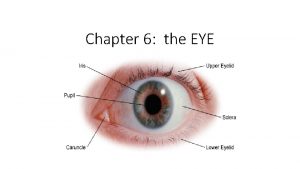
Polypharmacy in Older Adults Its in the eye













- Slides: 41

Polypharmacy in Older Adults It’s in the eye of the beholder sf. CARE Conference May 24, 2018 Lawrence Jackson, RPh, BSc. Phm, CTDP Pharmacy Clinical Coordinator, Sunnybrook Health Sciences Centre Adjunct Professor, Leslie Dan Faculty of Pharmacy, University of Toronto
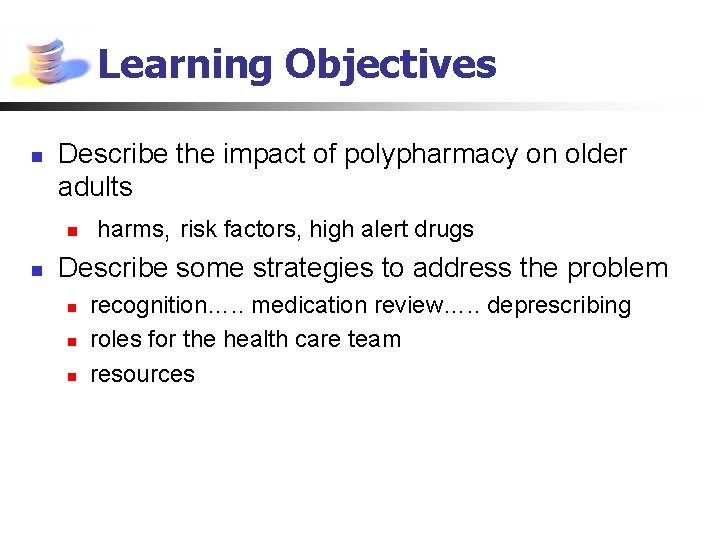
Learning Objectives n n Describe the impact of polypharmacy on older adults n harms, risk factors, high alert drugs Describe some strategies to address the problem n n n recognition…. . medication review…. . deprescribing roles for the health care team resources
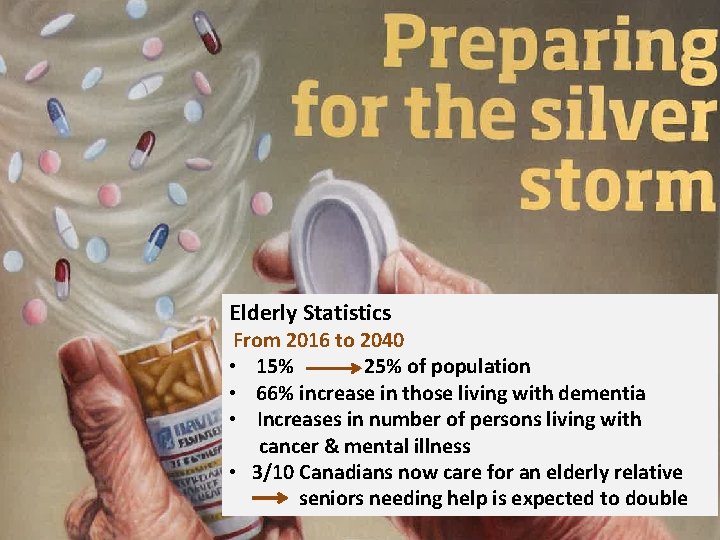
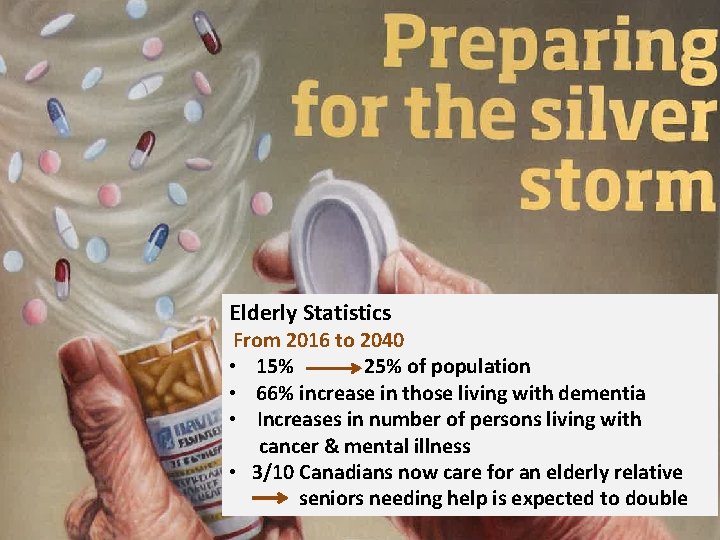
Elderly Statistics From 2016 to 2040 • 15% 25% of population • 66% increase in those living with dementia • Increases in number of persons living with cancer & mental illness • 3/10 Canadians now care for an elderly relative seniors needing help is expected to double
What is Polypharmacy? At least 24 distinct definitions 1 n Taking multiple medications* n Potential or actual negative consequences* n n Falls, confusion, functional impairments, loss of independence polypharmacy— bad vs multimodal— air of goodness A scenario created by the use of several concurrent medications in the setting of progressive decline in the functional reserves of multiple organs 2 (ie, frailty, or acute illness) 1. 2. Bushardt et al. Clinical Interventions in Aging 2008; 3(2): 383 -89 Leading Age. Medication Management Technologies for Long-Term and Post-Acute Care: A Primer and Provider Selection Guide. http: //www. leadingage. org/
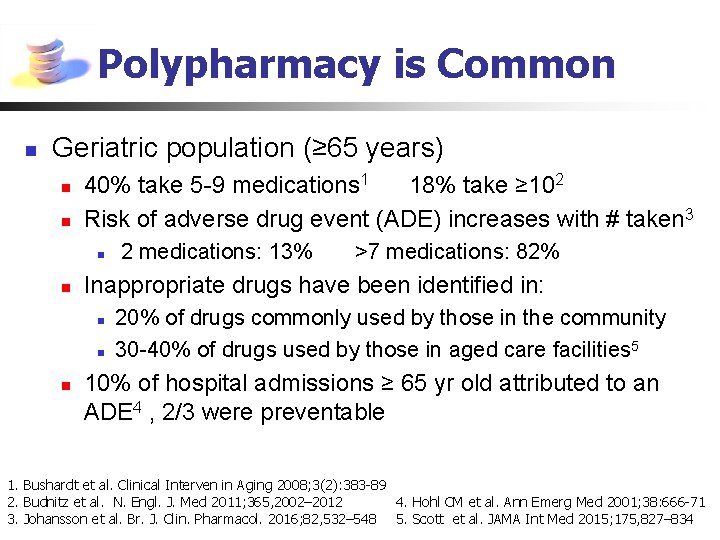
Polypharmacy is Common n Geriatric population (≥ 65 years) n n 40% take 5 -9 medications 1 18% take ≥ 102 Risk of adverse drug event (ADE) increases with # taken 3 n n >7 medications: 82% Inappropriate drugs have been identified in: n n n 2 medications: 13% 20% of drugs commonly used by those in the community 30 -40% of drugs used by those in aged care facilities 5 10% of hospital admissions ≥ 65 yr old attributed to an ADE 4 , 2/3 were preventable 1. Bushardt et al. Clinical Interven in Aging 2008; 3(2): 383 -89 2. Budnitz et al. N. Engl. J. Med 2011; 365, 2002– 2012 4. Hohl CM et al. Ann Emerg Med 2001; 38: 666 -71 3. Johansson et al. Br. J. Clin. Pharmacol. 2016; 82, 532– 548 5. Scott et al. JAMA Int Med 2015; 175, 827– 834
