Post partum Haemorrhage Assistant Prof Dr Esraa ALMaini










- Slides: 55
Post partum Haemorrhage Assistant Prof. Dr. Esraa AL-Maini
More than 100, 000 maternal deaths worldwide result from obstetric hemorrhage each year American college of obs and Gyn 140. 000 deaths per year or 1 women every 4 minutes
Primary postpartum hemorrhage (PPH) The traditional definition of primary PPH is the loss of 500 ml or more of blood from the genital tract within 24 hours of the birth of a baby. Secondary PPH is defined as abnormal or excessive bleeding from the birth canal between 24 hours and 12 weeks postnatal.
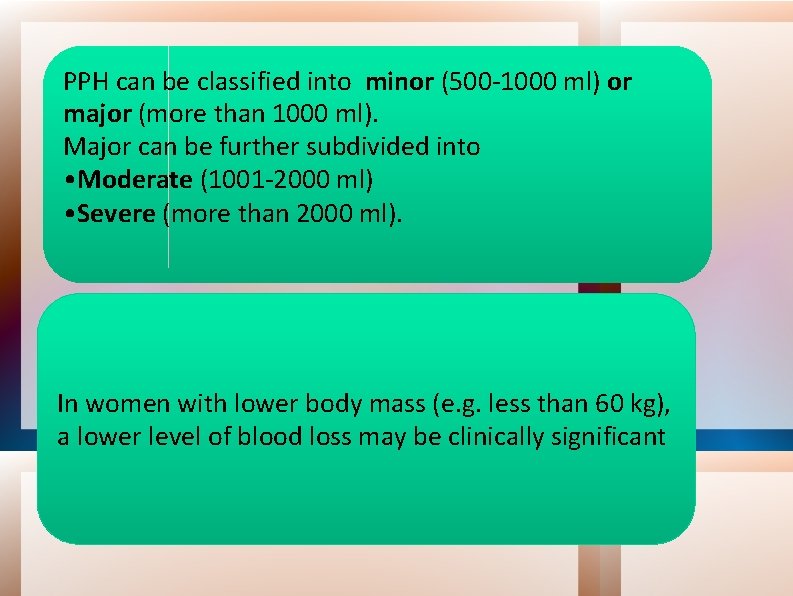
PPH can be classified into minor (500 -1000 ml) or major (more than 1000 ml). Major can be further subdivided into • Moderate (1001 -2000 ml) • Severe (more than 2000 ml). In women with lower body mass (e. g. less than 60 kg), a lower level of blood loss may be clinically significant
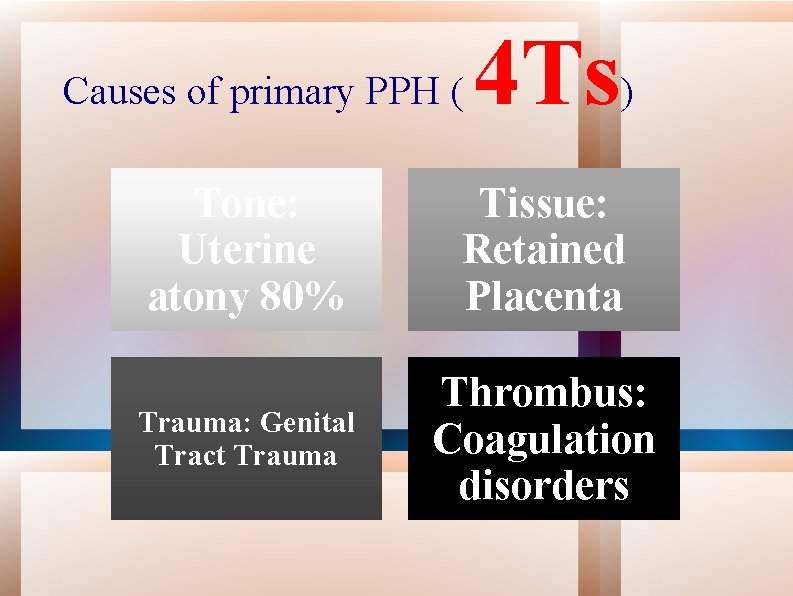
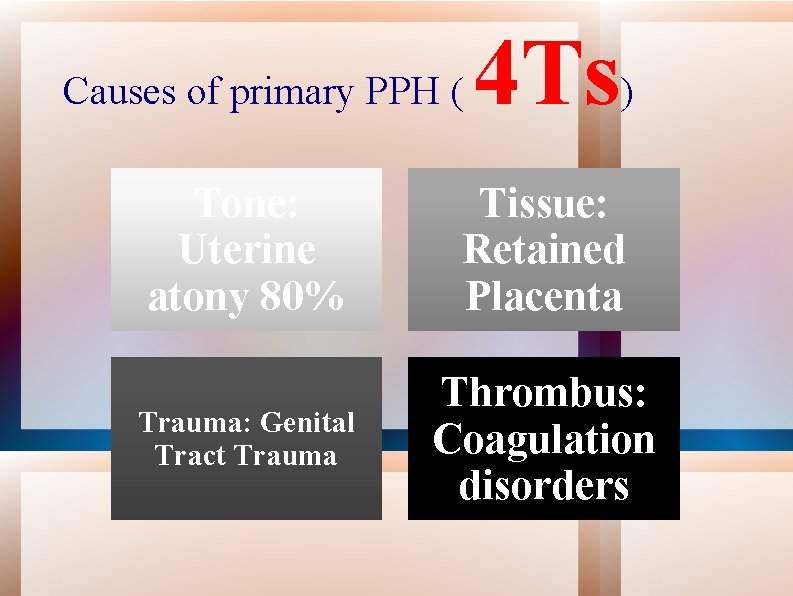
Causes of primary PPH ( 4 Ts) Tone: Uterine atony 80% Tissue: Retained Placenta Trauma: Genital Tract Trauma Thrombus: Coagulation disorders
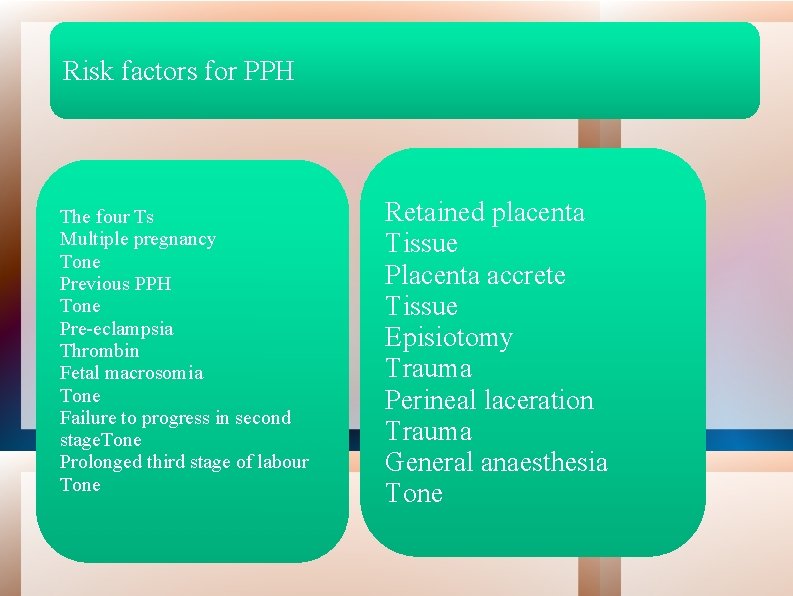
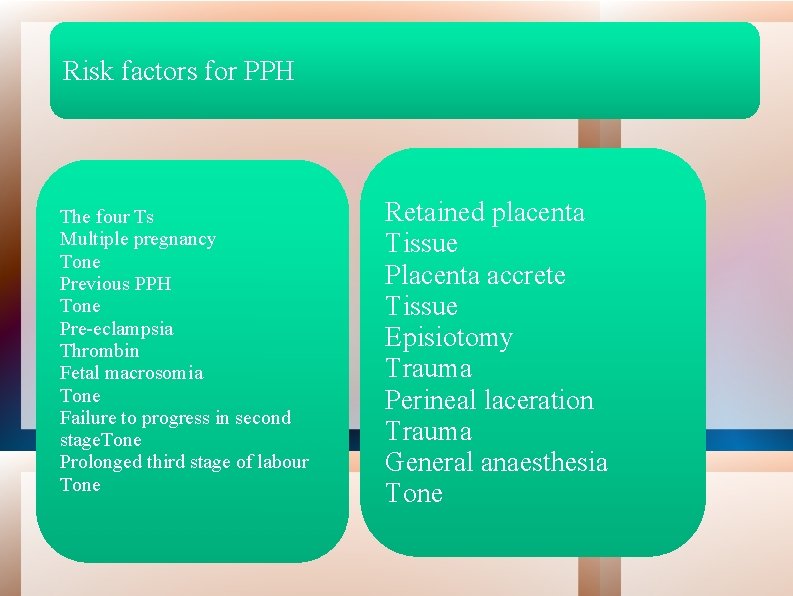
Risk factors for PPH The four Ts Multiple pregnancy Tone Previous PPH Tone Pre-eclampsia Thrombin Fetal macrosomia Tone Failure to progress in second stage. Tone Prolonged third stage of labour Tone Retained placenta Tissue Placenta accrete Tissue Episiotomy Trauma Perineal laceration Trauma General anaesthesia Tone
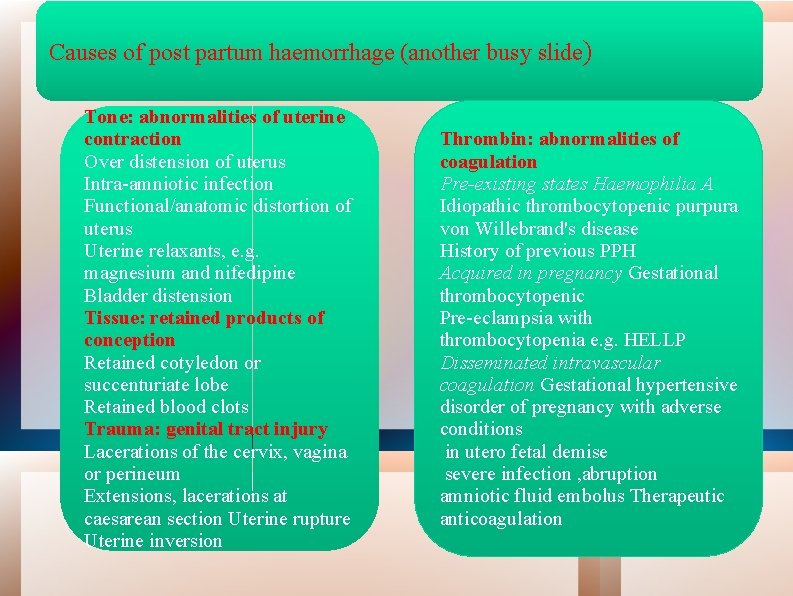
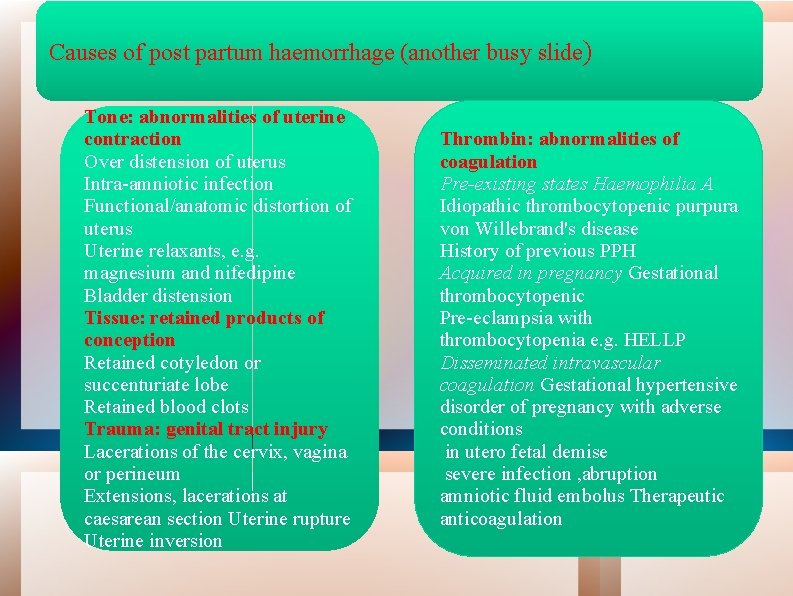
