Polypharmacy An introductory module for clinicians Lawrence Jackson
- Slides: 36
Polypharmacy An introductory module for clinicians Lawrence Jackson, BSc. Phm, CTDP Pharmacy Clinical Coordinator, Sunnybrook Health Sciences
This module is part of the sf. Care approach Power. Point Presentation 8. 5 x 11 Poster Patient Handout 2
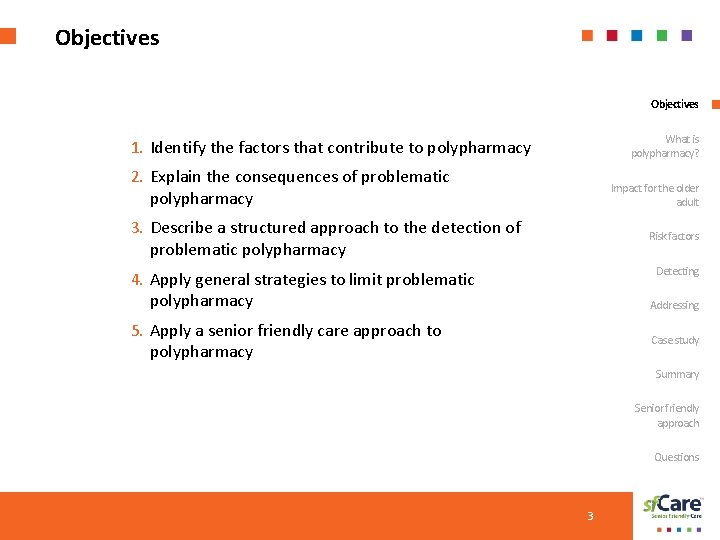
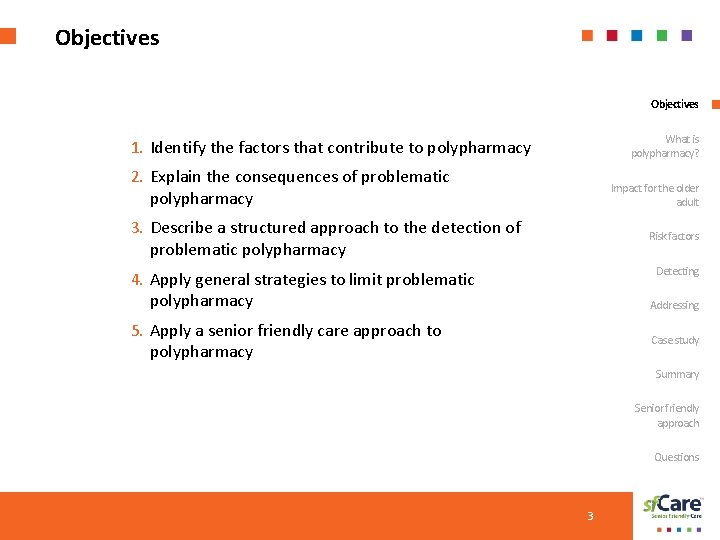
Objectives What is polypharmacy? 1. Identify the factors that contribute to polypharmacy 2. Explain the consequences of problematic Impact for the older adult polypharmacy 3. Describe a structured approach to the detection of Risk factors problematic polypharmacy Detecting 4. Apply general strategies to limit problematic polypharmacy Addressing 5. Apply a senior friendly care approach to Case study polypharmacy Summary Senior friendly approach Questions 3
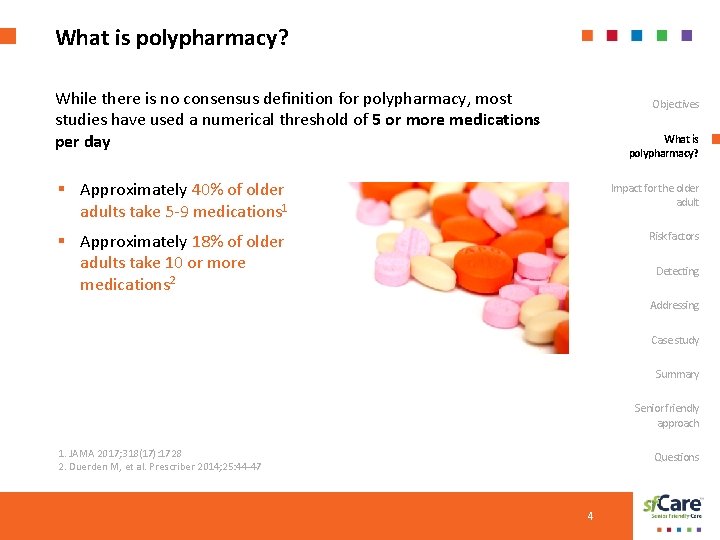
What is polypharmacy? While there is no consensus definition for polypharmacy, most studies have used a numerical threshold of 5 or more medications per day Objectives What is polypharmacy? § Approximately 40% of older Impact for the older adult § Approximately 18% of older Risk factors adults take 5 -9 medications 1 adults take 10 or more medications 2 Detecting Addressing Case study Summary Senior friendly approach 1. JAMA 2017; 318(17): 1728 2. Duerden M, et al. Prescriber 2014; 25: 44 -47 Questions 4
Appropriate versus problematic polypharmacy Objectives Appropriate Polypharmacy What is polypharmacy? § Medication optimization ensures benefits outweigh risks Impact for the older adult § Takes into consideration impact on outcomes important to the older adult, such as Risk factors • Improving the duration and quality of life Detecting • Symptom control • Prevention Addressing § It is evidence-based Case study Summary Senior friendly approach JAMA 2017; 318(17): 1728 Duerden M, et al. Prescriber 2014; 25: 44 -47 Questions 5
Appropriate versus problematic polypharmacy Objectives Problematic Polypharmacy What is polypharmacy? § Risk of harm exceeds the Impact for the older adult potential benefits or coexists with the benefits Risk factors Detecting Addressing Case study Summary Senior friendly approach JAMA 2017; 318(17): 1728 Duerden M, et al. Prescriber 2014; 25: 44 -47 Questions 6
Impact of polypharmacy on the older adult The following risks accompany polypharmacy: Objectives What is polypharmacy? 1. adverse drug reactions 2. drug interactions Impact for the older adult 3. cost 4. risk of non adherence Risk factors 5. risk of medication errors Detecting 6. Precipitate or exacerbate geriatric syndromes Addressing Case study Summary Senior friendly approach Questions 7