Detecting Polypharmacy (CSI meets the Mentalist)

Recognizing Polypharmacy Key Parameters: n n Many drugs (≥ 6) or “more than are medically necessary” Not indicated n safer or more effective option exists n changes in physiology, function or goals of care n prescribing cascade n medications with a high toxicity profile- sedative or anticholinergic properties or causing organ damage n n Duplicates/ drug interactions/ excessive dose or duration Medication taking problems (adherence issues, dysphagia or side effects) Bushardt et al. Clinical Interventions in Aging 2008; 3(2): 383 -89
Recognizing Polypharmacy Key Parameters: Context of: n n Recent changes to medications with subsequent decline in health or functioning Gradual or sudden decline in health, but maintenance medications are unchanged: n n Often in the setting of acute illness or worsening organ function or dehydration Manifested as: n Cognitive impairment, confusion or delirium, falls, functional decline, impaired mobility, social withdrawal Bushardt et al. Clinical Interventions in Aging 2008; 3(2): 383 -89
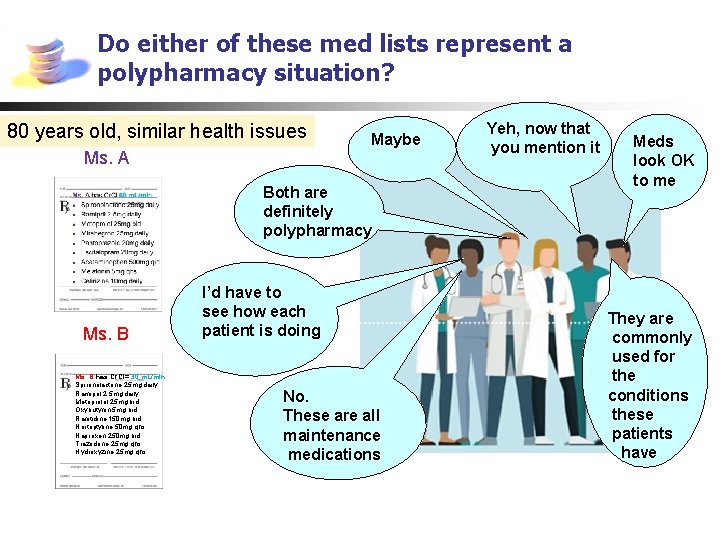
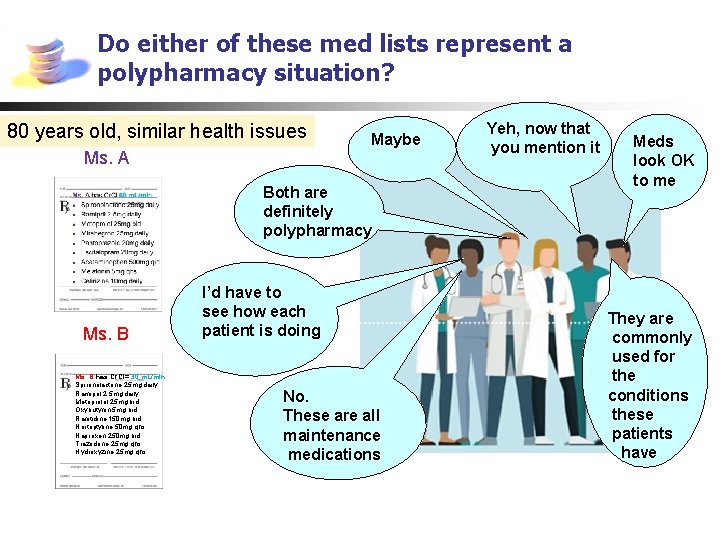
Do either of these med lists represent a polypharmacy situation? 80 years old, similar health issues Ms. A Maybe Both are definitely polypharmacy Ms. B has Cr. Cl= 30 m. L/min Spironolactone 25 mg daily Ramipril 2. 5 mg daily Metoprolol 25 mg bid Oxybutynin 5 mg bid Ranitidine 150 mg bid Nortriptyline 50 mg qhs Naproxen 250 mg bid Trazodone 25 mg qhs Hydroxyzine 25 mg qhs I’d have to see how each patient is doing No. These are all maintenance medications Yeh, now that you mention it Meds look OK to me They are commonly used for the conditions these patients have
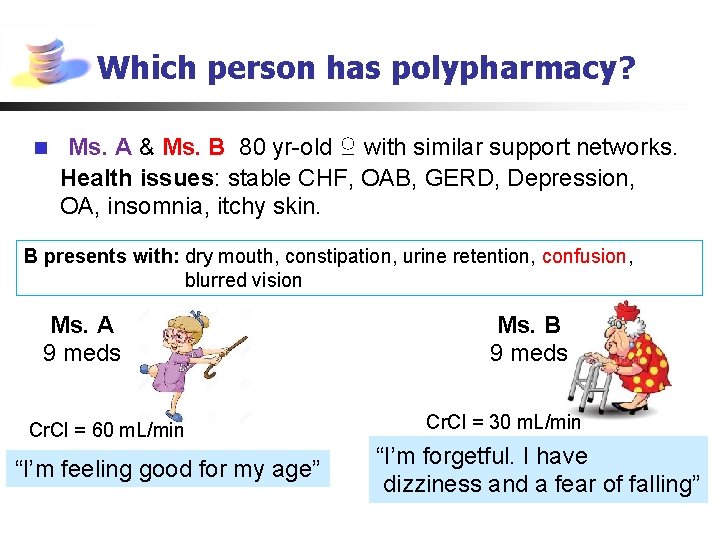
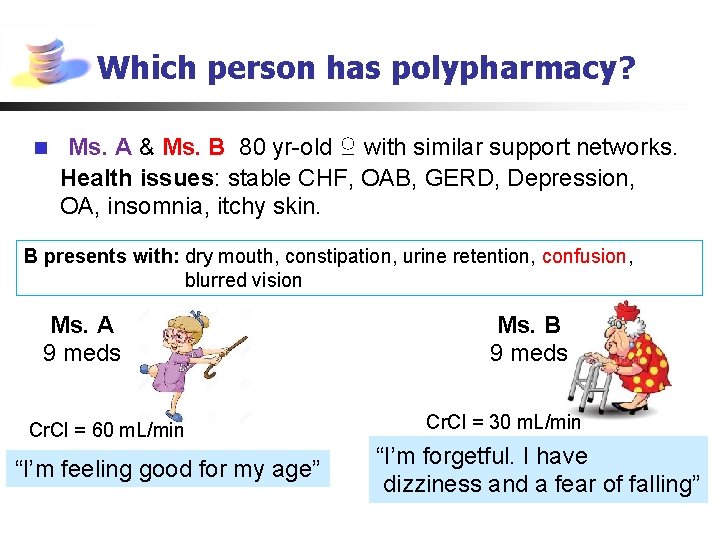
Which person has polypharmacy? n Ms. A & Ms. B 80 yr-old ♀ with similar support networks. Health issues: stable CHF, OAB, GERD, Depression, OA, insomnia, itchy skin. B presents with: dry mouth, constipation, urine retention, confusion, blurred vision Ms. A 9 meds Cr. Cl = 60 m. L/min “I’m feeling good for my age” Ms. B 9 meds Cr. Cl = 30 m. L/min “I’m forgetful. I have dizziness and a fear of falling”

