Polypharmacy in Older Adults A Learning Module for
- Slides: 38
Polypharmacy in Older Adults A Learning Module for Effective Social Work Practice with Older Adults Dr. Robin P. Bonifas, MSW, Ph. D Arizona State University School of Social Work
Acknowledgements § The development of this curriculum module was made possible through a Gero Innovations Grant from the CSWE Gero-Ed Center's Master's Advanced Curriculum (MAC) Project and the John A. Hartford Foundation.
Overview § § Definitions and demographics § Impact of the aging body on medication metabolism Risks associated with polypharmacy in older adults - adverse drug reactions § Pharmacokinetics § Pharmacodynamics § Potentially inappropriate medications for older adults § Social work interventions to reduce polypharmacy § Promoting medication adherence § The “brown bag”
Contents of this Learning Module Are Based on Materials Originally Developed By: § Advance for Long Term Care Management. Retrieved March 11, 2009 from http: //long-termcare. advanceweb. com/Editorial/Content/Editorial. aspx? CC=120132 § Laird, R. D. Polypharmacy in the Elderly. University of Kansas Medical Center, Center on Aging. Retrieved March 11. 2009 from coa. kumc. edu/GEC/password/Power. Point. Presentations/ Polyphar. ppt § Williams, C. M. (2002). Using medications appropriately in older adults. American Family Physician, 6(10), 1917 -1924.
Polypharmacy in Older Adults: Definitions § Polypharmacy means “many drugs. ” § In practice, polypharmacy refers to the use of more medication than is clinically indicated or warranted. § Polypharmacy can result in a gradual accumulation of side effects and/or adverse drug reactions, which negatively effects elders’ health and well-being.
Polypharmacy in Older Adults: Why is it an Issue? § The elderly use more drugs because illness is more common among the older population. § For example, an older person may have all of the following conditions and have one or more medications prescribed to treat each condition: § Cardiovascular disease § Arthritis § Gastrointestinal disorder § Bladder dysfunction § Depression
Polypharmacy in Older Adults: How Extensive is it? § Older adults comprise 12% of the U. S. population, but use 35% of the prescription medications and 50 percent of the over-the-counter medications. § The average medication usage for persons over 65 is: § 2 to 6 prescription drugs, plus … § 1 to 3. 4 over-the-counter medicines. § In 2006, 58 percent of adults 65 years or older reported taking 5 or more medications and 18% reported taking 10 or more (Slone Epidemiology Center). § The average American senior spends $670 annually for pharmaceuticals.
Polypharmacy in Older Adults: How Extensive is it? § Problems associated with polypharmacy may be increased if older adults take: § Medication dosages that are too high. § Medications that are incorrectly prescribed or filled. § Medications that interact with or duplicate the actions of other medications. § Herbal supplements/remedies that interact with prescription medication.
Polypharmacy in Older Adults: Implications for Social Work § Polypharmacy seems like a concern for doctors, nurses, and pharmacists. Why would social workers care about this issue? § Polypharmacy leads to: § More adverse drug reactions. § Decreased adherence to drug regimens. § Higher rates of disease symptomatology. § (Unnecessary) drug expenses. § All of the above contribute to client distress and poorer quality of life, which are social work concerns!
