Physician Information Regarding Organ Eye and Tissue Donation
- Slides: 67
Physician Information Regarding Organ, Eye and Tissue Donation Release Date: April 1, 2013 * Expiration Date: April 1, 2016 Jointly sponsored by Legacy Donor Foundation and Tulane University Health Sciences Center, Center for Continuing Education We would like to thank the Louisiana Office of Motor Vehicles for their educational grant in support of this educational activity © 2013, The Legacy Donor Foundation
Who We Are Legacy Donor Foundation - a 501(c)3 nonprofit organization whose mission is to save and heal lives by inspiring Louisiana residents to register as organ, eye and tissue donors Tulane University Health Sciences Center, Center for Continuing Education whose mission is dedicated to offering educational activities that provide healthcare professionals access to a system of lifelong learning © 2013, The Legacy Donor Foundation
CME Information STATEMENT OF NEED There is a disparity between the need for organs for transplantation (the waiting list), the number of transplants performed and the actual number of organ donors. While 90% of Americans say they support organ donation, only 35% of licensed drivers nationwide have registered to become an organ, eye and tissue donors. This activity is designed to provide the healthcare provider with increased knowledge and improved attitudes about organ donation in order to improve their competence in answering questions and initiating discussions about organ donation with their patients. LEARNER OBJECTIVES At the conclusion of this activity, the participant should be better able to • Dispel myths and misconceptions related to organ and tissue donation • Identify transplantation as an accepted treatment for specific diseases • Confidently initiate conversations with & answer questions from patients regarding organ donation TARGET AUDIENCE Physicians and healthcare professionals in all specialties © 2013, The Legacy Donor Foundation
ACCREDITATION This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education through the joint sponsorship of the Legacy Donor Foundation and Tulane University Health Sciences Center is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. DESIGNATION Tulane University Health Sciences Center designates this educational activity for a maximum of --AMA PRA Category 1 Credits TM. Physicians should only claim credit commensurate with the extent of their participation in the activity. Tulane University Health Sciences Center and Legacy Donor Foundation present this activity for educational purposes only and do not endorse any product, content of presentation or exhibit. Participants are expected to utilize their own expertise and judgment while engaged in the practice of medicine. The content of the presentations is provided solely by individuals who have been selected because of their recognized expertise. COMPETENCIES This activity addresses components of the six competencies identified by the ABMS (Medical knowledge, Patient care, Interpersonal & communication skills, Professionalism, Practice-based learning & improvement, Systems-based practice), as well as the competencies identified by the IOM (Provide patient-centered care; Work in interdisciplinary teams, Employ evidence-based practice, Apply quality improvement; and Utilize informatics). © 2013, The Legacy Donor Foundation
PRIVACY POLICY It is the policy of the Center for Continuing Education at Tulane University Health Sciences Center and the Legacy Donor Foundation that personal information of CME activities will be collected only to the extent necessary to provide the service or benefit desired. Only appropriate information will be collected and can be available to be reviewed by the individual providing the information. © 2013, The Legacy Donor Foundation
Disclosures It is the policy of the Center for Continuing Education at Tulane University Health Sciences Center to plan and implement all of its educational activities in accordance with the ACCME's Essential Areas and Policies to ensure balance, independence, objectivity and scientific rigor. In accordance with the ACCME’s Standards for Commercial Support, everyone who is in a position to control the content of an educational activity certified for AMA PRA Category 1 Credit TM is required to disclose all financial relationships with any commercial interests within the past 12 months that creates a real or apparent conflict of interest. Individuals who do not disclose are disqualified from participating in an