Causes of post partum haemorrhage (another busy slide) Tone: abnormalities of uterine contraction Over distension of uterus Intra-amniotic infection Functional/anatomic distortion of uterus Uterine relaxants, e. g. magnesium and nifedipine Bladder distension Tissue: retained products of conception Retained cotyledon or succenturiate lobe Retained blood clots Trauma: genital tract injury Lacerations of the cervix, vagina or perineum Extensions, lacerations at caesarean section Uterine rupture Uterine inversion Thrombin: abnormalities of coagulation Pre-existing states Haemophilia A Idiopathic thrombocytopenic purpura von Willebrand's disease History of previous PPH Acquired in pregnancy Gestational thrombocytopenic Pre-eclampsia with thrombocytopenia e. g. HELLP Disseminated intravascular coagulation Gestational hypertensive disorder of pregnancy with adverse conditions in utero fetal demise severe infection , abruption amniotic fluid embolus Therapeutic anticoagulation
Prophylactic measures : Women with known risk factors for PPH should only be delivered in a hospital with a blood bank on site Antenatal anaemia should be investigated and treated appropriately as this may reduce the morbidity associated with PPH for pregnancy -( if Hb 11 at first contact and 10. 5 at 28 weeks) should be investigated -
Preparation Postpartum Iron supplementationfor considered if indicated. Hemorrhage -It is recommended that parenteral iron therapy should be considered antenatally for -women with iron deficiency anaemia who do not respond to oral iron. -Antenatal anaemia (Hb less than 9 g/dl) and greater blood loss at delivery and postpartum Minimizing risk – reducing blood loss at delivery -Uterine massage is of no benefit in the prophylaxis of PPH. -Prophylactic uterotonics should be routinely offered in the management of the third stage of labour in all women as they reduce the risk of PPH. .
