POSTTERM PREGNANCY Dr Mona Shroff Dept of OG
- Slides: 11
POST-TERM PREGNANCY Dr. Mona Shroff (Dept. of O&G. SMIMER)
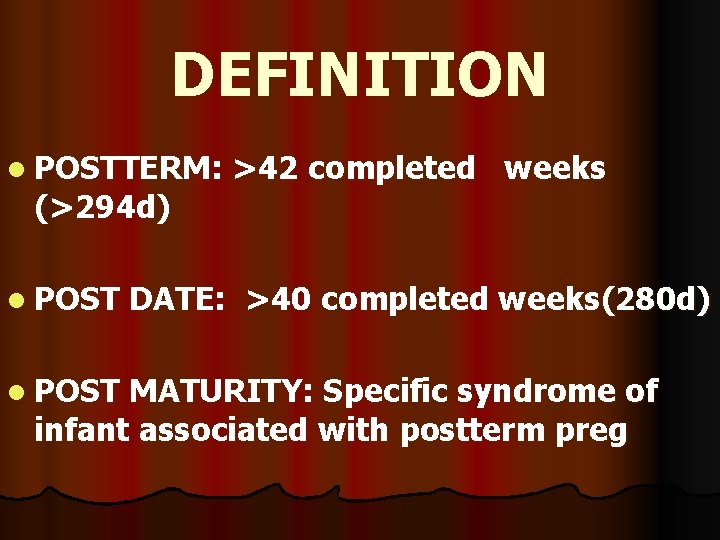
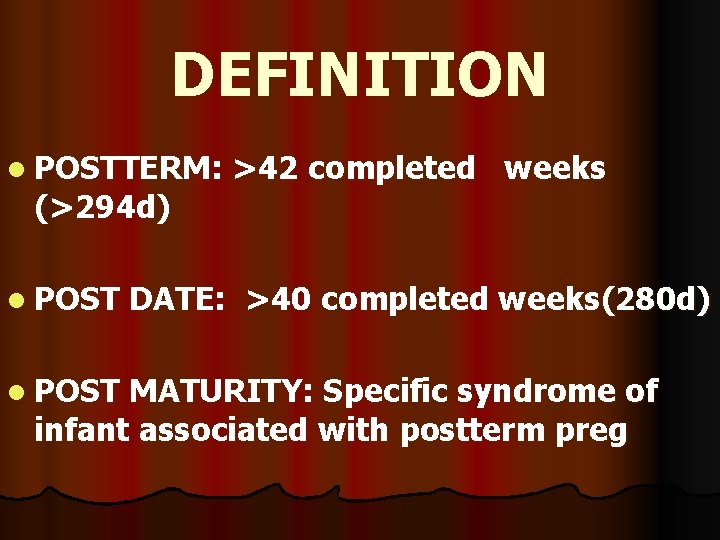
DEFINITION l POSTTERM: (>294 d) l POST >42 completed weeks DATE: >40 completed weeks(280 d) MATURITY: Specific syndrome of infant associated with postterm preg
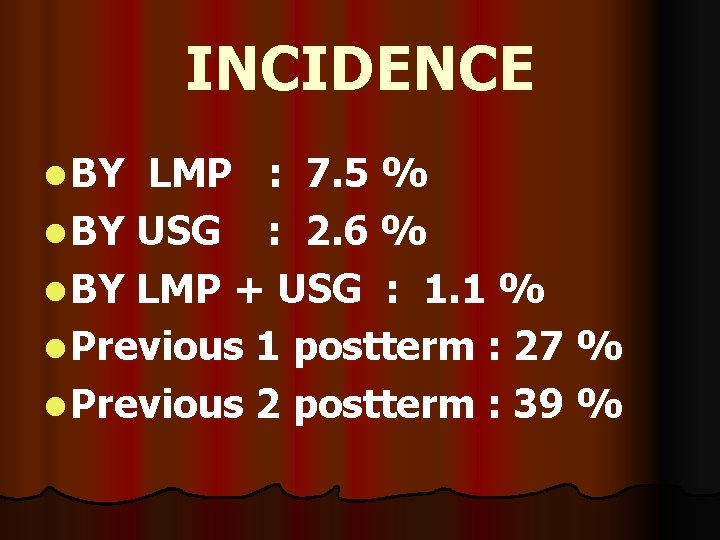
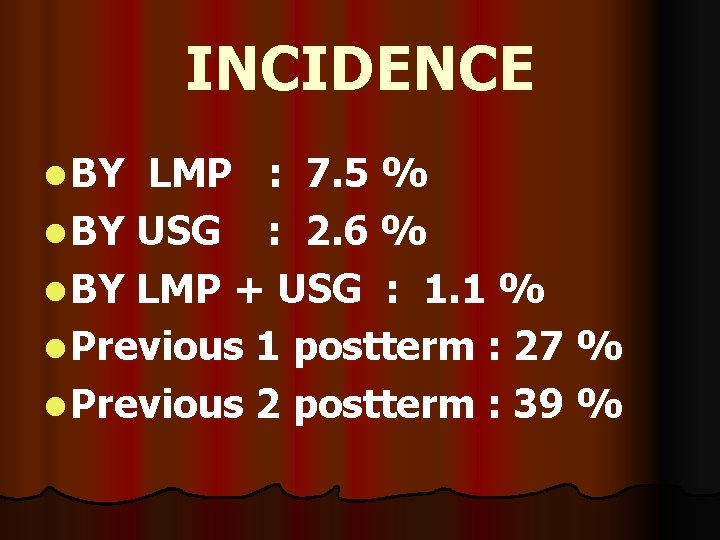
INCIDENCE l BY LMP : 7. 5 % l BY USG : 2. 6 % l BY LMP + USG : 1. 1 % l Previous 1 postterm : 27 % l Previous 2 postterm : 39 %
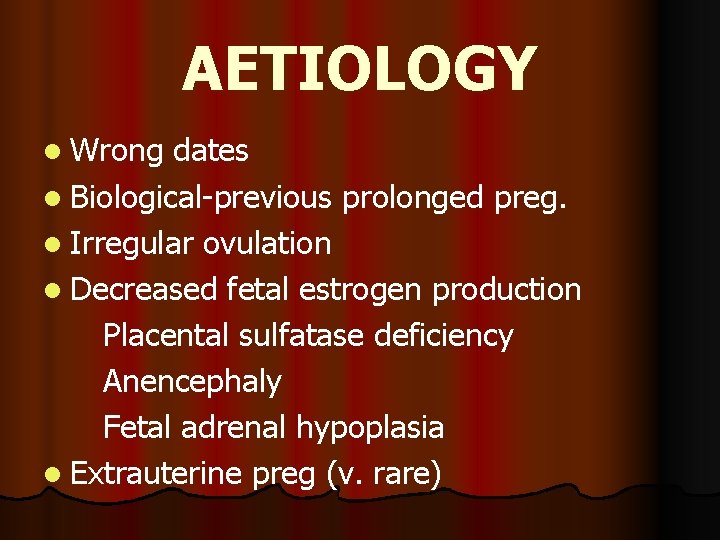