activity certified for AMA PRA Category 1 Credit TM. Individuals with potential for influence or control of content include planners and planning committee members, authors, teachers, educational activity directors, educational partners, and others who participate, e. g. facilitators and moderators. This disclosure pertains to relationships with pharmaceutical companies, biomedical device manufacturers or other corporations whose products or services are related to the subject matter of the presentation topic. Any real or apparent conflicts of interest related to the content of the presentations must be resolved prior to the educational activity. Disclosure of off-label, experimental or investigational use of drugs or devices must also be made known to the audience. Listed below is information disclosed by individuals who were involved in the development of this presentation. Any real or apparent conflicts of interest related to the content or their role have been resolved. Last Name Buras Epperson Forsyth Guarisco Hands Heintz Jobson-Wolfe Labadot. Nicole Oltmann Slakey Weimer First Name Role Disclosure William Planner, Southern Eye Bank Nothing to disclose Melinda Director, Tulane CME Nothing to disclose Ouida Evaluation, Tulane CME Nothing to disclose Whitney Planner, Legacy Donor Foundation Nothing to disclose Ana Planner, Author , Legacy Donor Foundation Nothing to disclose Kirsten Planner, Author , LOPA Nothing to disclose Anita Program Coord. , Tulane CME Nothing to disclose Planner, Legacy Donor Foundation Nothing to disclose Colleen Planner, Southern Eye Bank Nothing to disclose Douglas Tulane Faculty Liaison Grants: Covidien, Novartis, Nycomed, Doctors Compan Foundation, Valley Lab, Dept of State Jeanette Planner, Author , Legacy Donor Fndn Nothing to disclose Steven Chair, Tulane CME Advisory Cmte Nothing to disclose NOTE: All Tulane CME staff have documented that they have nothing to disclose and no conflicts of interest to resolve. © 2013, The Legacy Donor Foundation
Sections • • How to take the course Purpose Why you need to know about donation What you will learn - What are the myths you may encounter as a physician - History and Milestones - How a patient is listed on the transplant waiting list - What is considered when evaluating a potential donor - What is the criteria for donation - What are the tests that are done to determine brain death etc. - Who can authorize donation - Screening for donation - Legal aspects of transplantation - What is the consent process - Why discuss this with patients - How to register as a donor © 2013, The Legacy Donor Foundation
Purpose The goal of this program is to provide the proper tools to dispel myths and misconceptions related to donation, identify transplantation as an accepted treatment/cure for specific diseases, and allow physicians to confidently initiate conversations with, and answer questions from patients regarding organ, eye and tissue donation. © 2013, The Legacy Donor Foundation
Staggering Statistics • Nearly 117, 000 people are waiting for a life-saving organ transplant and almost 1, 800 are Louisiana residents • Approximately 19 people will die today while awaiting a life-saving transplant • Every 5 seconds someone goes blind • Every 13 minutes, another person is added to the waiting list • Only 2 -3% of all deaths have potential to be organ donors Sources: Donate Life America U. N. O. S. © 2013, The Legacy Donor Foundation
The Facts • Organ, eye and tissue donation are only an option after all life-saving measures have been taken • Anyone, regardless of age, race or medical history has the potential to be a donor • Organ, eye and tissue recovery is performed using surgical procedures, and the donor is treated with the utmost dignity and respect Sources: Donate Life America © 2013, The Legacy Donor Foundation
More Facts • All major religions support donation or regard it as an individual decision • It is illegal to buy or sell organs in the United States • It is illegal to distribute organs based on wealth, citizenship, or celebrity status • Donation will not prevent an open casket funeral Sources: Donate Life America © 2013, The Legacy Donor Foundation
One Donor Can… • • Save 9 lives Restore sight to 2 people Enhance the lives of 50 more Transplantation is a standard treatment option Sources: Donate Life America U. N. O. S. © 2013, The Legacy Donor Foundation
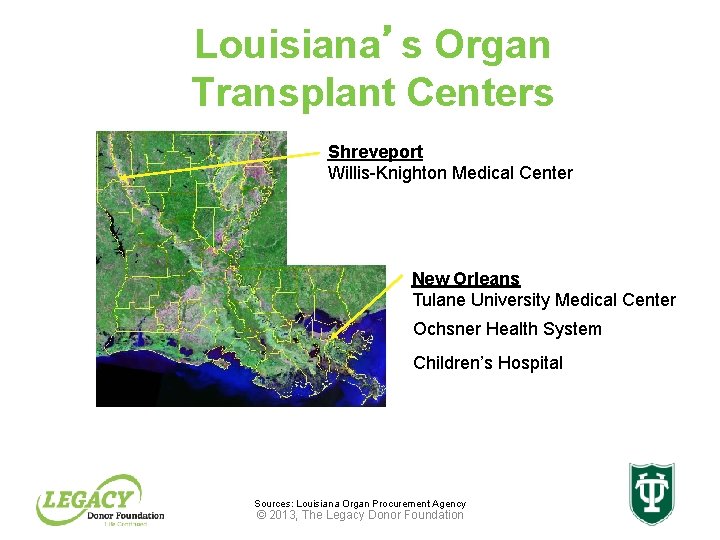
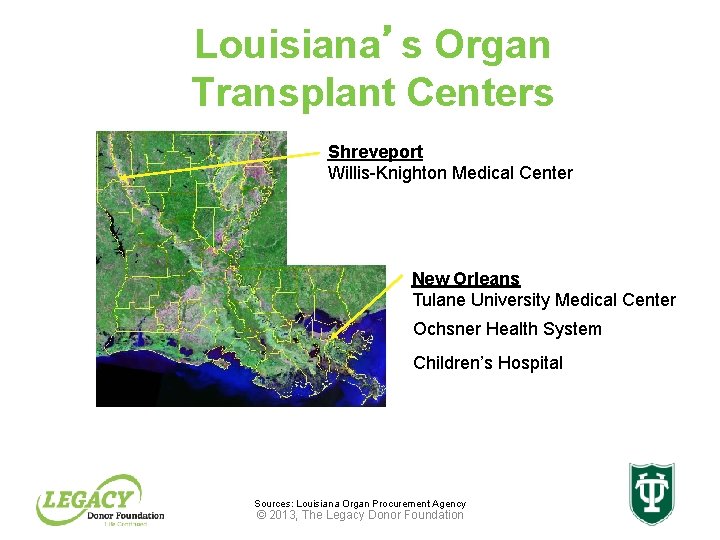