Two 80 yr-old females, Ms. A & Ms. B similar support networks, stable CHF, OAB, GERD, Depression, OA, insomnia, itchy skin, forgetfulness Ms. A has Cr. Cl 60 m. L/min n Spironolactone 25 mg daily n Ramipril 2. 5 mg daily n Metoprolol 25 mg bid n Mirabegron 25 mg daily n Pantoprazole 20 mg daily n Escitalopram 20 mg daily n Acetaminophen 500 mg qid n Melatonin 5 mg qhs n Cetirizine 10 mg daily 1 Ms. B has Cr. Cl= 30 m. L/min n Spironolactone 25 mg daily n Ramipril 2. 5 mg daily n Metoprolol 25 mg bid 3 n Oxybutynin 5 mg bid n Ranitidine 150 mg bid 1 n Nortriptyline 50 mg qhs 3 n Naproxen 250 mg bid n Trazodone 25 mg qhs 1 n Hydroxyzine 25 mg qhs 3 Anticholinergic Burden Scale A= 1 B= 11 Anticholinergic effects: dry mouth, constipation, urine retention, confusion, blurred vision
Recognizing polypharmacy is difficult to do Analogy: 6 blind men and the elephant Assume medications are continuously appropriate; failure to consider impact of meds on functional status
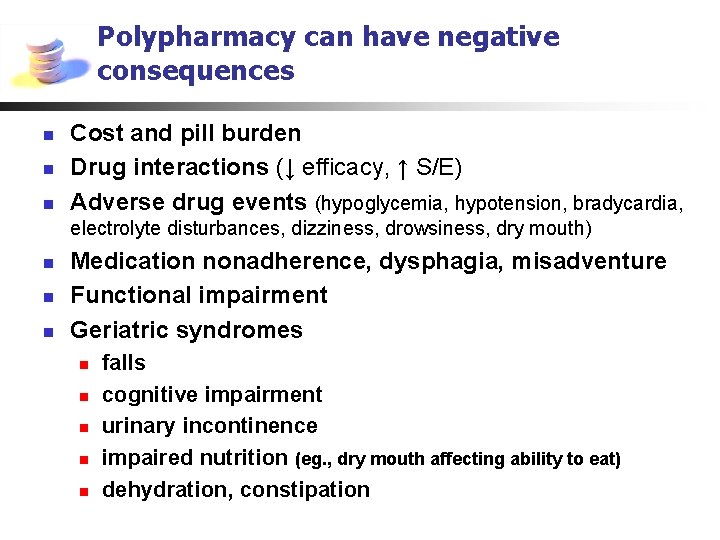
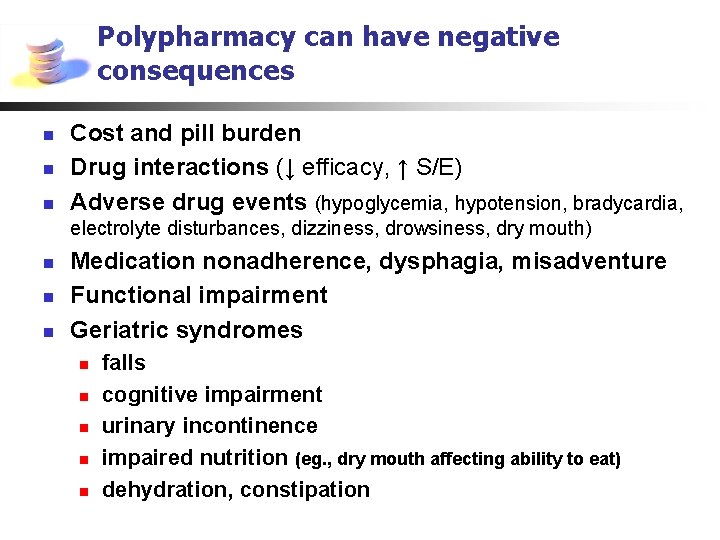
Polypharmacy can have negative consequences n n n Cost and pill burden Drug interactions (↓ efficacy, ↑ S/E) Adverse drug events (hypoglycemia, hypotension, bradycardia, electrolyte disturbances, dizziness, drowsiness, dry mouth) n n n Medication nonadherence, dysphagia, misadventure Functional impairment Geriatric syndromes n n n falls cognitive impairment urinary incontinence impaired nutrition (eg. , dry mouth affecting ability to eat) dehydration, constipation

Polypharmacy can have negative consequences on health and independent living n n n Loss of independence Increased health care utilization Emergency Room care Hospitalization Institutionalization Death Maher RL et al. Expert Opinion Drug Safety 2014; 13(1): 57 -65
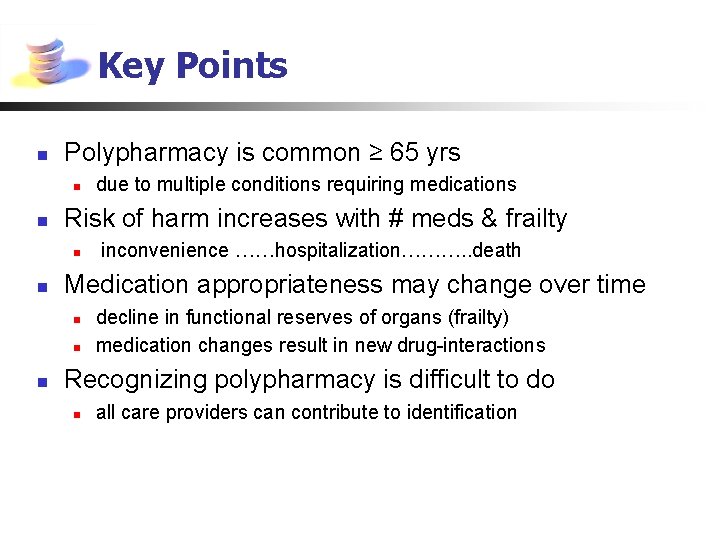
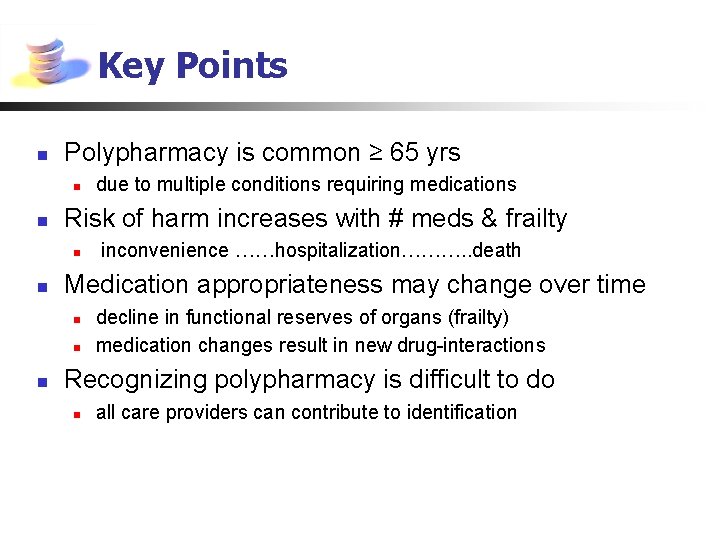
Key Points n Polypharmacy is common ≥ 65 yrs n n Risk of harm increases with # meds & frailty n n inconvenience ……hospitalization………. . death Medication appropriateness may change over time n n n due to multiple conditions requiring medications decline in functional reserves of organs (frailty) medication changes result in new drug-interactions Recognizing polypharmacy is difficult to do n all care providers can contribute to identification
Prescribers do their best n n n n Use medicines that are familiar Use the lowest effective dose Anticipate medication interactions Be alert to ADRs Monitor therapy Avoid prescribing cascades Seek patient engagement in therapy Involve care givers as necessary
What could possibly go wrong?

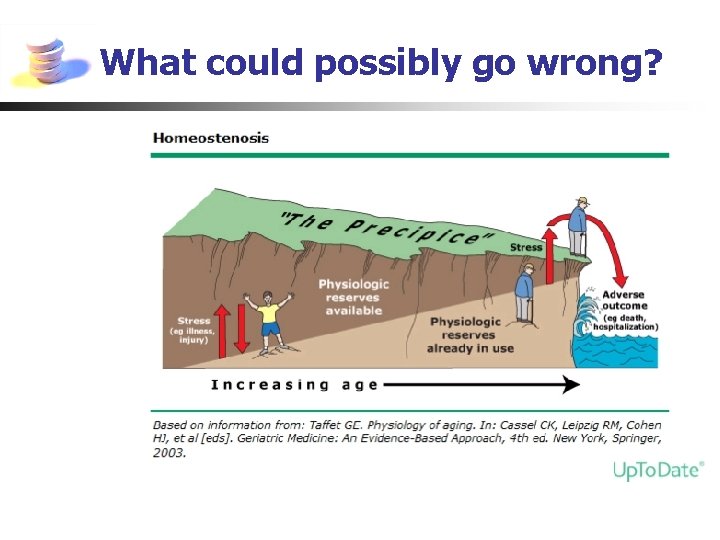
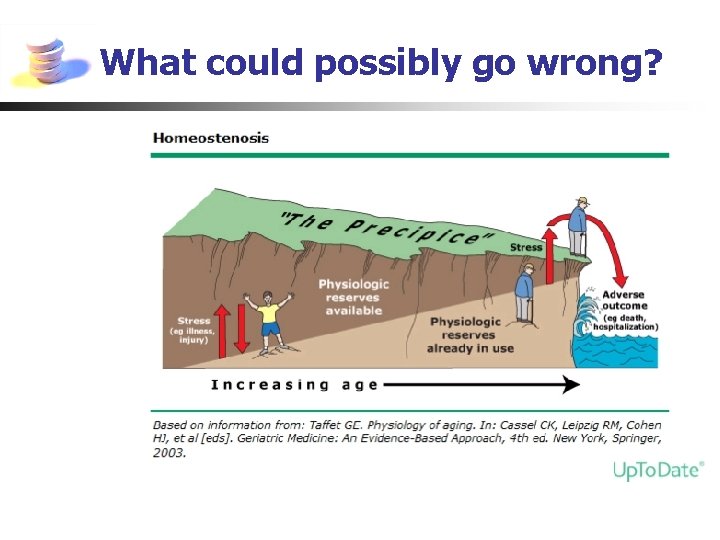