Polypharmacy in Older Adults: Implications for Social Work § By being knowledgeable about issues related to polypharmacy, social workers can: § Assist multidisciplinary teams in providing better quality of care to older adults. § Serve as more informed advocates for their clients. § Enable clients to effectively advocate for themselves regarding their own medical care. § On that note, let’s look at some of the medical aspects related to polypharmacy so we can better “speak the language” of our multidisciplinary colleagues…
Adverse Drug Reactions § An adverse drug reaction (ADR) is defined as the unwanted, negative consequences associated with the use of a medications or medications. § Over 100, 000 deaths a year are attributed to adverse drug reactions, making ADRs the fourth leading cause of death in the U. S. (Lazarou, Pomeranz, & Corey, 1998). § Other examples of ADRs include: § Peptic ulcers § Anemia § Deceased white blood cell production (which increases infection risk) § Liver damage § Kidney damage § Confusion/drowsiness (which can lead to falls and subsequent injuries)
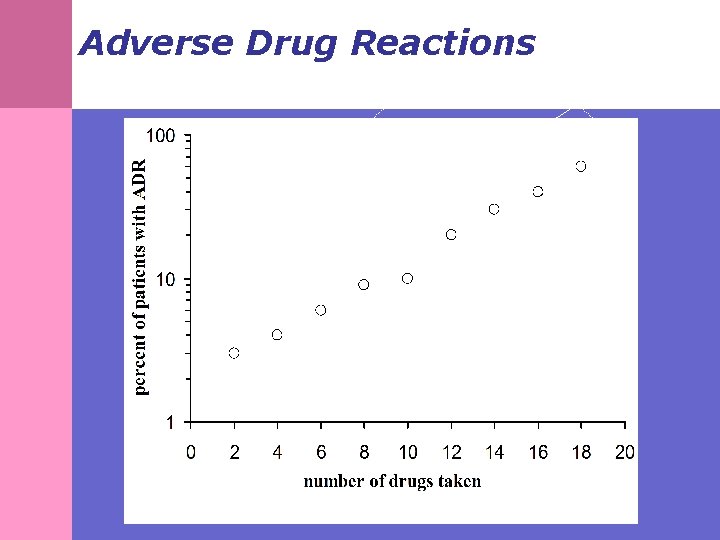
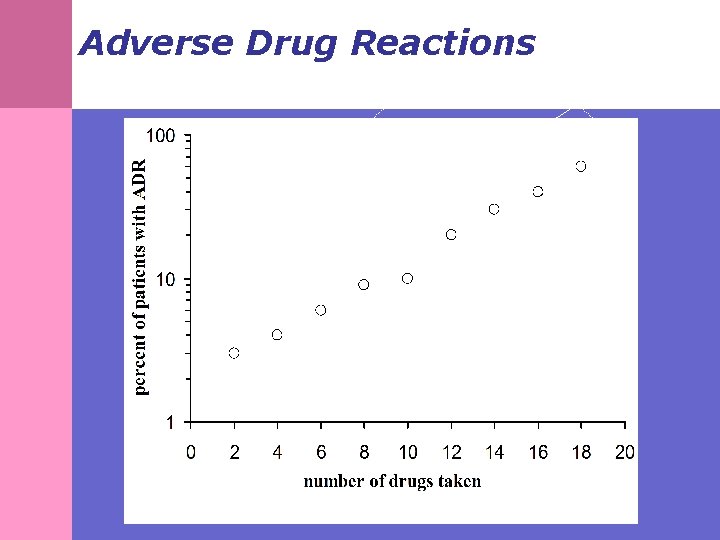
Adverse Drug Reactions § About 3 to 7% of all hospital admissions in the United States are for treatment of adverse drug reactions. § Adverse drug reactions occur during 10 to 20% of hospital admissions, and about 10 to 20% of these reactions are severe. § The most consistent risk factor for an adverse drug reactions is: The number of drugs being taken. § The risk increases exponentially as the number of drugs increases as illustrated in the following chart…
Adverse Drug Reactions
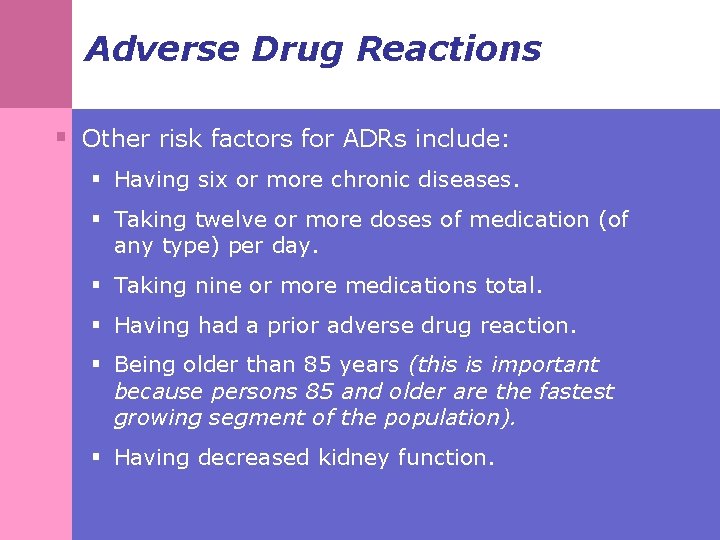
Adverse Drug Reactions § Other risk factors for ADRs include: § Having six or more chronic diseases. § Taking twelve or more doses of medication (of any type) per day. § Taking nine or more medications total. § Having had a prior adverse drug reaction. § Being older than 85 years (this is important because persons 85 and older are the fastest growing segment of the population). § Having decreased kidney function.