Impact of polypharmacy on the older adult Geriatric syndromes Objectives § Falls What is polypharmacy? § Functional impairment § Cognitive impairment Impact for the older adult § Urinary incontinence Risk factors § Impaired nutrition § Dehydration Detecting § Constipation Addressing Case study Summary Senior friendly approach Questions 8
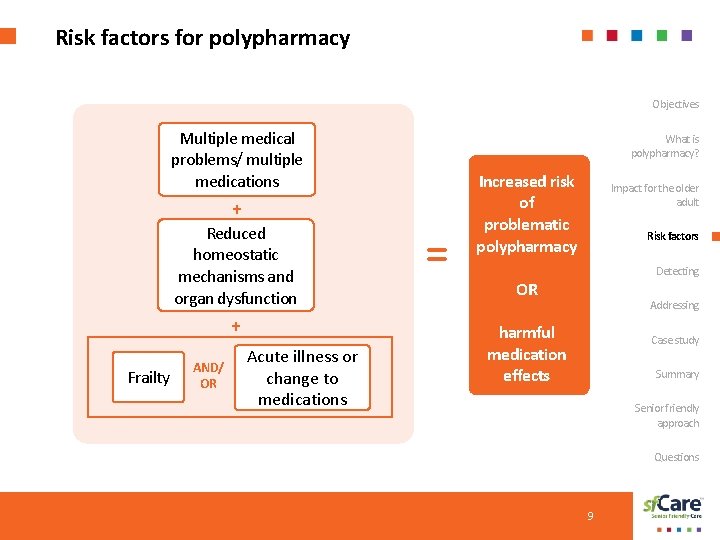
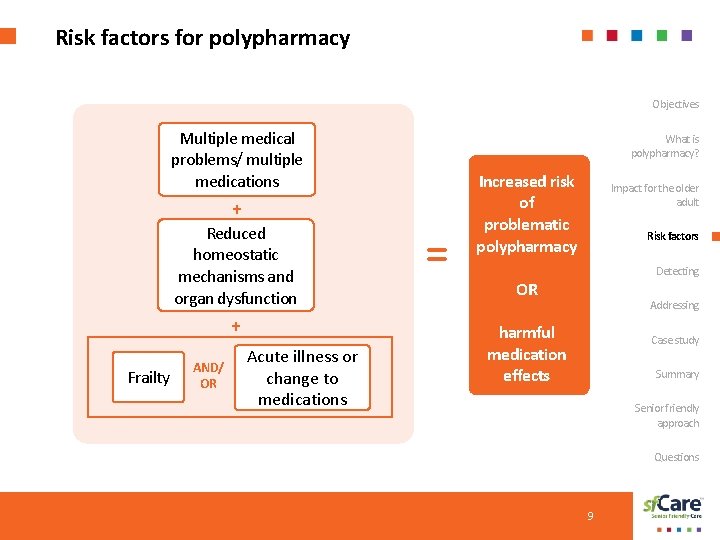
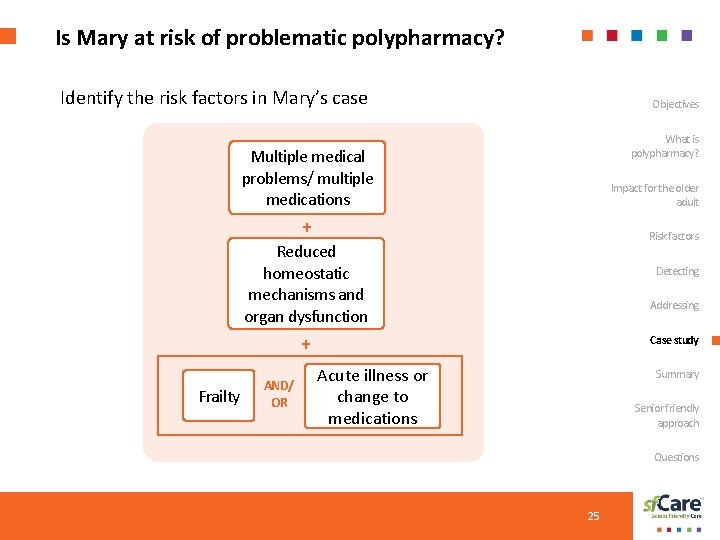
Risk factors for polypharmacy Objectives Multiple medical problems/ multiple medications What is polypharmacy? + Reduced homeostatic mechanisms and organ dysfunction + Frailty AND/ OR Acute illness or change to medications = Increased risk of problematic polypharmacy Impact for the older adult Risk factors Detecting OR Addressing harmful medication effects Case study Summary Senior friendly approach Questions 9
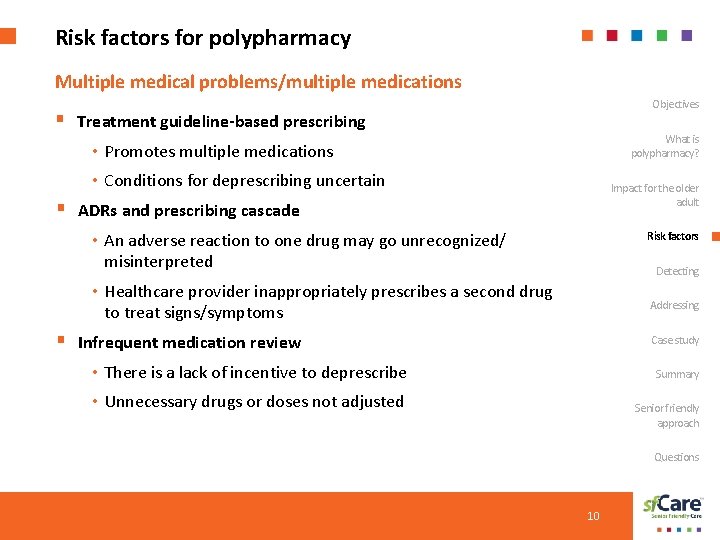
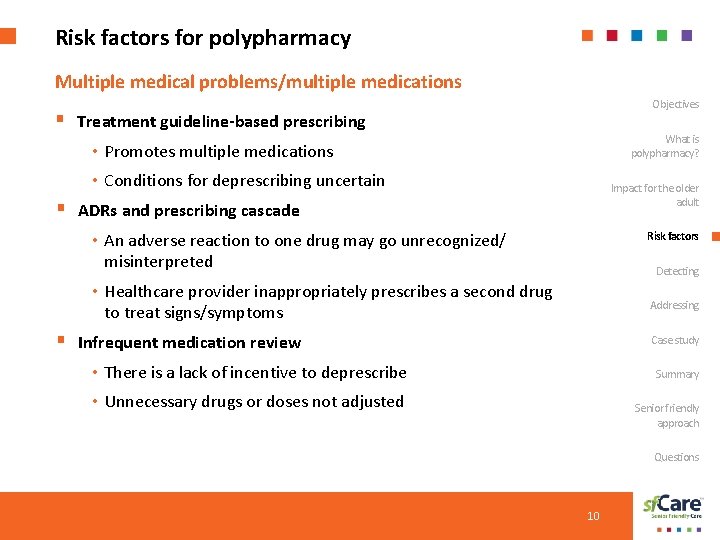
Risk factors for polypharmacy Multiple medical problems/multiple medications Objectives § Treatment guideline-based prescribing What is polypharmacy? • Promotes multiple medications • Conditions for deprescribing uncertain Impact for the older adult § ADRs and prescribing cascade • An adverse reaction to one drug may go unrecognized/ Risk factors misinterpreted Detecting • Healthcare provider inappropriately prescribes a second drug Addressing to treat signs/symptoms § Infrequent medication review Case study • There is a lack of incentive to deprescribe Summary • Unnecessary drugs or doses not adjusted Senior friendly approach Questions 10
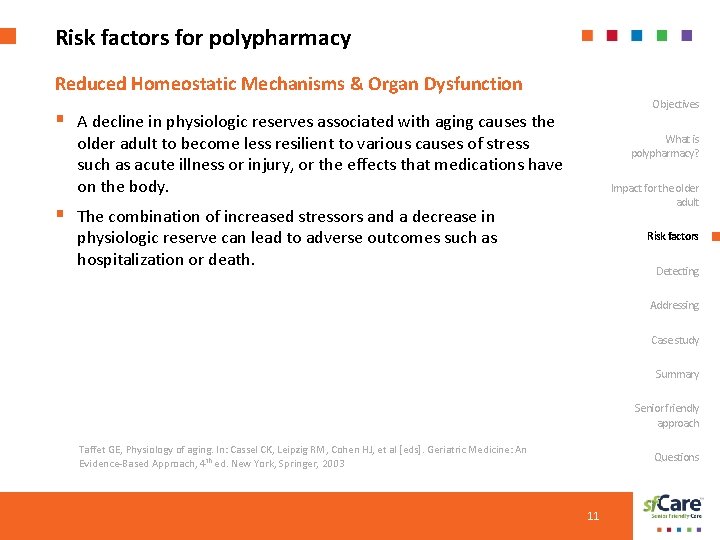
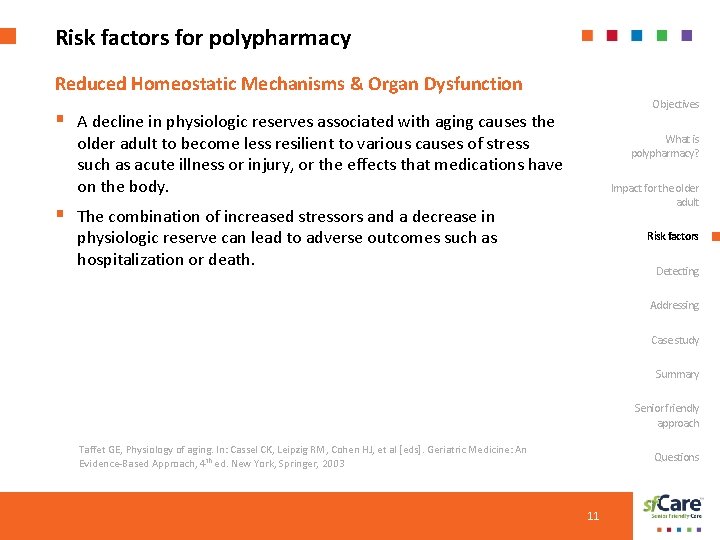
Risk factors for polypharmacy Reduced Homeostatic Mechanisms & Organ Dysfunction Objectives § A decline in physiologic reserves associated with aging causes the What is polypharmacy? older adult to become less resilient to various causes of stress such as acute illness or injury, or the effects that medications have on the body. Impact for the older adult § The combination of increased stressors and a decrease in physiologic reserve can lead to adverse outcomes such as hospitalization or death. Risk factors Detecting Addressing Case study Summary Senior friendly approach Taffet GE, Physiology of aging. In: Cassel CK, Leipzig RM, Cohen HJ, et al [eds]. Geriatric Medicine: An Evidence-Based Approach, 4 th ed. New York, Springer, 2003 Questions 11
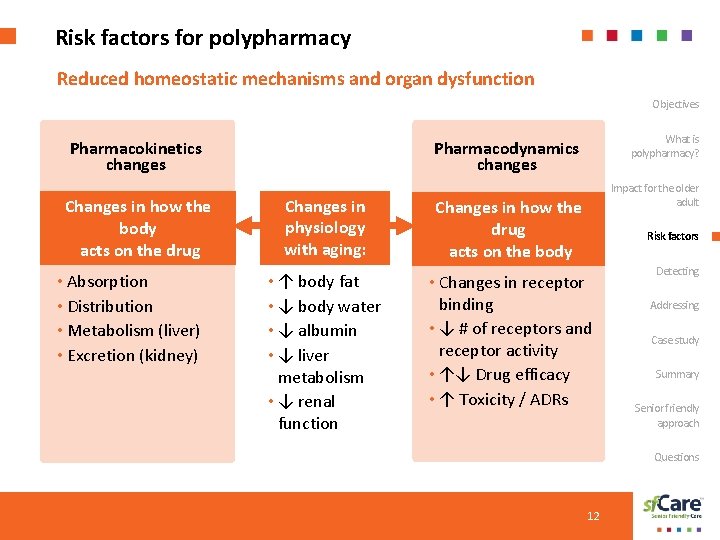
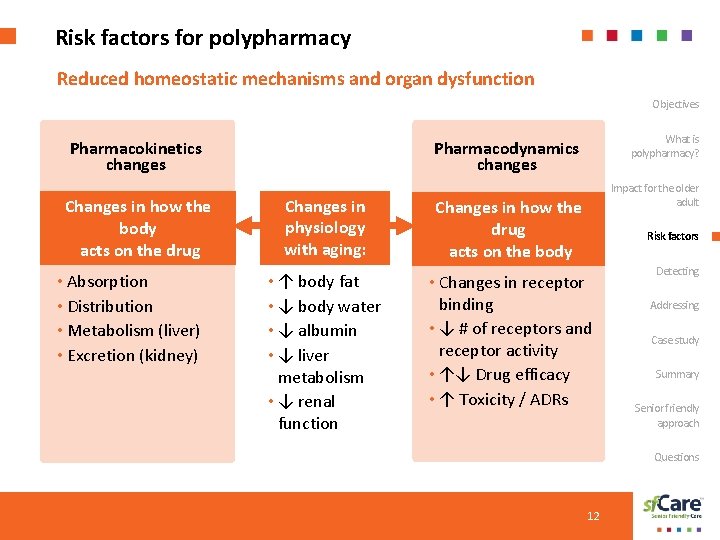