What could possibly go wrong? Multiple medical problems/Multiple medications + • • • weakness, fatigue, weight loss, impaired mobility, reduced strength compromised homeostatic mechanisms acute illness changes to medications Frailty = Increased risk of altered or harmful medication effects

Age-Related Changes in the Elderly Changes in physiology with aging: ↑body fat, ↓ body water , ↓ albumin, ↓ liver metabolism, ↓ renal func’n • • ∆ Pharmacokinetics ∆ Pharmacodynamics Absorption unaltered by age alone Distribution altered physiology Metabolism (liver) CYP 450 Excretion (kidney) Cr. Cl ∆ in receptor binding ↓ # of receptors & activity → Δ Drug efficacy → Δ Toxicity / ADRs Changes how the body acts on the drug Changes how the drug acts on the body

What could go wrong? n Guideline-based prescribing n n n Multi-system illness or frailty are not considered Focus is on starting. . . not stopping or reducing Safety ratio changes with age & multiple meds AGE n Benefit/Harm Benefit/ HARM Changing goals of care or ↓ life expectancy ADRs masquerade as normal aging Atypical presentation of disease or ADRs

Atypical or misleading presentation of disease
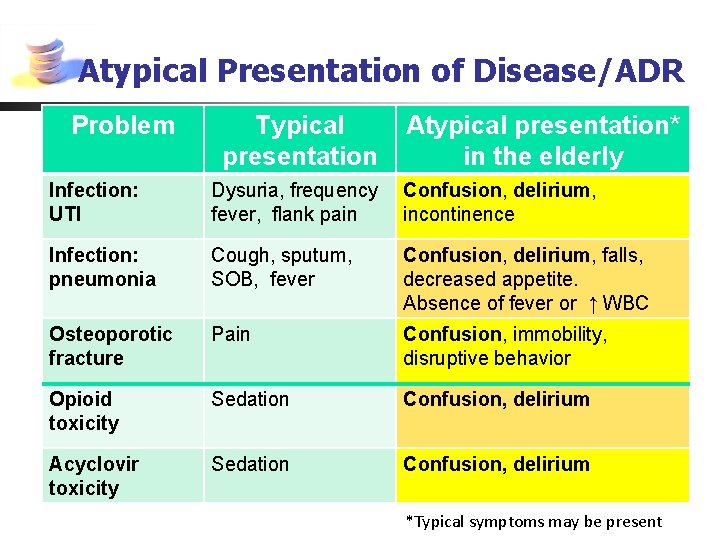
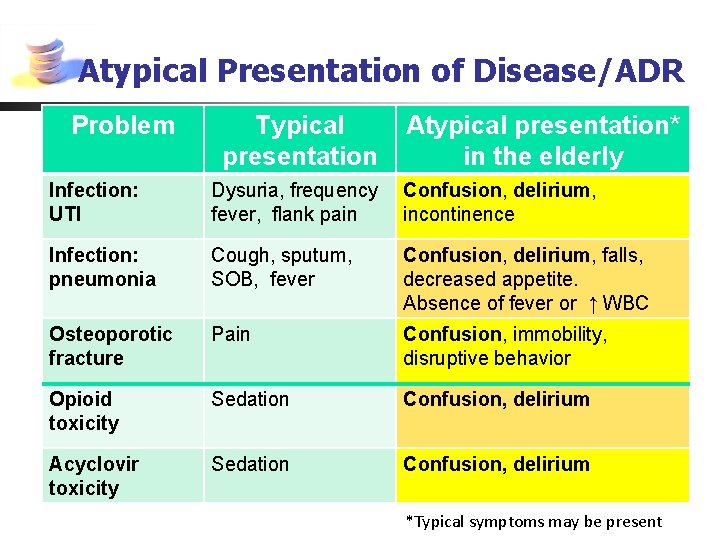
Atypical Presentation of Disease/ADR Problem Typical presentation Atypical presentation* in the elderly Infection: UTI Dysuria, frequency fever, flank pain Confusion, delirium, incontinence Infection: pneumonia Cough, sputum, SOB, fever Confusion, delirium, falls, decreased appetite. Absence of fever or ↑ WBC Osteoporotic fracture Pain Confusion, immobility, disruptive behavior Opioid toxicity Sedation Confusion, delirium Acyclovir toxicity Sedation Confusion, delirium *Typical symptoms may be present
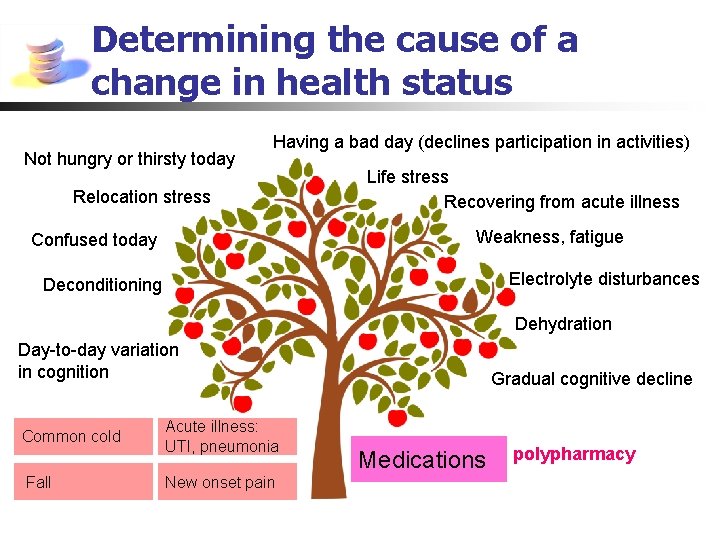
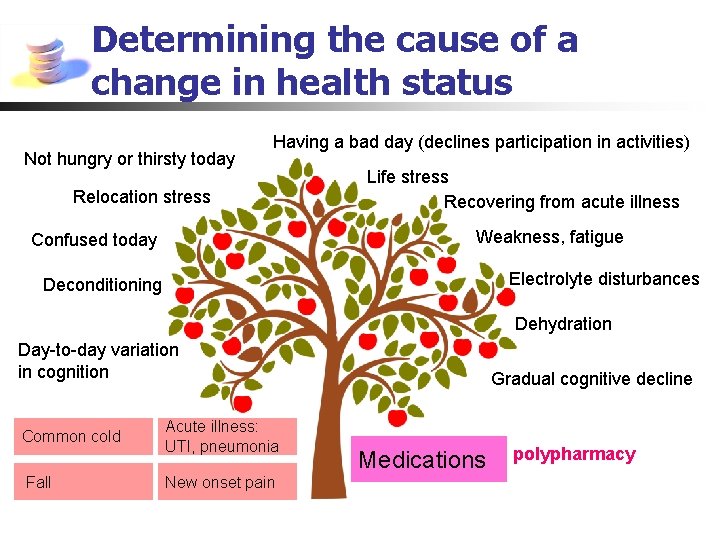
Determining the cause of a change in health status Not hungry or thirsty today Having a bad day (declines participation in activities) Relocation stress Life stress Recovering from acute illness Weakness, fatigue Confused today Electrolyte disturbances Deconditioning Dehydration Day-to-day variation in cognition Common cold Fall Acute illness: UTI, pneumonia New onset pain Gradual cognitive decline Medications polypharmacy

Key Points n n n Prescribing medication in the elderly is complex Elderly are at high risk of adverse drug reactions Identifying ADRs requires vigilance n n n Appreciating the impact of drugs on physiology Factoring in decline in physiologic reserves Benefit/Harm ratio can flip in an instant or gradually over time