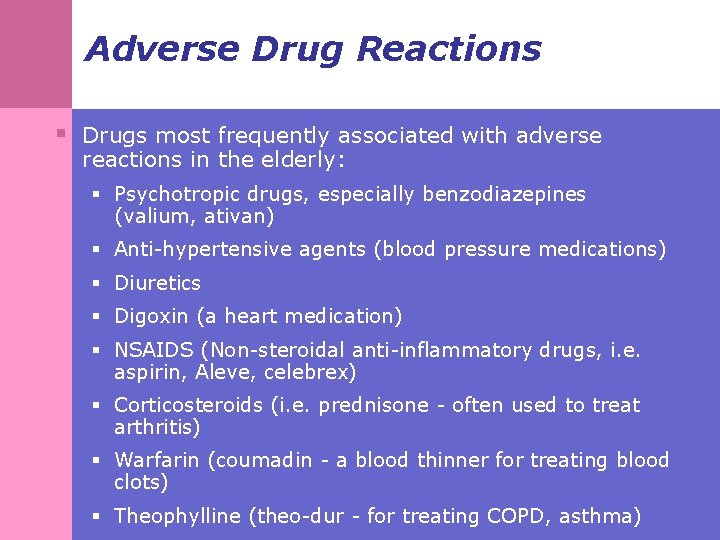
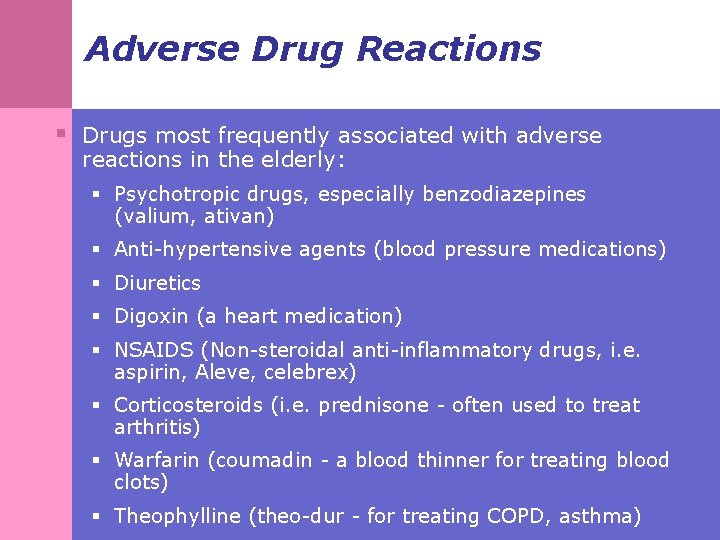
Adverse Drug Reactions § Drugs most frequently associated with adverse reactions in the elderly: § Psychotropic drugs, especially benzodiazepines (valium, ativan) § Anti-hypertensive agents (blood pressure medications) § Diuretics § Digoxin (a heart medication) § NSAIDS (Non-steroidal anti-inflammatory drugs, i. e. aspirin, Aleve, celebrex) § Corticosteroids (i. e. prednisone - often used to treat arthritis) § Warfarin (coumadin - a blood thinner for treating blood clots) § Theophylline (theo-dur - for treating COPD, asthma)
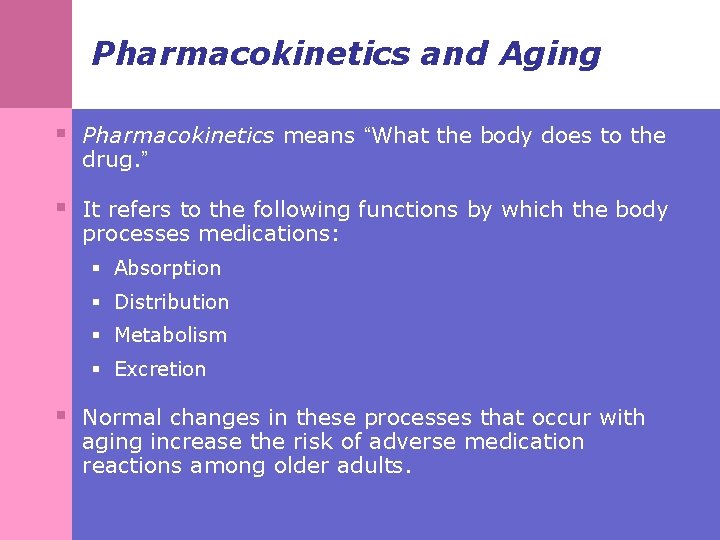
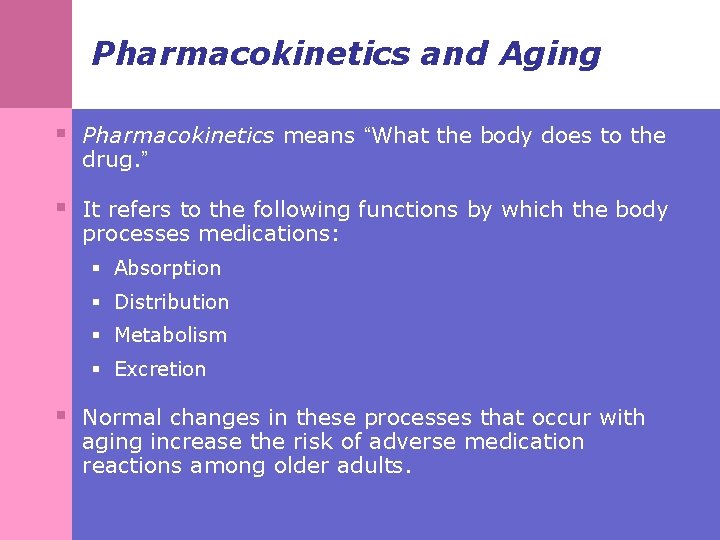
Pharmacokinetics and Aging § Pharmacokinetics means “What the body does to the drug. ” § It refers to the following functions by which the body processes medications: § Absorption § Distribution § Metabolism § Excretion § Normal changes in these processes that occur with aging increase the risk of adverse medication reactions among older adults.
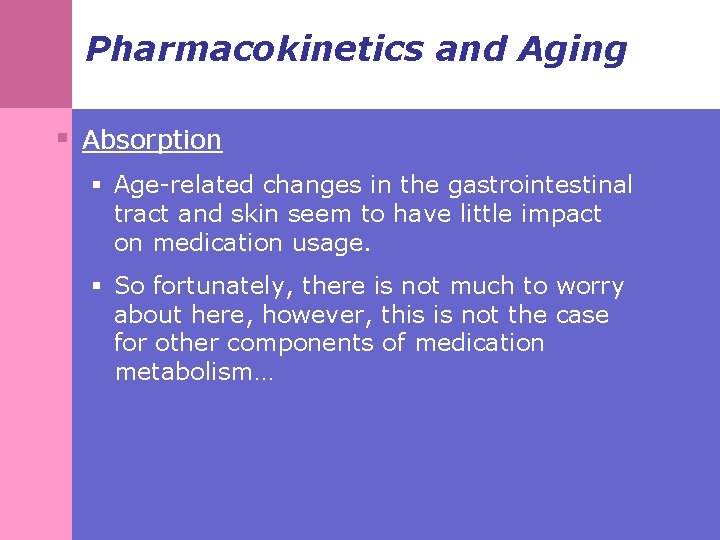
Pharmacokinetics and Aging § Absorption § Age-related changes in the gastrointestinal tract and skin seem to have little impact on medication usage. § So fortunately, there is not much to worry about here, however, this is not the case for other components of medication metabolism…
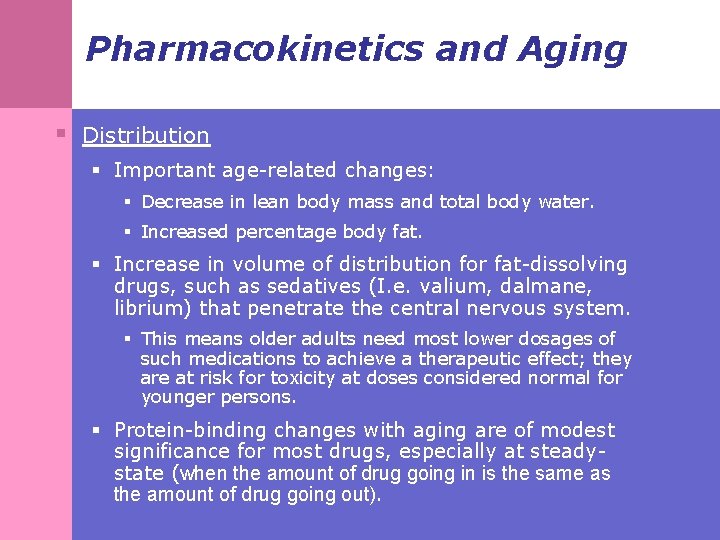