Risk factors for polypharmacy Reduced homeostatic mechanisms and organ dysfunction Objectives Pharmacokinetics changes Changes in how the body acts on the drug • Absorption • Distribution • Metabolism (liver) • Excretion (kidney) What is polypharmacy? Pharmacodynamics changes Impact for the older adult Changes in physiology with aging: Changes in how the drug acts on the body • ↑ body fat • ↓ body water • ↓ albumin • ↓ liver metabolism • ↓ renal function • Changes in receptor binding • ↓ # of receptors and receptor activity • ↑↓ Drug efficacy • ↑ Toxicity / ADRs Risk factors Detecting Addressing Case study Summary Senior friendly approach Questions 12
Risk factors for polypharmacy Frailty Objectives Older people are vulnerable to medicationrelated problems associated with frailty. What is polypharmacy? Characteristics of frailty Impact for the older adult § Unintended weight loss due to inadequate nutrition Risk factors § Slow walking speed Detecting § Impaired grip strength Addressing § Exhaustion Case study § Self reported decline in activity levels Robust Pre-frail 0 1 -2 Summary Frail ≥ 3 Senior friendly approach Questions 13
Risk factors for polypharmacy Frailty (cont. ) Objectives Several factors are known to be associated with frailty: What is polypharmacy? § Older age § Multiple medical problems (or geriatric syndromes) Impact for the older adult § Taking multiple medications Risk factors § Multiple psychosocial problems § One or more sensory impairments (vision, hearing) Detecting § New onset urinary or fecal incontinence Addressing § Decrease in functional status Case study § Change in mental status- cognition/affect Summary § Disruptive behavior or personality changes Senior friendly approach § Frequent falls Questions 14
Risk factors for polypharmacy Objectives Acute illness or changes to medication can lead to problematic polypharmacy What is polypharmacy? § With acute illness, usual medications can cause unanticipated harm Impact for the older adult § With any change in medications or change in dose, adverse effects can result Risk factors Detecting Addressing Case study Summary Senior friendly approach Questions 15
Challenges in detecting polypharmacy Objectives § Problems due to medications may occur • Without any changes to the medication What is polypharmacy? • Advancing age Impact for the older adult • Coincident with acute illness or symptoms Risk factors § ADRs masquerade as age-related changes Detecting • Atypical presentation of adverse effects • Side effects difficult to interpret, may go unreported Addressing • Prescribing cascade Case study Summary § Infrequent Medication Review Senior friendly approach • There is a lack of incentive to deprescribe Questions 16
