Pharmacology in Nursing Womens Health Drugs Karen Ruffin




- Slides: 68

Pharmacology in Nursing Women’s Health Drugs Karen Ruffin RN, MSN Ed.
Female Reproductive Functions • Female sex steroid hormones – Estrogens – Progestins • Pituitary gonadotropin hormones – Follicle stimulating hormone (FSH) – Luteinizing hormone (LH)
Female Reproductive Functions (cont’d) • Development of primary and secondary sex characteristics • Menstrual cycle

Estrogens • Three major endogenous estrogens – Estradiol (principal & most active) – Estrone – Estriol • Synthesized from cholesterol in ovarian follicles • Basic chemical structure of a steroid

Exogenous Estrogenic Drugs– Synthetic • Steroidal – Conjugated estrogens, estradiol transdermal, many others • Nonsteroidal – Chlorotrianisene, diethylstilbestrol diphosphate, others – These drugs no longer available in the United States
Estrogens Required For • The development and maintenance of the female reproductive system • The development of female secondary sex characteristics
Estrogens: Indications • Treatment of or prevention of disorders that result from estrogen deficiency – Atrophic vaginitis – Hypogonadism – Oral contraception (given with a progestin) – Dysmenorrhea – “Hot flashes” of menopause
Estrogens: Indications (cont’d) • Treatment of or prevention of disorders that result from estrogen deficiency (cont’d) – Uterine bleeding – Palliative treatment of advanced breast and prostate cancer – Osteoporosis treatment and prophylaxis – Many other indications
Estrogens: Indications (cont’d) • Continuous-combined hormone replacement therapy (CCHRT) – Fixed estrogen/progestin combination products – Reduce complications, such as endometrial hyperplasia, that occur from using estrogen alone
Estrogens: Contraindications • • • Allergy to the medication Any estrogen dependent cancer Undiagnosed abnormal vaginal bleeding Pregnancy Active thromboembolic disorder or history
Estrogens: Adverse Effects • • Thrombolytic events—most serious Nausea—most common Hypertension, thrombophlebitis, edema Vomiting, diarrhea, constipation, abdominal pain • May cause photosensitivity, chloasma
Estrogens: Adverse Effects (cont’d) • Amenorrhea, breakthrough uterine bleeding • Tender breasts, fluid retention, headaches • Others
Progestins • Synthetic derivatives of progesterone – medroxyprogesterone (Provera) – hydroxyprogesterone – megestrol (Megace) – Many others
Progestins: Indications • Treatment of functional uterine bleeding caused by: – Hormonal imbalance, fibroids, or uterine cancer • Treatment of primary and secondary amenorrhea
Progestins: Indications (cont’d) • Palliative treatment of some cancers and endometriosis • Prevention of threatened miscarriage • Alleviation of symptoms of PMS
Progestins: Indications (cont’d) • megestrol – Adjunct therapy for treatment of breast and endometrial cancers – Also used for management of anorexia, cachexia, or unexplained weight loss in AIDS patients – Used to stimulate appetite and promote weight gain in patients with cancer • Used with estrogen replacement therapy after menopause
Progestins: Adverse Effects • Liver dysfunction—cholestatic jaundice • Thrombophlebitis, thromboembolic disorders, such as PE • Nausea, vomiting • Amenorrhea, breakthrough uterine bleeding, spotting • Edema, weight gain or loss • Others

Contraceptive Drugs • Medications used to prevent pregnancy • Oral medications – Monophasic, biphasic, and triphasic forms – Most contain estrogen-progestin combinations