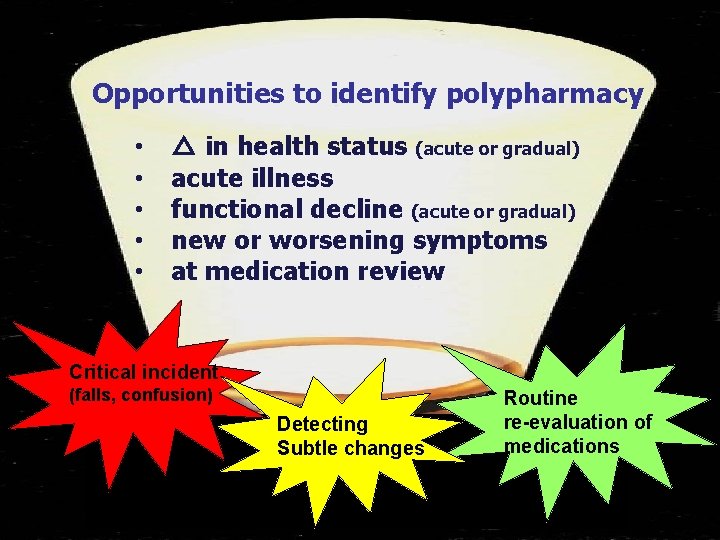
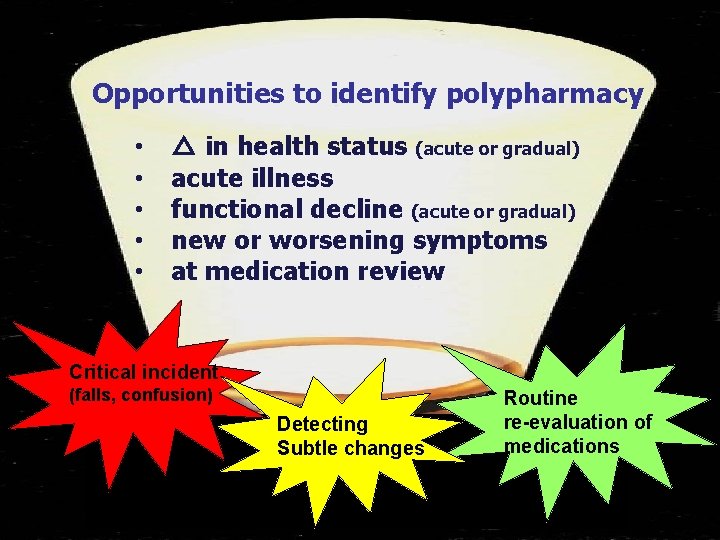
Opportunities to identify polypharmacy • • • △ in health status (acute or gradual) acute illness functional decline (acute or gradual) new or worsening symptoms at medication review Critical incident (falls, confusion) Detecting Subtle changes Routine re-evaluation of medications

What help is available to identify polypharmacy? Multiple conditions requiring multiple meds Benefits Harms Less Toxic More Toxic Assessment Tools: Explicit Criteria (PIM): Beers, STOPP, Mc. Leod Implicit Criteria: individualized assessment & clinical judgment, MAI, ARMOR, No TEARS
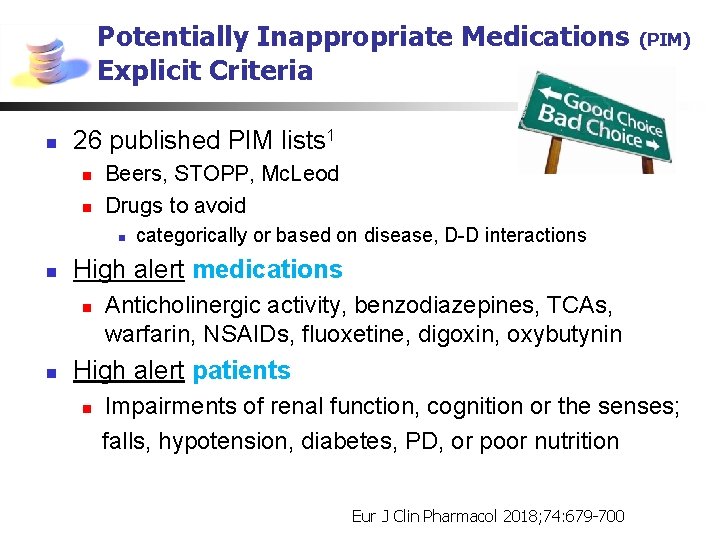
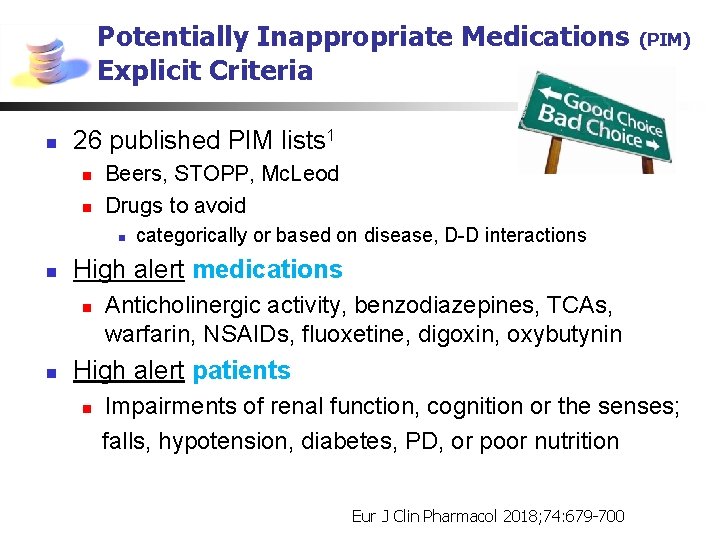
Potentially Inappropriate Medications Explicit Criteria n 26 published PIM lists 1 n n Beers, STOPP, Mc. Leod Drugs to avoid n n categorically or based on disease, D-D interactions High alert medications n n (PIM) Anticholinergic activity, benzodiazepines, TCAs, warfarin, NSAIDs, fluoxetine, digoxin, oxybutynin High alert patients n Impairments of renal function, cognition or the senses; falls, hypotension, diabetes, PD, or poor nutrition Eur J Clin Pharmacol 2018; 74: 679 -700

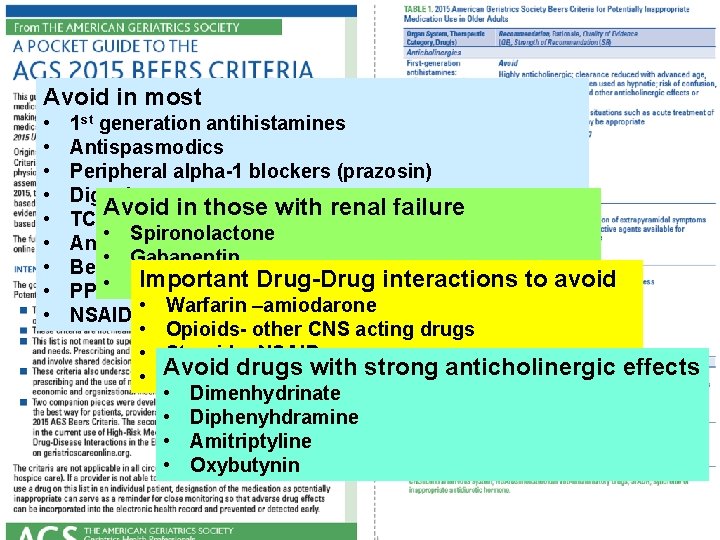
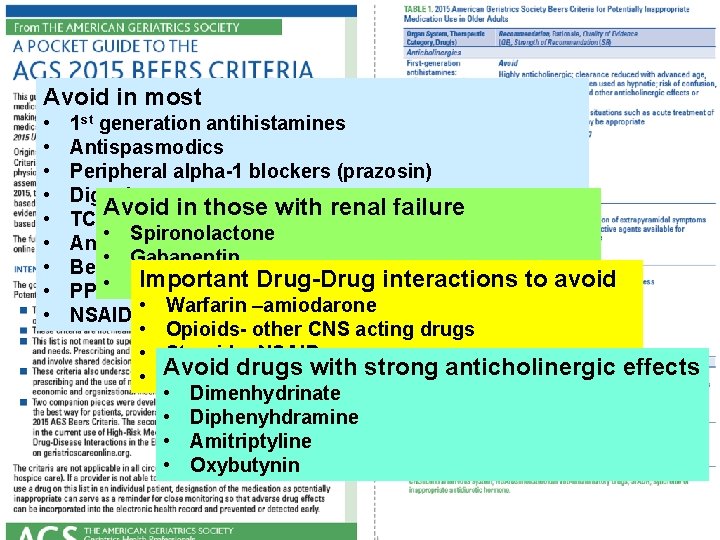
Avoid in most • • • 1 st generation antihistamines Antispasmodics Peripheral alpha-1 blockers (prazosin) Digoxin Avoid in those with renal failure TCAs (amitriptyline) • Spironolactone Antipsychotics for BPSD • Gabapentin Benzodiazepines Drug-Drug interactions to avoid RImportant anitidine PPI • long term –amiodarone NSAIDs • in. Warfarin CHF, renal failure • Opioids- other CNS acting drugs • Steroids- NSAIDs drugs with strong anticholinergic effects • Avoid Benzodiazepinesother CNS acting drugs • Dimenhydrinate • Diphenyhdramine • Amitriptyline • Oxybutynin
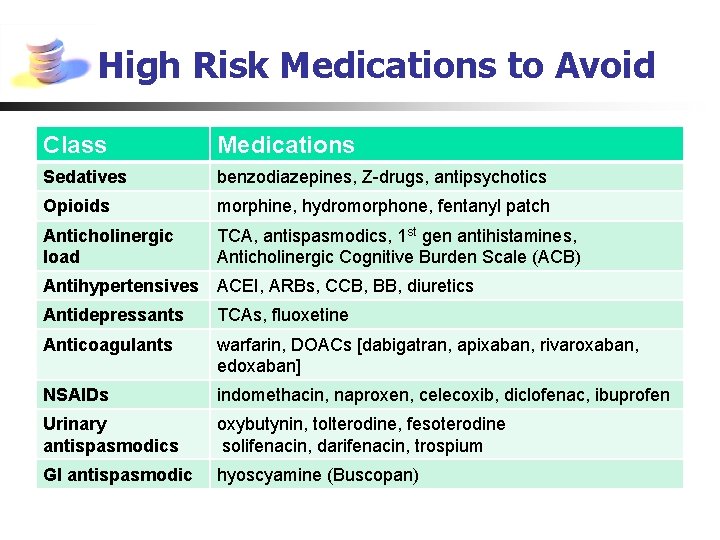
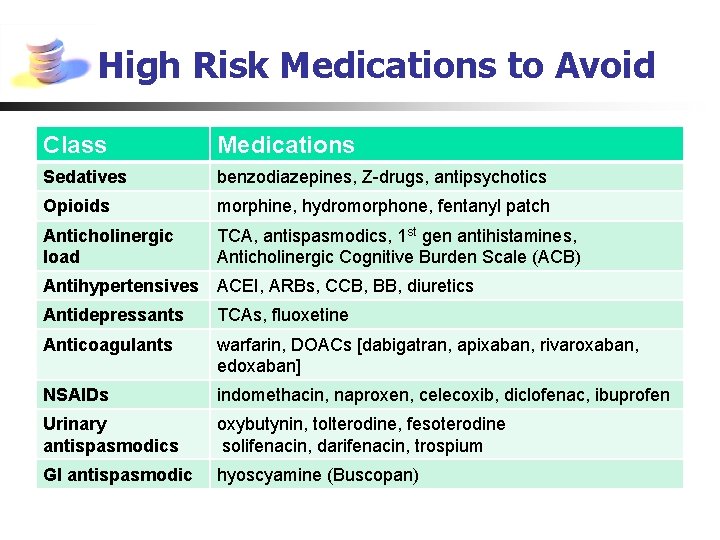
High Risk Medications to Avoid Class Medications Sedatives benzodiazepines, Z-drugs, antipsychotics Opioids morphine, hydromorphone, fentanyl patch Anticholinergic load TCA, antispasmodics, 1 st gen antihistamines, Anticholinergic Cognitive Burden Scale (ACB) Antihypertensives ACEI, ARBs, CCB, BB, diuretics Antidepressants TCAs, fluoxetine Anticoagulants warfarin, DOACs [dabigatran, apixaban, rivaroxaban, edoxaban] NSAIDs indomethacin, naproxen, celecoxib, diclofenac, ibuprofen Urinary antispasmodics oxybutynin, tolterodine, fesoterodine solifenacin, darifenacin, trospium GI antispasmodic hyoscyamine (Buscopan)