Detecting problematic polypharmacy Problematic polypharmacy can present in atypical ways, such as … § § § Objectives Exaggerated medication effects What is polypharmacy? Loss of medication’s effect Impact for the older adult Problems with taking medication New or worsening symptoms or conditions Risk factors Decline in functional and self-care abilities Detecting Decline in mobility Addressing Case study Confusion and falls are important clues that resilience is compromised in an older adult and should prompt a search for causes, including medications! Summary Senior friendly approach Questions 17
Addressing polypharmacy Assess medication list with an available tool Objectives What is polypharmacy? § Explicit criteria – list of potentially inappropriate medications Impact for the older adult § Implicit criteria or Risk factors comprehensive assessment § Medication assessment Detecting framework Addressing Case study Summary Senior friendly approach Questions 18
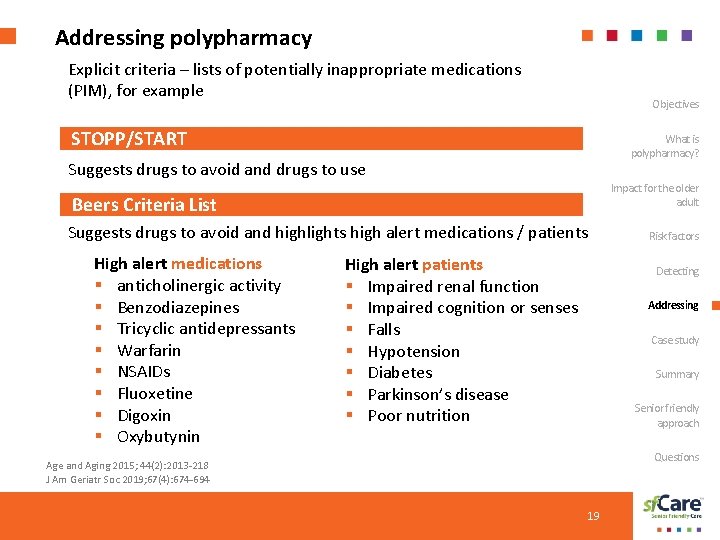
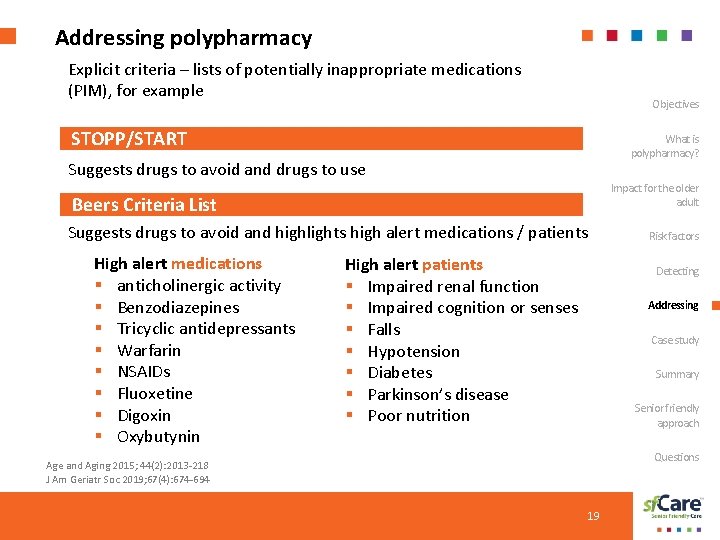
Addressing polypharmacy Explicit criteria – lists of potentially inappropriate medications (PIM), for example Objectives STOPP/START What is polypharmacy? Suggests drugs to avoid and drugs to use Impact for the older adult Beers Criteria List Suggests drugs to avoid and highlights high alert medications / patients High alert medications § anticholinergic activity § Benzodiazepines § Tricyclic antidepressants § Warfarin § NSAIDs § Fluoxetine § Digoxin § Oxybutynin Risk factors High alert patients § Impaired renal function § Impaired cognition or senses § Falls § Hypotension § Diabetes § Parkinson’s disease § Poor nutrition Detecting Addressing Case study Summary Senior friendly approach Questions Age and Aging 2015; 44(2): 2013 -218 J Am Geriatr Soc 2019; 67(4): 674 -694 19
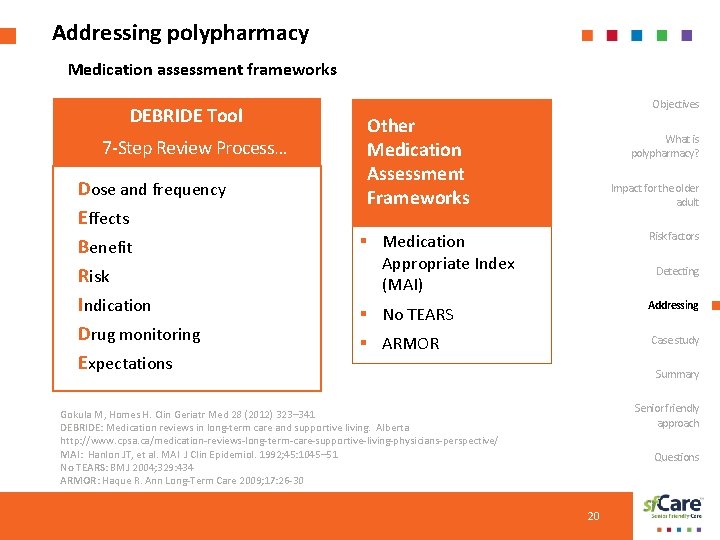
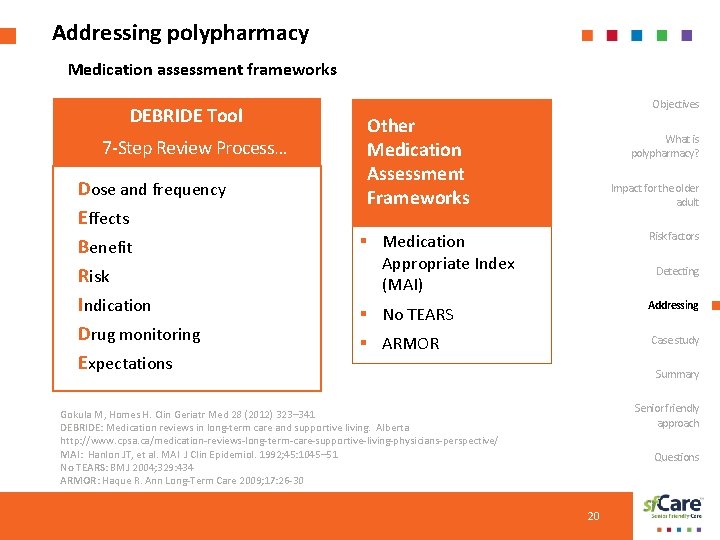
Addressing polypharmacy Medication assessment frameworks DEBRIDE Tool 7 -Step Review Process… Dose and frequency Effects Benefit Risk Indication Drug monitoring Expectations Objectives Other Medication Assessment Frameworks What is polypharmacy? Impact for the older adult § Medication Appropriate Index (MAI) Risk factors § No TEARS Addressing § ARMOR Case study Detecting Summary Senior friendly approach Gokula M, Homes H. Clin Geriatr Med 28 (2012) 323– 341 DEBRIDE: Medication reviews in long-term care and supportive living. Alberta http: //www. cpsa. ca/medication-reviews-long-term-care-supportive-living-physicians-perspective/ MAI: Hanlon JT, et al. MAI J Clin Epidemiol. 1992; 45: 1045– 51 No TEARS: BMJ 2004; 329: 434 ARMOR: Haque R. Ann Long-Term Care 2009; 17: 26 -30 Questions 20