Louisiana’s Organ Transplant Centers Shreveport Willis-Knighton Medical Center New Orleans Tulane University Medical Center Ochsner Health System Children’s Hospital Sources: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
History: How this came about • The U. S. Congress established the Organ Procurement and Transplantation Network (OPTN) when it enacted the National Organ Transplant Act (NOTA) of 1984 • The act called for a unified transplant network to be operated by a private, non-profit organization under federal contract • Following further study and recommendations from a task force commissioned through NOTA, the U. S. Department of Health and Human Services (HHS) solicited proposals in 1986 for the operation of the OPTN • The United Network for Organ Sharing (UNOS) was awarded the initial OPTN contract on September 30, 1986 Sources: U. N. O. S. © 2013, The Legacy Donor Foundation
Transplant Program Regulation • The Organ Procurement and Transplantation Network (OPTN) is the unified transplant network established by the United States Congress under the National Organ Transplant Act (NOTA) of 1984 • The act called for the network to be operated by a private, non-profit organization under federal contract • The primary goals of the OPTN are to: - Increase the effectiveness and efficiency of organ sharing and equity in the national system of organ allocation - Increase the supply of donated organs available for transplantation • The United Network for Organ Sharing (UNOS), administers the OPTN under contract with the Health Resources and Services Administration (HRSA) Source: U. N. O. S. © 2013, The Legacy Donor Foundation
Transplant Program Regulation Continued The U. S. Organ Procurement and Transplantation Network (OPTN) responsibilities include: • Facilitating the organ matching and placement process • Developing consensus based policies and procedures for organ recovery, distribution (allocation), and transportation • Collecting and managing scientific data about organ donation and transplantation • Providing data • Maintains the nation's organ transplant waiting list and recipient/donor organ characteristics • Providing professional and public education about donation and transplantation Source: U. N. O. S. © 2013, The Legacy Donor Foundation
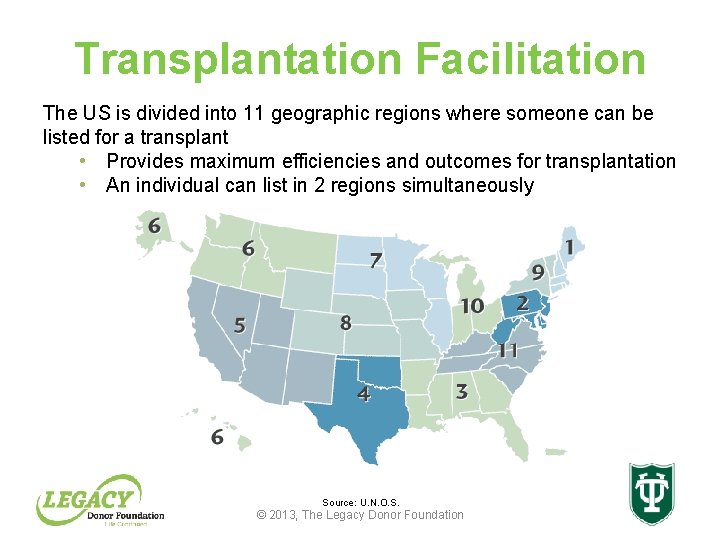
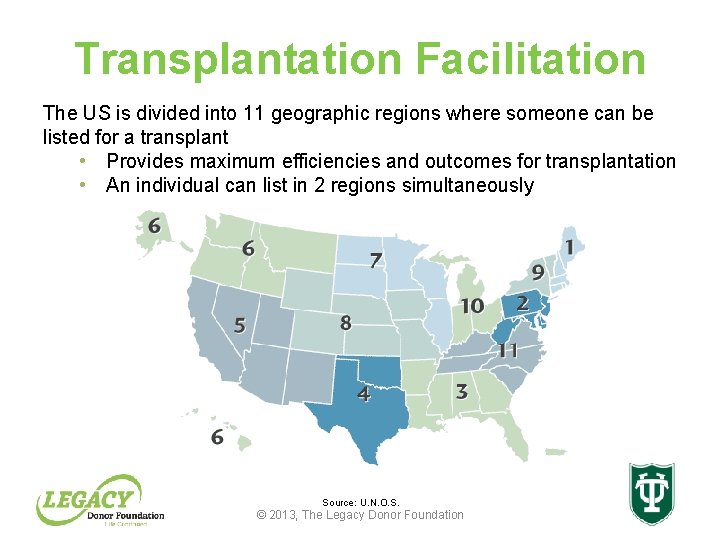
Transplantation Facilitation The US is divided into 11 geographic regions where someone can be listed for a transplant • Provides maximum efficiencies and outcomes for transplantation • An individual can list in 2 regions simultaneously Source: U. N. O. S. © 2013, The Legacy Donor Foundation
How does the process work? • When organs are donated, a complex process begins • UNOS maintains a centralized computer network, UNet. SM, which links all organ procurement organizations (OPOs) and transplant centers • Donation and transplant professionals can access this computer network 24 hours a day, seven days a week Source: U. N. O. S. © 2013, The Legacy Donor Foundation
Transplantation Milestones • • 1954 1966 1967 1968 • 1977 • • 1981 1983 1984 1986 First successful kidney transplant performed First simultaneous kidney/pancreas transplant performed First successful liver transplant performed First successful isolated pancreas transplant performed First successful heart transplant performed The first computer-based organ matching system, is implemented dubbed the "United Network for Organ Sharing” First successful heart-lung transplant performed First successful single-lung transplant performed National Organ Transplant Act (NOTA) passed First successful double-lung transplant performed Source: U. N. O. S. © 2013, The Legacy Donor Foundation
Transplantation Milestones, Continued • • • 1987 First successful intestinal transplant performed 1988 First split-liver transplant performed 1989 First successful living donor liver transplant performed 1990 First successful living donor lung transplant performed 1992 UNOS helps found Donate Life America to build public support for organ donation • 1998 First successful adult-to-adult living donor liver transplant performed • 1999 UNOS launches UNetsm, a secure, Internet-based transplant information database system for all organ matching and management of transplant data • 2006 UNOS launches Donor. Netsm, a secure, Internet-based system in which organ procurement coordinators send out offers of newly donated organs to transplant hospitals with compatible candidates Source: U. N. O. S. © 2013, The Legacy Donor Foundation