Pharmacokinetics and Aging § Distribution § Important age-related changes: § Decrease in lean body mass and total body water. § Increased percentage body fat. § Increase in volume of distribution for fat-dissolving drugs, such as sedatives (I. e. valium, dalmane, librium) that penetrate the central nervous system. § This means older adults need most lower dosages of such medications to achieve a therapeutic effect; they are at risk for toxicity at doses considered normal for younger persons. § Protein-binding changes with aging are of modest significance for most drugs, especially at steadystate (when the amount of drug going in is the same as the amount of drug going out).
Pharmacokinetics and Aging § Metabolism § Many medications are processed by the liver. § Although liver function is relatively unchanged with age, there is some overall decline in metabolic capacity § Plus, many of the chronic conditions common among older adults do negatively impact liver function. § Decreased liver mass and hepatic blood flow lead to: § High variability with no good estimation algorithms for doctors to determine appropriate medication dosages for older adults. § Minimal clinical manifestations of actual underlying problems, so it is difficult for doctors to determine when someone may be having problems.
Pharmacokinetics and Aging § Renal Excretion § Medications are eliminated from the body via the kidneys and urinary system. § Age-related decreases in renal blood flow and kidney function (specifically, glomerular filtration rate) impact older adults’ ability to eliminate medications. § In addition, decreased