Addressing polypharmacy Implicit criteria or comprehensive assessment Objectives § Health status What is polypharmacy? § Prognosis and goals of care Impact for the older adult § Benefit – risk assessment of each medication and overall combination of medications Risk factors Detecting Addressing Case study Summary Senior friendly approach Questions 21
Addressing polypharmacy Limiting potential harms Objectives 1. Assess risk for polypharmacy What is polypharmacy? 2. Annual review of medications in all older adults 3. Inform caregivers of medication changes to increase the chance of detecting problems as soon as possible Impact for the older adult Risk factors 4. Chose medications with the fewest side effects 5. Stop unnecessary medications Detecting 6. Consider the impact of medications on quality of life Addressing 7. Consider the person’s ability to take medications and remember to take them Case study Summary Senior friendly approach Questions 22
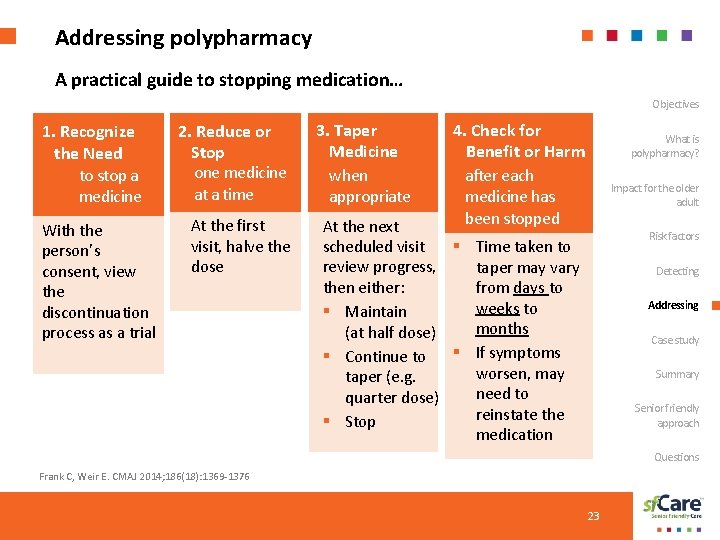
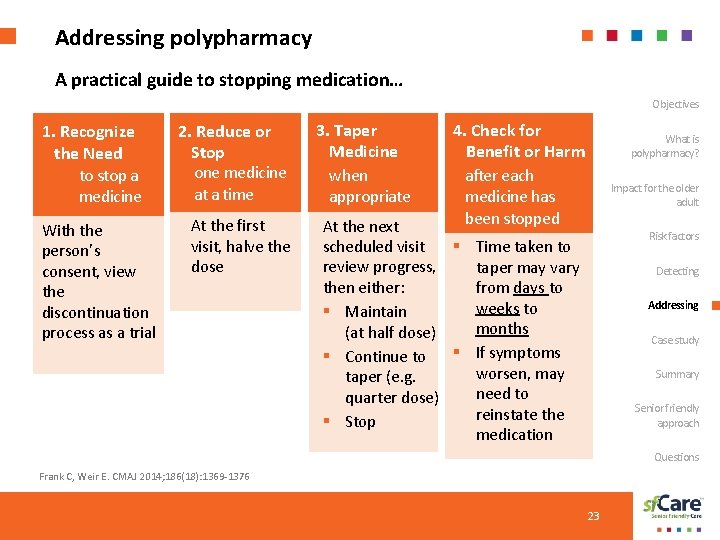
Addressing polypharmacy A practical guide to stopping medication… Objectives 1. Recognize the Need to stop a medicine With the person’s consent, view the discontinuation process as a trial 2. Reduce or Stop one medicine at a time At the first visit, halve the dose 3. Taper Medicine when appropriate 4. Check for Benefit or Harm after each medicine has been stopped What is polypharmacy? Impact for the older adult At the next scheduled visit § Time taken to review progress, taper may vary then either: from days to weeks to § Maintain months (at half dose) § Continue to § If symptoms worsen, may taper (e. g. need to quarter dose) reinstate the § Stop medication Risk factors Detecting Addressing Case study Summary Senior friendly approach Questions Frank C, Weir E. CMAJ 2014; 186(18): 1369 -1376 23
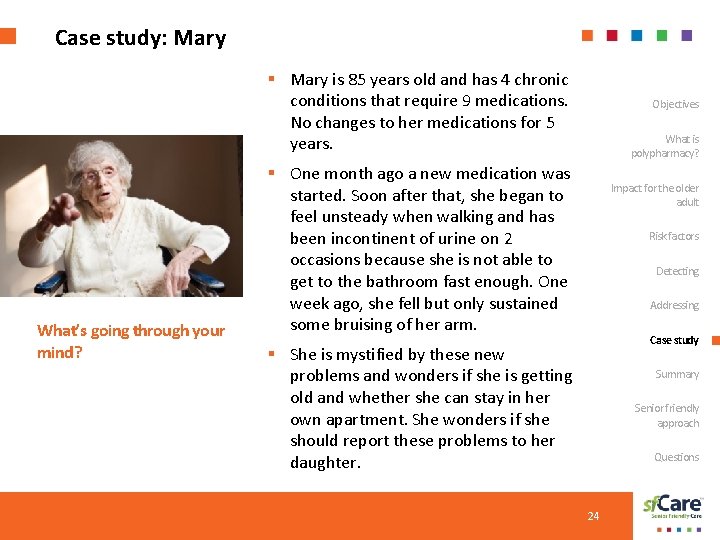
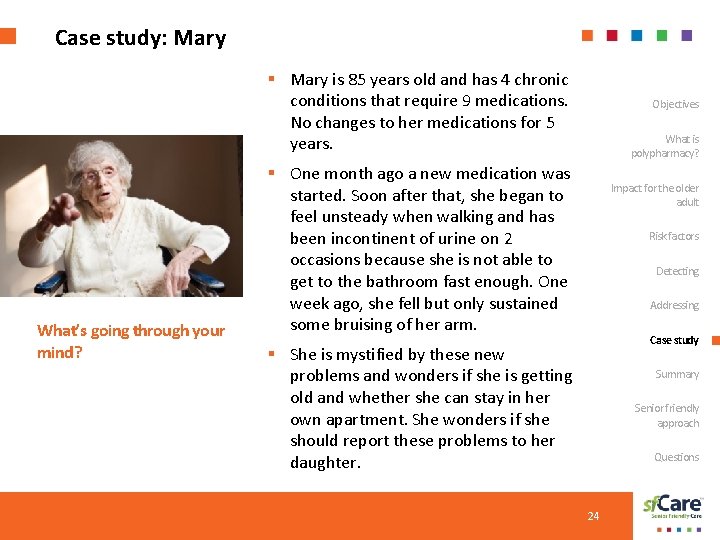
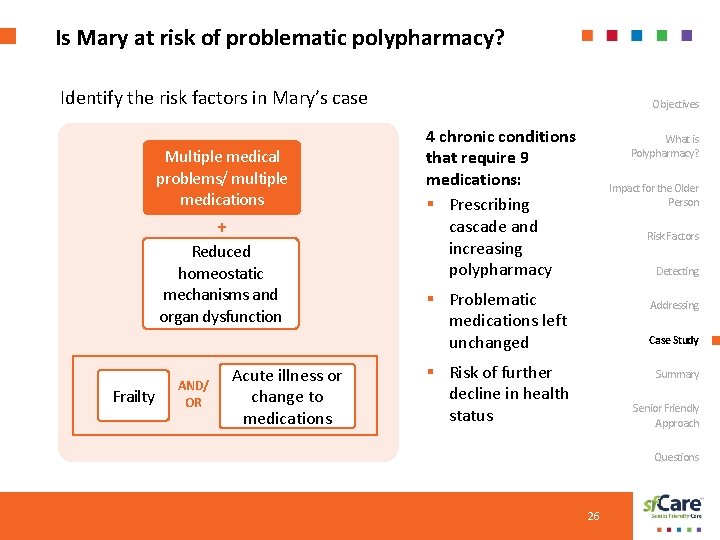
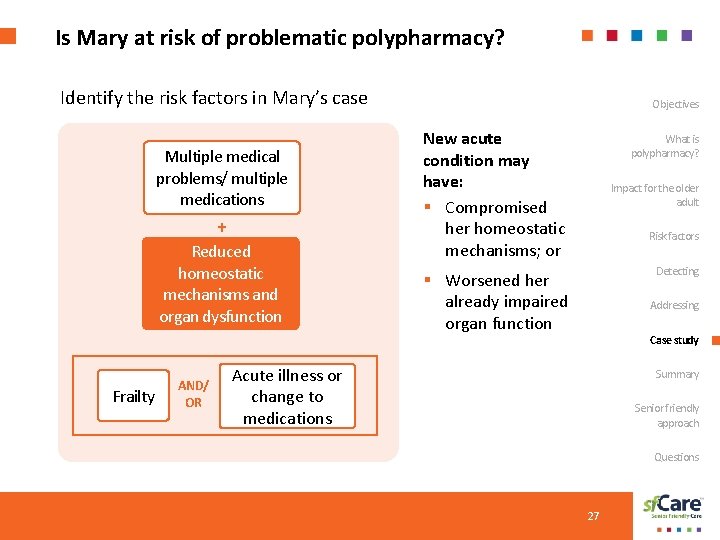
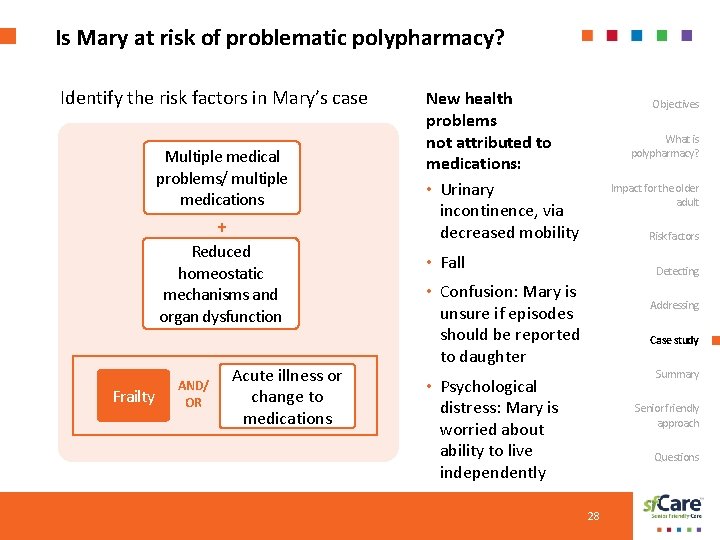
Case study: Mary § Mary is 85 years old and has 4 chronic conditions that require 9 medications. No changes to her medications for 5 years. What’s going through your mind? Objectives What is polypharmacy? § One month ago a new medication was started. Soon after that, she began to feel unsteady when walking and has been incontinent of urine on 2 occasions because she is not able to get to the bathroom fast enough. One week ago, she fell but only sustained some bruising of her arm. Impact for the older adult Risk factors Detecting Addressing Case study § She is mystified by these new problems and wonders if she is getting old and whether she can stay in her own apartment. She wonders if she should report these problems to her daughter. Summary Senior friendly approach Questions 24