Contraceptive Drugs (cont’d) • Other contraceptive forms available – Long-acting injectable form of medroxyprogesterone (Depo-Provera) – Transdermal contraceptive patch – Intravaginal contraceptive ring
Contraceptive Drugs: Mechanism of Action • Prevent ovulation by inhibiting the release of gonadotropins and increasing uterine mucous viscosity, resulting in: – Decreased sperm movement and fertilization of the ovum – Possible inhibition of implantation of a fertilized egg (zygote)
Contraceptive Drugs: Other Drug Effects • Improve menstrual cycle regularity • Decrease blood loss during menstruation • Decreased incidence of functional ovarian cysts and ectopic pregnancies
Contraceptive Drugs: Indications • Primarily used to prevent pregnancy • Other uses – Treatment of endometriosis and hypermenorrhea – To produce cyclic withdrawal bleeding – Postcoital emergency contraception
Contraceptive Drugs: Adverse Effects • Drawbacks to the use of these drugs include: – – Hypertension Thromboembolism, possible PE, MI, stroke Alterations in lipid and carbohydrate metabolism Increases in serum hormone concentrations • These effects are due to the estrogen component
Contraceptive Drugs: Adverse Effects (cont’d) • May also cause: – Edema, dizziness, headache, depression, nausea, vomiting, diarrhea, increased appetite, increased weight, breast changes, many others
Contraceptive Drugs: Interactions • Drugs that decrease effectiveness of oral contraceptive drugs – Antibiotics, barbiturates, isoniazid, rifampin, griseofulvin
Contraceptive Drugs: Interactions (cont’d) • Drugs that may have reduced effectiveness if given with oral contraceptive drugs – Anticonvulsants, beta-blockers, hypoglycemic drugs, oral anticoagulants, theophylline, TCAs, vitamins, hypnotics
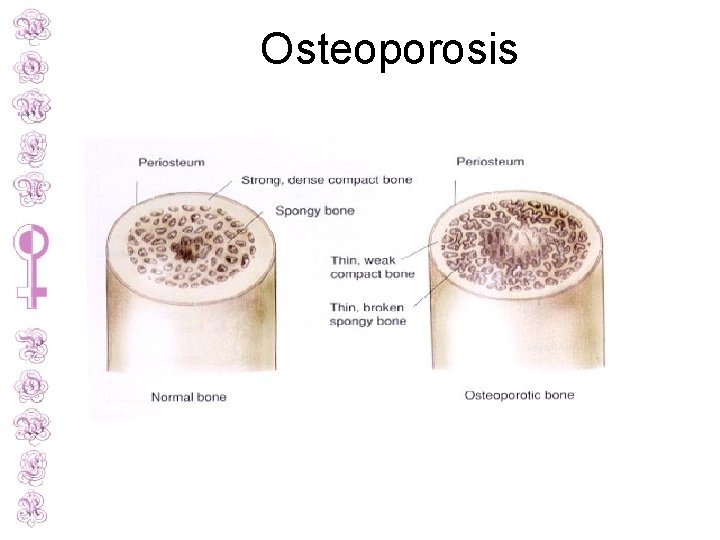
Osteoporosis • Low bone mass • Increased risk of fractures • Primarily affects women • 20% of those with this condition are men
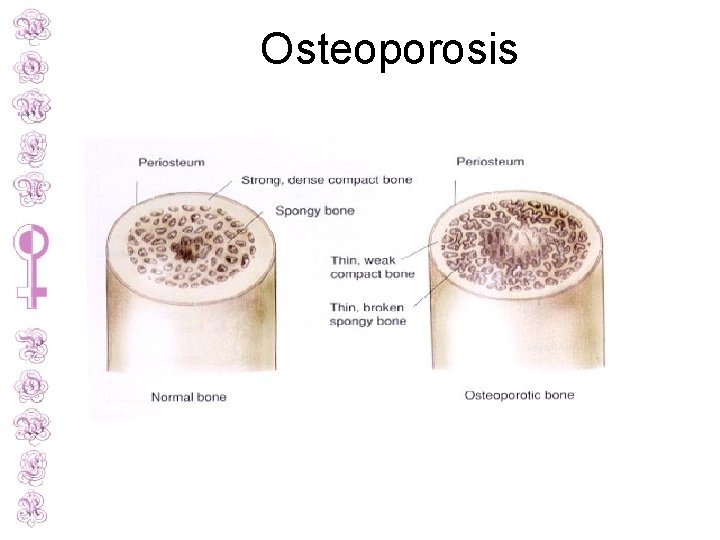
Osteoporosis
Osteoporosis: Risk Factors – Caucasian/Asian descent – Slender body build – Early estrogen deficiency – Smoking – Alcohol consumption – Low-calcium diet – Sedentary lifestyle – Family history
Drug Therapy for Osteoporosis • Calcium supplements and vitamin D may be recommended for women at high risk for osteoporosis
Drug Therapy for Osteoporosis (cont’d) – Bisphonates • alendronate (Fosamax), ibandronate (Boniva), risedronate (Actonel) – Selective estrogen receptor modifier (SERM) • raloxifene (Evista) – Hormone • calcitonin • teriparatide (Forteo)
Drug Therapy for Osteoporosis (cont’d) Biphosphonates • Work by inhibiting osteoclast-mediated bone resorption, thus preventing bone loss SERMs • Stimulate estrogen receptors on bone and increasing bone density
Drug Therapy for Osteoporosis (cont’d) calcitonin – Directly inhibits osteoclastic bone resorption teriparatide – Only drug that stimulates bone formation – Derivative of parathyroid hormone – Action similar to natural parathyroid hormone
Drug Therapy for Osteoporosis: Indications • Bisphonates and calcitonin – Both prevention and treatment of osteoporosis – Biphosphanates also used for glucocorticoidinduced osteoporosis and Paget’s disease
Drug Therapy for Osteoporosis: Indications (cont’d) • raloxifene – Prevention of postmenopausal osteoporosis • teriparatide – Used for those with highest risk of fracture (prior history of fractures)