lean body mass leads to decreased creatinine production (a measure of kidney function, with high levels being a cause for concern), thus, for older adults serum creatinine may appear normal even when significant renal impairment exists!
Pharmacodynamics and Aging § Pharmacodynamics is the opposite of pharmacokinetics; it refers to “What the drug does to the body. ” § Generally, lower drug doses are required to achieve the same effect with advancing age. § This is because: § Receptor numbers, affinity, or post-receptor cellular effects may change with age. § Changes in homeostatic mechanisms can increase or decrease drug sensitivity.
Pharmacodynamics and Aging § Panels of experts in pharmacology and geriatrics have compiled lists of medications to avoid prescribing for patients 65 years of age or older. § The most commonly used list is the Beers criteria, which include 48 "potentially inappropriate medications" (PIMs) for which there are more effective or safer alternatives for older patients (Fick, et al, 2003).
Pharmacodynamics and Aging § However in spite of the Beers criteria: § Numerous studies in the last 15 years have found that PIMs continue to be used in 12% to 40% of older patients in community and nursing home settings (Raebel, Charles, Dugan, & et al, 2007). § Administrative data from nearly 400 hospitals across the United States reveals that nearly half of all older patients hospitalized for 7 common conditions were prescribed at least 1 PIM (Rothberg et al, 2008).