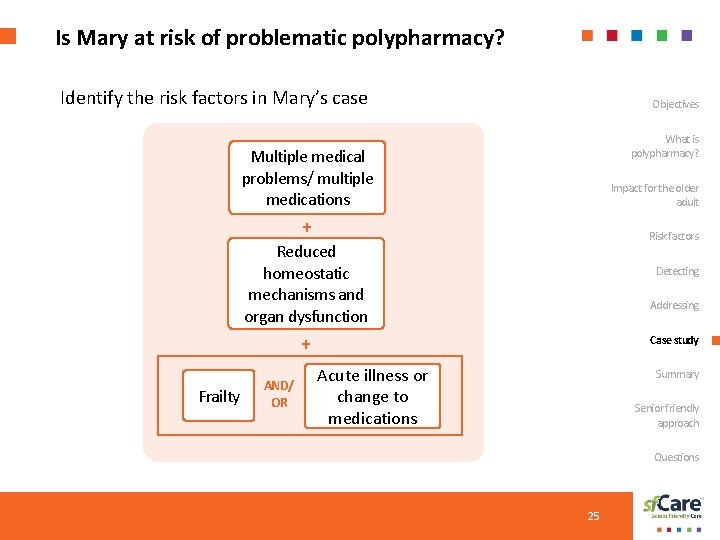
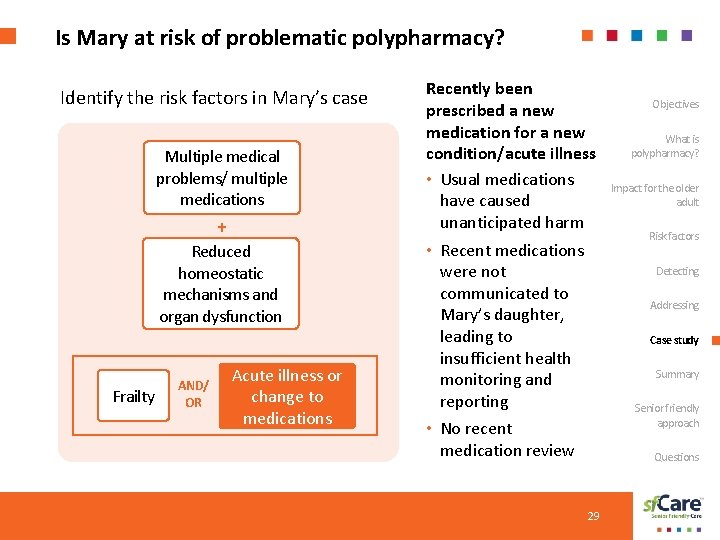
Is Mary at risk of problematic polypharmacy? Identify the risk factors in Mary’s case Objectives What is polypharmacy? Multiple medical problems/ multiple medications Impact for the older adult + Risk factors Reduced homeostatic mechanisms and organ dysfunction Detecting Addressing + Frailty AND/ OR Case study Acute illness or change to medications Summary Senior friendly approach Questions 25
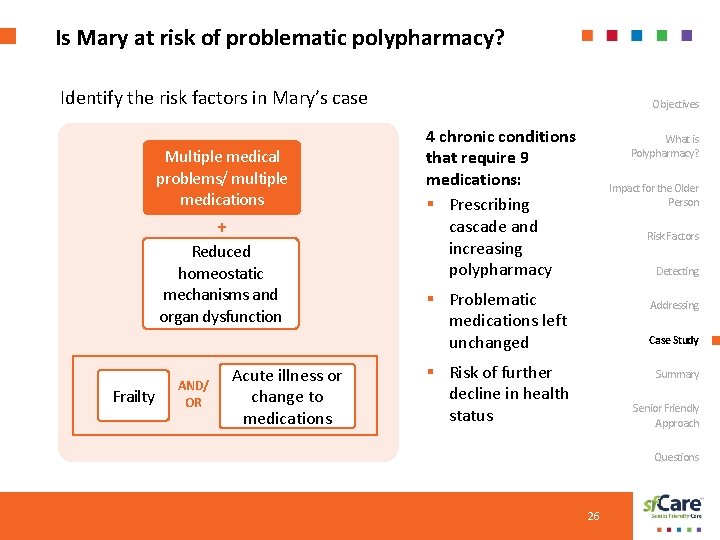
Is Mary at risk of problematic polypharmacy? Identify the risk factors in Mary’s case Multiple medical problems/ multiple medications + Reduced homeostatic mechanisms and organ dysfunction Frailty AND/ OR Acute illness or change to medications Objectives 4 chronic conditions that require 9 medications: § Prescribing cascade and increasing polypharmacy What is Polypharmacy? Impact for the Older Person Risk Factors Detecting § Problematic medications left unchanged Addressing Case Study § Risk of further decline in health status Summary Senior Friendly Approach Questions 26
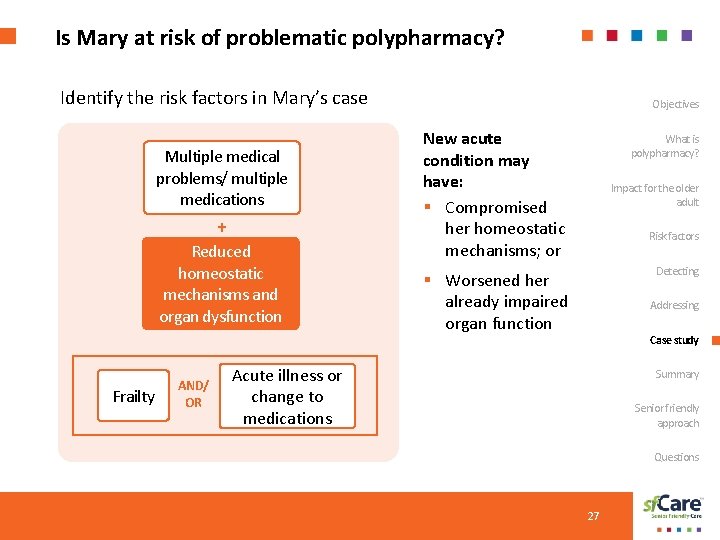
Is Mary at risk of problematic polypharmacy? Identify the risk factors in Mary’s case Multiple medical problems/ multiple medications + Reduced homeostatic mechanisms and organ dysfunction Frailty AND/ OR Objectives New acute condition may have: § Compromised her homeostatic mechanisms; or What is polypharmacy? Impact for the older adult Risk factors Detecting § Worsened her already impaired organ function Addressing Case study Acute illness or change to medications Summary Senior friendly approach Questions 27
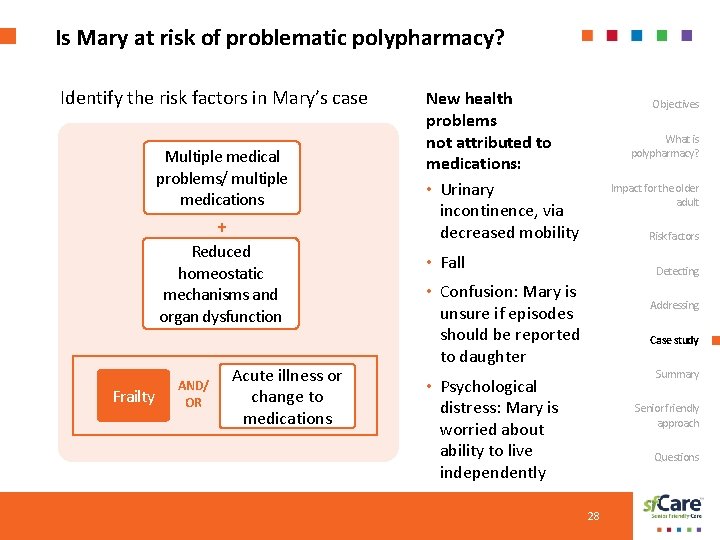
Is Mary at risk of problematic polypharmacy? Identify the risk factors in Mary’s case Multiple medical problems/ multiple medications + Reduced homeostatic mechanisms and organ dysfunction Frailty AND/ OR Acute illness or change to medications New health problems not attributed to medications: • Urinary incontinence, via decreased mobility Objectives What is polypharmacy? Impact for the older adult Risk factors • Fall Detecting • Confusion: Mary is unsure if episodes should be reported to daughter Addressing Case study Summary • Psychological distress: Mary is worried about ability to live independently Senior friendly approach Questions 28
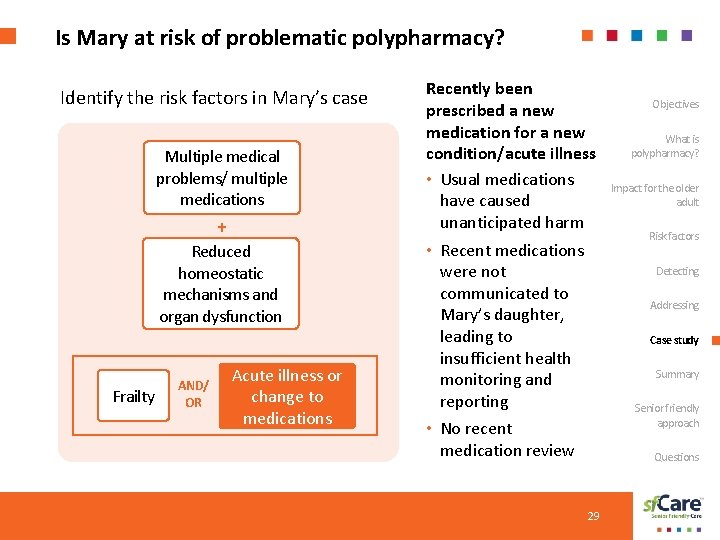
