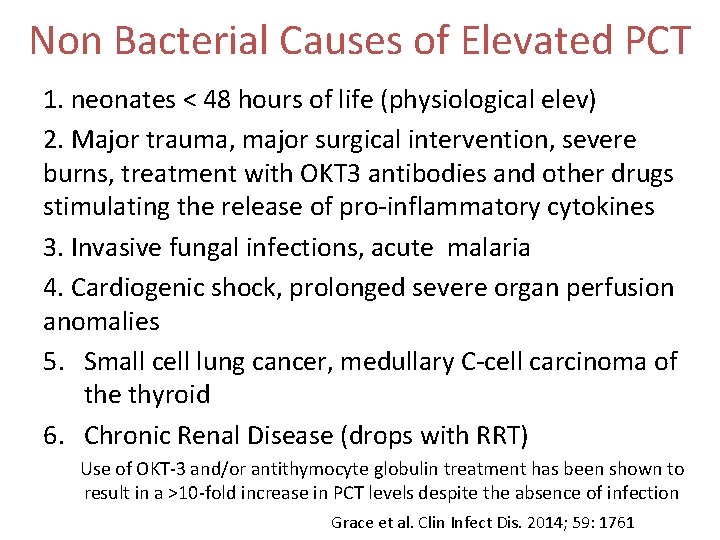
Non Bacterial Causes of Elevated PCT 1. neonates < 48 hours of life (physiological elev) 2. Major trauma, major surgical intervention, severe burns, treatment with OKT 3 antibodies and other drugs stimulating the release of pro-inflammatory cytokines 3. Invasive fungal infections, acute malaria 4. Cardiogenic shock, prolonged severe organ perfusion anomalies 5. Small cell lung cancer, medullary C-cell carcinoma of the thyroid 6. Chronic Renal Disease (drops with RRT) Use of OKT-3 and/or antithymocyte globulin treatment has been shown to result in a >10 -fold increase in PCT levels despite the absence of infection Grace et al. Clin Infect Dis. 2014; 59: 1761
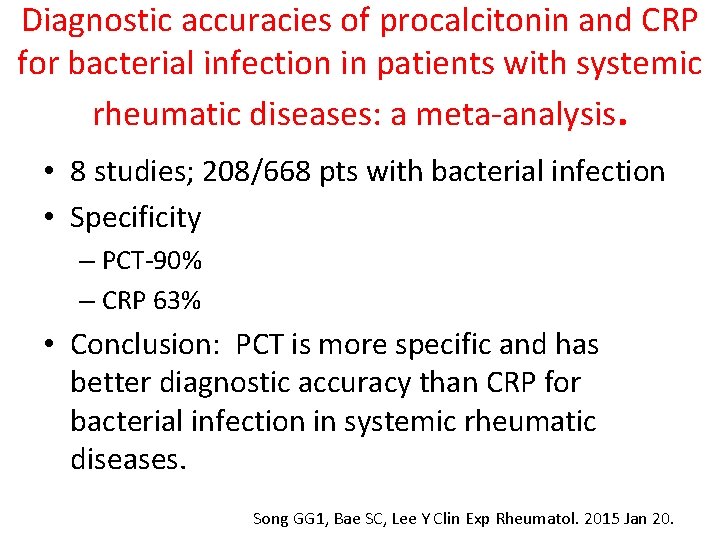
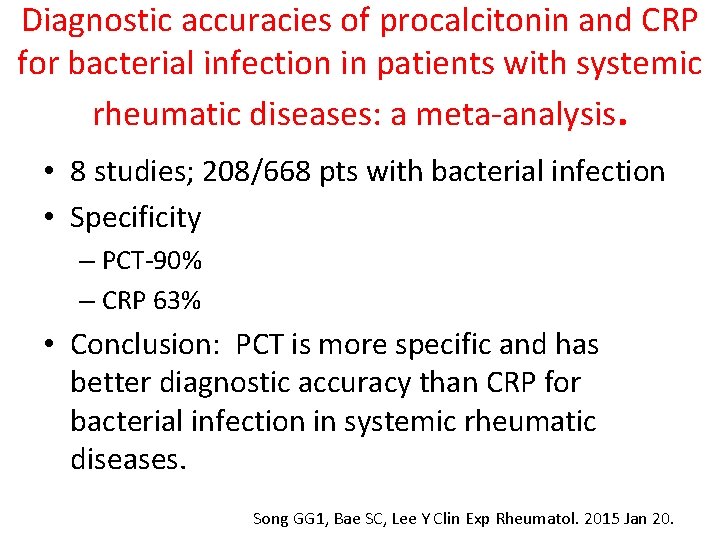
Diagnostic accuracies of procalcitonin and CRP for bacterial infection in patients with systemic rheumatic diseases: a meta-analysis. • 8 studies; 208/668 pts with bacterial infection • Specificity – PCT-90% – CRP 63% • Conclusion: PCT is more specific and has better diagnostic accuracy than CRP for bacterial infection in systemic rheumatic diseases. Song GG 1, Bae SC, Lee Y Clin Exp Rheumatol. 2015 Jan 20.