Pharmacodynamics and Aging § Such irrational polypharmacy can arise from several factors: § The prescriber hesitates to discontinue medications the patient has been taking a long time. § The prescriber may add more drugs to the patient's regimen without removing any. § The prescriber orders medication to alleviate adverse reactions to other medications. § The patient may be influenced by anecdotal reports touting the benefits of certain medications. § Please refer to the handout “Reasons for Polypharmacy” for specific examples and the how social workers can help combat some of these issues.
Example Potentially Inappropriate Medications for Older Adults § Here are some medications to pay attention to as you are reviewing medical charts or physician orders for your older clients: § Propoxephene (Darvon) § Diphenhydramine (Benadryl) § Amitryptiline (Elavil) § Alprazolam (Xanax) § Diazepam (Valium) § Note that many of these are commonly prescribed psychotropic medications used in the treatment of mental health disorders! Source: Beers, M. H. et al. (1991). Arch Intern Med, 151, 1825 -1832.
Polypharmacy in Older Adults: Social Work Interventions § Overview: Two important areas for social work involvement: § Polypharmacy and medication nonadherence § The “Brown Bag”
Polypharmacy and Medication Non-adherence § Sometimes being on multiple medications contributes to patients not taking those medications as the physician intended. § It is important to recognize that medication non-adherence is a two-way street! § Physician factors play a role. § Patient factors play a role.
Polypharmacy and Medication Non-adherence § Example contributing factors: § Patients § Underreporting symptoms § Use of multiple providers § Use of others’ medications § Physicians § Limited time for discussion, diagnostics § Limited knowledge of geriatric pharmacology § The power of inertia
Polypharmacy and Medication Non-adherence § Additional contributing factors: § Large number of medications § Expensive medications § Complex or frequently changing medication schedule § Adverse reactions § Confusion about brand name/trade name § Difficult-to-open containers § Rectal, vaginal, subcutaneous modes of administration § Limited patient understanding of medication’s purpose
Polypharmacy and Medication Non-adherence § Like polypharmacy itself, the strongest predictor of medication non-adherence is the number of medications. § Non-adherence rates are estimated at 25 -50 percent of older adults. § Non-adherence is intentional about 75% of the time: § Changes in medication regimen made by patients to: • Increase convenience • Reduce adverse effects • Decrease refill expense
Reducing Polypharmacy and Promoting Medication Adherence § Ask the right questions! § You can help protect older clients against polypharmacy by asking these questions: § Are you currently taking five or more prescription medications? § Do you ever borrow medications from other people? § Do you use over-the-counter medications, including vitamins, dietary supplements, or herbal preparations? § Do you request refills without seeing your health care provider? § Do you have prescription medications from more than one health care provider? § Do you have prescriptions filled at more than one pharmacy?
Reducing Polypharmacy and Promoting Medication Adherence § The “Brown Bag” § At least yearly, and more often if indicated, ask your older clients to bring in all medications they have at home (they often bring them in a big brown grocery bag, thus the name of this intervention!) § Prescription medications § Over-the-counter medications § Vitamins supplements § Herbal preparations § Intervention has four components - listing medications, discussing client’s understanding of why the medication is prescribed, discussing potential side effects, and reporting the findings.
The Brown Bag: Vitamin and Herbal Use in Older Adults § Use of vitamins and herbal remedies is highly prevalent among older adults! § Usage is generally not reported to the physician since older adults may not consider them to be medications. § Some serious drug interactions are possible with common herbal remedies, for example: § Ginkgo biloba interactions include bleeding when combined with warfarin (coumadin), raised blood pressure when combined with a thiazide diuretics and coma when combined with trazodone (desyrel). § The handout “ 10 Tips for Reducing Polypharmacy” can be given or discussed with your clients as a self advocacy tool.
What to Do with the Brown Bag Full of Bottles? § First: List the medications and the associated dosages and administration schedules - see the Brown Bag Patient Education Tool in Handouts. § Second: Ask the client to tell you what the medications are prescribed for. If you hear, “I don’t know…the doctor told me to…” this is cause for concern - additional patient education is needed!