Drug Therapy for Osteoporosis Adverse Effects • SERMs – Hot flashes, leg cramps – Can increase risk of venous thromboembolism – Not used if patient is near age of menopause due to possible hot flashes – Leukopenia
Drug Therapy for Osteoporosis Adverse Effects (cont’d) • Bisphonates – Headache, GI upset, joint pain – Risk of esophageal burns if medication lodges in esophagus before reaching the stomach
Fertility Drugs • Various medical techniques used to treat infertility • Include: – in vitro fertilization – Medication therapy: ovulation stimulation
Fertility Drugs (cont’d) • clomiphene (Clomid, others) – Nonsteroidal ovulation stimulant – Blocks estrogen receptors in the uterus and brain, resulting in a false signal of low estrogen levels
Fertility Drugs (cont’d) • Clomiphene (Clomid, others) (cont’d) – Causes increased production of Gn-RH, FSH, and LH – As a result, maturation of ovarian follicles is stimulated, leading to ovulation and increased chance of conception
Fertility Drugs (cont’d) • Mentropins (Pergonal) – Standardized mixture of FSH and LH – Stimulates development of ovarian follicles, leading to ovulation – May also be given to men to stimulate spermatogenesis
Fertility Drugs (cont’d) • chorionic gonadotropin alfa (Ovidrel) – Recombinant form of human chorionic gonadotropin – Causes rupture and ovulation of mature ovarian follicles, and maintenance of corpus luteum – Used to stimulate ovulation
Fertility Drugs: Indications • Used primarily to induce ovulation in anovulatory patients • Also may be used to promote spermatogenesis in infertile men
Fertility Drugs: Adverse Effects • Tachycardia, phlebitis, DVT • Dizziness, headache, flushing, depression, anxiety, nervousness, fatigue • Nausea, bloating, constipation, others • Ovarian hyperstimulation, multiple pregnancies, blurred vision, breast pain, others
Uterine-Active Medications • Medications used to alter uterine contractions • Used to: – Promote labor – Prevent the start or progression of labor – Postpartum use: to reduce the risk of postpartum hemorrhage
Uterine Stimulants Also called oxytocics • • Ergot derivatives Prostaglandins Progesterone antagonist oxytocin (hormonal drug)
Uterine Stimulants (cont’d) Ergot alkaloids • Increase force and frequency of uterine contractions • Used after delivery of the infant and placenta to prevent postpartum uterine atony and hemorrhage • methylergonovine (Methergine)
Uterine Stimulants (cont’d) Prostaglandins • Natural hormones • Cause potent contraction of myometrium, smooth muscle fibers of the uterus • Used to induce labor by softening the cervix and enhancing uterine muscle tone • dinoprostone (Prostin E 2) and misoprostol (Cytotec)
Uterine Stimulants (cont’d) Progesterone antagonist • mifepristone (Mifeprex) • RU-486, the “abortion pill” • Stimulates uterine contractions to induce abortion • Given with a prostaglandin drug for elective abortions
Uterine Stimulants: oxytocin (Pitocin)—Synthetic Form • Used to induce labor at or near full-term gestation, and to enhance labor when contractions are weak and ineffective
Uterine Stimulants: oxytocin (Pitocin)—Synthetic Form (cont’d) • Other uses – Prevent or control postpartum uterine bleeding – Complete an incomplete abortion (after miscarriage) – Promote milk ejection during lactation
Uterine Stimulants: Adverse Effects • • • Hypotension or hypertension, chest pain Headache, dizziness, fainting Nausea, vomiting, diarrhea Vaginal pain, cramping Leg cramps, joint swelling, chills, fever, weakness, blurred vision
