Postterm pregnancy pregnancies that last longer than 42


- Slides: 36

Postterm pregnancy: pregnancies that last longer than 42 weeks. Postdate pregnancies: pregnancies that last longer than the estimated date of confinement, (ie, 40 wk). ABOUBAKR ELNASHAR
ABOUBAKR ELNASHAR
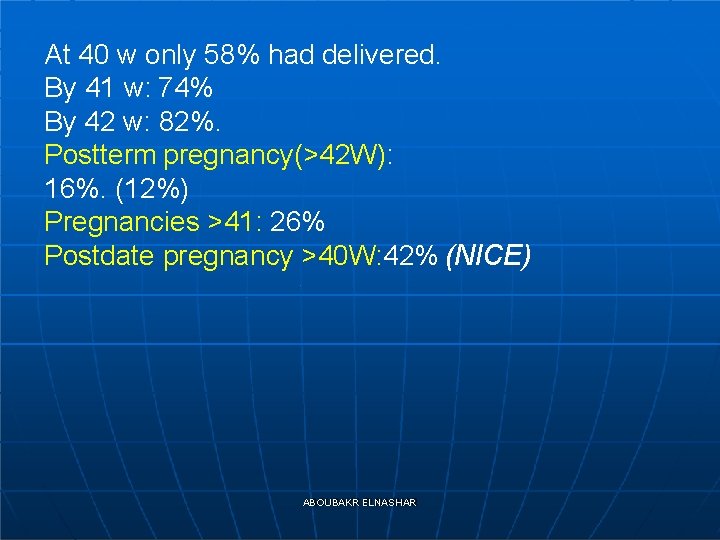
At 40 w only 58% had delivered. By 41 w: 74% By 42 w: 82%. Postterm pregnancy(>42 W): 16%. (12%) Pregnancies >41: 26% Postdate pregnancy >40 W: 42% (NICE) ABOUBAKR ELNASHAR
ABOUBAKR ELNASHAR
Both postterm and postdate pregnancy is inaccurate dating criteria. Ultrasound dating is inaccurate for a patient who presents late in pregnancy An ultrasound before 20 w reduces the need for induction for post term pregnancy (NICE, A) ABOUBAKR ELNASHAR
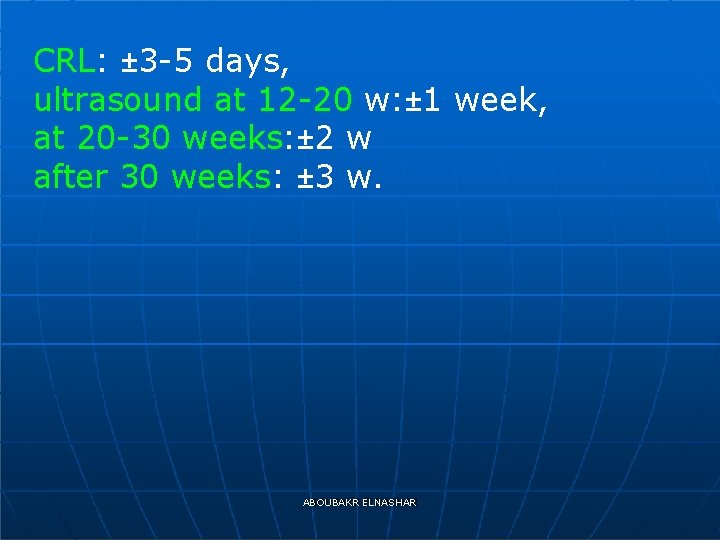
CRL: ± 3 -5 days, ultrasound at 12 -20 w: ± 1 week, at 20 -30 weeks: ± 2 w after 30 weeks: ± 3 w. ABOUBAKR ELNASHAR
ABOUBAKR ELNASHAR
ABOUBAKR ELNASHAR
• In high risk pregnancy • nonreassuring surveillance, • oligohydramnios, • growth restriction, • certain maternal diseases, The risks of remaining pregnant outweigh the risks of delivery ABOUBAKR ELNASHAR
Diabetes in pregnancy fivefold increase in perinatal mortality rate: induction of labour prior to their estimated date for delivery. (NICE C) ABOUBAKR ELNASHAR
B. In the low-risk pregnancy. • The certainty of gestational age, • cervical examination findings, • estimated fetal weight, and • past obstetrical history • Involving the patient in this discussion ABOUBAKR ELNASHAR
Inducing labor at 41 weeks’ gestation in an accurately dated, low-risk pregnancy, regardless of cervical examination findings. 1. Averts the need for antepartum fetal surveillance and 2. does not increase the cesarean delivery rate; in fact, it may decrease the cesarean delivery rate. ABOUBAKR ELNASHAR
3. Perinatal morbidity and mortality do not increase appreciably between 40 -41 weeks of gestation; 4. Several complications are associated with postterm pregnanciesa. ABOUBAKR ELNASHAR
a. macrosomia, shoulder dystocia, and cephalopelvic disproportion b. perinatal mortality increases c. risk of stillbirth increases from ABOUBAKR ELNASHAR
5. increasing the risk for cesarean delivery with a failed induction is far less likely in the era of safe and effective cervical ripening agents. ABOUBAKR ELNASHAR
In summary, routine induction at 41 weeks’ gestation does not increase the cesarean delivery rate, and may decrease it, without negatively affecting perinatal morbidity or mortality. In fact, there may be both maternal and neonatal benefits to a policy of routine induction of labor in well-dated low-risk pregnancies at 41 weeks’ gestation. ABOUBAKR ELNASHAR
From 40 weeks women who decline induction of labour should be offered increased antenatal monitoring consisting of a twice weekly CTG and ultrasound estimation of maximum amniotic pool depth. (NICE A) A modified biophysical profile consisting of a nonstress test and an amniotic fluid index have been shown to be as sensitive as a full biophysical profile. ABOUBAKR ELNASHAR
1. An amniotic fluid index of more than 8 cm and 2. a reactive fetal heart rate tracing are reassuring. ABOUBAKR ELNASHAR