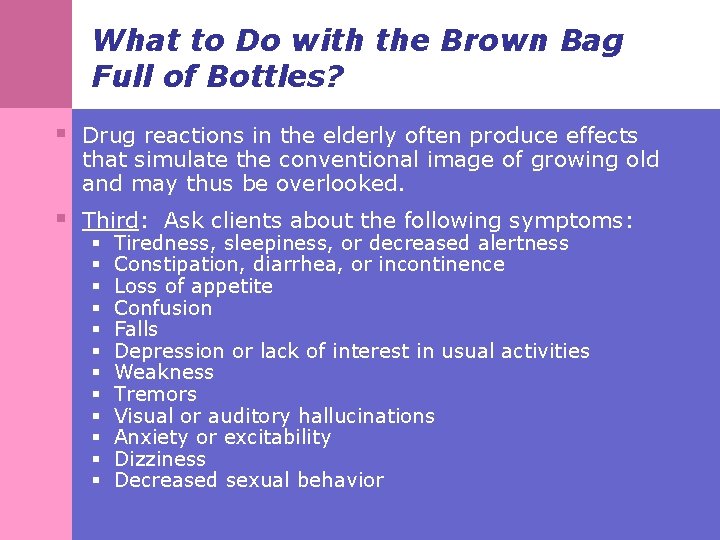
What to Do with the Brown Bag Full of Bottles? § Drug reactions in the elderly often produce effects that simulate the conventional image of growing old and may thus be overlooked. § Third: Ask clients about the following symptoms: § § § Tiredness, sleepiness, or decreased alertness Constipation, diarrhea, or incontinence Loss of appetite Confusion Falls Depression or lack of interest in usual activities Weakness Tremors Visual or auditory hallucinations Anxiety or excitability Dizziness Decreased sexual behavior
What to Do with the Brown Bag Full of Bottles? § Fourth: Report findings; depending on your work setting: § Discuss the findings with the client’s physician (nursing home, hospice, primary care, inpatient settings) - the pharmacist can also be helpful in nursing home settings. § Encourage the client to share the findings with his/her primary physician or pharmacist and role play the interaction as indicated (outpatient mental health clinics, home health, case management agencies…etc. )
General Patient Education Information § Encourage your clients to: § Use one pharmacist/pharmacy. § Use your PCP as intended…avoid seeing multiple physicians (except when necessary for second opinions). § Do not use medications from others. § Report all symptoms to PCP. § All medicines, even over-the-counter vitamins and herbal remedies, can have adverse effects. § Report all products used to PCP. § See handout “ 10 tips for reducing polypharmacy” for additional suggestions.
Additional Readings § Williams CM. (2002). Using medication appropriately in older adults. § § § § American Family Physician, 66(10), 1917 -1924. Klein D, et al. (2004). Elders who delay medication because of costs: health insurance, demographic, health and financial correlates. The Gerontologist, 44(6): 779 -787. Peterson E. (n. d. ) Aging gracefully. Reducing your risk of polypharmacy. Retrieved from Somerset Medical Center Web site: www. somersetmedicalcenter. com/frame. cfm? id=219. Arcangelo V, Peterson A. (2001). Pharmacotherapeutics for Advanced Practice. Philadelphia, Pa. : Lippincott, Williams & Wilkins. Schmader K, et al. (2004). Effects of geriatric evaluation and management on adverse drug reactions and suboptimal prescribing in the elderly. American Journal of Medicine, 116(6), 394 -401. Hanlon J, et al. (2004). Inappropriate medication use among frail elderly inpatients. Annals of Pharmacotherapy, 38(1), 9 -14. Flaherty J, et al. (2000). Polypharmacy and hospitalization among older home care patients. Journal of Gerontology: A Biological Sciences/Medical Sciences, 55(10), 554 -559. Zhan C, et al. (2001). Potentially inappropriate medication use in the community dwelling elderly. JAMA, 286(22), 2823 -2829. Fulton M, Allen E. (2005). Polypharmacy in the elderly: a literature review. Journal of the American Academy of Nurse Practitioners, 17(4), 123 -132.