High Risk Medications to Avoid Class Medications Sedatives benzodiazepines, Z-drugs, antipsychotics Opioids morphine, hydromorphone, fentanyl patch Anticholinergic load TCA, antispasmodics, 1 st gen antihistamines, Anticholinergic Cognitive Burden Scale (ACB) Antihypertensives ACEI, ARBs, CCB, BB, diuretics Antidepressants TCAs, fluoxetine Anticoagulants warfarin, DOACs [dabigatran, apixaban, rivaroxaban, edoxaban] NSAIDs indomethacin, naproxen, celecoxib, diclofenac, ibuprofen Urinary antispasmodics oxybutynin, tolterodine, fesoterodine solifenacin, darifenacin, trospium GI antispasmodic hyoscyamine (Buscopan)
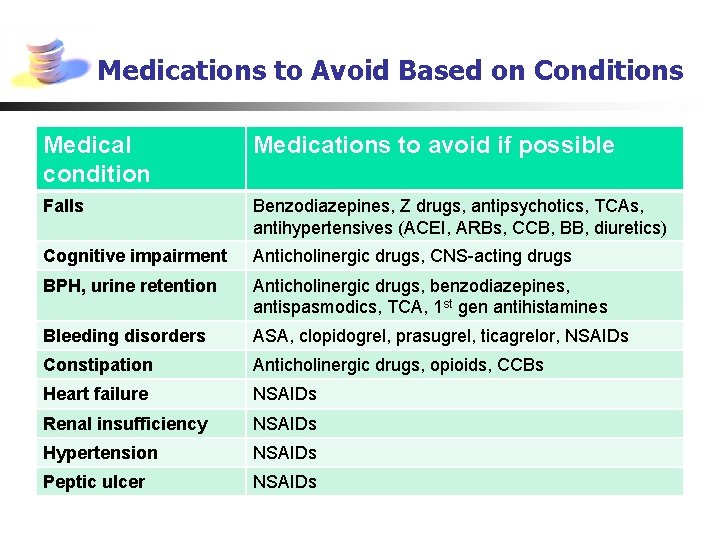
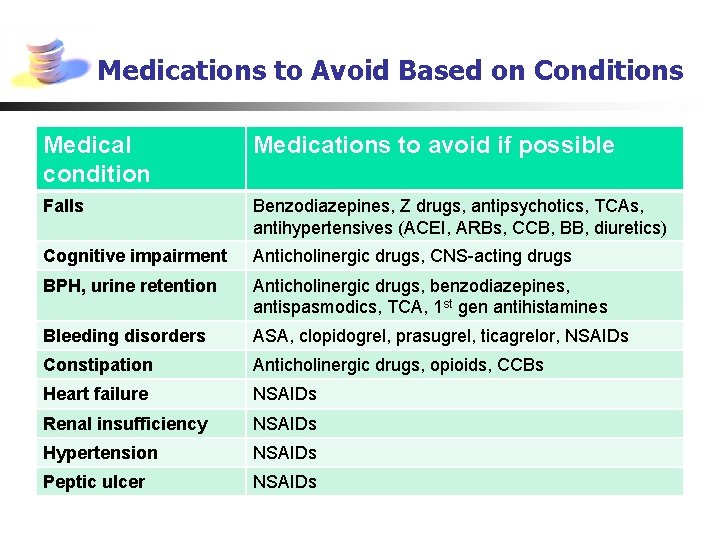
Medications to Avoid Based on Conditions Medical condition Medications to avoid if possible Falls Benzodiazepines, Z drugs, antipsychotics, TCAs, antihypertensives (ACEI, ARBs, CCB, BB, diuretics) Cognitive impairment Anticholinergic drugs, CNS-acting drugs BPH, urine retention Anticholinergic drugs, benzodiazepines, antispasmodics, TCA, 1 st gen antihistamines Bleeding disorders ASA, clopidogrel, prasugrel, ticagrelor, NSAIDs Constipation Anticholinergic drugs, opioids, CCBs Heart failure NSAIDs Renal insufficiency NSAIDs Hypertension NSAIDs Peptic ulcer NSAIDs
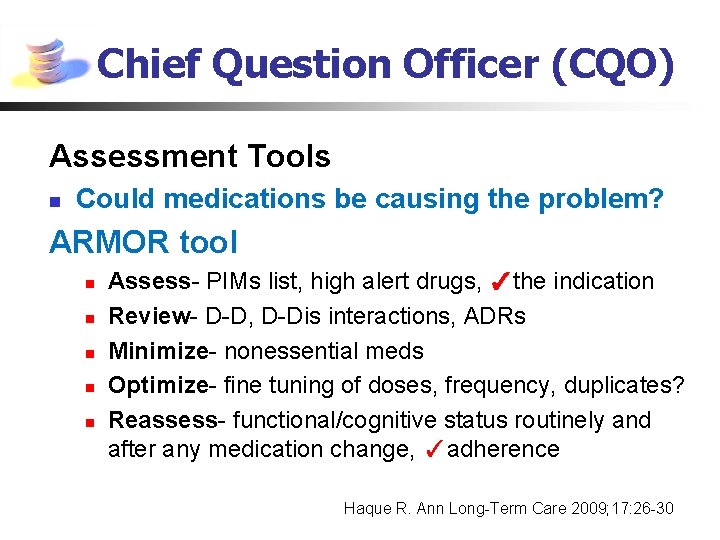
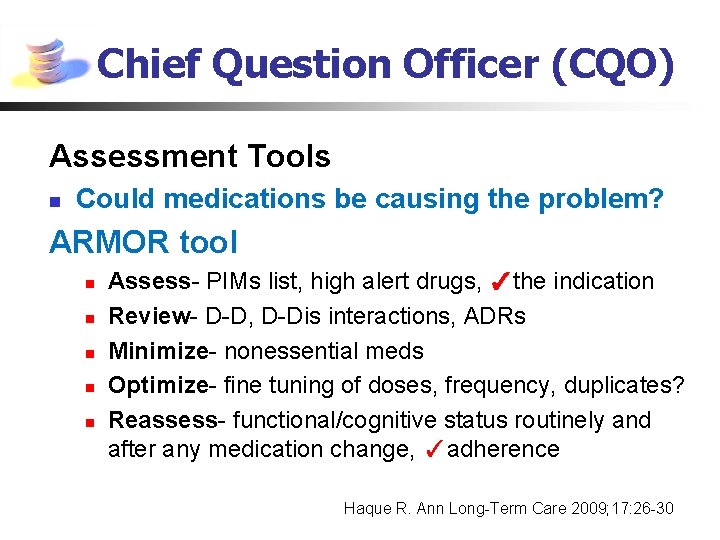
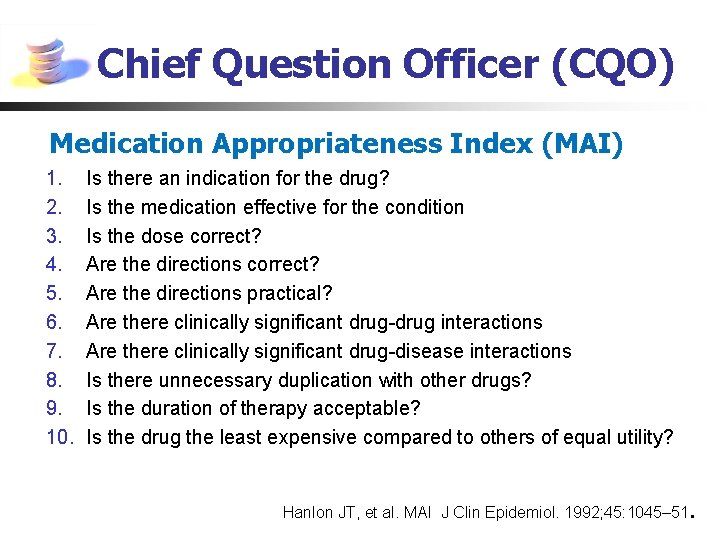
Chief Question Officer (CQO) Assessment Tools n Could medications be causing the problem? ARMOR tool n n n Assess- PIMs list, high alert drugs, ✓the indication Review- D-D, D-Dis interactions, ADRs Minimize- nonessential meds Optimize- fine tuning of doses, frequency, duplicates? Reassess- functional/cognitive status routinely and after any medication change, ✓adherence Haque R. Ann Long-Term Care 2009; 17: 26 -30
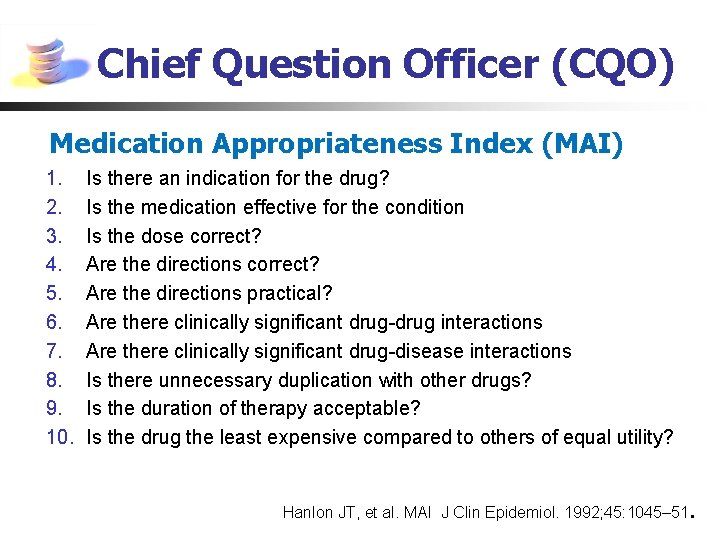
Chief Question Officer (CQO) Medication Appropriateness Index (MAI) 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Is there an indication for the drug? Is the medication effective for the condition Is the dose correct? Are the directions practical? Are there clinically significant drug-drug interactions Are there clinically significant drug-disease interactions Is there unnecessary duplication with other drugs? Is the duration of therapy acceptable? Is the drug the least expensive compared to others of equal utility? Hanlon JT, et al. MAI J Clin Epidemiol. 1992; 45: 1045– 51.