3. If the tracing remains nonreactive, a full biophysical profile should be performed. These may also be used if the tracing is reactive but shows fetal heart rate decelerations. However, in the pregnancy that is beyond 41 weeks of gestation, the threshold for delivery should be very low. ABOUBAKR ELNASHAR
In summary, the use of a nonstress test and an amniotic fluid index 2 times per week for postterm, not postdate, pregnancies may decrease fetal mortality. In addition, if any indication during antepartum surveillance leads the practitioner to question the intrauterine environment, delivery should be the rule. ABOUBAKR ELNASHAR
ABOUBAKR ELNASHAR
Once the decision to deliver a patient has been made, the route of delivery and the specifics of intrapartum management depend on individual circumstances, ABOUBAKR ELNASHAR
A. chemical 1. prostaglandin E 1 tablets for oral or vaginal use, 2. prostaglandin E 2 gel for intracervical application, and 3. a vaginal insert containing 10 mg of dinoprostone. ABOUBAKR ELNASHAR
Oxytocin compared to prostaglandins for induction of labour Prostaglandins should be used in preference to using oxytocin when induction of labour is undertaken in either nulliparous or multiparous women with intact membranes regardless of their cervical favourability. A Either prostaglandins or oxytocin may be used when induction of labour is undertaken in nulliparous or multiparous women who have ruptured membranes, regardless of cervical status, as they are equally effective. A ABOUBAKR ELNASHAR
Comparison of different regimens of oxytocin administration Oxytocin should not be started for 6 hours following administration of vaginal prostaglandins. C In women with intact membranes amniotomy should be performed where feasible prior to commencement of an infusion of oxytocin. C ABOUBAKR ELNASHAR
B. mechanical. 1. Membrane sweeping or stripping 2. Foley balloon catheters placed in the cervix (Sullivan, 1996), 3. extra-amniotic saline infusions, and 4. laminaria: effective (Guinn, 2000). ABOUBAKR ELNASHAR
. Membrane sweeping Prior to formal induction of labour, women should be offered sweeping of the membranes. A -is not associated with an increase in maternal or neonatal infection. -is associated with increased levels of discomfort during the procedure and bleeding. ABOUBAKR ELNASHAR
EFM Management of complications ABOUBAKR ELNASHAR
Intrapartum fetal monitoring: EFM If the fetal heart rate tracing is equivocal, fetal scalp blood sampling the practitioner cannot find reassurance that the fetus is tolerating labor, cesarean delivery is recommended. ABOUBAKR ELNASHAR
• Management of complications presence of meconium, macrosomia, and fetal intolerance to labor. ABOUBAKR ELNASHAR
A. meconium. {increased uteroplacental insufficiency, which leads to hypoxia in labor 2. suctioning of the oropharynx and nose upon delivery of the head ABOUBAKR ELNASHAR
B. Fetal macrosomia can lead to maternal and fetal birth trauma and to arrest of both firstand second-stage labor. Recognizing the limitations of ultrasound at term, it is still advisable to obtain 1. an estimated fetal weight prior to induction of the postdate pregnancy. 2. mid-pelvic instrument deliveries should not be attempted. 3. delivery plan is being prepared for shoulder dystocia ABOUBAKR ELNASHAR