Uterine Relaxants: Tocolytics • Used to stop labor that begins before term to prevent premature birth • Generally used after the 20 th week of gestation
Uterine Relaxants: Tocolytics (cont’d) • Uterine contractions that occur between the 20 th and 37 th weeks of gestation are considered premature labor • Nonpharmacologic measures – Bedrest, sedation, hydration
Uterine Relaxants • ritodrine (Yutopar) and terbutaline (Brethine) – Beta-adrenergic drugs – Stimulation of beta 2 -adrenergic receptors on the uterine smooth muscle – Results in relaxation of the uterus, thus stopping premature contractions – “Off-label” use • Magnesium sulfate IV also used to stop labor
Uterine Relaxants: Adverse Effects • Palpitations, tachycardia, hypertension, others • Tremors, anxiety, insomnia, headache, dizziness, others • Nausea, vomiting, anorexia, bloating, diarrhea, constipation • Hyperglycemia, hypokalemia • Dyspnea, hyperventilation, others
Nursing Implications • Assess baseline VS, weight, blood glucose levels, renal and liver function studies • Assess whether the patient smokes • Assess history and medication history • Assess contraindications, including potential pregnancy
Nursing Implications (cont’d) • Before giving any uterine stimulants, assess the mother’s vital signs and fetal heart rate • Uterine relaxants are used when premature labor occurs between the 20 th and 37 th weeks of gestation
Nursing Implications (cont’d) • For biphosphonates, ensure that the patient has no esophageal abnormalities and can remain upright or in a sitting position for 30 minutes after the dose
Nursing Implications (cont’d) • Estrogens and progestins – Take the smallest dose needed – Give IM doses deep in large muscle masses, and rotate sites – Give oral doses with meals to reduce GI problems – Teach patient about correct selfadministration and what to do if a dose is missed
Nursing Implications (cont’d) • Estrogens and progestins (cont'd) – Increased susceptibility to sunburn may occur—advise patient to wear sunscreen or avoid sunlight – Patients should report weight gain – Annual follow-up exams should be completed, including PAP smear and breast exam
Nursing Implications (cont’d) • Follow specific administration guidelines carefully for IV administration of uterine relaxants or stimulants • Monitor the patient’s vital signs and fetal condition during therapy
Nursing Implications (cont’d) • Instruct patient taking fertility drugs to take the medication as ordered • Recommend the patient keep a journal while on fertility drugs
Nursing Implications (cont’d) • Biphosphonates – Instruct patient to take medication upon rising in the morning, with a full glass of water, and 30 minutes before eating – Emphasize that the patient should sit upright for at least 30 minutes after taking the medication
Nursing Implications (cont’d) • SERMs – Instruct patient that the medication will need to be discontinued 72 hours before and during any prolonged immobility (such as surgery or a long trip)
Nursing Implications (cont’d) • Monitor for therapeutic responses • Monitor for adverse effects
 Karen ruffin
Karen ruffin Karen ruffin
Karen ruffin Karen ruffin
Karen ruffin Pharmacology of drugs acting on respiratory system
Pharmacology of drugs acting on respiratory system Adrenal drugs pharmacology
Adrenal drugs pharmacology Focus on pharmacology essentials for health professionals
Focus on pharmacology essentials for health professionals Lomotib
Lomotib Needs of adolescence