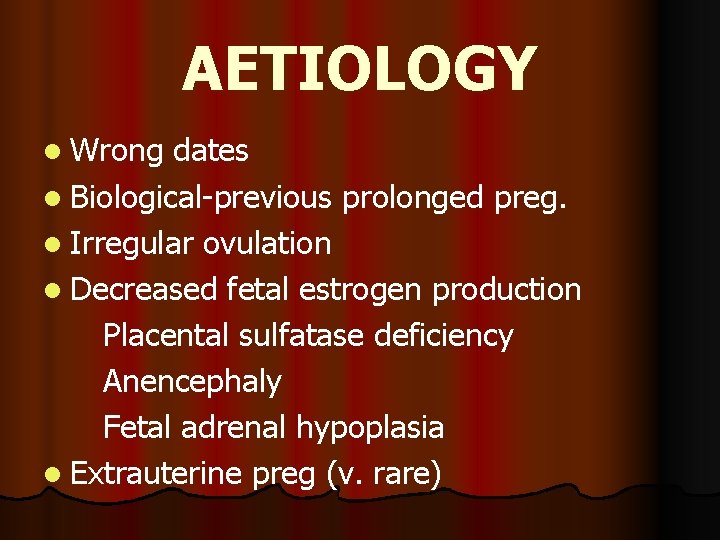
AETIOLOGY l Wrong dates l Biological-previous prolonged preg. l Irregular ovulation l Decreased fetal estrogen production Placental sulfatase deficiency Anencephaly Fetal adrenal hypoplasia l Extrauterine preg (v. rare)
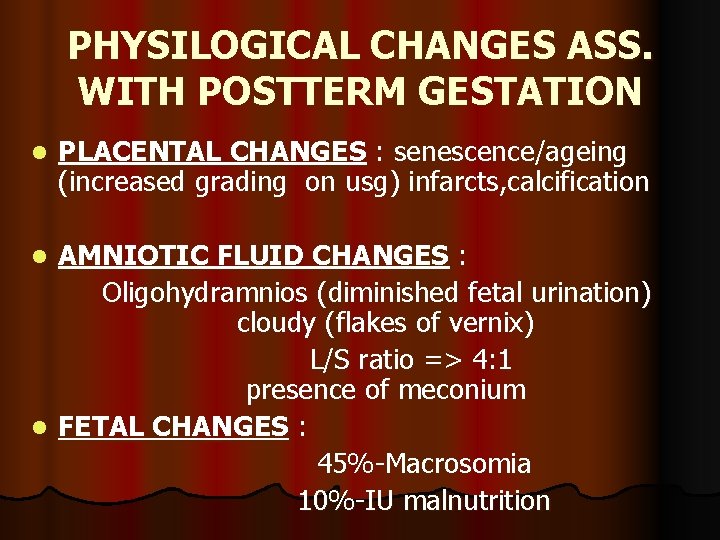
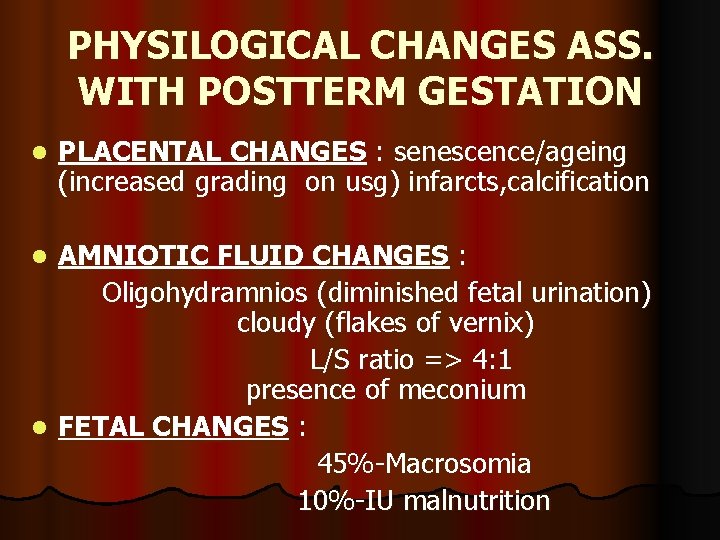
PHYSILOGICAL CHANGES ASS. WITH POSTTERM GESTATION l PLACENTAL CHANGES : senescence/ageing (increased grading on usg) infarcts, calcification AMNIOTIC FLUID CHANGES : Oligohydramnios (diminished fetal urination) cloudy (flakes of vernix) L/S ratio => 4: 1 presence of meconium l FETAL CHANGES : 45%-Macrosomia 10%-IU malnutrition l