GOOD NEWS B-Women at low risk for post partum B- Women at increased riskhemorrhage of PPH delivering vaginally, oxytocin (10 iu by intramuscular injection) is the agent of choice for prophylaxis in the third stage of labour. Intramuscular oxytocin should be administered with the birth of the anterior shoulder, or immediately after the birth of the baby and before the cord is clamped and cut. A higher dose of oxytocin is unlikely to be beneficial. For women delivering by caesarean section, oxytocin (5 iu by slow intravenous injection) should be used to encourage contraction of the uterus and to decrease blood loss. Ergometrine-oxytocin versus oxytocin alone not superior only increase the adverse effects of nausea and vomiting, and elevation of blood pressure 5 fold oxytocin is superior to misoprostol in the prevention of PPH. Carbetocin is licensed in the UK specifically for the indication of prevention of PPH in the context of caesarean delivery. Good news WE HAVE THE TOOLS
GOOD NEWS B-Women at increase risk for post risk partum B- Women at increased ofhaemorrhage PPH Ergometrine-oxytocin may be used in the absence of hypertension as it reduces the risk of minor PPH (500 -1000 ml might be superior to syntocinon alone to prevent PPH). Intravenous tranexamic acid(0. 5 -1. 0 g), inaddition to oxytocin, at caesarean section to reduce blood loss in women at increased risk of PPH. , but not vaginal birth. thromboembolic events should be considered. Good news WE HAVE THE TOOLS
Management of PPH Estimated blood loss 1 - The visual estimation of peripartum blood loss is inaccurate , that clinical signs and symptoms should be included in the assessment of PPH. • In pregnancy, pulse and blood pressure are usually maintained in the normal range until blood loss exceeds 1000 ml; • tachycardia, tachypnoea and a slight recordable fall in systolic blood pressure occur with blood loss of 1000 -1500 ml. A systolic blood pressure below 80 mm. Hg, associated with worsening tachycardia, tachypnoea and altered mental state, usually indicates a PPH in excess of 1500 ml.
A multidisciplinary team If major PPH (blood loss of more than 1000 ml) Ongoing bleeding Clinical shock

Measures for minor PPH (blood loss 5001000 ml) without clinical shock: What can done intravenous access (one 14 -gauge cannula) urgent venepuncture (20 ml) for: group and screen full blood count coagulation screen, including fibrinogen pulse, respiratory rate and blood pressure recording every 15 minutes commence warmed crystalloid infusion
Measures for major PPH What can done A and B - assess airway and breathing C - evaluate circulation position the patient flat keep the woman warm using appropriate available measures transfuse blood as soon as possible, if clinically required until blood is available, infuse up to 3. 5 l of warmed clear fluids Hydroxyethyl starch should not be used.
The main therapeutic goals of the management of massive blood loss as maintaining Hb greater than 80 g/l platelet count greater than 50 x 109/l prothrombin time (PT) less than 1. 5 times normal activated partial thromboplastin time (APTT) less than 1. 5 times normal fibrinogen greater than 2 g/l. -CMV-seronegative products should be used to avoid transmission of CMV to the fetus -The UK policy of universal leucocyte depletion substantially reduces the risk of CMV transmission, In an emergency, should be given to avoid delay -CMV-negative blood or platelets are not needed for transfusion during delivery or in the postpartum period. -The routine use of r. FVIIa is not recommended in the management of major PPH unless as part of a clinical trial. -
Full protocol for monitoring and investigation in major PPH (blood loss greater than 1000 ml) and ongoing haemorrhage or clinical shock immediate venepuncture (20 ml) for: cross-match (4 units minimum) full blood count coagulation screen, including fibrinogen renal and liver function for baseline continuous pulse, blood pressure recording and respiratory rate (using oximeter, electrocardiogram and automated blood pressure recording) Foley catheter to monitor urine output two peripheral cannulae, 14 gauge consider arterial line monitoring (once appropriately experienced staff available forinsertion) consider transfer to intensive therapy unitonce the bleeding is controlled or monitoring at high dependency unit on delivery suite, if appropriate documentation of fluid balance, blood products and procedures
Clinicians should be prepared to use a combination of pharmacological, mechanical and surgical methods to arrest PPH. , a sequence of these measures should be instituted in turn until the bleeding stops.
Initial Steps for PPH The simple mechanical and physiological measures of ‘rubbing up the fundus’ Emptying the bladder to stimulate uterine contraction represent first-line management of PPH Administer uterotonic agents Examine lower genital tract for lacerations.