Needs of adolescence Womens rights
Womens rights Late night womens hour
Late night womens hour Claire paine
Claire paine Womens right
Womens right Differences between men's and women's soccer
Differences between men's and women's soccer Womens college kumbakonam
Womens college kumbakonam Womens college kumbakonam
Womens college kumbakonam Womens right
Womens right Womens shelter edmonton
Womens shelter edmonton Womens rights
Womens rights Fornix of vagina
Fornix of vagina Womens history month door
Womens history month door Womens community shelters
Womens community shelters Ballybeen womens centre
Ballybeen womens centre Scarborough womens centre
Scarborough womens centre Womens lacrosse helmets
Womens lacrosse helmets Bristol womens voice
Bristol womens voice Chapter 19 lesson 1 the role of medicines worksheet answers
Chapter 19 lesson 1 the role of medicines worksheet answers Good host law nj
Good host law nj Venipuncture radiologic technologist
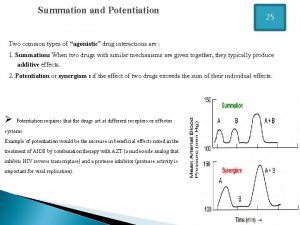
Venipuncture radiologic technologist Summation of drugs
Summation of drugs First order kinetics
First order kinetics What is ion trapping in pharmacology
What is ion trapping in pharmacology Metabolism of drug definition
Metabolism of drug definition Chapter 30 principles of pharmacology
Chapter 30 principles of pharmacology First pass effect drugs
First pass effect drugs What is pharmacology
What is pharmacology Advantages of iv route of drug administration
Advantages of iv route of drug administration First pass effect in pharmacology
First pass effect in pharmacology Receptors in pharmacology
Receptors in pharmacology First pass effect in pharmacology
First pass effect in pharmacology Basic principles of pharmacology
Basic principles of pharmacology What is pharmacology
What is pharmacology Slidetodoc
Slidetodoc Pharmacology introduction
Pharmacology introduction What is ion trapping in pharmacology
What is ion trapping in pharmacology Basic principles of pharmacology
Basic principles of pharmacology Chapter 15 diagnostic procedures and pharmacology
Chapter 15 diagnostic procedures and pharmacology Pharmacology for nurses: a pathophysiological approach
Pharmacology for nurses: a pathophysiological approach Respiratory pharmacology quiz
Respiratory pharmacology quiz Pharmacology module
Pharmacology module Hepatic extraction ratio formula
Hepatic extraction ratio formula Clinical pharmacology powered by clinicalkey
Clinical pharmacology powered by clinicalkey Pharmacology pay
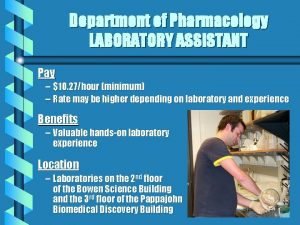
Pharmacology pay Pharmacology definition
Pharmacology definition Toxicology and applied pharmacology
Toxicology and applied pharmacology Rationale meaning in pharmacology
Rationale meaning in pharmacology Pharmacology chapter 1
Pharmacology chapter 1 Pharmacology tutor anderson
Pharmacology tutor anderson Clinical pharmacology
Clinical pharmacology Basic & clinical pharmacology
Basic & clinical pharmacology Dopamine synthesis
Dopamine synthesis Objectives of pharmacology
Objectives of pharmacology Pharmacology for veterinary technicians
Pharmacology for veterinary technicians Analglesia
Analglesia Clinical pharmacology residency
Clinical pharmacology residency Annual review of pharmacology and toxicology
Annual review of pharmacology and toxicology Dopamine pharmacology
Dopamine pharmacology Define pharmacology
Define pharmacology Essential drug concept in pharmacology
Essential drug concept in pharmacology Reductinist
Reductinist