Is Mary at risk of problematic polypharmacy? Identify the risk factors in Mary’s case Multiple medical problems/ multiple medications + Reduced homeostatic mechanisms and organ dysfunction Frailty AND/ OR Acute illness or change to medications Recently been prescribed a new medication for a new condition/acute illness • Usual medications have caused unanticipated harm • Recent medications were not communicated to Mary’s daughter, leading to insufficient health monitoring and reporting • No recent medication review 29 Objectives What is polypharmacy? Impact for the older adult Risk factors Detecting Addressing Case study Summary Senior friendly approach Questions
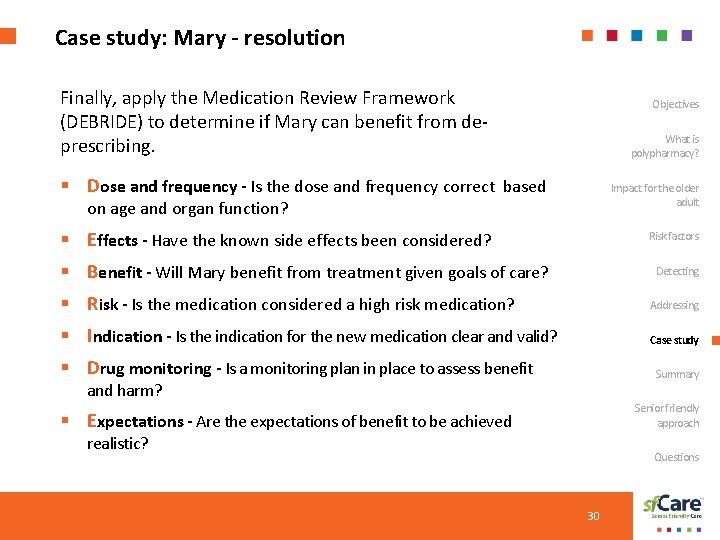
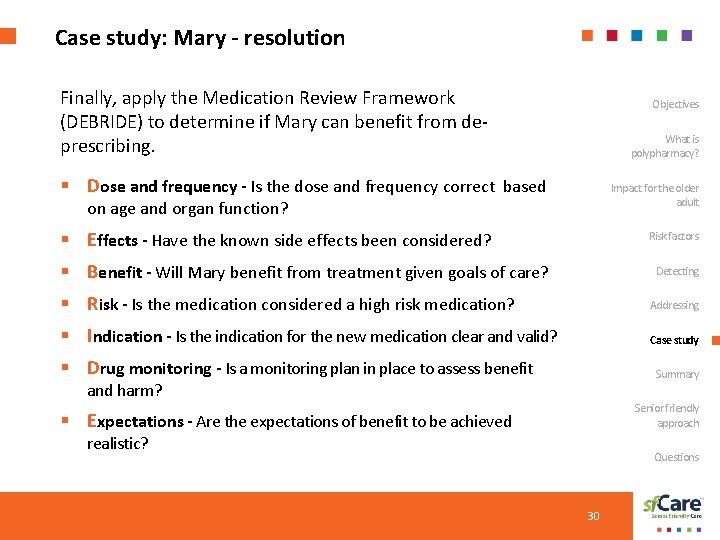
Case study: Mary - resolution Finally, apply the Medication Review Framework (DEBRIDE) to determine if Mary can benefit from deprescribing. Objectives What is polypharmacy? § Dose and frequency - Is the dose and frequency correct based Impact for the older adult on age and organ function? § Effects - Have the known side effects been considered? Risk factors § Benefit - Will Mary benefit from treatment given goals of care? Detecting § Risk - Is the medication considered a high risk medication? Addressing § Indication - Is the indication for the new medication clear and valid? Case study § Drug monitoring - Is a monitoring plan in place to assess benefit Summary and harm? Senior friendly approach § Expectations - Are the expectations of benefit to be achieved realistic? Questions 30
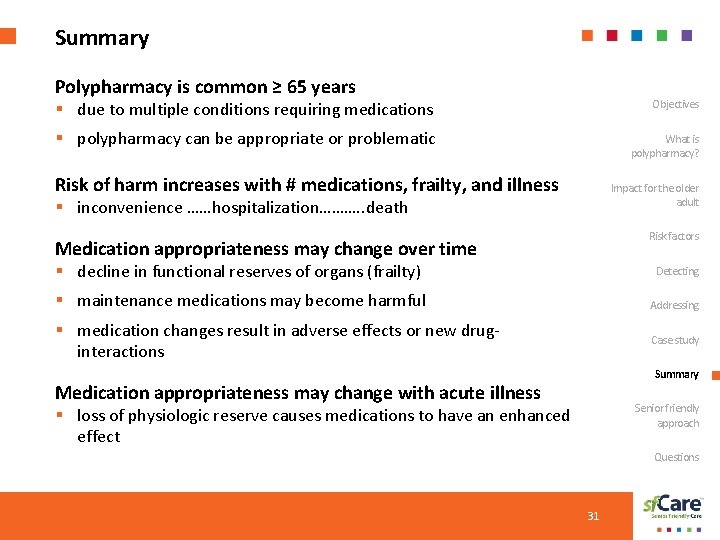
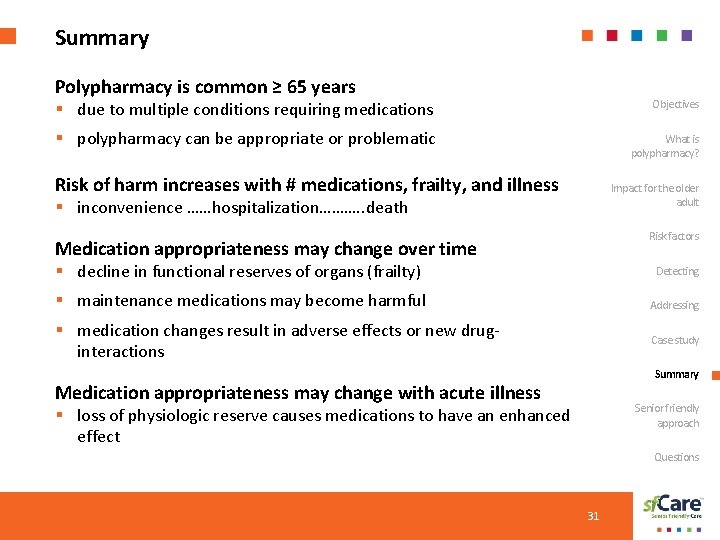
Summary Polypharmacy is common ≥ 65 years § due to multiple conditions requiring medications Objectives § polypharmacy can be appropriate or problematic What is polypharmacy? Risk of harm increases with # medications, frailty, and illness Impact for the older adult § inconvenience ……hospitalization………. . death Risk factors Medication appropriateness may change over time § decline in functional reserves of organs (frailty) Detecting § maintenance medications may become harmful Addressing § medication changes result in adverse effects or new druginteractions Case study Summary Medication appropriateness may change with acute illness Senior friendly approach § loss of physiologic reserve causes medications to have an enhanced effect Questions 31
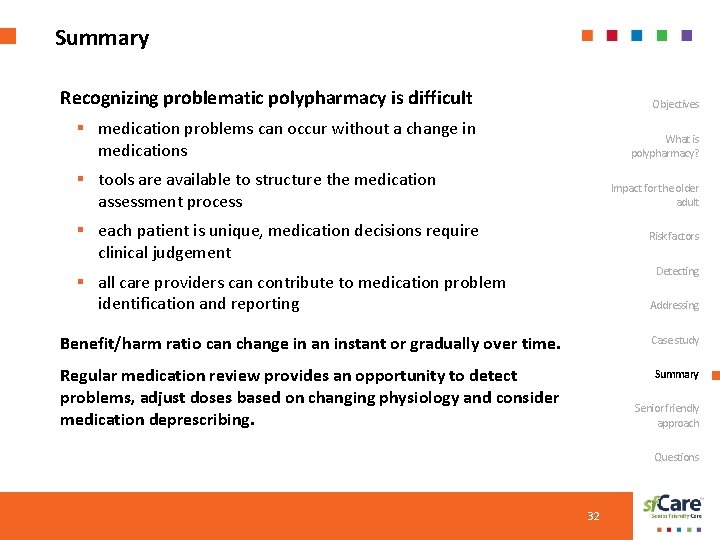
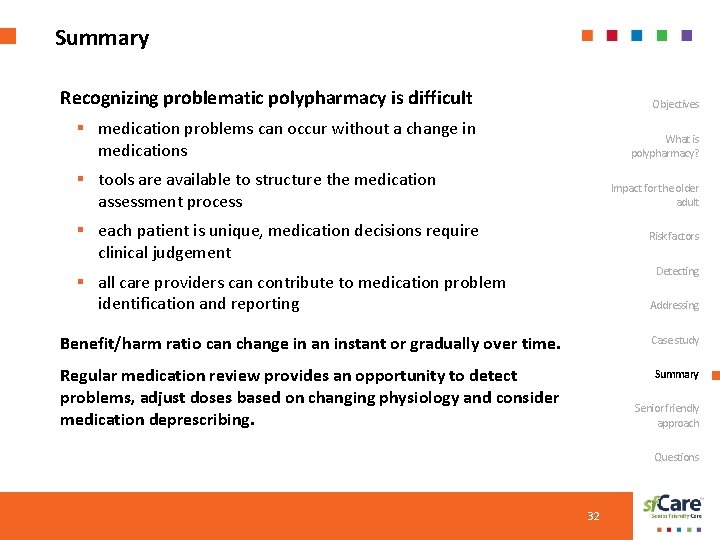