Medications for Uterine Atony E N I OXYTOCIN “The Champ” Cytotec Inexpensive (? ) Effective G R E ” H y T d E M pee “S
OXYTOCIN • . OXYTOCIN “The Champ” oxytocin 5 iu by slow intravenous injection (may have repeat dose if bleeding continue)
METHERGINE Ergometrine 0. 5 mg by slow intravenous or IM Ergometrine OR oxytocin as first-line agents for the treatment of PPH, It seems appropriate to use both agents, although oxytocin is to be preferred initially, especially in women with hypertension or pre-eclampsia. E N I G R E ” H T edy E M pe “S
Prostaglandin F 2 15 -methyl Carboprost 0. 25 mg by intramuscular injection repeated at intervals of not less than 15 minutes to a maximum of eight doses (use with caution in women with asthma) Misoprostol 800 micrograms. Misoprostol by any root took I. 0 -2. 5 hours to increase uterine tone
In summary intravenous bolus of oxytocin should be given slowly in a dose of not more than 5 iu dose may be repeated If bleeding occurs at the time of caesarean section, intramyometrial injection of carboprost may be used (although not licensed). It is also possible to inject intramyometrial carboprost through the abdominal wall in the absence of laparotomy. The recommended dose is 250 micrograms intramuscularly. This may be repeated every 15 minutes to a total dose of 2 mg (eight doses). However, if significant atonic haemorrhage continues after a third dose of carboprost, without significant improvement (i. e. 30 minutes or more after the first dose was given),
The patient should consider transfer to the operating theatre for that oxytocin infusion should be start oxytocin infusion (40 iu in 500 ml isotonic crystalloids at 125 ml/hour) unless fluid restriction is necessary Examination under anaesthesia, with an awareness of the impending need for laparotomy and/or hysterectomy. Surgical interventions should be initiated sooner rather than later.
Anesthesia While general anaesthesia with increased morbidity and mortality when compared with regional anaesthesia , it may be preferable in patients who are haemodynamically unstable or who have a coagulopathy.
Surgical treatments Intrauterine balloon tamponade is an appropriate first-line 'surgical' intervention for control of a tonic PPH Tamponade using various types of hydrostatic balloon catheter has superseded uterine packing (packing not recommended for the control of atonic PPH) Types Foley catheter Bakri balloon, Sengstaken- Blakemore oesophageal catheter Condom catheter The urological Rusch catheter
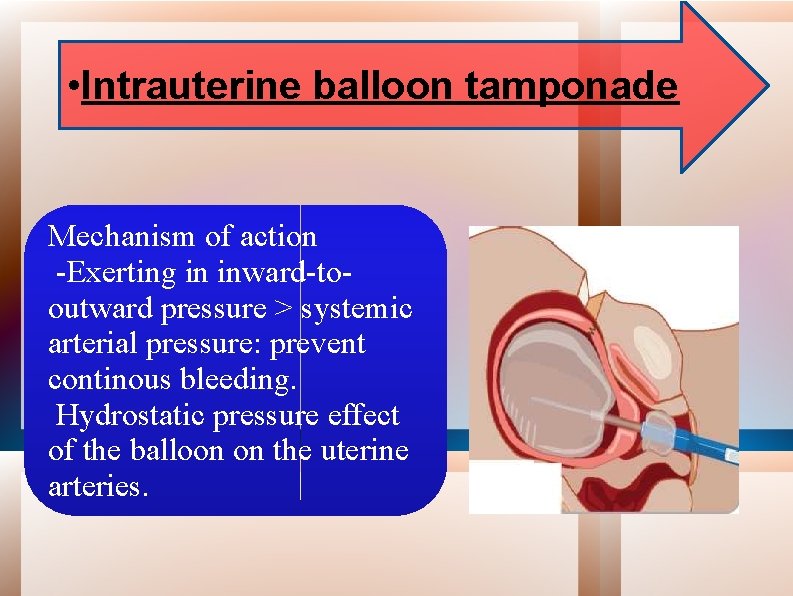
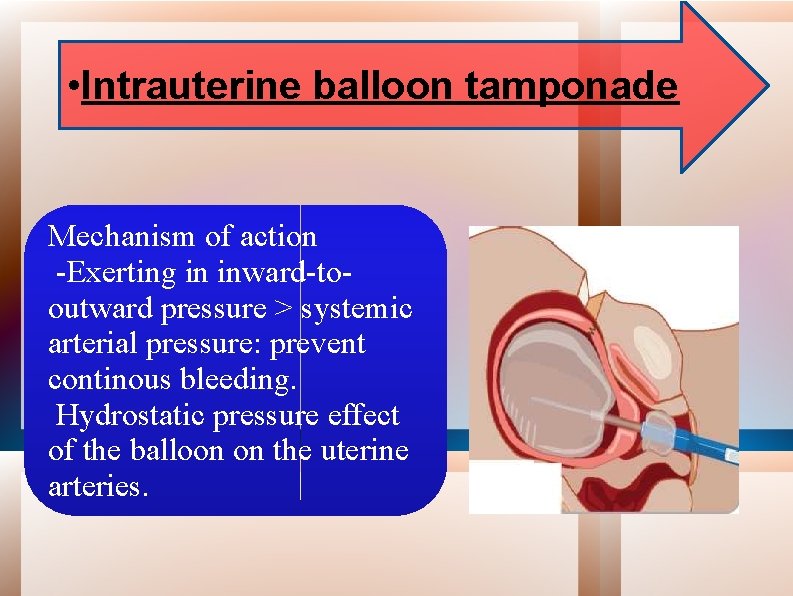
• Intrauterine balloon tamponade Mechanism of action -Exerting in inward-tooutward pressure > systemic arterial pressure: prevent continous bleeding. Hydrostatic pressure effect of the balloon on the uterine arteries.
Positive test(Tamponade Test) A ‘positive test’ (control of PPH following inflation of the balloon) indicates that laparotomy is not required, whereas a ‘negative test’ (continued PPH following inflation of the balloon) is an indication to proceed to laparotomy Method : inserted into uterine cavity balloon inflated 75 -150 ml warm saline. Warm saline speed up coagulation bleeding stop no further surgery needed There is no clear evidence on how long the balloon tamponade should be left in place. In most cases, 4 -6 hours of tamponade should be adequate to achieve and ideally it should be removed during daytime hours, in the presence of appropriate senior staff, in case further intervention is necessary. v papers have removed the balloon within 48 hours
Before its complete removal the blloon could be deflated but left in place to ensure that bleeding does not reoccur. Rate of deflation vary from 20 ml/hour to half the volume in the balloon at 12 hours.
Condom catheters Urinary bladder was kept empty by indwelling Foley's catheter. After putting the patient in the lithotomy position, the condom is inserted within the uterine cavity. Inner end of the catheter remained within the condom. Outer end of the catheter is connected with a saline set and the condom is inflated with 250 -500 m. L of running normal saline. Bleeding is observed, and when it is reduced considerably, further inflation is stopped and the outer end of the catheter is folded and tied with thread. Oxytocin drip for at least 6 h after the procedure. The uterine condom is kept tight in position by ribbon gauze pack or another inflated condom placed in the vagina. The condom catheter is kept for 24 -48 h and then is deflated gradually over (10 -15 m) and removed. Triple antibiotic coverage (amoxicillin [500 mg/6 h] + metronidazole [500 mg/8 h] + gentamicin [80 mg/8 hrs]) for 7 d.