Transplant Centers Requirements • Be members of UNOS (United Network for Organ Sharing) • Have a UNOS approved HLA lab • Have a signed contract with an OPO (Organ Procurement Organization) • Have a UNOS qualified surgeon Sources: U. N. O. S Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Waiting List • Overseen by UNOS • Allocation algorithm places organs based on: – Organ specific criteria – Blood type – Size (height and weight) – HLA typing – Geographic proximity (allocated geographically by region) – Degree of medical illness – Length of time on the waiting list Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Candidate Selection • Extensive medical, social, psychological and financial evaluation • Interdisciplinary decision • Allocation of scarce resources – Individual patient/waiting list – Responsibility to donor family – Societal responsibility to ensure best utility – Life saving/life enhancing Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Acceptance Criteria for Organ Transplant • • End stage organ disease No alternate treatment options Life threatening complications Compromised quality of life No contraindications to organ transplant Healthy except for diseased organ Ability to comply with follow up regimen Emotionally stable, motivated, compliant Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Organ Procurement Organization (OPO) • Regional, non-profit organizations responsible for coordinating organ donations at hospitals throughout the U. S. ; all OPOs are designated by the Federal Government to serve specific regions • In the state of Louisiana there is one OPO, Louisiana Organ Procurement Agency (LOPA) that coordinates the recovery of organs • All organ recovery and placement of deceased donors must be coordinated through LOPA Sources: U. N. O. S. Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Role of the Organ Procurement Organization OPO’s are responsible for coordinating the entire donation process – Receive referrals on hospital deaths – Evaluate potential donors for suitability – Approach families – Coordinate recovery – Oversee allocation of organs – Provide aftercare services for donor family Louisiana Organ Procurement Agency © 2013, The Legacy Source: Donor Foundation
Sources of Organs • Deceased – Donation after brain death – Donation after circulatory death (DCD) • Living – Living related – Living unrelated – Good Samaritan, altruistic donations Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Anatomical Donations • Generally, bodies are acceptable for anatomical donations to a specific medical institution if organs, eyes, or tissue have been donated for transplantation • This may vary by region, for individual questions, please check with the institution: – Anatomy Dept - LSU (New Orleans) - (504) 568 -2165 – Anatomy Dept – LSU (Shreveport) - (318) 675 -5320 – Anatomy Dept - Tulane University - (504) 988 -5255 Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Ideal Donor • Young (< 50 yrs) • Short hospital stay • Cause of death – acute injury/illness • No down time, minimal pressors, good oxygenation • No injury to solid organs • No infection • Negative serologies Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Brain Death Potential causes of brain death: – Intracranial hemorrhage – Cerebral anoxia – Acute neurological or neurosurgical trauma – Drug overdose – Metabolic disorder – Primary brain tumor • Mechanical support is provided in order to maintain the viability of organs for transplant • Brain dead patients can donate organs, eyes and tissues Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Brain Death Continued • The declaration of brain death requires neurological exams, which document the irreversible cessation of activity of both the brain and the brain stem • If donation is to occur, two physicians, licensed in Louisiana, must declare the patient brain dead. • They cannot be associated with the transplant team Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Establishing Brain Death The neurological criteria used to establish brain death are: – No pupil response to light – No corneal reflex – No response to pain – No cough or gag reflex – No response to cold caloric stimulus – No ability to breathe on their own (apnea test) – In some cases, an additional confirmatory test is conducted such as a cerebral angiogram or EEG Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Role of the Coroner • The duty of the coroner is to ensure that organ and tissue recovery does not interfere with the investigation leading to the determination of death • Most coroners are supportive of organ and tissue donation, and will cooperate in offering this option to a grieving family • The hospital must report the death to the coroner and LOPA will obtain clearance for donation © 2013, The Legacy Donor Foundation