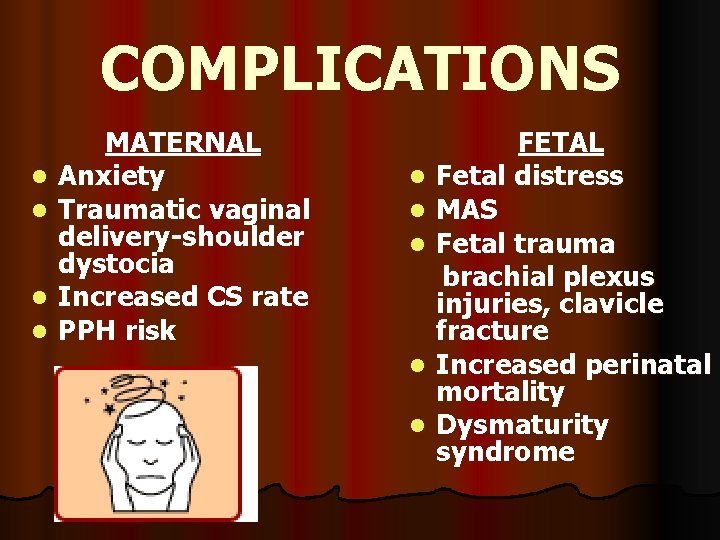
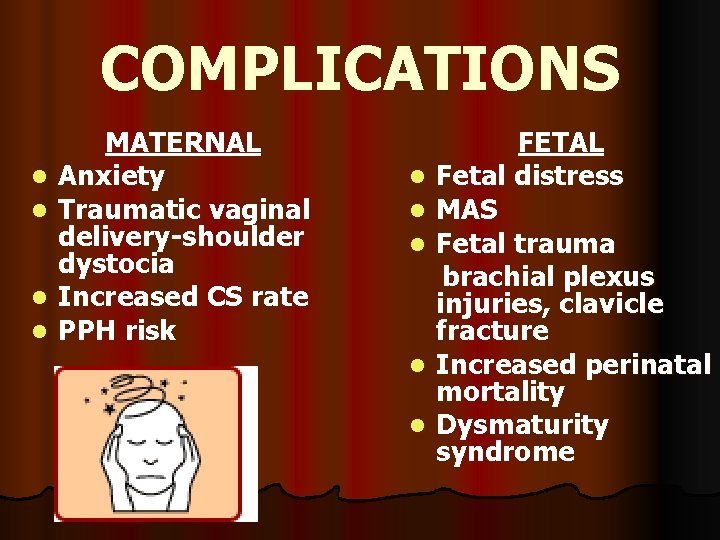
COMPLICATIONS l l MATERNAL Anxiety Traumatic vaginal delivery-shoulder dystocia Increased CS rate PPH risk l l l FETAL Fetal distress MAS Fetal trauma brachial plexus injuries, clavicle fracture Increased perinatal mortality Dysmaturity syndrome
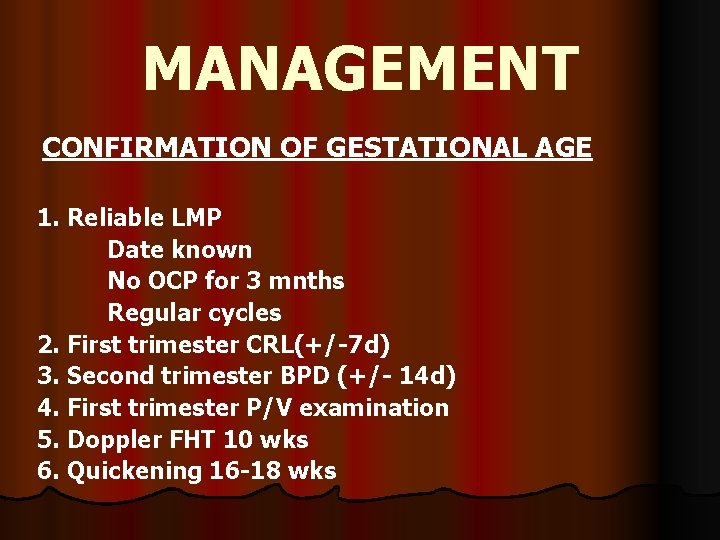
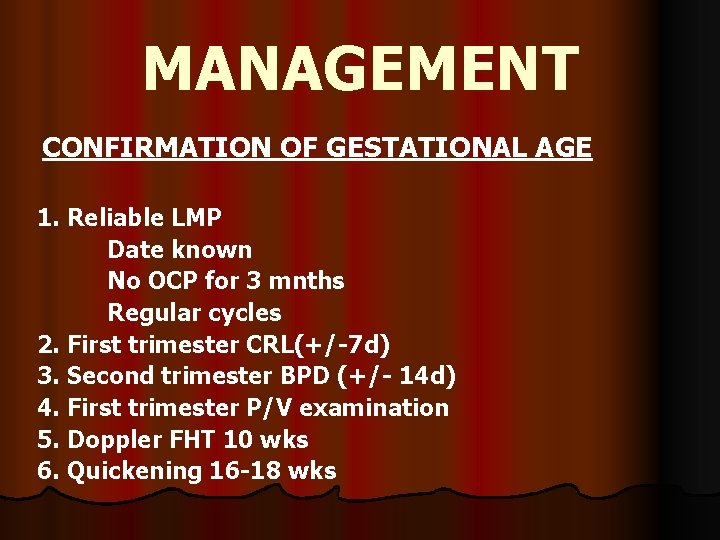
MANAGEMENT CONFIRMATION OF GESTATIONAL AGE 1. Reliable LMP Date known No OCP for 3 mnths Regular cycles 2. First