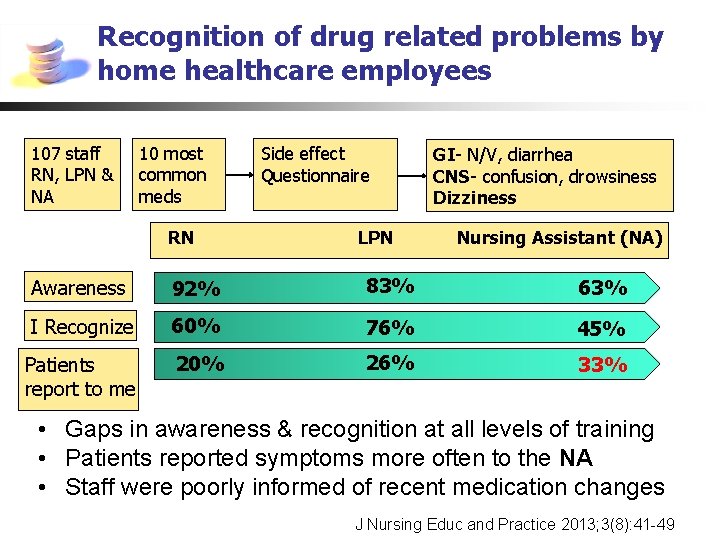
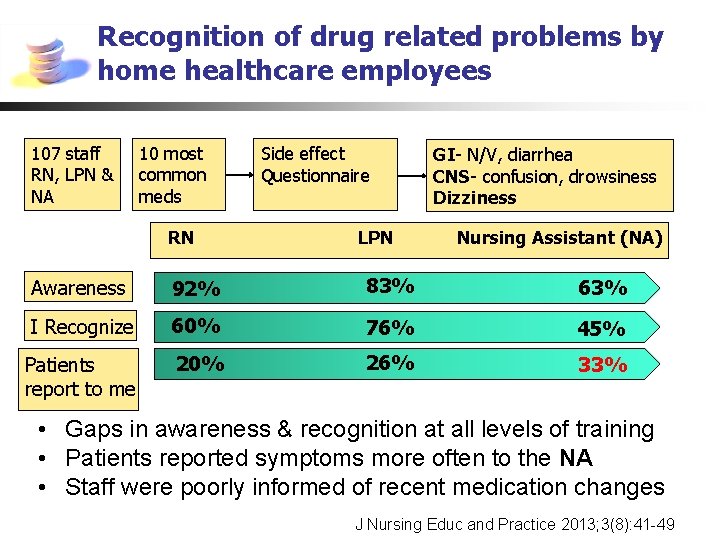
Recognition of drug related problems by home healthcare employees 107 staff RN, LPN & NA 10 most common meds RN Side effect Questionnaire LPN GI- N/V, diarrhea CNS- confusion, drowsiness Dizziness Nursing Assistant (NA) Awareness 92% 83% 63% I Recognize 60% 76% 45% Patients report to me 20% 26% 33% • Gaps in awareness & recognition at all levels of training • Patients reported symptoms more often to the NA • Staff were poorly informed of recent medication changes J Nursing Educ and Practice 2013; 3(8): 41 -49
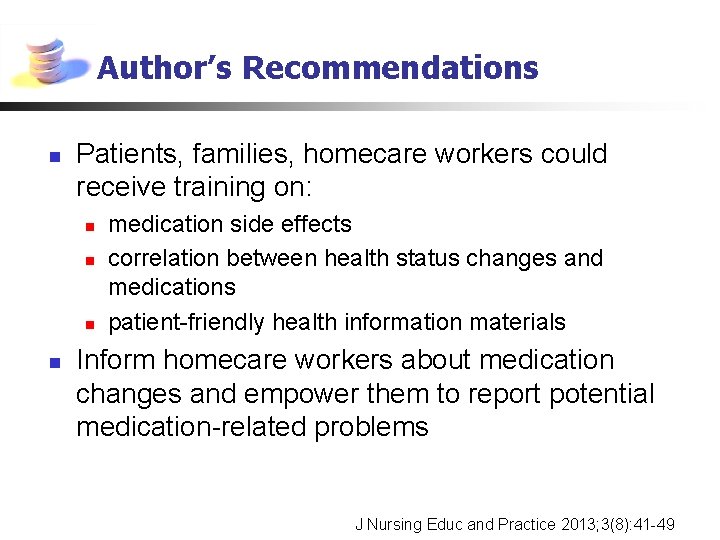
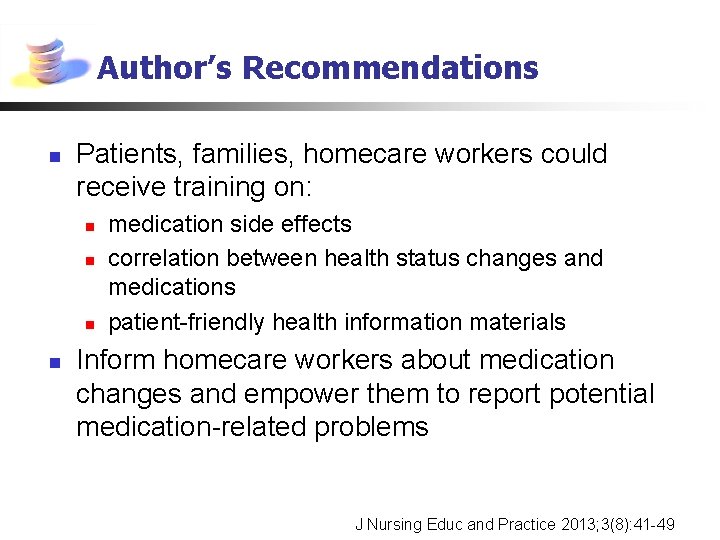
Author’s Recommendations n Patients, families, homecare workers could receive training on: n n medication side effects correlation between health status changes and medications patient-friendly health information materials Inform homecare workers about medication changes and empower them to report potential medication-related problems J Nursing Educ and Practice 2013; 3(8): 41 -49

Practical Guide to Stopping Medication in the Elderly Recognize the need to stop a medicine A general guide to tapering medicine Reduce or stop one medicine at a time Halve the dose. At the next scheduled visit review progress, then either: • Maintain (at half dose) • Continue to taper (e. g. quarter dose) • Stop Taper medicine when appropriate Check for benefit or harm after each medicine has been stopped Notes: • With the person’s consent • View the discontinuation process as a trial • Time taken to taper may vary from days to weeks to months • If symptoms worsen, may need to reinstate the medication Drugs that generally require a cautious stepwise withdrawal and/or specialist advice: Opioids/antidepressants/antipsychotics/anticonvulsants/centrally acting antihypertensives/ corticosteroids/hypnotics and tranquilizers Source: All Wales Medicines Strategy Group; Polypharmacy: Guidance for Prescribing
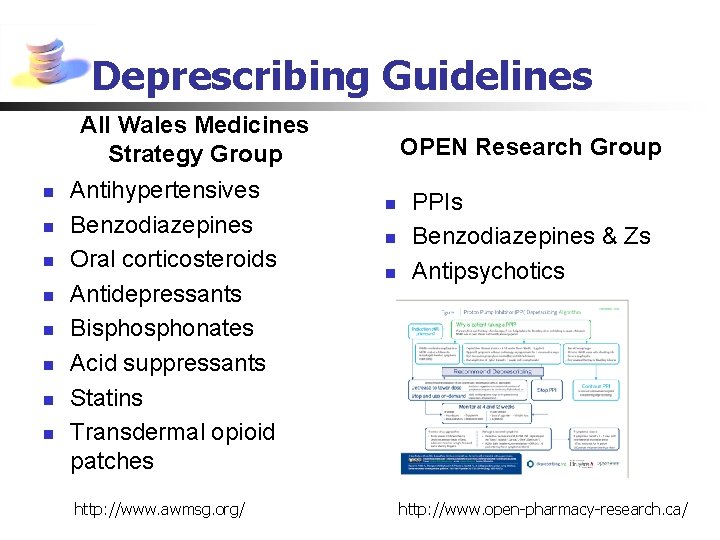
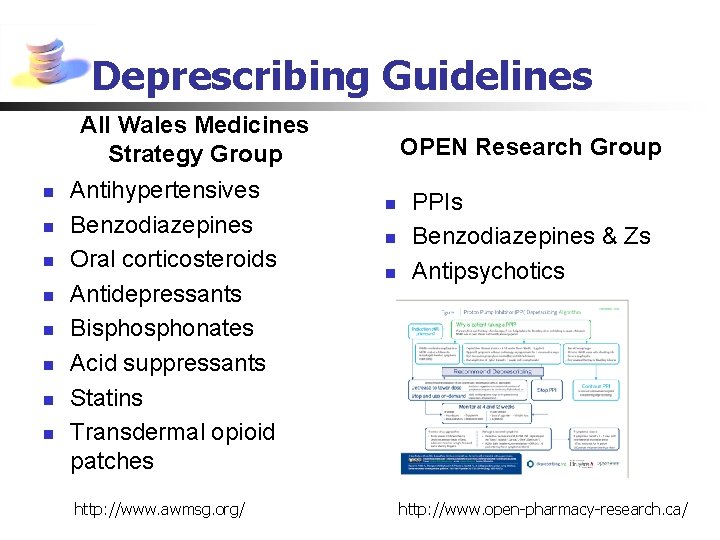
Deprescribing Guidelines All Wales Medicines Strategy Group n n n n Antihypertensives Benzodiazepines Oral corticosteroids Antidepressants Bisphonates Acid suppressants Statins Transdermal opioid patches http: //www. awmsg. org/ OPEN Research Group n n n PPIs Benzodiazepines & Zs Antipsychotics http: //www. open-pharmacy-research. ca/
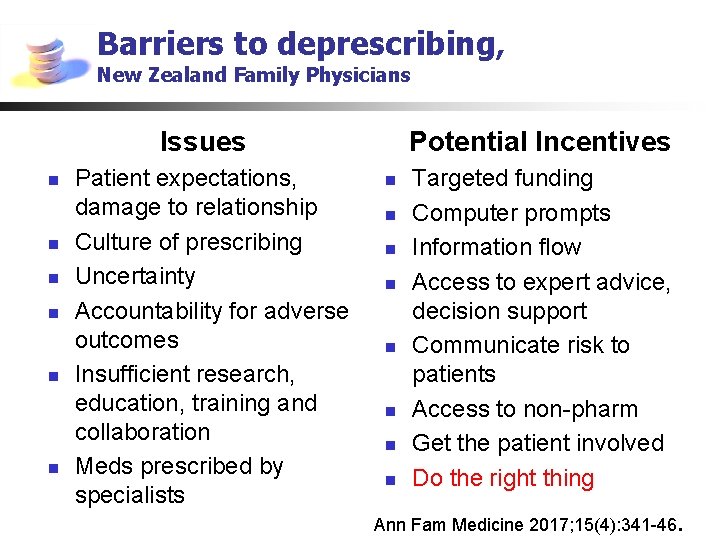
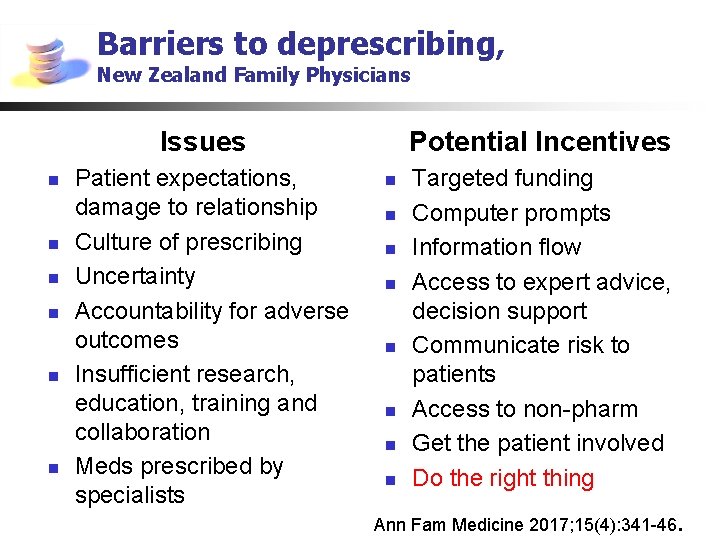
Barriers to deprescribing, New Zealand Family Physicians Issues n n n Patient expectations, damage to relationship Culture of prescribing Uncertainty Accountability for adverse outcomes Insufficient research, education, training and collaboration Meds prescribed by specialists Potential Incentives n n n n Targeted funding Computer prompts Information flow Access to expert advice, decision support Communicate risk to patients Access to non-pharm Get the patient involved Do the right thing Ann Fam Medicine 2017; 15(4): 341 -46.