Cardiac Death • Cardiac death is the irreversible cessation of cardiac function • If a potential donor meets donation after circulatory death (DCD) criteria, all organs except the heart may be donated • Eyes and tissues may be donated Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Deceased Donor Evaluation • • Age, height and weight Date, time and cause of death Medical record review History from family member or best historian Physical exam Social history ABO Serologies (HIV, Hepatitis B, Hepatitis C, CMV, RPR, EBV) Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Types of Living Donation • Living donors donate an organ or part of an organ in which the remaining organ can regenerate or take on the workload of the rest of the organ (primarily single kidney donation or partial donation of liver) • Living donors can be family members, good Samaritan (altruistic), or family members of another patient on the transplant waiting list (paired exchange, or domino transplant) • In living donation cases, donor safety is paramount, extensive medical and social evaluations are performed to ensure the health of the donor Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
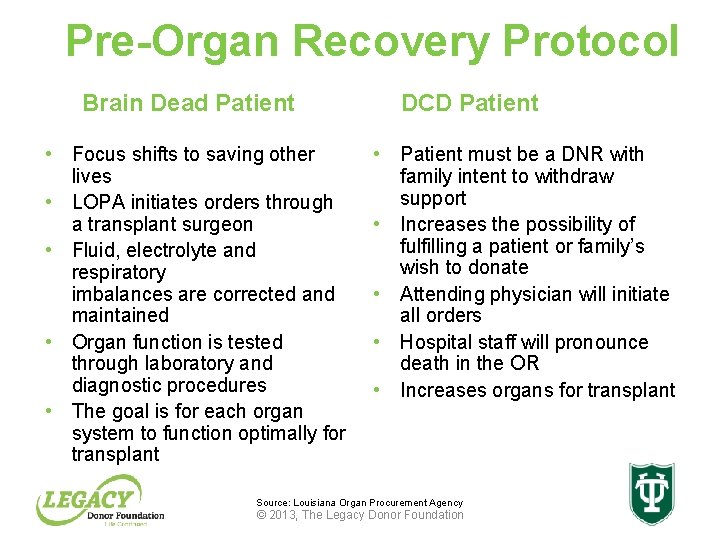
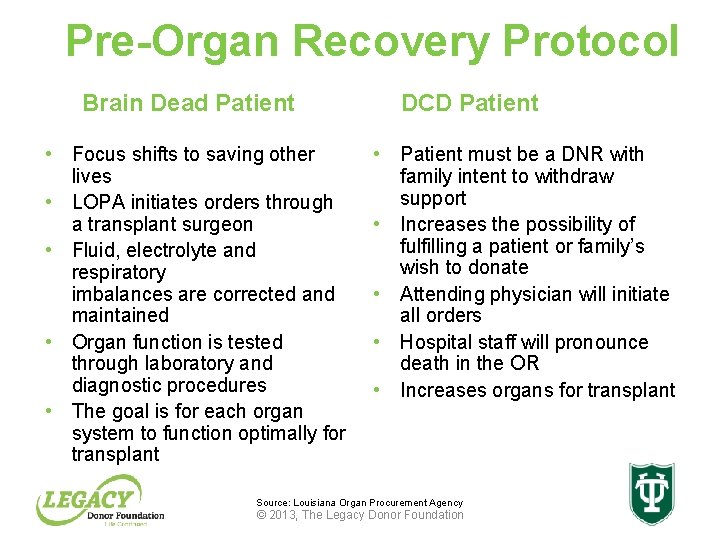
Pre-Organ Recovery Protocol Brain Dead Patient • Focus shifts to saving other lives • LOPA initiates orders through a transplant surgeon • Fluid, electrolyte and respiratory imbalances are corrected and maintained • Organ function is tested through laboratory and diagnostic procedures • The goal is for each organ system to function optimally for transplant DCD Patient • Patient must be a DNR with family intent to withdraw support • Increases the possibility of fulfilling a patient or family’s wish to donate • Attending physician will initiate all orders • Hospital staff will pronounce death in the OR • Increases organs for transplant Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
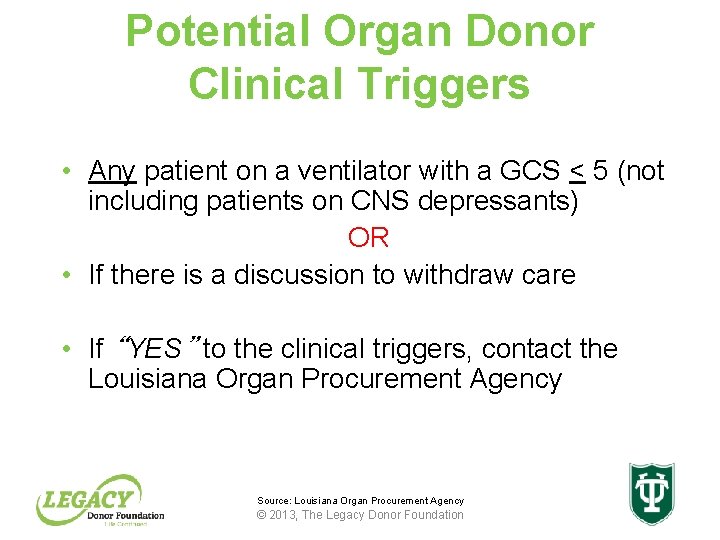
Potential Organ Donor Clinical Triggers • Any patient on a ventilator with a GCS < 5 (not including patients on CNS depressants) OR • If there is a discussion to withdraw care • If “YES” to the clinical triggers, contact the Louisiana Organ Procurement Agency Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
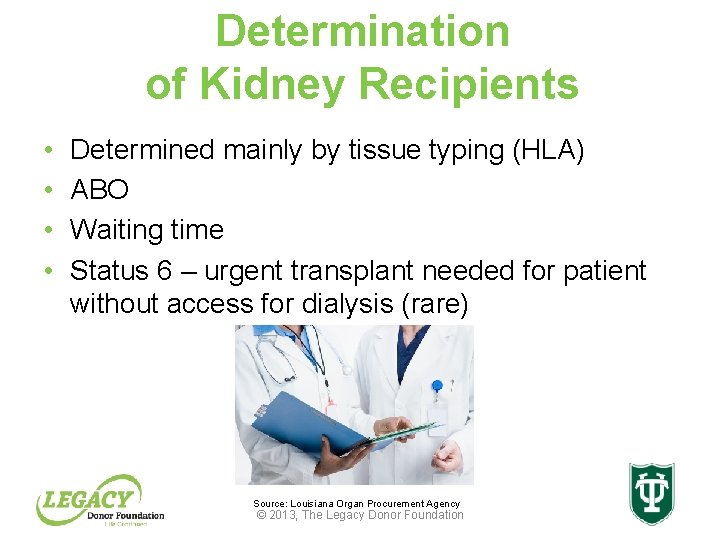
Determination of Kidney Recipients • • Determined mainly by tissue typing (HLA) ABO Waiting time Status 6 – urgent transplant needed for patient without access for dialysis (rare) Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
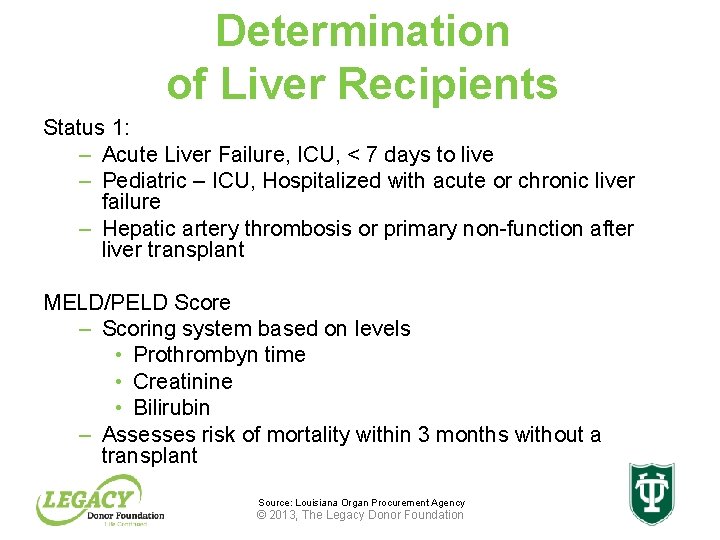
Determination of Liver Recipients Status 1: – Acute Liver Failure, ICU, < 7 days to live – Pediatric – ICU, Hospitalized with acute or chronic liver failure – Hepatic artery thrombosis or primary non-function after liver transplant MELD/PELD Score – Scoring system based on levels • Prothrombyn time • Creatinine • Bilirubin – Assesses risk of mortality within 3 months without a transplant Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Contraindications to Organ Transplant • Irreversible other organ disease • Severe cardio/pulmonary disease (except for heart/lung transplant) • Active infection • AIDS • Malignancy – (extra hepatic for Liver Transplant) • Uncontrolled psychiatric illness • Absence of psychosocial support structure • Noncompliance/non adherence Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
482. 45 Medicare Conditions of Participation • Hospitals must have a written agreement with their OPO (LOPA for Louisiana) • All deaths or imminent deaths must be referred to LOPA in a timely manner • Hospital staff must be trained by LOPA on donation issues • Any individual who provides information about donation to a family must be a trained designated requestor Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
482. 45 Medicare Conditions of Participation • Continuous Quality Improvement is a cooperative effort • Families of potential donors are to be treated with the utmost discretion and sensitivity during the approach process • Hospitals must ensure that potential donors are maintained in a manner that maintains the viability of their organs Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