Summary Recognizing problematic polypharmacy is difficult Objectives § medication problems can occur without a change in medications What is polypharmacy? § tools are available to structure the medication assessment process Impact for the older adult § each patient is unique, medication decisions require clinical judgement Risk factors Detecting § all care providers can contribute to medication problem identification and reporting Addressing Benefit/harm ratio can change in an instant or gradually over time. Case study Regular medication review provides an opportunity to detect problems, adjust doses based on changing physiology and consider medication deprescribing. Summary Senior friendly approach Questions 32
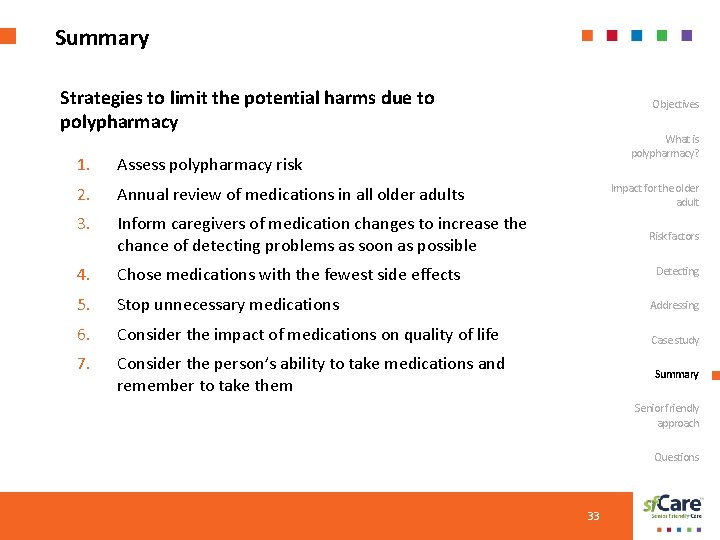
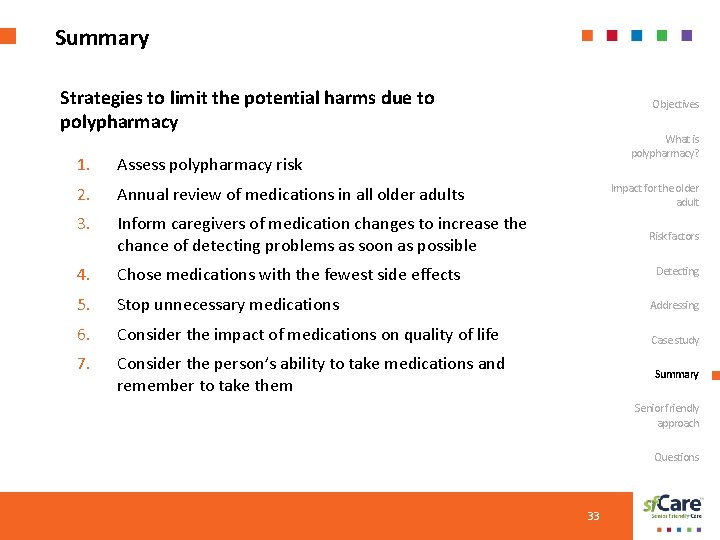
Summary Strategies to limit the potential harms due to polypharmacy Objectives What is polypharmacy? 1. Assess polypharmacy risk 2. Annual review of medications in all older adults 3. Inform caregivers of medication changes to increase the chance of detecting problems as soon as possible 4. Chose medications with the fewest side effects 5. Stop unnecessary medications Addressing 6. Consider the impact of medications on quality of life Case study 7. Consider the person’s ability to take medications and remember to take them Impact for the older adult Risk factors Detecting Summary Senior friendly approach Questions 33
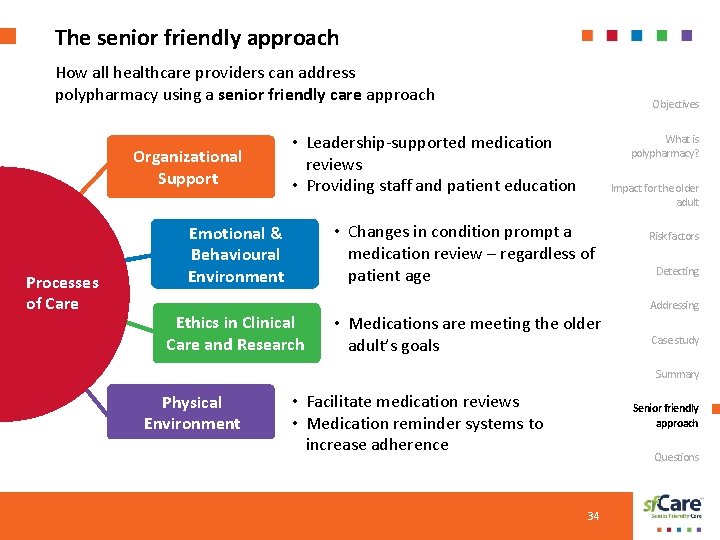
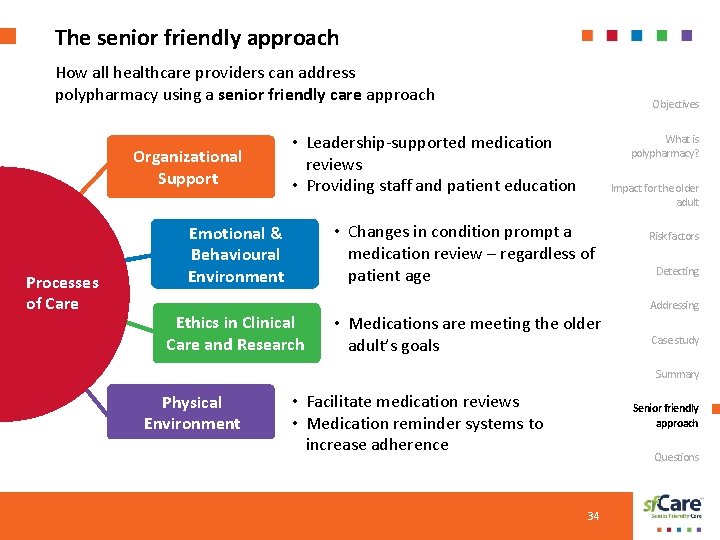
The senior friendly approach How all healthcare providers can address polypharmacy using a senior friendly care approach Organizational Support Processes of Care Objectives • Leadership-supported medication reviews • Providing staff and patient education Emotional & Behavioural Environment Ethics in Clinical Care and Research What is polypharmacy? Impact for the older adult • Changes in condition prompt a medication review – regardless of patient age • Medications are meeting the older adult’s goals Risk factors Detecting Addressing Case study Summary Physical Environment • Facilitate medication reviews • Medication reminder systems to increase adherence Senior friendly approach Questions 34
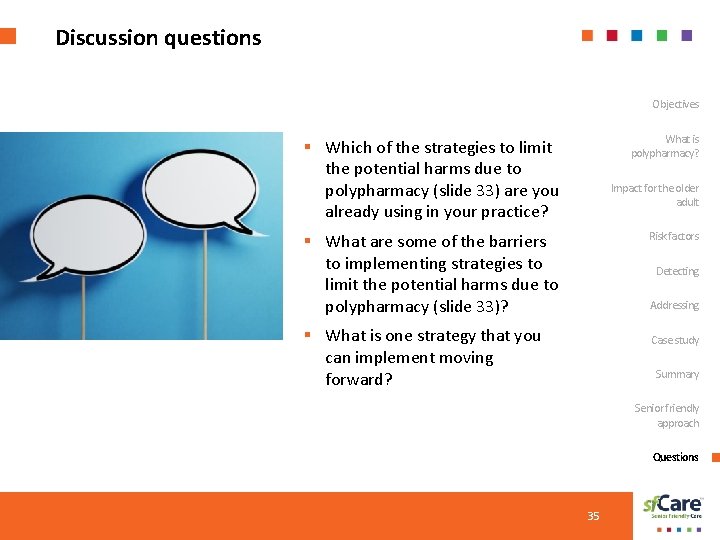
Discussion questions Objectives What is polypharmacy? § Which of the strategies to limit the potential harms due to polypharmacy (slide 33) are you already using in your practice? Impact for the older adult Risk factors § What are some of the barriers to implementing strategies to limit the potential harms due to polypharmacy (slide 33)? Detecting Addressing § What is one strategy that you can implement moving forward? Case study Summary Senior friendly approach Questions 35
The sf. Care Learning Series received support from the Regional Geriatric Programs of Ontario, through funding provided by the Ministry of Health and Long-Term Care. V 1 July 2019