Resources n Meds. Check- Ontario pharmacists, public access n n n 3 chronic meds, yearly or on request by MD, NP Choosing Wisely- lists of dos and don’ts Shared. Care-BC Physicians, med decision support tools http: //www. sharedcarebc. ca/ “ You Decide” n SADMANS- meds to hold on sick days Telehealth Ontario- patients OPA- Drug Information Service- for pharmacists n Geri. Med. Risk- n n high level consult service for HCP, Mc. Master U https: //www. gerimedrisk. com/partners/
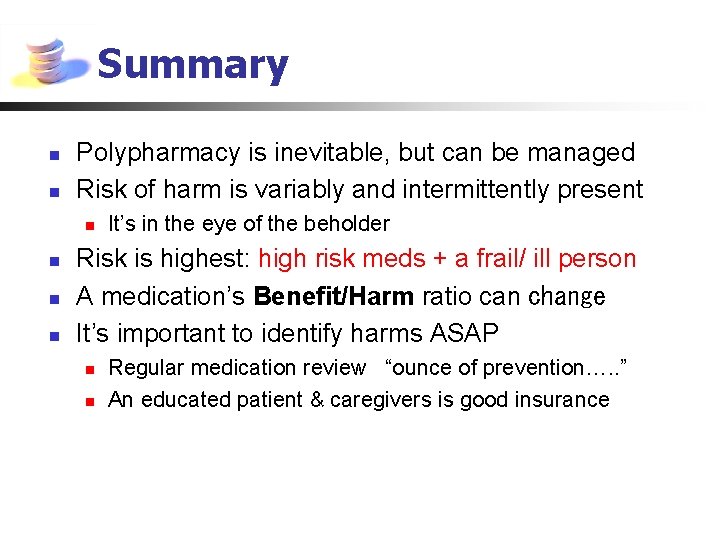
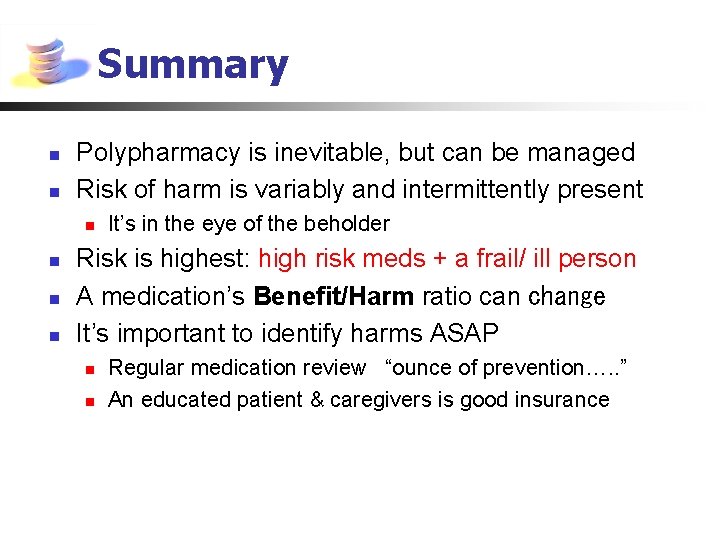
Summary n n Polypharmacy is inevitable, but can be managed Risk of harm is variably and intermittently present n n It’s in the eye of the beholder Risk is highest: high risk meds + a frail/ ill person A medication’s Benefit/Harm ratio can change It’s important to identify harms ASAP n n Regular medication review “ounce of prevention…. . ” An educated patient & caregivers is good insurance
 Life is older older than the trees
Life is older older than the trees Older adults
Older adults Mental health and older adults
Mental health and older adults Covids older adults
Covids older adults Altered cognition in older adults is commonly attributed to
Altered cognition in older adults is commonly attributed to Older adults mental health
Older adults mental health Shingles older adults
Shingles older adults Dynamic stretching for older adults
Dynamic stretching for older adults Mental health and older adults
Mental health and older adults Pf
Pf Every eye is an eye
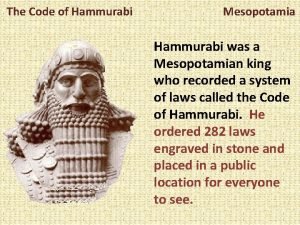
Every eye is an eye Hammurabi
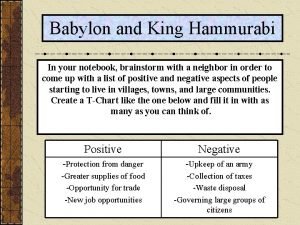
Hammurabi Code of hammurabi activity
Code of hammurabi activity Birds eye view examples
Birds eye view examples Blue eyes genetics
Blue eyes genetics An eye for an eye a tooth for a tooth sister act
An eye for an eye a tooth for a tooth sister act Hammurabi code eye for an eye
Hammurabi code eye for an eye An eye for an eye meaning
An eye for an eye meaning Does the needle ever wink its eye
Does the needle ever wink its eye Module 11 studying the brain
Module 11 studying the brain Late adulthood mental development
Late adulthood mental development Superlativo de trabajador
Superlativo de trabajador Sos spelling for older students
Sos spelling for older students The brother of the prodigal son
The brother of the prodigal son Syncope in the older patient is
Syncope in the older patient is Growing older poem
Growing older poem Future medical
Future medical Older individuals who are blind program
Older individuals who are blind program The virtues of growing older
The virtues of growing older Bartosz older owl
Bartosz older owl My rotten redheaded older brother
My rotten redheaded older brother Td st annes
Td st annes Pseudostratified vs simple columnar
Pseudostratified vs simple columnar Hoa/received/letter/her friend nien/today
Hoa/received/letter/her friend nien/today As people grow older
As people grow older Web accessibility for older users
Web accessibility for older users Patricia polacco family tree
Patricia polacco family tree Sos spelling for older students
Sos spelling for older students Ajayan is ten years older than vijayan
Ajayan is ten years older than vijayan Dq98 form
Dq98 form The breadwinner mother character traits
The breadwinner mother character traits Moses older sister
Moses older sister