HIPAA- Privacy Regulations Section 164. 512(h) Allows Covered Entities (your hospital) to: – Initiate contact with organ and tissue organizations (LOPA) and disclose protected health information to facilitate donation and transplantation Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Tissue Donor Referral • Death must be reported to LOPA within 4 hours • The Clinical Support Center will: – Screen patient for suitability and check the Donor Registry – Need Legal Next of Kin (LNOK) information such as name, phone number, and relationship to deceased – Notification of death paperwork must be completed and placed in patient chart. – Patients should not be released to the funeral home prior to their family making a decision in regards to donation Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Consent • Louisiana has a first person consent registry • This allows citizens to make legally binding decisions to register as donors • Family consent is required only for minors • If the potential donor is not registered, only then is consent of the legal next of kin required Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Timely Notification • Potential donors must be referred to LOPA ideally within 1 hour of a documented GCS<5 and prior to withdrawal of life sustaining therapies • Contact LOPA at (800) 833 -3666 • Have patient chart available • Notification must be documented in the patient’s medical record Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Why Is Timely Notification Important? • LOPA can assist the nurses/physician in preparing the family for end of life decisions • Avoids approaches that are in the wrong place at the wrong time and with inadequate information • Allows for ample time to work with coroner • LOPA will access the LA Donor Registry Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Organ Recovery • The donation process can take 12 -36 hours • The patient remains in the critical care area and their care is managed by LOPA • Your role in caring for the patient continues, however now you are potentially caring for nine patients • Once the organs are deemed suitable for transplant they are then allocated and when accepted an operating room time is scheduled at the donor hospital Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
Organ Recovery Facts Organs differ in the amount of time they can be without perfusion: • Heart and Lungs have 4 -6 hours • Liver has 12 -15 hours • Kidneys have up to forty eight hours – kidney pump machine used to increase kidney viability Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
The Tissue Recovery After consent – A medical/behavioral questionnaire is completed – Coroner clearance obtained – Blood is drawn and sent for screening – An operating room time is set or the patient is transported to the LOPA tissue recovery suite – Tissues are recovered by tissue recovery technicians – The donor is prepared appropriately for funeral services – The funeral home and coroner are contacted upon completion of case Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
What Happens After Donation? • Family support continues with a phone call within 10 days after donation • Within 30 days family and hospital staff receive a letter regarding the outcome of the donation • Donor family members and recipients can meet if both parties wish to have contact • Support then continues as long as a family requests it Source: Louisiana Organ Procurement Agency © 2013, The Legacy Donor Foundation
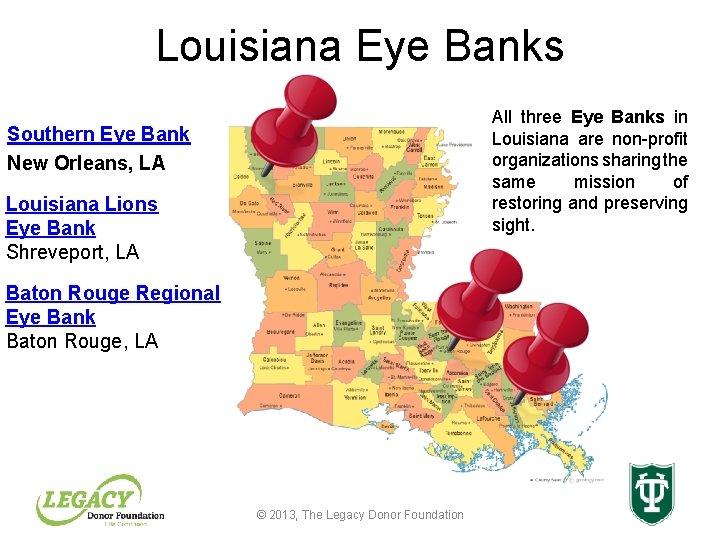
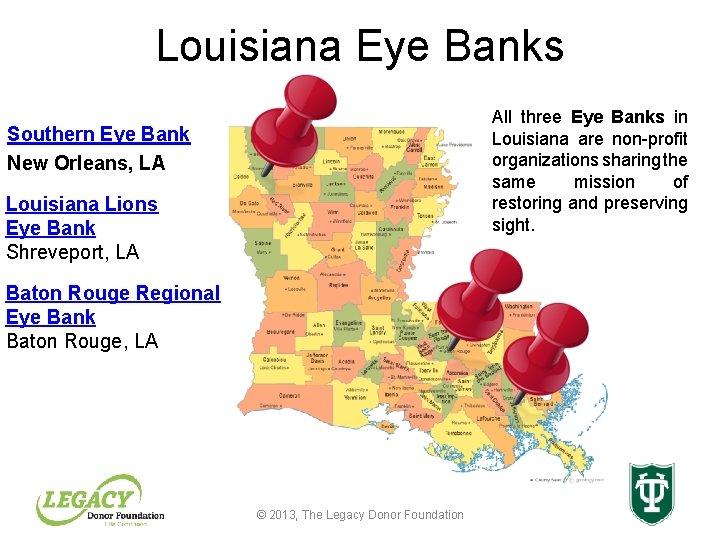
Louisiana Eye Banks All three Eye Banks in Louisiana are non-profit organizations sharing the same mission of restoring and preserving sight. Southern Eye Bank New Orleans, LA Louisiana Lions Eye Bank Shreveport, LA Baton Rouge Regional Eye Bank Baton Rouge, LA © 2013, The Legacy Donor Foundation
Eye Donation Protocol • Eye Donation follows the same protocol for recovery as tissue donation with the exception of recovery site and recovery times • Eye Donation can take place in a health care institution, funeral home, coroner’s office or similar locations • Eye Tissue must be recovered as soon as possible. Time limitations are between 12 and 24 hours depending upon the location and temperature of the donor © 2013, The Legacy Donor Foundation
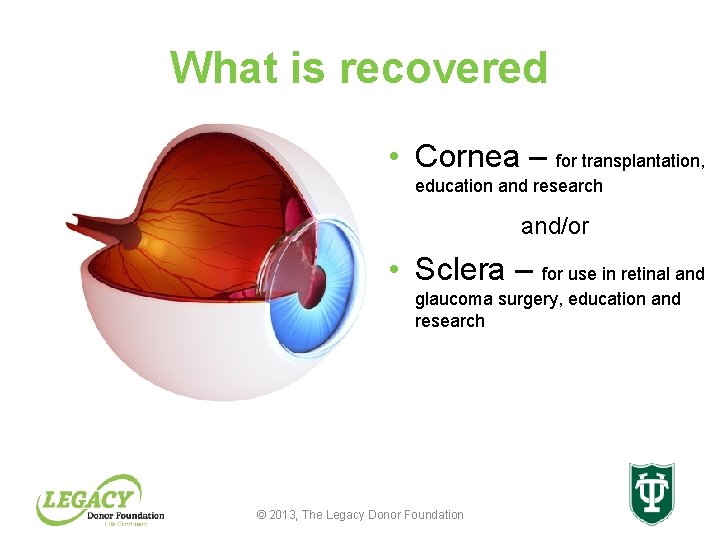
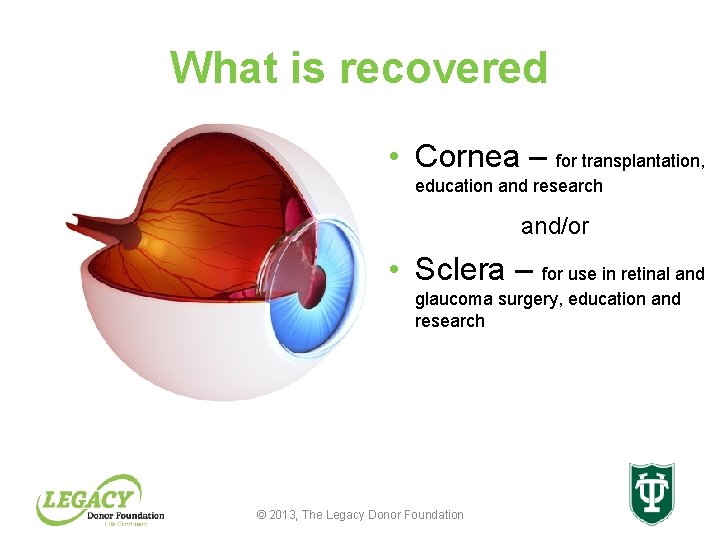
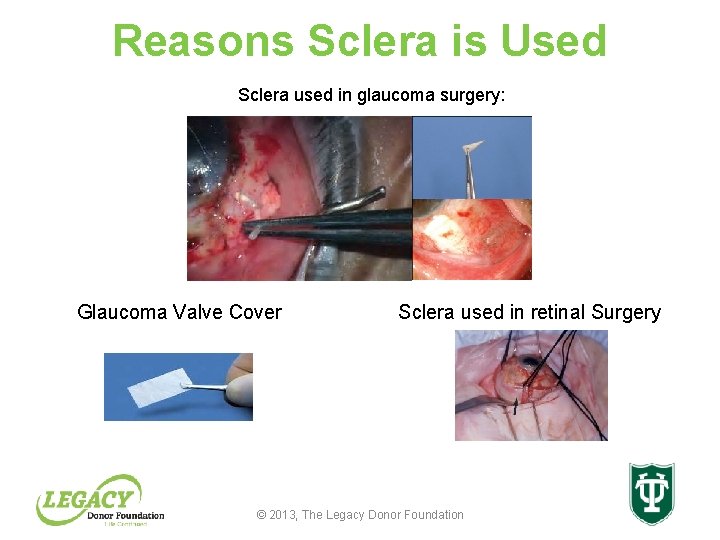
What is recovered • Cornea – for transplantation, education and research and/or • Sclera – for use in retinal and glaucoma surgery, education and research © 2013, The Legacy Donor Foundation