Procalcitonin: Approved Indication • “intended for use in conjuction with other laboratory findings and clinical assessments to aid in the risk assessment for critically ill patients on their first day of ICU admission, for progression to severe sepsis and septic shock” • FDA cleared assays: – BRAHMS PCT (BRAHMS Aktiengelsellschaft) – VIDAS BRAHMS PCT (bio. Merieux, Inc. ) – BRAHMS PCT KRYPTOR (BRAHMS Aktiengelsellschaft)
Surviving Sepsis Guideline • We suggest the use of low procalcitonin levels or similar biomarkers to assist the clinician in the discontinuation of empiric antibiotics in patients who appeared septic, but have no subsequent evidence of infection (Grade 2 C). Crit Care Med 2013; 41: 580 -637
Antibiotic consumption after implementation of a procalcitonin-guided antimicrobial stewardship programme in surgical ICU patients • Retrospective, Observational 2422 pts • ASP with PCT protocol • Results: – ABX use decrease by 21. 2% – Use of aminogly, Ceph, Quinolones with marked reduction; no change Penicillins – No relevant change mortality, ICU LOS, hospital mortality Hohn et al. Infection. 2015 Jan 15. [Epub ahead of print]
• Observational, historical control to assess impact of PCT in ICU • 50 patients with PCT at initial suspicion of infection and 48 hrs • 50 Control pts--same time frame, diagnosis, gendr, age, APACHE II • Active ASP in place • Findings: • Duration of ABX decreased by 3. 3 days (p=0. 0238) • Duration in hospital decreased by 4. 3 days (p=0. 029) • Readmission to hospital decreased by 16% (p=0. 055) • Mortality 2% vs 4% (p=0. 5)