Rusch balloon has been described as preferable by its large capacity, ease of use and low cost successfully avoiding hysterectomy in (9 I%) Rusch balloon and the condom catheter conforming naturally to the contour of the uterus do not allow drainage of the uterine cavity. Insufflation capacity of 1500 ml balloon was inflated with 400 -500 ml of warm saline removed after 24 h following deflation at a rate of 20 ml/h
Balloon tamponade catheter Contours to uterine shape Dual lumen catheter that allows infusion of saline to expand the balloon while providing uterine drainage (provides drainage at the fundus ) to monitor the progression of hemostasis
Multiple urinary Foley catheters inserted together applied to the oozing inner surface of the lower uterine segment The uterine incision site was then closed, and each of the balloonswas inflated with 35 -75 cm 3 of saline or water. Gentle traction was then applied to obtain a continuous tamponade effect, and the vagina was packed. • The catheters were then tied together, and plastic bag was used for the collection and measurement of blood loss prevent blood collection inside the uterine cavity and provide an accurate estimation of bleeding.
Sengstaken-Blakemore tube The Sengstaken-Blakemore two-balloon tube, originally designed for the management of bleeding oesophageal varices, The distal, gastric balloon was filled with 300 ml of normal saline Subsequently, the proximal oesophageal balloon The greater cost of the Sengstaken-Blakemore tube in comparison to the Bakri balloon If insufflated to a large volume so urological Rusch balloon can be used
Bakri ‘SOS’ (Surgical Obstetric Silicone) balloon Capacity: up to 500 ml of saline Drainage channel: large bore Uses: PPH resulting from a low-lying placenta/placenta praevia Under US guidance, the balloon portion of the catheter is inserted into the uterus, making certain that the entire balloon is inserted past the cervical canal and internal ostium
Oxytocin infusion No evidence that an oxytocin infusion is obligatory for all causes of PPH. If the syntocinon is continued for the duration of balloon placement, this can range from 2 to 82 hours. Prolonged: hyponatraemia {cross-reactivity of the oxytocin with antidiuretic hormone receptors. Carbetocin, a synthetic analogue of oxytocin, with a half life of 