C. uterine hypercontractility with a suspicious or pathological cardiotocograph (CTG), secondary to oxytocin infusions, 1. the oxytocin infusion should be decreased or discontinued. B 2. In the presence of abnormal FHR patterns and uterine hypercontractility (not secondary to oxytocin infusion) tocolysis should be considered. A suggested regime is subcutaneous terbutaline 0. 25 milligrams. A ABOUBAKR ELNASHAR
D. suspected or confirmed acute fetal compromise, delivery should be accomplished as soon as possible, taking account of the severity of the FHR abnormality and relevant maternal factors. The accepted standard has been that ideally this should be accomplished within 30 minutes. B ABOUBAKR ELNASHAR

THANK YOU
 Chapter 13 preterm and postterm newborns
Chapter 13 preterm and postterm newborns Spotting in pregnancy
Spotting in pregnancy Maui: making smartphones last longer with code offload
Maui: making smartphones last longer with code offload Maui: making smartphones last longer with code offload
Maui: making smartphones last longer with code offload Matthew 5:30
Matthew 5:30 It always takes longer than you think
It always takes longer than you think A meter is a little longer than a
A meter is a little longer than a One leg is longer than the other
One leg is longer than the other Walmart thất bại ở nhật
Walmart thất bại ở nhật Sau thất bại ở hồ điển triệt
Sau thất bại ở hồ điển triệt Block nhĩ thất cấp 1
Block nhĩ thất cấp 1 Tìm vết của đường thẳng
Tìm vết của đường thẳng Thể thơ truyền thống
Thể thơ truyền thống Tôn thất thuyết là ai
Tôn thất thuyết là ai Hãy nói thật ít để làm được nhiều
Hãy nói thật ít để làm được nhiều Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Gây tê cơ vuông thắt lưng
Gây tê cơ vuông thắt lưng Ngoại tâm thu thất chùm đôi
Ngoại tâm thu thất chùm đôi Numberblock 1 and 2
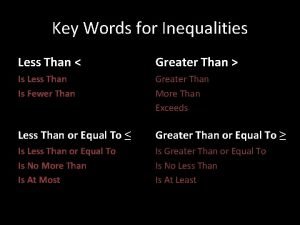
Numberblock 1 and 2 Greater than words
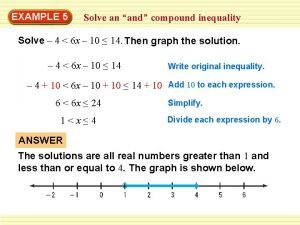
Greater than words Compound inequality examples
Compound inequality examples Er than more than
Er than more than Which is correct
Which is correct 5730x5
5730x5 Percents greater than 100 and less than 1
Percents greater than 100 and less than 1 Jesus lord of heaven
Jesus lord of heaven Greater than god more evil than the devil
Greater than god more evil than the devil Greater than less than fractions
Greater than less than fractions Present continuous past continuous
Present continuous past continuous Which line is longer
Which line is longer Optical illusion
Optical illusion Metanephridia
Metanephridia Colors seen in images made from electron microscopes are
Colors seen in images made from electron microscopes are Winds that blow over longer distances build up bigger
Winds that blow over longer distances build up bigger Why are jekyll and lanyon no longer friends
Why are jekyll and lanyon no longer friends Why do desert animals have longer loop of henle
Why do desert animals have longer loop of henle Dr jekyll and mr hyde quotes
Dr jekyll and mr hyde quotes