Reasons for Corneal Transplantation • Optical: To improve the optical qualities of the cornea and improve vision by replacing a damaged cornea with a healthy, clear one • Reconstructive: To reconstruct a perforated cornea and to preserve the eye in its whole form • Therapeutic: To treat a disease unresponsive to medical management or to alleviate pain © 2013, The Legacy Donor Foundation
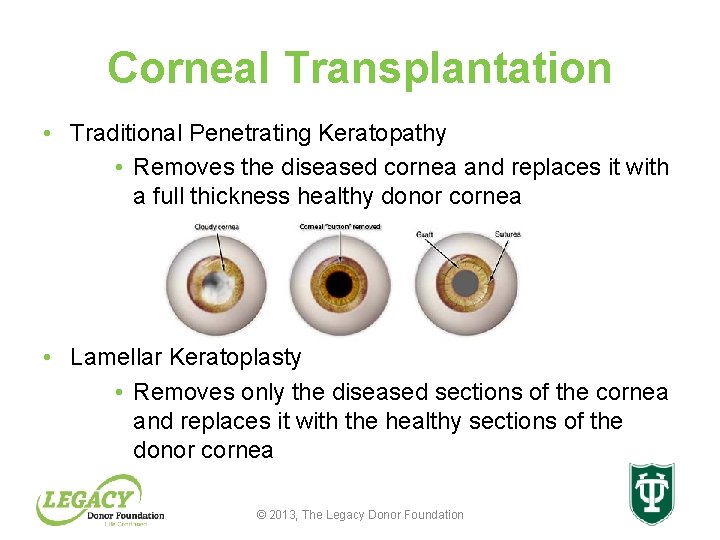
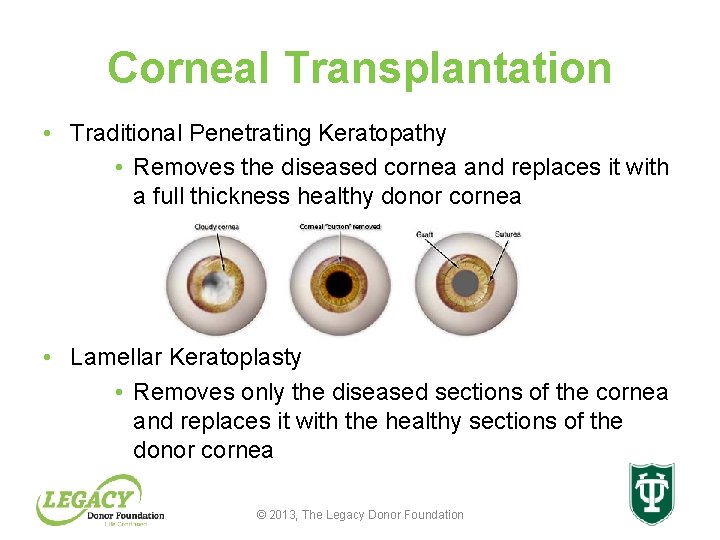
Corneal Transplantation • Traditional Penetrating Keratopathy • Removes the diseased cornea and replaces it with a full thickness healthy donor cornea • Lamellar Keratoplasty • Removes only the diseased sections of the cornea and replaces it with the healthy sections of the donor cornea © 2013, The Legacy Donor Foundation
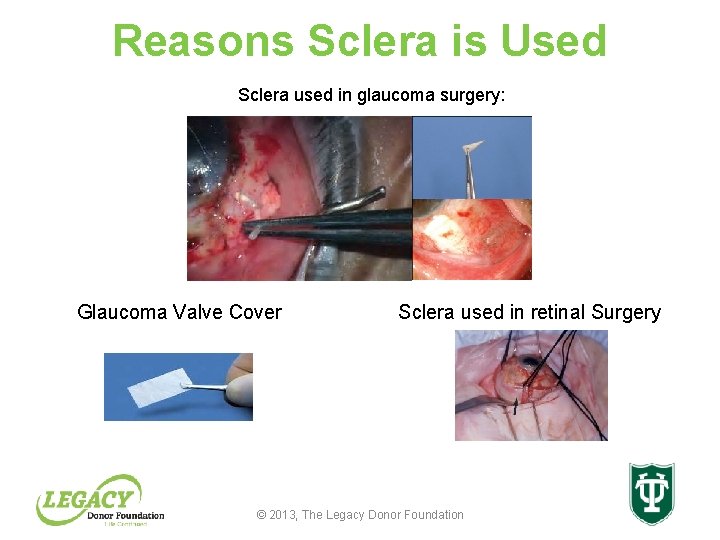
Reasons Sclera is Used Sclera used in glaucoma surgery: Glaucoma Valve Cover Sclera used in retinal Surgery © 2013, The Legacy Donor Foundation
Blindness Stats • There are more than 100 million people who suffer from corneal blindness – Less than 100, 000 corneal transplants are performed worldwide due to lack of tissue, lack of facilities and lack of physicians • 4 -5 million people suffer from glaucoma © 2013, The Legacy Donor Foundation
Distribution Process • Average time of transplantation of recovered tissue is 3 -4 days post recovery… • Most cornea transplants are scheduled surgeries therefore: – Local emergent patients are provided ocular tissue first – Non-local emergent patients are provided ocular tissue second – Local scheduled surgeries are offered third – Non-local and international doctors (Private practice, academic institution and missionary trips) are offered excess tissue © 2013, The Legacy Donor Foundation
Valued Gift • The Gift of ocular tissue is always used to the best of the eye bank’s ability • If tissue cannot be used for transplantation, the tissue will be offered to researchers and eye bank staff for education and research needs • More than 800 corneal transplants were performed in Louisiana in 2012 • More than 45, 000 people receive a corneal transplant in the United States • Approximately 90, 000 receive a corneal transplant worldwide • The need for ocular tissue is never satisfied © 2013, The Legacy Donor Foundation
Discussion With Your Patients As a medical professional, it is important for you to: – Be able to discuss various advanced directives with your patients – Assist patients with understanding the process of organ, eye and tissue donation – Encourage patients to make an informed decision about donation – Encourage patients to share their wishes with their family and friends © 2013, The Legacy Donor Foundation
Discussion with Your Patients • Many people are unaware of the critical need for organ, eye and tissue donation, and have therefore not considered the opportunity to donate • Others have learned about donation through unreliable sources such as medical dramas, or sensationalized news articles – These sources can encourage misconceptions about donation © 2013, The Legacy Donor Foundation
Discuss Donation With Your Patients • As a medical professional, your patients look to you for guidance with their end of life directives and living wills • Answering questions about donation should be part of your discussion with your patients • During these discussions, you can provide them with facts about donation rather than perpetuating myths and misconceptions, and encourage them to register as organ, eye and tissue donors © 2013, The Legacy Donor Foundation
Remember… • Organ, eye and tissue donation is the gift of life • Transplants offer patients a new chance at healthy, productive and normal lives and return them to their families, friend and communities • One organ, eye and tissue donor can save up to 9 lives, restore sight to 2 people and enhance the lives of 50 more through tissue donation • Talk with your patients about organ donation facts and encourage them to register at: Donate. Life. La. org or 1 -800 -404 -0708 © 2013, The Legacy Donor Foundation
How to Register • Say “yes” when getting or renewing driver’s license • Register at www. Donate. Life. LA. org © 2013, The Legacy Donor Foundation