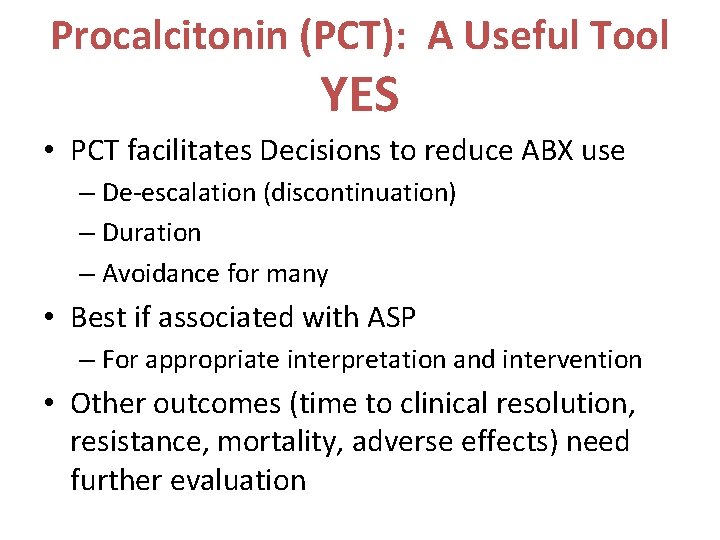
Implementation of a Procalcitonin Assay Requires Appropriate Stewardship to Result in Improved Antimicrobial Use • No systematic education provided to practitioners before introduction of the test: • ICU study at VA found a suboptimal result of antimicrobial discontinuation or de-escalation on the basis of a low PCT Ramanthan et al. Evaluation of procalcitonin use for bacterial infections at a VA Medical Center. ICAAC 2014
“An antimicrobial stewardship team that reviews rapid diagnostic testing results (ie, molecular diagnositc tests, PCT) and provides feedback to providers can help clinicians understand act upon these results. Without this oversight, there may be little change in behavior of practitioners. Procalcitonin does not replace clinical judgment but can be a valuable tool” 7 Inf Dis Clin Pract. 2015; 23: 1
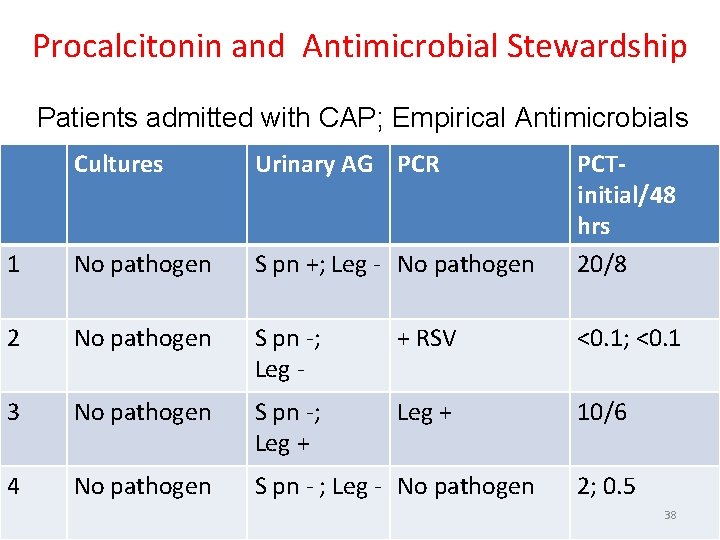
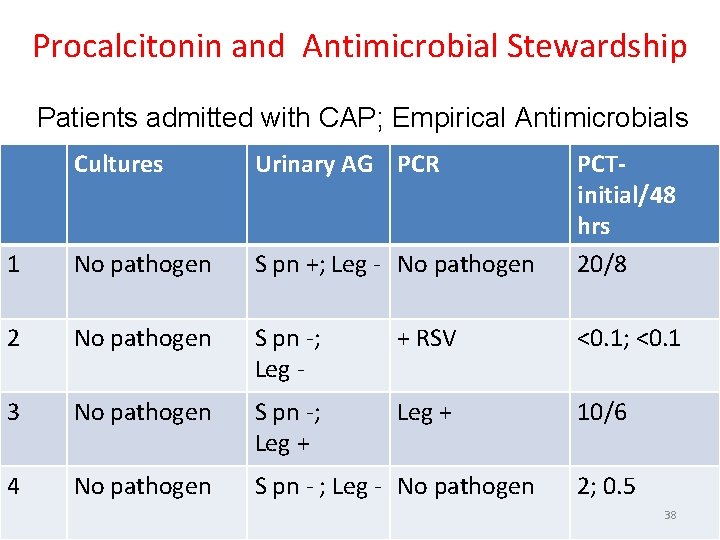
Procalcitonin and Antimicrobial Stewardship Patients admitted with CAP; Empirical Antimicrobials Cultures Urinary AG PCR PCTinitial/48 hrs 20/8 1 No pathogen S pn +; Leg - No pathogen 2 No pathogen S pn -; Leg - + RSV <0. 1; <0. 1 3 No pathogen S pn -; Leg + 10/6 4 No pathogen S pn - ; Leg - No pathogen 2; 0. 5 38
Procalcitonin (PCT): A Useful Tool YES • PCT facilitates Decisions to reduce ABX use – De-escalation (discontinuation) – Duration – Avoidance for many • Best if associated with ASP – For appropriate interpretation and intervention • Other outcomes (time to clinical resolution, resistance, mortality, adverse effects) need further evaluation