4 -10 times that of oxytocin is available. There were no significant changes in sodium, potassium or chloride values. Therefore, this may be a preferred drug in the presence of a uterine balloon for prolonged uterine contraction. Although not specifically mentioned, another means of increasing uterine tone is to encourage breastfeeding. However, this may be impractical or declined by the mother .
Antibiotic to reduce the risk of iatrogenic infection • E. g: cephalosporin. • Duration: ± prophylactic (single dose), continued for 24 -48 hours or recommended for the duration of balloon usage Pain relief During insertion: Following a vaginal delivery: No anaesthetic analgesia (pethidine) may be used’. After insertion: no pain relief
Complications: obstruction by uterine leiomyomata inadvertent damage to the balloon during preparation of Sengstaken-Blakemore tube while cutting off the tip • inability to place the balloon due to the presence of a B- Lynch suture insufficient insufflation requiring two balloons. • air emboli if air is used as the distension medium for the balloon. • uterine rupture from uterine overdistension uterine perforation during insertion. pregnancy reported following the use of the Rusch balloon And following the use of a Bakri balloon in combination with a B-Lynch suture.
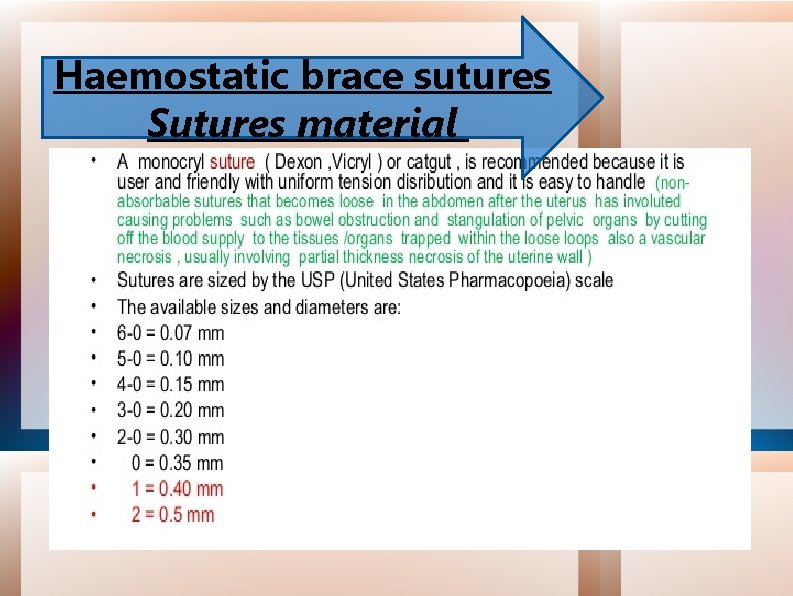
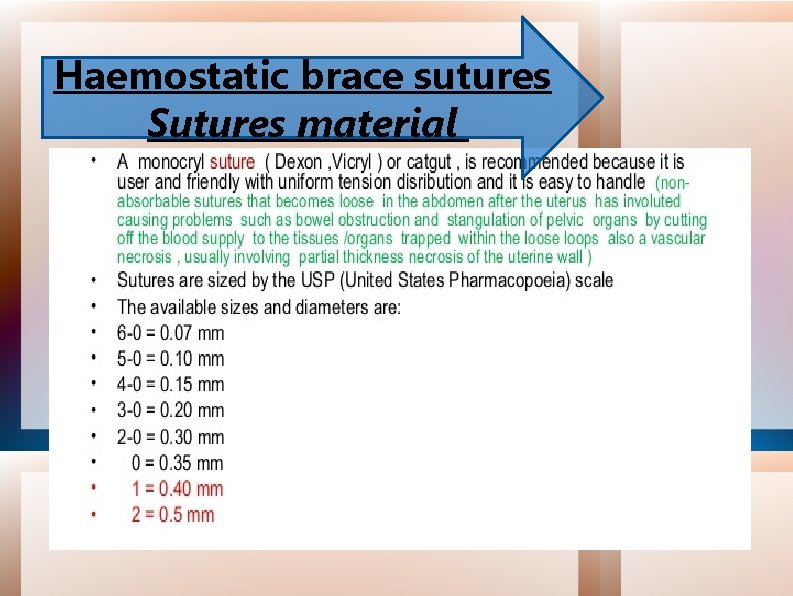
Haemostatic brace sutures Sutures material


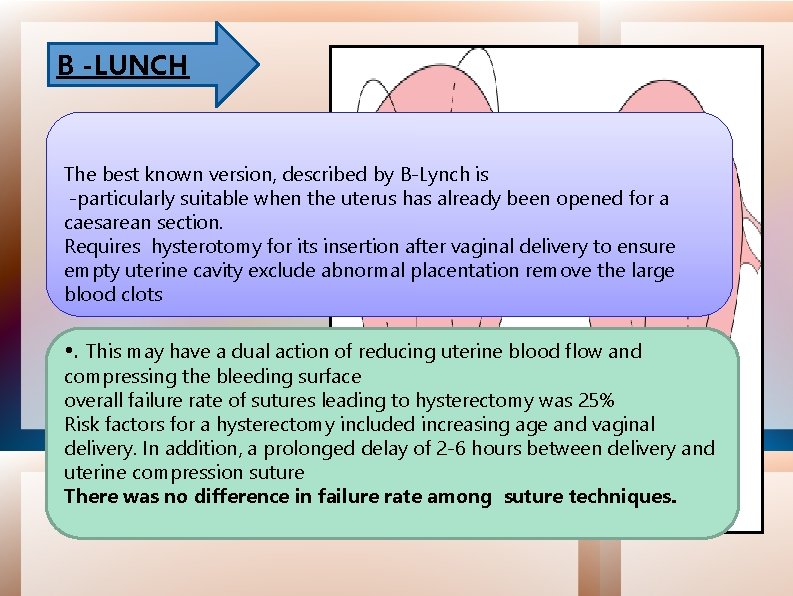
B -LUNCH The best known version, described by B-Lynch is -particularly suitable when the uterus has already been opened for a caesarean section. Requires hysterotomy for its insertion after vaginal delivery to ensure empty uterine cavity exclude abnormal placentation remove the large blood clots • . This may have a dual action of reducing uterine blood flow and compressing the bleeding surface overall failure rate of sutures leading to hysterectomy was 25% Risk factors for a hysterectomy included increasing age and vaginal delivery. In addition, a prolonged delay of 2 -6 hours between delivery and uterine compression suture There was no difference in failure rate among suture techniques.



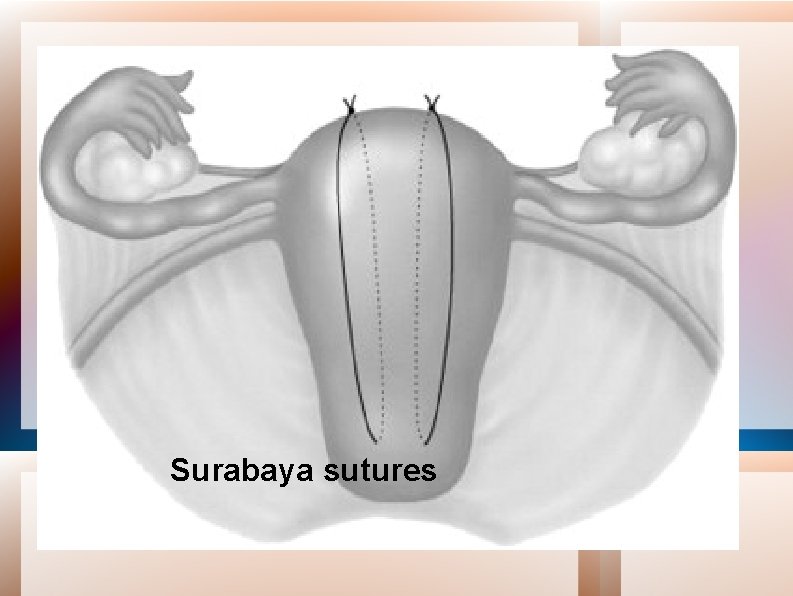
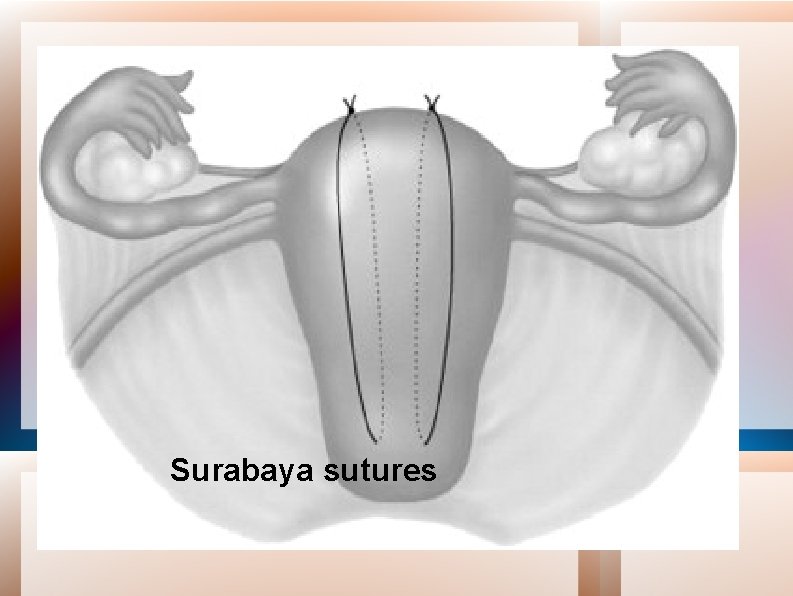
Surabaya sutures
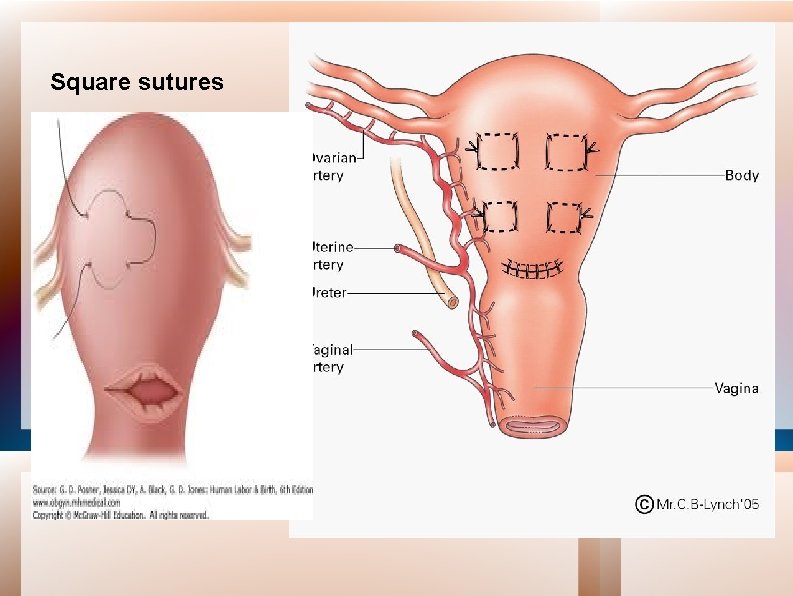