Contact Information If you have questions regarding this activity, please contact Legacy Donor Foundation or Tulane University Center for Continuing Education: Legacy Donor Foundation 2701 Kingman Street, Suite 101 Metairie, LA 70006 Telephone: (504) 558 -8900 Fax: (504) 558 -8999 Email: info@organawareness. org Center for Continuing Education Tulane University Health Sciences Center 1430 Tulane Avenue, TB 51 New Orleans, LA 70112 -2699 Telephone: (504) 988 -5466 Fax: (504) 988 -1779 Email: cme@tulane. edu http: //tulane. edu/cce © 2013, The Legacy Donor Foundation
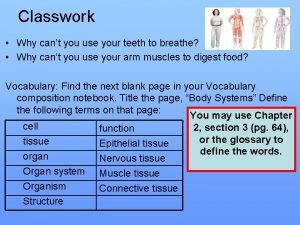
 Cell tissue organ organ system organism
Cell tissue organ organ system organism Cells group together to form
Cells group together to form Disadvantage of organ donation
Disadvantage of organ donation Utilitarianism organ donation
Utilitarianism organ donation Organ donation case studies
Organ donation case studies Definition of nursing who
Definition of nursing who Organ and organ system
Organ and organ system Organ organ penyusun sistem pencernaan
Organ organ penyusun sistem pencernaan Tractus respiratorius
Tractus respiratorius Keratomalasi
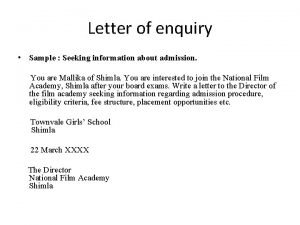
Keratomalasi Sample of enquiry letter
Sample of enquiry letter Equal area criterion examples
Equal area criterion examples Cell tissue organ system body
Cell tissue organ system body Examples of bird's eye view
Examples of bird's eye view Life membership fees in income and expenditure account
Life membership fees in income and expenditure account How is aerolar tissue different than aerenchyma tissue?
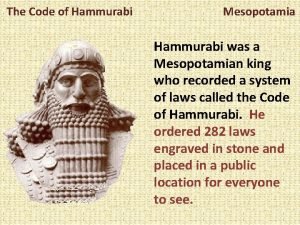
How is aerolar tissue different than aerenchyma tissue? Hammurabi mesopotamia
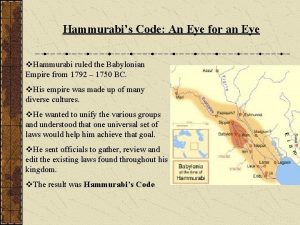
Hammurabi mesopotamia An eye for an eye hammurabi
An eye for an eye hammurabi Pf
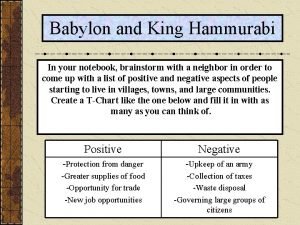
Pf Hammurabi's code activity
Hammurabi's code activity An eye for an eye a tooth for a tooth sister act
An eye for an eye a tooth for a tooth sister act Blue eyes genetics
Blue eyes genetics An eye for an eye meaning
An eye for an eye meaning Every eye is an eye
Every eye is an eye Hcp segment
Hcp segment Physician recruitment onboarding and retention
Physician recruitment onboarding and retention Blood donation disqualifications
Blood donation disqualifications Egg donation nashville
Egg donation nashville Donation project proposal
Donation project proposal Blood donation process flow chart
Blood donation process flow chart Akshaya patra donation online
Akshaya patra donation online Vedmata gayatri trust donation
Vedmata gayatri trust donation Unilatral
Unilatral Xilinx donation program
Xilinx donation program Pintos manual
Pintos manual Sperm donation greensboro nc
Sperm donation greensboro nc Blood donation definition
Blood donation definition Donation committee
Donation committee Everyday hero donation
Everyday hero donation Blood donation form
Blood donation form Pintos priority donation solution
Pintos priority donation solution 29 cfr 1910 regarding face head foot and hand protection
29 cfr 1910 regarding face head foot and hand protection A physician claims that joggers maximum volume
A physician claims that joggers maximum volume Physician reentry programs
Physician reentry programs Physician consortium for performance improvement
Physician consortium for performance improvement Physician time study
Physician time study Physician competency reference set
Physician competency reference set Coalition for physician enhancement
Coalition for physician enhancement Jeannie watkins
Jeannie watkins Safer sign out form
Safer sign out form Elijah goodman prayers
Elijah goodman prayers Colorado physicians health program
Colorado physicians health program Physician burnout retreat
Physician burnout retreat Physician employment models
Physician employment models Popliteal artery
Popliteal artery Daniel stok
Daniel stok Family physician facts
Family physician facts University of new england physician assistant program
University of new england physician assistant program Physician personas
Physician personas Uscis civil surgeon locator
Uscis civil surgeon locator Ethics doctor patient relationship
Ethics doctor patient relationship Computerized physician order entry definition
Computerized physician order entry definition Oklahoma board of nursing supervising physician
Oklahoma board of nursing supervising physician A physician claims that joggers maximum volume
A physician claims that joggers maximum volume The good physician treats the disease
The good physician treats the disease Wellstar physicians group
Wellstar physicians group Stanford physician wellness survey
Stanford physician wellness survey Ohio association of physician assistants
Ohio association of physician assistants