trimester CRL(+/-7 d) 3. Second trimester BPD (+/- 14 d) 4. First trimester P/V examination 5. Doppler FHT 10 wks 6. Quickening 16 -18 wks
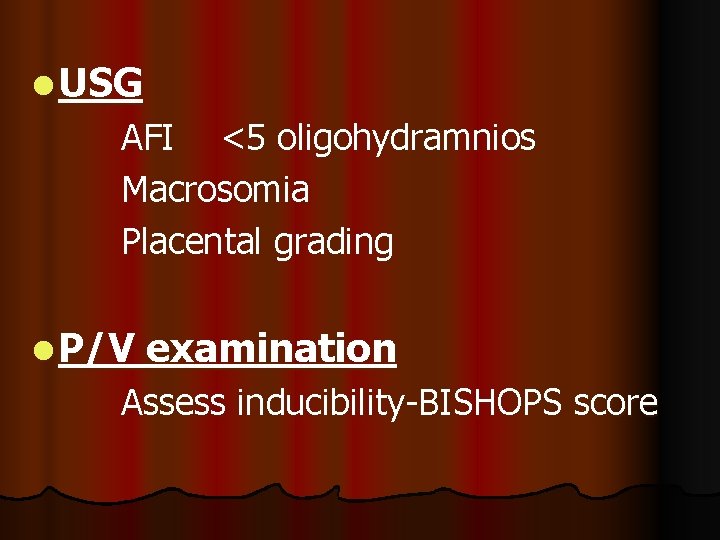
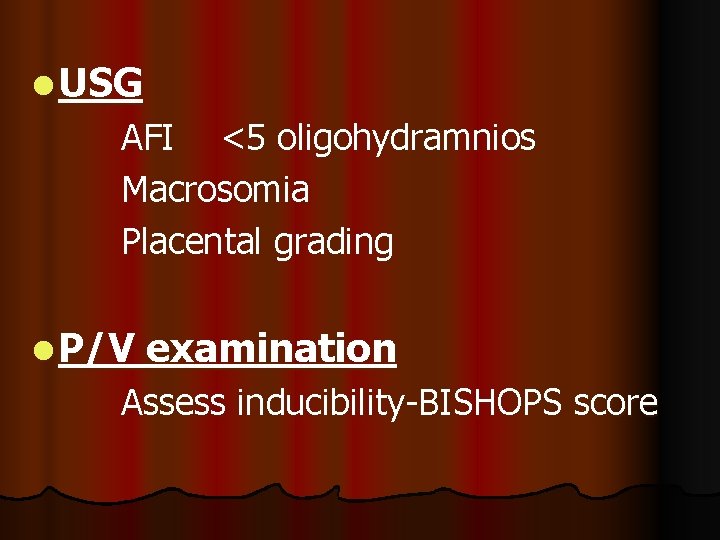
l USG AFI <5 oligohydramnios Macrosomia Placental grading l P/V examination Assess inducibility-BISHOPS score
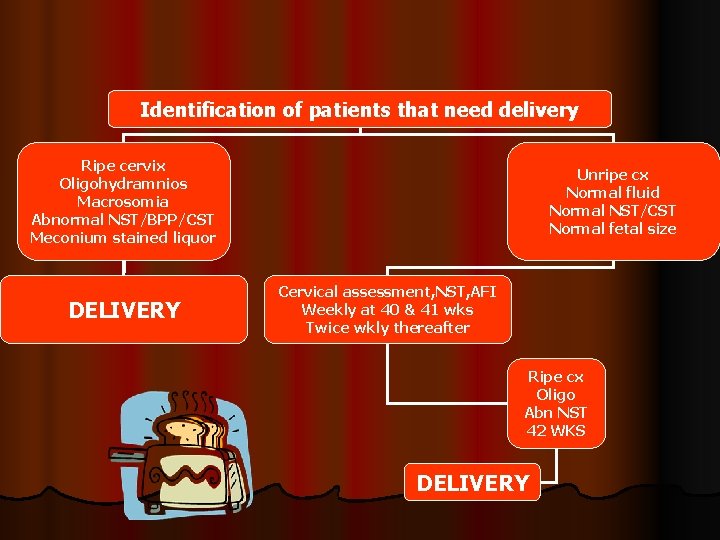
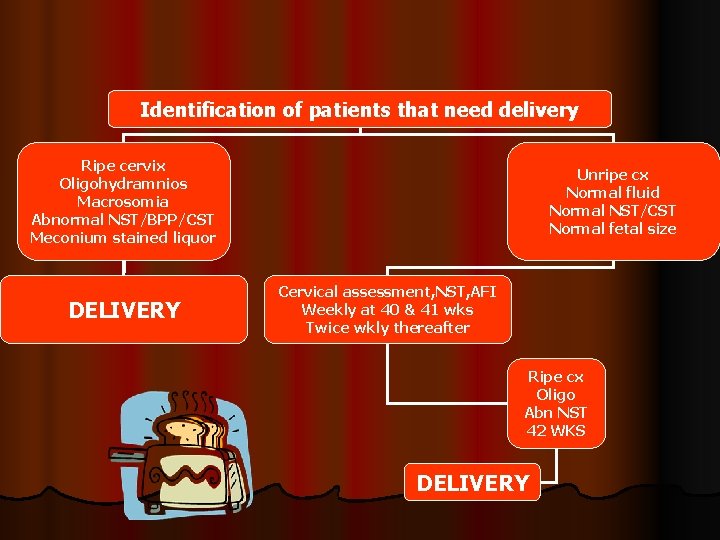
Identification of patients that need delivery Ripe cervix Oligohydramnios Macrosomia Abnormal NST/BPP/CST Meconium stained liquor DELIVERY Unripe cx Normal fluid Normal NST/CST Normal fetal size Cervical assessment, NST, AFI Weekly at 40 & 41 wks Twice wkly thereafter Ripe cx Oligo Abn NST 42 WKS DELIVERY
INTRAPARTUM MANAGEMENT l Left lateral position l Continuous electronic fetal monitoring l Early ARM in active phase (hastens progress, detects meconium) l LSCS if CPD/macrosomia, fetal distress l Amnioinfusion (750 -1000 ml NS/RL) –If meconium stained liquor, variable deccelerations l Paediatrician called at delivery
PREVENTION Sweeping/stripping of membranes at term if no vaginitis, malpresentation or placenta praevia
 Chapter 13 preterm and postterm newborns
Chapter 13 preterm and postterm newborns Definition of spotting during pregnancy
Definition of spotting during pregnancy Jessica fennelly
Jessica fennelly Gautam shroff tcs
Gautam shroff tcs Rewley house continuing education library
Rewley house continuing education library Dept of finance and administration
Dept of finance and administration Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Gome dept
Gome dept Albany county dept of social services
Albany county dept of social services Vaginal dept
Vaginal dept Dept of education
Dept of education Nys department of homeland security
Nys department of homeland security