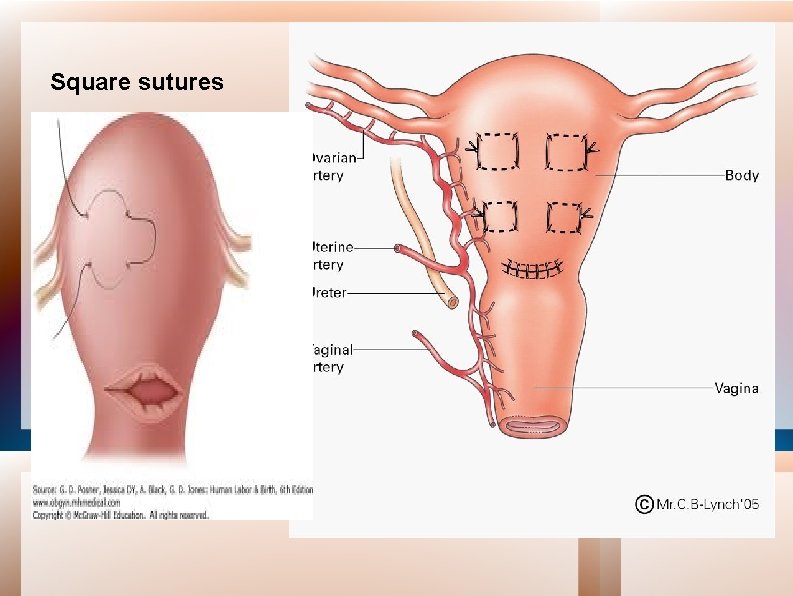
Square sutures

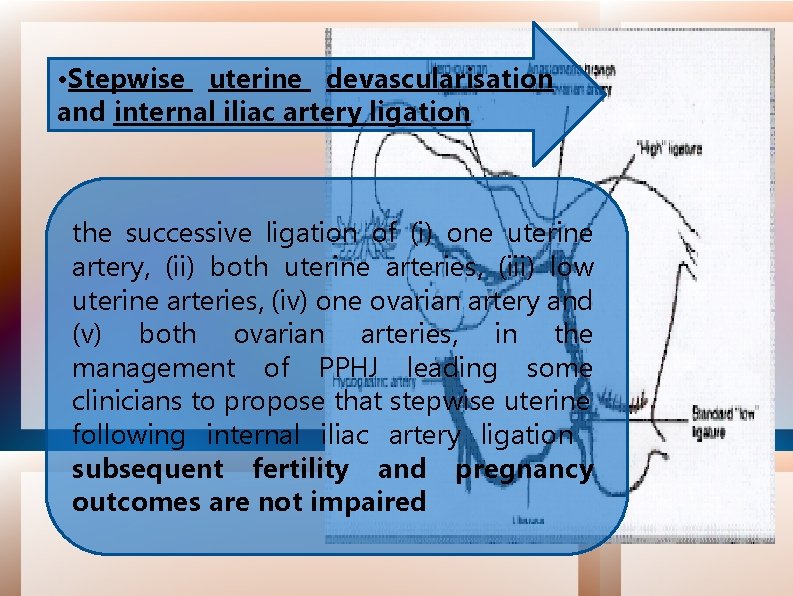
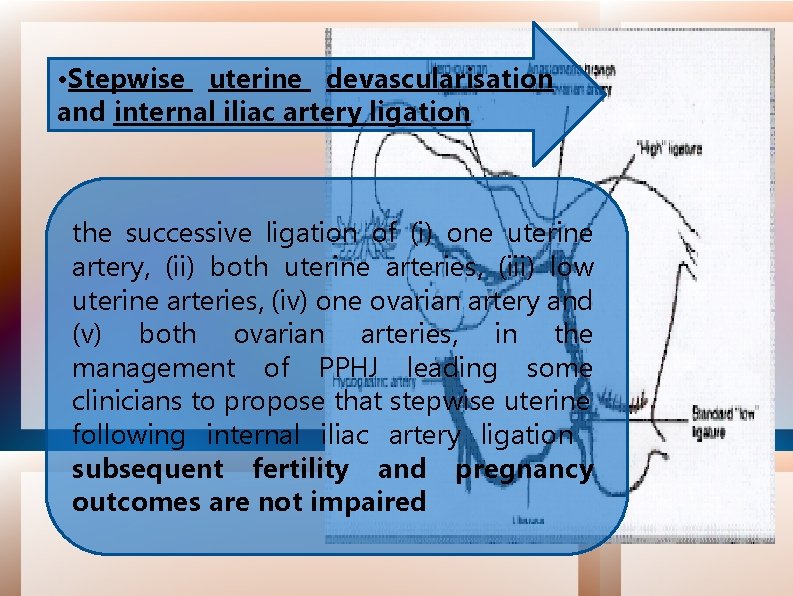
• Stepwise uterine devascularisation and internal iliac artery ligation the successive ligation of (i) one uterine artery, (ii) both uterine arteries, (iii) low uterine arteries, (iv) one ovarian artery and (v) both ovarian arteries, in the management of PPHJ leading some clinicians to propose that stepwise uterine following internal iliac artery ligation subsequent fertility and pregnancy outcomes are not impaired

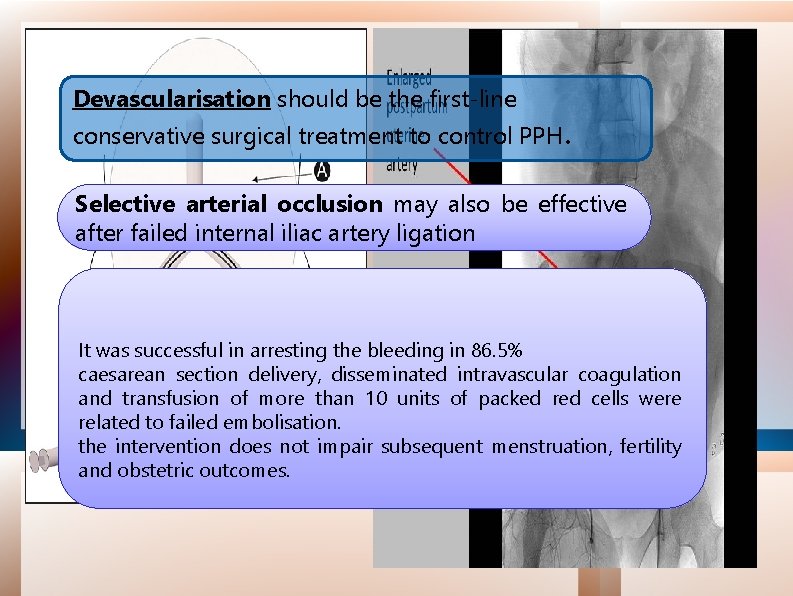
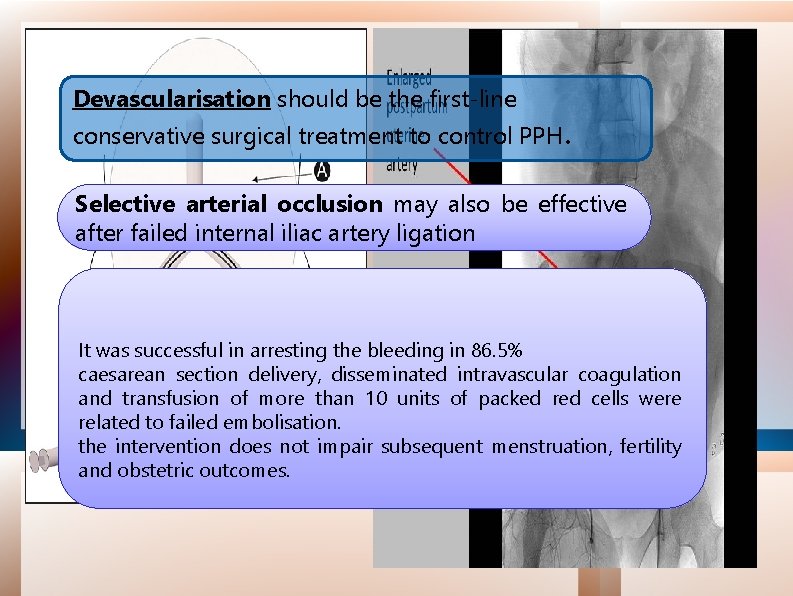
Devascularisation should be the first-line conservative surgical treatment to control PPH. Selective arterial occlusion may also be effective after failed internal iliac artery ligation It was successful in arresting the bleeding in 86. 5% caesarean section delivery, disseminated intravascular coagulation and transfusion of more than 10 units of packed red cells were related to failed embolisation. the intervention does not impair subsequent menstruation, fertility and obstetric outcomes.
Hysterectomy Early recourse to hysterectomy is recommended, especially where bleeding is associated with placenta accreta or uterine rupture . Hysterectomy should not be delayed until the woman is in extremis or while less definitive procedures with which the surgeon has little experience are attempted. Subtotal hysterectomy is the operation of choice in many instances of PPH requiring hysterectomy, unless there is trauma to the cervix or a morbidly adherent placenta in the lower segment.

The 4 “Ts” Recalled “THROMBIN” Check labs if suspicious.
 Hta post partum
Hta post partum Pph management
Pph management Uterine atony causes
Uterine atony causes Hemerriod
Hemerriod Haemorrhage
Haemorrhage Types of haemorrhage
Types of haemorrhage Pathophysiology of haemorrhage
Pathophysiology of haemorrhage Secondary postpartum haemorrhage
Secondary postpartum haemorrhage Haemorrhage
Haemorrhage Nursing care plan for postpartum hemorrhage slideshare
Nursing care plan for postpartum hemorrhage slideshare Ibm support assistant workbench
Ibm support assistant workbench Cisco sbcs
Cisco sbcs Laparoscopische cholecystectomie surgery assistant
Laparoscopische cholecystectomie surgery assistant Wheezing
Wheezing Cisco personal communications assistant
Cisco personal communications assistant Dental assistant
Dental assistant Siri dahl personal assistant
Siri dahl personal assistant Cashflow assistant
Cashflow assistant Good morning madam
Good morning madam Sql server migration assistant for sybase
Sql server migration assistant for sybase Chapter 2 the nursing assistant and the care team
Chapter 2 the nursing assistant and the care team Ibm support assistant workbench
Ibm support assistant workbench Hello good afternoon teacher
Hello good afternoon teacher Medical assistant telephone techniques
Medical assistant telephone techniques Home assistant fan template
Home assistant fan template D-kefs scoring assistant
D-kefs scoring assistant Executive assistant conference 2019
Executive assistant conference 2019 Assistant computer control
Assistant computer control Cisco unified cm assistant console
Cisco unified cm assistant console Role of a teaching assistant
Role of a teaching assistant Assistant
Assistant Assistant director vicky
Assistant director vicky Home assistant fglair
Home assistant fglair Ethical and legal issues affecting the nursing assistant
Ethical and legal issues affecting the nursing assistant What are the duties of assistant scorer?
What are the duties of assistant scorer? Roger lukoff
Roger lukoff Kpu health care assistant
Kpu health care assistant Qcm validation formation assistant maternel
Qcm validation formation assistant maternel Thermometer 97 degrees
Thermometer 97 degrees Comenius assistant
Comenius assistant Porcelain crown charting
Porcelain crown charting Tension moyenne
Tension moyenne Email to professor
Email to professor Anwser
Anwser What are writing conventions
What are writing conventions Manifesto for school head girl
Manifesto for school head girl Medicare assistant
Medicare assistant Bakersfield adults school medical assistant
Bakersfield adults school medical assistant Vms4200
Vms4200 Veternary course
Veternary course The assistant chapter 24
The assistant chapter 24 Promotion from assistant to associate professor
Promotion from assistant to associate professor Shopping conversation
Shopping conversation Akshay kumar assistant
Akshay kumar assistant Assistant secretary for aging
Assistant secretary for aging What is dragon assistant 3
What is dragon assistant 3